Abstract
Background
Nutrition is an important prevention in old patients with COVID-19. However, in China, there are few studies on the correlation between nutrition and COVID-19.
Methods
A total of 148 hospitalized COVID-19 (65.7 ± 16.0 [range: from 21 to 101] years old) patients were enrolled in this study. The information of demographic, biochemical results, vaccination doses, types of COVID-19, PCR test negative conversion time, and scores of Mini Nutritional Assessment Short Form (MNA-SF) for evaluating nutritional status were recorded. We first explored the relationships between MNA-SF performance and the severities of COVID-19 in the groups with non-vaccinated, vaccinated, and all the patients using multivariable ordinal logistic regression. Further, we explored the relationships between performance of MNA-SF and the time of negative conversion of PCR in the groups with non-vaccinated, vaccinated, and all the patients using COX proportional hazards survival regression.
Results
Group of patients with malnutrition or at risk of malnutrition group was associated with older of the age, those who had not been vaccinated, in fewer people who were asymptomatic type and in more people who showed longer of the negative conversion time of PCR, lower of the BMI, and the lower of the hemoglobin level. Each additional increase of one point of MNA-SF was associated with a 17% decrease in the odds of a worse type of COVID-19 in all patients, and the significant result exists in non-vaccinated patients. One point increase of MNA-SF was associated with increased 11% of hazard ratios of turning negative of PCR and well-nourished group was associated with increased 46% of hazard ratio of turning negative of PCR.
Conclusion
Higher nutrition is associated with less severity of COVID-19, especially in the non-vaccinated group. Higher nutrition is also associated with shorter time of turning negative of PCR in non-ICU COVID-19 patients.
Keywords: COVID-19, nutrition, MNA-SF, vaccination
Introduction
Coronavirus disease 2019 (COVID-19) is a serious global public health crisis. The virus is mainly transmitted between people through contact routes and respiratory droplets. The rapid spread of COVID-19 globally is attributable to its long incubation period, high transmission rate, and asymptomatic status among carriers.1 In December 2022, China changed the prevention strategy of COVID-19, with a policy of strict control to open policy, which may lead to the epidemic of diseases. Due to the general susceptibility of new coronaviruses, it is necessary to conduct in-depth research and evaluate the impact of different risk factors on the prognosis of patients.
The key management of early stage COVID-19 includes infection prevention, early diagnosis, and immediate isolation. Typical treatment of novel coronavirus pneumonia includes general supportive care, respiratory support and nutritional support.2 Antiviral drugs, vaccines, anti-SARS-CoV-2 antibody treatments, and convalescent plasma therapy are all promising therapeutic strategies.2 The COVID-19 epidemic is a challenge to the whole world. However, due to different medical and economic conditions, the same vaccine and drug support strategy is not realistic. In order to minimize the impact of COVID-19 on life, we need more preventions and interventions. For example, does sequential vaccination with different vaccines have different effects on preventing infection and severe illness? In the absence of vaccines and drugs, what treatment should be tailored to local conditions? In China, we have adopted methods of isolating patients and close contacts in the past three years to reduce the spread of diseases. For the treatment of COVID-19 infection, vital signs support strategies such as respiratory assistance are generally used. At that time, the application of messenger RNA vaccines, multivalent vaccines, and small molecule antiviral drugs in China was not widespread. We need to explore more effective treatment measures, and nutritional interventions have therefore come into our sight. Because nutritional risk is a modifiable factor that can be reduced or controlled with early, individualized nutritional therapy, identifying risk can help prevent worsening disease and improve patients’ prognoses.3 On the one hand, there was evidence that COVID-19 is associated with high risk of malnutrition, primarily in older people.3 On the other hand, it was reported that strengthening the nutritional status of COVID-19 inpatients may improve disease outcomes in older adult patients.4
The induction of immune response is essential for fighting against the coronavirus.5 However, enormous secretion of cytokines will also trigger hyperreaction, often leading to inflammation, lung damage, acute respiratory distress syndrome (ARDS) and even development of pulmonary fibrosis.5 So, maintaining the balanced function of the immune system helps fight infectious diseases. Malnutrition in all its forms alters the immune response which is a driving force for the prevention, treatment, and progression of COVID-19.6 The effects of malnutrition and COVID-19 may be bidirectional. The inflammatory response caused by infection leads to decreased appetite and altered intestinal absorption, limiting the intake, uptake, and utilization of macronutrients and key micronutrients, leading to malnutrition accompanied by micronutrient deficiency. Malnutrition, in turn, can exacerbate inflammation regulation, damage immune function, and increase the risk of infection.6 The European Food Safety Authority (EFSA) evaluated and deemed six vitamins (D, A, C, Folate, B6, B12) and four minerals (zinc, iron, copper and selenium) to be essential for the normal functioning of the immune system. The optimal status of specific nutrients helps keep immune components within their normal activity, then helps to avoid and overcome infections.7
Conducting early assessment of nutritional risk, defined as “chances of a better or worse outcome from disease or surgery according to actual or potential nutritional and metabolic status”,5 can help determine the most appropriate nutritional therapy and improve the immune response and prognosis of patients with COVID-19. There is scarce research focusing on the relationship between nutritional risk and the outcomes in COVID-19 patients in a wide age range, as well as the effects of nutritional status on patient outcome with different vaccination conditions in China. Therefore, we conducted a study among COVID-19 patients hospitalized in non-intensive care units in China to assess the associations between nutritional status and outcome.
