Abstract
Pediatric disc herniation is an uncommon but significant illness in children that can cause debilitating symptoms. The prevalence rate of lumbar disc herniation in this group is unknown. We present 4 rare cases of lumbar disc herniation in children. All patients complained from low back pain with radiation to the corresponding leg along with other neurological manifestations. Trauma and family history for all patients were negative. Magnetic Resonance Imaging (MRI) was performed for all patients and confirmed the diagnosis in all cases. All patients were treated conservatively without any improvement, thus surgical intervention (minimally invasive discectomy with foraminotomy) was performed. The importance of early identification and adequate care in pediatric patients with lumbar disc herniation cannot be overstated. More study is needed to better understand the risk factors, pathophysiology, and best treatments for this illness in children and adolescents.
Keywords: Lumbar disc herniation, Discectomy, Laminectomy, Pediatrics, Disc prolapse
Introduction
Pediatric disc herniation is a rare but serious condition that can lead to debilitating symptoms in children and the prevalence rate of lumbar disc herniation in this population remains unclear. Compared to adults, the diagnosing of lumbar disc herniation in children is often delayed [1,2]. It occurs when the soft tissue cushioning between the vertebrae in the spine (disc) ruptures, causing the inner material to leak out and press on nearby nerves.
While most cases of disc herniation occur in adults, it can also occur in children, with the incidence estimated to be around 1%-2%. According to reports, pediatric patients account for 0.4%-15.4% of lumbar disc herniation patients who undergo surgery [2].
In contrast to adults, who mainly develop chronic degenerative changes leading to lumbar disc herniation, trauma resulting from axial load or sports-related injuries are the primary factors linked to lumbar disc herniation in children [3], [4], [5], [6].
Symptoms can range from mild back pain to severe neurological deficits, depending on the location and severity of the herniation [7].
L4/L5 and L5/S1 are the primary levels affected by lumbar disc herniation in pediatric patients (about 93%), although other levels and multiple-level disease can occur, but they are not common [8]. Surgery for lumbar disc herniation should be deliberated in cases where neurological deficiency or debilitating pain prevents the patient from functioning normally or when conservative treatment fails. Nonetheless, the majority of patients do not show significant improvement with conservative treatment and therefore necessitate surgical intervention [9].
Here we reported 4 cases of disc herniation in pediatric age group in the same center which were successfully treated by surgical interventions after the failure of conservative treatment.
Case 1
A 10-year-old female patient, previously active and playful, presented with a history of lower back pain radiating to the left leg, associated with numbness, paresthesia, and limping. The pain started after a back bump and wrong movement. She had a family history with her uncle who has discopathy and had cervical and lumbar discectomies.
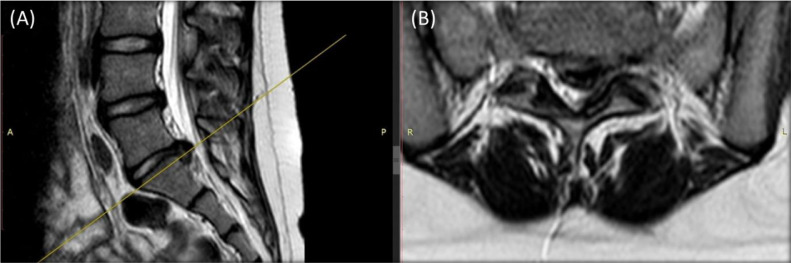
On Physical examination, a weakness in the left leg was observed. Cardiac, pulmonary, and abdominal examinations were all unremarkable and laboratory tests were within normal limits. An MRI was ordered and revealed a disc herniation at the L5\S1 level (Fig. 1).
Fig. 1.
T2- weighted sagittal (A) and axial (B) MRI demonstrating disc herniation at the L5\S1 level.
Conservative management was first initiated but did not improve symptoms. A left L5/S1 minimally invasive discectomy through an 11 mm tube, a left L5 laminectomy, and a left L5/S1 flavectomy were performed. Intraoperatively, a highly calcified disc shelf and disc material were seen.
