Abstract
PURPOSE
This study aims to clinically compare the fitness and trueness of zirconia crowns fabricated by different combinations of open CAD-CAM systems.
MATERIALS AND METHODS
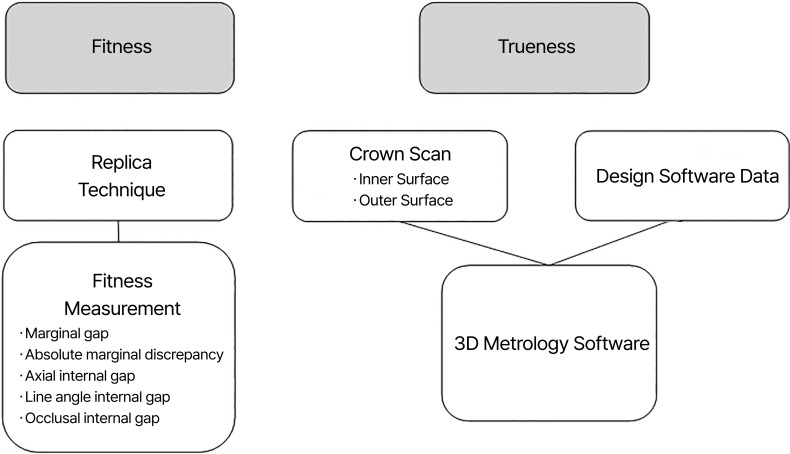
Total of 40 patients were enrolled in this study, and 9 different zirconia crowns were prepared per patient. Each crown was made through the cross-application of 3 different design software (EZIS VR, 3Shape Dental System, Exocad) with 3 different processing devices (Aegis HM, Trione Z, Motion 2). The marginal gap, absolute marginal discrepancy, internal gap(axial, line angle, occlusal) by a silicone replica technique were measured to compare the fit of the crown. The scanned inner and outer surfaces of the crowns were compared to CAD data using 3D metrology software to evaluate trueness.
RESULTS
There were significant differences in the marginal gap, absolute marginal discrepancy, axial and line angle internal gap among the groups (P < .05) in the comparison of fit. There was no statistically significant difference among the groups in terms of occlusal internal gap. The trueness ranged from 36.19 to 43.78 µm but there was no statistically significant difference within the groups (P > .05).
CONCLUSION
All 9 groups showed clinically acceptable level of marginal gaps ranging from 74.26 to 112.20 µm in terms of fit comparison. In the comparison of trueness, no significant difference within each group was spotted. Within the limitation of this study, open CAD-CAM systems used in this study can be assembled properly to fabricate zirconia crown.
Keywords: CAD-CAM, Zirconia crown, Fitness, Trueness
INTRODUCTION
Computer-aided design (CAD) and computer-aided manufacturing (CAM) systems have been broadly used for fabricating crowns and have already appeared to be a valid alternative to traditional prosthetic fabrication methods. All CAD-CAM systems are composed of three elements: scanners, design software and processing devices.1 CAD-CAM systems are divided into closed and open types depending on their compatibility with scanners, design software, or processing devices from other manufacturers. As closed CAD-CAM systems rely on their own data format for fabrication, the system can only collaborate with their specifically provided scanner, design software, and processing devices. On the other hand, open CAD-CAM systems, which use the Stereolithography (STL) format, can be combined with other open systems, which provide a larger range of products to choose from. Therefore, the open systems can provide higher flexibility and compatibility compared to closed systems.
As CAD-CAM products of various manufacturers are released in the dental field, comparative studies on closed and open CAD-CAM systems were being carried out.2,3,4 Jang et al.2 compared three-unit bridges fabricated by combining open type Exocad (Exocad, Darmstadt, Germany) and EZIS HM (DDS, Seoul, Korea) to those fabricated by representative closed type. The open type showed lower marginal and internal gaps than those of the closed type. In the study of Kricheldorf et al.,3 the closed CAD-CAM system group had higher marginal gap compared to the open system group using Exocad and DM5 (Tecnodrill, Nova Hamburgo, Rio Grande do Sul, Brazil). Alqahtani5 reported the group using 3Shape Dental System (3Shape, Copenhagen, Denmark) with Wieland Zenotec (Wieland Dental, Pforzheim, Germany) showed lower marginal gap compared to the group using conventional lost wax technique and the closed system.
Outcome of CAD-CAM crown can be mainly influenced by CAD-CAM system used. The success of CAD-CAM crown is determined by several factors: esthetic aspect, fracture resistance, and marginal adaptation.5 Marginal and internal fit is significant in assuring the success of crowns,6,7 and can be affected by cement space, marginal design, cement film thickness, seating force, material type, and CAD-CAM system used.8,9,10 Inadequate marginal fit of a crown may increase microleakage and plaque accumulation, which consequently causes caries and periodontal diseases.11 In the conventional crown, a cement space of 25 - 50 µm is required to obtain an ideal marginal fit.12,13 Considering life expectancy of crowns, it has been reported that a marginal gap of 100 - 200 µm is clinically acceptable.14,15 Appropriate internal gap is another crucial factor dedicating to the success of crown. An excessive internal gap may weaken the fracture strength of the crown.16 Moreover, an insufficient internal gap may cause the incomplete placement of the crown.
CAD-CAM crowns are usually fabricated by processing CAD-CAM blanks.17 The milling process can influence marginal and internal gap and therefore should be precise.18 In order to assess the accuracy of the milling process, the surface of the final crown should be compared to the CAD data.2
Various materials, such as zirconia, composite resin, glass ceramic, cobalt chrome and hybrid biomaterials, may be used in the milling process.22,23 Primarily, zirconia prostheses, which is a crystalline dioxide of zirconium, showed esthetically similar outcomes as natural teeth and have been utilized in the anterior region as crowns or implant abutments.20 Zirconia has high flexural strength of 900 - 1200 MPa and compressive strength of 2000 MPa, which is similar to the mechanical properties of stainless steel,21 while presintered zirconia blocks can be milled easily. Thus, zirconia crowns fabricated using CAD-CAM systems have been the most widely used. Furthermore, several studies reported that marginal and internal fit of CAD-CAM fabricated zirconia crowns resided within a clinically acceptable range.21,22
The majority of studies that compared open type CAD-CAM systems to either a conventional method or closed type systems was in vitro evaluations or used a small number of systems. In addition, there have been few clinical studies comparing the fit and trueness of zirconia crowns fabricated by various different open type CAD-CAM systems. Therefore, this present study was conducted to clinically evaluate the fit and trueness of zirconia crowns fabricated by cross application of the commercially available open systems including 3 design software and 3 processing devices in patients.
