Abstract
There is inconsistent conclusion for the relationship of social isolation and loneliness with poor sleep. We investigated the associations of social isolation and loneliness with new-onset insomnia symptoms in a nationally-representative sample of 9,430 adults aged ≥50 who were free of any insomnia symptoms/sleep disorders at baseline (wave 12/13) and followed up to 4 years from the Health and Retirement Study. Social isolation was measured by Steptoe’s Social Isolation Index. Loneliness was measured by the revised 3-item UCLA-Loneliness Scale. Insomnia symptoms were quantified using the modified Jenkins Sleep Questionnaire. During a mean follow-up of 3.52 years, 1,522 (16.1%) participants developed at least one insomnia symptom. Cox models showed that loneliness was associated with the onset of difficulties initiating or maintaining sleep, early-morning awakening, nonrestorative sleep, and at least one of these symptoms after adjusting for potential covariates; while social isolation was not associated with the onset of difficulties maintaining sleep, early-morning awakening, or at least one insomnia symptom after adjusting for health indicators. These results are consistent in sensitivity analyses and stratified analyses by age, sex, race/ethnicity, and obesity. Public health interventions aimed at fostering close emotional relationships may reduce the burden of poor sleep among middle-aged and older adults.
Keywords: Social Relationship, Social Connection, Sleep Disturbance, Sleep Disorders, Survival Analysis
1. Introduction
Aging is often accompanied by sleep disturbance, which is defined as impaired sleep quality and insomnia symptoms (Kocevska et al., 2020). Nearly half of older adults aged ≥65 experienced insomnia symptoms (Miner & Kryger, 2017), including difficulty initiating sleep, difficulty maintaining sleep, early-morning awakening, and nonrestorative sleep (Bloom et al., 2009). Research suggests that insomnia symptoms are associated with higher risks of cardiovascular diseases (He et al., 2017), dementia (Beydoun et al., 2021), increased hospitalization and nursing home admission (Kaufmann et al., 2013), and mortality (Mahmood et al., 2022). The health burden attributable to insomnia is expected to rise in response to worldwide population aging.
Meaningful social connection is a fundamental aspect of the human experience (Cacioppo & Cacioppo, 2018). Social isolation and loneliness are two distinct concepts that tend to be only weakly correlated (J. McHugh et al., 2017). Social isolation refers to the lack of social connections or interactions with others, while loneliness represents a perceived discrepancy between one’s actual and desired social relationships (National Academies of Sciences, Engineering, and Medicine, 2020). Individuals having frequent social contact with others may feel lonely; conversely, socially isolated individuals can be satisfied with their social relationships (National Academies of Sciences, Engineering, and Medicine, 2020; Qi, Pei, et al., 2022). Both social isolation and loneliness have been linked to various negative health outcomes, including psychological distress, cardiovascular diseases, cognitive impairment/dementia, suicide risk, and even premature mortality (Evans et al., 2019; Holt-Lunstad et al., 2015; Motillon-Toudic et al., 2022; Qi, Zhang, et al., 2022; Valtorta et al., 2016). It is well-recognized that these health outcomes are associated with insomnia symptoms (Kocevska et al., 2020; Liu et al., 2020). However, mixed evidence exists for the influences of social isolation and loneliness on sleep disturbance in the adult population, and there is no consensus about the independent effects of social isolation and loneliness on sleep disturbance. Some studies have reported that social isolation, but not loneliness, was associated with sleep disturbances (Yu et al., 2018). Other studies have reported that only loneliness was associated with sleep disturbances (Kurina et al., 2011; J. E. McHugh & Lawlor, 2013; J. McHugh & Lawlor, 2011). Lastly, a few studies have suggested that both social isolation and loneliness are associated with sleep disturbance (Benson et al., 2021; Cho et al., 2019). Possibilities for these discrepancies are that the associations may be affected by risk factors that were not consistently considered (Griffin, Williams, Mladen, et al., 2020) or methodological deficiencies (e.g., small sample size (Kurina et al., 2011), homogenous sample (J. E. McHugh & Lawlor, 2013; J. McHugh & Lawlor, 2011), lack of representativeness of the population) (Benson et al., 2021; Cho et al., 2019; Yu et al., 2018) in previous studies. Although one recent meta-analysis examined the association between loneliness and sleep quality, the synthesized results suggest that longitudinal relationship between loneliness and sleep remains unclear (Griffin, Williams, Ravyts, et al., 2020). To address these limitations, there is a need to further examine these associations by using a large representative sample that covers diverse populations.
Existing studies have focused on insomnia as a generic condition, but little is known about whether social isolation and loneliness are uniquely associated with specific insomnia symptoms. Nonrestorative sleep is a distinct insomnia symptom that occurs independently of other symptoms, including difficulties initiating or maintaining sleep (Roth et al., 2010). These symptoms are key components of diagnosing insomnia according to the DSM-5 (American Psychiatric Association & American Psychiatric Association, 2013) and International Classification of Diseases-11(Olufsen et al., 2020). However, little is known about the relationships between the onset of specific insomnia symptoms with social isolation and loneliness. These knowledge gaps introduce challenges to developing targeted interventions for poor sleep later in life. We aimed to extend the existing literature by examining the association of social isolation and loneliness, individually and simultaneously, with the onset of insomnia symptoms in a nationally-representative sample of middle-aged and older adults in the United States (US).
