The work produced by this manuscript can be used by hospitals and healthcare organizations to understand sick leave duration and its predictors among their workers. The results can inform improving and changing sick leave policies for HCWs during pandemics.
Key Words: COVID-19, Healthcare workers, Sick leave, Tertiary medical center
Background
Little has been published on predictors of prolonged sick leaves during the COVID-19 pandemic. This study aims to determine the rate of COVID-19 infections among healthcare workers (HCWs) and to identify the predictors of longer sick leave days.
Methods
We identified predictors of longer sick leave using linear regression analysis in a cross-sectional study design.
Results
Thirty-three percent of the total workforce contracted COVID-19. On average, HCWs took 12.5 sick leave days after COVID-19 infection. The regression analysis revealed that older employees, nurses, and those who caught COVID-19 earlier in the pandemic were more likely to take longer sick leave.
Conclusions
Age, job position, and month of infection predicted sick leave duration among HCWs in our sample. Results imply that transmission was most likely community-based. Public health interventions should consider these factors when planning for future pandemics.
LEARNING OUTCOMES
Identify the predictors associated with longer sick leave duration among healthcare workers (HCWs) during the COVID-19 pandemic.
Understand the COVID-19 prevalence among HCWs in a tertiary medical center and the professions with the highest infection rate.
Discuss COVID-19 prevalence and transmission in a healthcare setting compared with the community.
Because of the nature of their work, healthcare workers (HCWs) are more likely to contract infections as compared with the general population.1 Since the start of the COVID-19 pandemic in late December 2019, HCWs were deemed to be at higher risk of exposure to SARS-CoV-2 infection.2 A large study conducted in the United Kingdom (UK) found that HCWs were at a seven times higher risk of being infected with SARS-CoV-2.3 Identified risk factors for acquiring the infection among this group include improper use of personal protective equipment, workplace setting, profession, exposure, contacts, and testing.2 As of December 31, 2020, more than 1.6 million HCWs were reported to be infected with SARS-CoV-2 in 34 countries.4 In countries with available data, the prevalence of COVID-19 infections among HCWs varied between 2.2% and 29% earlier in the pandemic.5 In a study identifying infection rates among HCWs using data from 37 countries (including Lebanon) between July and August 2020,6 it was found that a large number of HCWs were getting infected, with a mortality rate of 0–0.90 per 100,000.2 According to the Lebanese Ministry of Public Health data on COVID-19 infections among HCWs, approximately 2500 HCWs were infected as of February 14, 2021, before the start of vaccination campaigns.7
Sick leave among HCWs has been a major concern during the COVID-19 pandemic. A systematic review on COVID-19 infections among HCWs globally revealed that the overall infection and deaths trends were similar to the general population, while infections were highest among nurses and deaths highest among doctors.8 While a few studies assessed predictors of sick leave post COVID-19 in the general population, little has been published on the predictors of sickness-related absences secondary to COVID-19 among HCWs.9 A Swedish study investigated the predictors of taking long sick leave among HCWs and residential care workers (defined as sick leave longer than 3 weeks) and found that working in residential care, having obesity, depression or anxiety, and taking longer sick leave before the pandemic were significant predictors of longer sick leave during the pandemic.10
Infection rates and sick leave trends among HCWs differ between the prevaccination and postvaccination periods. While studies provided evidence that HCWs took longer sick leave periods because of their COVID-19 infection, evidence also suggests that vaccinated HCWs take shorter sick leave periods and have lower incidence of COVID-19 infections.11,12
Our study aims to determine the rate of COVID-19 infections among HCWs before the start of vaccination and to identify the predictors of taking more sick leave days among HCWs who tested positive for COVID-19 in a tertiary medical center.
