ABSTRACT
COVID-19 vaccine coverage in most countries in Africa remains low. Determinants of uptake need to be better understood to improve vaccination campaigns. Few studies from Africa have identified correlates of COVID-19 vaccination in the general population. We surveyed adults at 32 healthcare facilities across Malawi, purposively sampled to ensure balanced representation of adults with and without HIV. The survey, informed by the World Health Organization’s Behavioural and Social Drivers of Vaccination Framework, asked about people’s thoughts and feelings about the vaccine, social processes, motivation to vaccinate, and access issues. We classified respondents’ COVID-19 vaccination status and willingness to vaccinate, and used multivariable logistic regression to assess correlates of these. Among 837 surveyed individuals (median age was 39 years (IQR 30–49) and 56% were female), 33% were up-to-date on COVID-19 vaccination, 61% were unvaccinated, and 6% were overdue for a second dose. Those up-to-date were more likely to know someone who had died from COVID-19, feel the vaccine is important and safe, and perceive pro-vaccination social norms. Despite prevalent concerns about vaccine side effects, 54% of unvaccinated respondents were willing to vaccinate. Access issues were reported by 28% of unvaccinated but willing respondents. Up-to-date COVID-19 vaccination status was associated with positive attitudes about the vaccine and with perceiving pro-vaccination social norms. Over half of unvaccinated respondents were willing to get vaccinated. Disseminating vaccine safety messages from trusted sources and ensuring local vaccine availability may ultimately increase vaccine uptake.
KEYWORDS: COVID-19, vaccination, vaccine uptake, vaccine acceptance, Sub-Saharan Africa
Introduction
COVID-19 vaccines were introduced globally in late 2020, following a remarkably rapid vaccine development process – however, three years later, global inequities in coverage persist. As of early 2023, only approximately 28% of people in low-income countries – versus approximately 65% of people in lower-middle income countries and 80% of people in upper-middle and high income countries – have received at least one dose of a COVID-19 vaccine.1–5 As COVID-19 moves toward endemicity, vaccination remains an essential strategy for preventing serious illness, hospitalizations, and deaths related to the virus.
There have been well-documented supply-side factors constraining COVID-19 vaccine availability (and thus coverage) in low- and middle-income countries (LMICs), including delayed or incomplete delivery of promised vaccines, lack of local infrastructure and intellectual property to produce the vaccine locally, and high cost.6,7 There are also country-level challenges with vaccine delivery, and demand-side factors – such as vaccine hesitancy – that further contribute to low vaccine coverage.8
Elucidating these demand-side factors is crucial for designing vaccine delivery and communication strategies for optimizing vaccine uptake. However, most research about COVID-19 vaccine attitudes in LMICs was conducted prior to large-scale vaccine roll-out, or among specific sub-populations such as pregnant women or healthcare workers, and thus may not reflect vaccination decisions and behaviors among the general population.9–17 Since many LMICs do not routinely vaccinate adults,18,19 understanding determinants of COVID-19 vaccination could also help improve the delivery of other vaccines and health services for adults.19,20
As of April 2023, Malawi has reported 88,620 confirmed COVID-19 cases, and has vaccinated 4.8 million people, or about 20% of its population (with 3.7 million people fully vaccinated).21 However, the country has received enough vaccine doses for over double this number of people, indicating a gap between vaccine availability and vaccine uptake.7 There have been ongoing vaccination challenges; for example, the Malawi Ministry of Health destroyed about 20,000 vaccine doses in May 2021 because they expired before they could be used.22
Given low COVID-19 vaccination rates in Malawi, and a lack of information on factors shown to be associated with COVID-19 vaccine uptake in LMICs, we undertook a cross-sectional survey of Malawian adults in order to assess vaccine coverage and motivation to vaccinate among the unvaccinated, and to identify factors associated with vaccine uptake and motivation.
Materials and methods
Study design
We conducted a cross-sectional survey of adults presenting at health care facilities in Malawi, informed by the World Health Organization’s Behavioral and Social Drivers of Vaccination (BeSD) framework.23
Conceptual framework
The Behavioural and Social Drivers of Vaccination framework, established by the BeSD global working group in 2018, conceptualizes four distinct domains that drive vaccination, can be well-measured, and are potentially modifiable through intervention (Figure 1). This study uses the BeSD framework for COVID-19 vaccination specifically, including questions recommended by the World Health Organization (WHO) for measuring the four BeSD domains.
Figure 1.
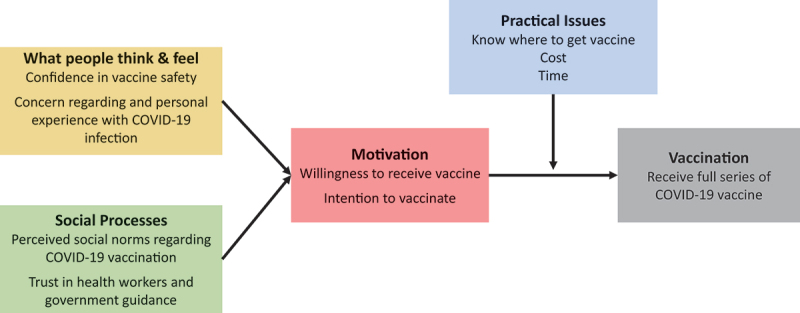
Conceptual framework, based upon the World Health Organization’s behavioral and social drivers of vaccination framework adapted for COVID-19 vaccination23.
Site & participant selection
The survey was administered at outpatient departments, antiretroviral therapy (ART) clinics treating people living with HIV, and non-communicable disease (NCD) clinics (primarily serving clients with hypertension or diabetes) at 32 health facilities. These facilities were purposively selected from the Partners in Hope PEPFAR/USAID-funded HIV care and treatment program to represent public and faith-based health facilities in urban, peri-urban, and rural areas across all three of Malawi’s regions (Northern, Central, and Southern). Eligible survey respondents at these participating health facilities were at least 18 years old; systematic random sampling was used, with every second individual in queue to see a provider at the clinic approached and invited to participate in the study. As people living with HIV were a priority group for COVID-19 vaccination in Malawi,24 we strove for half of our sample to be people living with HIV (PLHIV) so we could assess differences by HIV status. Our target sample size of 870 respondents was calculated based on to being able to detect a 5% difference in vaccination coverage (chosen to represent a programmatically-meaningful difference) between respondents with and without HIV with 95% confidence and 80% power.
Data collection
The survey tool included questions reflecting the four domains of the BeSD framework: what people think and feel about the vaccine (confidence in vaccine safety, concerns about contracting COVID-19 and about vaccine side effects), social processes (level of trust in healthcare workers and government information about COVID-19, perceived social norms such as whether community members are getting vaccinated or that family members think getting vaccinated is a good idea), motivation or intention to vaccinate, and practical (access) issues (anticipated and experienced logistical barriers to vaccination). We also asked respondents about their experiences with COVID-19 illness and with the COVID-19 vaccine. Individuals self-reported how many doses of COVID-19 vaccine they had received, as well as the manufacturer, date, and vaccination location for each dose. The survey instrument was developed in English and then translated to Chichewa, the local language, and was reviewed by bilingual (English/Chichewa) study team members to ensure clarity and meaning.
The survey was administered one-on-one in a private area at each participating health facility, by a trained research assistant. Research assistants adhered to the Malawi Ministry of Health’s COVID-19 Guidelines on Conducting Health Research in place at the time to minimize COVID-19 related risks, including maintaining physical distancing, proper use of personal protective equipment (PPE), and conducting activities outdoors when possible. Responses were recorded using the SurveyCTO mobile data collection platform on Android tablets. All respondents provided oral informed consent prior to the survey, and received 4000 Malawi kwacha (approximately US$5) as compensation for their participation. Data were collected from 19 May to 30 June, 2022. Ethical approval for the study was obtained from the National Health Sciences Research Committee in Malawi (#2883) and the University of California Los Angeles Institutional Review Board (#22–000380).
Variable definitions & data analysis
We classified individuals as up-to-date on COVID-19 vaccination if they had received: 1 or more doses of the Johnson & Johnson vaccine, 2 or more doses of any manufacturer’s vaccine, or 1 dose of a 2-dose series vaccine (AstraZeneca or Pfizer) but it had been 12 weeks or less since their first dose (as they were not yet overdue for their second dose). Unvaccinated individuals and those who had received one dose of a 2-dose series vaccine (AstraZeneca or Pfizer) more than 12 weeks prior were considered to be not up-to-date. Individuals who had received only one dose of a vaccine and did not know which vaccine type/manufacturer (n = 58) were excluded from the main analysis, as their up-to-date status could not be ascertained. A sensitivity analysis was conducted exploring vaccination status as either vaccinated (received 1+ doses of any COVID-19 vaccine) or unvaccinated (received zero doses).