2. Methods
2.1. Data source
Data were from the Health and Retirement Study (HRS), which is a nationally-representative, longitudinal survey of middle-aged and older adults in the United States, conducted since 1992. The HRS has been designed specifically to investigate the health, economic, and social factors that impact the well-being of individuals as they age (Sonnega et al., 2014). Its rich and comprehensive data, collected biennially, include information on demographics, socio-economic status, physical and mental health, health behaviors, social connections, and caregiving. Additional details on the sample design and procedures have been described previously (Sonnega et al., 2014). Importantly, the HRS utilizes standardized and validated measures of sleep quality, social isolation, and loneliness, ensuring the reliability and validity of our findings. Furthermore, the longitudinal design of the HRS enables us to examine the temporal relationships between these variables and control for potential covariates, thereby increasing the rigor and validity of our analyses. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
2.2. Study population
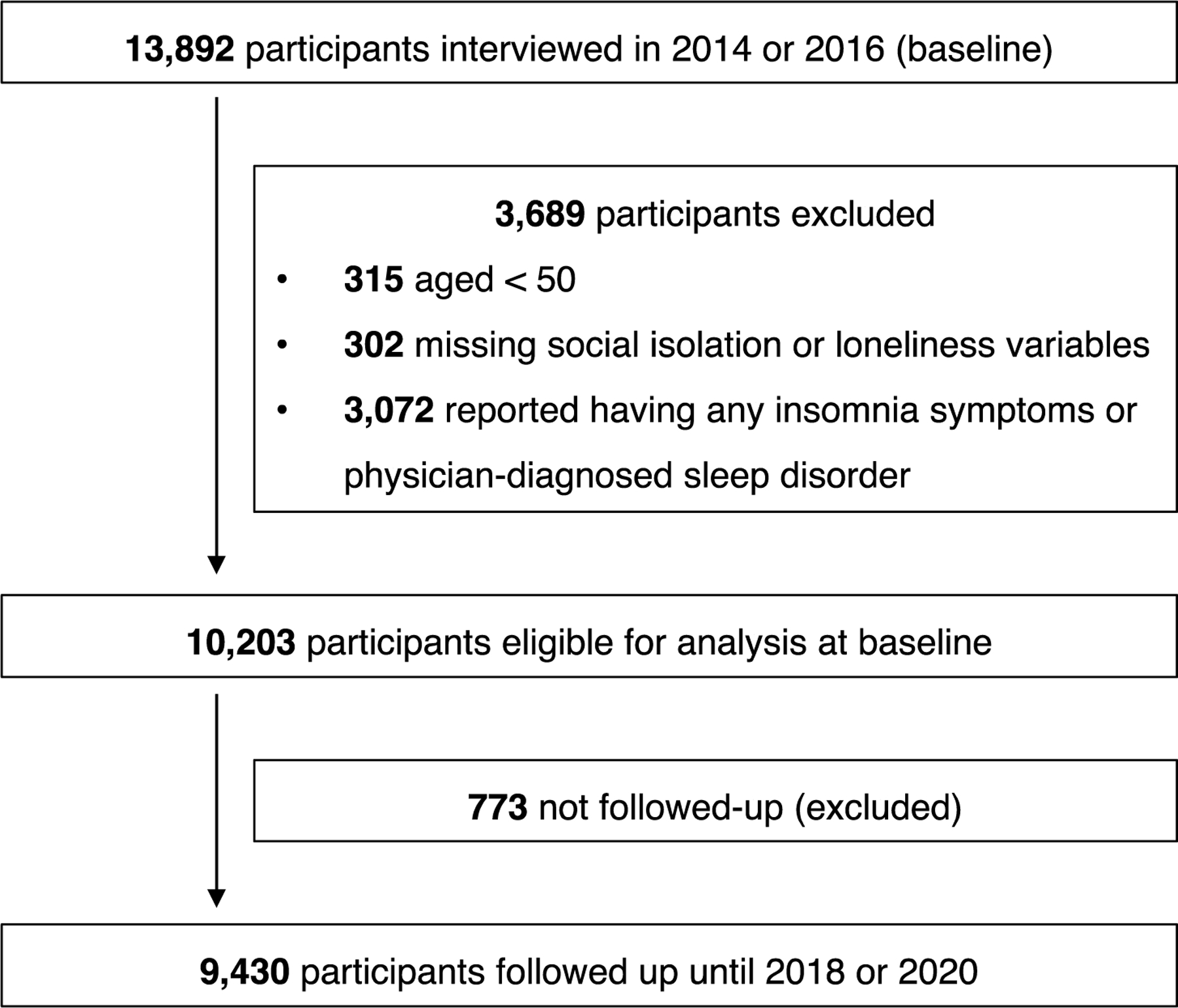
Since wave 8, HRS initiated a mixed-mode follow-up, whereby 50% of random subsamples were assigned to in-person follow-up, and the remaining 50% were assigned to telephone follow-up. The in-person follow-up group was requested to complete and return by postal mail the Psychosocial and Lifestyle Questionnaire (PLQ) that collects psychosocial characteristics (e.g., social isolation, loneliness). The PLQ response rate among interviewees was around 90% (Smith et al., 2017). Furthermore, three out of four insomnia symptoms were not evaluated in the HRS wave 9 and wave 11 (Mahmood et al., 2022). To ensure the measurements of social isolation and loneliness precede insomnia symptoms, we restricted our sample to 13,892 HRS participants who completed the PLQ in wave 12 or wave 13. We then applied the following exclusion criteria: participants aged <50 (n = 315), and participants who reported having insomnia symptoms or physician-diagnosed sleep disorders at baseline (n = 3,072), as the study aimed to investigate new-onset insomnia symptoms. Additionally, we were unable to include 302 participants with missing social isolation or loneliness data due to the unavailability of complete information for our analysis. Lastly, we noted that 773 participants were lost to follow-up and not included in the final analytic sample. After applying these exclusions and accounting for participants lost to follow-up, the final analytic sample included 9,430 participants (see Figure 1 for sample selection). Included participants were younger, more likely to be white, more educated, higher income, and had lower levels of depressive symptoms and fewer chronic conditions than those excluded from these analyses (all P < .001).
Figure 1. Flowchart of the sample selection.
2.3. Measures
2.3.1. Social isolation
Social isolation was estimated at baseline using the Steptoe’s Social Isolation Index that was first validated in the English Longitudinal Study of Aging (Steptoe et al., 2013) and adapted to the HRS (Crowe et al., 2021; Qi, Pei, et al., 2023). We assigned a social isolation score to each participant based on whether they 1) were unmarried or not cohabiting, 2) had less than monthly contact (whether face-to-face, written, or telephone) with children, 3) had less than monthly contact with other family members, 4) had less than monthly contact with friends, and 5) did not participate in any religious groups, clubs, or other social organizations, yielding scores 0–5. We followed the procedure of previous studies (Qi, Ng, et al., 2023; Steptoe et al., 2013) and classified participants in the top quintile of scale scores as socially isolated (scoring ≥2).
2.3.2. Loneliness
Loneliness was estimated using the revised 3-item UCLA Loneliness Scale at baseline (Hughes et al., 2004). Participants rated how frequently they felt 1) lacking companionship, 2) left out, and 3) isolated from others on a 3-point scale. Previous analysis showed that this 3-item version had similar psychometric properties to the original 20-item version (Hughes et al., 2004). This 3-item version has been used extensively in this population (Crowe et al., 2021; Qi, Belsky, et al., 2023; Qi, Pei, et al., 2023). We coded item responses so that higher scores correspond to a higher loneliness level. Final scores ranged from 3 to 9. We followed the same procedure used for social isolation and classified participants in the top quintile of scale scores as lonely (scoring ≥6).
2.3.3. Insomnia symptoms
Insomnia symptoms were estimated using a modified version of the Jenkins Sleep Questionnaire, a validated and widely used screening tool that measures self-reported insomnia symptoms (Jenkins et al., 1988). Participants were asked how often they 1) had trouble falling asleep, 2) woke up during the night, 3) woke up too early and were unable to fall asleep again, and 4) felt really rested when waking up in the morning. The responses were “most of the time,” “sometimes,” and “rarely or never.” We defined individuals as experiencing a specific insomnia symptom if they answered “most of the time” or “sometimes” to the first three questions and “rarely or never” or “sometimes” to the fourth question (Beydoun et al., 2021; Kaufmann et al., 2013).
2.3.4. Covariates
Baseline covariates were selected based on previous studies on social isolation, loneliness, and sleep disturbance (Benson et al., 2021; Cho et al., 2019; Yu et al., 2018). Participants reported their socio-demographic characteristics, including age, sex, race/ethnicity, education, and income. Lifestyle includes smoking, alcohol consumption, and physical exercise. Additionally, health indicators include obesity (body mass index ≥30 kg/m2), depressive symptoms, activities of daily living (ADL), cognitive function, and chronic conditions. Details of measurement for each covariate are reported in the Supplementary Table S1.