METHODS
We conducted a cross-sectional study at the American University of Beirut Medical Center (AUBMC) on data collected between March 2020 and February 2021. The AUBMC is a 364-bed tertiary care private hospital and is one of the largest medical facilities in the country. The AUBMC played a major role in managing the pandemic and serving as a model to other hospitals in the country and the region. A separate hospital building initially functioning as a pediatric cancer center was transformed to a Pandemic Evaluation Clinic and Center to exclusively treat and admit COVID-19 patients. A “train the trainer” model was implemented to reach and train the largest number of HCWs on infection prevention and control measures for management of COVID-19 including proper personal protective equipment donning and doffing. Overall, 1631 HCWs (representing approximately 70% of staff involved in direct patient care) were trained between March 10 and April 30, 2020.
The deidentified data set of all HCWs infected with SARS-CoV-2 at the AUBMC since the beginning of the pandemic and until February 14, 2021 was reviewed to determine the predictors of longer sick leave periods. The number of cases among our healthcare workforce was compared with the surge in cases nationally.
The variables on HCWs included sex, age, position in the medical center, department, month of infection, date of positive polymerase chain reaction result, number of sick leave days, and the source of infection (community, hospital-acquired, or unknown). The source of COVID-19 infections among HCWs was investigated by the infection control team through direct phone calls with the staff who tested positive and review of their medical records from March to December 2020. Starting January 2021, investigations were limited to review of medical records only.
The study was approved by the institutional review board at the American University of Beirut (AUB).
As per the latest data obtained from the human resource department at the AUBMC, the medical center has 3132 HCWs. Age was classified into the following four categories to look at differences in COVID-19 sick leaves by age group: 30 years or younger, 31 to 40 years, 41 to 50 years, and 51 years and older. The HCWs were classified into the following four major areas based on their work activities: high-risk areas (workers in areas with potential or confirmed COVID-19 cases), inpatient care areas (workers in direct contact with non–COVID-19 patients), outpatient care areas (workers in contact with outpatients), and support services (workers providing support services such as administrators, IT staff, etc.). As for job positions, we followed the categorization adopted by the human resource department. As such, HCWs were classified into the following nine categories: doctors (attending physicians, residents, and fellows), nurses (registered nurses, practical nurses, and nursing assistants), administrative (clerks, cashiers, etc.), allied health personnel (technicians, therapists, laboratory staff, etc.), general services and support (housekeeping, kitchen staff, etc.), technology and engineering (IT staff), students (medical students), research staff (research assistants and research fellows), and others.
The timeline of COVID-19 infection was divided into the following three categories: March 2020 to August 13, 2020; August 14, 2020 to November 2020, and December 2020 to February 2021. The cutoff for August 13 was chosen because it represents the day when contact tracing for HCWs stopped by employee health unit due to the increase in the number of cases nationally.
Sources of infections were classified into the following three different categories:
Community-acquired infections: this applies for HCWs who were exposed to a known or suspected COVID-19 person outside their work in the medical center.
Hospital-acquired infections: this described HCWs whose exposures were attributed to an unprotected exposure to a confirmed COVID-19 case in the hospital.
Source of COVID-19 infection was labeled as unknown when the source of transmission could not be identified.
Data were entered into the Statistical Package for Social Sciences (SPSS, version 27), which was used for data cleaning, management, and analyses. Descriptive statistics were summarized by presenting the frequency and percentages for categorical variables and mean and standard deviation for continuous variables.
The main outcome of this study was the number of sick leave days among HCWs. Predictors of sick leave days were identified using linear regression analysis. The regression model included variables that either had a P value less than 0.2 at the bivariate analysis level or known to be associated with sick leave days from previous literature. The variable “source of infection” was excluded from the analysis as more than 50% of the infections were of unidentified source. Results were presented in terms of coefficients and 95% confidence intervals. A P value of 0.05 was considered statistically significant.
The infection rate among specific HCW categories was calculated by dividing the number of infected HCWs by the total number of HCWs. In addition, Pearson correlation analysis was used to assess the correlation between the positive cases among HCWs and the COVID-19 cases at the national level.
