Key Clinical Message
A 64‐year‐old female presented with malaise and fever 11 days after a closed, minimally displaced humerus surgical neck fracture. MR imaging revealed an abscess around the fracture, which is a very rare occurrence in adults. Two open debridements and IV antibiotics eradicated the infection. Reverse total shoulder arthroplasty was eventually performed for fracture nonunion.
Keywords: abscess, acute osteomyelitis, fracture nonunion, infection, proximal humerus fracture
Coronal MR image of the right shoulder showing abscess formation within and around a closed fracture of the proximal humerus.
1. INTRODUCTION
Deep infection at the site of an acute closed fracture is very rare in an adult. In fact, we were able to identify just 15 adult cases of osteomyelitis occurring acutely at the site of any closed appendicular bone fracture since the late 1950s (Table 1). 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Of the 15 cases, only five were at the site of proximal humerus, similar to our patient. 3 , 5 , 6 , 7 , 8 Immunosuppression appears to be a major risk factor in these cases. 12 , 13
TABLE 1.
Acute infections of closed fractures (appendicular bones) in adults.
| Reference | Patient age, sex | Fracture/infection site | Time from injury | Possible primary infection source | Organism | Factors affecting infection resistance | Antibiotic treatment a | Outcome |
|---|---|---|---|---|---|---|---|---|
| Cozen 1958 a | Adult, F | Proximal tibia | 5.5 months | NA | Staphylococcus sp. | NA | NA | Nonunion |
| 60, M | Femoral neck | 5 months | NA | Pseudomonas sp. | Rheumatoid arthritis | Polymyxin | Femoral head resection | |
| Watson and Whitesides 1976 | 58, F | Humeral neck | 4 days | NA | Penicillin‐resistant Staphylococcus aureus | Chronic alcoholism | Nafcillin | Likely humeral head resection |
| 61, F | Humeral neck | 20 days | NA | Group B beta‐hemolytic Streptococcus | Diabetes | Penicillin | Likely humeral head resection | |
| 96, F | Femoral neck | 12 days | NA | Klebsiella pneumoniae | NA | Gentamicin, penicillin | Femoral head resection | |
| 59, M | Humeral neck | 22 days | NA | Bacteroides | Diabetes | Primarily polymixcin and kanamycin; chloramphenicol, tetracycline and nitrofurantoin | Died | |
| Aluisio and Scully 1996 | 61, F | Humeral neck | 6 weeks | NA | Salmonella enteriditis & Methicillin‐resistant Staphylococcus aureus | Diabetes | Ciprofloxacin, vancomycin | Humeral head and shaft resection (8 cm) |
| Baskaran et al. 2004 | 38, F | Femoral diaphysis | 15 days | NA | Methicillin‐sensitive Staphylococcus aureus | NA | Gentamicin‐impregnated beads, cloxacillin | 2 cm shorter limb |
| Martínez et al. 2006 | 88, M | Humeral neck | 8 days | Indwelling catheter | Escherichia coli | Bladder carcinoma | Amoxicillin/clavulanate, ciprofloxacin, clindamycin, cotrimoxazole | Died |
| Weidle et al. 2009 a | 77, F | Distal radius | 3 days | Pneumonia | Group A beta‐hemolytic Streptococcus | Diabetes, bronchial carcinoma | Linezolid, meropenem, clindamycin | Died, necrotizing fasciitis |
| Kim and Tufesco 2012 | 31, F | Patella | 2 days | NA | Group A beta‐hemolytic Streptococcus | NA | Cefazolin, ceftriaxone, cefalexin | No long‐term deficits |
| Baruah et al. 2016 a | 50, M | Humeral diaphysis | 14 days | NA | Staphylococcus aureus | NA | Cephalosporin | Fibular graft |
| Kocutar et al. 2016 | 54, M | Clavicle | 24 days | Toe wound | Escherichia coli | Chronic alcoholism, smoker | Floxacillin, cefotaxime | Died |
| Gellman et al. 2018 | 28, M | Humeral diaphysis | 11 days | Chest tube, skin abrasions | Methicillin‐sensitive Staphylococcus aureus | NA | Cefazolin, gentamicin‐impregnated beads, cloxacillin, rifampicin | No long‐term deficits |
| Current case 2022 | 64, F | Humeral neck | 13 days | NA | Methicillin‐sensitive Staphylococcus aureus | Chronic alcoholism | Cefazolin, vancomycin impregnated absorbable calcium sulfate beads | Reverse total shoulder arthroplasty |
Abbreviations: F, female; humeral neck, surgical neck of the humerus; M, male; NA, not available/not known.
