Abstract
Audience
This simulation-based scenario is appropriate for senior level emergency medicine residents.
Introduction
Pulseless electrical activity (PEA) accounts for up to 25% of sudden cardiac arrest;1 therefore the ability to recognize and care for this condition is an essential skill of emergency medicine physicians. Management of PEA arrest in the emergency department centers on Advanced Cardiac Life Support (ACLS) algorithms and the identification and treatment of potentially reversible causes. Massive pulmonary embolism (PE) is one of several causes of PEA cardiac arrest.2 However, diagnosis by CT-angiographic or nuclear imaging may not be obtainable in the hemodynamically unstable patient, requiring physicians to have a high index of suspicion. Systemic thrombolytic therapy is indicated in cardiac arrest due to known or presumed massive pulmonary embolism.3,4,5
Educational Objectives
After competing this simulation-based session, the learner will be able to:
Identify PEA arrest
Review the ACLS commonly recognized PEA arrest etiologies via the H &T mnemonic
Review and discuss the risks and benefits of tissue plasminogen activator (tPA) for massive PE
Educational Methods
This is a high-fidelity simulation that allows learners to evaluate and treat a PEA arrest secondary to massive PE in a safe environment. The learners will demonstrate their ability to recognize a PEA arrest, sort through possible etiologies, and demonstrate treatment of a massive PE with tPA. Debriefing will focus on diagnosis and management of the PEA arrest.
Research Methods
This case was piloted with 12 PGY-2 and PGY-3 residents. Group and individual debriefing occurred post-case.
Results
Post-simulation feedback from the faculty suggested two potential issues. First was fidelity, which we increased by using our ultrasound simulator. Second, the elevated presenting glucose with lactic acidosis could be a poor cue, leading some towards diabetic ketoacidosis (DKA).
Discussion
Learners felt more confident about running a PEA arrest. The simulation improved resident awareness of the value of point of care ultrasound (POCUS) in cardiac arrest. It also clarified the dosing of tPA in massive PE. Faculty felt simulating the actual US without breaking simulation would be more challenging without our US simulator. Although there was concern about results pointing towards possible DKA, this did not occur in any of the pilot simulations. The presenting glucose was reduced to make this less likely in future simulations.
Topics
Pulseless electrical activity (PEA), syncope, cardiac arrest, Hs and Ts from ACLS PEA instruction, tPA for massive PE, critical care medicine, simulation.
USER GUIDE
| List of Resources: | |
|---|---|
| Abstract | 1 |
| User Guide | 3 |
| Instructor Materials | 5 |
| Operator Materials | 15 |
| Debriefing and Evaluation Pearls | 18 |
| Simulation Assessment | 21 |
Learner Audience:
Senior residents
Time Required for Implementation:
Instructor Preparation: 30–60 minutes
Time for case: 15–30 minutes
Time for debriefing: 15–30 minutes
Recommended Number of Learners per Instructor:
1
Topics:
Pulseless electrical activity (PEA), syncope, cardiac arrest, Hs and Ts from ACLS PEA instruction, tPA for massive PE, critical care medicine, simulation.
Objectives:
By the end of this simulation session, the learner will be able to:
Identify PEA arrest
Review the ACLS commonly recognized PEA arrest etiologies via the H &T mnemonic
Review and discuss the risks and benefits of (tPA) for massive PE
Linked objectives and methods
By completing this simulation, learners will take a brief history and physical before the patient arrests. After intubation, the patient will arrest and cardiopulmonary resuscitation (CPR) will be initiated. The learner will identify PEA as the rhythm (objective 1) and continue the resuscitation while divulging the possible etiologies via the H&Ts mnemonic (objective 2). Once PE is recognized as a likely cause, the learner with discuss the pros & cons of tPA administration or be prompted to do so. Although learners are familiar with PE, most learners have not all seen cardiac arrest secondary to massive PE. Simulation develops comfort with diagnostic uncertainty and the administration of tPA without confirmatory imaging findings. This case forces them to process the tPA administration risk and benefits in a safe environment (objective 3). Debriefing will ensure that any potential misconceptions or knowledge gaps are addressed.
Recommended pre-reading for instructor
-
DePalo VA, Kharnaf AE. Venous Thromboembolism (VTE) Treatment & Management. In: Medscape. Panchbhavi VK, ed.
https://emedicine.medscape.com/article/1267714-treatment#d10. Published June 12, 2019. Accessed July 2, 2019.
Kline JA. Pulmonary embolism and deep vein thrombosis. In: Walls RM, Hockberger RS, Gausche-Hill M, et al. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:1051–1066.