RESULTS
Table 1 below describes the characteristics of our study population of COVID-19–positive HCWs. Most HCWs (55.4%) were males and younger than 30 years (39.2%). Nurses represented the largest group of COVID-19–positive HCWs, followed by doctors, and auxiliary hospital services staff. Most HCWs who tested positive for COVID-19 worked in non–COVID-19 inpatient areas (54.9%) or in outpatient settings (27%). Those who worked in high-risk COVID-19 areas constituted only 10.8 % of the cases.
TABLE 1.
Descriptive Statistics of COVID-19–Positive Healthcare Workers at AUBMC
| N = 1,028 | |
|---|---|
| Frequency (%) | |
| Sex (n = 1,016) | |
| Male | 563 (55.4) |
| Female | 453 (44.6) |
| Age (n = 1,014) | |
| 30 y or less | 398 (39.2) |
| 31–40 y | 328 (32.3) |
| 41–50 y | 172 (16.9) |
| 51 y and older | 116 (11.6) |
| Job position-based on AUB categorization (n = 1,014) | |
| Nurses | 374 (36.9%) |
| Allied health (lab staff, pharmacy staff, physical therapy staff, technician, radiology staff) | 155 (15.3%) |
| General services and support (kitchen/catering, and housekeeping) | 152 (15.0%) |
| Doctors | 135 (13.3%) |
| Administrative (administrator, clerk) | 65 (6.4%) |
| Student | 20 (2%) |
| Technology and engineering (IT) | 18 (1.8%) |
| Research staff | 11 (1.1%) |
| Other | 84 (8.3%) |
| Department (n = 636) | |
| Inpatient non–COVID-19 | 349 (54.9) |
| Outpatient | 172 (27.0) |
| High-risk COVID-19 areas | 69 (10.8) |
| Support services | 46 (7.2) |
| Infection source (n = 1,025) | |
| Unspecified | 528 (51.4) |
| Community exposure | 321 (31.2) |
| Hospital acquired | 179 (17.4) |
| Month of infection (n = 1,106) | |
| December 2020–February 2021 | 552 (54.3) |
| August 14–November 2020 | 429 (42.2) |
| March–August 13, 2020 | 35 (3.4) |
| Mean ± SD | |
| Sick leave days | 12.50 ± 4.00 |
The source of infection was unknown for approximately half of HCWs (51.4%). For participants with known infection source, community exposure (31.2%) was higher than hospital exposure (17.4%).
During the peak of the pandemic, the risk for COVID-19 transmissions was increased among HCWs as most cases occurred in January and February 2021 (43.4%). On average, HCWs took 12.5 days of sick leave because of COVID-19 infection.
As of February 14, 2021, approximately 33% of the HCWs at the AUBMC got infected with COVID-19 (Table 2).
TABLE 2.
COVID-19 Infection Rate Among the Specific HCWs Professions
| Job Family | Total No. HCWs (N = 3,132) | No. Infected HCWsa (n = 899) | Infection Rate |
|---|---|---|---|
| Allied health | 409 | 155 | 37.8% |
| Nursing (professionals, support staff) | 999 | 374 | 37.4% |
| Medical doctors (attending, fellows, residents) | 417 | 135 | 32.3% |
| Administrative staff | 529 | 152 | 28.7% |
| General services and support | 294 | 65 | 22.1 % |
| Technology and engineering | 84 | 18 | 21.4% |
aExcluding students, research staff, and others, as the denominator for these categories was unavailable.
HCWs, healthcare workers.
Data on predictors of longer sick leave days due to COVID-19 infections among HCWs (Table 3) showed that older employees took longer sick leave compared with employees who are younger than 30 years. Employees 51 years and older took an additional 1.4 sick leave days (P = 0.001**), while those aged 41 to 50 years took an additional 1.23 days (P = 0.001**). When compared with doctors, nurses took an additional 1.2 day on average (P = 0.003**). Females did not take longer sick leave compared with males. More sick leave days were taken early in the pandemic (March–August 13, 2021). An average of 4.5 additional days was taken between March and August 13, 2020, followed by 1.4 day between August 13 and November 2020, as compared with the period between December 2020 and February 2021. Based on our model, older age, working as a nurse, and contracting COVID-19 earlier in the pandemic are all factors associated with a higher number of sick leave days in our hospital.