Dosage and duration of antibiotics not specified in original study.
We present the case of a 64‐year‐old female with chronic alcoholism who had osteomyelitis at the site of a closed minimally displaced surgical neck humerus fracture that resulted from a ground‐level fall (Figure 1). The infection was eradicated with two open surgical debridements and 6 weeks of intravenous (IV) antibiotics for the methicillin‐sensitive Staphylococcus aureus (MSSA) that grew in tissue cultures. At the second debridement, absorbable calcium sulfate beads loaded with tobramycin and vancomycin were implanted within and around the fracture site, but the fracture did not heal. A reverse total arthroplasty was ultimately done to restore shoulder function.
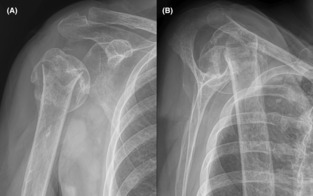
FIGURE 1.

Radiographs showing our patient's minimally displaced and mildly comminuted two‐part surgical neck humerus fracture in anterior–posterior (A, B) and lateral (C) views. Asterisks (*) indicate the coracoid process and arrows indicate the fracture. Mild lucency along the fracture site seems consistent with fracture of poor‐quality bone, but some readers might consider this as subtle lysis to be consistent with a subacute infection.
2. CASE PRESENTATION
A 64‐year‐old female with chronic alcoholism was admitted to a local hospital on September 6, 2020, after falling while intoxicated earlier that same day. Radiographs revealed a minimally displaced and mildly comminuted surgical neck fracture of the right humerus (Figure 1). Although examination of the radiographs revealed reduced bone density consistent with chronic alcoholism, 14 the admitting physicians and a radiologist concluded that the relatively obvious lytic changes that are typically seen in chronic osteomyelitis were not present. 15 , 16 After a 3‐day hospitalization that focused on correcting hyponatremia, she was discharged with the anticipation of nonoperative treatment.
At the initial hospitalization, white blood cell count was normal and there was no evidence of a urinary tract infection or other known or suspected location of a chronic infection. Inflammatory markers were not obtained. She was also afebrile and denied any prior fevers/chills/sweats or right shoulder or upper arm swelling, pain, or dysfunction.
She returned to the same hospital 7 days later with malaise, tactile fevers, chills, and increasing pain around the fracture site. Her vital signs included blood pressure of 104/71, oral temperature 36.1°C, pulse 78 beats/minute, respiratory rate 16/minute, and oxygen saturation at 97% (finger oximeter). Leukocytosis (28,000/mm3) and high C‐reactive protein at 36.1 (normal is <1 mg/dL) raised concern for emerging sepsis, prompting transfer to our tertiary medical center. Erythrocyte sedimentation rate (ESR) was normal at 18 (normal range 0–30 mm/hr). Blood cultures were obtained and a fluoroscopic aspiration of her right shoulder joint revealed mildly turbid non‐serosanguinous fluid. IV antibiotic (Zosyn®, piperacillin and tazobactam) treatment was started.
On the third hospital day at our tertiary hospital, MSSA grew from the blood and shoulder fluid samples, and an orthopedic consultation was requested. Arthroscopic debridement was then promptly done by JGS and revealed minimal evidence of infection (three milliliters of mildly turbid non‐serosanguinous fluid and mild glenohumeral synovitis). Additional cultures were not obtained from that debridement. A drain was placed in the glenohumeral joint and IV antibiotic (Zosyn®, piperacillin and tazobactam) treatment continued.
