ABSTRACT
HPV vaccine uptake remains low in China, especially among girls. Recently, China has initiated a pilot program on HPV immunization for girls 9–14. From November to December 2021, a cross-sectional study was conducted among parents of girls 9–14 in China through a web-based anonymous online questionnaire survey. Descriptive epidemiological analysis was used to analyze parental acceptability. Hierarchical regression analysis and structural equation modeling were to determine associated factors. A total of 5623 participants were included in the analysis. 21.2% girls had received HPV vaccine, and 94.3% parents intended to receive vaccination for their daughters, the Kappa values between them was −0.016. 31.9% of vaccinated mothers had received HPV vaccine for their daughters, vaccination history had a positive impact on behavior (β = 0.048). Attitude (β = 0.186), subjective norms (β = 0.148) and perceived behavioral control (β = 0.648) had a positive impact on intention. Vaccination intention mediated the relationships between attitude (β = 0.044), subjective norms (β = 0.035), and perceived behavioral control (β = 0.154) with behavior. There is a gap between vaccination intention and behavior in parents of girls 9–14. Perceived behavior control had a strong association on HPV vaccination behavior.
KEYWORDS: Human papillomavirus vaccine, parents of female adolescents aged 9–14, theory of planned behavior (TPB), intention, behavior
Introduction
Human papillomavirus (HPV) has a high carcinogenic potential to cause lesions in the genital mucosa and can lead to genital warts, cervical cancer, vulvar cancer, and oropharyngeal cancer, etc.1 Current estimates indicate that 2869 million women 15 years of age or older are at risk of developing cervical cancer.2 The World Health Organization (WHO) recommends HPV vaccination for the primary prevention of cervical cancer, particularly for female adolescents between the ages of 9 and 13 years.3,4 Multiple studies have shown that HPV vaccination of female adolescents aged 9–14 prevents more deaths from cervical cancer and is more cost effective than not vaccinating.5,6 Since the HPV vaccine was licensed in the United States in 2006, 107 countries have officially included HPV vaccines in their national immunization programs as of June 2020.7 According to WHO estimates of global HPV vaccine coverage, countries including Portugal, Iceland, and Seychelles have reached full vaccination rates of more than 90% among female adolescents aged 9–14.8 However, as a country with a large burden of cervical cancer, China has not yet included HPV vaccine into the national immunization program and still implements a voluntary, self-funded vaccination strategy.9 Data from the 2019 national survey showed that the HPV vaccination rate of female adolescents aged 9–14 years was low, only 1.37%.10
In recent years, in order to actively respond to the call of WHO’s “Strategy to accelerate the Elimination of Cervical Cancer,” and strive to achieve the goal of 90% girls completing HPV vaccination before the age of 15 by 2030, the Chinese government has begun to attach great importance to the promotion of HPV vaccination. In 2021, the National Health Commission launched a pilot expanded program on HPV immunization for local female adolescents aged 9–14 in selected cities and regions.11,12 However, the current HPV vaccination rate among adolescents remains extremely low, and China is still far from achieving a high HPV vaccine uptake rate in eligible female adolescents. Because HPV vaccination in adolescents is usually determined by parents and families, parental intention has a major impact on the initiation of vaccination.13 However, a study in the USA in 2016 documented that parents were willing to vaccinate their children with HPV vaccine as high as 75%−96%, while the actual vaccination coverage was only 38%−57%.14 A study in China in 2020 reported that the proportion of people aged 50–69 willing to receive influenza vaccine was as high as 70.5%, while the actual vaccination coverage rate was only 10.8%.15 These findings demonstrated the complexity in the “achieving from intention to behavior.” In order to effectively formulate vaccination intervention strategies, it is necessary to study whether there is a large gap between “intention and behavior” and the factors that affect vaccination behavior. However, there is a lack of study to explore the relationship between the intention and behavior of Chinese parents for HPV vaccination of their daughters.
Furthermore, previous studies have found that the level of knowledge, daughters’ age, awareness of HPV infection risks, vaccine safety, and efficacy are significant factors influencing parents’ intention and behavior to vaccinate their daughters against HPV in mainland China.16–20 However, most studies have been descriptive and have lacked a systematic explanation of the factors influencing parents’ HPV vaccination of their daughters. Currently, the theory of planned behavior (TPB) is one of the most used psychological theories to explain health behaviors, which helps describe the intention and behavioral aspects of vaccination.21 Askelson et al.22 showed that attitude was the strongest predictor of mothers’ intention to vaccinate their daughters against HPV. Other determinants, including media use, perception of the risk of HPV infection and vaccination, descriptive norms, and expected regret, were also included in the extended planned behavior model to explore their influence on intention and behavior.23–29
However, the social and cultural background of China is different from that of Western countries. Compared with Western societies, Chinese parents emphasize child-centered family traditions, and have a higher tolerance for uncertainty. Meanwhile, parents are more willing to overcome some behavioral barriers for children’s health.30 In addition, China has a different health system than Western societies, and HPV vaccination is not yet part of the national immunization program, meaning guardians must pay out-of-pocket costs.31 Therefore, many HPV vaccination studies based on the TPB model in Western countries do not fully explain parental HPV vaccination intention and behavior in the sociocultural context of mainland China. In addition, although Webb et al.32 found that interventions theory based on TPB were more effective than interventions based on other theories, the existing researches on TPB have not been in-depth, and a systematic review33 showed that most researchers did not address adaptive feedback, instead only focusing on intention as a result while ignoring the mediating role between intention and behavior.
Therefore, based on TPB, the aim of this study was to evaluate the gap between parents’ intention and behavior of HPV vaccination for their daughters aged 9–14 in China. We sought to explore the beliefs and drivers of parents’ behavior to vaccinate their daughters against HPV, and their relationships with and influence on parents’ vaccination intention and practices, to provide direct and prompt evidence for the implementation of effective interventions to improve HPV vaccination coverage in female adolescents aged 9–14.
Materials and methods
Study design and participants
This cross-sectional study was designed for HPV vaccination in China and was conducted from November to December 2021. We adopted a convenience sampling method. We created questionnaires link on the Wenjuanxing which was a platform dedicated to the creation and dissemination of questionnaires in China, and forwarded by the social network platform of WeChat. The participants were also encouraged to send a questionnaire link to other network members. The platform’s user identification system (i.e., a mobile phone number was required to complete the questionnaire) was used to ensure the authenticity, non-repeatability, and representativeness of the participants. Participants were informed of the purpose of the survey and informed consent was obtained before they completed the questionnaire. The protocol was approved by the Ethics Committee of the Wuxi Center for Disease Control and Prevention (2020No10). Parents of daughters aged 9–14 years were recruited for the study. Inclusion criteria were: a) parents of female adolescents aged 9–14; and b) people who volunteered to participate in this survey. In addition, we set up submission control for the answer sheet in advance, so that incomplete questionnaires could not be submitted; thus, all submitted questionnaires were answered completely.