Motivation to vaccinate among those unvaccinated was self-reported along a five-point scale from “eager to get a COVID-19 vaccine” to “anti-vaccination for COVID-19/extremely opposed to the COVID-19 vaccine.” For analysis, we compared three motivation categories: eager or willing, ambivalent, and anti-vaccination/opposed.
We used chi-squared, rank sum, and t-tests for univariate analyses, depending on the variable’s structure. Multivariable logistic regression was used to assess correlates of (1) being up-to-date on vaccination, (2) being motivated (eager/willing) to vaccinate, and (3) sensitivity analysis of being vaccinated (any doses). Adjusted odds ratios included all considered sociodemographic characteristics: gender, age (modeled as a categorical variable), HIV status, marital status, having children, residence (urban or rural), religion, clinic type where recruited, education, employment status, and household income adequacy (based on a previously-validated 6-point scale, and collapsed into a three-point scale: insufficient, just met expenses, or allowed for savings25). Regression models included clustered standard errors at the sampling level (health facility). P-values were considered to be statistically significant at the < 0.05 level, and were not corrected for multiple testing. All data cleaning, management, and analyses were conducted using Stata 17.0.26
Results
Sample description
A total of 895 individuals were surveyed; 58 respondents who had received one dose of a COVID-19 vaccine but did not recall the brand/manufacturer of the vaccine were excluded as their vaccination status could not be determined, resulting in an analytic sample of 837 individuals. Characteristics of the sample are shown in Table 1. Approximately 56% were female, three-quarters were married, 93% had children, and 82% lived in a rural area. Most respondents (70.1%) were employed, and 28.2% had completed secondary school or higher education. When asked about household income, 52.5% said their income over the past year had just met their expenses while 32% said it was insufficient. Most respondents were of Christian faith (n = 766, 91.5%), had no comorbidities (n = 671, 80.2%), and did not report having had COVID-19 in the past (n = 777, 92.8%).
Table 1.
Sample characteristics, stratified by up-to-date COVID-19 vaccination status.
| Overall (full sample) (n = 837) |
Not up-to-date on COVID-19 vaccination (n = 563) |
Up-to-date on COVID-19 vaccination (n = 274) |
||
| |
n (%) |
n (row %) |
n (row %) |
p-value |
| Gender | ||||
| Male | 365 (43.61%) | 240 (65.75%) | 125 (34.25%) | .413 |
| Female | 472 (56.39%) | 323 (68.43%) | 146 (30.93%) | |
| Age | ||||
| 18–29 | 199 (23.78%) | 158 (79.4%) | 41 (20.6%) | <.0001 |
| 30–39 | 226 (27%) | 163 (72.12%) | 63 (27.88%) | |
| 40–49 | 210 (25.09%) | 137 (65.24%) | 73 (34.76%) | |
| 50–59 | 117 (13.98%) | 67 (57.26%) | 50 (42.74%) | |
| 60+ | 85 (10.16%) | 38 (44.71%) | 47 (55.29%) | |
| Median (IQR) | 39 (30–49) | 36 (28–47) | 44 (34–55) | <.0001 |
| HIV status | ||||
| HIV negative or unknown | 412 (49.22%) | 276 (66.99%) | 136 (33.01%) | .868 |
| Living with HIV | 425 (50.78%) | 287 (67.53%) | 138 (32.47%) | |
| Among those living with HIV: On ART | 424 (99.76%) | 286 (67.45%) | 138 (32.55%) | |
| Marital status | ||||
| Unmarried | 207 (24.73%) | 137 (66.18%) | 70 (33.82%) | .703 |
| Married | 630 (75.27%) | 426 (67.62%) | 204 (32.38%) | |
| Have children | ||||
| Yes | 778 (92.95%) | 517 (66.45%) | 261 (33.55%) | .069 |
| No | 59 (7.05%) | 46 (77.97%) | 13 (22.03%) | |
| Place of residence | ||||
| Urban | 154 (18.4%) | 103 (66.88%) | 51 (33.12%) | .911 |
| Rural | 683 (81.6%) | 460 (67.35%) | 223 (32.65%) | |
| Religion | ||||
| Christian | 766 (91.52%) | 513 (66.97%) | 253 (33.03%) | .786 |
| Other religion | 45 (5.38%) | 31 (68.89%) | 14 (31.11%) | |
| Not religious | 26 (3.11%) | 19 (73.08%) | 7 (26.92%) | |
| Clinic type recruited from | ||||
| ART clinic | 410 (48.98%) | 278 (67.8%) | 132 (32.2%) | <.001 |
| Outpatient department (OPD) | 350 (41.82%) | 252 (72%) | 98 (28%) | |
| Non-communicable disease clinic (NCD) | 77 (9.2%) | 33 (42.86%) | 44 (57.14%) | |
| Educational attainment (highest completed) | ||||
| None | 225 (26.88%) | 166 (73.78%) | 59 (26.22%) | .034 |
| Primary school | 376 (44.92%) | 249 (66.22%) | 127 (33.78%) | |
| Secondary school or higher | 236 (28.20%) | 148 (62.71%) | 88 (37.29%) | |
| Employment status | ||||
| Employed | 587 (70.13%) | 385 (65.59%) | 202 (34.41%) | .113 |
| Not employed | 250 (29.87%) | 178 (71.2%) | 72 (28.8%) | |
| Household income adequacy over past year | ||||
| Insufficient | 253 (30.23%) | 171 (67.59%) | 82 (32.41%) | .51 |
| Just met expenses | 416 (49.7%) | 288 (69.23%) | 128 (30.77%) | |
| Allowed for saving | 124 (14.81%) | 79 (63.71%) | 45 (36.29%) |
Vaccination information
Of the 837 respondents, 39.1% (n = 327) had received at least one dose of a COVID-19 vaccine and 60.9% (n = 510) were unvaccinated.
Among the 327 vaccinated respondents, 57.5% received the AstraZeneca vaccine (n = 188), and 30.9% (n = 101) received the Johnson & Johnson vaccine; approximately 11% of respondents did not know or report which brand they received but had received 2 doses or more, and 2 had received the Pfizer vaccine. The vast majority (89%) reported that their main motivation for getting vaccinated was to protect themselves. Approximately half of respondents (n = 175, 53.5%) had received their first dose at a public health facility, and 20.2% of respondents (n = 66) had received it through a community-based program (full information on locations and timing of vaccine doses available in Appendix Table A1).
Overall, nearly one in three respondents (n = 274, 32.7%) was up-to-date on COVID-19 vaccination. The remaining two-thirds (n = 563, 66.3%) were not up-to-date, including 53 respondents who had started the vaccine series but were overdue for a second dose.
Correlates of up-to-date vaccination status
Demographic correlates
Over half (55.3%) of people 60+ years old were up-to-date on COVID-19 vaccination, as compared to one-fifth (20.6%) of respondents under the age of 30 (p < .0001) (Table 1). Being up-to-date was more common among people with a secondary school education or higher, versus no school (37.3% versus 26.2%, p = .03). Respondents recruited from NCD clinics were most likely to be up-to-date (57.1%, versus 32.2% of those recruited from ART clinics and 28.0% of those recruited from outpatient departments, p < .001). Vaccination status did not differ by HIV status. In an adjusted model including all considered demographic correlates, only age (>40 years), being recruited from an NCD clinic, and having completed secondary school or higher were significant predictors of up-to-date vaccination status (Appendix Table A3). Results were similar in a sensitivity analysis assessing any vaccination (Appendix Table A2), with age, education, and clinic type remaining significantly associated with uptake in bivariate and adjusted models; household income was also associated, with lower vaccine uptake among those whose household income only just met expenses in the past year.