On her latest follow-up 3 months after the surgery, the patient retained to normal activities, and was doing very well.
Case 2
A 13-year-old female patient, medically free, presented with a history of lower back pain of 9-month duration radiating to the right leg, worsened in the last 5-month and unresponsive to analgesia. She retains sphincters control. On Physical examination she had a straight leg raise test of 10\60 and right extensor hallucis longus power of 4\5.
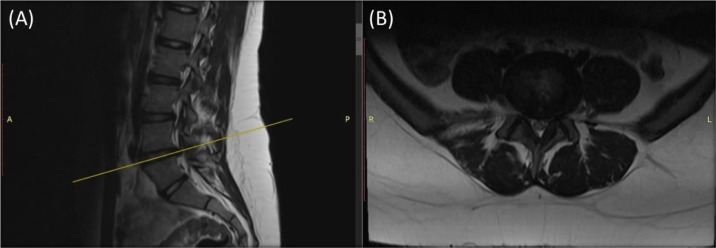
A nerve conduction study and electromyography were ordered and showed chronic denervation/radiculopathy at the level of right L4\L5 along with acute radiculopathy at the level of right L5/S1. An MRI was ordered and revealed a central disc herniation with bilateral recess stenosis at the level of L4/L5 (Fig. 2).
Fig. 2.
T2- weighted sagittal (A) and axial (B) MRI demonstrating disc herniation at L4\L5 level with bilateral recess stenosis.
Conservative management was first initiated but did not improve symptoms. Afterwards, a right L4/L5 endoscopic discectomy with a right L4/L5 foraminotomy were performed. Intraoperatively, a hypertrophied ligamentum flavum and facet compression to the lateral recess of the left L4/L5 space accompanied by a disc protrusion compressing the left L5 root. The ligamentum flavum was dehydrated as usually seen in adults.
On her latest follow-up 6 months after surgery, the patient was doing very well, free of symptoms, and off her sciatica.
Case 3
A 17-year-old male patient, medically free, presented with lower back pain radiating to the left leg of a 7-month duration associated with numbness and paresthesia but good sphincter control. Pain was unresponsive to analgesia. On physical examination he had a straight leg raise test of 30\60 and left extensor halluces longus power of 4\5 and left L5 hypoesthesia.
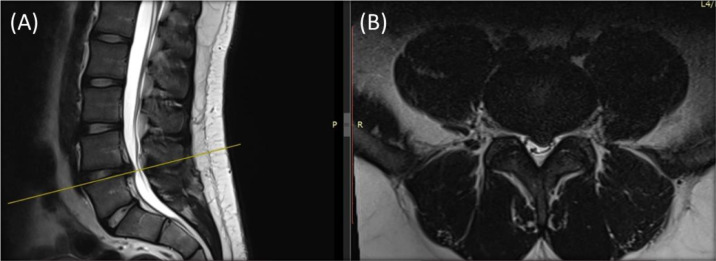
An MRI was ordered and revealed a left L4\L5 disc herniation (Fig. 3).
Fig. 3.
T2- weighted sagittal (A) and axial (B) MRI demonstrating disc herniation at L4\L5 level.
Conservative management was first initiated but did not improve symptoms. Afterwards, a left L4/L5 endoscopic discectomy with foraminotomy was performed. Intraoperatively, a matured left L4/L5 disc extrusion compressing the left L5 nerve root was observed.
On follow-up 6 months after surgery, the patient was doing very well, and all of his symptoms have subsided.
Case 4
A 15-year-old female patient, medically free, presented with right leg pain for 4-months duration, numbness, and paresthesia but with good sphincter control.
On Physical examination she had a straight leg raise test of 30/45 and right extensor hallucis longus power of 4\5 and right L5 hypoesthesia.