-
Nickson C. Thrombolysis for submassive pulmonary embolus. Life in the Fast Lane.
https://litfl.com/thrombolysis-for-submassivepulmonary-embolus/ Updated June 9, 2019. Accessed July 2, 2019.
Results and tips for successful implementation
This case is best implemented with a team comprised of the learner/upper level resident, pharmacist, nurse, paramedic and family member. We recommend inviting your ED nurses, pharmacists or medics to participate. Faculty or other residents can act as family or embedded participants if staff is not available. The case was initially completed by 12 PGY-2 and PGY-3 residents. Verbal debriefing evaluating the simulation efficacy showed that learners became more comfortable initiating tPA without confirmatory imaging after completing this case. After the initial pilot, laboratory data (eg, venous blood gas, glucose) was amended to prevent exploration of diabetic ketoacidosis as potential etiology. Stimuli were modified to improve the image quality after case feedback.
Supplementary Information
INSTRUCTOR MATERIALS
Case Title: Pulseless Electrical Activity Cardiac Arrest
Case Description & Diagnosis (short synopsis): Patient is a 40-year-old female brought in by EMS for a suspected syncopal episode after being found unconscious. She was awake and alert at time of EMS arrival but grew increasingly agitated. Paramedics have grown frustrated with her agitation, and her agitation continues upon arrival. She will complain of pain but will not localize and grows progressively distressed. The patient is unable to provide further detailed history, though her family confirms she began birth control in the last few months. She is negative for any other PE risk factors. While in the emergency department she grows increasingly tachypneic, tachycardic, and hypoxic, eventually requiring intubation. Following intubation her blood pressure and pulse are lost and she has a PEA arrest. Participants will need to consider possible etiologies for PEA arrest and implement a treatment strategy. If Hs & Ts are not fully discussed, learners will be verbally prompted by an embedded participant. Participants should establish the diagnosis of massive PE. Ultrasound (US) confirms dilated right ventricle, and participants should discuss the risk and benefits of tPA administration. Embedded