Abstract
Audience
This simulation was developed to educate emergency medicine residents on the diagnosis and management of high-altitude pulmonary edema (HAPE). This case is also appropriate for senior medical students and advanced practice providers. The principles of crisis resource management, teamwork, and communication are incorporated into the case.
Introduction
High altitude pulmonary edema may present similarly to pneumonia with nonspecific symptoms, including decreased exercise tolerance, cough, dyspnea with exertion, and fever. Symptoms more specific to HAPE include dyspnea at rest, tachypnea, history of rapid ascent to high altitude, a lowlander patient exposed to high-altitude, or a highlander patient on re-entrance to high altitude after lowland stay. Laboratory and imaging workup may include infiltrates on chest x-ray and leukocytosis.1,2 Of the various forms of altitude sickness, HAPE has the highest fatality rate, estimated at 50% in travellers to the Himalayas who are unable to descend.1 Providers should inquire as to the current elevation of their facility, the patient’s recent altitude gain, and the rate of ascent. Treatment priorities include oxygen and immediate descent, as well as supplemental treatment with nifedipine and phosphodiesterase (PDE) inhibitors such as sildenafil or tadalafil.
Educational Objectives
At the conclusion of the simulation session, learners will be able to:
obtain a thorough history relevant to altitude illnesses
develop a differential for dyspnea in a patient with environmental exposures
discuss prophylaxis and management of HAPE
discuss appropriate disposition of the patient including descent and subsequent appropriate level of care
Educational Methods
This session was conducted using high-fidelity simulation followed by a debriefing session and lecture on the diagnosis and management of HAPE. Debriefing methods may be left to the discretion of participants, but the authors have utilized advocacy-inquiry techniques. This technique includes an observation statement, a statement describing the framework of the observer, and an invitation to review further to explore the participants’ frames. An example of this advocacy-inquiry is as follows: “I heard Sam suggest to the team that acetazolamide be given, but then I didn’t hear any follow-up discussion. Acetazolamide is often utilized for acute mountain illness prophylaxis or treatment. I wasn’t sure if the team did not hear his suggestion or disagreed with the treatment plan. Tell me more.” This scenario was designed as a simulation, but it could be adapted as an oral boards case.
Research Methods
Our residents were provided with a survey at the completion of the simulation and debriefing to rate different aspects of the simulation, as well as to provide qualitative feedback.
Results
Participants expressed positive feedback, with comments focused on appreciating the review of the presentation, diagnosis, and treatment of altitude illness. The emergency medicine residents surveyed currently practice in a low altitude setting and were appreciative to simulate a scenario to which they might otherwise not get exposure during their residency. Our simulation center’s feedback form is based on the Center of Medical Simulation’s Debriefing Assessment for Simulation in Healthcare (DASH) Student Version Short Form. This session received all 6 or 7 scores (consistently effective/very good or extremely effective/outstanding) other than a 5 for setting the stage, a 4 for maintaining an engaging context for learning, and two 5s for structured debriefing.
Discussion
This was an effective method to review high altitude illness with learners that may otherwise get limited exposure to such clinical cases during residency. Learners had a broad range of differential diagnoses and demonstrated variable levels of knowledge related to the diagnosis and treatment of high-altitude illness. We used visual stimuli and a reminder from our nurse to reinforce for the learners that the case was taking place at a critical access emergency room at 11,000 feet of elevation.
Topics
Medical simulation, high altitude pulmonary edema, high altitude cerebral edema, altitude sickness, emergency medicine, wilderness medicine.
USER GUIDE
| List of Resources: | |
|---|---|
| Abstract | 78 |
| User Guide | 80 |
| Instructor Materials | 82 |
| Operator Materials | 92 |
| Debriefing and Evaluation Pearls | 96 |
| Simulation Assessment | 99 |
Learner Audience:
Medical students, interns, junior residents, senior residents
Time Required for Implementation:
Instructor Preparation: 30 minutes
Time for case: 20 minutes
Time for debriefing: 40 minutes
Recommended Number of Learners per Instructor:
4
Topics:
Medical simulation, high altitude pulmonary edema, high altitude cerebral edema, altitude sickness, emergency medicine, wilderness medicine.