MATERIALS AND METHODS
The present study was conducted from May 2019 to December 2020 at Pusan National University Dental Hospital and was approved by the Institutional Review Board of Pusan National University Dental Hospital (IRB No. PNUDH-2019-017-MD). Patients who were offered a single full veneer crown prosthetic treatment were given an explanation on the purpose, and the study only enrolled patients who expressed voluntary consent to participation. Patients who had remaining healthy tooth structures and could be treated with prosthetic treatment were included. A total of 40 patients (5 males, 24 females; mean age, 40 years) were screened and enrolled in this study. The tooth distribution of 40 patients were 4 maxillary incisors, 6 maxillary premolars, 7 mandibular premolars, 9 maxillary molars, and 14 mandibular molars (Table 1).
Table 1. Locations of abutment teeth used in this study.
| Incisor | Premolar | Molar | Total | |
|---|---|---|---|---|
| Maxilla | 4 | 6 | 9 | 19 |
| Mandible | 0 | 7 | 14 | 21 |
| Total | 4 | 13 | 23 | 40 |
The flow chart of the zirconia crown fabrication is represented in Figure 1. First, tooth preparation was performed for the fabrication of zirconia crowns. A skilled prosthodontist prepared the abutment teeth following the recommended zirconia prep guidelines. A deep chamfer margin was formed, and all line angles were rounded off.
Fig. 1. Flow chart of zirconia crown fabrication in this study.
A double cord technique was performed using gingival retraction cords (Ultrapak; Ultradent, South Jordan, UT, USA) for gingival displacement to clearly scan the abutment margin. An intraoral scanner (i500; Medit, Seoul, Korea) was used to scan the abutment teeth and record the occlusion. To design a zirconia crown, the scanned file was transferred to respective CAD software: EZIS VR (DDS, Seoul, Korea), 3Shape Dental System (3Shape, Copenhagen, Denmark), and Exocad (Exocad, Darmstadt, Germany) (Table 2). Corresponding to the recommendation of a previous study, the cement space was uniformly assigned as 40 µm using a recommended method provided by the manufacturer.23
Table 2. Parameter options for different design software.
| Design software (Manufacturer) | EZIS VR (DDS, Korea) | 3Shape Dental System (3shape, Denmark) | Exocad (Exocad, Germany) |
|---|---|---|---|
| Space | ○ | ○ | ○ |
| Proximal Contact | ○ | ○ | ○ |
| Occlusal Contact | ○ | ○ | ○ |
| Minimum Thickness | ○ | ○ | ○ |
| Margin Cement Thickness | ○ | ○ | ○ |
| Internal Cement Thickness | ○ | ○ | ○ |
| Additional Occlusal Space | - | ○ | ○ |
| Additional Axial Space | - | ○ | ○ |
| Margin Space Length | ○ | ○ | ○ |
| Tool Compensation Radius | ○ | ○ | ○ |
In this study, the cement space was set to 40 µm equally.
-: No adjustable option
Zirconia blanks (Luxen; Dentalmax, Seoul, Korea) were respectively processed using milling machines: Aegis HM (DDS, Seoul, Korea), Trione Z (Dio, Busan, Korea), Ceramil motion 2 (Amann Girrbach, Pforzheim, Germany) (Table 3). The milled zirconia crowns were sintered in the sintering machine (DuoTron Pro; ADD-IN, Yang-ju, Korea) according to the manufacturers’ instructions. All crowns were designed and fabricated by a single trained dental technician (Fig. 2). A total of 360 zirconia crowns (9 crowns per each patient) were fabricated and divided into 9 groups (Table 4).
Table 3. Operating conditions of processing devices used in this study.
| Processing Device | Axis (Number of Spindle) | Spindle Speed(max) | Processing Environment | Accuracy Presented by Manufacturer | Machine Tool | Manufacturer |
|---|---|---|---|---|---|---|
| Aegis HM | 4 (2) | 63,000 rpm | Wet | 10 µm | Grinding with diamond bur | DDS, Korea |
| Trione Z | 5 (1) | 25,000 rpm | Dry | Unknown | Grinding with diamond bur | Dio, Korea |
| Motion 2 | 5 (1) | 100,000 rpm | Dry | Unknown | Grinding with diamond bur | Amann Girrbach, Germany |
Fig. 2. Fabricated zirconia crowns of each group (mandibular second premolar).
EZIS/Ae: EZIS VR/Aegis HM, EZIS/Tri: EZIS VR/Trione Z, EZIS/Mo: EZIS VR/Ceramil motion 2, 3Shape/Ae: 3Shape Dental System/Aegis HM, 3Shape/Tri: 3Shape Dental System/Trione Z, 3Shape/Mo: 3Shape Dental System/Ceramil motion 2, Exocad/Ae: Exocad/Aegis HM, Exocad/Tri: Exocad/Trione Z, Exocad/Mo: Exocad/Ceramil motion 2.
Table 4. Experimental groups investigated in this study.
| Groups | CAD software | Milling machines | n |
|---|---|---|---|
| EZIS/Ae | EZIS VR | Aegis HM | 40 |
| EZIS/Tri | Trione Z | 40 | |
| EZIS/Mo | Motion 2 | 40 | |
| 3Shape/Ae | 3Shape Dental System | Aegis HM | 40 |
| 3Shape/Tri | Trione Z | 40 | |
| 3Shape/Mo | Motion 2 | 40 | |
| Exocad/Ae | Exocad | Aegis HM | 40 |
| Exocad/Tri | Trione Z | 40 | |
| Exocad/Mo | Motion 2 | 40 |
EZIS/Ae: EZIS VR/Aegis HM, EZIS/Tri: EZIS VR/Trione Z, EZIS/Mo: EZIS VR/Ceramil motion 2, 3Shape/Ae: 3Shape Dental System/Aegis HM, 3Shape/Tri: 3Shape Dental System/Trione Z, 3Shape/Mo: 3Shape Dental System/Ceramil motion 2, Exocad/Ae: Exocad/Aegis HM, Exocad/Tri: Exocad/Trione Z, Exocad/Mo: Exocad/Ceramil motion 2.
