Abstract
Background:
The coronavirus disease 2019 (COVID-19) pandemic has caused the cancellation or postponement of virtually every sporting event, resulting in training disruptions, income loss, and career uncertainties for athletes around the world. At present, the effect of the COVID-19 pandemic on the mental and emotional health of athletes is not well understood.
Purpose:
To investigate the effect of the COVID-19 pandemic on the mental and emotional health of athletes and to identify risk factors associated with poor mental health outcomes.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
The PubMed, Embase, and Cochrane Library databases were searched to identify all articles reporting on athletes’ mental and emotional health during the COVID-19 pandemic. Articles were selected based on relevant inclusion and exclusion criteria. Study characteristics, athlete demographics, and COVID-19 mental health data (sex-, type of sport—, and level of play—specific differences) were collected from each included article and analyzed.
Results:
A total of 35 studies were included in the final analysis, comprising athletes around the world and across numerous sports and levels of play. Most studies utilized at least 1 validated mental health questionnaire and assessed for outcomes such as depression, anxiety, stress, motivation, and athletic identity. Overall, athletes reported worse mental and emotional health during the COVID-19 pandemic, although these effects were attenuated by home training programs and quarantine training camps. Female sex and more elite levels of play were associated with an increased risk for poor mental health outcomes. Type of sport was associated with mixed results, with individual and team sports carrying different increased risks for poor mental and emotional health. Nearly all studies recommended the need for increased psychological support of athletes during the COVID-19 pandemic.
Conclusion:
The effect of the COVID-19 pandemic on the mental and emotional health of athletes is complex and multifaceted. Increased social interactions with coaches and teammates, continued access to training facilities and mental health professionals, and active utilization of healthy coping mechanisms can improve mental health outcomes for athletes in the era of COVID-19.
Keywords: anxiety, athletes, coronavirus disease 2019, depression, mental health, stress
The SARS-CoV-2 virus (COVID-19) has produced the most severe health crisis since the Spanish flu. 18 As of January 15, 2022, more than 318 million people have tested positive for COVID-19, and over 5.5 million people have died from the disease. 55 In response to the growing pandemic, many countries imposed significant restrictions aimed at slowing the spread of COVID-19. For athletes around theworld, this meant the cancellation or postponement of virtually every sporting event, resulting in training disruptions, income loss, and career uncertainties that have profoundly affected mental health.2,25,37
The detraining effect of the COVID-19 pandemic on athlete performance has been well–documented in the literature.10,15,21,28 However, the effect of the COVID-19 pandemic on athletes’ mental and emotional health is less well understood. Previous studies have shown that periods of inactivity, isolation, and loss of social support from the sports community can cause emotional distress and psychological disorders in athletes. 32 Therefore, the purpose of the present study was to investigate the effect of the COVID-19 pandemic on the mental and emotional health of athletes and to identify risk factors associated with poor mental health outcomes. We hypothesized that the COVID-19 pandemic would have an overall negative effect on athlete mental health, with an appreciation of sex-, type of sport—, and level of play—specific differences.
Methods
A systematic review of the literature was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Figure 1). The PubMed MEDLINE, Embase, and Cochrane Library databases were accessed and searched to identify all articles reporting on athletes during COVID-19. The following Boolean search terms were used: ((return to sport*) OR (return to play) OR (return to competition) OR (athlete*) OR (athletic*)) AND ((COVID-19) OR (Sars-CoV-2) OR (coronavirus) OR (pandemic)). To increase specificity, a filter was applied excluding articles published before January 1, 2020.
Figure 1.
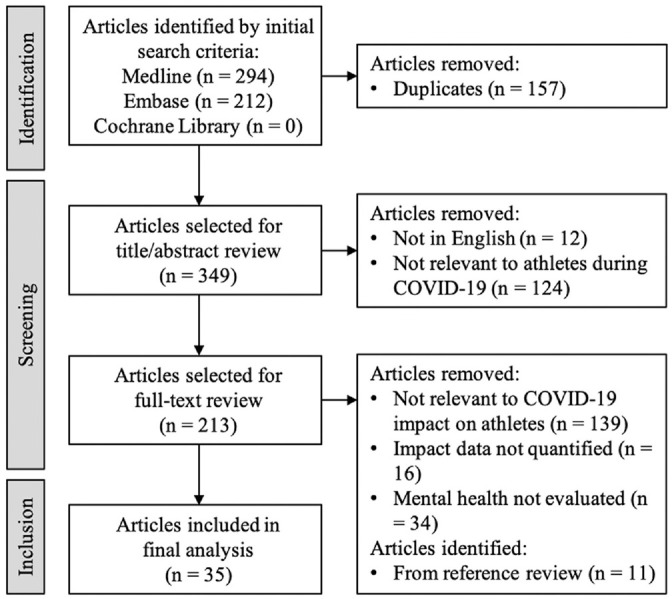
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram depicting search strategy.