Objectives:
By the end of this simulation session, the learner will be able to:
Obtain a thorough history, including current altitude, rate of ascent, peak altitude, patient’s baseline altitude, and assessment for other causes of dyspnea and altered mental status
Develop a differential for dyspnea in a patient with significant environmental exposures
Discuss prophylaxis and management of HAPE
Discuss appropriate disposition of the patient in both the field and in the high-altitude ED or clinic, including descent and subsequent appropriate level of care
Linked objectives and methods
High altitude pulmonary edema is an uncommon ED presentation, and many of the symptoms are consistent with much more common diagnoses such as cardiogenic pulmonary edema or pneumonia. This scenario enforces the importance of obtaining a thorough history including ascent profile, baseline altitude, and maintaining a high clinical suspicion for altitude illness in the appropriate setting (objective 1). Learners will be required to develop a differential for dyspnea in a patient with environmental exposures (objective 2). Learners will need to identify the appropriate management of HAPE, as well as prophylaxis (objective 3), including appropriate disposition, including descent to lower altitude and inpatient level of care (objective 4). This simulation scenario allows learners to reinforce their HAPE management skills in a psychologically safe learning environment, and then receive formative feedback on their performance.
Recommended pre-reading for instructor
We recommend that instructors review the Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update.7 Other suggested readings include materials listed below under the “References/suggestions for further reading” section.
Results and tips for successful implementation
This simulation was written to be performed as a high-fidelity simulation scenario, but also may be used as a mock oral board case.
The case was written for emergency medicine residents and may be presented in an outdoor setting or simulation lab. We conducted this simulation with emergency medicine residents during the 2019–2020 academic year. Despite having a sign on the door that informed participants that they were moonlighting at an ED in the Rocky Mountains for this scenario, some groups needed further reinforcement to remind them that they are not in their usual ED location. Once participants realized they were at a high-altitude location, their differentials then immediately expanded to include altitude-related illnesses. For this reason, we did not have nursing consistently remind them that they were in a high-altitude critical access ED in order to minimize diagnostic anchoring.
During debriefing, participants expressed overall positive feedback including reviewing the spectrum of altitude related illnesses with approaches for both prophylaxis and treatment. The emergency medicine residents currently practice in a lowaltitude setting and appreciated the simulation of a scenario to which they might not otherwise be exposed in their clinical residency training.
Our simulation center’s feedback form is based on the Center of Medical Simulation’s Debriefing Assessment for Simulation in Healthcare (DASH) Student Version Short Form with the inclusion of required qualitative feedback if an element was scored less than a 6 or 7. This session received all 6 or 7 scores (consistently effective/very good or extremely effective/outstanding) other than a 5 for setting the stage, a 4 for maintaining an engaging context for learning, and two 5s for structured debriefing. Our form also includes an area for general feedback about the case at the end. Qualitative comments for the “setting the stage” category included, “Would have preferred more info from nurse about physically where we are and what type of hospital and what information we had?” reflecting the earlier sentiment that many residents needed further prompting that they were at a high-altitude ED instead of their typical practice location. The qualitative comment for the 4 score for the maintaining an engaging context for learning was, “When we were struggling in simulation it would have been nice to have a nudge or a clue rather than just more silence.” Our typical practice is to allow the participants to work through their differentials and give them opportunity to revisit their decision-making processes without prompting unless they are unable to move forward. All other scores in this area were 6s and 7s. Qualitative comments for debriefing were for both 5 scores and included, “Went well overall, I just didn’t know a whole lot about the topic,” and “great case,” so the authors wonder if one of those 5 scores was more reflective of the learner’s baseline knowledge about HAPE, rather than how the debriefing was structured or conducted.
Supplementary Information
INSTRUCTOR MATERIALS
Case Title: High Altitude Pulmonary Edema
Case Description & Diagnosis (short synopsis): Patient is a 27-year-old healthy female hiker who presents from the wilderness with dyspnea. Per EMS, the patient was backpacking in the Rocky Mountains with friends. Throughout the day, she was having increasing trouble keeping up and appeared to be mildly short of breath. The shortness of breath worsened and did not resolve with rest, despite more frequent breaks to rest and a slower pace. When she did not improve while resting in camp, her friends hiked down to town to call for rescue. She was evacuated in a litter by search and rescue. She is currently too dyspneic to speak. Participants should obtain an oxygen saturation, temperature, electrocardiogram (ECG), arterial blood gas (ABG), chest x-ray (CXR), and blood work. Diagnostics will reveal low oxygen saturation, low partial pressure of oxygen (PaO2), mild leukocytosis, and CXR findings consistent with pulmonary edema. The patient should be treated with oxygen and nifedipine with additional consideration of sildenafil or tadalafil treatment. Given the patient’s leukocytosis, infiltrates on CXR, and fever, it would be reasonable to concurrently treat for pneumonia with antibiotics. The patient should be transferred by ground to a hospital with ICU capabilities at lower elevation.