The flow chart of the zirconia crown evaluation is represented in Figure 3.
Fig. 3. Flow chart of the zirconia crown evaluation.
Prior to the seating of zirconia crown, a prosthodontist confirmed that all the zirconia crowns of each group were completely seated to the teeth by adjusting the proximal contact of the zirconia crowns (Fig. 4). To prepare the fit evaluation using replica technique, each crown was filled by Fit Checker Advanced (GC, Tokyo, Japan) and placed on the abutment by applying constant finger pressure for 1 min until the Fit Checker was polymerized. The crown was carefully removed from the abutment, and then a polyvinylsiloxane impression material (Imprint II; 3M, St. Paul, MN, USA) was injected into the Fit Checker applied inner surface of the crown for the purpose of stabilizing the film layer and preventing deformation. A total of 360 polyvinylsiloxane replicas were made using this method.
Fig. 4. (A, B) Right and occlusal views of final zirconia crown (mandibular right first molar), (C) Periapical radiograph.
The collected silicone replicas were embedded into a 3D printed jig and polyvinylsiloxane impression material (Imprint II; 3M, St. Paul, MN, USA) was applied for exact cutting (Fig. 5, Fig. 6).24 The replica was sectioned in bucco-lingual and mesio-distal directions (Fig. 6E). After taking the image of the specimen at 100× magnification using a camera-equipped microscope (Olympus BX 51; Olympus, Tokyo, Japan), the film thicknesses at the reference points (9 points on bucco-lingual side, 9 points on mesio-distal side) were measured with an image analysis software (I-Solution; IMT i-solution, Daejeon, Korea).
Fig. 5. (A) Prepared mandibular right first molar, (B) The zirconia crown was filled by Fit Checker Advanced (GC, Tokyo, Japan) and placed on the abutment, (C, D) The zirconia crown and Fit Checker film was carefully removed from the abutment, (E) A vinyl polysiloxane impression material (Imprint II; 3M, St. Paul, MN, USA) was injected into the Fit Checker applied inner surface of the crown.
Fig. 6. (A, B) 3D printed jig for silicone replica technique, (C) Blue-colored Fit Checker and yellow-colored vinyl polysiloxane impression material separated from zirconia crown are buried in the jig, (D) Filling remaining space with green-colored vinyl polysiloxane impression material, (E) Bucco-lingual and mesio-distal cutting of replica.
According to the classification of Holmes et al.,25 the fit of CAD-CAM zirconia crown was measured by the absolute marginal discrepancy, marginal gaps, and internal gaps (Fig. 7). The absolute marginal discrepancy (AMD) is the vertical distance starting from the edge of the tooth margin to the edge of the crown margin (Fig. 7A, a, I, i). The marginal gap (MG) is the vertical distance from the edge of the tooth margin to the inner surface of the crown (Fig. 7B, b, H, h). The internal gap is the vertical distance from the tooth surface to the inner surface of the crown. To measure the internal gap, the axial internal gap, line angle internal gap, and occlusal internal gap were measured in this study. The axial internal gap (AG) was measured at the center of the axial wall (Fig. 7C, c, G, g), the line angle internal gap (LG) was measured on the line angle transitioning from the occlusal surface to the axial wall (Fig. 7D, d, F, f), and the occlusal internal gap (OG) was measured at the center of the occlusal surface (Fig. 7E, e). All the measurements were performed by blinded single investigator, and were repeated 3 times.
Fig. 7. Reference points to measure the thickness of the Fit Checker.
[A, a, I, i: Absolute marginal discrepancy (AMD); B, b, H, h: Marginal gap (MG); C, c, G, g: Axial internal gap (AG); D, d, F, f: Line angle internal gap (LG); E: Occlusal internal gap (OG)].
The inner and outer surfaces of zirconia crown were scanned with a digital scanner (Trios3; 3shape, Copenhagen, Denmark). The design software data and scan data were compared using a 3D metrology software (Geomagic Control X; Geomagic, Stuttgart, Germany). The trueness in an optimal alignment was analyzed by obtaining root mean square (RMS) values in the order of the initial alignment of design data and scan data. The formula to obtain the RMS value used in this study is as follows.26
X1,i: position of measurement point No. i in the CAD reference model
X2,i: position of measurement point No. i in the CAD test model
n: number of all points measured in each analysis
According to the International Organization for Standard (ISO) 12836, the RMS values mean a higher degree of 3D agreement as the value approaches zero.27 A color difference map with a specified range of 100 µm (20 color segments) was presented to show a 3D comparison. The red zone (10 - 100 µm) indicates a positive error. The blue zone (-10 to -100 µm) represents a negative error. The green zone (± 10 µm) shows precise machining accuracy.
SPSS software (version 25.0; SPSS, Chicago, IL, USA) was used for the statistical analyses. Normality and homogeneity of variance were verified with the Shapiro-Wilk test. Since fit and trueness values did not show normality in the normality test, Kruskal Wallis test (α = .05) was used to assess the statistical significance. For post hoc analyses, the Mann-Whitney U test was used with the Bonferroni correction for multiple comparisons (α = .05/3 = .017).
RESULTS
The following fit results were obtained by measuring the Fit Checker film thickness of the reference point on the specimen (Fig. 8).
Fig. 8. Bucco-lingual cross-section view of replica specimen at measuring points. [Magnification: × 100; (A) Absolute marginal discrepancy (AMD) and Marginal gap (MG), (B) Axial internal gap (AG), (C) Line angle internal gap (LG), (D) Occlusal internal gap (OG)].