Methods
Participants
A total of 148 hospitalized (non-ICU) patients who were admitted to Ruijin Hospital North, a designated hospital for treating COVID-19, between April 2022 and June 2022 were enrolled in this study. Demographic information (age and sex), biochemical results including fibrinogen, ferritin, haemoglobin, albumin protein, body mass index (BMI), vaccination doses, types of COVID-19 (asymptomatic type/mild type/ordinary type), time PCR negative conversion time, and scores of Mini Nutritional Assessment Short Form (MNA-SF) for evaluating nutritional status were recorded, and all of the above data were collected within three days after COVID-19.
Patients who had a confirmed diagnosis of COVID-19, with an age >20 years, with no restriction on gender, maintained stable physical status, able to complete the scale assessment independently, and had a good compliance were included in this study. Patients were excluded if their conditions were critical or life-threatening, if they were unable to understand the procedures and methods of this clinical study, or if they refused to participate.
MNA-SF
Newly revised MNA-SF was created by calculating all possible combinations of six questions from the full form of the Mini Nutritional Assessment (MNA) and evaluating these versions of the MNA-SF against the complete version of MNA. The MNA-SF test consists of six items that can be completed in less than 5 minutes: anthropometric measurements (body mass index, weight loss); global assessment (mobility); dietary questionnaire and subjective assessments (food intake, neuropsychological problems, acute disease). The total score of MNA-SF≤11 indicated malnutrition or a risk of malnutrition, while a score of >11 indicated no malnutrition.8,9
The investigation conformed to the Declaration of Helsinki. Written informed consent was received from the patients themselves or their agents, and ethical approval was given by Ruijin Hospital affiliated to Medical College of Shanghai Jiaotong University (No 2022–119). The registration number of this clinical study is ChiCTR2200064302.
Statistical Analyses
We first explored the associations between MNA-SF performance and disease severity of COVID-19 (asymptomatic/mild/ordinary) by applying multivariable ordinal logistic regression. Then, we used COX proportional hazards survival regression to explore the associations between MNA-SF performance and the negative conversion time of PCR. We adjusted for sex, age, and vaccination situations (with or without vaccinations), which had previously been found to be associated with recovery from COVID-19. We used MNA-SF scores and binary MNA-SF index (MNASF ≤11 or MNASF >11) in the above analyses. Then, we applied Kaplan–Meier survival curve comparing different effects of nutritional status (MNASF ≤11 versus MNASF >11) on the negative conversion time of PCR in patients. To explore further if there were different effects of nutritional performance in patients with different vaccination conditions, we divided all patients into two groups: those that had no vaccination and those had at least one dose of vaccination. We then performed multivariable