2.4. Statistical analysis
Baseline characteristics were compared between participants who are isolated vs. non-isolated or lonely vs. not lonely using t-tests for continuous variables and Chi-square tests for dichotomous variables. No issues with multicollinearity were detected using variance inflation factors (all ≤ 2.0). Cox models that satisfied the proportional hazard assumption were performed to calculate hazard ratios (HRs) and 95% Confidence Intervals (CIs). Individuals who did not develop insomnia symptoms, died, or were lost to follow-up were censored at their last assessment. We fitted five separate models to discern the extent to which socio-demographic, lifestyle, health characteristics, and loneliness explained observed associations between social isolation and the onset of at least one insomnia symptom over a 4-year follow-up [Model 1: unadjusted. Model 2: adjusted for demographic characteristics. Model 3: further adjusted for lifestyle factors. Model 4: further adjusted for health indicators. Model 5: further adjusted for loneliness]. Similar models were fitted to test the independent associations of loneliness with insomnia symptoms. There was a small percentage of missing data on covariates (all <3.7%). All non-missing data points were used in the analyses. Cox models were stratified by age (50–64, 65–75, >75 years), sex (men, women), race/ethnicity (white, black, Hispanics), and obesity (yes, no) at baseline to assess potential modification effects because of major differences in the prevalence and risk factors of insomnia symptoms in these subgroups (Kocevska et al., 2020). Cox models were also used to determine the independent associations of social isolation and loneliness with the onset of each specific insomnia symptom at follow-ups.
Sensitivity analyses were performed. First, social isolation and loneliness were analyzed as continuous variables. Second, although complete case analyses were conducted in primary analyses, we also conducted multiple imputations for missing values (Sullivan et al., 2017). We created 10 imputed data sets using multivariate imputation by chained equations (MICE), including all variables used in the analysis and combined each estimate based on Rubin’s rule (White et al., 2011).
HRS’s sampling weights were applied to all analyses to account for the unequal probability of participants’ selection. All analyses were conducted using Stata version 17 MP (StataCorp, 2022). A two-tailed P < .05 indicated statistical significance.
3. Results
The mean age of the participants was 68.0 years (SD 10.2), 58.3% were women, and 1,522 had developed at least one insomnia symptom (16.1%). Specifically, 1,394 (14.8%) participants reported difficulties initiating sleep, 1,108 (11.7%) reported difficulties maintaining sleep, 1,333 (14.1%) reported early-morning awakening, and 1,225 (13.0%) reported nonrestorative sleep. Table 1 shows the characteristics of all participants and subgroups based on social isolation and loneliness. Significant differences in participants’ characteristics were observed between non-isolated vs. isolated and non-lonely vs. lonely groups. Being socially isolated or lonely was associated with being a person reporting a racial/ethnic minority background, less education, less income, and being a current/former smoker or less physically active, being ADL impaired, having more depressive symptoms, lower levels of cognitive function, and more chronic conditions.
Table 1.
Baseline participants characteristics according to categories of social isolation and loneliness (N = 9,430)a.
| Characteristics | All participants, mean (SD) or N (%) | Not socially isolated, mean (SD) or N (%) | Socially isolated, mean (SD) or N (%) | P b | Not lonely, mean (SD) or N (%) | Lonely, mean (SD) or N (%) | P b |
|---|---|---|---|---|---|---|---|
| N | 9,430 | 6,728 (71.4) | 2,702 (28.6) | 7,471 (79.2) | 1,959 (20.8) | ||
| Age in years | 68.0 (10.2) | 66.9 (9.9) | 70.5 (10.5) | <.001 | 68.2 (10.2) | 67.1 (10.4) | <.001 |
| Women | 5,495 (58.3) | 4,026 (59.8) | 1,469 (54.4) | <.001 | 4,308 (57.7) | 1,187 (60.6) | .019 |
| Race/ethnicity | <.001 | <.001 | |||||
| Non-Hispanic white | 6,294 (66.8) | 4,643 (69.0) | 1,651 (61.2) | 5,003 (67.0) | 1,291 (65.9) | ||
| Non-Hispanic black | 1,633 (17.3) | 1,067 (15.8) | 566 (21.0) | 1,239 (16.6) | 394 (20.1) | ||
| Hispanics | 1,177 (12.5) | 784 (11.7) | 393 (14.5) | 990 (13.3) | 187 (9.6) | ||
| Other | 320 (3.4) | 232 (3.5) | 88 (3.3) | 234 (3.1) | 86 (4.4) | ||
| Education | <.001 | .009 | |||||
| <High school | 1,477 (15.7) | 784 (11.7) | 693 (25.6) | 1,147 (15.3) | 330 (16.8) | ||
| High school diploma | 2,901 (30.8) | 1,855 (27.5) | 1,046 (38.7) | 2,255 (30.2) | 646 (33.0) | ||
| Some/completed college | 3,711 (39.3) | 2,948 (43.8) | 763 (28.3) | 2,986 (40.0) | 725 (37.0) | ||
| Graduate degree | 1,341 (14.2) | 1,141 (17.0) | 200 (7.4) | 1,083 (14.5) | 258 (13.2) | ||
| Income levels ($) | <.001 | <.001 | |||||
| ≤49,999 | 4,855 (51.6) | 2,965 (44.2) | 1,890 (70.1) | 3,679 (49.4) | 1,176 (60.3) | ||
| 50,000–99,999 | 2,441 (26.0) | 1,905 (28.4) | 536 (19.9) | 2,005 (26.9) | 436 (22.3) | ||
| 100,000–200,000 | 1,489 (15.8) | 1,277 (19.0) | 212 (7.9) | 1,252 (16.8) | 237 (12.2) | ||
| >200,000 | 620 (6.6) | 563 (8.4) | 57 (2.1) | 518 (6.9) | 102 (5.2) | ||
| Smoking status | <.001 | <.001 | |||||
| Never | 4,406 (46.9) | 3,271 (48.8) | 1,125 (41.8) | 3,510 (47.2) | 886 (45.4) | ||
| Former | 3,974 (42.3) | 2,817 (42.1) | 1,157 (43.0) | 3,192 (42.9) | 782 (40.0) | ||
| Current | 1,020 (10.8) | 613 (9.1) | 407 (15.2) | 735 (9.9) | 285 (14.6) | ||
| Alcohol consumption | <.001 | <.001 | |||||
| Never | 5,532 (58.9) | 3,681 (54.9) | 1,851 (68.8) | 4,291 (57.6) | 1,241 (63.6) | ||
| Light | 2,818 (30.0) | 2,242 (33.4) | 576 (21.4) | 2,302 (30.9) | 516 (26.5) | ||
| Heavy | 1,048 (11.1) | 784 (11.7) | 264 (9.8) | 855 (11.5) | 193 (9.9) | ||
| Have regular physical exercise | 2,572 (27.4) | 2,046 (30.5) | 526 (19.5) | <.001 | 2,148 (28.9) | 424 (21.7) | <.001 |
| Obesity (BMI ≥30 kg/m 2 ) | 5,948 (63.1) | 4,250 (63.2) | 1,698 (62.8) | .766 | 4,766 (63.8) | 1,182 (60.3) | .005 |
| Depressive symptoms | .68 (1.24) | .57 (1.13) | .95 (1.44) | <.001 | .50 (1.01) | 1.35 (1.71) | <.001 |
| Cognitive function | 15.22 (4.50) | 15.84 (4.33) | 13.66 (4.55) | <.001 | 15.36 (4.44) | 14.68 (4.71) | <.001 |
| ADL disability | 452 (4.8) | 244 (3.6) | 208 (7.7) | <.001 | 316 (4.2) | 136 (6.9) | <.001 |
| Number of chronic conditions | 1.84 (1.27) | 1.73 (1.25) | 2.09 (1.27) | <.001 | 1.81 (1.26) | 1.93 (1.29) | <.001 |
Note:
Abbreviations: SD, standard deviation; BMI, body mass index (kilograms divided by height in meters squared), ADL, activities of daily living.