Thirty‐six hours later, grossly purulent fluid in the drain prompted magnetic resonance (MR) scanning with and without intravenous contrast, which revealed a large collection of fluid around and within the fracture site, consistent with osteomyelitis with abscess (Figures 2 and 3). An MRI scan was not obtained earlier, which in retrospect was unfortunate because this delayed definitive control of the source of the infection (discussed further below as a shortcoming in the work‐up of our patient's case). Open and arthroscopic surgical debridement was then done and revealed 30 mL of pus around and within the fracture site. A small tear in the glenohumeral capsule explained how purulent fluid entered the glenohumeral joint. Using a deltopectoral approach, the anterior aspect of the fracture was elevated to allow for debridement of the pus in the medullary region and for the insertion of a hand‐made dowel‐like structure (approximately 7 cm x 0.9 cm) consisting of polymethyl methacrylate (PMMA) cement. This was loaded with tobramycin powder (1.2 g) and vancomycin powder (1.0 g). Antibiotic‐containing PMMA beads (~8 mm diameter) were also placed around the fracture.
FIGURE 2.
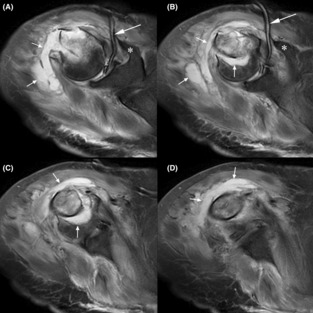
Sequential T2 (fluid enhancing) MR images in coronal view (A is most proximal, D is most distal). Asterisks (*) indicate the coracoid process, longer arrows indicate a Jackson–Pratt drain within the glenohumeral joint (A, B), and shorter arrows indicate the abscess. The abscess clearly extends into the medullary region of the bone at the fracture site (e.g., vertical arrows in B and C). The scan was obtained 13 days after the fracture.
FIGURE 3.

T2 MR images in axial view (A is most posterior, B is just anterior to A, and C is most anterior). Asterisks (*) indicate the coracoid process and the long arrows indicate the Jackson–Pratt drain and the short arrows indicate the abscess. The scan was obtained 13 days after the fracture.
The PMMA beads were removed several days later and were replaced with 30 mL of ~3 mm diameter absorbable calcium sulfate beads containing vancomycin and tobramycin (Stimulan®, Biocomposites Ltd., Keele, United Kingdom). To maintain placement of the beads at the fracture site, the medullary canal was occluded with Gelfoam® (sterile absorbable gelatin sponge; Pfizer Inc., USA). About 75% of the calcium sulfate beads were then manually packed into the humerus fracture site. The remaining beads were packed around the fracture site (Figure 4). Although stabilization of the fracture with open reduction and internal fixation (ORIF) can help eradicate a bone infection, 17 we used an alternative method because concerns for bacterial colonization on the hardware and fixation failure due to the poor‐quality bone. The alternative method utilized holes drilled in the anterior, anteromedial, and anterolateral humeral neck and shaft, and figure‐of‐eight (tension band) suturing using No. 2 antibiotic‐containing resorbable monofilament polydioxanone suture, 18 which reduces the chance of bacterial colonization. 19 , 20
FIGURE 4.

Anterior–posterior (A) and lateral (B) radiographs obtained at 2 weeks after the final debridement surgery (skin staples can be seen). The intramedullary calcium sulfate beads are indicated by the arrows. Note some of the beads subsided into the proximal diaphyseal medullary canal.
Treatment of the MSSA grown in tissue cultures included IV cefazolin that was given for 6 weeks after the final debridement surgery. The fracture did not heal, the nonunion became painful, and radiographs obtained 4 months later showed a pseudoarthrosis (Figure 5). On February 2, 2021, open surgery was performed to obtain multiple tissue specimens from the nonunion site for cultures in order to rule‐out infection in anticipation for reconstructive surgery. 21 There was no growth of these multiple cultures at 14 days of incubation.
FIGURE 5.
Anterior–posterior (A) and lateral (B) radiographs obtained at 4 months after the final debridement surgery. The fracture is clearly a displaced atrophic nonunion and a pseudarthrosis has formed.
The patient then decided to seek future care at a local university medical center, which was prompted by her daughter who was employed at that institution. The surgeon at that facility performed a reverse total shoulder arthroplasty (RTSA) on May 19, 2021. At final follow‐up at 24 months after the RTSA (28 months after the final debridement surgery) there was no evidence of infection and the patient was very satisfied with her shoulder function and with her final outcome.