When design software are compared to one another by processing devices, the lowest marginal gap (µm) was shown in the Ezis/Tri (74.26 ± 68.68), while the highest was in the Exocad/Ae (112.20 ± 68.96) (Table 5). There was a statistically significant difference between the EZIS/Ae (84.58 ± 67.35) and Exocad/Ae (112.20 ± 68.96), EZIS/Tri (74.26 ± 68.68) and 3Shape/Tri (108.11 ± 78.52), and EZIS/Tri (74.26 ± 68.68) and Exocad/Tri (102.12 ± 81.36), respectively (P < .017).
Table 5. Means and standard deviations of marginal gap (Comparison of processing devices by design software, µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 84.58 ± 67.35a | 74.26 ± 68.68c,d | 87.20 ± 78.06e |
| 3Shape | 105.84 ± 74.13b | 108.11 ± 78.52d | 104.94 ± 79.45f | |
| Exocad | 112.20 ± 68.96a | 102.12 ± 81.36c | 98.85 ± 81.16g | |
a, b, c, d, e, f, gSame lowercase letters indicate significant difference at P < .017 in a column.
There was no statistically significant difference between the groups (P > .05) when processing devices are compared to each other by design software (Table 6).
Table 6. Means and standard deviations of marginal gap (Comparison of design software by processing devices, µm, n = 40).
| Design Software | ||||
|---|---|---|---|---|
| EZIS VR | 3Shape Dental System | Exocad | ||
| Processing Devices | Aegis HM | 84.58 ± 67.35a | 105.84 ± 74.13a | 112.20 ± 68.96a |
| Trione Z | 74.26 ± 68.68a | 108.11 ± 78.52a | 102.12 ± 81.36a | |
| Motion 2 | 87.20 ± 78.06a | 104.94 ± 79.45a | 98.85 ± 81.16a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
When design software are compared to each other by processing devices, the lowest mean absolute marginal discrepancy (µm) was in the Ezis/Ae (120.31 ± 68.14), while the highest was in the Exocad/Tri (184.85 ± 79.57) (Table 7). There was a statistically significant difference between the EZIS/Ae (120.31 ± 68.14) and the Exocad/Ae (160.18 ± 67.18), EZIS/Tri (126.65 ± 83.93) and 3Shape/Tri (166.68 ± 76.01), EZIS/Tri (126.65 ± 83.93) and Exocad/Tri (184.85 ± 79.57), and EZIS/Mo (150.66 ± 91.42) and 3Shape/Mo (174.42± 68.22), respectively (P < .017).
Table 7. Means and standard deviations of absolute marginal discrepancy (Comparison of processing devices by design software, µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 120.31 ± 68.14a | 126.65 ± 83.93c,d | 150.66 ± 91.42e |
| 3Shape | 142.02 ± 69.28b | 166.68 ± 76.01d | 174.42 ± 68.22e | |
| Exocad | 160.18 ± 67.18a | 184.85 ± 79.57c | 172.69 ± 75.42f | |
a, b, c, d, e, fSame lowercase letters indicate significant difference at P < .017 in a column.
When processing devices are compared to each other by design software (Table 8), there was no statistically significant difference between the groups (P > .05).
Table 8. Means and standard deviations of absolute marginal discrepancy (Comparison of design software by processing devices, µm, n = 40).
| Design Software | ||||
|---|---|---|---|---|
| EZIS VR | 3Shape Dental System | Exocad | ||
| Processing Devices | Aegis HM | 120.31 ± 68.14a | 142.02 ± 69.28a | 160.18 ± 67.18a |
| Trione Z | 126.65 ± 83.93a | 166.68 ± 76.01a | 184.85 ± 79.57a | |
| Motion 2 | 150.66 ± 91.42a | 174.42 ± 68.22a | 172.69 ± 75.42a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
When design software are compared to each other by processing devices, the lowest axial internal gap (µm) was in the Exocad/Ae (41.26 ± 33.81), while the highest was in the EZIS/Ae (100.31 ± 65.03) (Table 9). There was a statistically significant difference between the EZIS/Ae (100.31 ± 65.03) and 3Shape/Ae (53.12 ± 43.84), EZIS/Ae (100.30 ± 65.03) and Exocad/Ae (41.26 ± 33.81), 3Shape/Ae (53.12 ± 43.84) and Exocad/Ae (41.26 ± 33.81), EZIS/Tri (97.20 ± 66.79) and 3Shape/Tri (54.13 ± 45.69), EZIS/Tri (97.20 ± 66.79) and Exocad/Tri (54.61 ± 45.64), EZIS/Mo (99.49 ± 69.05) and 3Shape/Mo (51.12 ± 49.58), and EZIS/Mo (99.49 ± 69.05) and Exocad/Mo (48.49 ± 52.28), respectively (P < .017).
Table 9. Means and standard deviations of axial internal gap (Comparison of processing devices by design software, µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 100.31 ± 65.03a,b | 97.20 ± 66.79d,e | 99.49 ± 69.05f,g |
| 3Shape | 53.12 ± 43.84a,c | 54.13 ± 45.69d | 51.12 ± 49.58f | |
| Exocad | 41.26 ± 33.81b,c | 54.61 ± 45.64e | 48.49 ± 52.28g | |
a, b, c, d, e, f, gSame lowercase letters indicate significant difference at P < .017 in a column.
When processing devices are compared to each other by design software (Table 10), there was no statistically significant difference between the groups (P > .05).