TABLE 3.
Linear Regression of the Predictors of Number of Sick Leave Days
| Model | Unstandardized Coefficients | Sig. | 95.0% Confidence Interval for B | ||
|---|---|---|---|---|---|
| B | Std. Error | Lower Bound | Upper Bound | ||
| (Constant) | 10.959 | 0.506 | <0.001 | 9.966 | 11.952 |
| Sex | |||||
| Female | −0.235 | 0.253 | 0.352 | −0.731 | 0.261 |
| Age group | |||||
| 31–40 y | −0.091 | 0.301 | 0.762 | −0.682 | 0.500 |
| 41–50 y | 1.230 | 0.364 | 0.001** | 0.516 | 1.944 |
| 51 y and older | 1.396 | 0.420 | 0.001** | 0.571 | 2.221 |
| Infection month | |||||
| March–August 13 2020 | 4.561 | 0.714 | <0.001*** | 3.159 | 5.963 |
| August 14–Nov 2020 | 1.403 | 0.252 | <0.001*** | 0.909 | 1.897 |
| Position | |||||
| Nurses | 1.178 | 0.397 | 0.003** | 0.399 | 1.957 |
| General services and support | 0.549 | 0.600 | 0.360 | −0.627 | 1.726 |
| Administrative staff | 0.779 | 0.467 | 0.096 | −0.139 | 1.696 |
| Allied Health | .851 | 0.469 | 0.070 | −0.069 | 1.771 |
| Technology and engineering | −0.270 | 0.973 | 0.781 | −2.179 | 1.639 |
| Students | 1.626 | 0.932 | 0.081 | −0.202 | 3.455 |
| Research staff | 2.088 | 1.211 | 0.085 | −0.288 | 4.465 |
| Other | 0.367 | 0.556 | 0.509 | −0.724 | 1.458 |
Variables included in the model were as follows: sex (reference: male); age (reference: <30 years); month (reference: December 2020–February 2021); position (reference: doctors.
*P < 0.05; **P < 0.01; ***P < 0.001
The number of COVID-19 cases among HCWs strongly correlated with the number of cases diagnosed in the country. Numbers were correlated by week and the correlation coefficient was 0.99 with a P value less than 0.001***. This result suggests that the number of HCWs who tested positive for COVID-19 increased with the rise in the number of cases nationally (Figure 1).
FIGURE 1.
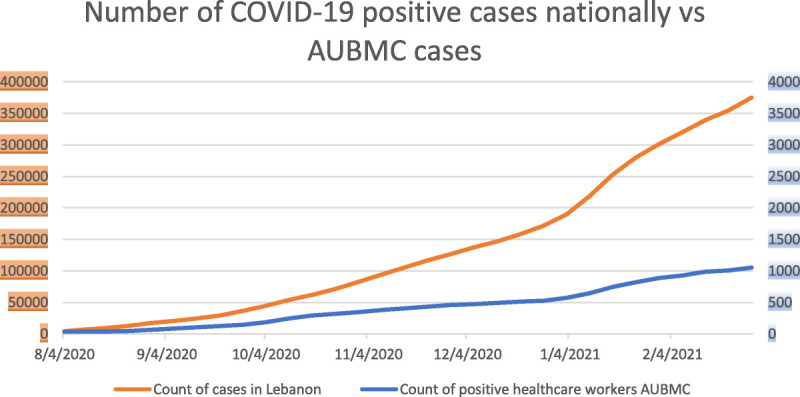
COVID-19 cases nationally versus AUBMC from August 2020 to February 28, 2021.