The questionnaire was used to collect socio-demographic information (participants’ age, gender, ethnicity, marital status, education, whether they worked in a healthcare-related occupation, and annual household income), and whether they had heard of the HPV vaccine. After compiling a preliminary questionnaire, we invited 18 students and 3 professors from Southeast University to conduct a pilot test. Based on the model test results, the questionnaire was revised to ensure clarity, readability, and logicality.
Measures
Currently, theory of planned behavior is one of the most commonly used psychological theories to explain health behavior. In this model, intention is considered the most direct predictor of behavior and is weighted according to attitudes, subjective norms, and perceived behavioral control. Besides, according to Ajzen, the founder of the TPB, proposed that past behavior may have a huge influence on later action and should be added as a mediator role in framework.34 Therefore, in this study, we focused on the possible influence of previous behavior on later behavior, and used vaccination history as a moderating variable to explore attitude, subjective norms, perceived behavioral control and intention influence on vaccination behavior. The theoretical model is shown in Figure 1. Measurement items were referenced and modified from existing literature.26,35–37 The complete questionnaire is shown in Supplement 1.
Figure 1.
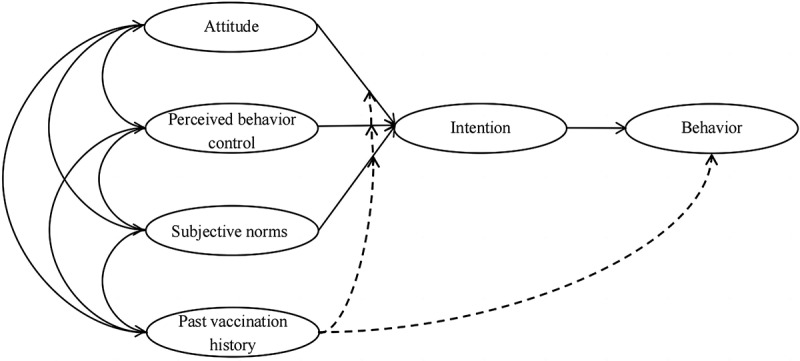
The conceptual framework of the model.
Attitude
The scale of attitude [from 1 (strongly disagree) to 5 (strongly agree)], which is understood as the parental positive or negative perceptions of HPV vaccination, includes four items, namely, “(a) You think that HPV vaccination for children is necessary; (b) You think that HPV vaccination for children is good for children’s health; (c) You worry about the side effect (pain at injection site, tired, diarrhea, etc.) of HPV vaccine; (d) You worry about the serious adverse effect (muscle spasm, blurred vision, disability etc.) of HPV vaccine.” The answers to items (a), (c), and (d) were flipped because the wording of the three questions was negative.
H1:
(a) Attitudes have a positive association with HPV vaccination intention. (b) Attitudes have a positive association with HPV vaccination behavior.
Subjective norms
The subjective norms [from 1 (strongly disagree) to 5 (strongly agree)], which are the expectations of family, friends, government, and physicians on the parents, consist of six items: “People around you (colleagues, friends) are in favor of vaccinating your child against HPV/If your family, relatives/friends or colleagues/your child’s teachers/doctors/community or government suggests that you should get your child vaccinated against HPV, would you let your child get vaccinated?”
H2:
(a) Subjective norms have a positive association with HPV vaccination intention. b) Subjective norms have a positive association with HPV vaccination behavior.
Perceived behavioral control
The questionnaire measured perceived behavioral control, which indicates the parents’ beliefs about the barriers to HPV vaccination (e.g. the time and cost of vaccination), using three items, with the scale [from 1 (strongly disagree) to 5 (strongly agree)]: “(a) You will still let your child get the vaccine, even you need to pay for the HPV vaccine; (b) You will still let your child get the vaccine, even it would take up more time; (c) You will still let your child get the vaccine, even the vaccination place was far away from where you and your children live.”
H3:
(a) Perceived behavioral controls have a positive association with HPV vaccination intention. (b) Perceived behavioral controls have a positive association with HPV vaccination behavior.
HPV vaccination intention
The intention dimension is understood as the likelihood of parent to accept the HPV vaccine for their daughters. Intention was measured using three items: “(a) Will you consider vaccinating your child against HPV vaccine? (b) Will you get vaccination of HPV vaccine for your child in the six months? (c) If you were offered a self-payment HPV vaccine for your child now, would you choose to get it right away?” The scale ranges from 1 (strongly disagree) to 5 (strongly agree). Similarly, we flipped the scores for the reverse intention items (a) and (c). In this study, the HPV vaccination intention sores was equal to the average score of the three vaccination intention items. The higher the score, the higher the vaccination intention. The cutoff value is 3 points, and more than 3 points meant “intend to vaccinate.”
H4:
HPV vaccination intention is positively associated with HPV vaccination behavior.
H5:
HPV vaccination intention mediates the relationship between attitudes (Hypothesis 5i), subjective norms (Hypothesis 5ii), perceived behavioral controls (Hypothesis 5iii), with HPV vaccine behavior
Past vaccination history
The questionnaire uses one item to measure this scale: “Have you (the parent) ever received the HPV vaccine?” We used a binary response format, where 1 means “no” and 2 means “yes.”
H6:
(a) Past vaccination history moderates the strength of the mediating relationships between attitudes (Hypothesis 6i), subjective norms (Hypothesis 6ii), and perceived behavioral controls (Hypothesis 6iii) with HPV vaccine behavior through intention. b) Past vaccination history is positively associated with HPV vaccination behavior.
Vaccination behavior
The daughters’ HPV vaccination behavior was assessed by one items (“Is your child currently vaccinated against HPV?”). We using a binary response format, where 1 means “no” and 2 means “yes”.