Unless indicated otherwise, data are expressed as N (%) of participants. Percentages have been rounded and may not total 100, and numbers may not total numbers in column headings owing to missing data.
Comparisons were performed using t-tests for continuous variables and the Chi-squared tests for categorical variables.
Figure 2 presents the adjusted associations of social isolation with the onset of at least one insomnia symptom. In the unadjusted model, HR for the isolated group was 1.37 [95% CI 1.23–1.52; P < .001] compared with the non-isolated group. Adjusting for other covariates, including socio-demographics and lifestyle, did not substantially affect the estimates. However, when health indicators were adjusted, the association was attenuated and became insignificant (HR, 1.06; 95% CI, 0.95–1.17; P = .460).
Figure 2. The associations of social isolation with developing any insomnia symptoms (N = 9,430).
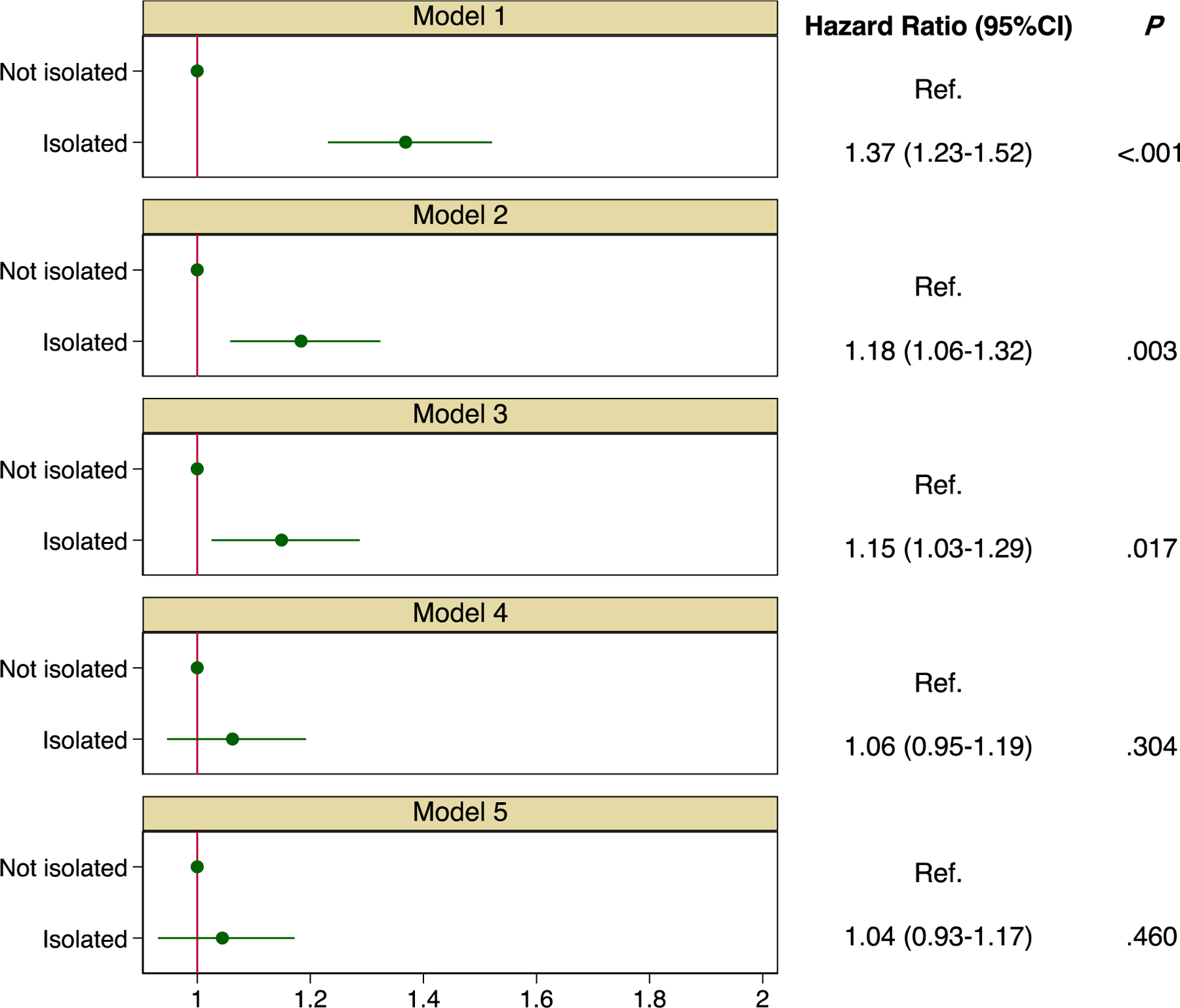
Notes:
All hazard ratios (HRs) are weighted to account for the complex survey design. 95% CI, 95% confidence interval. Model 1: Unadjusted. Model 2: Adjusting for age, sex, race/ethnicity, education, and income. Model 3: Additionally adjusting for smoking, alcohol consumption, and physical exercise. Model 4: Additionally adjusting for obesity, depressive symptoms, activities of daily living, cognitive function, and chronic conditions. Model 5: Additionally adjusting for loneliness.
The unadjusted HR for loneliness was statistically significant (1.91; 95% CI 1.71–2.12; P < .001, Figure 3). This association was only slightly reduced when additional adjustments were made for socio-demographic, lifestyle, and health indicators (HR, 1.55; 95% CI, 1.38–1.74; P < .001). HR also remained unchanged (HR, 1.55; 95% CI, 1.37–1.74; P < .001) when social isolation was additionally considered. The full Cox models, including all variables, are shown in the Supplementary Table S2.
Figure 3. The associations of loneliness with developing any insomnia symptoms (N = 9,430).