3. DISCUSSION
While osteomyelitis can occur in approximately 12%–20% of open fractures in adults, 22 , 23 the occurrence of osteomyelitis at the site of a closed fracture is very rare. Our literature review of PubMed and Google Scholar revealed only seven cases of adults who had closed humerus fractures that were complicated with what was reported as “acute osteomyelitis” 3 , 5 , 6 , 7 , 8 (Table 1). Of these seven cases, two were of the humeral diaphysis 3 , 8 and the other five occurred in the region of the humeral surgical neck. One case isolated penicillin‐resistant Staphylococcus aureus from the infected fracture site and was similar to our case (described further below). 7 Another case isolated methicillin‐resistant Staphylococcus aureus (MRSA) with concurrent Salmonella enteriditis, 5 and the remaining four cases reported other causative organisms, including MSSA, 3 Group B Streptococcus (Case 2 from 7 ), Bacteroides sp. (Case 5 from 7 ), and Escherichia coli. 6 S. aureus is the most common cause of osteomyelitis in adults. 1 , 2 , 24 , 25
In our case and in some of these prior cases, it is possible that the osteomyelitis was subacute or chronic, resulting in weakening of the bone. In this theoretical context, these fractures would be considered pathological. 26 , 27 In other words, if an intraosseous abscess was already present, then the acute fracture enabled its extraosseous dissemination. This seems unlikely in our patient because of the lack of (1) prior right upper arm or shoulder pain or swelling, (2) local or constitutional symptoms such as warmth, achiness, fevers, chills or sweats, (3) a known locus of chronic infection, 28 and (4) current or prior laboratory values and vital signs that could raise concern for infection. Additionally, within the 6 months prior her index right humerus fracture, our patient had MR scan of her contralateral (left) shoulder in order to evaluate for a rotator cuff tear after a fall. This suggests that MR scanning was readily available for evaluation of her right shoulder had there been significant symptoms in that region. Definitive proof that our patient's osteomyelitis was acute would require CT or MR scanning within days or a few weeks of the fracture and/or histological examination of the material from the acute fracture site or from the nascent infection site. 29 Neither of these was done in our patient's case.
The prior reported case that resembles our patient was a 58‐year‐old female that also: (1) was an alcoholic, (2) had a closed proximal humerus fracture from a ground‐level fall, and (3) had S. aureus (likely MSSA) as the causative organism (Case 1 in 7 ). Treatment then (early 1970s) did not include the use of absorbable calcium sulfate beads, and nonabsorbable tobramycin‐impregnated PMMA beads were just being introduced. Although that patient's infection was eradicated, humeral head resection was the treatment for the painful nonunion.
Although our patient's nonunion may have resulted from compromised blood flow at the time of fracture, 30 , 31 the displacement of fracture that was done to insert a PMMA dowel and to place calcium sulfate beads likely further perturbed blood flow. This is important because these beads require adequate blood supply to enable bone healing. 32 , 33 Surgical perturbation of the fracture site could have been avoided if the metaphyseal region had been debrided through a drill hole made near the supraspinatus tendon insertion. 34 Drilling in this location (as when employing intramedullary nailing for proximal two‐part humerus fractures) does not compromise humeral head blood flow. 35 Although this is an established method for debriding the medullary canal of the humerus and other long bones, 16 , 36 we felt that it would not have allowed for adequate debridement in our case (Figure 2).
4. CONCLUSION
We describe a rare case of an infection at the site of a closed acute proximal humerus fracture in an adult with chronic alcoholism. Whether or not this infection was acute, subacute, or chronic, it is rare to have a deep infection at the site of a closed fracture in an adult. When faced with similar circumstances of unexplained leukocytosis, malaise, fever, and increasing pain at a fracture site, and/or positive blood cultures in an immunocompromised patient, healthcare providers should consider immediate MR or CT scanning to help determine if an infection is present at the fracture site.
AUTHOR CONTRIBUTIONS
John G. Skedros: Conceptualization; data curation; investigation; supervision; writing – original draft; writing – review and editing. Tyler R. Smith: Data curation; writing – original draft; writing – review and editing. John T. Cronin: Data curation; writing – original draft; writing – review and editing.