Equipment or Props Needed:
High fidelity simulation mannequin
Flannel shirt, jeans, and hiking boots to place on the mannequin to signify patient has been hiking
Angiocaths for peripheral intravenous access = 18g, 20g, 22g
Cardiac monitor
Pulse oximetry
IV pole
Normal saline (1L ×2)
Nasal cannula oxygen
Non-rebreather mask
Continuous positive airway pressure (CPAP) or Bilevel positive airway pressure (BiPAP) mask Simulated medications with labeling: nifedepine, acetazolamide, sildenafil, dexamethasone
Confederates needed:
primary nurse
Stimulus Inventory:
| #1 | Complete blood count (CBC) |
| #2 | Basic metabolic panel (BMP) |
| #3 | Arterial blood gas (ABG) |
| #4 | Troponin |
| #5 | BNP |
| #6 | D-dimer |
| #7 | Urinalysis |
| #8 | hCG qualitative |
| #9 | Electrocardiogram (ECG) |
| #10 | Chest Radiograph (CXR) |
| #11 | Computed tomography pulmonary embolism (CT PE) study |
Background and brief information: Search and rescue were called by the patient’s friend for shortness of breath. They brought the patient to the ED after a ground evacuation from a backpacking camp 8 miles from the nearest paved road.
Initial presentation: The patient is a 27-year-old female with no past medical history who presents from the wilderness via EMS with severe dyspnea.
She reports shortness of breath and chest tightness. She is occasionally coughing. Her cough is productive of pink frothy sputum.
She is too dyspneic to converse in full sentences. She denies headache, ataxia or vomiting. She endorses nausea. Last meal was 12 hours ago. Her friends tried to feed her in camp, but she was too nauseous and dyspneic to eat. She hiked 8 miles today and drank 2 liters of water.
If asked, she lives in Ohio (sea level) and flew to Colorado 2 days ago for a backpacking trip with friends. She hiked from 8,000 feet of elevation to 12,000 feet of elevation today. She noticed some initial exercise intolerance that worsened as she continued to hike.
The nurse may share that the hospital is a critical access hospital at 11,000 ft. It has an emergency room and 25 medical beds. There is not an inpatient critical care unit.
Past medical history: none
Past surgical history: appendectomy at age 12
Medications: combined estrogen/progesterone oral contraceptive pill (OCP)
Allergies: none
Family history: noncontributory.
Weight: 60 kg
Assessment: Lying supine, extremely tachypneic with little ability to converse, appears to be cyanotic and somewhat drowsy, occasionally coughing
How the scenario unfolds: Patient is a 27-year-old healthy female hiker who presents from the wilderness with dyspnea. Per EMS, the patient was backpacking in the Rocky Mountains with friends. Throughout the day, she was having increasing trouble keeping up and appeared to be mildly short of breath. The shortness of breath worsened and did not resolve with rest, despite more frequent breaks to rest and a slower pace. When she did not improve while resting in camp, her friends hiked down into town to call for rescue. She was evacuated in a litter by a search and rescue team. She is currently too dyspneic to converse in full sentences. Participants should obtain an oxygen saturation (O2 sat), temperature, ECG, ABG, chest x-ray, and blood work. Diagnostics will reveal a respiratory alkalosis with low PaO2, hypoxia, an elevated WBC, and pulmonary edema. The patient should be treated with oxygen and nifedipine with consideration for use of sildenafil or tadalafil. Given the patient’s elevated WBC, infiltrates on CXR and fever, it would be reasonable to concurrently treat for pneumonia with antibiotics. Patient’s tachypnea, tachycardia, and hypoxia improve with oxygenation with a modest improvement with the addition of nifedipine. If providers do not apply supplemental oxygen, the patient will become progressively more somnolent and bradycardic until pulseless electrical activity (PEA) arrest. Return of spontaneous circulation (ROSC) will be achieved once patient is appropriately ventilated with a bag-valve mask or intubated. When the transfer center is contacted, they should offer admission to an ICU several minutes away at the same altitude or a hospital that is an hour away by ground and is 3000 feet lower in elevation. If the nearby hospital is chosen, the transfer center will call back in 3 minutes and will state they are currently on diversion. The patient should be evacuated by ground to a hospital with ICU capabilities at lower elevation.
Critical actions:
Place patient on monitor and obtain a full set of vitals, including temperature and pulse oximetry
Apply supplemental oxygen
Obtain IV access
Obtain further history, including current altitude and patient’s rate of ascent
Obtain an ABG, labs, CXR, and ECG
Identify pulmonary edema on CXR
Treat with nifedipine or a PDE-5 inhibitor
Cover for possible pneumonia with antibiotic therapy
Arrange for transport to a hospital at lower elevation with critical care capabilities
Case Title: High Altitude Pulmonary Edema
Chief Complaint: Patient is a 27-year-old female who presents from the wilderness by EMS for severe dyspnea
| Vitals: | Heart Rate (HR) 120 | Blood Pressure (BP) 110/76 | Respiratory Rate (RR) 36 |
| Temperature (T) 100.9°F | Oxygen Saturation (O2Sat) 73% on room air | ||
| Weight (Wt) 60 kg | |||
General Appearance: lying supine in bed, visibly short of breath with labored respirations, cyanotic, having difficulty conversing secondary to dyspnea, drowsy
Primary Survey:
Airway: intact
Breathing: diffuse rales, severely tachypneic, accessory muscle use present, perioral cyanosis
Circulation: tachycardic rate and regular rhythm. 2+ symmetric pulses. Cyanosis present to distal fingers and to toes.