participant will prompt the tPA discussion if necessary as well. Participants should then administer tPA, after which they will obtain return of spontaneous circulation (ROSC). Participants may then order computed tomography (CT), which reveals massive PE with bilateral segmental emboli. If participants fail to follow ACLS guidelines, establish the diagnosis of PE, or fail to administer tPA, the patient will proceed to asystole and death.
Equipment or Props Needed:
High fidelity simulator
Infusion pump
IV pole
Cardiac monitor/defibrillator
Crash cart & medications
Intubation equipment
tPA
Confederates needed:
Nurse
Paramedic (control room)
Pharmacist (control room)
Family member (control room)
Stimulus Inventory:
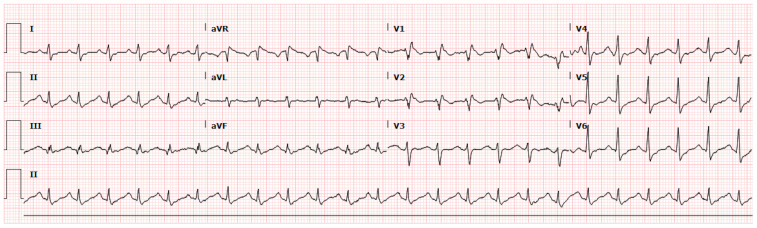
| #1 | Electrocardiogram (ECG) |
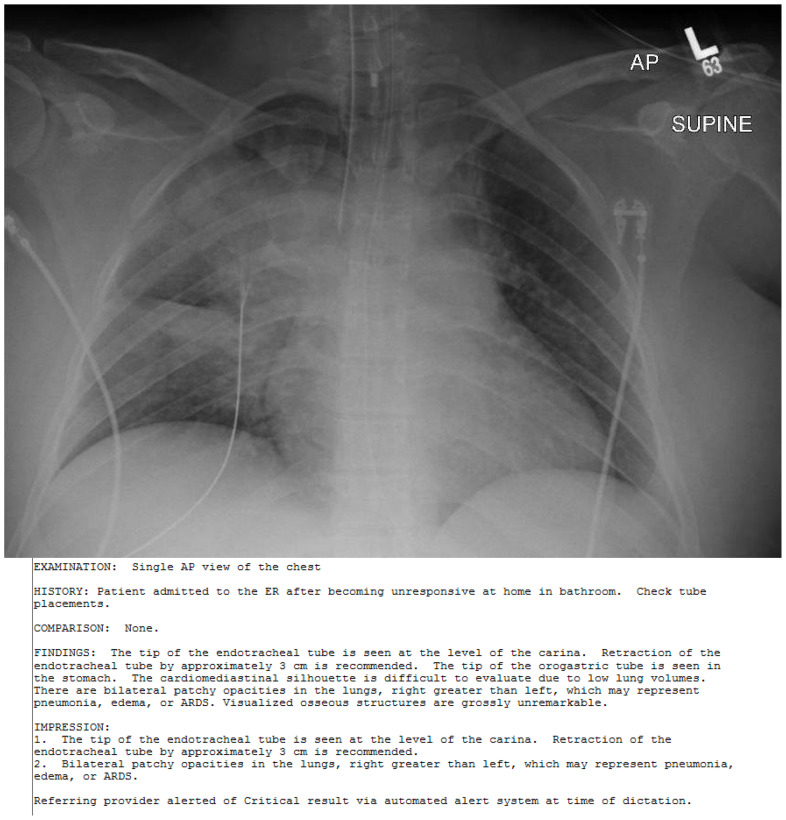
| #2 | Chest Radiograph (CXR) |
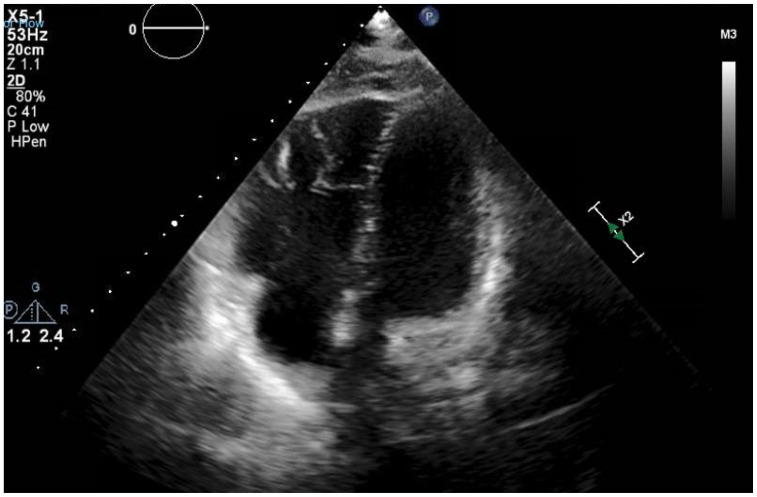
| #3 | Ultrasound/Echocardiogram |
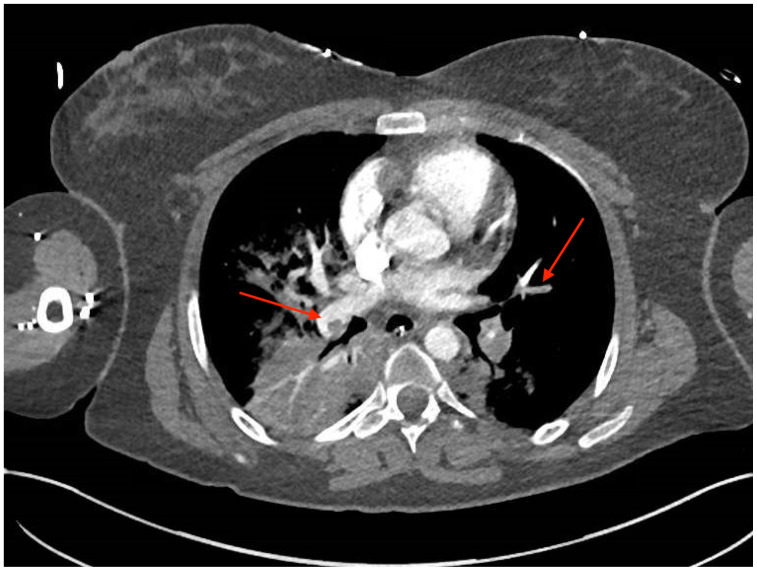
| #4 | Computed Tomography (CT) |
| #5 | Basic Metabolic Profile |
| #6 | Lactic Acid |
| #7 | Venous Blood Gas |
Background and brief information: The scenario occurs in the emergency department at a tertiary care center. The patient is a 40-year-old female brought in by EMS for a suspected syncopal episode. The patient was found unconscious on bathroom floor at work by coworker. She was awake and alert at time of EMS arrival but grew increasingly agitated. Paramedics have grown frustrated with her agitation and refusal to cooperate with their assessment, and this continues on their arrival. She will complain of pain but will not localize and grows progressively distressed in the emergency department. The patient is unable to provide further detailed history, though her family will confirm that she began birth control in the last few months. She is negative for any other PE risk factors. While in the emergency department she grows increasingly tachypneic, tachycardic, and hypoxic, eventually requiring intubation. Following intubation her blood pressure and pulse are lost and she has a PEA arrest. Participants will need to consider possible etiologies for PEA arrest and implement a treatment strategy. If Hs & Ts are not fully discussed, learners will be verbally prompted by an embedded participant.