Measurement model testing and fitting
Cronbach’s alpha was calculated to determine the reliability of the measurement model. We performed the confirmatory factor analysis (CFA) to evaluate the reliability and validity of each item. Average variances extracted (AVE) and composite reliability (CR) were calculated to evaluate convergence effectiveness. Discriminant validity was assessed by correlation between the square root of AVE and latent factors. Cronbach’s alpha values higher than 0.70 indicate acceptable reliability, while AVE values higher than 0.50 and CR values higher than 0.70 are considered acceptable validity.38 According to the research of Gerbing et al.,39 goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), comparative fitness index (CFI) and the root means square error of approximation (RMSEA) were used to evaluate model fit. For GFI, CFI, and AGFI, values closer to 1 are better, and values greater than 0.90 indicate a relatively good data fit; RMSEA value closer to 0 are better, and value less than 0.08 indicates a relatively good model-data fit.39,40
Statistical analysis
It took at least 60 seconds to complete the questionnaire through the pre-questionnaire survey, so the quality control set 60 seconds as the cutoff time for the shortest questionnaire answer, thereby excluding participants who did not seriously participate in the survey. After all investigations, data cleaning was performed to eliminate unqualified questionnaires. Exclusion criteria were as follows: (1) parents who completed the questionnaire in less than 60 seconds; (2) participants were not parents of female adolescents aged 9–14 years; (3) there were obvious logical errors in the answers to the above questions.
Descriptive methods were used to describe the characteristics and vaccination uptake of adolescents. In addition, the Kappa test was used to analyze the consistency of parent vaccination intention and adolescent vaccination uptake. Furthermore, hierarchical moderator regression was used to examine the moderating effects (Figure 2). Control variables were entered in the block 1 (gender, age, ethnicity, marital status, education, occupation, healthcare occupation, annual household income, and knowledge of the HPV vaccine), followed by the standardized values of the main effects (attitude, subjective norms, perceived behavioral control, and past vaccination history) in block 2. Finally, the moderators (attitude * past vaccination history, subjective norms * past vaccination history, and perceived behavioral control * past vaccination history) were used in block 3. We constructed a structural equation model to estimate the relationships and coefficients between the variables. Bootstrapping (5000 trials) was used to test mediator effects.
Figure 2.
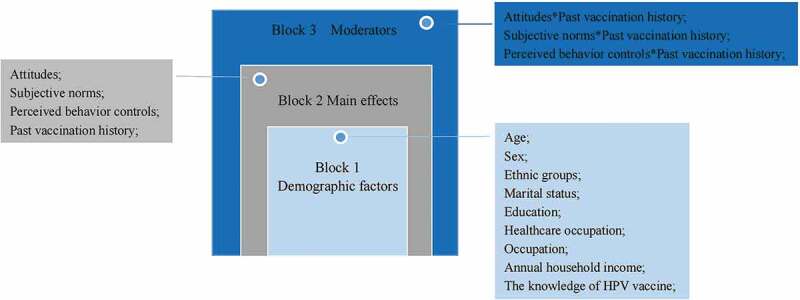
The framework of the hierarchical moderator regression.
Further, since involvement in child health-related decision making may differ between mothers and fathers,41 we investigate maternal and paternal characteristics separately. We employed the multi-group SEM to analyze the differences between fathers and mothers. We performed the analysis to compare the measurement weights, structural weights, structural covariance, structural residual, and measurement residual of fathers and mothers.
Statistical analyses were performed using IBM SPSS Statistics 25.0. and Amos 25.0. Statistical significance was defined as a two-sided P-value <.05.
Results
Sociodemographic characteristics of the study population
A total of 6,480 responses were received. After excluding unqualified questionnaires, 5,623 questionnaires were included in the study. A flowchart of the questionnaire survey is shown in Figure 3. The sociodemographic characteristics of the participants are presented in Table 1. Overall, the majority of parents were aged 36–41 (n = 2,563; 45.6%) and more than two-thirds were female (n = 4,268; 75.9%). Nearly half of the parents had a high school education or an equivalent degree (n = 3,131; 55.7%). The proportion of households with an income less than RMB 100,000 was the highest at 50.6% (n = 2,848). A total of 2,795 (49.7%) parents were employed in the enterprise/business/service industry and 200 (3.6%) parents engaged in healthcare occupations. A total of 5,236 parents (93.1%) reported that they had heard of HPV vaccination. A total of 448 mothers (8.0%) reported that they had received HPV vaccinations.
Figure 3.
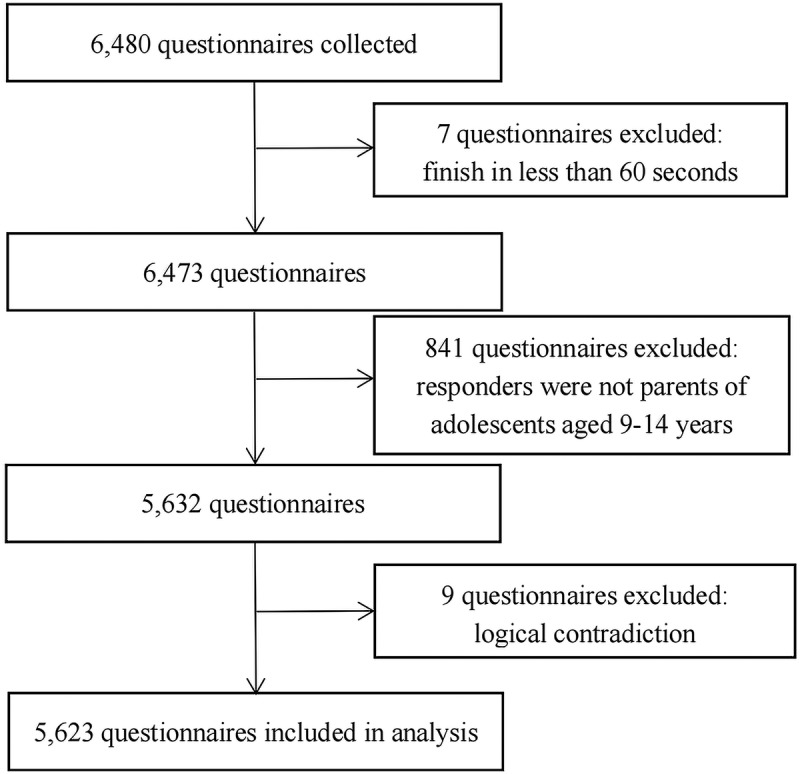
Flow chart of questionnaire inclusion.
Table 1.