All search returns were extracted, and duplicate search returns were discarded. Titles and abstracts were first screened for relevance, followed by full–text reviews of the relevant articles. Articles were excluded based on the following criteria: (1) non-English text; (2) only abstract available; (3) population not athlete specific; (4) outcome not COVID-19 specific; (5) mental health data not quantified; (6) editorial; or (7) review article or meta–analysis. Studies evaluating a mixed population (eg, athletes and nonathletes) were included only if their COVID-19 mental health data were stratified by population. Additionally, the references of all included studies were reviewed to ensure that all relevant studies were captured.
Study characteristics, athlete demographics, and COVID-19 mental health data were collected from each study. Study characteristics included study period, country, number of athletes, and data collection tool. Athlete demographics included age, sex, sport, and level of play. COVID-19 mental health data included the effect of lockdown on athletes’ mental health (before vs during/after), as well as differences associated with sex (male vs female), type of sport (individual vs team), and level of play (more elite vs less elite). Finally, athlete mental health recommendations were recorded if reported by the study.
It was anticipated that many of the included studies would be limited in methodological quality because of the rapid and unforeseen onset of the COVID-19 pandemic. Most studies were expected to be cross–sectional, subject to convenience sampling, and lacking in an appropriate control (if one was present at all). Only a few studies of higher methodological quality were expected, representing longitudinal athlete mental health studies that had fortuitously been implemented before the start of the lockdown. An overall high risk of bias was therefore presumed, and no additional risk of bias assessment was performed.
Results
Of the 360 studies identified in the initial search and reference review, 35 studies †† met the inclusion criteria. All 35 studies were conducted between November 2019 and March 2021, with a mean study period of about 2.5 months (Table 1). Most studies evaluated athletes from a single country but across multiple sports and levels of play. Additionally, all but 2 studies utilized at least 1 validated mental health questionnaire, such as the Depression Anxiety and Stress Scales, Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder (GAD-7), Profile of Mood States, and Athletic Identity Measurement Scale. The 2 studies that did not were those conducted by Jagim et al, 26 which assessed for mental well–being using a visual analog scale, and by Soares et al, 50 which assessed for anxiety symptoms using a semistructured questionnaire. Overall, athletes’ mental and emotional health was found to be negatively affected by the COVID-19 lockdown and associated with sex-, type of sport—, and level of play—specific differences (Table 2).
Table 1.
Characteristics of Included Studies on Mental Health a
| Author | Study Period | Country | Sport | Level of Play | Athletes, N | Age, y | Male, % |
|---|---|---|---|---|---|---|---|