Initial presentation: Patient is brought in by EMS, who appear frustrated with the patient’s lack of cooperation. She is alert, but in severe distress. She is oriented to self but otherwise minimally able to cooperate with history and exam. She is tachypneic and complains of pain and discomfort but cannot localize cause of her distress. She is very agitated, attempting to remove her gown and oxygen mask.
How the scenario unfolds: This patient has a massive PE. Paramedics will be present at the beginning of the case and will give her presenting history in a calm, dismissive tone. The participants should recognize that the patient is sicker than this report suggests and establish IV access, place the patient on the monitor, and apply oxygen. Laboratory and bedside imaging (CXR/US) may be requested at this time, but participants will be told the patient is too unstable for CT. Other than the agitation, tachycardia, and respiratory distress, the exam is largely unremarkable. The patient quickly grows increasingly distressed, tachypneic and tachycardic and eventually hypoxic. If the participants do not elect to intubate early, the patient will become progressively hypoxic until this decision is reached (if they attempt to place BiPAP, they will be told that the patient tears it off). Following intubation, the patient has a rapid decline in blood pressure, eventually resulting in loss of pulses and a PEA arrest. The participants should then verbalize Hs and Ts or another approach to determining reversible causes of PEA arrest. The patient will remain in PEA arrest as long as the participants follow ACLS. The participants should identify a massive PE as the most likely cause of the arrest and administer tPA (100 mg IV over two hours). The patient will then have ROSC. Bedside US should be available and if asked for will show right ventricular dilation. Following ROSC and stabilization, if the participants request a CT this will show PE with bilateral segmental emboli. The learners should then discuss with the ICU for admission.
Critical actions:
Establish IV access, place the patient on the monitor, and apply oxygen
Recognize critically ill patient
Intubate
Recognize PEA arrest and perform ACLS
Discuss reversible causes of PEA
Establish diagnosis of PE
Administer tPA
Admit to ICU
Case Title: Pulseless Electrical Activity Cardiac Arrest
Chief Complaint: Arrives via EMS. Found in bathroom pale after possible syncope vs. seizure.
| Vitals: | Heart Rate (HR) 137 | Blood Pressure (BP) 110/68 | Respiratory Rate (RR) 23 |
| Temperature (T) 36.9°C | Oxygen Saturation (O2Sat) 76% on room air (RA) | ||
General Appearance: 40-year-old female who appears agitated, mottled and dyspneic.
Primary Survey:
Airway: moaning and making incomprehensible noises but not able to state her name when asked
Breathing: rather tachypneic, increased work of breathing
Circulation: pale, cool extremities; no palpable distal pulses
History:
History of present illness: 40-year-old female presents in acute respiratory distress. Per EMS she was found on the bathroom floor by a family member after a loss of consciousness. Initially, they were called for a possible seizure, but on arrival, the patient was agitated and combative. She reports pain and severe trouble breathing but is unable to localize her pain. Her family member arrives and provides history that the patient is on birth control.
Past medical history: Attention deficit disorder
Past surgical history: none
Patient’s medications: oral contraceptive pills, amphetamine 20mg
Allergies: No known allergies (NKDA)
Social history: negative for tobacco or recreational drug usage. Occasional alcohol consumption
Family history: unremarkable
Secondary Survey/Physical Examination:
General appearance: patient appears tachypneic and in significant respiratory distress
-
HEENT:
○ Head: normocephalic, atraumatic
○ Eyes: Pupils equal and reactive bilaterally
○ Ears: Within normal limits (WNL)
○ Nose: WNL
○ Throat: WNL
Neck: WNL
Heart: tachycardic, no murmurs/rubs/gallops
Lungs: diminished but present lung sounds bilaterally; no rales. Severe respiratory distress noted.