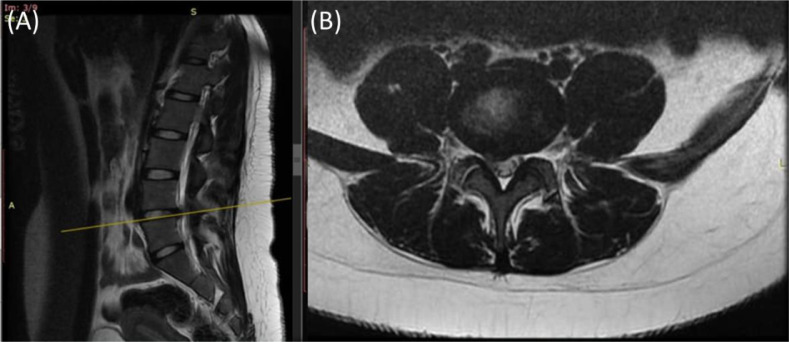
An MRI was ordered and revealed a right L4/L5 disc protrusion compressing the thecal sac and the right L5 nerve root (Fig. 4).
Fig. 4.
T2- weighted sagittal (A) and axial (B) MRI demonstrating disc herniation at L4\L5 level.
A right L4/L5 discectomy was performed. Intraoperatively, both the disc and ligamentum flavum were well hydrated. There was a disc extrusion through an opening in the annulus compressing the L5 nerve root. Postoperatively, the patient was free of symptoms and had restored full power.
Discussion
Pediatric lumbar disc herniation is a rare but potentially debilitating condition that can affect children and adolescents [2]. Although it is most commonly seen in adults, lumbar disc herniation can occur in children, especially those who are involved in sports or other physically demanding activities [10].
The exact causes of pediatric lumbar disc herniation are not well understood. However, it is believed to be the result of a combination of genetic and environmental factors [11]. Some of the risk factors associated with pediatric lumbar disc herniation include certain genetic factors that may increase a child's susceptibility to developing lumbar disc herniation [12]. In addition to trauma to the lumbar spine, such as a fall or a blow to the back. Moreover, repetitive activities that place a significant amount of stress on the lumbar spine, such as gymnastics, dance, and football, can also increase the risk of lumbar disc herniation [13], [14], [15]. Also, children born with congenital abnormalities of the spine may be at a higher risk of developing lumbar disc herniation [16].
Interestingly, Obukhov and colleagues reported the occurrence of multi-level disc herniation in two 12-year-old twins. twin A, experienced backache and radiating left leg pain after helping move some tables. Her neurological examination revealed a left tibial H-reflex latency 1.3 ms greater than the right, and a lumbar CT scan revealed central disc herniation at the L4-5 and L5-S1 levels. Her twin sister, twin B, had a history of back pain, and a lumbar MRI at the level of L4/L5 revealed obvious disc herniation. Their mother had a history of back pain and a maternal aunt had back problems complicating rheumatoid arthritis/lupus syndrome. Both of the cases were managed conservatively, and the symptoms of both twins resolved [17].
The diagnosis of pediatric lumbar disc herniation can be challenging. Children may have difficulty articulating their symptoms, which can lead to delays in diagnosis and treatment [1]. Some of the common symptoms of pediatric lumbar disc herniation include lower back pain that is worse when they are active or when they bend forward. They may also experience pain, numbness, or tingling in one or both legs. In addition to that, they may experience weakness in one or both legs, which can make it difficult for them to walk or stand [18].
To diagnose lumbar disc herniation in children, a thorough physical exam and imaging studies, such as an MRI, may be necessary. X-rays may also be used to rule out other conditions, such as scoliosis [19].
The treatment of pediatric lumbar disc herniation typically involves a combination of conservative and surgical approaches, depending on the severity of the condition [20]. Conservative treatments include resting the back and avoiding activities that exacerbate symptoms which can help reduce pain and inflammation. Physical therapy can also help strengthen the muscles surrounding the spine and improve flexibility, which can reduce the risk of future injuries. Furthermore, over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help reduce pain and inflammation. In some cases, strong prescription medications may be necessary. Also, wearing a brace can help support the spine and reduce the risk of further injury [20,21].