Table 10. Means and standard deviations of axial internal gap (Comparison of design software by processing devices, µm, n = 40).
| Design Software | ||||
|---|---|---|---|---|
| EZIS VR | 3Shape Dental System | Exocad | ||
| Processing Devices | Aegis HM | 100.31 ± 65.03a | 53.12 ± 43.84a | 41.26 ± 33.81a |
| Trione Z | 97.20 ± 66.79a | 54.13 ± 45.69a | 54.61 ± 45.64a | |
| Motion 2 | 99.49 ± 69.05a | 51.12 ± 49.58a | 48.49 ± 52.28a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
When design software are compared to each other by processing devices, the lowest line angle internal gap (µm) was in the EZIS/Ae (83.05 ± 65.14), while the highest was in the 3Shape/Mo (141.36 ± 79.69) (Table 11). There was a statistically significant difference between the EZIS/Ae (83.05 ± 65.14) and 3Shape/Ae (103.47 ± 69.49), EZIS/Ae (83.05 ± 65.14) and Exocad/Ae (110.87 ± 77.89), EZIS/Tri (98.82 ± 73.00) and 3Shape/Tri (123.84 ± 73.91), EZIS/Tri (98.82 ± 73.00) and Exocad/Tri (124.41 ± 78.28), and EZIS/Mo (117.64 ± 76.53) and 3Shape/Mo (141.36 ± 79.69), respectively (P < .017).
Table 11. Means and standard deviations of line angle internal gap (Comparison of processing devices by design software, µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 83.05 ± 65.14a,b | 98.82 ± 73.00c,d | 117.64 ± 76.53e |
| 3Shape | 103.47 ± 69.49a | 123.84 ± 73.91c | 141.36 ± 79.69e | |
| Exocad | 110.87 ± 77.89b | 124.41 ± 78.28d | 134.12 ± 80.83f | |
a, b, c, d, e, fSame lowercase letters indicate significant difference at P < .017 in a column.
When processing devices are compared to each other by design software (Table 12), there was a statistically significant difference between the Aegis/EZ (83.05 ± 65.14) and Motion/EZ (117.64 ± 76.53), Aegis/3S (103.47 ± 69.49) and Motion/3S (141.36 ± 79.69), respectively (P < .017).
Table 12. Means and standard deviations of line angle internal gap (Comparison of design software by processing devices, µm, n = 40).
| Design Software | ||||
|---|---|---|---|---|
| EZIS VR | 3Shape Dental System | Exocad | ||
| Processing Devices | Aegis HM | 83.05 ± 65.14a | 103.47 ± 69.49c | 110.87 ± 77.89e |
| Trione Z | 98.82 ± 73.0b | 123.84 ± 73.91d | 124.41 ± 78.28f | |
| Motion 2 | 117.64 ± 76.53a | 141.36 ± 79.69c | 134.12 ± 80.83g | |
a, b, c, d, e, f, gSame lowercase letters indicate significant difference at P < .017 in a column.
When design software are compared to each other by processing devices, the occlusal internal gap results (µm) of each group were as follows (Table 13): EZIS/Ae (90.32 ± 64.49), 3Shape/Ae (103.99 ± 65.09), Exocad/Ae (113.97 ± 87.76), EZIS/Tri (117.33 ± 85.00), 3Shape/Tri (133.78 ± 91.47), Exocad/Tri (142.09 ± 79.70), EZIS/Mo (122.62 ± 77.08), 3Shape/Mo (143.99 ± 84.89), and Exocad/Mo (144.17 ± 81.30). There was no statistically significant difference among the groups (P > .05).
Table 13. Means and standard deviations of occlusal internal gap (Comparison of processing devices by design software, µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 90.32 ± 64.49a | 117.33 ± 85.00a | 122.62 ± 77.08a |
| 3Shape | 103.99 ± 65.09a | 133.78 ± 91.47a | 143.99 ± 84.89a | |
| Exocad | 113.97 ± 87.76a | 142.09 ± 79.70a | 144.17 ± 81.30a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
When processing devices are compared to each other by design software (Table 14), there was no statistically significant difference between the groups (P > .05).
Table 14. Means and standard deviations of occlusal internal gap (Comparison of design software by processing devices, µm, n = 40).
| Design Software | ||||
|---|---|---|---|---|
| EZIS VR | 3Shape Dental System | Exocad | ||
| Processing Devices | Aegis HM | 90.32 ± 64.49a | 103.99 ± 65.09a | 113.97 ± 87.76a |
| Trione Z | 117.33 ± 85.00a | 133.78 ± 91.47a | 142.09 ± 79.70a | |
| Motion 2 | 122.62 ± 77.08a | 143.99 ± 84.89a | 144.17 ± 81.30a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
The means and standard deviations of trueness results (µm) are shown in Table 15 and Figure 9: EZIS/Ae (39.68 ± 7.28), 3Shape/Ae (43.78 ± 7.80), Exocad/Ae (41.73 ± 6.89), EZIS/Tri (39.20 ± 9.52), 3Shape/Tri (42.00 ± 25.75), Exocad/Tri (37.67 ± 7.76), EZIS/Mo (36.19 ± 7.18), 3Shape/Mo (37.15 ± 8.26), and Exocad/Mo (36.79 ± 6.37). There was no significant statistical difference among the groups (P > .05).
Table 15. Means and standard deviations of RMS value results (µm, n = 40).
| Processing Devices | ||||
|---|---|---|---|---|
| Aegis HM | Trione Z | Motion 2 | ||
| Design Software | EZIS | 39.68 ± 7.28a | 39.20 ± 9.52a | 36.19 ± 7.18a |
| 3Shape | 43.78 ± 7.80a | 42.00 ± 25.75a | 37.15 ± 8.26a | |
| Exocad | 41.73 ± 6.89a | 37.67 ± 7.76a | 36.79 ± 6.37a | |
aSame lowercase letter means no significant difference in the columns (P > .05).
Fig. 9. Comparison of the 3D color difference map of trueness. The deviation range is color coded from -100 µm (blue) to +100 µm (red). A negative deviation (blue) indicates more removal of block during the milling process, while a positive deviation (red) indicates less removal of block compared to the digital-calculated crown dimensions. (A) outer surfaces of the crowns. (B) inner surfaces of the crowns.
DISCUSSION
As the CAD-CAM system evolves, the results with CAD-CAM are becoming more precise,28 and systems have evolved to be more compatible with those of other manufacturers. Numerous different open CAD-CAM systems are being released. Meanwhile, studies comparing them are insufficient. Thus, this study aims to comprehensively view the fit including the marginal gap and trueness through cross application of three different design software and processing devices.