DISCUSSION
Almost a third of the AUBMC workforce contracted COVID-19 between the beginning of the pandemic and the start of the vaccination campaign. The highest affected percentage was nurses and the overwhelming majority of cases were not working in the COVID-19 unit. As a result of these infections, an average of 12.5 sick leave days was given for each HCW with COVID-19.
Although HCWs might be at high risk of acquiring COVID-19 through occupational exposure, we observed an increase in cases when the transmission increased in the community. In addition, cases observed among our HCWs were not reported in high-risk settings, such as COVID-19 clinical areas. In fact, approximately 90% of infected HCWs worked in non-COVID units inside the hospital. With wide community spread of infections, it would be difficult to ascertain the source of transmission. However, community transmissions could result in secondary in-hospital transmission between HCWs during breaks or lunches, in the context of lack of implementation of safety guidelines. This has been shown in a previous study where having lunch in the same break room was considered as one of the most important risk factors for COVID transmission between HCWs.13 Our data are in accordance with previous reports revealing that the number of HCWs cases secondary to occupational exposure increased between September and November 2020, which was simultaneous with the rise in the number of cases in the Midwest.14 Along the same token, similar studies found that infection trends among HCWs correlate with community infection rates.15,16 These findings suggest that HCWs were infected from a community source, potentially spreading the infection to their colleagues at work, resulting in an increased risk for occupational exposure.17 This hypothesis could only be confirmed by further assessments of the source of infection of HCWs.
Consistent with studies reported in other countries, approximately 33% of our workforce got infected with COVID-19 during a 1-year period (until February 14, 2021), the majority being infected in 2021. A systematic review conducted in August 2020 on COVID-19 among HCWs included 82 studies from countries around the world, with infection rates among HCWs ranging from 1% to 24% in some settings.18 This was also the case in other countries, as absenteeism due to COVID-19 was leading to significant losses in productivity, and HCWs took on average 10 to 14 days to be back to work, which was comparable with our medical center.18 The resulting absenteeism created a major impact on the workforce at AUBMC by increasing the workload on the remaining staff. This is consistent with previous studies conducted, showing an association between absenteeism and high workload in healthcare settings.19
The results of our study showed that most HCWs infected with COVID-19 in our institution were males, 30 years or younger, worked in inpatient settings, and were mostly nurses. The age of our infected HCWs aligns with a systematic review and meta-analysis on COVID-19–infected HCWs, which revealed that most HCWs infected with COVID-19 belonged to a young working age population.2 Contrary to our study, however, females made up the majority of infected HCWs included in this review.2 It was also reported that the risk of infection was the highest for those working in inpatient settings,20 and this is what the distribution of cases in our sample reflected. Looking at the risk of infection by profession, physicians were found to be at increased risk as compared with nurses or general service employees.21,22 Our study similarly showed that physicians and nurses had a higher infection rate compared with general services employees, with nurses having the highest rate of infection with COVID-19.
When investigating the sick leave period for HCWs who tested positive for COVID-19, our data showed that older age, job position, and month of COVID-19 infection were significant predictors of taking a higher number of sick leave days. The sick leave period did not statistically differ between males and females in our study. This finding is comparable with a similar study investigating predictors of prolonged sick leave in a sample of Swedish HCWs.10 Previous studies showed that older age is a significant predictor of longer sick leave period among HCWs.23 Older age is associated with comorbidities like hypertension, diabetes, heart disease, and cancer, all of which correlate well with severe disease when infected with COVID-19.24 As for job categories, it is well known that workers involved in direct patient care and high-risk areas (such as nurses and doctors) take more sick leave compared with other workers. The fact that HCWs were taking longer sick leave during earlier months of the pandemic is probably secondary to the medical center’s policy, as isolation periods were longer earlier in the pandemic.
In one medical center in London, it was shown that the sick leave did not differ between clinical and nonclinical staff and that medical doctors took the lowest number of sick leave days during their infection.15 This is comparable with our study, as our data have shown no association between sick leave days and working in different areas (high-risk COVID areas, direct patient care areas, outpatient care areas, and support services). This could be since working in a high risk COVID area necessitates implementing workplace control measures to reduce exposures, thus diluting the extra risk imposed on them during their work shifts.