Demographic characteristics of study participants (N = 5623).
| Characteristics | Frequency (%) | |
|---|---|---|
| Age (years) | <36 | 832 (14.8%) |
| 36-<41 | 2563 (45.6%) | |
| 41-<46 | 1468 (26.1%) | |
| ≥46 | 760 (13.5%) | |
| Gender | Male | 1355 (24.1%) |
| Female | 4268 (75.9%) | |
| Ethnic groups | Han | 5525 (98.3%) |
| Other | 98 (1.7%) | |
| Marital status | Married | 5328 (94.8%) |
| Other | 295 (5.2%) | |
| Primary school and below | 320 (5.7%) | |
| Education | Junior high school | 2172 (38.6%) |
| Senior high school | 1493 (26.6%) | |
| University diploma or above | 1638 (29.1%) | |
| Healthcare occupation | Yes | 200 (3.6%) |
| No | 5423 (96.4%) | |
| Occupation | Government organs and institutions | 292 (5.2%) |
| Enterprise/business/service industry | 2795 (49.7%) | |
| Freelancer | 1555 (27.7%) | |
| Other | 981 (17.4%) | |
| Annual household income (10,000 RMB) | <10 | 2848 (50.6%) |
| 10–<20 | 1939 (34.5%) | |
| ≥20 | 836 (14.9%) | |
| The knowledge of HPV vaccine | Yes | 5236 (93.1%) |
| No | 387 (6.9%) | |
| HPV vaccination history | Yes | 448 (8.0%) |
| No | 5175 (92.0%) | |
HPV vaccination intention and behavior
The results showed that 21.2% of the participants’ adolescent daughters received the HPV vaccine. Notably, among mothers who had already been vaccinated, 31.9% had their daughters vaccinated. In contrast, 20.3% of non-vaccinated parents had their daughters vaccinated. Univariate regression analysis showed that maternal HPV vaccination history had a statistically significant effect on daughters’ vaccination (OR: 1.559; 95% CI: 1.150–2.115; P < .001). In addition, 94.3% of parents intended to obtain HPV vaccination for their daughters. We further compared the vaccination uptake of female adolescents aged 9–14 years with their parents’ intentions to vaccinate. It showed that poor consistency was observed in the group with Kappa values of −0.016 (P = .004).
Measurement model and fitting
We examined the items of each scale in terms of factor loading, followed by the modification indices. Items with factor loading below 0.5 were mainly not retained [3,4]. Each item had reliability and validity based on the estimated error variance and modification index of each item. Cronbach’s alpha coefficients for attitude, subjective norms, perceived behavioral control, and intention were 0.619, 0.911, 0.763, and 0.687, respectively (Supplementary 2). The CR values of all the dimensions were greater than 0.6 (Table 2). The overall model fit well (GFI = 0.962; CFI = 0.970; AGFI = 0.946; RMSEA = 0.054); therefore, the measurements and the structural model were acceptable. Except for the dimension of perceived behavioral control, the square roots of the average variance extracted of the dimensions of attitude, subjective norms, and intention exceeded the related correlations (Table 3).
Table 2.
Convergent validity of the revised scale.
| Dimension | Item | Factor loading value | AVE | CR |
|---|---|---|---|---|
| Attitude | Q1 | 0.774 | 0.474 | 0.640 |
| Q2 | 0.591 | |||
| Subjective norms | Q5 | 0.500 | 0.691 | 0.928 |
| Q6 | 0.818 | |||
| Q7 | 0.861 | |||
| Q8 | 0.941 | |||
| Q9 | 0.875 | |||
| Q10 | 0.913 | |||
| Perceived behavioral control | Q11 | 0.659 | 0.596 | 0.748 |
| Q12 | 0.828 | |||
| Q13 | 0.817 | |||
| Intention | Q14 | 0.714 | 0.405 | 0.749 |
| Q15 | 0.647 | |||
| Q16 | 0.590 |
Table 3.
Discriminant validity of the revised scale.
| Dimension | Intention | Perceived behavioral control | Subjective norms | Attitude |
|---|---|---|---|---|
| Intention | 0.636 | |||
| Perceived behavioral control | 0.842* | 0.772 | ||
| Subjective norms | 0.608* | 0.498* | 0.831 | |
| Attitude | 0.645* | 0.537* | 0.736* | 0.688 |
*P < .05.
Hierarchical moderator regression analysis
Participants who had heard of the HPV vaccine were more willing to vaccinate their daughters (β = 0.104; P = .006). Parents at different income stages showed slightly different intentions. Compared with parents with an annual income of less than RMB 10,000, parents with an annual income of more than RMB 20,000 showed a higher intention (β = 0.019; P = .021). Parents with higher educational levels were more likely to have vaccinated their daughters (β = 0.023; P = .050). Ethnicity, age, gender, marital status, and occupation did not affect vaccination intention. In addition, compared to the block 1 model with control variables, the block 2 model changed significantly (∆R2 = 0.411; P < .001). Attitudes (β = 0.076; P < .001), subjective norms (β = 0.311; P < .001), and perceived behavioral control (β = 0.432; P < .001) were positively correlated with HPV vaccination intentions. In block 3, the added moderator (i.e., past vaccination history) did not significantly change the model compared with block 2 (∆R2 = 0.000; P = .847; Table 4). Attitudes * Previous vaccination history (β = −0.053; P = .451), subjective norms * past vaccination history (β = −0.002; P = .979), and perceived behavioral control * past vaccination history (β = 0.031; P = .549) had no moderating effect on attitude → HPV vaccination behavior, subjective norms → HPV vaccination behavior, and perceived behavioral control → HPV vaccination behavior, respectively. Therefore, Hypotheses 6i, 6ii, and 6iii are rejected.
Table 4.
Hierarchical moderator regression analysis.
| Model | ∆R2 | F value | P value |
|---|---|---|---|
| Block 1 | 0.046 | 15.137 | <.001 |
| Block 2 | 0.411 | 529.885 | <.001 |
| Block 3 | 0.000 | 0.269 | .847 |
Structural equation model and test results
The final model construction and test results are listed in Table 5. The goodness-of-fit results were GFI = 0.968, AGFI = 0.953, CFI = 0.973, NFI = 0.970, RMSEA = 0.049, and all model-fitting indices were qualified. Attitude (β = 0.186; P = .003), subjective norms (β = 0.148; P = .005), and perceived behavioral control (β = 0.648; P = .006) had positive impacts on vaccination intention, supporting H1a, H2a, and H3a. There were no significant associations between attitudes, subjective norms, and behaviors. Therefore, these results did not support H1b and H2b. Perceived behavioral control was negatively associated with behavioral presentation, failing to confirm H3b. Intention (β = 0.238; P = .004) and past vaccination history (β = 0.048; P = .044) significantly affected vaccination behavior; thus, H3 and H6b were proved. Bootstrap analysis showed that vaccination intention mediated the relationships between attitude (indirect effect β = 0.044; P = .002), subjective norms (indirect effect β = 0.035; P = .002), and perceived behavioral control (indirect effect β = 0.154; P = .004) with vaccination behavior, confirming H5. In addition, the differences between the indirect effects of attitudes, subjective norms, and perceived behavioral control on behavior were statistically significant (diff attitude-subjective norms = 0.009, P < .001; diff attitude-perceived behavioral control = −0.110, P < .001; diff subjective norms-perceived behavioral control = −0.119, P < .001). The model explained 74% of the variation in vaccination intention and 2% of the variation in vaccination behavior.