History:
History of present illness: Patient is a 27-year-old female with no previous medical history (PMH) who presents from the wilderness via EMS with severe dyspnea and reported hallucinations without other signs of altered mental status.
She is too dyspneic to converse in full sentences. She denies headache, ataxia or vomiting. She endorses nausea. Last meal was 12 hours ago. Her friends tried to feed her in camp, but she was too nauseous to eat. She hiked 8 miles today and drank 2 L of water.
If asked, she lives in Ohio (sea level) and flew to Colorado 2 days ago for a backpacking trip with friends. She hiked from 8000 ft of elevation to 12,000 ft of elevation today.
The nurse may share that the hospital is a critical access hospital at 11,000 ft. It has an emergency room and 25 floor-level beds.
Past medical history: none
Past surgical history: appendectomy at age 12
Medications: combined estrogen/progesterone OCP
Allergies: none
Social history: social drinker, had 2 beers last night. No other alcohol this week. Denies drug use. Not currently sexually active.
Family history: noncontributory
Secondary Survey/Physical Examination:
General appearance: Lying in bed, severely tachypneic with difficulty speaking, appears cyanotic, drowsy
-
HEENT:
○ Head: within normal limits other than perioral cyanosis
○ Eyes: within normal limits
○ Ears: within normal limits
○ Nose: within normal limits
○ Throat: within normal limits
Neck: within normal limits
Heart: tachycardic, otherwise, within normal limits
Lungs: diffuse rales in all lung fields, very tachypneic at rest, using accessory muscles to breathe
Abdominal/GI: within normal limits
Genitourinary: within normal limits
Rectal: within normal limits
Extremities: Cyanosis present to distal fingers and to toes.
Back: within normal limits
Neuro: Drowsy but awake and oriented ×3. No focal motor or sensory deficits. Coordinated in all extremities, if tested. No clonus. Cranial nerves intact. GCS 15 (E4V5M6).
Skin: within normal limits other than cyanosis as noted above
Lymph: within normal limits
Psych: within normal limits
Results:
| Complete blood count (CBC) | |
| White blood count (WBC) | 16.0 ×1000/mm3 |
| Hemoglobin (Hgb) | 14.5 g/dL |
| Hematocrit (HCT) | 45.0% |
| Platelet (Plt) | 270 ×1000/mm3 |
| Basic metabolic panel (BMP) | |
| Sodium | 135 mEq/L |
| Chloride | 100 mEq/L |
| Potassium | 4.2 mEq/L |
| Bicarbonate (HCO3) | 23 mEq/L |
| Blood Urea Nitrogen (BUN) | 19 mg/dL |
| Creatine (Cr) | 1.0 mg/dL |
| Glucose | 85 mg/dL |
| Calcium | 8.6 mg/dL |
| Arterial blood gas (ABG) | |
| pH | 7.55 |
| pCO2 | 15 mmHg |
| pO2 | 39 mmHg |
| HCO3 | 22 mEq/L |
| O2 saturation | 73% on room air |
| Lactic acid | 1.2 mmol/L |
| Troponin | <0.015 ng/mL |
| NT-pro BNP | 110 pg/mL |
| D-dimer | <0.1 ug/mL |
| Urinalysis (UA) | |
| Leukocyte esterase | negative |
| Nitrites | negative |
| Blood | none |
| Protein | none |
| Ketones | none |
| Glucose | none |
| Color | dark yellow |
| White blood cells (WBC) | 0–5 WBCs/high powered field (HPF) |
| Red blood cells (RBC) | 0–5 RBCs/HPF |
| Squamous epithelial cells | 0–5 cells/HPF |
| Specific gravity | 1.015 |
| hCG qualitative | negative |
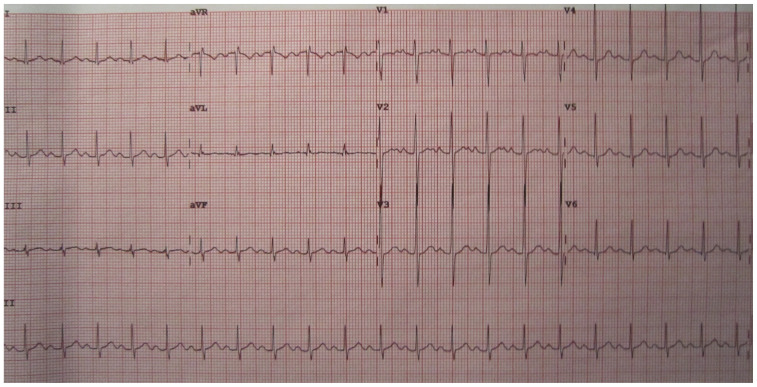
Electrocardiogram (EKG)
Heilman, J. Sinus tachycardia as seen on ECG. In: Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Sinustachy.JPG. Published June 15, 2012. CC BY-SA 3.0.