Limitations
Our study has several limitations. The variables available on infected HCWs are limited, making it hard to identify all potential risk factors and to test for any confounders. For example, data on existing health conditions and whether the HCW required hospitalization was not available. Although we lacked data on employees who developed long COVID, which in some studies has affected about a third of HCWs,25 we calculated the average days of sickness-related absences among employees who developed COVID versus those who did not. Those who had developed COVID previously took on average of 0.79 more sick leave day than those who hadn’t (4.68 vs 3.89). In addition, because this study was done in a single medical center, the results cannot be generalized to the broader population of HCWs in Lebanon. Nevertheless, this study fills an important gap in the literature by providing data on predictors of the sick leave period among HCWs infected with COVID-19. During the COVID-19 pandemic, studies on HCWs mostly focused on risk factors for COVID-19 transmission and changes in sick leave patterns compared with the pre pandemic period. Few studies have investigated predictors of taking longer sick leave periods among HCWs.
CONCLUSIONS
The nature of the COVID-19 pandemic and the burden exerted on healthcare systems stressed on the primordial role of the HCWs and underlined the necessity of making their safety a priority. Surveillance of workers during pandemics through an integrated strategy was critical to detect and manage COVID-19 cases. Despite all the measures taken, almost a third of our HCWs got infected with COVID-19 and had to be absent from work for a significant period. This may have led to an increased pressure on the remaining HCWs and on the hospital administration. Older employees, nurses, and those who caught COVID-19 earlier in the pandemic were more likely to take longer sick leave. Public health interventions and hospital policies should consider these factors when planning for future pandemics. Infections trends among our workforce implied that transmission was not secondary to COVID-19 patient contact and was most likely community based.
Footnotes
Funding: None to disclose.
Conflict of interest: None declared.
Authors’ Contributions: C.J.S. and L.F. designed the study, worked on data analysis, and wrote the first draft of the manuscript. N.M.M. edited the manuscript and oversaw aspects of the study design. M.F. worked on some parts of the manuscript. H.B., N.K.Z., S.K., R.D., and J.T. edited the manuscript. U.M. participated in designing the study and provided feedback on the manuscript. M.S. and C.A.R. supported in the data analysis and edited the manuscript. D.R. oversaw all aspects of the study and edited the manuscript.
C.J.S. and L.F. equally contributed to the manuscript.
All authors reviewed, edited, and approved the final manuscript.
Ethical approval: The study was approved by the institutional review board at the American University of Beirut (protocol number SBS-2020-0463).
Contributor Information
Carine J. Sakr, Email: cs56@aub.edu.lb.
Lina Fakih, Email: lf32@aub.edu.lb.
Nada M. Melhem, Email: melhemn@aub.edu.lb.
Mohammad Fakhreddine, Email: maf54@mail.aub.edu.
Umayya Musharrafieh, Email: um00@aub.edu.lb.
Hanin Banna, Email: hb77@aub.edu.lb.
Rita Doudakian, Email: rd01@aub.edu.lb.
Nada Kara Zahreddine, Email: nk13@aub.edu.lb.
Joseph Tannous, Email: tannousj@hotmail.com.
Souha S. Kanj, Email: sk11@aub.edu.lb.
Martin Slade, Email: martin.slade@yale.edu.
Carrie A. Redlich, Email: carrie.redlich@yale.edu.
REFERENCES
- 1.Jones N, Carver C. Are Interventions Such as Social Distancing Effective at Reducing the Risk of Asymptomatic Healthcare Workers Transmitting COVID-19 Infection to Other Household Members. United Kingdom: Centre for Evidence Based Medicine; 2020. [Google Scholar]
- 2.Gholami M Fawad I Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis 2021;104:335–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mutambudzi M Niedzwiedz C Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med 2021;78:307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ICN . International Council of Nurses COVID-19 Update. 2021. Available at: https://www.icn.ch/sites/default/files/inline-files/IND2021-Factsheet-01-UPDATED-EN.pdf. Accessed May 6, 2023.