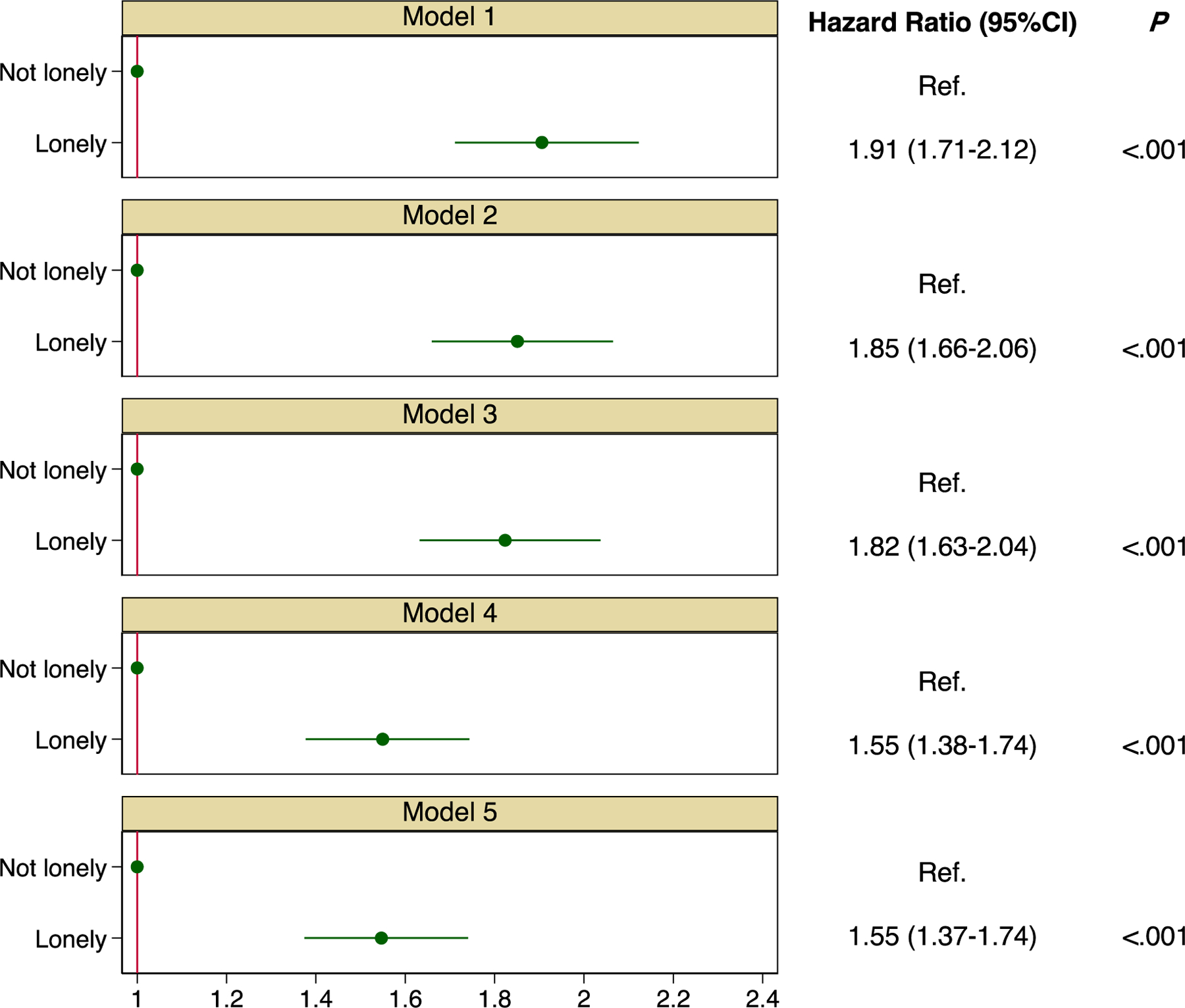
Notes:
All hazard ratios (HRs) are weighted to account for the complex survey design. 95% CI, 95% confidence interval. Model 1: Unadjusted. Model 2: Adjusting for age, sex, race/ethnicity, education, and income. Model 3: Additionally adjusting for smoking, alcohol consumption, and physical exercise. Model 4: Additionally adjusting for obesity, depressive symptoms, activities of daily living, cognitive function, and chronic conditions. Model 5: Additionally adjusting for social isolation.
Stratified analyses by age, sex, race/ethnicity, and obesity at baseline were then conducted (Supplementary Table S3). Results followed a pattern similar to that described earlier. The association of loneliness with the onset of at least one insomnia symptom was significant across different stratifications. For social isolation, further adjustment for health indicators reduced the HRs but became insignificant in stratified subgroups.
The same approach was used to examine the associations of social isolation and loneliness with the onset of each insomnia symptom (Table 2). Loneliness was associated with the onset of difficulties initiating or maintaining sleep, early-morning awakening, and nonrestorative sleep adjusting for all covariates (HR, 1.17–1.49, all P < .01). Social isolation was associated with the onset of difficulty maintaining sleep (HR, 1.15; 95% CI, 1.01–1.31; P < .05) and early-morning awakening (HR, 1.19; 95% CI, 1.06–1.34; P < .01), but not with the onset of difficulty initiating sleep (HR, 1.09; 95% CI, 0.98–1.22; P = .103) or nonrestorative sleep (HR, 1.11; 95% CI, 0.99–1.26; P = .083) after adjusting for health indicators.
Table 2.
Hazard ratios (HRs) for the associations of social isolation and loneliness with onset of each specific insomnia symptom (N = 9,430).
| No. of events/No. of participants (%) | No. of events/No. of participants | |||||||
|---|---|---|---|---|---|---|---|---|
| Insomnia symptoms | Socially isolated |
Not socially isolated |
HR (95% CI) | P | Lonely | Not lonely | HR (95% CI) | P |
| Difficulty initiating sleep | 459/2,702 (17.0) |
935/6,728 (13.9) |
1.09 (0.98, 1.22) | .103 | 337/1959 (17.2) |
1,057/7,471 (14.1) |
1.17 (1.05, 1.32) | <.01 |
| Difficulty maintaining sleep | 408/2,702 (15.1) |
700/6,728 (10.4) |
1.15 (1.01, 1.31) | .038 | 318/1,959 (16.2) |
790/7,471 (10.6) |
1.31 (1.14, 1.50) | <.001 |
| Early-morning awakening | 492/2,702 (18.2) |
841/2,702 (12.5) |
1.19 (1.06, 1.34) | .003 | 398/1,959 (20.3) |
935/7,471 (12.5) |
1.36 (1.20, 1.53) | <.001 |
| Nonrestorative sleep | 438/2,702 (16.2) |
787/6,728 (11.7) |
1.11 (0.99, 1.26) | .083 | 388/1,959 (19.8) |
837/7,471 (11.2) |
1.49 (1.31, 1.69) | <.001 |
Note:
All hazard ratios (HRs) are weighted to account for the complex survey design. 95% CI, 95% confidence interval. Models adjusted for age, sex, race/ethnicity, education, income, smoking, alcohol consumption, physical exercise, obesity, depressive symptoms, activities of daily living, cognitive function, and chronic conditions.
The sensitivity analysis showed that applying continuous measures of social isolation and loneliness did not change the results from those in the dichotomous measures, with the fully-adjusted HRs for the onset of at least one insomnia symptom 1.13 (95% CI, 1.10–1.17; P < .001) for every unit increase in loneliness but no significant association with social isolation (HR, 1.04; 95% CI, 0.99–1.08; P = .102; Supplementary Table S4). The results of the sensitivity analysis that imputed the missing values using MICE were essentially unchanged from those of the complete-case analyses (social isolation: HR, 1.04; 95% CI, 0.93–1.15; P = .525; loneliness: HR, 1.53; 95% CI, 1.37–1.71; P < .001; Supplementary Table S5).