ordinal logistic regression to explore the associations between scores and binary indexes of MNA-SF and disease severity of COVIDS-19, and COX proportional hazards survival regression was also applied to explore the associations between scores and binary indexes of MNA-SF and the negative conversion time of PCR in the two vaccination groups, respectively. We adjusted for sex and age in these models. Odds ratios (ORs) and their 95% confidence interval (CI) were presented for multivariable ordinal logistic regression, hazard ratios (HRs) and their 95% CI were given for COX proportional hazard survival regression. We compared baseline characteristics of two nutritional groups using χ2 for categorical variables, a two-tailed t-test for variables following a normal distribution (age and body mass index) or Mann–Whitney U-test for variables which have a non-normal distribution. All the statistical analyses were performed with R v4.2.2.10
Results
Baseline Participant Characteristics
We enrolled 148 patients (mean ± SD age, 65.7 ± 16.0 years; 75 [50.7%] were female) and stopped enrollment in June 2022 because of institutional restrictions resulting from the COVID-19 pandemic. China changed Shanghai’s epidemic prevention policy at that time, resulting in a significant reduction in the number of cases, so we stopped enrollment. The baseline characteristics of all patients are shown in Table 1. There were 64 patients who had been vaccinated between one and three doses, while 84 patients who had not been vaccinated. Forty-eight patients in our study were of the asymptomatic type for COVID-19, 64 patients were of mild type, and 36 patients were of ordinary type. The median time of PCR test negative conversion was nine (IQR 5–15) days. The mean ± SD value of BMI was 23.4 ± 4.9 kg/m2, and median score of MNA-SF of all the patients was 12 (IQR 10–13). There were 67 (45.3%) patients with MNA-SF score ≤11, and 81 patients (54.7%) with MNA-SF score >11. We further divided the patients into a malnourished or at risk of malnourished group and a well-nourished group according to their MNA-SF scores. We defined the malnourished or at risk of malnutrition group with MNASF <=11, and the well-nourished group with MNASF >11. The characteristics of the two groups are shown in Table 2. Results showed that the malnutrition or at risk of malnutrition group was associated with older age, more people who had not been vaccinated, fewer people who were of the asymptomatic type and more people of the ordinary type, longer time for negative conversion of PCR, lower BMI, and lower hemoglobin level.
Table 1.
Characteristics of COVID Patients. Values are Expressed as n (%), Mean ± SD, or Median (Interquartile Range)
| Characteristic | All Patients (n=148) |
|---|---|
| Age (years) | 65.7±16.0 |
| Sex (n, male %) | 49.3% |
| Vaccination dose (0/1~3, 0.5 mL for every dose which has 600SU covid-19 antigen) | 84/64 |
| COVID types (asymptomatic type/mild type/ordinary type) (n) | 48/64/36 |
| Time of turning negative of PCR (d) | 9.0 (5.0, 15.0) |
| BMI (kg/m2) | 23.4±4.9 |
| Fibrinogen (mg/dL) | 3.4 (3.0, 3.9) |
| Ferritin (μg/L) | 149.3 (83.0, 311.5) |