A study by Wang et al. [22] reported to cases of pediatric lumbar disc herniation who were aged 10- and 13-year-old. Both patients underwent nonsurgical treatment and had favorable outcomes with no recurrence after follow-up. The study suggested that nonsurgical treatment may be effective in treating pediatric disc herniation.
If conservative treatments were not effective, surgical options may be necessary including microdiscectomy which is a minimally invasive procedure that involves removing a small portion of the herniated disc to relieve pressure on the nerves. Also, fusion surgery may be considered for such cases which involves fusing 2 or more vertebrae together to stabilize the spine and prevent further injury [23].
In a study by Fakouri et al, 6 pediatric patients were reported to have disc herniation at the levels of L4/L4 and L5/S1. All patients underwent microdiscectomies after the ineffectiveness of conservative treatment. All patients had a smooth postsurgery recovery with no complications, experiencing significant pain relief. Their final follow-up showed complete pain disappearance and a negative straight-leg-raise test was seen in all patients. All patients had normal muscle power, and only 1 patient had a residual sensory deficit that improved compared to preoperative assessment [23].
The choice of surgical procedure depends on the child's age, the severity of the condition, and other factors, such as the child's overall health. Pediatric lumbar disc herniation is a rare but potentially serious condition that can cause significant pain and functional impairment in children. Early diagnosis and treatment are essential to prevent further injury and promote healing.
Conclusion
In conclusion, pediatric lumbar disc herniation is a rare but serious condition that can cause significant pain and disability in children and adolescents. Risk factors for the condition include trauma, repetitive activities, congenital abnormalities of the spine, and certain genetic factors. In the cases presented, minimally invasive discectomy with foraminotomy were effective in treating the patients, and they all returned to normal activities without symptoms after surgery. Early diagnosis and appropriate management are crucial for achieving optimal outcomes in pediatric patients with lumbar disc herniation. Further research is needed to better understand the risk factors, pathophysiology, and optimal treatment approaches for this condition in children and adolescents.
Patient consent
Written informed consent was obtained from the patients for publication of this case report and accompanying images. written consent is available for review by the Editor-in Chief of this journal on request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Haidar R, Ghanem I, Saad S, Uthman I. Lumbar disc herniation in young children. Acta Paediatr. 2010;99(1):19–23. doi: 10.1111/j.1651-2227.2009.01460.x. [DOI] [PubMed] [Google Scholar]
- 2.Lavelle WF, Bianco A, Mason R, Betz RR, Albanese SA. Pediatric disk herniation. J Am Acad Orthop Surg. 2011;19(11):649–656. doi: 10.5435/00124635-201111000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Martínez-Lage JF, Fernández Cornejo V, López F, Poza M. Lumbar disc herniation in early childhood: case report and literature review. Childs Nerv Syst. 2003;19(4):258–260. doi: 10.1007/s00381-003-0720-6. [DOI] [PubMed] [Google Scholar]
- 4.Benifla M, Melamed I, Barrelly R, Aloushin A, Shelef I. Unilateral partial hemilaminectomy for disc removal in a 1-year-old child. J Neurosurg Pediatr. 2008;2(2):133–135. doi: 10.3171/ped/2008/2/8/133. [DOI] [PubMed] [Google Scholar]
- 5.Revuelta R, De Juambelz PP, Fernandez B, Flores JA. Lumbar disc herniation in a 27-month-old child. Case report. J Neurosurg. 2000;92(1 Suppl):98–100. doi: 10.3171/spi.2000.92.1.0098. [DOI] [PubMed] [Google Scholar]