Abdominal/GI: soft, mild diffuse tenderness to palpation; no guarding/rebound
Genitourinary: N/A
Rectal: N/A
Extremities: WNL
Back: WNL
Neuro: alert to self only, otherwise uncooperative
Skin: pale/mottled
Lymph: WNL
Psych: agitated, barely conscious
Results:
Electrocardiogram (ECG)
(author’s own image)
Chest Radiograph (CXR)
(author’s own image)
If chest x-ray is ordered early in the case, learners will be informed it is on the way. CXR can be taken following intubation, arrest, and tPA and is shown below.
Ultrasound/Echocardiogram
(author’s own image)
Computed Tomography (CTA)
(author’s own image)
Following arrest, tPA, resuscitation, and ROSC, a CTA may be requested, with image below:
Impression:
Extensive pulmonary embolism as described with right ventricular strain
Large areas of consolidation in the right lung and to a lesser degree in the left lower lobe indicating pneumonia
Periportal edema in the liver and mild ascites
Fluid surrounding the pancreas suspicious for acute pancreatitis
A 3 cm gastric mass in the distal stomach suspicious for a neoplasm
| Basic metabolic panel (BMP) | |
| Sodium | 140 mEq/L |
| Chloride | 101 mEq/L |
| Potassium | 3.6 mEq/L |
| Bicarbonate (HCO3) | 18 mEq/L |
| Blood Urea Nitrogen (BUN) | 13 mg/dL |
| Creatine (Cr) | 1.1 mg/dL |
| Glucose | 160 mg/dL |
| Ionized Calcium | 4.4 mg/dL |
| Lactic Acid | 4.1 mEq/L |
| Venous Blood Gas (VBG) | |
| pH | 7.1 |
| PaCO2 | 57 mmHg |
| PaO2 | 48 mmHg |
| Bicarbonate (HCO3) | 16.9 mEq/L |
| O2 saturation, arterial | 79% |
If further labs are requested, the learners should be informed that lab is running them.
OPERATOR MATERIALS
SIMULATION EVENTS TABLE:
| Minute (state) | Participant action/trigger | Patient status (simulator response) & operator prompts | Monitor display(vital signs) |
|---|---|---|---|
|
| |||
| 0:00 (Baseline) | Participants enter the room. | Patient is lying on stretcher, agitated, tachypneic. Paramedics are at bedside to give report. Should be given in a casual/dismissive tone. | Not on monitor |
|
| |||
| 01:00 | Assess ABCs | A: Patient is alert, oriented to self, protecting her airway, speaking and moaning in pain. | T 36.9°C HR 137 BP 110/68 RR 23 O2 76% room air |
| Place patient on monitor | B: Tachypneic, breathing in high 20s. In severe respiratory distress but with clear lung sounds. | ||
| Establish IV access | C: She is tachycardic, pale, mottled, but with adequate initial blood pressure. | ||
| Place patient on supplemental oxygen | When placed on supplemental O2 nonrebreather (NRB) patient is adamant it be removed, states “I can’t breathe.” | ||
| Attempt further history from EMS and patient, perform exam | She is able to say her name, but otherwise does not answer questions. Only states “it hurts” and “I can’t breathe.” Does not localize pain when asked. | ||
|
| |||
| 03:00 (Initial Resuscitation) | Begin IV fluids | Tachycardia and blood pressure will stabilize with IVF; however, she will not improve. | T 36.6°C HR 150 BP 96/50 RR 32 O2 88% NRB |
| Oxygen supplementation | Patient continues to require increasing amount of supplemental oxygen. | ||
| Obtain ECG | ECG provided. | ||
| Obtain labs | Participants will be provided with labs if requested and should be prompted for them when IV is started if they do not request labs. Despite adequate resuscitation the patient’s condition continues to decline. Oxygenation worsens despite NRB and patient will not tolerate BiPAP. Tachycardia and hypoxia should continue to progress until decision is made to intubate. |
||
| Decision to intubate | Proceed to intubation state. | ||
|
| |||
| 05:00(Delay in treatment) | Despite IV fluids | Tachycardia increases and blood pressure decreases. | T 36.6°C HR 162 BP 84/41 RR 35 O2 75% nasal cannula |
| Despite Oxygen supplementation | Hypoxia worsens. | ||
| No Decision to Intubate | Patient arrests—proceed to arrest state. | ||
|
| |||
| 05:00 Intubation | Prepare for intubation:
|
Patient paralyzed and sedated. | T 36.6°C HR 162 BP 102/51 RR 12 O2 92% ventilator |