- 5.ECDC . Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK–ninth update. 2020. Available at: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-pandemic-ninth-update. Accessed May 6, 2023.
- 6.Erdem H, Lucey DR. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis 2021;102:239–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MOPH . Coronavirus COVID-19 Lebanon cases. 2022. Available at: https://www.moph.gov.lb/maps/covid19.php. Accessed January 17, 2022.
- 8.Bandyopadhyay S Baticulon RE Kadhum M, et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health 2020;5:e003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westerlind E, Palstam A, Sunnerhagen KS, Persson HC. Patterns and predictors of sick leave after COVID-19 and long COVID in a national Swedish cohort. BMC public health 2021;21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kisiel MA, Nordqvist T, Westman G, Svartengren M, Malinovschi A, Janols H. Patterns and predictors of sick leave among Swedish non-hospitalized healthcare and residential care workers with COVID-19 during the early phase of the pandemic. PLoS One 2021;16:e0260652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palladino R Mercogliano M Fiorilla C, et al. Association between COVID-19 and sick leave for healthcare workers in a large academic hospital in southern Italy: an observational study. Int J Environ Res Public Health 2022;19:9670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prato S, et al. Effect of BNT162b2 mRNA vaccination on the incidence of COVID-19 and duration of sick leave among healthcare workers: a retrospective cohort study. J Occup Environ Med 2021. doi: 10.1097/JOM.0000000000002389. PMID: 34538839; PMCID: PMC8630929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Çelebi G Pişkin N Çelik Bekleviç A, et al. Specific risk factors for SARS-CoV-2 transmission among health care workers in a university hospital. Am J Infect Control 2020;48:1225–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ibiebele J, Silkaitis C, Dolgin G, Bolon M, JaneCullen, Zembower T. Occupational COVID-19 exposures and secondary cases among healthcare personnel. Am J Infect Control 2021;49:1334–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng C Hafezi-Bakhtiari N Cooper V, et al. Characteristics and transmission dynamics of COVID-19 in healthcare workers at a London teaching hospital. J Hosp Infect 2020;106:325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wight E Swift M O'Horo JC, et al. COVID-19 infections in health care personnel by source of exposure and correlation with community incidence. J Occup Envi Med 2022;64:675–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farah W, Breeher L, Shah V, Wang Z, Hainy C, Swift M. Coworkers are more likely than patients to transmit SARS-CoV-2 infection to healthcare personnel. Occup Environ Med 2022;79:713–716. [DOI] [PubMed] [Google Scholar]
- 18.Yaghoubi M, Salimi M, Meskarpour-Amiri M. Systematic review of productivity loss among healthcare workers due to COVID-19. Int J Health Plan Manag 2022;37:94–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kowalczuk K, Krajewska-Kułak E, Sobolewski M. Working excessively and burnout among nurses in the context of sick leaves. Front Psychol 2020;11:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen LH Drew DA Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 2020;5:e475–e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen T Wu D Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garzaro G Clari M Ciocan C, et al. COVID-19 infection and diffusion among the healthcare workforce in a large university-hospital in northwest Italy. La Medicina del Lavoro 2020;111:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donders NC, Bos JT, van der Velden K, van der Gulden JWJ. Age differences in the associations between sick leave and aspects of health, psychosocial workload and family life: a cross-sectional study. BMJ Open 2012;2:e000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geng J Yu X Bao H, et al. Chronic diseases as a predictor for severity and mortality of COVID-19: a systematic review with cumulative meta-analysis. Front Med 2021;8:1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaber TAK, Ashish A, Unsworth A. Persistent post-COVID symptoms in healthcare workers. Occup Med (Lond) 2021;71:144–146. [DOI] [PMC free article] [PubMed] [Google Scholar]