4. Discussion
In this 4-year population-based prospective cohort study in adults aged 50 and older, we found that loneliness was associated with the onset of any insomnia symptoms, including difficulties initiating or maintaining sleep, early-morning awakening, and nonrestorative sleep. The associations were independent of social isolation and other potential covariates. The association of social isolation with the onset of difficulty initiating sleep, nonrestorative sleep, and at least one insomnia symptom became insignificant when baseline health indicators (e.g., obesity, depressive symptoms, activities of daily living, cognitive function, and chronic conditions) were considered, suggesting that the association may be driven partly by health status.
The present findings are consistent with most existing studies concerning loneliness as a significant and independent risk factor for sleep disturbance. In a recent meta-analysis of 16 studies involving 23,485 participants, Deng et al. concluded that lonely older adults were more likely to suffer from sleep disturbances than their counterparts without loneliness (Deng et al., 2023). In a cross-sectional study of 759 US older adults, increased loneliness was associated with actigraphy-estimated disrupted sleep and short sleep duration, self-reported insomnia symptoms (Benson et al., 2021), In contrast, a longitudinal study of 639 older adults in Taiwan found that the association between loneliness and sleep disturbances was insignificant after controlling for demographic and health-related factors (Yu et al., 2018). A possible explanation for this discrepancy includes differences in the operationalization of exposure and outcome variables. For example, the study in Taiwan (Yu et al., 2018) used a single item regarding the perception of loneliness in the last week to measure loneliness rather than the UCLA Loneliness Scale in our study.
Several explanations have been proposed for the underlying mechanisms by which loneliness affects insomnia symptoms. First, from an evolutionary perspective, humans must have relied on a safe environment to survive and thrive (Cacioppo & Cacioppo, 2018; Hawkley & Cacioppo, 2010). The absence of secure social surroundings may result in feelings of loneliness, that in turn, heighten feelings of vulnerability and unconscious vigilance to social threats, which are the opposite of relaxation and sound sleep (Hawkley & Cacioppo, 2010). Second, stress has been shown to significantly mediate associations between loneliness and sleep disturbances (J. E. McHugh & Lawlor, 2013). Feelings of loneliness have the potential to deplete individuals physically by impairing their sleep at night and contributing to daytime exhaustion (Hawkley & Cacioppo, 2010). Such exhaustion might result in a vicious cycle between stress and sleep, affecting sleep quality and causing additional worries of difficulty falling asleep (Aanes et al., 2011). Therefore, persistent intrusive thoughts about how to inadequately satisfy one’s needs in social interactions will lead to new-onset insomnia symptoms. Furthermore, from a psychophysiological perspective, loneliness can lower immune system function and raise neuroendocrine dysregulation (Walker et al., 2019), both of which are associated with sleep disturbances and may induce insomnia symptoms (Floam et al., 2015).
Social isolation was unassociated with insomnia symptoms after health indicators were considered. It is possible that social isolation is associated with other health-related risk factors for insomnia, so that in multivariate analysis it does not emerge as an independent risk factor. This finding is consistent with several systematic reviews which conclude loneliness may contribute more to sleep disturbance than social isolation (Choi, 2015; Deng et al., 2023). When each insomnia symptom was analyzed separately, insignificant associations were found for difficulties initiating sleep and nonrestorative sleep. Indeed, difficulty initiating sleep is more strongly associated with depression than difficulties maintaining sleep and early-morning awakening (Chen & Saito, 2021; Ikeda et al., 2017), and individuals who experience difficulties initiating sleep or nonrestorative sleep often have a poorer health status (e.g., cardio-cerebral vascular diseases) than individuals with difficulties maintaining sleep and early-morning awakening (He et al., 2017). Thus, difficulties initiating sleep and nonrestorative sleep may simply be indicators of poor health, and the associations of social isolation with them could be explained by pre-existing health status. This also suggests that social isolation might influence insomnia in complex ways that cannot be robustly assessed with subjective measures of insomnia symptoms. Previous studies have suggested a relationship between increased screen time, particularly in the evening hours, and poor sleep quality, as exposure to blue light emitted from screens can disrupt circadian rhythms and delay the onset of sleep (Gradisar et al., 2013). In addition, the advancement in social media and the constant connectivity it provides may contribute to feelings of social isolation and loneliness, even when individuals are physically surrounded by others (Primack et al., 2017). In light of these findings, our study further emphasizes the importance of addressing both the emotional and technological aspects of modern life that may contribute to the onset of insomnia symptoms among middle-aged and older adults.
4.1. Strengths & limitations
To our knowledge, this is the first large-scale study to investigate the associations of social isolation and loneliness with insomnia symptoms in a nationally-representative sample of middle-aged and older adults. Nevertheless, several limitations should be noted. First, insomnia symptoms were evaluated using a self-reported questionnaire, and no objective measurements were available in HRS. Second, insomnia symptoms in this study may reflect different sleep disorders, such as obstructive sleep apnea. However, stratifying for two obstructive sleep apnea risk factors (i.e., age and obesity) did not change the results from the main analyses. Third, the duration of insomnia symptoms (e.g., at least three nights a week for three consecutive months in DSM-5) is important for the insomnia diagnosis. Nevertheless, due to the way in which the questions about insomnia symptoms were asked, we were unable to determine the period of time of having these insomnia symptoms. Fourth, there may be survival bias in the current study because those who remained in the study were younger, with higher socioeconomic and health status at baseline. Fifth, it has been shown that depressive symptoms, including major depressive disorder (MDD), can influence both sleep quality and social relationships (Baglioni et al., 2011; Wakefield et al., 2020). However, the information on MDD is not included in HRS. Future studies are needed to investigate the complex interplay between loneliness, MDD, and insomnia to gain a better understanding of the mechanisms at play and inform targeted interventions. Finally, reverse causality could not be eliminated as a potential explanation for the observed associations since individuals with insomnia symptoms may suffer from greater feelings of loneliness (Griffin, Williams, Mladen, et al., 2020; Hom et al., 2020). Future research should continue disentangling the complex relationship between psychosocial factors and insomnia using both subjective and objective instruments (e.g., actigraphy, polysomnography).
5. Conclusions
In this 4-year population-based prospective cohort study in US middle-aged and older adults, loneliness was associated with difficulties initiating or maintaining sleep, early-morning awakening, nonrestorative sleep, and at least one of these insomnia symptoms. The associations were independent of social isolation, socio-demographics, lifestyle, and health factors. Individuals’ sleep may benefit from psychosocial interventions toward fostering close emotional relationships. Programs that aim to change individuals’ social and interpersonal interactions may reduce loneliness, thereby preventing the onset of insomnia symptoms with age and potentially reducing the excess burden of poor sleep.
Supplementary Material
Highlights.
Loneliness was associated with the onset of difficulties initiating or maintaining sleep, early-morning awakening, nonrestorative sleep, and any of these insomnia symptoms after adjusting for socio-demographics, lifestyle, health indicators, and social isolation.