| Hb (g/L) | 134.0 (119.2, 144.0) |
| Alb (g/L) | 39.0 (37.0, 42.0) |
| MNA-SF (scores) | 12.0 (10.0, 13.0) |
| MNA-SF types (≤11: malnourished or at risk of malnutrition,>11: well-nourished, n) | 67/81 |
Table 2.
Characteristics of COVID Patients in Malnourished or at Risk of Malnourished and Well-Nourished Groups
| Characteristics | MNASF≤11 (n=67) | MNASF>11 (n=81) | P |
|---|---|---|---|
| Age (years) | 69.6±16.5 | 62.5±14.9 | 0.0077 |
| Sex (n, male %) | 33, 49.3% | 40, 49.4% | 1 |
| Vaccination dose (0/1~3, 0.5 mL for every dose which has 600SU covid-19 antigen) (%) | 67.16%/32.84% | 48.15%/51.85% | 0.0310 |
| COVID types (asymptomatic type/mild type/ordinary type) (%) | 26.86%/38.81%/34.33% | 37.04%/46.91%/16.05% | 0.0340 |
| Time of turning negative of PCR (d) | 12.0 (7.0, 18.0) | 8.0 (5.0, 13.0) | 0.0017 |
| BMI (kg/m2) | 21.8±6.1 | 24.6±3.4 | 0.0021 |
| Fibrinogen (mg/dL) | 3.5 (3.0, 4.2) | 3.5 (3.0, 4.2) | 0.1767 |
| Ferritin (μg/L) | 214.9 (116.2, 333.2) | 127.9 (75.5, 214.0) | 0.0276 |
| Hb (g/L) | 127.0 (110.0, 139.0) | 137.0 (125.5, 147.0) | 0.0020 |
| Alb (g/L) | 38.0 (34.0, 40.0) | 40.0 (38.0, 42.0) | 7.452e-05 |
Exploration of Associations Between Nutrition and COVID-19 Disease Severity
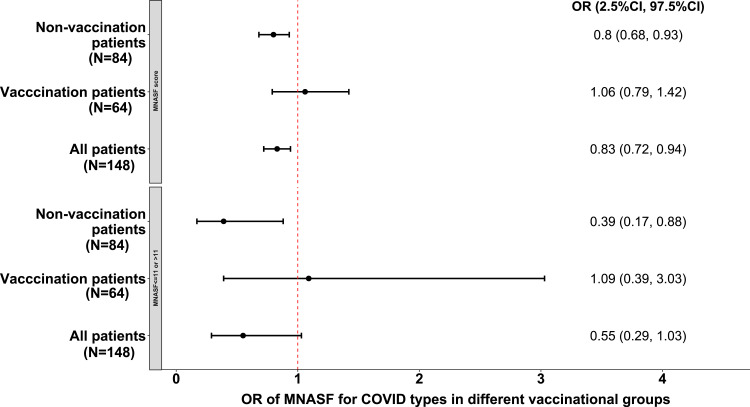
We calculated ORs and their 95% CIs of nutrition on COVID types in all COVID-19 patients, then divided the patients into non-vaccinated (n = 84) and vaccinated groups (n = 64) and calculated the ORs in the two groups, respectively. Results showed that each additional increase of one point of MNA-SF was associated with a 17% decrease in the odds of a worse type of COVID in all patients (OR = 0.83, 95% CI = 0.72–0.94), and both scores and binary index of MNA-SF showed significantly decrease severity of COVID-19 in non-vaccinated group (OR = 0.80, 95% CI = 0.68–0.93, and OR = 0.39, 95% CI = 0.17–0.88 in the two groups respectively), while results were not significant in the vaccinated group (Figure 1). All the ORs and their 95% CIs of the confounders in each model are presented in Supplements 1–4.
Figure 1.
Associations between scores and binary index of MNA-SF and COVID-19 types in non-vaccination group, vaccination group, and in all patients.
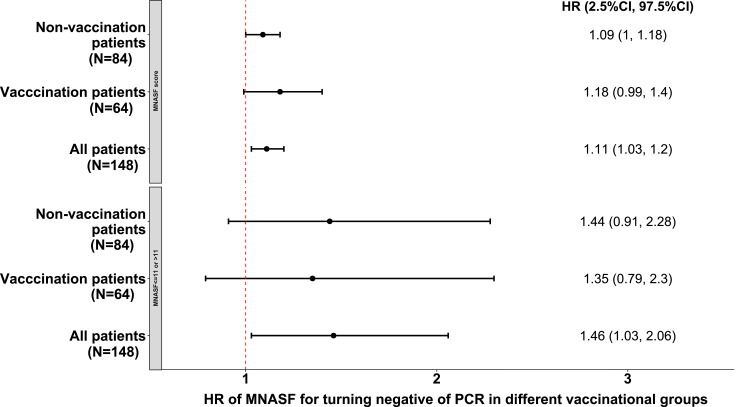
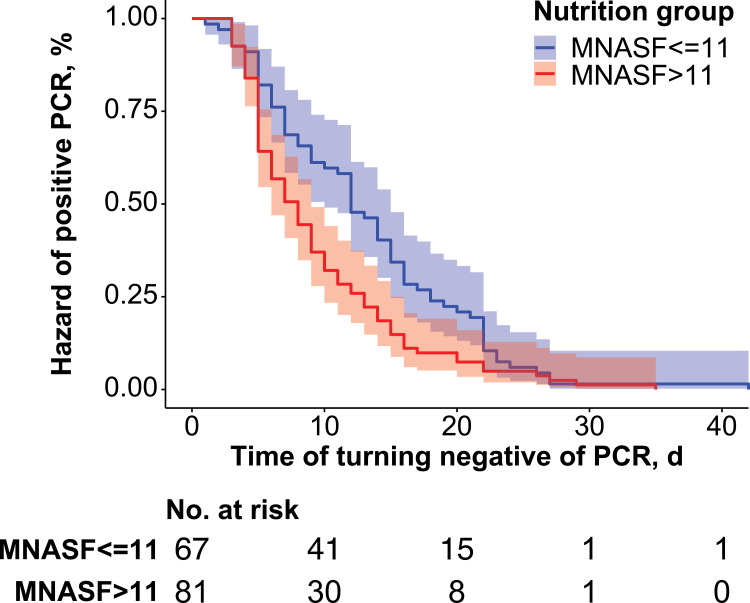
We calculated HRs and their 95% CIs of nutrition on negative conversion time of PCR in all COVID-19 patients, then divided the patients into non-vaccinated (n = 84) and vaccinated groups (n = 64) and calculated the HRs in the two groups, respectively. Results showed that each additional increase of one point of MNA-SF was associated with 11% PCR negative conversion PCR (HR = 1.11, 95% CI = 1.03–1.20) and being well nourished was associated with 46% PCR negative conversion (HR = 1.46, 95% CI = 1.03–2.06) in all patients (Figure 2). Figure 3 shows the Kaplan–Meier curves by MNA-SF scores (≤11 vs >11). However, there were no significant results in either non-vaccinated or vaccinated group (Figure 2); this may be due to the small sample size of each sub-group. All HRs and their 95% CIs of the confounders in each model are presented in Supplements 5–8.
