Abstract
Background
The second decade of this millennium was characterized by a widespread availability of chimeric antigen receptor T-cell (CAR-T) therapies to treat relapsed and refractory lymphomas. As expected, the role and indication of allogeneic haematopoietic stem cell transplant (allo-HSCT) in the management of lymphoma changed. Currently, a non-neglectable proportion of patients will be considered candidate for an allo-HSCT, and the debate of which transplant platform should be offered is still active.
Objectives
to report the outcome of patients affected with relapsed/refractory lymphoma and transplanted following reduced intensity conditioning at King's College Hospital, London, between January 2009 and April 2021.
Methods
Conditioning was with 150mg/m2 of fludarabine and melphalan of 140mg/m2. The graft was unmanipulated G-CSF mobilized peripheral blood haematopoietic stem cells (PBSC). Graft-versus-host disease (GVHD) prophylaxis consisted of pre-transplant Campath at the total dose of 60 mg in unrelated donors and 30 mg in fully matched sibling donors and ciclosporin.
Results
One-year and five years OS were 87% and 79.9%, respectively, and median OS was not reached. The cumulative incidence of relapse was 16%. The incidence of acute GVHD was 48% (only grade I/II); no cases of grade III/IV were diagnosed. Chronic GVHD occurred in 39% of patients. TRM was 12%, with no cases developed within day 100 and 18 months after the procedure.
Conclusions
The outcomes of heavily pretreated lymphoma patients are favorable, with median OS and survival not reached after a median of 49 months. In conclusion, even if some lymphoma subgroups cannot be treated (yet) with advanced cellular therapies, this study confirms the role of allo-HSCT as a safe and curative strategy.
Keywords: Allogeneic hematopoietic cell transplantation, Lymphoma
Introduction
The second decade of this millennium was characterized by the widespread availability of chimeric antigen receptor T-cell (CAR-T) therapies to treat relapsed and refractory lymphomas, changing these entities' prognosis and treatment landscape.1–5
Also, the development of antibody-conjugated therapies or bi-specific antibodies further enriched the treatment algorithm creating more therapeutic dilemmas in selecting the most effective and safe therapy after the second relapse and beyond.6,7
As expected, the role and indication of allogeneic haematopoietic stem cell transplant (allo-HSCT) in the management of lymphoma changed, and it is currently redefining its role in the treatment pathway of our patients.
Interestingly, the first decade of the millennium can be remembered with a global effort in proving a graft-versus-lymphoma effect and in identifying the safest conditioning regimens before the infusion of the graft.8 Different groups previously showed that reduced intensity conditioning (RIC) regimens could offer the engraftment of the donor immune system without exposing the patients to an unacceptable risk of transplant-related mortality (TRM) .9,10,11
Despite the new treatment options mentioned before, a not neglectable proportion of patients, due to the lack of CAR-T products or any other modern therapy, will be considered a candidate for an allo-HSCT.12 Therefore, the debate of which transplant platform/conditioning regimen should be offered is still active.
Herein we report the outcome of patients affected with relapsed/refractory lymphoma and transplanted following RIC administration.
Material and Methods
Conditioning was administered with 150 mg/m2 of fludarabine and melphalan of 140 mg/m2.
Graft-versus-host disease (GVHD) prophylaxis consisted of pre-transplant Campath at the total dose of 60 mg in unrelated donors and 30 mg in fully matched sibling donors, and ciclosporin 3 mg/Kg from day −1 (therapeutic level of 150–200) until d+56 and then tapered in the absence of GVHD aiming to stop it on day +90.
Between January 2012 and April 2022, 35 patients (9 females and 26 males) affected with different lymphoma subtypes underwent allo-HSCT at King's College Hospital in London, United Kingdom. Table 1 summarizes the patients' characteristics and shows the transplant details. Median follow-up was 49 months (range 1–109).
Table 1.