Table 5.
Structural equation model and test results.
| Bootstrapping |
|||||
|---|---|---|---|---|---|
| Effects | Standardized point estimate | SE | 95% CI lower | 95% CI upper | P value |
| Direct | |||||
| Attitude – Intention | 0.186 | 0.047 | 0.111 | 0.264 | .003 |
| Subjective norms – Intention | 0.148 | 0.037 | 0.083 | 0.210 | .005 |
| Perceived behavioral control – Intention | 0.648 | 0.032 | 0.594 | 0.710 | .006 |
| Intention – Behavior | 0.238 | 0.070 | 0.133 | 0.356 | .004 |
| Attitude – Behavior | −0.037 | 0.048 | −0.120 | 0.044 | .485 |
| Subjective norms – Behavior | −0.030 | 0.039 | −0.095 | 0.032 | .443 |
| Perceived behavioral control – Behavior | −0.115 | 0.056 | −0.214 | −0.030 | .027 |
| Past vaccination history – Behavior | 0.048 | 0.021 | 0.010 | 0.078 | .044 |
| Indirect | |||||
| Attitude – Behavior | 0.044 | 0.018 | 0.023 | 0.083 | .002 |
| Subjective norms – Behavior |
0.035 | 0.013 | 0.017 | 0.061 | .002 |
| Perceived behavioral control – Behavior | 0.154 | 0.048 | 0.084 | 0.241 | .004 |
| Total | |||||
| Attitude – Behavior | 0.007 | 0.026 | −0.071 | 0.078 | .909 |
| Subjective norms – Behavior | 0.005 | 0.039 | −0.065 | 0.062 | .986 |
| Perceived behavioral control – Behavior | 0.040 | 0.044 | −0.002 | 0.082 | .119 |
| Intention – Behavior | 0.238 | 0.070 | 0.133 | 0.356 | .004 |
| Past vaccination history – Behavior | 0.048 | 0.021 | 0.010 | 0.078 | .044 |
Supplementary 2 (Tables S7-S15) lists the multi-group analysis results. The standardized path coefficients of the fathers and mothers groups were basically consistent with the significant results of the overall SEM model path test done above. Perceived behavioral control was the strongest predictor of both father and mother’s intention to vaccinate their daughters. Slightly different is that, perceived behavioral control showed a higher positive effect of mothers (β = 0.677; P = .004) than fathers (β = 0.243; P = .007).
Discussion
In this study, the HPV vaccination uptake of female adolescents aged 9–14 in China was 21.2%, which was significantly higher than the results of the national survey on vaccination status from September to October 2019 (1.37%).10 This indicates that the HPV vaccination pilot project, which began in 2021 to provide domestic bivalent HPV vaccine to female students aged 9–14 years based on government subsidies or basic medical insurance payment in some areas such as Ordos in Inner Mongolia, Wuxi in Jiangsu province, and Xiamen in Fujian province,42 has achieved initial success. Meanwhile, we compared the concordance between vaccination rates and parental HPV vaccination intentions. Then we found that parents of female adolescents aged 9–14 in China had high intention to vaccinate their daughters (94.3%), but the gap between the vaccination rate and the intention was large (>50%). This is the similar gap to previous findings on HPV vaccination among adolescents aged 13–17 in the United States14 and influenza vaccination among adults aged 50–69 in China,15 which suggests that the “intention-behavior gap” is a common occurrence, occurring across different vaccines and populations.
Additionally, the SME results showed that, vaccination intention mediated between attitude, subjective norms, perceived behavioral control, and vaccination behavior. Researchers of a cross-sectional online survey in the United States also emphasized the role of intention and attitude, subjective norms, and perceived behavioral control as proximal and distal predictors of health behaviors.43 Similar results have been found in studies conducted in Canada21 and mainland China.37 Our results provide further evidence of this relationship.
Notably, our results showed that the perceived behavioral control dimension had a greater indirect impact on HPV vaccination behavior than the attitude and subjective norms dimensions. Previous studies have shown that perceived behavioral control only marginally improved the overall predictive power of TPB.44 This may be due to the fact that most of the previous studies on the influencing factors of parents’ HPV vaccination behavior for their children based on the TPB theory were conducted in Western countries, which have incorporated HPV vaccine into their national immunization programs, thus guaranteeing the HPV vaccination of millions of girls against the main cause of cervical cancer. But in China, the HPV vaccines in most cities are self-funded.9 What’s more, the supplies are far behind the market demand in China. So far, 7 million doses of HPV vaccines have been released to mainland China’s target market – the female population aged 9–45 years. Yet, even when population projections are restricted to WHO’s recommended primary target group – aged 9–14 years – there are at least 41 million girls in need of vaccination in China.45 Normally, people who get vaccinated must make an appointment and wait for more than half a year to receive the vaccine. This suggests that cost and accessibility play an important role in the final decision of parents in mainland China to vaccinate their children against HPV.
On this basis, our SEM results also showed that the path coefficient between perceived behavior control and intention was larger than behavior, which indicated that there was a large gap between “intention and behavior.” This may be due to China’s social culture and actual behavioral disorders (such as high price of vaccines). Actually, in China, the price ranges from $254 to $586 for three doses of imported vaccine, which is expensive for most parents, especially for people with low incomes.46 But under the influence of Chinese traditional social culture, parents emphasize child-centered family traditions, and have a higher tolerance for uncertainty. Particularly, since the 1982s, China has taken the family planning policy as a basic national program, in order to achieve the goal of controlling the excessive growth of the population and improving the level of eugenics, so that most families only have one child. Many children are called “little emperors” by the media. Parents and grandparents put all their expectations on children and take good care of them.47,48 Although vaccination is not always easy, every Chinese parent is willing to overcome obstacles for their children’s health, so the perceived behavioral control has a larger path coefficient of intention. However, in our study, 50.6% households have an annual income of less than RMV100,000 (equal to about $14500), and the cost of three doses would be 1.75% to 4.04% of the annual household income. Given the high price, most parents may have made an opposite choice to their intention, resulting in a smaller path coefficient between perceived behavioral control and behavior. The study analysis by Qiu et al.49 showed that the HPV vaccination coverage rate was lower among Chinese girls aged 9–14 years in families with lower parental income, which also provided reference for our findings.