In this study, software which are commonly used in dental clinics and laboratories were selected.3,4 Domestic design software developed and used relatively recently was also adopted to be compared with existing products in the present study.10 In terms of the milling machine selection, one of the machine (Motion 2) commonly used was selected and a domestic machine (Trione Z) was selected as a comparison. Since the two milling machines both were 5-axis, another newly developed machine (Aegis HM) was added to compare with those with 4-axis.
In this study, the fit of nine different groups of crowns were compared through a replica technique. There are basically four methods of measuring marginal fitness: direct view, cross-sectional, impression technique, and explorer and visual examination.29 The replica technique has been used positively in measuring fit as it uses materials with improved precision.30 When considering the preparation of abutment teeth, there was a study on the effect of margin shapes on the fit of the crown.31,32 Pera et al.31 measured the marginal fit according to the shape of the margin and the gap size increased accordingly in the order of chamfer margin, 50° shoulder margin, and 90° shoulder margin. Koo et al.32 reported that the margin gap of 90° shoulder margin was larger than those of chamfer and 130° shoulder margin. Therefore, in this study, abutment preparation was performed with a deep chamfer margin. A cement space of 40 µm of all the design software was established, as Mously et al.23 recommended a spacer thickness of 30 - 60 µm when fabricating ceramic crowns with CAD-CAM.
The fit evaluation results of this study showed that the overall marginal gap values were 74.26 - 112.20 µm. Current study reported that CAD-CAM systems achieved marginal gaps which were below 80 µm.33 Although there have been arguments regarding the clinically acceptable marginal gap, a number of researches have accepted the marginal gap of 120 µm as described by McLean and von Fraunhofer.34,35,36 Thus, all the marginal gaps in this study fit the clinically acceptable level. 9 groups of zirconia crowns had appropriate marginal gap. However, the standard deviation of fit including marginal gap tended to be large when compared with other studies. The present study was conducted in a clinical environment, being influenced by varying parameters in the process of tooth preparation, including saliva, bleeding, finish lines, limited access, and their effects on the impression techniques.4 Therefore, chronic and uncontrolled medical history was controlled at the patient level to obtain unaffected data from various parameters. In addition, the optimal marginal gap was obtained by applying the double cord technique to minimize the effects of bleeding, saliva, and gingiva. The definitive zirconia restoration was controlled to have the same cement space by only one skilled dental technician. Seating force is another important factor influencing marginal fit.37,38 It is difficult to apply such force with finger pressure, which is thought to be one of the causes explaining the large standard deviation compared to previous studies.
The gap of CAD-CAM fabricated crowns is wider in the internal areas than at the marginal region in this study, as in a number of previous studies.39,40 Edges of the prepared tooth may appear to be slightly rounded on the design software, which may cause premature contacts. To prevent this, a spacer parameter of the design software or adjustment by the technician should take place, and this may lead to larger internal gaps.41 If there is a structure smaller than the diameter of the bur on the milling machine, larger amount than necessary will be removed, which may be the cause of wider internal gaps.17
In this study, there were also differences in the values according to the reference points of the internal gap. The occlusal internal gap (90.32 - 144.17 µm) tended to be larger than the axial internal gap (41.26 - 100.41 µm). This suggests that narrow axial internal gap prevents Fit Checker or cement escape at the margin of the crown and results in poor seating and a thick occlusal internal gap.16 Differences in the functions of design software may have caused differences in the internal gap of crown.42
Trueness, explaining the closeness between a measurement value and the true value, is used to evaluate accuracy.43 The milling device accuracy and the sintering shrinkage compensation can influence the trueness of the crowns.44 Previous studies reported that five-axis milling machine showed excellence in trueness compared to the 4-axis milling machine,45,46 but no significant difference in trueness according to the number of axes of the milling machine was spotted in the present study. The results reveal that the open type design programs and processing devices used in this study have compatibility with other manufacturers’ products.
Studies discussing whether prostheses fabricated with open CAD-CAM systems are clinically acceptable have been previously reported. Ben-Izhack et al.47 reported a prosthetic marginal gap of 38.4 ± 4.354 µm when the Exocad design software and CEREC inLab MC XL processing device (Dentsply Sirona, Milford, DE, USA) were used in combination. According to Jang et al.,2 the prosthesis fabricated with Exocad design software and EZIS HM showed a clinically acceptable marginal fit of less than 120 µm (113 ± 62.3 µm). The crowns fabricated with the 9 groups of open type systems tested in this study also showed a clinically acceptable marginal gap (74.26 - 112.20 µm).
Unlike comparing design software by processing devices, when processing devices are compared to each other by design software, the statistically significant difference was less in fit values. This may support the fact that differences in the fit depending on the choice of processing device do not stand out and is in line with the trueness results of the present study.
It was not possible to target the same tooth due to the limitations of the clinical study. Therefore, by setting the number of patient to 40, we tried to minimize the error. Further studies on the length of the prosthesis or area of the edentulous part are required,48 and a comparative study using a new measurement method seems to be necessary.49 Follow-up studies using various materials are also needed.10 The fit and trueness of the zirconia crowns fabricated by cross application of open CAD-CAM systems were compared in this study. All the different zirconia crowns showed clinically acceptable trueness and fit in a single tooth restoration. However, as new CAD-CAM systems are being released in the dental field,50 continuous follow-up studies on newly released open systems are necessary.
CONCLUSION
In this study, there was no problematic combination of open CAD-CAM systems. Within the limitation of this study, all nine combinations of open CAD-CAM systems are clinically acceptable for fabricating zirconia crowns.
Footnotes
This work was supported by the Industrial Strategic Technology Development Program (No. 10062635) and funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea).