Figure 2.
Associations between scores and binary index of MNA-SF and PCR negative conversion time in non-vaccination group, vaccination group, and in all patients.
Figure 3.
Kaplan–Meier survival curves comparing time of PCR negative conversion of MNASF<=11 vs MNASF>11 groups. Shading represents 95% CIs.
Discussion
At present, there is no gold standard for assessing the risk of malnutrition, and professionals generally adopt different screening scales for various studies.3 Different nutrition screening scales like MNA-SF, Nutrition Risk Screening 2002 (NRS 2002), Nutrition Risk Index (NRI) have different advantages and disadvantages. MNA-SF had higher sensitivity and demonstrated better predictive validity for poor appetite and weight loss.3 NRS 2002, MNA-SF and NRI are useful and practical tools with respect to screening for patients with COVID-19 who are at nutritional risk, as well as in need of additional nutritional intervention.9 So far, no measurement tool has been considered to be the best nutrition screening tool in older adults with COVID-19.3 We have adopted the Mini Nutritional Assessment-Short Form (MNA-SF) because it is easy to use in clinical practice as it contains only six items including decrease in food intake, weight loss, mobility, psychological distress or acute disease, neuropsychological problems, and body mass index.9 The sensitivity, specificity and diagnostic accuracy of malnutrition prediction were 97.9%, 100% and 98.7%, respectively, using a cut-off of 11 in MNA-SF.8
Our results revealed that malnutrition or at risk of malnutrition was associated with older age. One reason is that the physiological decline of food intake is very common in the elderly.11 The elderly themselves face a high risk of malnutrition also because of the diversity of their complications. For this segment of the population, nutritional intervention should be taken to address the current situation of nutritional deficiency and promote a healthy lifestyle. Our results showed that the vaccination rate was lower in the malnutrition or at risk of malnutrition group who were older. The elderly population often had the problem of decreased immunity.12,13 These findings suggest that there is a need to strengthen guidance in clinical practice and improve the vaccination proportion of this segment of the population.
A previous study has suggested that underweight (BMI <18.5) increased the risk of in-hospital mortality in patients with COVID-19, and malnutrition (0–7 points) increased the risk of in-hospital mortality in patients with COVID-19 and other causes.14 Our study suggests that MNA-SF scores were significantly associated with symptom relief in COVID-19 non-ICU patients and higher MNA-SF scores were associated with better prognosis, which were consistent with other studies.14,15
Nutrition is one of the important factors that determine the immune response of the human body, and good nutritional status helps to support immune function. On the contrary, malnourished people may have impaired immunity, which increases their susceptibility to infection,16 and the infectious disease may progress to more serious states; for example, the asymptomatic type may progress to the ordinary type. The normal operation of the immune system requires a much nutritional support, such as providing energy for the efficient function of the immune system, building blocks for the generation of RNA and DNA, the production of proteins and new cells, specific substrates for the production of immune-active metabolites, and regulators of immune cell metabolism.13 Therefore, an adequate amount of nutritional support is needed in patients with COVID-19.
Moreover, malnutrition is associated with inflammation and oxidative stress, which in turn affects the immune system. Maintaining the optimal state of protein, vitamin A, zinc, vitamin C, vitamin E, vitamin D and other related nutrients can effectively reduce inflammation and oxidative stress, thus playing a beneficial role in interfering with viral cell infection, optimizing antibody production, anti-inflammation, and anti-oxidation.16 Although the MNA-SF scale has no options for specific intake of protein, energy and vitamins, its assessment of food intake may indicate the nutritional support deficiencies of patients to some extent.