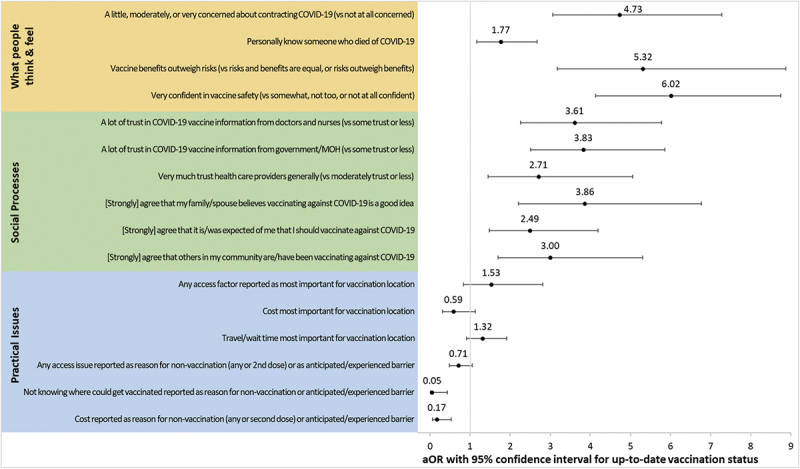
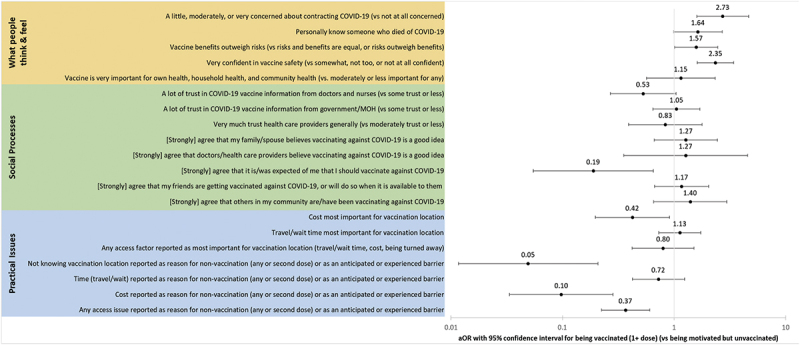
Thinking and feeling
Individuals who were up-to-date on COVID-19 vaccination were more likely to know someone who had illness or died from COVID-19 (had COVID-19: 73.4%, versus 64.1% of those not up-to-date, p = .008; died from COVID-19: 59%, versus 41% of those not up-to-date, p < .001). In adjusted models, knowing someone who had died due to COVID-19 was associated with a significantly higher odds of being up-to-date (aOR 1.77, 95% CI 1.17–2.67) (Figure 2). Those who were concerned about contracting COVID-19 were also more likely to be up-to-date on vaccination (aOR 4.73, 95% CI 3.07–7.28) than those who were not at all concerned. Being up-to-date on COVID-19 vaccination was strongly associated with feeling the vaccine is important for health (of oneself, of one’s household and community members), that it is safe, and that its benefits outweigh its potential risks.
Figure 2.
Correlates of being up-to-date on COVID-19 vaccination across WHO BeSD Domains of practical issues, social processes, and what people think and feel.
Social processes
Perceiving pro-vaccination community and social norms was associated with up-to-date vaccination status (Figure 2): for example, those who agreed that one’s family or spouse believes vaccinating is a good idea had higher odds of being up-to-date (aOR 3.86, 95%CI 2.21–6.77), as were those who agreed that other community members are getting vaccinated (aOR 3.00, 95%CI 1.70–5.31). Having strong trust in health care workers (aOR 2.71, 95%CI 1.45–5.06) and in information about the vaccine from the Ministry of Health (aOR 3.83, 95%CI 2.50–5.86) and from health care workers (aOR 3.61, 95%CI 2.26–5.78) were also correlated with up-to-date vaccination status.
Practical issues
Practical issues were generally not strongly associated with up-to-date vaccination status (Figure 2), although not knowing where one could get vaccinated and concern about costs (including travel costs) of seeking and receiving the vaccine were associated with decreased odds of being up-to-date (not knowing where to get vaccine: aOR 0.05, 95%CI 0.01–0.43, p = .006; costs: aOR 0.17, 95%CI 0.06–0.53, p = .002). Those who reported any access-related factor (such as cost, time, or being turned away) as being most important in choosing a vaccination location did not have significantly higher odds of being up-to-date on vaccination (aOR 1.53, 95%CI 0.83–2.81, p = .171).
Results for all three domains (thinking and feeling, social processes, practical issues) were similar across in sensitivity analyses that used the outcome variable of uptake of any COVID-19 vaccine doses (Appendix Figure A1).
Correlates of vaccine uptake among those motivated to vaccinate
We compared vaccinated respondents to respondents who said they were motivated (eager/willing) but unvaccinated, to understand what factors were associated with successfully achieving vaccination among those wanting to do so.
Motivated but unvaccinated respondents (n = 274) were younger (median age 35 versus 43, p < .0001) and more likely to be female (59.9%, versus 51.7%, p = .045), rural residents (87.6% versus 79.5%, p = .008), to have no schooling (29.6% versus 20.5%, p = .002), and to report household income just meeting expenses over the past 12 months (55.8% versus 44.3%, p = .032), than people who had achieved vaccination (n = 327) (Appendix Table A4). Adjusting for these factors, many thinking and feeling correlates were more common among people who achieved vaccination compared to those who were motivated but unvaccinated (Appendix Figure A2) – including being very confident in vaccine safety, being concerned about contracting COVID-19, and knowing someone who had died of COVID-19 – while social process variables were largely uncorrelated with achieving vaccination (Appendix Figure A2). Practical issues were associated with decreased odds of achieving vaccination among those motivated (Appendix Figure A2).
Vaccination attitudes and barriers among the unvaccinated
Just over half of unvaccinated respondents said they had been offered the COVID-19 vaccine (n = 276, 54.1%) and 45.9% had not (n = 234). Women were more likely to have been offered the vaccine (57.8% of unvaccinated women versus 48.8% of unvaccinated men, p = .046), as were individuals aged 30 years or older (59.0% versus 42.3% of those 18–29 years, p = .001), respondents with children (56.6% versus 25.0% of those without children, p < .001), and married respondents (56.6% of married versus 46.4% of unmarried, p = .046); there was no difference by HIV status (Appendix Table A5).
We asked unvaccinated respondents about their current motivation to get vaccinated against COVID-19. Approximately half (53.7%) were eager or willing to get the vaccine, 28.6% were neutral or ambivalent, and 17.7% were opposed. There were no significant differences in motivation between people who had and had not been offered the vaccine. Compared to their counterparts, rural respondents were more likely to be eager/willing to vaccinate (56.7% vs 39.1% of urban respondents, p = .001), as were those who self-identified as not religious (88.9% vs 52.4% of Christians and 53.6% of those who identified with another religion, p = .047) and those who had a primary school education (59.6% vs 51.3% of those with no school, 49.5% of those with a secondary school education, and 25.0% of those with higher education, p = .021). There were no significant differences in motivation to vaccinate by gender, age, marital status, having children, HIV status, or income (Appendix Table A6).
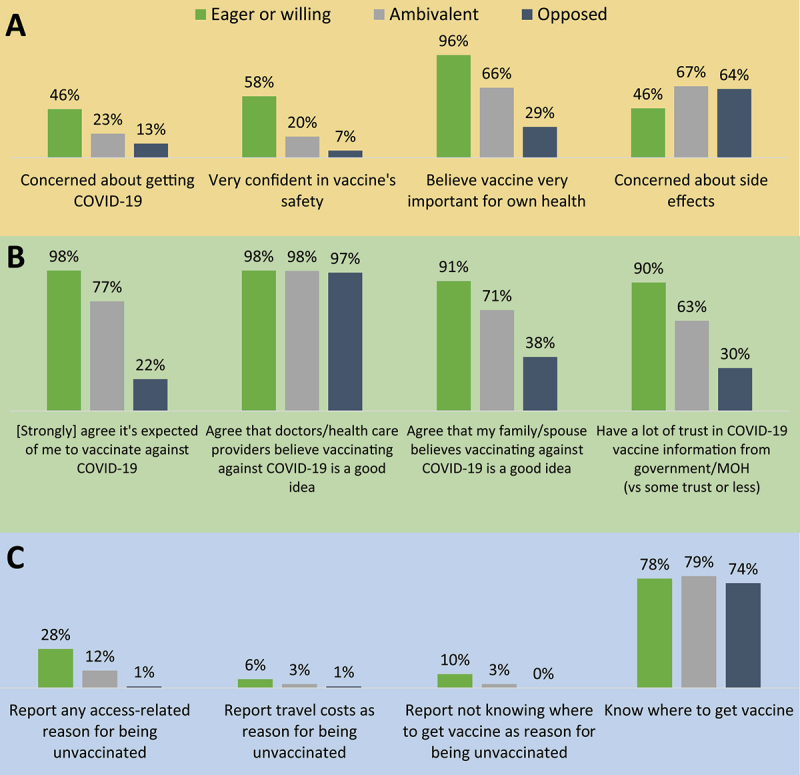
Thinking and feeling
Individuals who were eager/willing to get vaccinated were most concerned about contracting COVID-19, and were confident in the vaccine’s safety and importance, while those opposed to vaccination were the least convinced of the vaccine’s safety and importance (Figure 3A). Concerns regarding long- and short-term side effects from the vaccine were common, especially among those less eager to vaccinate: about two-thirds of ambivalent (67%) and opposed (64%) individuals reported concerns about side effects as a reason for being unvaccinated, as compared to 46% of those who were eager/willing to get vaccinated (p < .001). Feeling that the vaccine was unnecessary, too new, or “satanic” were each reported by approximately 10% of unvaccinated respondents.
Figure 3.
Beliefs, attitudes, and reasons for being unvaccinated among 510 Malawian adults who had not been vaccinated against COVID-19, per WHO BeSD framework domains: (a) what people think and feel; (b) social processes; and (c) practical issues.