References
- 1.Beuer F, Schweiger J, Edelhoff D. Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J. 2008;204:505–511. doi: 10.1038/sj.bdj.2008.350. [DOI] [PubMed] [Google Scholar]
- 2.Jang D, Son K, Lee KB. A comparative study of the fitness and trueness of a three-unit fixed dental prosthesis fabricated using two digital workflows. Appl Sci. 2019;9:2778 [Google Scholar]
- 3.Kricheldorf F, Bueno CRS, Amaral WDS, Junior JFS, Filho HN. Analysis of vertical marginal discrepancy in feldspathic porcelain crowns manufactured with different CAD/CAM systems: Closed and open. Eur J Dent. 2018;12:123–128. doi: 10.4103/ejd.ejd_368_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alqahtani F. Marginal fit of all-ceramic crowns fabricated using two extraoral CAD/CAM systems in comparison with the conventional technique. Clin Cosmet Investig Dent. 2017;9:13–18. doi: 10.2147/CCIDE.S130856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunter AJ, Hunter AR. Gingival margins for crowns: a review and discussion. Part II: Discrepancies and configurations. J Prosthet Dent. 1990;64:636–642. doi: 10.1016/0022-3913(90)90286-l. [DOI] [PubMed] [Google Scholar]
- 6.Valderrama S, Van Roekel N, Andersson M, Goodacre CJ, Munoz CA. A comparison of the marginal and internal adaptation of titanium and gold-platinum-palladium metal ceramic crowns. Int J Prosthodont. 1995;8:29–37. [PubMed] [Google Scholar]
- 7.Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991;65:357–364. doi: 10.1016/0022-3913(91)90225-l. [DOI] [PubMed] [Google Scholar]
- 8.Wang CJ, Millstein PL, Nathanson D. Effects of cement, cement space, marginal design, seating aid materials, and seating force on crown cementation. J Prosthet Dent. 1992;67:786–790. doi: 10.1016/0022-3913(92)90583-v. [DOI] [PubMed] [Google Scholar]
- 9.Piemjai M. Effect of seating force, margin design, and cement on marginal seal and retention of complete metal crowns. Int J Prosthodont. 2001;14:412–416. [PubMed] [Google Scholar]
- 10.Ahn JJ, Bae EB, Lee JJ, Choi JW, Jeon YC, Jeong CM, Yun MJ, Lee SH, Lee KB, Huh JB. Clinical evaluation of the fit of lithium disilicate crowns fabricated with three different CAD/CAM systems. J Prosthet Dent. 2022;127:239–247. doi: 10.1016/j.prosdent.2020.06.031. [DOI] [PubMed] [Google Scholar]
- 11.Björn AL, Björn H, Grkovic B. Marginal fit of restorations and its relation to periodontal bone level. II. Crowns. Odontol Revy. 1970;21:337–346. [PubMed] [Google Scholar]
- 12.Paffenbarger GC, Beall JR. American dental association specification No. 8 for dental zinc phosphate cement. J American Dent Assoc Dent Cosmos. 1937;24:2019–2023. [Google Scholar]
- 13.Sorensen SE, Larsen IB, Jörgensen KD. Gingival and alveolar bone reaction to marginal fit of subgingival crown margins. Scand J Dent Res. 1986;94:109–114. doi: 10.1111/j.1600-0722.1986.tb01373.x. [DOI] [PubMed] [Google Scholar]
- 14.McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971;131:107–111. doi: 10.1038/sj.bdj.4802708. [DOI] [PubMed] [Google Scholar]
- 15.Kydd WL, Nicholls JI, Harrington G, Freeman M. Marginal leakage of cast gold crowns luted with zinc phosphate cement: an in vivo study. J Prosthet Dent. 1996;75:9–13. doi: 10.1016/s0022-3913(96)90411-4. [DOI] [PubMed] [Google Scholar]
- 16.Schriwer C, Skjold A, Gjerdet NR, Øilo M. Monolithic zirconia dental crowns. Internal fit, margin quality, fracture mode and load at fracture. Dent Mater. 2017;33:1012–1020. doi: 10.1016/j.dental.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Tinschert J, Natt G, Hassenpflug S, Spiekermann H. Status of current CAD/CAM technology in dental medicine. Int J Comput Dent. 2004;7:25–45. [PubMed] [Google Scholar]
- 18.Lee KB, Park CW, Kim KH, Kwon TY. Marginal and internal fit of all-ceramic crowns fabricated with two different CAD/CAM systems. Dent Mater J. 2008;27:422–426. doi: 10.4012/dmj.27.422. [DOI] [PubMed] [Google Scholar]
- 19.Zimmermann M, Mehl A, Reich S. New CAD/CAM materials and blocks for chairside procedures. Int J Comput Dent. 2013;16:173–181. [PubMed] [Google Scholar]
- 20.Naveau A, Rignon-Bret C, Wulfman C. Zirconia abutments in the anterior region: A systematic review of mechanical and esthetic outcomes. J Prosthet Dent. 2019;121:775–781. doi: 10.1016/j.prosdent.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Deng Y, Lawn BR, Lloyd IK. Characterization of damage modes in dental ceramic bilayer structures. J Biomed Mater Res. 2002;63:137–145. doi: 10.1002/jbm.10091. [DOI] [PubMed] [Google Scholar]
- 22.Kelly JR, Denry I. Stabilized zirconia as a structural ceramic: an overview. Dent Mater. 2008;24:289–298. doi: 10.1016/j.dental.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 23.Mously HA, Finkelman M, Zandparsa R, Hirayama H. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J Prosthet Dent. 2014;112:249–256. doi: 10.1016/j.prosdent.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Rödiger M, Heinitz A, Bürgers R, Rinke S. Fitting accuracy of zirconia single crowns produced via digital and conventional impressions-a clinical comparative study. Clin Oral Investig. 2017;21:579–587. doi: 10.1007/s00784-016-1924-y. [DOI] [PubMed] [Google Scholar]
- 25.Holmes JR, Bayne SC, Holland GA, Sulik WD. Considerations in measurement of marginal fit. J Prosthet Dent. 1989;62:405–408. doi: 10.1016/0022-3913(89)90170-4. [DOI] [PubMed] [Google Scholar]
- 26.Son K, Yu BY, Yoon TH, Lee KB. Comparative study of the trueness of the inner surface of crowns fabricated from three types of lithium disilicate blocks. Appl Sci. 2019;9:1798 [Google Scholar]