Many modifiable factors such as stress, physical fitness, frailty, body fatness and diet also affect the immune response.13 Frailty may influence adverse outcomes following infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).17 It follows, therefore, that those with a weak immune system should minimize their contact with the general population to reduce the risk of COVID-19 infection.18 MNA-SF also includes options of weight loss, mobility, and body mass index, which are also related with the patient’s degree of weakness.
On the other hand, the obesity paradox is widespread among the elderly.19 Our previous research showed the correlation between vascular function and obesity paradox.19,20 Interestingly, the obesity paradox also exists in COVID-19 patients. Patients with lower BMI had a worse prognosis.14 The average age of our study population was 65.7 years. The relationship between weight and physical health is complex for these segments of the older population. Central fat and relative loss of fat-free mass may become relatively more important than BMI in determining the health risk associated with obesity in the elderly.21 In the future, it can be considered to include body assessment indicators other than BMI (such as fat-free weight, muscle strength, grip strength) into the nutritional assessment to reduce the impact of confounding factors and better identify whether the obesity paradox exists in COVID-19 patients.
Harmful health behaviors, such as overeating, sedentary behavior with reduced physical activity, elevated alcohol and tobacco use, impaired sleep, are not only related to non-infectious diseases but also interfere with immunity.22 The options included in MNA-SF such as psychological distress or acute disease, neuropsychological problems may reflect the patient’s stress and some lifestyles. In the future, we can consider to further evaluate the mental and behavioral factors of patients and analyze their impact on the risk of COVID-19.
Our results also revealed that MNA-SF performance was related to the time of PCR negative conversion in COVID-19 patients. The higher the score, the shorter the time of negative conversion. Moderate-quality evidence suggests that dietary patterns and individual nutrients can influence systemic markers of immune function.22 A variety of diets and nutrients may provide anti-inflammatory and immunomodulatory effects on cardiovascular diseases, pulmonary diseases, and a variety of non-infectious diseases.23 For COVID-19 infection, these effects may still exist. COVID-19 mortality risk correlates with vitamin D3 status, and a mortality rate with close to zero could theoretically be achieved at 50 ng/mL 25(OH)D3.24 Sufficient 25(OH)D3 level may prevent or mitigate new outbreaks due to escape mutations or decreasing antibody activity. Adequate supplement of zinc, selenium and vitamin D can resist virus infection, improve immune function and reduce inflammation.25 Although our study did not provide parameters of nutritional elements for patients, a good MNA-SF score may indicate if the patient has adequate dietary intake including trace elements which may be beneficial to disease improvement. The effects of trace elements on immunity and inflammation will make PCR turn negative more quickly.
Interestingly, our study suggests that good nutritional status can significantly reduce the disease severity of COVID-19 patients in the non-vaccinated group. There were no significant correlations in the vaccinated group. Considering there is approximately around 10% of the population in China who did not receive vaccinations,26 supplement of nutritional supplementation could be critical for decreasing the disease severity of COVID-19 in non-vaccinated patients. Reasons for refusing to accept vaccinations are complex, including concerns about side effects of vaccines, perceived need for more clinical studies on the effectiveness and safety of the vaccines, and personal beliefs.27 Clearly, vaccination is an important preventive measure for symptomatic and severe COVID-19. Vaccine promotion activities should be carried out, and the elderly and other high-risk groups should be encouraged to participate in the vaccination programs. We should resolve misunderstanding through publicity and improve the level of awareness of COVID-19 infection and vaccines. The uninoculated population may have more complications and worse nutritional status, which also lead to patient hesitation to partake in vaccinations. Based on the interaction of relevant factors, more large-scale studies to assess the complex relationships within vaccines, nutritional status and disease severity of COVID should be further conducted.
As far as we know, there are only a few studies that have evaluated the nutritional risk and the severity of COVID-19 in Chinese patients.27 Due to different immunization strategies in different countries, the basic health status of the population also varies. It is undoubtedly of great significance to understand the correlation between the nutritional status of Chinese people and the severity of COVID-19 and to carry out nutritional intervention research in the future. Due to the scarcity of relevant research, our research may have certain advantages.
There are two main limitations of this study: The sample size of our study was small, and ICU patients with severe diseases were excluded. As the designated hospital in Shanghai to treat COVID-19 patients, we included as many high-quality samples as possible during the pandemic, but based on the epidemic time and policy changes, the research was carried out for a short time. In the future, a large sample size study which includes the entire disease severity of COVID-19 can be managed to assess the effects of nutrition on outcomes of patients with COVID-19.