Chest Radiograph (CXR)
Jones, Jeremy. AP portable CXR of a patient in acute pulmonary edema. In: Wikimedia Commons. https://commons.wikimedia.org/w/index.php?curid=7371914. Published July 23, 2009. CC BY-SA 3.0. ros.
Computed Tomography Pulmonary Embolism Study
Hellerhoff. Pulmonary edema in CT-scan coronal MPR. https://commons.wikimedia.org/wiki/File:18-01-Lungenoedem_CT_coronar.png. In: Wikimedia Commons. Published December 5, 2010. CC BY-SA 3.0. ros.
OPERATOR MATERIALS
SIMULATION EVENTS TABLE:
| Minute (state) | Participant action/trigger | Patient status (simulator response) & operator prompts | Monitor display (vital signs) |
|---|---|---|---|
| 0:00 (Baseline) | Patient moved into bed in the emergency department. | Participants should begin by placing the patient on a monitor, obtaining a history and performing a physical exam. | No vitals should be displayed until requested T 100.9 HR 120 BP 110/76 RR 36 O2 73% RA |
| 04:00 | IV placed, labs drawn. Participant should apply supplemental oxygen, perform a thorough physical exam, obtain ECG, order labs and CXR. | If the team administers oxygen, tachypnea and O2 saturation will improve. If the team does not administer oxygen, patient will become obtunded, further desaturate and will begin to have a drop in respiratory rate. If team intubates successfully on first attempt, hypoxia will improve to 92%. If team has difficulty intubating (more than 2 attempts or a prolonged attempt), go straight to PEA arrest (15:00 vitals). |
On a non-rebreathing mask: T 100.9 F HR 110 BP 110/76 RR 35 O2 86% on 15L O2 On a positive pressure mask: T 100.9 F HR 110 BP 110/76 RR 30 O2 90% on BiPAP or CPAP Intubated: T 100.9F HR 90 RR (set by team) - bagged O2 92% bag valve mask (BVM) Without oxygen: T 100.9F HR 130 BP 90/60 RR 26 O2 65% on RA |
| 10:00 | Administer nifedipine and oxygen. | If team administers nifedipine to the non-intubated patient, RR decreases to 26 and oxygenation improves to 92%. It not, vitals remain unchanged from previous step. If team administers nifedipine to the non-intubated patient, oxygenation improves to 94%. It not, vitals remain unchanged from previous step. If oxygen is still not administered regardless if nifedipine is given, patient’s respiratory rate will slow as the patient decompensates (from 8:00–10:00). After two more minutes (10:00), the patient will go into PEA cardiac arrest secondary to respiratory arrest for two rounds of appropriately performed ACLS until ROSC is achieved. |
Nifedipine given with oxygen: T 100.9 F HR 100 BP 110/76 RR 24 O2 92% on 15L O2 or positive pressure oxygen Intubated with nifedipine: T 100.9F HR 90 RR (set by team) - bagged O2 94% BVM Without oxygen: T 100.9F HR 70 BP 90/60 RR 16 O2 60% on RA |
| 15:00 (A) PEA arrest/ROSC | If patient arrests, ROSC will be achieved with 2 rounds of appropriate ACLS, as long as appropriate bag-valve mask respirations or airway secured. OSH hospital at lower elevation should be contacted for direct admission to ICU and transport arranged. | Once ICU is contacted, they will ask why the patient arrested. They may provide further treatment guidance as felt appropriate per facilitator. When the transfer center is contacted, they should offer admission to an ICU several minutes away at the same altitude or a hospital that is an hour away by ground and is 3000 feet lower in elevation. If the nearby hospital is chosen, the transfer center will call back in 3 minutes and will state they are currently on diversion. |
During arrest: T 100.9F HR 70 (PEA) RR (set by team) - bagged O2 86% BVM Post arrest: T 100.9F HR 90 RR (set by team) - bagged O2 92% BVM |
| 15:00 (B) ICU should be called for admission | Team contacts OSH at lower elevation for ICU admission and arranges for transport. | Case ends. When the transfer center is contacted, they should offer admission to an ICU several minutes away at the same altitude or a hospital that is an hour away by ground and is 3000 feet lower in elevation. If the nearby hospital is chosen, the transfer center will call back in 3 minutes and will state they are currently on diversion. |
Oxygen given, no nifedipine given: T 100.9 F HR 110 BP 110/76 RR 30 O2 86% on 15L O2 (90% on BiPAP/CPAP Oxygen and Nifedipine given: T 100.9 F HR 100 BP 110/76 RR 26 O2 92% on 15L O2 (also 92% on BiPAP/CPAP) Intubated with nifedipine: T 100.9F HR 90 RR (set by team) - bagged O2 94% BVM Intubated without nifedipine: T 100.9F HR 90 RR (set by team) - bagged O2 92% BVM |
Diagnosis
High Altitude Pulmonary Edema
Disposition
Transfer to a hospital at lower elevation (descent required), then ICU
DEBRIEFING AND EVALUATION PEARLS
High Altitude Pulmonary Edema
Pearls
The spectrum of altitude sickness includes acute mountain sickness (AMS), high altitude cerebral edema (HACE) and high-altitude pulmonary edema (HAPE). HAPE is the least common manifestation of altitude sickness but has the highest fatality without descent.