In addition, our findings are consistent with the results of Kornides,50 which results suggested that vaccination history had a direct effect on vaccination behavior. According to dual process theories, previously vaccinated mothers may behave in two ways: a reasoned route, modeled by the influence of belief-based constructs from the TPB mediated by intentions, and an unconscious, habitual route represented by the influence of past behavior.51 This suggests that we can use mothers’ own vaccination status as a motivation to vaccinate their children, tailoring HPV vaccination promotion messages to mothers who have already been vaccinated themselves to effectively motivate their children to be vaccinated, especially in areas with low coverage.
The influence of some demographic characteristics on vaccination intention is also noteworthy. In this study, household income, HPV vaccine knowledge and education were associated with parents’ intention to vaccinate their daughters against HPV. With the increase of family income level, parents’ intention showed an upward trend, and parents who had heard about the vaccine or were more educated were more likely to vaccinate their daughters. These are consistent with the results of previous studies in Fujian, China52 and Shenzhen, China.53 In addition, the gender of the parents did not prove to be a statistically significant factor in vaccination intention in our study, which is different from the findings in Poland54 and Italy.55 This may be related to the social culture in which fathers become actively involved in child-care activities in contemporary Chinese families.56 Especially in recent years, with the popularity of the concept of gender equality and the improvement of women’s socioeconomic status, there are growing social calls for fathers to share child-care activities.
Our study has some limitations. First, because of the COVID−19 pandemic, the survey was conducted online. The lack and restriction of quality control measures involved in online survey methods may have resulted in reduced accuracy. Second, most people who actively participated in the survey were those who were actively considering vaccination, resulting in potential selectivity bias. Third, all records including vaccination behavior were self-reported, which may carry risk of recall and social expectation bias. Fourth, given the conciseness of the questionnaire, we did not provide more details about parents’ vaccination history, which may resulted in the false reporting. Fourth, despite the trend suggested by Ajzen that past behavior might have a huge influence on future behavior, adding only one variable to test its moderating effect makes a limited contribution to the innovation of the theoretical model. Therefore, future researches should consider more other determinants to explore their influence on intention and behavior. Fifth, considering that HPV vaccination for males has not been popularized in mainland China, exploration on the vaccination of boys are not included in this study. Sixth, pilot sample size was small, although this questionnaire has been used in another large survey of parents of female teenagers aged 9–14 that have not yet been published by the research group before this survey, its reliability and validity analysis ensured that the questionnaire was clear, readable and logical. Finally, this study had a cross-sectional design and was unable to illustrate the dynamic trends. Further longitudinal studies are needed to determine the predictive power of intention for behavior.
Conclusions
In this study, HPV vaccination uptake among female adolescents aged 9–14 years in China was low (21.2%), but parents had high intention to vaccinate their daughters (94.3%). There is a gap between vaccination intention and behavior among the parents of girls aged 9–14. In addition, 31.9% of the vaccinated mothers had gotten the HPV vaccine for their daughters, and vaccination history had a positive impact on parents’ behavior. Vaccination intention had a mediating effect on attitude, subjective norms, perceived behavioral control, and vaccination behavior. Perceived behavioral control had greater indirect effects on behavior than did attitude or subjective norms. Further studies are needed to explore the mechanism between intention and behavior to implement effective interventions to bridge the intention-behavior gap and improve HPV vaccination coverage in female adolescents aged 9–14 years in China.
Supplementary Material
Acknowledgments
We would like to thank Xuxi Center for Disease Prevention and Control; all parents who participated in this survey for their contributions to this study.
Funding Statement
This study was supported by Postgraduate Research & Practice Innovation Program of Jiangsu Province [grant number KYCX20_0153]; Wuxi City Technology Development Fund [grant number N20191007].
Author contributions
YQY, YS and HJ designed the study. SXX, NYS, QW and TTC conducted the literature review and designed the questionnaire. YH, SHZ, LQY, YNW and NYS assisted with the online investigation. YQY, QW and LQY analyzed the data. HJ, QW, and SXX interpreted the results. All authors critically revised the manuscript for important intellectual content. And that all authors agree to be accountable for all aspects of the work and approve the version for publication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical approval and patient consent
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was ethically reviewed and approved by the Ethics Committee of the Wuxi Center for Disease Prevention and Control (2020No10). Oral informed consent was obtained from all participants.
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2225994.
References
- 1.Zardo GP, Farah FP, Mendes FG, Franco CAGDS, Molina GVM, Melo GND, Kusma SZ.. Vaccine as an immunization agent against HPV. Cien Sau Colet. 2014;19(9):3799–10. doi: 10.1590/1413-81232014199.01532013. [DOI] [PubMed] [Google Scholar]
- 2.Bruni LAG, Serrano B, Mena M, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and related diseases in the world. Summary Report; 2021. https://hpvcentre.net/statistics/reports/XWX.pdf.
- 3.Cervical cancer [Internet] . Switzerland: World Health Organization; 2022. [accessed 2022 July 1]. https://www.who.int/health-topics/cervical-cancer#tab=tab1. [Google Scholar]
- 4.New WHO guide to prevent and control cervical cancer [Internet] . Switzerland: World Health Organization; 2014. [accessed 2022 July 1]. https://www.who.int/news/item/03-12-2014-new-who-guide-to-prevent-and-control-cervical-cancer. [Google Scholar]
- 5.Jit M, Brisson M. Potential lives saved in 73 countries by adopting multi-cohort vaccination of 9-14-year-old girls against human papillomavirus. Int J Cancer. 2018;143(2):317–23. doi: 10.1002/ijc.31321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drolet M, Laprise JF, Martin D, Jit M, Bénard É, Gingras G, Boily M-C, Alary M, Baussano I, Hutubessy R, et al. Optimal human papillomavirus vaccination strategies to prevent cervical cancer in low-income and middle-income countries in the context of limited resources: a mathematical modelling analysis. Lancet Infect Dis. 2021;21(11):1598–610. doi: 10.1016/S1473-3099(20)30860-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bruni L, Saura-Lazaro A, Montoliu A, Brotons M, Alemany L, Diallo MS, Afsar OZ, LaMontagne DS, Mosina L, Contreras M, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev Med. 2021;144:106399. doi: 10.1016/j.ypmed.2020.106399. [DOI] [PubMed] [Google Scholar]
- 8.WHO|Data, statistics and graphics World Health Organization [Internet] . Switzerland: World Health Organization; 2020. [accessed 2020 Mar 2]. https://www.who.int/immunization/monitoring_surveillance/data/en.