Conclusion
Based on past long-term risk control measures, during this round of the Shanghai epidemic, we face significant challenges - a lack of experience in the application of mRNA vaccines and drugs. In the context of such a large-scale epidemic and temporary lockdown, nutrition is a promising intervention measure. Our study suggested that the group of patients with malnutrition or at risk of malnutrition is associated with older individuals, less vaccinated individuals, fewer asymptomatic types, and more individuals with longer PCR negative conversion times, lower BMI, and lower hemoglobin levels. With the increase of MNA-SF, the probability of all patients suffering from COVID-19 reduced. In conclusion, higher nutrition is associated with lower severity of COVID-19, especially in the non-vaccinated group. Higher nutrition is also associated with shorter time of PCR negative conversion in non-ICU COVID-19 patients. Adequate nutritional support is important for patients with COVID-19, especially for those who did not receive vaccinations.
Acknowledgments
We gratefully acknowledge the invaluable assistance of the physicians of the Department of Geriatrics, Department of Neurology and Institute of Neurology and Department of Nutrition, Ruijin Hospital, Shanghai Jiaotong University School of Medicine; the study would not have been possible without their support.
Funding Statement
This research was funded by Clinical Science and Shanghai Municipal Hospital New Frontier Technology Joint Project (SHDC12019X20), Shanghai Municipal Commission of Health and Family Planning (Grant No.2020YJZX0124).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Tan CX, Wong SC, Tan SS, Tan ST. Knowledge, attitudes, and practices towards COVID-19 among undergraduates during emergency remote learning. Discov Soc Sci Health. 2022;2(1):13. PMID: 35936821; PMCID: PMC9342596. doi: 10.1007/s44155-022-00017-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Majumder J, Minko T. Recent developments on therapeutic and diagnostic approaches for COVID-19. AAPS J. 2021;23(1):14. PMID: 33400058; PMCID: PMC7784226. doi: 10.1208/s12248-020-00532-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silva DFO, Lima SCVC, Sena-Evangelista KCM, Marchioni DM, Cobucci RN, Andrade FB. Nutritional risk screening tools for older adults with COVID-19: a systematic review. Nutrients. 2020;12(10):2956. PMID: 32992538; PMCID: PMC7599513. doi: 10.3390/nu12102956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu G, Zhang S, Mao Z, Wang W, Hu H. Clinical significance of nutritional risk screening for older adult patients with COVID-19. Eur J Clin Nutr. 2020;74:876–883. doi: 10.1038/s41430-020-0659-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lochs H, Allison SP, Meier R, et al. Introductory to the ESPEN guidelines on enteral nutrition: terminology, definitions and general topics. Clin Nutr. 2006;25(2):180–186. PMID: 16697086. doi: 10.1016/j.clnu.2006.02.007 [DOI] [PubMed] [Google Scholar]
- 6.Antwi J, Appiah B, Oluwakuse B, Abu BAZ. The nutrition-COVID-19 interplay: a review. Curr Nutr Rep. 2021;10(4):364–374. PMID: 34837637; PMCID: PMC8627159. doi: 10.1007/s13668-021-00380-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galmés S, Serra F, Palou A. Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework. Nutrients. 2020;12(9):2738. PMID: 32911778; PMCID: PMC7551697. doi: 10.3390/nu12092738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol a Biol Sci Med Sci. 2001;56:M366–M372. doi: 10.1093/gerona/56.6.M366 [DOI] [PubMed] [Google Scholar]
- 9.Kaluźniak-Szymanowska A, Krzymińska-Siemaszko R, Lewandowicz M, Deskur-śmielecka E, Stachnik K, Wieczorowska-Tobis K. Diagnostic performance and accuracy of the MNA-SF against GLIM criteria in community-dwelling older adults from Poland. Nutrients. 2021;13(7):2183. PMID: 34202898; PMCID: PMC8308417. doi: 10.3390/nu13072183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. Available from: https://www.R-project.org/. Accessed June 20, 2023. [Google Scholar]