- 6.Fitzer PM. Anterior herniation of the nucleus pulposus: radiologic and clinical features. South Med J. 1985;78(11):1296–1300. doi: 10.1097/00007611-198511000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Andrew S., Zhang M.D., Andrew Xu, Kashif Ansari, Kyle Hardacker M.D., George Anderson B.S., Daniel Alsoof MBBS, Alan H., Daniels M.D. Lumbar disc herniation: diagnosis and management. Am J Med. 2023 doi: 10.1016/j.amjmed.2023.03.024. [DOI] [PubMed] [Google Scholar]
- 8.Gulati S., Madsbu M.A., Solberg T.K., Sørlie A., Charalampis C., Skram M.K., et al. Lumbar microdiscectomy for sciatica in adolescents: a multicentre observational registry-based study. Acta Neurochir (Wien) 2017;159(3):509–516. doi: 10.1007/s00701-017-3077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurihara A, Kataoka O. Lumbar disc herniation in children and adolescents. A review of 70 operated cases and their minimum 5-year follow-up studies. Spine (Phila Pa 1976) 1980;5(5):443–451. [PubMed] [Google Scholar]
- 10.Purcell L, Micheli L. Low back pain in young athletes. Sports Health. 2009;1(3):212–222. doi: 10.1177/1941738109334212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zielinska N, Podgórski M, Haładaj R, Polguj M, Olewnik Ł. Risk factors of intervertebral disc pathology-a point of view formerly and today-a review. J Clin Med. 2021;10(3):409. doi: 10.3390/jcm10030409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ala-Kokko L. Genetic risk factors for lumbar disc disease. Ann Med. 2002;34(1):42–47. doi: 10.1080/078538902317338634. [DOI] [PubMed] [Google Scholar]
- 13.Battié MC, Videman T. Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am. 2006;88(Suppl 2):3–9. doi: 10.2106/jbjs.E.01313. [DOI] [PubMed] [Google Scholar]
- 14.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–24. doi: 10.2106/jbjs.E.01273. [DOI] [PubMed] [Google Scholar]
- 15.Shiri R, Lallukka T, Karppinen J, Viikari-Juntura E. Obesity as a risk factor for sciatica: a meta-analysis. Am J Epidemiol. 2014;179(8):929–937. doi: 10.1093/aje/kwu007. [DOI] [PubMed] [Google Scholar]
- 16.Atabey C, Eroğlu A, Topuz AK, Velioğlu M, Demircan MN. Lumbar disc herniation in a patient with congenital vertebral body anomaly: a case report. Korean J Spine. 2014;11(4):245–248. doi: 10.14245/kjs.2014.11.4.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obukhov SK, Hankenson L, Manka M, Mawk JR. Multilevel lumbar disc herniation in 12-year-old twins. Childs Nerv Syst. 1996;12(3):169–171. doi: 10.1007/bf00266823. [DOI] [PubMed] [Google Scholar]
- 18.Houghton KM. Review for the generalist: evaluation of low back pain in children and adolescents. Pediatr Rheumatol Online J. 2010;8:28. doi: 10.1186/1546-0096-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J.-H., van Rijn R.M., van Tulder M.W., Koes B.W., de Boer M.R., Ginai A.Z., et al. Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; a systematic review. Chiropr Man Therap. 2018;26:37. doi: 10.1186/s12998-018-0207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dang L, Liu Z. A review of current treatment for lumbar disc herniation in children and adolescents. Eur Spine J. 2010;19(2):205–214. doi: 10.1007/s00586-009-1202-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slotkin JR, Mislow JM, Day AL, Proctor MR. Pediatric disk disease. Neurosurg Clin N Am. 2007;18(4):659–667. doi: 10.1016/j.nec.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Xu Y, Tian G, Dai G. Pediatric lumbar disc herniation: a report of two cases and review of the literature. Eur J Med Res. 2022;27(1):82. doi: 10.1186/s40001-022-00696-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buy X, Gangi A. Percutaneous treatment of intervertebral disc herniation. Semin Intervent Radiol. 2010;27(2):148–159. doi: 10.1055/s-0030-1253513. [DOI] [PMC free article] [PubMed] [Google Scholar]