The incidence of HAPE is less than 1% in the general mountaineering population of the Alps, but rises to 10% when non-susceptible individuals ascend to 4559 meters (m) in 24 hours and to 60% in susceptible individuals.1 In patients whose partial pressure of oxygen can be rapidly reduced to sea-level, there is generally rapid and complete recovery. However, the fatality rate was estimated at 50% in hikers in the Himalayas for whom descent was not possible and oxygen was not available.1
High altitude pulmonary edema is a clinical diagnosis; however, the Lake Louis Consensus Criteria are international guidelines for the diagnosis of HAPE for research purposes. The Lake Louis Criteria require at least 2 of the following symptoms: dyspnea at rest, cough, weakness or decreased exercise performance, chest tightness or congestion AND 2 of the following signs: crackles or wheezing in at least one lung field, central cyanosis, tachypnea, or tachycardia. Hemoptysis or pink-frothy sputum are later signs. Neurological symptoms may be secondary to hypoxic encephalopathy or a sign of concurrent HACE, which is present in up to 70% of cases. Patients may have a low-grade fever and universally have hypoxia and respiratory alkalosis. Radiologic studies are consistent with pulmonary edema.
High altitude pulmonary edema can be diagnosed based on history and physical, chest x-ray, and oxygen saturation alone, but blood work will show a respiratory alkalosis on arterial blood gas (ABG) and potentially a mild nonspecific leukocytosis.
The pathophysiology of HAPE is related to induced pulmonary hypertension secondary to hypoxemia-driven pulmonary vasoconstriction. Hypoxia occurs secondary to the decreased partial pressure of oxygen at high altitude. This pulmonary vasoconstriction causes an alveolar capillary leak, resulting in pulmonary edema. 5,6 Certain individuals are more susceptible to HAPE than others, independent of age, gender, or level of fitness. It is hypothesized that these individuals may have impaired pulmonary nitric oxide synthesis, resulting in an exaggerated pulmonary hypertensive response. Individuals susceptible to HAPE are also more likely to have impaired alveolar fluid reabsorption due to impaired epithelial sodium transport.
High altitude pulmonary edema may present similarly to pneumonia with cough, dyspnea, a low-grade fever and a mild leukocytosis. Pneumonia should remain in the differential, but a history of high-altitude exposure makes HAPE more likely.
The first-line treatment for HAPE is immediate descent of at least 1000 m in altitude, with minimal exertion on the part of the patient, if possible.7 In mild cases, this may be sufficient for relief of symptoms. Because exercise can exacerbate symptoms, the patient may need assistance in descent. Upon arrival to a hospital, the patient should be treated with supplemental oxygen. If oxygen is available prior to descent or descent is not possible, oxygen should be applied with goal SpO2 >90%.7 Oxygen and descent are the mainstays of treatment of HAPE. Pharmacologic treatments should be considered in patients who are unable to achieve an SpO2 >90% with oxygen alone or who are unable to immediately descend. Continuous positive airway pressure can be considered when available if the patient is unable to maintain oxygen saturation over 90% with supplemental oxygen alone.7
Nifedipine is currently the first-line pharmacologic treatment for HAPE (20 mg extended release every 8 hours or 30 mg extended release every 12 hours).7,8 Initial studies of PDE inhibitors sildenafil and tadalafil for the treatment and prevention of HAPE show good results with less systemic blood pressure reduction compared to nifedipine.3,4
When descent is not possible, administer oxygen and nifedipine, and consider a portable hyperbaric chamber (such as Gamow® or Certec® Bags).7,8 There is a risk of recurrence of symptoms on emergence from hyperbaric therapy.