| Patient should be reevaluated following intubation | Following intubation, patient’s HR decreases steadily into 70s. BP should be rechecked and is no longer obtainable. Proceed to arrest state. |
T 36.6°C HR 74 BP– RR 12 O2 80% ventilator |
|
|
| |||
| 10:00PEA Arrest | Begin CPR and progress through ACLS for treatment of PEA Arrest | Patient remains in PEA arrest with unchanged condition. | T 36.6°C HR PEA bagged BP– RR 12 O2 60% ventilator |
| Discussion of Reversible causes (Hs and Ts) | Participants may need to be prompted for this discussion while progressing through ACLS. Disparity between patient’s presentation of tachypnea and respiratory acidosis/hypoxia should be discussed. Patient’s family member may be interviewed and will confirm that she is on birth control. | ||
| Administer tPA | Proceed to ROSC. | ||
|
| |||
| 15:00 No tPA Administered | Continue CPR, ACLs | If tPA is not given for presumed PE, patient will progress to asystole and family member will ask for team to “stop everything.” | |
| Administer tPA | Proceed to ROSC. | ||
|
| |||
| 15:00 ROSC | Request for pressor infusion | Blood pressure stabilizes, HR increases. | T 36.6°C HR 96 BP 112/60 RR 12 O2 90% ventilator |
| Obtain bedside US and CXR if not done so already | Provide CXR and US images as requested. | ||
| Call for CTA | Provide CT images and reports. | ||
| Initiate Heparin Infusion | |||
|
| |||
| (Case Completion) | Call ICU for admission | ICU accepts the patient. | Case Ends |
Diagnosis
Massive PE; PEA arrest with ROSC
Disposition
Admission to the medical ICU.
DEBRIEFING AND EVALUATION PEARLS
PEA Arrest
Pearls:
Reversible Causes:
Hs and Ts
- Hypovolemia, hypoxia, hydrogen ions (acidosis), hypokalemia, hyperkalemia, Hypoglycemia, Hypothermia
- Toxins, tamponade (cardiac), tension pneumothorax, thromboembolism (pulmonary or cardiac)
Alternate Approach
Fix with airway
- Hypoxia
- Acidosis (if respiratory)
Fix with a needle
- Tension pneumothorax
- Cardiac tamponade
Fix with an IV
- Hypovolemia – fluid, blood
- Hyperkalemia – calcium, bicarbonate, insulin
- Hypokalemia – potassium/magnesium
- Acidosis (if metabolic) – bicarb
- Hypoglycemia - dextrose
- Massive PE – tPA
- Toxins – antidote
Fix with Dialysis
- Hyperkalemia
- Acidosis
- Toxins
Fix with warming
- Hypothermia
Fix with tPA or heart catheterization
- Acute myocardial infarction
ECG findings of PE
- S1Q3T3 associated with PE (S1Q3 seen on case ECG)
- Most commonly sinus tachycardia
- Signs of Right heart strain including Right bundle branch block
Ultrasound Findings
- Right ventricular dilation
- Hyperdynamic cardiac function
- McConnell’s sign (relative hyperkinesis of apex of right ventricle)
Other debriefing points:
- Discuss the index of suspicion created on entering the room. Report by EMS and their causal air in contrast to patient’s appearance. How quickly was safety net established and did initial vitals change participant’s perception of the case?
- Discuss the treatment and evaluation of PEA arrest, including progression through analyzing reversible causes and what factors change index of suspicion for each one.
- Discuss the dosing of tPA in massive PE.
- Why did this patient arrest after intubation? (blunting catecholamine response)
- If bedside US was not obtained, discuss how else this patient’s likelihood of PE could have been assessed.
- What are this patient’s risk factors for PE vs other causes of PEA? What about her presentation suggested PE?
Further reading
- 1.DePalo VA, Kharnaf AE.Panchbhavi VK, editor. Venous Thromboembolism (VTE) Treatment & Management. Medscape. [Accessed July 2, 2019]. https://emedicine.medscape.com/article/1267714-treatment#d10. Published June 12, 2019.
- 2.Kline JA. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier Inc; 2018. [Accessed October 30, 2019]. Pulmonary Embolism and Deep Vein Thrombosis. https://www-clinicalkeycom.siumed.idm.oclc.org/#!/content/book/3-s2.0-B9780323354790000787?indexOverride=GLOBAL . [Google Scholar]
- 3.Nickson C.Thrombolysis for submassive pulmonary embolus. Life in the FastLane. [Accessed July 2, 2019]. https://litfl.com/thrombolysis-for-submassive-pulmonary-embolus/. Published June 9, 2019.