| Batalla-Gavalda et al 3 | Mar 2020—May 2020 | Spain | Various | Youth | 45 | 16.16 | 31.1 |
| Clemente-Suárez et al 6 | Mar 2020—Apr 2020 | Spain | Various | Olympic, Paralympic | 175 | 27.62 ± 7.33 | 41.1 |
| Costa et al 7 | Mar 2020 | Italy | Various | Elite | 1125 | 27.47 ± 8.47 | 45.8 |
| Dauty et al 8 | Mar 2020—May 2020 | France | Soccer | Elite | 25 | 14.2 | 100 |
| Davila-Torres et al 9 | Feb 2021 | Peru | Rugby | Elite | 74 | 20.5 ± 4.4 | 56.8 |
| Denerel et al 11 | NR | Turkey | Various | Youth | 1214 | 14.6 | 80.7 |
| di Cagno et al 12 | Apr 2020—May 2020 | Italy | Various | Elite | 1508 | 19.32 | 52.3 |
| Facer-Childs et al 14 | May 2020—Jun 2020 | Australia | Various | Elite | 399 | 26.5 ± 0.4 | 42.6 |
| Fiorilli et al 16 | Mar 2020—May 2020 | Italy | Various | Elite | 800 | 28.30 ± 10.93 | 53.3 |
| Garver et al 17 | Aug 2020—Oct 2020 | USA | Various | Collegiate | 249 | 20 ± 1.6 | 50.2 |
| Gouttebarge et al 19 | Mar 2020—Apr 2020 | NR | Soccer | Elite | 1909 | 24.9 | 68.6 |
| Graupensperger et al 20 | Feb 2020—Apr 2020 | USA | Various | Collegiate | 369 | 19.84 ± 1.38 | 37 |
| Hagiwara et al 23 | Apr 2020—Mar 2021 | Japan | Various | Collegiate | 537 | 19.79 | 100 |
| Håkansson et al 24 | May 2020—Jun 2020 | Sweden | Various | Elite | 327 | ≥15 | 61.9 |
| Jagim et al 26 | Apr 2020—Jun 2020 | USA | Various | Collegiate | 105 | 19.86 ± 2.13 | 29.5 |
| Knowles et al 27 | Jun 2020—Jul 2020 | UK, Ireland | Various | Elite | 360 | >18 | 55.3 |
| Leguizamo et al 29 | Apr 2020 | Various b | Various | Elite | 310 | 22.26 ± 4.98 | 54.5 |
| Martínez-González et al 30 | Nov 2019— May 2020 | Spain | Various | Collegiate | 127 | 21.14 ± 2.77 | 49.6 |
| McGuine et al 31 | May 2020 | USA | Various | Youth | 13,002 | 16.3 ± 1.2 | 47.1 |
| Mehrsafar et al 33 | Apr 2020—Jul 2020 | Iran | Various | Elite | 525 | 27.85 ± 9.09 | 39 |
| Melnyk et al 34 | Jan 2021 | Ukraine | Various | Elite | 403 | 18-25 | 59.1 |
| Mon-López et al 35 | Apr 2020 | Spain | Handball | Elite | 187 | 23.3 | 64.7 |
| Ozen et al 38 | Mar 2020 | Turkey | Various | Elite | 255 | 23.4 | 61.2 |
| Parm et al 39 | May 2020—Jun 2020 | Estonia | Various | Elite | 102 | 24.68 ± 8.55 | 43.1 |
| Pensgaard et al 40 | Jun 2020—Sep 2020 | Norway | Various | Elite | 378 | 26.86 ± 6.13 | 57.9 |
| Pillay et al 42 | Apr 2020 | South Africa | Various | Elite | 692 | >18 | 66.8 |
| Pons et al 43 | NR | Spain | Various | Youth | 544 | 15.9 ± 1.51 | 51.5 |
| Roberts and Lane 45 | Apr 2020 | UK | Boxing | Elite | 44 | 19.4 ± 4.6 | 75 |
| Rubio et al 46 | Apr 2020—May 2020 | Spain | Various | NR | 274 | 35.8 ± 14.1 | 47.8 |
| Ruffault et al 47 | Apr 2020-May 2020 | France | Various | Elite | 759 | 27 ± 10 | 51 |
| Şenışık et al 48 | NR | Turkey | Various | Elite | 392 | 24.53 ± 5.09 | 74 |
| Simons et al 49 | Feb 2020—Jun 2020 | Australia | Various | Elite | 15 | 22.9 ± 4.4 | 40 |
| Soares et al 50 | Aug 2020—Sep 2020 | Brazil | Various | Elite | 206 | 24.61 ± 8.73 | 56.3 |
| Vaughan et al 51 | NR | UK | Various | Elite | 894 | 32.66 ± 12.14 | 45.9 |
| Washif et al 54 | Jun 2020 | Malaysia | Various | Olympic, Paralympic | 76 | 26 ± 5 | 69.70 |
Values presented as mean, mean ± SD, or range. NR, nor reported.
Countries included China, Mexico, Portugal, Russia, and Spain.
Table 2.