FUNDING INFORMATION
No funding was obtained for this case report.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
ETHICAL APPROVAL
Each author certifies that his institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Skedros JG, Smith TR, Cronin JT. Osteomyelitis with abscess associated with acute closed upper humerus fracture in an adult: A case report. Clin Case Rep. 2023;11:e7640. doi: 10.1002/ccr3.7640
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Grigorian A, Schubl S, Scolaro J, et al. No increased risk of acute osteomyelitis associated with closed or open long bone shaft fracture. J Clin Orthop Trauma. 2019;10(Suppl 1):S133‐S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kocutar T, Snoj Z, Salapura V. Complicated acute haematogenous osteomyelitis with fatal outcome following a closed clavicle fracture‐a case report and literature review. BJR Case Rep. 2016;2(2):20150389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gellman YN, el‐Haj M, Khoury A, Weil YA. Closed humeral fracture complicated with acute hematogenous osteomyelitis: a case report. J Orthop Case Rep. 2018;8(2):61‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim C, Tufescu TV. Infection in closed fractures: a case report and literature review. JBJS Case Connect. 2012;2(3):e44. [DOI] [PubMed] [Google Scholar]
- 5. Aluisio FV, Scully SP. Acute hematogenous osteomyelitis of a closed fracture with chronic superinfection. Clin Orthop Relat Res. 1996;325:239‐244. [DOI] [PubMed] [Google Scholar]
- 6. Martίnez AR, Duca A, Rubio EM, Herreros MLV, Feito CR. Osteomielitis por Eschericia coli sobre fractura cerrada de húmero [in Spanish]. Anales de Medicina Interna (Madrid). 2006;23(12):588‐590. [DOI] [PubMed] [Google Scholar]
- 7. Watson FM, Whitesides TE Jr. Acute hematogenous osteomyelitis complicating closed fractures. Clin Orthop Relat Res. 1976;117:296‐302. [PubMed] [Google Scholar]
- 8. Baruah RK, Kumar S, Haque R. Acute osteomyelitis in closed fracture of adult humerus‐ case report and review of the literature. J Dental Med Sciences. 2016;15(3):31‐34. [Google Scholar]
- 9. Cozen L. Four unusual cases of osteomyelitis in adults. West J Surg Obstet Gynecol. 1958;66(1):36‐39. [PubMed] [Google Scholar]
- 10. Weidle PA, Brankamp J, Dedy N, Haenisch C, Windolf J, Jonas M. Complication of a closed Colles‐fracture: necrotising fasciitis with lethal outcome. A case report. Arch Orthop Trauma Surg. 2009;129(1):75‐78. [DOI] [PubMed] [Google Scholar]
- 11. Baskaran S, Nahulan T, Kumar AS. Close fracture complicated by acute haematogenous osteomyelitis. Med J Malaysia. 2004. 59(Suppl F):72‐74. [PubMed] [Google Scholar]
- 12. Wald ER. Risk factors for osteomyelitis. Am J Med. 1985;78(6B):206‐212. [DOI] [PubMed] [Google Scholar]
- 13. Thein R, Tenenbaum S, Chechick O, Leshem E, Chechik A, Liberman B. Delay in diagnosis of femoral hematogenous osteomyelitis in adults: an elusive disease with poor outcome. Isr Med Assoc J. 2013;15(2):85‐88. [PubMed] [Google Scholar]
- 14. Berg KM, Kunins HV, Jackson JL, et al. Association between alcohol consumption and both osteoporotic fracture and bone density. Am J Med. 2008;121(5):406‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Prodinger PM, Pilge H, Banke IJ, et al. Acute osteomyelitis of the humerus mimicking malignancy: Streptococcus pneumoniae as exceptional pathogen in an immunocompetent adult. BMC Infect Dis. 2013;13:266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu H, Yu S, Fu J, et al. Investigating clinical characteristics and prognostic factors in patients with chronic osteomyelitis of humerus. Burns Trauma. 2019;7:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Foster AL, Moriarty TF, Zalavras C, et al. The influence of biomechanical stability on bone healing and fracture‐related infection: the legacy of Stephan Perren. Injury. 2021;52(1):43‐52. [DOI] [PubMed] [Google Scholar]
- 18. Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2007;89(8):1700‐1709. [DOI] [PubMed] [Google Scholar]
- 19. Fowler JR, Perkins TA, Buttaro BA, Truant AL. Bacteria adhere less to barbed monofilament than braided sutures in a contaminated wound model. Clin Orthop Relat Res. 2013;471(2):665‐671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chu CC, Williams DF. Effects of physical configuration and chemical structure of suture materials on bacterial adhesion. A possible link to wound infection. Am J Surg. 1984;147(2):197‐204. [DOI] [PubMed] [Google Scholar]
- 21. Tashjian RZ, Granger EK, Zhang Y. Utility of prerevision tissue biopsy sample to predict revision shoulder arthroplasty culture results in at‐risk patients. J Shoulder Elbow Surg. 2017;26(2):197‐203. [DOI] [PubMed] [Google Scholar]
- 22. Momodu II, Savaliya V. Osteomyelitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532250/ 2021.