- 9.Gynecological Oncology Society of Chinese Medical Association . Chinese society for colposcopy and cervical pathology. Chinese expert consensus on clinical application of human papilloma virus vaccine. Chin Med Front J (Electronic Edition). 2021;13(2):1–12. [Google Scholar]
- 10.Shi JJ. Acceptability of human papillomavirus vaccine for 9-14 year-old girls among parents in four provinces of China. Beijing (China): Chinese Center for Disease Control and Prevention; 2020. [Google Scholar]
- 11.National Health Commission of the People’s Republic of China [Internet] . Proposal on strengthening popular science publicity and improving HPV vaccination. 2021. [accessed 2022 July 1]. http://www.nhc.gov.cn/wjw/tia/202112/af51b14c0ca04799b55b8322559751ac.Shtml.
- 12.Na Y. [Internet]. Universal HPV vaccination to make women bid farewell to cervical cancer. China Women’s News; 2021. [accessed 2022 July 1]. http://epaper.cnwomen.com.cn/html/2021-12/01/nw.D110000zgfnb_20211201_2-8.htm.
- 13.Sonawane K, Zhu YA, Montealegre JR, Lairson DR, Bauer C, McGee LU, Giuliano AR, Deshmukh AA. Parental intent to initiate and complete the human papillomavirus vaccine series in the USA: a nationwide, cross-sectional survey. Lancet Public Health. 2020;5(9):e484–492 . doi: 10.1016/S2468-2667(20)30139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Auslander BA, Meers JM, Short MB, Zimet GD, Rosenthal SL. A qualitative analysis of the vaccine intention–behaviour relationship: parents’ descriptions of their intentions, decision-making behaviour and planning processes towards HPV vaccination. Psychol Health. 2019;34(3):271–88. doi: 10.1080/08870446.2018.1523408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xinyue L, Jia L, Liping Z, Mei K, Guan B, Lu Y. Gap between willingness and behavior in the vaccination against influenza, pneumonia, and herpes zoster among Chinese aged 50–69 years. Expert Rev Vaccines. 2021;20(9):1147–52. doi: 10.1080/14760584.2021.1954910. [DOI] [PubMed] [Google Scholar]
- 16.Wang ZX, Wang JJ, Fang Y, Gross DL, Wong MCS, Wong ELY, Lau JTF. Parental acceptability of HPV vaccination for boys and girls aged 9–13 years in China – a population-based study. Vaccine. 2018;36(19):2657–65. doi: 10.1016/j.vaccine.2018.03.057. [DOI] [PubMed] [Google Scholar]
- 17.Zhang SK, Pan XF, Wang SM, Yang C-X, Gao X-H, Wang Z-Z, Li M, Ren Z-F, Zhao F-H, Qiao Y-L, et al. Perceptions and acceptability of HPV vaccination among parents of young adolescents: a multicenter national survey in China. Vaccine. 2013;31(32):3244–9. doi: 10.1016/j.vaccine.2013.05.046. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Ma YY, Wang X, Zou H, Zhao F, Wang S, Zhang S, Zhao Y, Marley G, Ma W, et al. Acceptability of human papillomavirus vaccine among parents of junior middle school students in Jinan, China. Vaccine. 2015;33(22):2570–6. doi: 10.1016/j.vaccine.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Yu Y, Xu ML, Sun JD, Li R, Li M, Wang J, Zhang D, Xu A. Human papillomavirus infection and vaccination: awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong, China. PLoS One. 2016;11(1):e0146741. doi: 10.1371/journal.pone.0146741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang YR, Wang Y, Liu L, Fan Y, Liu Z, Wang Y, Nie S. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16(1):216. doi: 10.1186/s12889-016-2873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greyson D, Dubé È, Fisher WA, Cook J, Sadarangani M, Bettinger JA. Understanding influenza vaccination during pregnancy in Canada: attitudes, norms, intentions, and vaccine uptake. Health Educ Behav. 2021;48(5):680–9. doi: 10.1177/10901981211001863. [DOI] [PubMed] [Google Scholar]
- 22.Askelson NM, Campo S, Lowe JB, Smith S, Dennis LK, Andsager J. Using the theory of planned behavior to predict mothers’ intentions to vaccinate their daughters against HPV. J Sch Nurs. 2010;26(3):194–202. doi: 10.1177/1059840510366022. [DOI] [PubMed] [Google Scholar]
- 23.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 24.Trim K, Nagji N, Elit L, Roy K. Parental knowledge, attitudes, and behaviours towards human papillomavirus vaccination for their children: a systematic review from 2001 to 2011. Int J Gynecol Obstet. 2012;921236:1–12. doi: 10.1155/2012/921236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang LDL, Lam WWT, Fielding R. Determinants of human papillomavirus vaccination uptake among adolescent girls: a theory-based longitudinal study among Hong Kong Chinese parents. Prev Med. 2017;102:24–30. doi: 10.1016/j.ypmed.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 26.Shah SFA, Ginossar T, Bentley JM, Zimet G, McGrail JP. Using the theory of planned behavior to identify correlates of HPV vaccination uptake among college students attending a rural university in Alabama. Vaccine. 2021;39(51):7421–8. doi: 10.1016/j.vaccine.2021.10.082. [DOI] [PubMed] [Google Scholar]
- 27.Catalano HP, Knowlden AP, Birch DA, Leeper JD, Paschal AM, Usdan SL. Using the theory of planned behavior to predict HPV vaccination intentions of college men. J Amer Coll Health. 2017;65(3):197–207. doi: 10.1080/07448481.2016.1269771. [DOI] [PubMed] [Google Scholar]
- 28.Li L, Li JH. Factors affecting young Chinese women’s intentions to uptake human papillomavirus vaccination: an extension of the theory of planned behavior model. Hum Vaccin Immunother. 2020;16(12):3123–30. doi: 10.1080/21645515.2020.1779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juraskova I, O’Brien M, Mullan B, Bari R, Laidsaar-Powell R, McCaffery K. HPV vaccination and the effect of information framing on intentions and behaviour: an application of the theory of planned behaviour and moral norm. Int J Behav Med. 2012;19(4):518–25. doi: 10.1007/s12529-011-9182-5. [DOI] [PubMed] [Google Scholar]
- 30.Pan SY, Zhang D, Zhang JW. Caught in the crossfire: how contradictory information and norms on social media influence young women’s intentions to receive HPV vaccination in the United States and China. Front Psychol. 2020;11:548365. doi: 10.3389/fpsyg.2020.548365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zou ZR, Fairley CK, Ong JJ, Hocking J, Canfell K, Ma X, Chow EPF, Xu X, Zhang L, Zhuang G. Domestic HPV vaccine price and economic returns for cervical cancer prevention in China: a cost-effectiveness analysis. Lancet Glob Health. 2020;8(10):e1335–e44. doi: 10.1016/S2214-109X(20)30277-1. [DOI] [PubMed] [Google Scholar]