Social isolation was not significantly associated with the onset of difficulties maintaining sleep, early-morning awakening, or at least one insomnia symptom after adjusting for health indicators.
Public health interventions aimed at fostering close emotional relationships may reduce the burden of poor sleep among middle-aged and older adults.
Acknowledgment
The Health and Retirement Study is sponsored by the National Institute on Aging (grant number U01AG009740) and is conducted by the University of Michigan. The authors thank all participants and staff for their contribution to this study.
Funding Source
This study is partially supported by the National Institutes of Health (P30AG059304, P50MD017356).
Role of the Funder/Sponsor
The sponsor has no role in the study design, methods, subject recruitment, data collection and analysis, and preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT author statement
Xiang Qi: Conceptualization, Methodology, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. Susan K. Malone: Methodology, Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing. Yaolin Pei: Methodology, Writing – original draft, Writing – review & editing, Supervision. Zheng Zhu: Methodology, Writing – original draft, Writing – review & editing, Supervision. Bei Wu: Conceptualization, Methodology, Validation, Investigation, Data curation, Writing – original draft, Writing – review & editing, Supervision, Funding acquisition.
Conflict of Interest Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability statement
The Health and Retirement Study (HRS) datasets are publicly available at the University of Michigan Institute for Social Research. Researchers may obtain the datasets after sending a data user agreement to the HRS team (https://hrs.isr.umich.edu/data-products).
References
- Aanes MM, Hetland J, Pallesen S, & Mittelmark MB (2011). Does loneliness mediate the stress-sleep quality relation? The Hordaland Health Study. International Psychogeriatrics, 23(6), 994–1002. 10.1017/S1041610211000111 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, & American Psychiatric Association (Eds.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed). American Psychiatric Association. [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, & Riemann D (2011). Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders, 135(1–3), 10–19. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Benson JA, McSorley VE, Hawkley LC, & Lauderdale DS (2021). Associations of loneliness and social isolation with actigraph and self-reported sleep quality in a national sample of older adults. Sleep, 44(1), zsaa140. 10.1093/sleep/zsaa140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun HA, Beydoun MA, Weiss J, Hossain S, Huang S, Alemu BT, & Zonderman AB (2021). Insomnia as a predictor of diagnosed memory problems: 2006–2016 Health and Retirement Study. Sleep Medicine, 80, 158–166. 10.1016/j.sleep.2021.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom HG, Ahmed I, Alessi CA, Ancoli-Israel S, Buysse DJ, Kryger MH, Phillips BA, Thorpy MJ, Vitiello MV, & Zee PC (2009). Evidence-Based Recommendations for the Assessment and Management of Sleep Disorders in Older Persons: ASSESSMENT AND MANAGEMENT OF SLEEP DISORDERS IN OLDER PERSONS. Journal of the American Geriatrics Society, 57(5), 761–789. 10.1111/j.1532-5415.2009.02220.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Cacioppo S (2018). Loneliness in the Modern Age: An Evolutionary Theory of Loneliness (ETL). In Advances in Experimental Social Psychology (Vol. 58, pp. 127–197). Elsevier. 10.1016/bs.aesp.2018.03.003 [DOI] [Google Scholar]
- Chen T-Y, & Saito Y (2021). Longitudinal effects of nocturnal insomnia symptom subtypes and nonrestorative sleep on the incidence of depression among community-dwelling older adults: Results from the Health and Retirement Study. Sleep Medicine, 79, 155–163. 10.1016/j.sleep.2021.01.003 [DOI] [PubMed] [Google Scholar]
- Cho JH-J, Olmstead R, Choi H, Carrillo C, Seeman TE, & Irwin MR (2019). Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging & Mental Health, 23(9), 1130–1138. 10.1080/13607863.2018.1481928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi H (2015). Impact of social isolation on behavioral health in elderly: Systematic review. World Journal of Psychiatry, 5(4), 432. 10.5498/wjp.v5.i4.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe CL, Domingue BW, Graf GH, Keyes KM, Kwon D, & Belsky DW (2021). Associations of Loneliness and Social Isolation with Healthspan and Lifespan in the US Health and Retirement Study. The Journals of Gerontology: Series A, glab128. 10.1093/gerona/glab128 [DOI] [PMC free article] [PubMed]
- Deng M, Qian M, Lv J, Guo C, & Yu M (2023). The association between loneliness and sleep quality among older adults: A systematic review and meta-analysis. Geriatric Nursing, 49, 94–100. 10.1016/j.gerinurse.2022.11.013 [DOI] [PubMed] [Google Scholar]
- Evans IEM, Martyr A, Collins R, Brayne C, & Clare L (2019). Social Isolation and Cognitive Function in Later Life: A Systematic Review and Meta-Analysis. Journal of Alzheimer’s Disease, 70(s1), S119–S144. 10.3233/JAD-180501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floam S, Simpson N, Nemeth E, Scott-Sutherland J, Gautam S, & Haack M (2015). Sleep characteristics as predictor variables of stress systems markers in insomnia disorder. Journal of Sleep Research, 24(3), 296–304. 10.1111/jsr.12259 [DOI] [PubMed] [Google Scholar]
- Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, & Czeisler CA (2013). The Sleep and Technology Use of Americans: Findings from the National Sleep Foundation’s 2011 Sleep in America Poll. Journal of Clinical Sleep Medicine, 09(12), 1291–1299. 10.5664/jcsm.3272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SC, Williams AB, Mladen SN, Perrin PB, Dzierzewski JM, & Rybarczyk BD (2020). Reciprocal Effects Between Loneliness and Sleep Disturbance in Older Americans. Journal of Aging and Health, 32(9), 1156–1164. 10.1177/0898264319894486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SC, Williams AB, Ravyts SG, Mladen SN, & Rybarczyk BD (2020). Loneliness and sleep: A systematic review and meta-analysis. Health Psychology Open, 7(1), 205510292091323. 10.1177/2055102920913235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Q, Zhang P, Li G, Dai H, & Shi J (2017). The association between insomnia symptoms and risk of cardio-cerebral vascular events: A meta-analysis of prospective cohort studies. European Journal of Preventive Cardiology, 24(10), 1071–1082. 10.1177/2047487317702043 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hom MA, Chu C, Rogers ML, & Joiner TE (2020). A Meta-Analysis of the Relationship Between Sleep Problems and Loneliness. Clinical Psychological Science, 8(5), 799–824. 10.1177/2167702620922969 [DOI] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Research on Aging, 26(6), 655–672. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda H, Kayashima K, Sasaki T, Kashima S, & Koyama F (2017). The relationship between sleep disturbances and depression in daytime workers: A cross-sectional structured interview survey. INDUSTRIAL HEALTH, 55(5), 455–459. 10.2486/indhealth.2017-0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins CD, Stanton B-A, Niemcryk SJ, & Rose RM (1988). A scale for the estimation of sleep problems in clinical research. Journal of Clinical Epidemiology, 41(4), 313–321. 10.1016/0895-4356(88)90138-2 [DOI] [PubMed] [Google Scholar]