- 4.Shah SN, Kharnaf AE.Dizon JM, editor. Pulseless Electrical Activity. Medscape. [Accessed October 30, 2019]. https://emedicine.medscape.com/article/161080-overview. Published March 27, 2018.
- 5.Tapson VF, Weinberg AS. Thrombolytic (fibrinolytic) therapy in acute pulmonary embolism and lower extremity deep vein thrombosis. In: Mandel J, Finlay G, editors. UpToDate. Waltham, MA: 2019. https://www.uptodate.com/contents/search?search=thrombolytic-fibrinolytic-therapy-in-acute-pulmonary-embolism-and-lower-extremity-deep-veinthrombosis. Updated May 3, 2019. [Google Scholar]
- 6.Tapson VF, Weinberg AS. Treatment, prognosis, and follow-up of acute pulmonary embolism in adults. In: Mandel J, Hockberger RS, Finlay G, editors. UpToDate. Waltham, MA: 2019. https://www.uptodate.com/contents/treatment-prognosis-and-follow-up-of-acute-pulmonary-embolism-in-adults. Updated Dec 12, 2019. [Google Scholar]
SIMULATION ASSESSMENT
PEA Arrest
Learner: _________________________________________
Assessment Timeline
This timeline is to help observers assess their learners. It allows observer to make notes on when learners performed various tasks, which can help guide debriefing discussion.
Critical Actions:
|
0:00 |
Critical Actions:
□ Established IV access, place patient on monitor, apply oxygen
□ Recognized critically ill patient and began resuscitation early
□ Established definitive airway
□ Performed ACLS and recognized PEA arrest
□ Discussed reversible causes of PEA
□ Establish diagnosis of PE
□ Administer tPA
□ Patient admitted to ICU
Summative and formative comments:
Milestones assessment:
| Milestone | Did not achieve level 1 | Level 1 | Level 2 | Level 3 | |
|---|---|---|---|---|---|
| 1 | Emergency Stabilization (PC1) | □ Did not achieve Level 1 |
□ Recognizes abnormal vital signs |
□ Recognizes an unstable patient, requiring intervention Performs primary assessment Discerns data to formulate a diagnostic impression/plan |
□ Manages and prioritizes critical actions in a critically ill patient Reassesses after implementing a stabilizing intervention |
| 2 | Performance of focused history and physical (PC2) | □ Did not achieve Level 1 |
□ Performs a reliable, comprehensive history and physical exam |
□ Performs and communicates a focused history and physical exam based on chief complaint and urgent issues |
□ Prioritizes essential components of history and physical exam given dynamic circumstances |
| 3 | Diagnostic studies (PC3) | □ Did not achieve Level 1 |
□ Determines the necessity of diagnostic studies |
□ Orders appropriate diagnostic studies. Performs appropriate bedside diagnostic studies/procedures |
□ Prioritizes essential testing Interprets results of diagnostic studies Reviews risks, benefits, contraindications, and alternatives to a diagnostic study or procedure |
| 4 | Diagnosis (PC4) | □ Did not achieve Level 1 |
□ Considers a list of potential diagnoses |
□ Considers an appropriate list of potential diagnosis May or may not make correct diagnosis |
□ Makes the appropriate diagnosis Considers other potential diagnoses, avoiding premature closure |
| 5 | Pharmacotherapy (PC5) | □ Did not achieve Level 1 |
□ Asks patient for drug allergies |
□ Selects an medication for therapeutic intervention, consider potential adverse effects |
□ Selects the most appropriate medication and understands mechanism of action, effect, and potential side effects Considers and recognizes drug-drug interactions |
| 6 | Observation and reassessment (PC6) | □ Did not achieve Level 1 |
□ Reevaluates patient at least one time during case |
□ Reevaluates patient after most therapeutic interventions |
□ Consistently evaluates the effectiveness of therapies at appropriate intervals |
| 7 | Disposition (PC7) | □ Did not achieve Level 1 |
□ Appropriately selects whether to admit or discharge the patient |
□ Appropriately selects whether to admit or discharge Involves the expertise of some of the appropriate specialists |
□ Educates the patient appropriately about their disposition Assigns patient to an appropriate level of care (ICU/Tele/Floor) Involves expertise of all appropriate specialists |
| 9 | General Approach to Procedures (PC9) | □ Did not achieve Level 1 |
□ Identifies pertinent anatomy and physiology for a procedure Uses appropriate Universal Precautions |