Social processes
Individuals who were eager/willing to get vaccinated largely perceived pro-vaccination social norms, while significantly lower proportions of the ambivalent and opposed did so (Figure 3B): for example, 98% of those eager or willing to vaccinate felt that it was expected of them to get vaccinated, versus 77% of ambivalent and 22% of opposed individuals (p < .001). Perceiving that doctors and healthcare providers believe COVID-19 vaccination was a good idea was almost universal, with 97–98% agreeing, regardless of motivation to vaccinate.
Practical issues
Practical issues and concerns were more common among individuals who were eager/willing to vaccinate than those neutral or opposed (Figure 3C). Twenty-eight percent reported any access-related reason for being unvaccinated, such as time or costs associated with traveling to get vaccinated or not knowing where to get vaccinated, while only 1% of those opposed to vaccination reported these reasons. The majority of unvaccinated respondents knew where they could get the COVID-19 vaccine, with no difference by willingness to vaccinate. Practical issues were also salient when thinking about where to get vaccinated: when asked what is the most important factor when choosing a preferred vaccination location, travel time was the most common across all three levels of motivation.
Discussion
In this sample, 33% of Malawian adults presenting at healthcare facilities in mid-2022 were up-to-date on COVID-19 vaccination – significantly higher than national figures which indicated that only 10% of the population had received at least one dose by July 2022.27,28 Notably, respondents for this survey were older29 and more educated30 than Malawi’s general population, were recruited at health facilities, and likely reflect a population with more interaction with the health system and easier access to the vaccine.
Older individuals and respondents recruited from non-communicable diseases clinics were more likely to be up-to-date on COVID-19 vaccination – suggesting that, as previously reported,17 Malawi’s national COVID-19 vaccination program successfully targeted older individuals and those with comorbidities.24 However, despite the Malawi COVID-19 Vaccine National Deployment Plan listing people living with HIV as another priority group,24 our survey found no difference in vaccination by HIV status – suggesting that NCD clinics have been more successfully leveraged as an opportunity for vaccination compared to ART clinics. Since this study, activities specifically aiming to increase vaccination among people living with HIV have been implemented at ART clinics, including demand creation health talks, systematic screening for vaccination status, and offering the COVID-19 vaccine during clinic visits.31
In this study, what people think and feel about the COVID-19 vaccine – especially its safety and benefits – was correlated with up-to-date vaccination status and, among the unvaccinated, with being eager or willing to get vaccinated. Concerns about vaccine side effects were very common: about two-thirds of respondents ambivalent and opposed to vaccination and about half of those willing to vaccinate reported side effect concerns as a reason for being unvaccinated. These findings reinforce previous work in Malawi and in other settings in Africa showing that concerns regarding COVID-19 vaccine safety, effectiveness, and side effects are prevalent and a major reason for vaccine hesitancy,12,17,33–40 and that being concerned about COVID-19 infection and having positive perceptions of the vaccine are associated with vaccine uptake and willingness to vaccinate.34,38–40 Interventions that can change people’s attitudes will therefore be important for increasing vaccine uptake, such as educational campaigns and dialogue-based interventions like one-on-one counseling.23
We also found that trusting the healthcare system and government, perceiving societal acceptance of COVID-19 vaccination, and feeling expected to vaccinate (social processes) were strong correlates of being both up-to-date on vaccination and motivated to vaccinate. Other studies have likewise identified how social processes affect COVID-19 vaccination: a qualitative study conducted in Malawi found that some unvaccinated people felt that governmental pressure to vaccinate was infringing on their personal autonomy,33 and a study from Nigeria found that individuals who intended to or had vaccinated against COVID-19 perceived greater approval/encouragement from their family, friends, and community leaders.41 Studies in Ethiopia, South Africa, and a large multi-country survey have also shown trust in the government to be associated with COVID-19 vaccination motivation or hesitancy.32,42,43 These findings highlight how norms and trust may be leveraged to motivate vaccination attitudes and behaviors, for example by disseminating interventions via trusted sources. Although most unvaccinated respondents in our study said that healthcare workers and the government/ministry of health was a trusted source of vaccine information, individuals who were opposed to vaccination had the lowest levels of trust in the health system. Therefore, to reach the most hesitant, programs should engage other trusted messengers, such as religious leaders and community members. Dialogue-based interventions, community engagement, and engaging “vaccine champions” have been identified by the WHO as promising strategies for modifying social processes driving vaccination.23 Other approaches that capitalize on social norms and pressures could include social media campaigns where individuals share their vaccination experiences or disseminating storytelling narrative videos.44
Practical issues were strong predictors of achieving vaccination among those motivated to vaccinate, suggesting that addressing access barriers (such as time, travel costs, and knowing where to get vaccinated) is key to ensuring uptake among those who want to be vaccinated. In our sample, 51% of people who wanted to get vaccinated reported an anticipated or experienced access-related barrier to vaccination. Clearer communication about vaccination locations, financial incentives or reimbursements for travel costs or lost wages, and community-based vaccination campaigns could thus increase uptake among those already motivated to vaccinate. In April 2022, Malawi introduced the “Vaccinate my village” strategy, in which community health workers offered door-to-door COVID-19 vaccination – and it is estimated that this contributed to a three-fold increase in national vaccine coverage.45
Over half of unvaccinated respondents in our sample reported having been offered the COVID-19 vaccine, so vaccine acceptance may be a challenge in this group. Unvaccinated respondents with children (both men and women) were more likely to report having been offered the than unvaccinated respondents without children; parents may encounter more opportunities for COVID-19 vaccination due to more frequent interaction with the health system when their children need care. Additionally, among both those with and without children, women were more likely to report offer of vaccination. This gender difference was especially pronounced among those without children, and may reflect that in Malawi, women interface more often with the healthcare system than men,46 not only for child-related care but also for services such as family planning and antenatal care. To achieve high population coverage, programs must reach people who are less likely to routinely encounter opportunities for vaccination.
We found that respondents who were motivated but unvaccinated were more likely than vaccinated respondents to be younger, female, rural residents, and less educated. These sociodemographic characteristics may make it harder to translate vaccination intentions into action, for example via reduced autonomy or access to health services. Identifying factors that separate the vaccinated from those that are motivated to vaccinate but unvaccinated is important for identifying populations for whom improved access will have the greatest impact.
We acknowledge several limitations of this study. Respondents were recruited at health facilities; our sample thus likely over-represents people with greater health care use, greater trust in the health care system and providers, and/or better access to health services. The higher COVID-19 vaccination coverage in this study (compared to national data) also reflects our over-sampling of older adults (who were a target population for vaccination). Secondly, vaccination status was ascertained based on self-report, which may have been influenced by social desirability bias. Social desirability bias also might have influenced self-report of vaccine attitudes and trust in healthcare workers, particularly because the survey was conducted face-to-face in a health care setting. Third, it is possible that some of these factors are correlated, and there may be vaccination “types” that combine determinants. Although beyond the design and scope of this study, we encourage future research that aims to identify such “types” – as this could represent a more efficient approach to developing and targeting interventions for specific groups. Lastly, as this was a cross-sectional study, we were not able to assess changes in vaccine attitudes or uptake over time. Strengths of this study include representing all three geographic regions in Malawi, including adults across the lifespan, and having been conducted while COVID-19 vaccines were available to the general public – which allowed us to explore correlates of actual vaccine uptake, rather than reported vaccination intentions.
In conclusion, in this study of Malawian adults, up-to-date COVID-19 vaccination status was associated with positive attitudes about the vaccine’s importance and safety, and perceiving pro-vaccination social norms. Over half of unvaccinated respondents were willing to get vaccinated, but many were concerned about vaccine side effects or faced logistical barriers to accessing the vaccine. Disseminating accurate messages about vaccine safety by trusted sources and ensuring availability of the vaccine may help increase COVID-19 vaccine coverage in Malawi.
Acknowledgments
We are deeply grateful for the field assistants for their excellent work collecting these data, all respondents for sharing their experiences and perspectives with us, the participating health facilities and their management for enabling the conduct of this study, and Partners in Hope program leadership and the Science Department for supporting this study. We also thank the Demand and Behavioural Sciences group at the Essential Programme on Immunization for sharing information about the BeSD COVID-19 tools with our team.
Appendix.
Table A1.