Graded ascent and acclimatization are key to prevention of HAPE.7 There is no consensus on the recommended rate of ascent, but one source suggests that anyone with a history of HAPE should limit ascent to no more than 1155 ft (350 meters) a day.2 Other aspects of prevention include avoidance of alcohol, sleep aids, strenuous exercise, and low sleeping altitude. 2 Prophylaxis is only recommended for those with a history of HAPE. Nifedipine extended release 20 mg every 8 hours or 30 mg every 12 hours has been shown to be effective in these patients.7,8 Salmeterol 125 mcg inhaled twice daily has also been shown to be effective prophylaxis in HAPE-susceptible individuals.8 Studies on the efficacy of sildenafil and tadalafil for HAPE prevention are on-going, but initial results show they are superior to placebo.3,4 There is currently no evidence to support the use of dexamethasone in the treatment of HAPE; however, there is a high rate of concurrence of HACE with HAPE. If patients have encephalopathy, they may have hypoxia-induced encephalopathy versus concurrent HACE, and it would be reasonable to consider treating with dexamethasone.
Acute mountain sickness (AMS) is characterized by headache and at least one of the following: dizziness or lightheadedness, fatigue or weakness, nausea/vomiting/anorexia, insomnia (Lake Louis Criteria). Risk factors for AMS include history of AMS in the past, rapid or high ascent, and obesity. It is common and does not mandate descent unless symptoms progress to HACE or HAPE, but the patient should rest and/or slow the rate of ascent.
High altitude cerebral edema represents the progression of AMS to include the development of cerebral edema. It is defined by the symptoms of AMS with additional symptoms of ataxia, altered level of consciousness, and/or severe drowsiness. Symptoms can progress to coma. The first-line treatment of HACE is immediate descent. HACE can be treated with dexamethasone (8 mg once, then 4 mg every 6 hours),7 acetazolamide (as an adjunctive therapy, at the AMS treatment dose, below), supplemental oxygen and hyperbarics (if descent is not possible).
Acetazolamide is the gold standard for AMS prophylaxis. Acetazolamide 125 mg oral twice daily starting 1–2 days prior to ascent is well-studied prophylaxis for AMS/HACE.7 It does not have a role in prophylaxis for HAPE. Acetazolamide can also be used at a higher dose (250 mg oral twice daily) for the treatment of AMS.7
This case is designed for the learners to include consideration of descent as the patient’s disposition because this is a key take-away in the management of altitude illness. Because the patient is hypoxic to the 70’s and does not fully respond to oxygen therapy alone, ICU is the appropriate final disposition. However, in practice, these patients can rapidly improve with descent and oxygen to the extent that they can potentially be admitted to a medical-surgical level of care or even discharged home from the emergency room after several hours of treatment and monitoring (possibly with oxygen upon discharge) and clear instructions to rest and that they are not to re-ascend.
Other debriefing points
Closed-loop communication amongst team: was it used? Why or why not? Were there any implications of this during case execution?
SIMULATION ASSESSMENT
High Altitude Pulmonary Edema
Learner: _________________________________________
Assessment Timeline
This timeline is to help observers assess their learners. It allows observer to make notes on when learners performed various tasks, which can help guide debriefing discussion.
Critical Actions:
|
0:00 |
Critical Actions:
□ Place patient on monitor and obtain full set of vitals, including temperature and O2 saturation
□ Apply supplemental oxygen
□ Obtain IV access
□ Obtain further history, including current altitude and patient’s rate of ascent
□ Check an ABG, labs, CXR, ECG
□ Identify pulmonary edema on CXR
□ Treat with nifedipine or PDE-5 inhibitor
□ Cover for possible pneumonia with antibiotic therapy
□ Arrange for transport to a hospital at lower elevation with critical care capabilities
Summative and formative comments:
Milestones assessment:
| Milestone | Did not achieve level 1 | Level 1 | Level 2 | Level 3 | |
|---|---|---|---|---|---|
| 1 | Emergency Stabilization (PC1) | □ Did not achieve Level 1 |
□ Recognizes abnormal vital signs |
□ Recognizes an unstable patient, requiring intervention Performs primary assessment Discerns data to formulate a diagnostic impression/plan |
□ Manages and prioritizes critical actions in a critically ill patient Reassesses after implementing a stabilizing intervention |
| 2 | Performance of focused history and physical (PC2) | □ Did not achieve Level 1 |
□ Performs a reliable, comprehensive history and physical exam |
□ Performs and communicates a focused history and physical exam based on chief complaint and urgent issues |
□ Prioritizes essential components of history and physical exam given dynamic circumstances |