- 23. Fernandes MDC, Peres LR, de Queiroz AC Jr, et al. Open fractures and the incidence of infection in the surgical debridement 6 hours after trauma. Acta Ortop Bras. 2015;23(1):38‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976). 2000;25(13):1668‐1679. [DOI] [PubMed] [Google Scholar]
- 25. Kumar A, Sandoe J, Kumar N. Three cases of vertebral osteomyelitis caused by Streptococcus dysgalactiae subsp. equisimilis. J Med Microbiol. 2005;54(Pt 11):1103‐1105. [DOI] [PubMed] [Google Scholar]
- 26. Krebs NM, Krebs RC, Yaish AM. Femoral osteomyelitis presenting as a pathologic fracture in a 53 year old male: a rare case report. J Orthop Case Rep. 2017;7(6):85‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gelfand MS, Cleveland KO, Goswami R, Heck RK. Pathological fracture in acute osteomyelitis of long bones secondary to community‐acquired methicillin‐resistant Staphylococcus aureus: two cases and review of the literature. Am J Med Sci. 2006;332(6):357‐360. [DOI] [PubMed] [Google Scholar]
- 28. Walmsley BH. Pathological fracture in acute osteomyelitis in an adult. J R Soc Med. 1983;76(1):77‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tiemann A, Hofmann GO, Krukemeyer MG, Krenn V, Langwald G. Histopathological Osteomyelitis Evaluation Score (HOES) – an Innovative Approach to Histopathological Diagnostics and Scoring of Osteomyelitis. GMS Interdiscip Plast Reconstr Surg DGPW. 2014;3:Doc08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head. An anatomical study. J Bone Joint Surg Am. 1990;72(10):1486‐1494. [PubMed] [Google Scholar]
- 31. Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13(4):427‐433. [DOI] [PubMed] [Google Scholar]
- 32. Masrouha KZ, Raad ME, Saghieh SS. A novel treatment approach to infected nonunion of long bones without systemic antibiotics. Strategies Trauma Limb Reconstr. 2018;13(1):13‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Strocchi R, Orsini G, Iezzi G, et al. Bone regeneration with calcium sulfate: evidence for increased angiogenesis in rabbits. J Oral Implantol. 2002;28(6):273‐278. [DOI] [PubMed] [Google Scholar]
- 34. Johnston PS, Hatzidakis AM, Tagouri YM, Curran‐Everett D, Sears BW. Anatomic evaluation of radiographic landmarks for accurate straight antegrade intramedullary nail placement in the humerus. JSES Int. 2020;4(4):745‐752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sears BW, Johnston PS, Garrigues GE, Boileau P, Hatzidakis AM. Intramedullary nailing of the proximal humerus – not just for 2‐part fractures. Annals of Joint. 2020;5:1‐8. [Google Scholar]
- 36. Kanakaris N, Gudipati S, Tosounidis T, Harwood P, Britten S, Giannoudis PV. The treatment of intramedullary osteomyelitis of the femur and tibia using the reamer‐irrigator‐aspirator system and antibiotic cement rods. Bone Joint J. 2014;96‐B(6):783‐788. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