- 11.Kaur D, Rasane P, Singh J, et al. Nutritional interventions for elderly and considerations for the development of geriatric foods. Curr Aging Sci. 2019;12(1):15–27. PMID: 31109282; PMCID: PMC6971894. doi: 10.2174/1874609812666190521110548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pawelec G, Larbi A, Derhovanessian E. Senescence of the human immune system. J Comp Pathol. 2010;142:S39–44. doi: 10.1016/j.jcpa.2009.09.005 [DOI] [PubMed] [Google Scholar]
- 13.Agarwal S, Busse PJ. Innate and adaptive immunosenescence. Ann Allergy Asthma Immunol. 2010;104:183–190. doi: 10.1016/j.anai.2009.11.009 [DOI] [PubMed] [Google Scholar]
- 14.Kananen L, Eriksdotter M, Boström AM, et al. Body mass index and mini nutritional assessment-short form as predictors of in-geriatric hospital mortality in older adults with COVID-19. Clin Nutr. 2022;41(12):2973–2979. PMID: 34389208; PMCID: PMC8318666. doi: 10.1016/j.clnu.2021.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang K, Gui H, Cong J, He P. A modified nutrition risk screening 2002 predicts the risk of death among hospitalized patients with COVID-19. Clin Nutr ESPEN. 2022;52:365–370.PMID: 36513477; PMCID: PMC9482444. doi: 10.1016/j.clnesp.2022.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calder PC. Nutrition and immunity: lessons for COVID-19. Eur J Clin Nutr. 2021;75(9):1309–1318. PMID: 34163017; PMCID: PMC8220366. doi: 10.1038/s41430-021-00949-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolford SJ, D’Angelo S, Curtis EM, et al. COVID-19 and associations with frailty and multimorbidity: a prospective analysis of UK Biobank participants. Aging Clin Exp Res. 2020;32(9):1897–1905. PMID: 32705587; PMCID: PMC7377312. doi: 10.1007/s40520-020-01653-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landi F, Barillaro C, Bellieni A, et al. The new challenge of geriatrics: saving frail older people from the Sars-COV-2 pandemic infection. J Nutr Health Aging. 2020;24:466–470. doi: 10.1007/s12603-020-1356-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang H, Zhao J, Deng X, et al. Pulse wave velocity is decreased with obesity in an elderly Chinese population. J Clin Hypertens. 2019;21(9):1379–1385. PMID: 31471955; PMCID: PMC8030623. doi: 10.1111/jch.13659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tang B, Luo F, Zhao J, et al. Relationship between body mass index and arterial stiffness in a health assessment Chinese population. Medicine. 2020;99(3):e18793. PMID: 32011479; PMCID: PMC7220472. doi: 10.1097/MD.0000000000018793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. 2021;26(1):27–35. PMID: 31865598. doi: 10.1007/s40519-019-00815-4 [DOI] [PubMed] [Google Scholar]
- 22.Lange KW, Nakamura Y. Lifestyle factors in the prevention of COVID-19. Glob Health J. 2020;4(4):146–152. PMID: 33520339; PMCID: PMC7834031. doi: 10.1016/j.glohj.2020.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zabetakis I, Lordan R, Norton C, Tsoupras A. COVID-19: the inflammation link and the role of nutrition in potential mitigation. Nutrients. 2020;12(5):1466. PMID: 32438620; PMCID: PMC7284818. doi: 10.3390/nu12051466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borsche L, Glauner B, von Mendel J. COVID-19 mortality risk correlates inversely with Vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/mL 25(OH)D3: results of a systematic review and meta-analysis. Nutrients. 2021;13(10):3596. PMID: 34684596; PMCID: PMC8541492. doi: 10.3390/nu13103596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alexander J, Tinkov A, Strand TA, Alehagen U, Skalny A, Aaseth J. Early nutritional interventions with zinc, selenium and Vitamin D for raising anti-viral resistance against progressive COVID-19. Nutrients. 2020;12(8):2358. PMID: 32784601; PMCID: PMC7468884. doi: 10.3390/nu12082358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y, Wang Y, Ning G, Ping H, Wang W. Protecting older people: a high priority during the COVID-19 pandemic. Lancet. 2022;400(10354):729–730. doi: 10.1016/S0140-6736(22)01530-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kacimi SEO, Klouche-Djedid SN, Riffi O, et al. Determinants of COVID-19 vaccine engagement in Algeria: a population-based study with systematic review of studies from Arab countries of the MENA region. Front Public Health. 2022;10:843449.PMID: 35712268; PMCID: PMC9196869. doi: 10.3389/fpubh.2022.843449 [DOI] [PMC free article] [PubMed] [Google Scholar]