Patients’ characteristics and transplant details. VOD/SOS: veno-occlusive disease/sinusoidal obstructive syndrome. UF: unfractionated.
| Patients Characteristics | N (%) |
|---|---|
|
| |
| Total | 35 (100) |
|
| |
| Male | 26 (72) |
| Female | 9 (28) |
|
| |
| Median age (range) | 43(25 – 64) |
|
| |
| Diagnosis | |
| Classical Hodgkin Lymphoma | 10 (30) |
| Follicular Lymphoma | 9 (27) |
| Large B-Cell Lymphoma | 5 (15) |
| Mantle cell lymphoma | 4 (9) |
| Peripheral T-cell Lymphoma | 7 (18) |
|
| |
| Previous auto-HSCT | 19 (58) |
|
| |
| Previous CAR-T | 1 (3) |
|
| |
| Pet negative pre allo-HSCT | 22 (66) |
|
| |
| Pet positive pre allo-HSCT | 11 (34) |
| Partial response to salvage therapy | 6 |
| Stable disease after salvage therapy | 5 |
|
| |
| Full-matched sibling donor | 13 |
|
| |
| Matched unrelated donor | 22 |
|
| |
| Primary graft failure | 2 |
|
| |
| Secondary graft failure | 0 |
|
| |
| VOD/SOS* | 2 |
|
| |
| Months of median follow-up (range) | 49 (1–109) |
|
| |
| Median days to neutrophil engraftment (range) | 12 (10 – 24) |
|
| |
| Median days to platelets engraftment (range) | 11 (8 – 29) |
|
| |
| Median chimerism at day 100 (UF+/CD3/CD15) | 98/94.5/99 |
|
| |
| Median chimerism at 1 year (UF+/CD3/CD15) | 99/99/99 |
|
| |
| Median days to first CMV reactivation | 28 |
|
| |
| Median days to first EBV detectable viraemia | 108 |
Donors and recipients were typed using Third Generation Sequencing (TGS) and Next Generation Sequencing (NGS) techniques for HLA-A, -B, -C, - DRB1, -DQ at a high-resolution level. Donors were considered mismatched if <10/10 match was present.
Probabilities of overall survival (OS) and GVHD-relapse-free survival (GRFS) were calculated using the Kaplan-Meier method. Relapse incidence (RI) and transplant-related mortality (TRM) rates were estimated using cumulative incidence (CI) functions and considered as competing risks. For GvHD, death and relapse were considered competing events. Univariate analyses were performed using the log-rank test for OS, GRFS, and Gray's test for RI and TRM. Statistical analyses were performed with GraphPad Prism Version 9.4.1.
Results
The graft was unmanipulated G-CSF mobilized peripheral blood haematopoietic stem cells PBSC). A median of 7×106 CD34+/Kg was infused (range 1.8 – 11.2). Median time to neutrophils ≥ 1000/μL was 12 days (10–24), and 11 days (8–29) to platelets ≥ 20.000/μL; no deaths before engraftment were recorded. Two cases of primary graft failure occurred; despite autologous reconstitution, these patients achieved complete remission (CR).
Median unfractionated, CD3+, and CD15 chimerism at 365 days after transplant were 99% and 99%, respectively.
One-year and five years OS were 87% and 79.9%, respectively, and median OS was not reached.
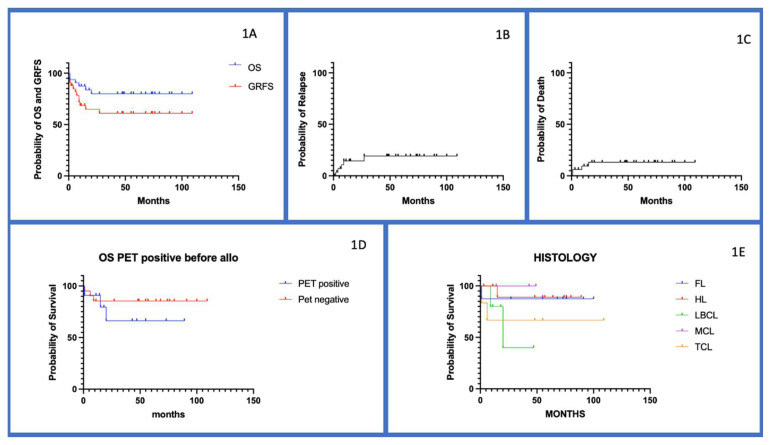
One-year and five years GFRS were 69% and 61%, respectively, with median GRFS not reached (Figure 1A).
Figure 1.
(A) Overall survival (OS) and GVHD-Relapse free survival (GRFS) of the whole cohort. (B) Cumulative incidence of relapse; Figure (C) Cumulative incidence of transplant related mortality (TRM); (D) OS according to disease status at time of transplant; (E) OS according to histology subtypes. FL= follicular lymphoma, HL= Hodgkin Lymphoma, LBCL= large B cell lymphoma, MCL= mantle cell lymphoma, TCL= T-cell lymphoma.