- Kaufmann CN, Canham SL, Mojtabai R, Gum AM, Dautovich ND, Kohn R, & Spira AP (2013). Insomnia and Health Services Utilization in Middle-Aged and Older Adults: Results From the Health and Retirement Study. The Journals of Gerontology: Series A, 68(12), 1512–1517. 10.1093/gerona/glt050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocevska D, Lysen TS, Dotinga A, Koopman-Verhoeff ME, Luijk MPCM, Antypa N, Biermasz NR, Blokstra A, Brug J, Burk WJ, Comijs HC, Corpeleijn E, Dashti HS, de Bruin EJ, de Graaf R, Derks IPM, Dewald-Kaufmann JF, Elders PJM, Gemke RJBJ, … Tiemeier H (2020). Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta-analysis. Nature Human Behaviour, 5(1), 113–122. 10.1038/s41562-020-00965-x [DOI] [PubMed] [Google Scholar]
- Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, & Ober C (2011). Loneliness Is Associated with Sleep Fragmentation in a Communal Society. Sleep, 34(11), 1519–1526. 10.5665/sleep.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Steele SJ, Hamilton JL, Do QBP, Furbish K, Burke TA, Martinez AP, & Gerlus N (2020). Sleep and suicide: A systematic review and meta-analysis of longitudinal studies. Clinical Psychology Review, 81, 101895. 10.1016/j.cpr.2020.101895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood A, Ray M, Ward KD, Dobalian A, & Ahn S (2022). Longitudinal associations between insomnia symptoms and all-cause mortality among middle-aged and older adults: A population-based cohort study. Sleep, 45(6), zsac019. 10.1093/sleep/zsac019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh JE, & Lawlor BA (2013). Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. British Journal of Health Psychology, 18(3), 546–555. 10.1111/j.2044-8287.2012.02101.x [DOI] [PubMed] [Google Scholar]
- McHugh J, Kenny R, Lawlor B, Steptoe A, & Kee F (2017). The discrepancy between social isolation and loneliness as a clinically meaningful metric: Findings from the Irish and English longitudinal studies of ageing (TILDA and ELSA): Social asymmetry and cognitive function. International Journal of Geriatric Psychiatry, 32(6), 664–674. 10.1002/gps.4509 [DOI] [PubMed] [Google Scholar]
- McHugh J, & Lawlor B (2011). Living alone does not account for the association between loneliness and sleep in older adults: Response to Hawkley, Preacher, and Cacioppo, 2010. Health Psychology, 30(2), 135–135. 10.1037/a0022433 [DOI] [PubMed] [Google Scholar]
- Miner B, & Kryger MH (2017). Sleep in the Aging Population. Sleep Medicine Clinics, 12(1), 31–38. 10.1016/j.jsmc.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motillon-Toudic C, Walter M, Séguin M, Carrier J-D, Berrouiguet S, & Lemey C (2022). Social isolation and suicide risk: Literature review and perspectives. European Psychiatry, 65(1), e65. 10.1192/j.eurpsy.2022.2320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (Ed.). (2020). Social isolation and loneliness in older adults: Opportunitiies for the health care system the National Academies Press. [PubMed] [Google Scholar]
- Olufsen IS, Sørensen ME, & Bjorvatn B (2020). Nye diagnosekriterier for insomni og sammenhengen mellom insomni, angst og depresjon. Tidsskrift for Den norske legeforening 10.4045/tidsskr.19.0041 [DOI] [PubMed]
- Primack BA, Shensa A, Sidani JE, Whaite EO, Lin LY, Rosen D, Colditz JB, Radovic A, & Miller E (2017). Social Media Use and Perceived Social Isolation Among Young Adults in the U.S. American Journal of Preventive Medicine, 53(1), 1–8. 10.1016/j.amepre.2017.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi X, Belsky DW, Yang YC, & Wu B (2023). Association Between Types of Loneliness and Risks of Functional Disability in Older Men and Women: A Prospective Analysis. The American Journal of Geriatric Psychiatry, S1064748123002336. 10.1016/j.jagp.2023.02.046 [DOI] [PMC free article] [PubMed]
- Qi X, Ng TKS, & Wu B (2023). Sex differences in the mediating role of chronic inflammation on the association between social isolation and cognitive functioning among older adults in the United States. Psychoneuroendocrinology, 149, 106023. 10.1016/j.psyneuen.2023.106023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi X, Pei Y, Malone SK, & Wu B (2023). Social Isolation, Sleep Disturbance, and Cognitive Functioning (HRS): A Longitudinal Mediation Study. The Journals of Gerontology: Series A, glad004. 10.1093/gerona/glad004 [DOI] [PMC free article] [PubMed]
- Qi X, Pei Y, Wang K, Han S, & Wu B (2022). Social isolation, loneliness and accelerated tooth loss among Chinese older adults: A longitudinal study. Community Dentistry and Oral Epidemiology, cdoe.12727. 10.1111/cdoe.12727 [DOI] [PMC free article] [PubMed]
- Qi X, Zhang W, Wang K, Pei Y, & Wu B (2022). Social isolation and psychological well‐ being among older Chinese Americans: Does resilience mediate the association? International Journal of Geriatric Psychiatry, 37(8), gps.5791. 10.1002/gps.5791 [DOI] [PubMed] [Google Scholar]
- Roth T, Zammit G, Lankford A, Mayleben D, Stern T, Pitman V, Clark D, & Werth JL (2010). Nonrestorative Sleep as a Distinct Component of Insomnia. Sleep, 33(4), 449–458. 10.1093/sleep/33.4.449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Ryan L, Fisher G, Sonnega A, & Weir D (2017). HRS Psychosocial and Lifestyle Questionnaire 2006–2016 https://hrs.isr.umich.edu/publications/biblio/9066
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort Profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Shankar A, Demakakos P, & Wardle J (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences, 110(15), 5797–5801. 10.1073/pnas.1219686110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan TR, Lee KJ, Ryan P, & Salter AB (2017). Multiple imputation for handling missing outcome data when estimating the relative risk. BMC Medical Research Methodology, 17(1), 134. 10.1186/s12874-017-0414-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S, & Hanratty B (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart, 102(13), 1009–1016. 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield JRH, Bowe M, Kellezi B, Butcher A, & Groeger JA (2020). Longitudinal associations between family identification, loneliness, depression, and sleep quality. British Journal of Health Psychology, 25(1), 1–16. 10.1111/bjhp.12391 [DOI] [PubMed] [Google Scholar]
- Walker E, Ploubidis G, & Fancourt D (2019). Social engagement and loneliness are differentially associated with neuro-immune markers in older age: Time-varying associations from the English Longitudinal Study of Ageing. Brain, Behavior, and Immunity, 82, 224–229. 10.1016/j.bbi.2019.08.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White IR, Royston P, & Wood AM (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- Yu B, Steptoe A, Niu K, Ku P-W, & Chen L-J (2018). Prospective associations of social isolation and loneliness with poor sleep quality in older adults. Quality of Life Research, 27(3), 683–691. 10.1007/s11136-017-1752-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Health and Retirement Study (HRS) datasets are publicly available at the University of Michigan Institute for Social Research. Researchers may obtain the datasets after sending a data user agreement to the HRS team (https://hrs.isr.umich.edu/data-products).