- 32.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lareyre O, Gourlan M, Stoebner-Delbarre A, Cousson-Gélie F. Characteristics and impact of theory of planned behavior interventions on smoking behavior: a systematic review of the literature. Prev Med. 2021;143:106327. doi: 10.1016/j.ypmed.2020.106327. [DOI] [PubMed] [Google Scholar]
- 34.Ajzen I. Residual effects of past on later behavior: habituation and reasoned action perspectives. Pers Soc Psychol Rev. 2002;6(2):107–22. doi: 10.1207/S15327957PSPR0602_02. [DOI] [Google Scholar]
- 35.Wijayanti KE, Schutze H, MacPhail C. Parents’ attitudes, beliefs and uptake of the school-based human papillomavirus (HPV) vaccination program in Jakarta, Indonesia – a quantitative study. Prev Med Reports. 2021;24:24; 101651. doi: 10.1016/j.pmedr.2021.101651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laura JH, Peter GS, Gregory Z, Saville AW, Gurfinkel D, Albertin C, Breck A, Vangala S, Kempe A. A validated modification of the vaccine hesitancy scale for childhood, influenza and HPV vaccines. Vaccine. 2021;39(13):1831–9. doi: 10.1016/j.vaccine.2021.02.039. [DOI] [PubMed] [Google Scholar]
- 37.Liuqing Y, Lili J, Qiang W, Xu Y, Yang G, Cui T, Shi N, Zhu L, Xiu S, Jin H, et al. Vaccination intention and behavior of the general public in China: cross-sectional survey and moderated mediation model analysis. JMIR Public Health Surveill. 2022;8(6):e34666. doi: 10.2196/34666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Minqi L, Tingting C, Qiang W, Han Y, Han Y, Yang L, Shi N, Yi Y, Jin H. Using an extended protection motivation theory to explain vaccine hesitancy: a cross-sectional study among Chinese adults. Hum Vaccin Immunother. 2022;18(1):2026136. doi: 10.1080/21645515.2022.2026136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gerbing DW, Anderson JC. Monte Carlo evaluations of goodness of fit indices for structural equation models. Soc Meth Res. 1992;21(2):132–60. doi: 10.1177/0049124192021002002. [DOI] [Google Scholar]
- 40.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 41.Zvara BJ, Schoppe-Sullivan SJ, Dush CK. Fathers’ involvement in child health care: associations with prenatal involvement, parents’ beliefs, and maternal gatekeeping. Fam Relat. 2013;62(4):649–61. doi: 10.1111/fare.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.The People’s Daily [Internet] . Six of the 15 healthy China pilot cities have launched free or subsidized HPV vaccination. 2021. [accessed 2023 Apr 20]. https://baijiahao.baidu.com/s?id=1717542890748588604&wfr=spider&for=pc.
- 43.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–80. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roberto AJ, Krieger JL, Katz ML, Goei, R., Jain, P.. Predicting pediatricians’ communication with parents about the human papillomavirus (hpv) vaccine: an application of the theory of reasoned action. Health Commun. 2011;26(4):303–12. doi: 10.1080/10410236.2010.550021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao F, Qiao Y. Cervical cancer prevention in China: a key to cancer control. Lancet. 2019;393(10175):9969–70. doi: 10.1016/S0140-6736(18)32849-6. [DOI] [PubMed] [Google Scholar]
- 46.Hu SY, Xu XQ, Zhang YY, Liu Y, Yang C, Wang Y, Wang Y, Yu Y, Hong Y, Zhang X, et al. A nationwide post-marketing survey of knowledge, attitude and practice toward human papillomavirus vaccine in general population: implications for vaccine roll-out in mainland China. Vaccine. 2021;39(1):35–44. doi: 10.1016/j.vaccine.2020.11.029. [DOI] [PubMed] [Google Scholar]
- 47.Qi Y. A study on new China’s family planning policy and its historical impact. Jilin (China): Jilin University of Finance and Economics; 2019. [Google Scholar]
- 48.Zhang LM, Yang J, Cao Y, Kang W. Sociocultural–psychological predictors influencing parents’ decision-making regarding HPV vaccination for their adolescent daughters in mainland China: an extended TPB model. Front Public Health. 2023;10(10):1035658. doi: 10.3389/fpubh.2022.1035658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qiu LR, Niu ZQ. Analysis of human papillomavirus vaccination status and its influencing factors in women aged 9 to 14 years. Chin Reprod Health. 2022;33:262–5. [Google Scholar]
- 50.Kornides M, Head KJ, Feemster K, Zimet GD, Panozzo CA. Associations between HPV vaccination among women and their 11–14-year-old children. Hum Vaccin Immunother. 2019;15(7–8):1824–30. doi: 10.1080/21645515.2019.1625642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hagger MS, Polet J, Lintunen T. The reasoned action approach applied to health behavior: role of past behavior and tests of some key moderators using meta-analytic structural equation modeling. Social Sci Med. 2018;213:85–94. doi: 10.1016/j.socscimed.2018.07.038. [DOI] [PubMed] [Google Scholar]
- 52.Lin YL, Su ZT, Chen FL, Zhao Q, Zimet GD, Alias H, He S, Hu Z, Wong LP. Chinese mothers’ intention to vaccinate daughters against human papillomavirus (HPV), and their vaccine preferences: a study in Fujian Province. Hum Vaccin Immunother. 2020;17(1):304–15. doi: 10.1080/21645515.2020.1756152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin W, Wang YY, Liu ZH, Chen B, Yuan S, Wu B, Gong L. Awareness and attitude towards human papillomavirus and its vaccine among females with and without daughter(s) who participated in cervical cancer screening in Shenzhen, China. Tro Med Internat Health. 2019;24(9):1054–63. doi: 10.1111/tmi.13283. [DOI] [PubMed] [Google Scholar]
- 54.Sobierajski T, Malecka I, Augustynowicz E. Feminized vaccine? Parents’ attitudes toward HPV vaccination of adolescents in Poland: a representative study. Hum Vaccin Immunother. 2023;19(1). doi: 10.1080/21645515.2023.2186105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Montalti M, Rallo F, Guaraldi F, Bartoli L, Po G, Stillo M, Perrone P, Squillace L, Dallolio L, Pandolfi P, et al. Would parents get their children vaccinated against SARS-CoV-2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines. 2021;9(4):366. doi: 10.3390/vaccines9040366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qi X, Jinshui W. Where is dad going? Father involvement in parenting and its impact on adolescent development in China. Res Soc Develop. 2019;6:68–85. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