□ Obtains informed consent Knows indications, contraindications, anatomic landmarks, equipment, anesthetic and procedural technique, and potential complications for common ED procedures |
□ Determines a back-up strategy if initial attempts are unsuccessful Correctly interprets results of diagnostic procedure |
| 20 | Professional Values (PROF1) | □ Did not achieve Level 1 |
□ Demonstrates caring, honest behavior |
□ Exhibits compassion, respect, sensitivity and responsiveness |
□ Develops alternative care plans when patients’ personal beliefs and decisions preclude standard care |
| 22 | Patient centered communication (ICS1) | □ Did not achieve level 1 |
□ Establishes rapport and demonstrates empathy to patient (and family) Listens effectively |
□ Elicits patient’s reason for seeking health care |
□ Manages patient expectations in a manner that minimizes potential for stress, conflict, and misunderstanding. Effectively communicates with vulnerable populations, (at risk patients and families) |
| 23 | Team management (ICS2) | □ Did not achieve level 1 |
□ Recognizes other members of the patient care team during case (nurse, techs) |
□ Communicates pertinent information to other healthcare colleagues |
□ Communicates a clear, succinct, and appropriate handoff with specialists and other colleagues Communicates effectively with ancillary staff |
References/suggestions for further reading
- 1.Podrid PJ. Pathophysiology and etiology of sudden cardiac arrest. In: Olshansky B, Manaker S, Downey BC, editors. UpToDate. Waltham, MA: UpToDate Inc; https://www.uptodate.com/contents/pathophysiologyand-etiology-of-sudden-cardiac-arrest. Updated Apr 18, 2018. [Google Scholar]
- 2.Kline JA. Venous Thromboembolism. In: Tintinalli JE, Stapczynski JS, Ma OJ, et al., editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, NY: McGraw-Hill; 2016. pp. 388–398. [Google Scholar]
- 3. Kasper W, Konstantinides S, Geibel A, et al. Management strategies and determinants of outcome in acute major pulmonary embolism: results of a multicenter registry. J Am Coll Cardiol. 1997;30(5):1165–1171. doi: 10.1016/s0735-1097(97)00319-7. [DOI] [PubMed] [Google Scholar]
- 4. Sharifi M, Berger J, Beeston P, Bay C, Vajo Z, Javadpoor S. Pulseless electrical activity in pulmonary embolism treated with thrombolysis (from the “PEAPETT” study) Am J Emerg Med. 2016;34(10):1963–1967. doi: 10.1016/j.ajem.2016.06.094. [DOI] [PubMed] [Google Scholar]
- 5. Wan S, Quinlan D, Agnelli G, Eikelboom J. Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials. Circulation. 2004;13(11):38–39. doi: 10.1161/01.CIR.0000137826.09715.9C. [DOI] [PubMed] [Google Scholar]
- 6.DePalo VA, Kharnaf AE.Panchbhavi VK, editor. Venous Thromboembolism (VTE) Treatment & Management. Medscape. [Accessed July 2, 2019]. https://emedicine.medscape.com/article/1267714-treatment#d10 Published June 12, 2019.
- 7.Kline JA. Pulmonary embolism and deep vein thrombosis. In: Walls RM, Hockberger RS, Gausche-Hill M, et al., editors. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018. pp. 1051–1065. [Google Scholar]
- 8.Nickson C.Thrombolysis for submassive pulmonary embolus. Life in the FastLane. [Accessed July 2, 2019]. https://litfl.com/thrombolysis-for-submassive-pulmonary-embolus/. Published June 9, 2019.
- 9.Shah SN, Kharnaf AE.Dizon JM, editor. Pulseless Electrical Activity. Medscape. [Accessed October 30, 2019]. https://emedicine.medscape.com/article/161080-overview. Published March 27, 2018.
- 10.Tapson VF, Weinberg AS. Thrombolytic (fibrinolytic) therapy in acute pulmonary embolism and lower extremity deep vein thrombosis. In: Mandel J, Finlay G, editors. UpToDate. Waltham, MA: UpToDate Inc; https://www.uptodate.com/contents/search?search=thrombolytic-fibrinolytic-therapy-in-acute-pulmonaryembolism-and-lower-extremity-deep-veinthrombosis. Updated May 3, 2019. [Google Scholar]
- 11.Tapson VF, Weinberg AS. Treatment, prognosis, and follow-up of acute pulmonary embolism in adults. In: Mandel J, Hockberger RS, Finlay G, editors. UpToDate. Waltham, MA: UpToDate Inc; https://www.uptodate.com/contents/treatmentprognosis-and-follow-up-of-acute-pulmonary-embolism-inadults. Updated Dec 12, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.