The global CI of relapse was 16%, with no late relapses seen beyond 24 months after transplant (Figure 1B); it is worth highlighting that one of the relapsed patients achieved durable complete remission following the withdrawal of immune suppressive therapy, and two patients following the infusion of donor lymphocyte infusions (DLI).
The overall incidence of acute GVHD was 48% (15 patients were affected with grade I, and only one patient had grade II); no grade III/IV cases were diagnosed. The median time to acute GVHD was 57 days (range 23–112). Chronic GVHD occurred in 39% of patients; within this group, moderate and severe cases were noted in 4 and 3 patients, respectively. The median time to chronic GVHD was 171 days (range 107–511).
Overall TRM was 12%, with no cases developed within day 100 and 18 months after the procedure (Figure 1C). The leading causes of death were infections (3 cases) and disease progression (1).
CMV reactivation occurred in 41% with a median time to first CMV reactivation of 28 days (range −6 – 251). No CMV disease occurred, and all the patients received pre-emptive therapy per local policy.
EBV-detectable viraemia occurred in 51% of the patients at a median time of 108 days (range 22 – 713); two monomorphic PTLD cases required treatment with rituximab achieving CR.
Disease status at the time of transplant has an impact on OS: patients in complete remission at the time of transplant had a five years OS of 80% compared to 65% in those with a partial response at the time of transplant (Figure 1D); an analogous situation for those who underwent up-front allo-HSCT. These results confirm that chemo-sensitive disease can benefit from allo-HSCT even in partial response.
From a histological point of view, non-large B-cell lymphoma (LBCL) had a better outcome, with median OS never reached compared to LBCL (Figure 1E). It is worth highlighting that the two LBCL patients that failed HSCT underwent the procedure with detectable disease at the PET scan before transplant, suggesting that high proliferative tumour burden cannot be controlled with the GVL effect.13
Discussion
The RIC conditioning and the infusion of unmanipulated PBSC are both effective and safe: the TRM of 12% is dramatically low compared to early experiences of allo-HSCT in lymphoma.14
The low incidence of early relapse and the absence of late relapse confirms a durable GVL effect that cures patients heavily pretreated.
The GVHD prophylaxis with the administration of Campath before the infusion of the graft and the single agent ciclosporin did not expose the patient to the risk of severe forms of acute GVHD. Interestingly, only seven patients affected with chronic GVHD required systemic treatment, but none developed recurrent infective complications, and none reported severe impairment of quality of life from that complication. Also, the in-vivo T-cell depletion did not endanger the GVL effect nor trigger lethal viral infections.
These encouraging results can offer a reflection regarding the costs of transplant compared to CAR-T therapies, which are the current competitors of allograft in the third-line setting for B-cell CD19 positive NHL.
The dissimilarities in prices between cellular therapy products and allo-HSCT should not drive the clinician's choice of the best treatment to offer to patients; with this assumption, it is important to remember that none CAR-T product has the same curative trait of allo-HSCT, as still 60% of B-cell lymphoma patients are not cured with CAR-T therapy.
Despite that, it is important to highlight that allo-HSCT will not replace CAR-T as the standard of care in a third-line setting for CD19-positive lymphoma due to favourable toxicity profile and its efficacy in progression-free survival and OS.
Lymphoma subtypes still lacking an available CAR-T product can be cured with allo-HSCT. Our study confirms the long-term survival of this strategy and, most importantly, the safety of our RIC transplant platform. Also, the low TRM should finally eliminate any doubt about the safety of in-vivo T-cell depletion with Campath.
Our experience showed that MCL and LBCL can also be cured with allo-HSCT; this manuscript will feed the new debate on when to offer an allo-HSCT for these entities.
Considering the availability of highly effective bridging new therapies to CAR-T infusion, it is not uncommon to meet patients in complete metabolic remission (CMR) in third- or fourth-line settings.6,7 Should CD19-positive lymphoma be in CMR after the third line of therapy consolidated with CAR-T infusion or with allo-HSCT? Only a randomized prospective clinical trial will provide the answer to this dilemma.15
Also, there is evidence of the safety and efficacy of CAR-T infusion after allo-HSCT; therefore, his strategy should not be considered the condition sine qua non to preclude CAR-T therapies.16
Our experience shows that the FMC allo-HSCT platform is highly effective and safe, with low TRM and GVHD rates, and cheaper than CAR-T therapy.