COVID-19 vaccination details by vaccination status, among those with 1+ dose.
| All with 1+ dose n = 327 |
Overdue for 2nd dose n = 53 |
Up-to-date n = 274 |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Vaccine brand/manufacturer (1st dose) | ||||||
| Don’t know/refuse | 36 | 11.0% | 0 | 0.0% | 36 | 100% |
| AstraZeneca | 188 | 57.5% | 52 | 27.7% | 136 | 72.3% |
| Pfizer | 2 | 0.6% | 1 | 50.0% | 1 | 50.0% |
| Johnson & Johnson | 101 | 30.9% | 0 | 0.0% | 101 | 100% |
| Vaccination location (1st dose) | ||||||
| Public health facility | 175 | 53.5% | 23 | 13.1% | 152 | 86.9% |
| CHAM health facility | 29 | 8.9% | 5 | 17.2% | 23 | 79.3% |
| Community health worker | 52 | 15.9% | 11 | 21.2% | 41 | 78.8% |
| Vaccine program in the community | 66 | 20.2% | 12 | 18.2% | 54 | 81.8% |
| Private health facility | 6 | 1.8% | 2 | 33.3% | 4 | 66.7% |
| Vaccination timing (1st dose) | ||||||
| March – May 2021 | 55 | 16.8% | 8 | 14.5% | 47 | 85.5% |
| June – August 2021 | 51 | 15.6% | 9 | 17.6% | 42 | 82.4% |
| September – November 2021 | 61 | 18.7% | 14 | 23.0% | 47 | 77.0% |
| December 2021 - February 2022 | 80 | 24.5% | 21 | 26.3% | 59 | 73.8% |
| March – June 2022 | 42 | 12.8% | 1 | 2.4% | 41 | 97.6% |
| Date unknown |
38 |
11.6% |
0 |
0.0% |
38 |
100.0% |
| Received 2+ doses & up-to-date n = 163 |
||||||
| |
n |
% |
||||
| Received 3 doses | 8 | 4.9% | ||||
| Vaccine brands mixed | 5 | 3.1% | ||||
| Doses received at different locations | 33 | 20.2% | ||||
| Timing between 1st and 2nd doses | ||||||
| <8 weeks | 5 | 3.1% | ||||
| 8–12 weeks (recommended) | 21 | 12.9% | ||||
| >12 weeks | 105 | 64.4% | ||||
| Vaccine brand/manufacturer (2nd dose) | ||||||
| Don’t know/refuse | 28 | 17.2% | ||||
| AstraZeneca | 28 | 17.2% | ||||
| Pfizer | 1 | 0.6% | ||||
| Johnson & Johnson | 1 | 0.6% | ||||
| Vaccination location (2nd dose) | ||||||
| Public health facility | 91 | 55.8% | ||||
| CHAM health facility | 13 | 8.0% | ||||
| Community health worker | 24 | 14.7% | ||||
| Vaccine program in the community | 32 | 19.6% | ||||
| Private health facility | 3 | 1.8% | ||||
| Vaccination timing (2nd dose) | ||||||
| March – May 2021 | 3 | 1.8% | ||||
| June – August 2021 | 30 | 18.4% | ||||
| September – November 2021 | 23 | 14.1% | ||||
| December 2021 - February 2022 | 41 | 25.2% | ||||
| March – June 2022 | 34 | 20.9% | ||||
| Date unknown | 32 | 19.6% | ||||
Table A2.
Sample characteristics, stratified by COVID-19 vaccination status (sensitivity analysis: vaccinated (1+ doses) vs unvaccinated (0 doses)).
| Overall | Unvaccinated (0 doses) |
Vaccinated (1+ doses) |
p-value | aOR (95%CI) for vaccinated | ||||
|---|---|---|---|---|---|---|---|---|
| (n = 837) |
(n = 510) |
(n = 327) |
||||||
| n | Col % | n | Row % | n | Row % | |||
| Gender | ||||||||
| Male | 365 | 43.6% | 207 | 56.7% | 158 | 43.3% | .028 | 1 |
| Female | 472 | 56.4% | 303 | 64.2% | 169 | 35.8% | 1.0 (0.70–1.43) | |
| Age | ||||||||
| 18–29 | 199 | 23.8% | 149 | 74.9% | 50 | 25.1% | <.001 | 1 |
| 30–39 | 226 | 27.0% | 153 | 67.7% | 73 | 32.3% | 1.71 (1.05–2.79) | |
| 40–49 | 210 | 25.1% | 117 | 55.7% | 93 | 44.3% | 3.02 (1.83–5.00) | |
| 50–59 | 117 | 14.0% | 56 | 47.9% | 61 | 52.1% | 3.67 (1.97–6.84) | |
| 60+ | 85 | 10.2% | 35 | 41.2% | 50 | 58.8% | 4.69 (2.35–9.39) | |
| Median (IQR) | 39 | (30–49) | 35 | (28–46) | 43 | (35–52) | <.001 | |
| HIV status | ||||||||
| HIV- or unknown | 412 | 49.2% | 247 | 60.0% | 165 | 40.0% | .567 | 1 |
| Living with HIV | 425 | 50.8% | 263 | 61.9% | 162 | 38.1% | 0.55 (0.30–1.03) | |
| Among those living with HIV: On ART | 424 | 99.8% | 262 | 61.8% | 162 | 38.2% | .432 | |
| Marital status | ||||||||
| Unmarried | 207 | 24.7% | 125 | 60.4% | 82 | 39.6% | .853 | 1 |
| Married | 630 | 75.3% | 385 | 61.1% | 245 | 38.9% | 1.05 (0.72–1.53) | |
| Have children | 0.0% | |||||||
| Yes | 778 | 93.0% | 470 | 60.4% | 308 | 39.6% | .262 | 0.78 (0.36–1.73) |
| No | 59 | 7.0% | 40 | 67.8% | 19 | 32.2% | 1 | |
| Place of residence | ||||||||
| Urban | 154 | 18.4% | 87 | 56.5% | 67 | 43.5% | .211 | 1 |
| Rural | 683 | 81.6% | 423 | 61.9% | 260 | 38.1% | 1.15 (0.71–1.85) | |
| Religion | ||||||||
| Christian | 766 | 91.5% | 464 | 60.6% | 302 | 39.4% | .662 | 1 |
| Other religion | 45 | 5.4% | 28 | 62.2% | 17 | 37.8% | 1.04 (0.50–2.15) | |
| Not religious | 26 | 3.1% | 18 | 69.2% | 8 | 30.8% | 0.66 (0.22–1.98) | |
| Clinic type recruited from | ||||||||
| ART | 410 | 49.0% | 251 | 61.2% | 159 | 38.8% | <.001 | 1.88 (1.03–3.43) |
| Outpatient department (OPD) | 350 | 41.8% | 228 | 65.1% | 122 | 34.9% | 1 | |
| Non-communicable disease clinic (NCD) | 77 | 9.2% | 31 | 40.3% | 46 | 59.7% | 1.83 (0.96–3.48) | |
| Educational attainment | ||||||||
| None | 225 | 26.9% | 158 | 70.2% | 67 | 29.8% | .001 | 1 |
| Primary school | 376 | 44.9% | 225 | 59.8% | 151 | 40.2% | 1.75 (1.17–2.61) | |
| Secondary school or higher | 236 | 28.2% | 127 | 53.8% | 109 | 46.2% | 2.52 (1.68–3.80) | |
| Employment status | ||||||||
| Employed | 587 | 70.1% | 346 | 58.9% | 241 | 41.1% | .071 | 1 |
| Not employed | 250 | 29.9% | 164 | 65.6% | 86 | 34.4% | 0.78 (0.53–1.15) | |
| Household income adequacy over past 12 months | ||||||||
| Insufficient | 253 | 30.2% | 147 | 58.1% | 106 | 41.9% | .069 | 1 |
| Just met expenses | 416 | 49.7% | 271 | 65.1% | 145 | 34.9% | 0.66 (0.44–0.98) | |
| Allowed for saving | 124 | 14.8% | 69 | 55.6% | 55 | 44.4% | 0.94 (0.64–1.37) | |
Table A3.
Sample characteristics, stratified by up-to-date COVID-19 vaccination status, and adjusted Odds Ratios for being up-to-date (adjusting for all displayed characteristics).