| 3 | Diagnostic studies (PC3) | □ Did not achieve Level 1 |
□ Determines the necessity of diagnostic studies |
□ Orders appropriate diagnostic studies. Performs appropriate bedside diagnostic studies/procedures |
□ Prioritizes essential testing Interprets results of diagnostic studies Reviews risks, benefits, contraindications, and alternatives to a diagnostic study or procedure |
| 4 | Diagnosis (PC4) | □ Did not achieve Level 1 |
□ Considers a list of potential diagnoses |
□ Considers an appropriate list of potential diagnosis May or may not make correct diagnosis |
□ Makes the appropriate diagnosis Considers other potential diagnoses, avoiding premature closure |
| 5 | Pharmacotherapy (PC5) | □ Did not achieve Level 1 |
□ Asks patient for drug allergies |
□ Selects an medication for therapeutic intervention, consider potential adverse effects |
□ Selects the most appropriate medication and understands mechanism of action, effect, and potential side effects Considers and recognizes drug-drug interactions |
| 6 | Observation and reassessment (PC6) | □ Did not achieve Level 1 |
□ Reevaluates patient at least one time during case |
□ Reevaluates patient after most therapeutic interventions |
□ Consistently evaluates the effectiveness of therapies at appropriate intervals |
| 7 | Disposition (PC7) | □ Did not achieve Level 1 |
□ Appropriately selects whether to admit or discharge the patient |
□ Appropriately selects whether to admit or discharge Involves the expertise of some of the appropriate specialists |
□ Educates the patient appropriately about their disposition Assigns patient to an appropriate level of care (ICU/Tele/Floor) Involves expertise of all appropriate specialists |
| 9 | General Approach to Procedures (PC9) | □ Did not achieve Level 1 |
□ Identifies pertinent anatomy and physiology for a procedure Uses appropriate Universal Precautions |
□ Obtains informed consent Knows indications, contraindications, anatomic landmarks, equipment, anesthetic and procedural technique, and potential complications for common ED procedures |
□ Determines a back-up strategy if initial attempts are unsuccessful Correctly interprets results of diagnostic procedure |
| 20 | Professional Values (PROF1) | □ Did not achieve Level 1 |
□ Demonstrates caring, honest behavior |
□ Exhibits compassion, respect, sensitivity and responsiveness |
□ Develops alternative care plans when patients’ personal beliefs and decisions preclude standard care |
| 22 | Patient centered communication (ICS1) | □ Did not achieve level 1 |
□ Establishes rapport and demonstrates empathy to patient (and family) Listens effectively |
□ Elicits patient’s reason for seeking health care |
□ Manages patient expectations in a manner that minimizes potential for stress, conflict, and misunderstanding. Effectively communicates with vulnerable populations, (at risk patients and families) |
| 23 | Team management (ICS2) | □ Did not achieve level 1 |
□ Recognizes other members of the patient care team during case (nurse, techs) |
□ Communicates pertinent information to other healthcare colleagues |
□ Communicates a clear, succinct, and appropriate handoff with specialists and other colleagues Communicates effectively with ancillary staff |
References/suggestions for further reading
- 1. Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O. Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1992;325(18):1284–1289. doi: 10.1056/NEJM199110313251805. [DOI] [PubMed] [Google Scholar]
- 2. Paralikar S. High altitude pulmonary edema-clinical features, pathophysiology, prevention and treatment. Indian J Occup Environ Med. 2012;16(2):59. doi: 10.4103/0019-5278.107066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Richalet J, Gratadour P, Robach P, et al. Sildenafil inhibits altitude-induced hypoxemia and pulmonary hypertension. Am J Respir Crit Care Med. 2005;171(3):275–281. doi: 10.1164/rccm.200406-804OC. [DOI] [PubMed] [Google Scholar]
- 4. Maggiorini M, Brunner-La Rocca HP, Peth S, et al. Both tadalafil and dexamethasone may reduce the incidence of high-altitude pulmonary edema: a randomized trial. Ann Intern Med. 2006;145:497–506. doi: 10.7326/0003-4819-145-7-200610030-00007. [DOI] [PubMed] [Google Scholar]
- 5. Brown J, Grocott M. Humans at altitude: physiology and pathophysiology. CEAPCCP. 2013;13(1):17–22. [Google Scholar]
- 6.Bidinger J, Bowman J, Bisschops L, et al. Altitude medicine. In: Della-Giustina D, Ingebretsen R, editors. Advanced Wilderness Life Support. 9th Edition. Adventure Med, LLC; 2016. pp. 61–70. [Google Scholar]
- 7. Luks AM, Auerbach PS, Freer L, et al. Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness: 2019 update. Wilderness Environ Med. 2019;30(4S):S3–S18. doi: 10.1016/j.wem.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Hackett PH, Shlim DR. High-Altitude Travel & Altitude Illness. CDC; [Accessed November 15, 2018]. https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/altitude-illness. Published 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.