- 27.ISO 12836. Dentistry - Digitizing devices for CAD/CAM systems for indirect dental restorations - Test methods for assessing accuracy. Geneva; Switzerland: International Standards Organization (ISO); 2015. Available at: https://www.iso.org/standard/68414.html . [Google Scholar]
- 28.Bindl A, Mörmann WH. Fit of all-ceramic posterior fixed partial denture frameworks in vitro. Int J Periodont Restor Dent. 2007;27:567–575. [PubMed] [Google Scholar]
- 29.Sorensen JA. A standardized method for determination of crown margin fidelity. J Prosthet Dent. 1990;64:18–24. doi: 10.1016/0022-3913(90)90147-5. [DOI] [PubMed] [Google Scholar]
- 30.Rahme HY, Tehini GE, Adib SM, Ardo AS, Rifai KT. In vitro evaluation of the “replica technique” in the measurement of the fit of Procera crowns. J Contemp Dent Pract. 2008;9:25–32. [PubMed] [Google Scholar]
- 31.Pera P, Gilodi S, Bassi F, Carossa S. In vitro marginal adaptation of alumina porcelain ceramic crowns. J Prosthet Dent. 1994;72:585–590. doi: 10.1016/0022-3913(94)90289-5. [DOI] [PubMed] [Google Scholar]
- 32.Koo JY, Lim JH, Cho IH. Marginal fidelities according to the margin types of all ceramic crowns. J Korean Acad Prosthodont. 1997;35:445–457. [Google Scholar]
- 33.Boitelle P, Mawussi B, Tapie L, Fromentin O. A systematic review of CAD/CAM fit restoration evaluations. J Oral Rehabil. 2014;41:853–874. doi: 10.1111/joor.12205. [DOI] [PubMed] [Google Scholar]
- 34.Reich S, Uhlen S, Gozdowski S, Lohbauer U. Measurement of cement thickness under lithium disilicate crowns using an impression material technique. Clin Oral Investig. 2011;15:521–526. doi: 10.1007/s00784-010-0414-x. [DOI] [PubMed] [Google Scholar]
- 35.Ahrberg D, Lauer HC, Ahrberg M, Weigl P. Evaluation of fit and efficiency of CAD/CAM fabricated all-ceramic restorations based on direct and indirect digitalization: a double-blinded, randomized clinical trial. Clin Oral Investig. 2016;20:291–300. doi: 10.1007/s00784-015-1504-6. [DOI] [PubMed] [Google Scholar]
- 36.Pradíes G, Zarauz C, Valverde A, Ferreiroa A, Martínez-Rus F. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions based on wavefront sampling technology. J Dent. 2015;43:201–208. doi: 10.1016/j.jdent.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 37.White SN, Yu Z, Kipnis V. Effect of seating force on film thickness of new adhesive luting agents. J Prosthet Dent. 1992;68:476–481. doi: 10.1016/0022-3913(92)90414-6. [DOI] [PubMed] [Google Scholar]
- 38.Lee B, Oh KC, Haam D, Lee JH, Moon HS. Evaluation of the fit of zirconia copings fabricated by direct and indirect digital scanning procedures. J Prosthet Dent. 2018;120:225–231. doi: 10.1016/j.prosdent.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005;113:174–179. doi: 10.1111/j.1600-0722.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 40.Carbajal Mejía JB, Yatani H, Wakabayashi K, Nakamura T. Marginal and internal fit of CAD/CAM crowns fabricated over reverse tapered preparations. J Prosthodont. 2019;28:e477–e484. doi: 10.1111/jopr.12715. [DOI] [PubMed] [Google Scholar]
- 41.Bornemann G, Lemelson S, Luthardt R. Innovative method for the analysis of the internal 3D fitting accuracy of Cerec-3 crowns. Int J Comput Dent. 2002;5:177–182. [PubMed] [Google Scholar]
- 42.Wang W, Yu H, Liu Y, Jiang X, Gao B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J Prosthet Dent. 2019;121:285–291. doi: 10.1016/j.prosdent.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 43.Moldovan O, Luthardt RG, Corcodel N, Rudolph H. Three-dimensional fit of CAD/CAM-made zirconia copings. Dent Mater. 2011;27:1273–1278. doi: 10.1016/j.dental.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 44.Alghazzawi TF. Advancements in CAD/CAM technology: Options for practical implementation. J Prosthodont Res. 2016;60:72–84. doi: 10.1016/j.jpor.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 45.Kirsch C, Ender A, Attin T, Mehl A. Trueness of four different milling procedures used in dental CAD/CAM systems. Clin Oral Investig. 2017;21:551–558. doi: 10.1007/s00784-016-1916-y. [DOI] [PubMed] [Google Scholar]
- 46.Bosch G, Ender A, Mehl A. A 3-dimensional accuracy analysis of chairside CAD/CAM milling processes. J Prosthet Dent. 2014;112:1425–1431. doi: 10.1016/j.prosdent.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 47.Ben-Izhack G, Shely A, Koton O, Meirowitz A, Levartovsky S, Dolev E. (In-vitro comparison between closed versus open CAD/CAM systems) Comparison between closed and open CAD/CAM systems by evaluating the marginal fit of zirconia-reinforced lithium silicate ceramic crowns. Appl Sci. 2021;11:4534 [Google Scholar]
- 48.Kunii J, Hotta Y, Tamaki Y, Ozawa A, Kobayashi Y, Fujishima A, Miyazaki T, Fujiwara T. Effect of sintering on the marginal and internal fit of CAD/CAM-fabricated zirconia frameworks. Dent Mater J. 2007;26:820–826. doi: 10.4012/dmj.26.820. [DOI] [PubMed] [Google Scholar]
- 49.Park JY, Bae SY, Lee JJ, Kim JH, Kim HY, Kim WC. Evaluation of the marginal and internal gaps of three different dental prostheses: comparison of the silicone replica technique and three-dimensional superimposition analysis. J Adv Prosthodont. 2017;9:159–169. doi: 10.4047/jap.2017.9.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ahn JJ, Bae EB, Lee WS, Cho WT, Huh JB. Comparison of clinical fit of three-unit zirconia fixed prostheses fabricated using chairside and labside CAD/CAM systems. J Dent Sci. 2020;15:239–242. doi: 10.1016/j.jds.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]