| Overall (full sample) | Not up-to-date on COVID-19 vaccination | Up-to-date on COVID-19 vaccination | p-value | aOR (95%CI) for being up-to-date on COVID-19 vaccination | ||||
|---|---|---|---|---|---|---|---|---|
| (n = 837) |
(n = 563) |
(n = 274) |
||||||
| n | Col % | n | Row % | n | Row % | |||
| Gender | ||||||||
| Male | 365 | 43.61 | 240 | 65.75 | 125 | 34.25 | .413 | 1 |
| Female | 472 | 56.39 | 323 | 68.43 | 146 | 30.93 | 1.14 (0.75–1.72) | |
| Age | ||||||||
| 18–29 | 199 | 23.78 | 158 | 79.4 | 41 | 20.6 | <.0001 | 1 |
| 30–39 | 226 | 27 | 163 | 72.12 | 63 | 27.88 | 1.59 (0.94–2.67) | |
| 40–49 | 210 | 25.09 | 137 | 65.24 | 73 | 34.76 | 2.28 (1.34–3.90) | |
| 50–59 | 117 | 13.98 | 67 | 57.26 | 50 | 42.74 | 2.73 (1.45–5.14) | |
| 60+ | 85 | 10.16 | 38 | 44.71 | 47 | 55.29 | 4.34 (1.93–9.78) | |
| Median (IQR) | 39 | (30–49) | 36 | (28–47) | 44 | (34–55) | <.0001 | |
| HIV status | ||||||||
| HIV- or unknown | 412 | 49.22 | 276 | 66.99 | 136 | 33.01 | .868 | 1 |
| Living with HIV | 425 | 50.78 | 287 | 67.53 | 138 | 32.47 | 0.84 (0.48–1.47) | |
| Among those living with HIV: On ART | 424 | 99.76 | 286 | 67.45 | 138 | 32.55 | ||
| Marital status | ||||||||
| Unmarried | 207 | 24.73 | 137 | 66.18 | 70 | 33.82 | .703 | 1 |
| Married | 630 | 75.27 | 426 | 67.62 | 204 | 32.38 | 1.01 (0.68–1.50) | |
| Have children | ||||||||
| Yes | 778 | 92.95 | 517 | 66.45 | 261 | 33.55 | 0.069 | 1.17 (0.52–2.65) |
| No | 59 | 7.05 | 46 | 77.97 | 13 | 22.03 | 1 | |
| Place of residence | ||||||||
| Urban | 154 | 18.4 | 103 | 66.88 | 51 | 33.12 | 0.911 | 1 |
| Rural | 683 | 81.6 | 460 | 67.35 | 223 | 32.65 | 1.40 (0.94–2.10) | |
| Religion | ||||||||
| Christian | 766 | 91.52 | 513 | 66.97 | 253 | 33.03 | 0.786 | 1 |
| Other religion | 45 | 5.38 | 31 | 68.89 | 14 | 31.11 | 0.91 (0.43–1.96) | |
| Not religious | 26 | 3.11 | 19 | 73.08 | 7 | 26.92 | 0.72 (0.24–2.18) | |
| Clinic type recruited from | ||||||||
| ART | 410 | 48.98 | 278 | 67.8 | 132 | 32.2 | <0.001 | 1.30 (0.74–2.29) |
| Outpatient department (OPD) | 350 | 41.82 | 252 | 72 | 98 | 28.00 | 1 | |
| Non-communicable disease clinic (NCD) | 77 | 9.2 | 33 | 42.86 | 44 | 57.14 | 2.26 (1.19–4.30) | |
| Educational attainment | ||||||||
| None | 225 | 26.88 | 166 | 73.78 | 59 | 26.22 | 0.034 | 1 |
| Primary school | 376 | 44.92 | 249 | 66.22 | 127 | 33.78 | 1.55 (1.00–2.39) | |
| Secondary school or higher | 236 | 28.2 | 148 | 62.71 | 88 | 37.29 | 2.24 (1.47–3.43) | |
| Employment status | ||||||||
| Employed | 587 | 70.13 | 385 | 65.59 | 202 | 34.41 | 0.113 | 1 |
| Not employed | 250 | 29.87 | 178 | 71.2 | 72 | 28.8 | 0.76 (0.51–1.12) | |
| Household income adequacy over past 12 months | ||||||||
| Insufficient | 253 | 30.23 | 171 | 67.59 | 82 | 32.41 | 0.51 | 1 |
| Just met expenses | 416 | 49.7 | 288 | 69.23 | 128 | 30.77 | 0.82 (0.54–1.24) | |
| Allowed for saving | 124 | 14.81 | 79 | 63.71 | 45 | 36.29 | 1.02 (0.70–1.49) | |
Table A4.
Sample characteristics among those unvaccinated but motivated to vaccinate and those with 1+ dose of a COVID-19 vaccine.
| Motivated but unvaccinated | Vaccinated, 1+ dose |
||||
|---|---|---|---|---|---|
| (n = 274) |
(n = 327) |
||||
| n | % | n | % | p-value | |
| Gender | |||||
| Male | 110 | 40.1% | 158 | 48.3% | .045 |
| Female | 164 | 59.9% | 169 | 51.7% | |
| Age | |||||
| 18–29 | 85 | 31.0% | 50 | 15.3% | <.001 |
| 30–39 | 84 | 30.7% | 73 | 22.3% | |
| 40–49 | 56 | 20.4% | 93 | 28.4% | |
| 50–59 | 29 | 10.6% | 61 | 18.7% | |
| 60+ | 20 | 7.3% | 50 | 15.3% | |
| Median (IQR) | 35 | (28–46) | 43 | (35–52) | <.0001 |
| HIV status | |||||
| HIV- or unknown | 134 | 48.9% | 165 | 50.5% | .704 |
| Living with HIV | 140 | 51.1% | 162 | 49.5% | |
| Among those living with HIV: On ART | 139 | 99.3% | 162 | 100.0% | |
| Marital status | |||||
| Unmarried | 72 | 26.3% | 82 | 25.1% | .737 |
| Married | 202 | 73.7% | 245 | 74.9% | |
| Have children | |||||
| Yes | 251 | 91.6% | 308 | 94.2% | .216 |
| No | 23 | 8.4% | 19 | 5.8% | |
| Place of residence | |||||
| Urban | 34 | 12.4% | 67 | 20.5% | .008 |
| Rural | 240 | 87.6% | 260 | 79.5% | |
| Religion | |||||
| Christian | 243 | 88.7% | 302 | 92.4% | .103 |
| Other religion | 15 | 5.5% | 17 | 5.2% | |
| Not religious | 16 | 5.8% | 8 | 2.4% | |
| Clinic type recruited from | |||||
| ART clinic | 134 | 48.9% | 159 | 48.6% | .004 |
| Outpatient department (OPD) | 123 | 44.9% | 122 | 37.3% | |
| Non-communicable disease clinic (NCD) | 17 | 6.2% | 46 | 14.1% | |
| Educational attainment | |||||
| None | 81 | 29.6% | 67 | 20.5% | .002 |
| Primary school | 134 | 48.9% | 151 | 46.2% | |
| Secondary school or higher | 59 | 21.5% | 109 | 33.3% | |
| Employment status | |||||
| Employed | 191 | 69.7% | 241 | 73.7% | .278 |
| Not employed | 83 | 30.3% | 86 | 26.3% | |
| Household income adequacy over past 12 months | |||||
| Insufficient | 71 | 25.9% | 106 | 32.4% | .032 |
| Just met expenses | 153 | 55.8% | 145 | 44.3% | |
| Allowed for saving | 38 | 13.9% | 55 | 16.8% | |
Table A5.
Correlates of being offered COVID-19 vaccination, among 510 unvaccinated respondents.
| Overall | Have been offered vaccine | Have not been offered vaccine | ||||
| (n = 510) |
(n = 276) |
(n = 234) |
||||
| |
n |
n |
% |
n |
% |
p-value |
| Gender | ||||||
| Male | 207 | 101 | 48.8% | 106 | 51.2% | .046 |
| Female | 303 | 175 | 57.8% | 128 | 42.2% | |
| Age | ||||||
| 18–29 | 149 | 63 | 42.3% | 86 | 57.7% | .009 |
| 30–39 | 153 | 95 | 62.1% | 58 | 37.9% | |
| 40–49 | 117 | 69 | 59.0% | 48 | 41.0% | |
| 50–59 | 56 | 30 | 53.6% | 26 | 46.4% | |
| 60+ | 35 | 19 | 54.3% | 16 | 45.7% | |
| Median (IQR) | 36 | (30–47) | 35 | (25–46) | .037 | |
| HIV status | ||||||
| HIV- or unknown | 247 | 137 | 55.5% | 110 | 44.5% | .554 |
| HIV+ | 263 | 139 | 52.9% | 124 | 47.1% | |
| Marital status | ||||||
| Unmarried | 125 | 58 | 46.4% | 67 | 53.6% | .046 |
| Married | 385 | 218 | 56.6% | 167 | 43.4% | |
| Have children | ||||||
| Yes | 470 | 266 | 56.6% | 204 | 43.4% | <.001 |
| No | 40 | 10 | 25.0% | 30 | 75.0% | |
| Place of residence | ||||||
| Urban | 87 | 47 | 54.0% | 40 | 46.0% | .984 |
| Rural | 423 | 229 | 54.1% | 194 | 45.9% | |
| Religion | ||||||
| Christian | 464 | 252 | 54.3% | 212 | 45.7% | .116 |
| Other religion | 28 | 18 | 64.3% | 10 | 35.7% | |
| Not religious | 18 | 6 | 33.3% | 12 | 66.7% | |
| Educational attainment | ||||||
| None | 158 | 93 | 58.9% | 65 | 41.1% | .106 |
| Primary School | 225 | 110 | 48.9% | 115 | 51.1% | |
| Secondary School or higher | 127 | 73 | 57.5% | 54 | 42.5% | |
| Employment status | ||||||
| Employed | 346 | 181 | 52.3% | 165 | 47.7% | .235 |
| Not employed | 164 | 95 | 57.9% | 69 | 42.1% | |
| Household income adequacy over past 12 months* | ||||||
| Insufficient | 147 | 87 | 59.2% | 60 | 40.8% | .323 |
| Just met expenses | 271 | 144 | 53.1% | 127 | 46.9% | |
| Allowed for saving | 69 | 34 | 49.3% | 35 | 50.7% | |
*Household income not reported by 23 unvaccinated respondents.