In conclusion, RIC allo-HSCT can still cure lymphomas, and prospective clinical trials are needed to further define its role, particularly in sequencing new strategies for managing CD-19-positive lymphomas.
Acknowledgments
The authors want to thank all the staff of the haematology department at King's College Hospital for the care provided to all patients.
Footnotes
Competing interests: The authors declare no conflict of Interest.
References
- 1.Schuster SJ, et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med. 2019;380:45–56. doi: 10.1056/NEJMoa1804980. [DOI] [PubMed] [Google Scholar]
- 2.Neelapu SS, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N Engl J Med. 2017;377:2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamdar M, et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet Lond Engl. 399(2022):2294–2308. doi: 10.1016/S0140-6736(22)00662-6. [DOI] [PubMed] [Google Scholar]
- 4.Locke FL, et al. Axicabtagene Ciloleucel as Second-Line Therapy for Large B-Cell Lymphoma. N Engl J Med. 386(2022):640–654. doi: 10.1056/NEJMoa2116133. [DOI] [PubMed] [Google Scholar]
- 5.Wang M, et al. KTE-X19 CAR T-Cell Therapy in Relapsed or Refractory Mantle-Cell Lymphoma. N Engl J Med. 382(2020):1331–1342. doi: 10.1056/NEJMoa1914347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castaneda-Puglianini O, Chavez JC. Bispecific antibodies for non-Hodgkin's lymphomas and multiple myeloma. Drugs Context. 2021;10:2021-2-4. doi: 10.7573/dic.2021-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sehn LH, et al. Polatuzumab Vedotin in Relapsed or Refractory Diffuse Large B-Cell Lymphoma. J Clin Oncol Off J Am Soc Clin Oncol. 38(2020):155–165. doi: 10.1200/JCO.19.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peniket AJ, et al. An EBMT registry matched study of allogeneic stem cell transplants for lymphoma: allogeneic transplantation is associated with a lower relapse rate but a higher procedure-related mortality rate than autologous transplantation. Bone Marrow Transplant. 2003;31:667–678. doi: 10.1038/sj.bmt.1703891. [DOI] [PubMed] [Google Scholar]
- 9.Hari P, et al. Allogeneic transplants in follicular lymphoma: higher risk of disease progression after reduced-intensity compared to myeloablative conditioning. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant. 2008;14:236–45. doi: 10.1016/j.bbmt.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Genadieva-Stavrik S, et al. Myeloablative versus reduced intensity allogeneic stem cell transplantation for relapsed/refractory Hodgkin's lymphoma in recent years: a retrospective analysis of the Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. Ann Oncol Off J Eur Soc Med Oncol. 2016;27:2251–2257. doi: 10.1093/annonc/mdw421. [DOI] [PubMed] [Google Scholar]
- 11.Thomson KJ, et al. Favorable long-term survival after reduced-intensity allogeneic transplantation for multiple-relapse aggressive non-Hodgkin's lymphoma. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27:426–432. doi: 10.1200/JCO.2008.17.3328. [DOI] [PubMed] [Google Scholar]
- 12.Snowden JA, et al. Indications for haematopoietic cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2022. Bone Marrow Transplant. 57(2022):1217–1239. doi: 10.1038/s41409-022-01691-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sammassimo S, et al. A Cellular Therapy with Haploidentical Peripheral Hematopoietic STEM CELL Transplantation MAY be a Therapeutic Option in Patients with Relapsed Lymphoma with Chemorefractory. Disease Blood. 2018;132:2189. doi: 10.1182/blood-2018-99-119752. [DOI] [Google Scholar]
- 14.Sureda A, et al. Reduced-Intensity Conditioning Compared With Conventional Allogeneic Stem-Cell Transplantation in Relapsed or Refractory Hodgkin's Lymphoma: An Analysis From the Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol. 2008;26:455–462. doi: 10.1200/JCO.2007.13.2415. [DOI] [PubMed] [Google Scholar]
- 15.Dreger P, et al. CAR T cells or allogeneic transplantation as standard of care for advanced large B-cell lymphoma: an intent-to-treat comparison. Blood Adv. 4(2020):6157–6168. doi: 10.1182/bloodadvances.2020003036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zurko J, et al. Allogeneic transplant following CAR T-cell therapy for large B-cell lymphoma. Haematologica. 108(2023):98–109. doi: 10.3324/haematol.2022.281242. [DOI] [PMC free article] [PubMed] [Google Scholar]