Table A6.
Sample description and demographic correlates of motivation to vaccinate against COVID-19, among 510 unvaccinated adults.
| All unvaccinated | Eager/willing | Ambivalent | Opposed | |||||
| (n = 510) |
(n = 274) |
(n = 146) |
(n = 90) |
|||||
| |
n |
n |
% |
n |
% |
n |
% |
p-value |
| TOTAL | 510 | 274 | 53.7% | 146 | 28.6% | 90 | 17.6% | |
| Gender | ||||||||
| Male | 207 | 110 | 53.1% | 65 | 31.4% | 32 | 15.5% | .386 |
| Female | 303 | 164 | 54.1% | 81 | 26.7% | 58 | 19.1% | |
| Age | ||||||||
| 18–29 | 149 | 85 | 57.0% | 38 | 25.5% | 26 | 17.4% | .894 |
| 30–39 | 153 | 84 | 54.9% | 46 | 30.1% | 23 | 15.0% | |
| 40–49 | 117 | 56 | 47.9% | 37 | 31.6% | 24 | 20.5% | |
| 50–59 | 56 | 29 | 51.8% | 16 | 28.6% | 11 | 19.6% | |
| 60+ | 35 | 20 | 57.1% | 9 | 25.7% | 6 | 17.1% | |
| Median (IQR) | 35 | (28–46) | 36 | (29–47) | 37.5 | (28–47) | ||
| HIV status | ||||||||
| HIV- or unknown | 247 | 134 | 54.3% | 67 | 27.1% | 46 | 18.6% | .719 |
| HIV+ | 263 | 140 | 53.2% | 79 | 30.0% | 44 | 16.7% | |
| Marital status | ||||||||
| Unmarried | 125 | 72 | 57.6% | 31 | 24.8% | 22 | 17.6% | .519 |
| Married | 385 | 202 | 52.5% | 115 | 29.9% | 68 | 17.7% | |
| Have children | ||||||||
| Yes | 470 | 251 | 53.4% | 136 | 28.9% | 83 | 17.7% | .854 |
| No | 40 | 23 | 57.5% | 19 | 47.5% | 7 | 17.5% | |
| Place of residence | ||||||||
| Urban | 87 | 34 | 39.1% | 26 | 29.9% | 27 | 31.0% | .001 |
| Rural | 423 | 240 | 56.7% | 120 | 28.4% | 63 | 14.9% | |
| Educational attainment | ||||||||
| No School | 158 | 81 | 51.3% | 41 | 25.9% | 36 | 22.8% | .024 |
| Primary School | 225 | 134 | 59.6% | 64 | 28.4% | 27 | 12.0% | |
| Secondary School or higher | 127 | 59 | 46.5% | 41 | 28.6% | 27 | 21.3% | |
| Employment status | ||||||||
| Employed | 346 | 191 | 55.2% | 96 | 27.7% | 59 | 17.1% | .555 |
| Not employed | 5 | 4 | 80.0% | 1 | 20.0% | 0 | 0.0% | |
| Household income over past 12 months | ||||||||
| Insufficient | 147 | 71 | 48.3% | 48 | 32.7% | 28 | 19.0% | .490 |
| Just met expenses | 271 | 153 | 56.5% | 75 | 27.7% | 43 | 15.9% | |
| Allowed for saving | 69 | 38 | 55.1% | 17 | 24.6% | 14 | 20.3% | |
| Religion | ||||||||
| Christian | 464 | 243 | 52.4% | 136 | 29.3% | 85 | 18.3% | .047 |
| Other religion | 28 | 15 | 53.6% | 8 | 28.6% | 4 | 14.3% | |
| Not religious | 18 | 16 | 88.9% | 1 | 5.6% | 1 | 5.6% | |
Figure A1.
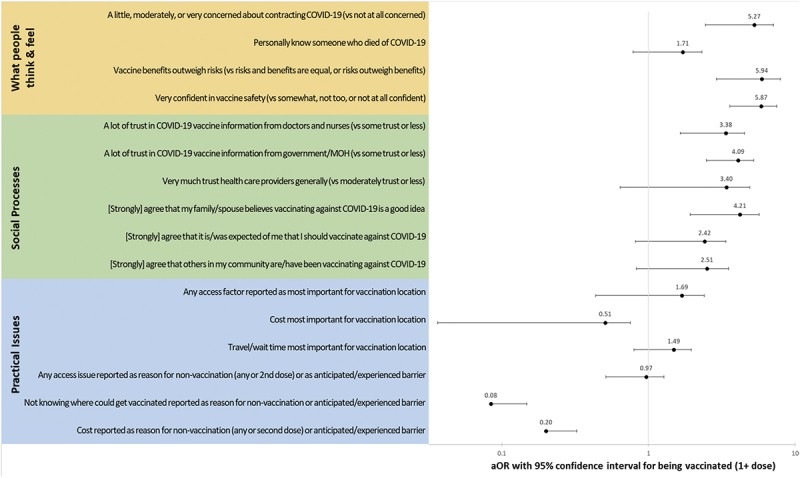
Correlates of COVID-19 vaccination (1+ dose) across WHO BeSD Domains of practical issues, social processes, and what people think and feel.
Figure A2.
Correlates of being vaccinated against COVID-19, as opposed to unvaccinated but motivated (eager/willing) to vaccinate, across WHO BeSD Domains of practical issues, social processes, and what people think and feel.
Funding Statement
This work was supported by the United States Agency for International Development under Cooperative Agreement 72061221CA00010. The views in this publication do not necessarily reflect the views of the U. S. Agency for International Development (USAID), the U. S. President’s Emergency Plan for AIDS Relief (PEPFAR) or the United States Government.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Hunter DJ, Abdool Karim SS, Baden LR, Farrar JJ, Hamel MB, Longo DL, Morrissey S, Rubin EJ.. Addressing vaccine inequity — COVID-19 vaccines as a global public good. N Engl J Med. 2022;386(12):1176–15. doi: 10.1056/NEJMe2202547. [DOI] [PubMed] [Google Scholar]
- 2.Bajaj SS, Maki L, Stanford FC. Vaccine apartheid: global cooperation and equity. Lancet. 2022;399(10334):1452–3. doi: 10.1016/S0140-6736(22)00328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz IT, Weintraub R, Bekker L-G, Brandt AM. From vaccine nationalism to vaccine equity - finding a path forward. N Engl J Med. 2021;384(14):1281–3. doi: 10.1056/NEJMp2103614. [DOI] [PubMed] [Google Scholar]
- 4.Yamey G, Garcia P, Hassan F, Mao W, McDade KK, Pai M, Saha S, Schellekens P, Taylor A, Udayakumar K. It is not too late to achieve global COVID-19 vaccine equity. BMJ. 2022;376:e070650. doi: 10.1136/bmj-2022-070650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, Giattino C, Rodés-Guirao L. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–53. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 6.Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–34. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations Development Programme (UNDP), World Health Organization (WHO), University of Oxford . Global dashboard for vaccine equity. UNDP Data Futures Platform; 2023. https://data.undp.org/vaccine-equity/. [Google Scholar]
- 8.Lawal L, Aminu Bello M, Murwira T, Avoka C, Yusuf Ma’aruf S, Harrison Omonhinmin I, Maluleke P, Tsagkaris C, Onyeaka H. Low coverage of COVID-19 vaccines in Africa: current evidence and the way forward. Hum Vaccin Immunother. 2022;18(1):2034457. doi: 10.1080/21645515.2022.2034457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoque A, Buckus S, Hoque M, Hoque M, Van Hal G. COVID-19 vaccine acceptability among pregnant women at a primary health care facility in Durban, South Africa. Eur J Med Health Sci. 2020;2(5). doi: 10.24018/ejmed.2020.2.5.493. [DOI] [Google Scholar]
- 10.Adeniyi OV, Stead D, Singata-Madliki M, Batting J, Wright M, Jelliman E, Abrahams S, Parrish A. Acceptance of COVID-19 vaccine among the healthcare workers in the Eastern Cape, South Africa: a cross sectional study. Vaccines. 2021;9(6):666. doi: 10.3390/vaccines9060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ajonina-Ekoti IU, Ware KB, Nfor CK, Akomoneh EA, Djam A, Chia-Garba M, Wepnyu GN, Awambeng D, Abendong K, Manjong FT. COVID-19 perceptions and vaccine hesitancy: acceptance, attitude, and barriers among Cameroonians. J Am Pharm Assn. 2022;62(6):1823–9. doi: 10.1016/j.japh.2022.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanyanda S, Markhof Y, Wollburg P, Zezza A. Acceptance of COVID-19 vaccines in Sub-Saharan Africa: evidence from six national phone surveys. BMJ Open. 2021;11(12):e055159. doi: 10.1136/bmjopen-2021-055159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carcelen AC, Prosperi C, Mutembo S, Chongwe G, Mwansa FD, Ndubani P, Simulundu E, Chilumba I, Musukwa G, Thuma P, et al. COVID-19 vaccine hesitancy in Zambia: a glimpse at the possible challenges ahead for COVID-19 vaccination rollout in Sub-Saharan Africa. Hum Vaccin Immunother. 2022;18(1):1–6. doi: 10.1080/21645515.2021.1948784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Figa Z, Temesgen T, Getnet A, Ganta M, Alemu A, Abebe M, Ashuro Z. Acceptance of COVID-19 vaccine among healthcare workers in Africa, systematic review and meta-analysis. Public Health In Practice. 2022;4:100343. doi: 10.1016/j.puhip.2022.100343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moucheraud C, Phiri K, Whitehead HS, Songo J, Lungu E, Chikuse E, Phiri S, van Oosterhout JJ, Hoffman RM. Uptake of the COVID-19 vaccine among health care workers in Malawi. Int Health. 2022;15:77–84. doi: 10.1093/inthealth/ihac007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385–94. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aron MB, Connolly E, Vrkljan K, Zaniku HR, Nyirongo R, Mailosi B, Ruderman T, Barnhart DA, on behalf of the Partners In Health Cross-Site Covid-Cohort Research Network. Attitudes toward COVID-19 vaccines among patients with complex non-communicable disease and their caregivers in rural Malawi. Vaccines. 2022;10(5):792. doi: 10.3390/vaccines10050792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sauer M, Vasudevan P, Meghani A, Luthra K, Garcia C, Knoll MD, Privor-Dumm L. Situational assessment of adult vaccine preventable disease and the potential for immunization advocacy and policy in low-and middle-income countries. Vaccine. 2021;39(11):1556–64. doi: 10.1016/j.vaccine.2021.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perroud JM, Soldano S, Avanceña AL, Wagner A. Adult vaccination uptake strategies in low-and middle-income countries: a systematic review. Vaccine. 2022;40(36):5313–21. doi: 10.1016/j.vaccine.2022.07.054. [DOI] [PubMed] [Google Scholar]
- 20.Agus DB, Nguyen A, Bell J. COVID-19 and other adult vaccines can drive global disease prevention. Lancet. 2022;401(10370):8–10. doi: 10.1016/S0140-6736(22)02084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . WHO COVID-19 dashboard. 2020. [accessed 2022 Mar 8].
- 22.Odhiambo R. Malawi burns thousands of expired AstraZeneca Covid-19 vaccine doses. Lilongwe, Malawi: BBC News; 2021. [Google Scholar]
- 23.World Health Organization . Understanding the behavioural and social drivers of vaccine uptake WHO position paper–May 2022. Wkly Epidemiol Rec. 2022;97(20):209–24. [Google Scholar]
- 24.Malawi Ministry of Health . The Malawi COVID-19 vaccine deployment plan. Lilongwe, Malawi: Malawi Ministry of Health. 2021. [Google Scholar]
- 25.Malawi National Statistical Office . Integrated household panel survey 2010–2013: household socio-economic characteristics report. Zomba, Malawi: Malawi National Statistical Office; 2014 Nov. [Google Scholar]
- 26.StataCorp . Stata statistical software: release 17. College Station, TX: StataCorp LLC; 2021. [Google Scholar]
- 27.Impouma B, Mboussou F, Farham B, Makubalo L, Mwinga K, Onyango A, Sthreshley L, Akpaka K, Balde T, Atuhebwe P, et al. COVID-19 vaccination rollout in the World Health Organization African region: status at end June 2022 and way forward. Epidemiol Infect. 2022;150:150(e143). doi: 10.1017/S0950268822001212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edouard Mathieu HR, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, Roser M. Coronavirus pandemic (COVID-19). 2020. https://ourworldindata.org/coronavirus.
- 29.United Nations, Department of Economic and Social Affairs, Population Division . World Population Prospects 2022 . United Nations; 2022. [Google Scholar]
- 30.UNICEF . MICS-EAGLE Malawi Education Fact Sheets. Lilongwe, Malawi: UNICEF Malawi; 2022. [Google Scholar]
- 31.Partners in Hope . Standard operating procedure for implementing COVID-19 vaccinations among ART clients. Lilongwe, Malawi; Partners in Hope; 2022. Jul. [Google Scholar]
- 32.Strupat C, Shigute Z, Bedi AS, Rieger M, Mugo PM. Willingness to take COVID-19 vaccination in low-income countries: evidence from Ethiopia. PLoS One. 2022;17(3):e0264633. doi: 10.1371/journal.pone.0264633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safary E, Mtaita C. A qualitative exploration of perceptions of the COVID-19 vaccine in Malawi during the vaccine rollout phase. One Health Implement Res. 2022;2(2):79–87. doi: 10.20517/ohir.2022.08. [DOI] [Google Scholar]
- 34.Mundagowa PT, Tozivepi SN, Chiyaka ET, Mukora-Mutseyekwa F, Makurumidze R, Sobh E. Assessment of COVID-19 vaccine hesitancy among Zimbabweans: a rapid national survey. PLoS One. 2022;17(4):e0266724. doi: 10.1371/journal.pone.0266724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dereje N, Tesfaye A, Tamene B, Alemeshet D, Abe H, Tesfa N, Gedion S, Biruk T, Lakew Y. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-method study. BMJ Open. 2022;12(5):e052432. doi: 10.1136/bmjopen-2021-052432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ackah M, Ameyaw L, Gazali Salifu M, Afi Asubonteng DP, Osei Yeboah C, Narkotey Annor E, Abena Kwartemaa Ankapong E, Boakye H, Aslam MS. COVID-19 vaccine acceptance among health care workers in Africa: a systematic review and meta-analysis. PLoS One. 2022;17(5):e0268711. doi: 10.1371/journal.pone.0268711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ackah BBB, Woo M, Stallwood L, Fazal ZA, Okpani A, Ukah UV, Adu PA. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Health Res Policy. 2022;7(1):21. doi: 10.1186/s41256-022-00255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orangi S, Pinchoff J, Mwanga D, Abuya T, Hamaluba M, Warimwe G, Austrian K, Barasa E. Assessing the level and determinants of COVID-19 vaccine confidence in Kenya. Vaccines. 2021;9(8):936. doi: 10.3390/vaccines9080936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dula J, Mulhanga A, Nhanombe A, Cumbi L, Júnior A, Gwatsvaira J, Fodjo JN, Faria de Moura Villela E, Chicumbe S, Colebunders R. COVID-19 vaccine acceptability and its determinants in Mozambique: an online survey. Vaccines. 2021;9(8):828. doi: 10.3390/vaccines9080828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ao Q, Egolet RO, Yin H, Cui F. Acceptance of COVID-19 vaccines among adults in Lilongwe, Malawi: a cross-sectional study based on the health belief model. Vaccines. 2022;10(5):760. doi: 10.3390/vaccines10050760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ozoh OB, Akinkugbe AO, Olukoya MA, Adetifa IMO. Enablers and barriers to COVID-19 vaccine uptake in an urban slum in Lagos, Nigeria: informing vaccine engagement strategies for the marginalized. Int Health. 2023;ihad009. doi: 10.1093/inthealth/ihad009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Katoto PDMC, Parker S, Coulson N, Pillay N, Cooper S, Jaca A, Mavundza E, Houston G, Groenewald C, Essack Z, et al. Predictors of COVID-19 vaccine hesitancy in South African local communities: the VaxScenes study. Vaccines. 2022;10(3):353. doi: 10.3390/vaccines10030353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reñosa MDC, Landicho J, Wachinger J, Dalglish SL, Bärnighausen K, Bärnighausen T, McMahon SA. Nudging toward vaccination: a systematic review. BMJ Glob Health. 2021;6(9):e006237. doi: 10.1136/bmjgh-2021-006237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sethy G, Chisema MN, Sharma L, Singhal S, Joshi K, Nicks PO, Laher B, Mamba KC, Deokar K, Damte T, et al. ‘Vaccinate my village’ strategy in Malawi: an effort to boost COVID-19 vaccination. Expert Rev Vaccines. 2023;22(1):180–5. doi: 10.1080/14760584.2023.2171398. [DOI] [PubMed] [Google Scholar]
- 46.Yeatman S, Chamberlin S, Dovel K, Anglewicz P. Women’s (health) work: a population-based, cross-sectional study of gender differences in time spent seeking health care in Malawi. PLoS One. 2018;13(12):e0209586. doi: 10.1371/journal.pone.0209586. [DOI] [PMC free article] [PubMed] [Google Scholar]