Risk Factors Associated With Poor Mental Health Outcomes
| Author | COVID-19 Lockdown |
Sex |
Type of Sport |
Level of Play |
||||
|---|---|---|---|---|---|---|---|---|
| Before | During/After | Male | Female | Individual | Team | Less Elite | More Elite | |
| Batalla-Gavalda et al 3 | ✓ a | ✓ | ||||||
| Clemente-Suárez et al 6 | ✓ a | ✓ | ✓ | ✓ | ||||
| Costa et al 7 | ✓ a | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Dauty et al 8 | b | |||||||
| Davila-Torres et al 9 | ✓ a | |||||||
| Denerel et al 11 | ✓ a | ✓ | ||||||
| dI Cagno et al 12 | ✓ a | ✓ | ✓ | ✓ | ||||
| Facer-Childs et al 14 | ✓ a | |||||||
| Fiorilli et al 16 | ✓ a | ✓ | ✓ | ✓ | ✓ | |||
| Garver et al 17 | ✓ a | ✓ | ||||||
| Gouttebarge et al 19 | ✓ | ✓ | ✓ | |||||
| Graupensperger et al 20 | ✓ | |||||||
| Hagiwara et al 23 | ✓ a | ✓ | ||||||
| Håkansson et al 24 | ✓ a | ✓ | ✓ | |||||
| Jagim et al 26 | ✓ a | |||||||
| Knowles et al 27 | ✓ a | ✓ | ||||||
| Leguizamo et al 29 | ✓ | |||||||
| Martínez-González et al 30 | ✓ | |||||||
| McGuine et al 31 | ✓ a | ✓ | ✓ | ✓ | ||||
| Mehrsafar et al 33 | ✓ a | |||||||
| Melnyk et al 34 | ✓ a | ✓ | ✓ | |||||
| Mon-López et al 35 | ✓ a | ✓ | ||||||
| Ozen et al 38 | ✓ a | |||||||
| Parm et al 39 | ✓ a | ✓ | ||||||
| Pensgaard et al 40 | ✓ a | ✓ | ✓ | ✓ | ||||
| Pillay et al 42 | ✓ a | ✓ | ||||||
| Pons et al 43 | ✓ a | ✓ | ✓ | |||||
| Roberts and Lane 45 | ✓ | |||||||
| Rubio et al 46 | ✓ a | ✓ | ✓ | |||||
| Ruffault et al 47 | ✓ a | ✓ | ✓ | ✓ | ||||
| Şenışık et al 48 | ✓ a | |||||||
| Simons et al 49 | ✓ | |||||||
| Soares et al 50 | ✓ a | |||||||
| Vaughan et al 51 | ✓ a | ✓ | ✓ | ✓ | ||||
| Washif et al 54 | b | |||||||
Increased risk for poor mental health.
Risk for poor mental health described as “high” without direct pre-COVID-19 comparison data.
Mental health remained stable or improved with intervention (eg, training program, quarantine camp).
Effect of COVID-19 Lockdown
All 35 included studies evaluated the effect of the COVID-19 pandemic on athlete mental health. Of these, 32 studies ‡‡ associated the pandemic with poor mental health outcomes.
Among the 32 studies, 5 studies19,20,30,45,49 directly compared athlete mental health before versus during/after lockdown. Graupensperger et al 20 and Martínez-González et al 30 found that athletic identity, autonomous goal motives, and eudaimonic well–being were all negatively affected by the pandemic. Additionally, Simons et al 49 found that the highest risk of athlete adjustment disorder coincided with the enactment of the harshest lockdown restrictions. Using pre-COVID-19 data from a comparison group enrolled in a longitudinal mental health study, Gouttebarge et al 19 calculated the 2–week prevalence of anxiety and depression in professional soccer players to be significantly higher during lockdown than before lockdown. Likewise, Roberts and Lane 45 collected pre-COVID-19 data using a retrospective approach and observed the intensity of unpleasant moods (eg, anger, confusion, depression, fatigue, and tension) to be significantly higher during lockdown than before lockdown.
Three of the 32 studies3,33,46 assessed athlete mental health at various time points across lockdown. Mehrsafar et al 33 found that mental health, mood, and life satisfaction worsened throughout confinement. Although Batalla-Gavalda et al 3 and Rubio et al 46 also reported poor athlete mental health during the lockdown, they identified characteristics of adaptation rather than deterioration over time.Specifically, Batalla-Gavalda et al observed a statistically significant reduction in total mood disturbance, depression, and confusion scores among Spanish youth athletes at weeks 6 and 10 compared with week 1 after lockdown. Similarly, Rubio et al observed a consistent decline in somatic symptoms across 7 weeks of lockdown.
Twenty-four of the 32 studies §§ assessed athlete mental health at a single time point during the lockdown. This included measurements of the severity and/or prevalence of depression, ‖‖ anxiety, ¶¶ stress,12,16,17,29,38,39,48,51 motivation,42,47 hyperarousal,12,16 and insomnia,39,40 among others. Håkansson et al 24 found that 66% of athletes expressed worry about the future of their sport and 51% about their future playing sports. Depression was reported in 19% of women and 3% of men, and anxiety in 20% of women and 5% of men. Likewise, two–thirds of athletes in the Parm et al 39 study exhibited distress, with 39.7% of women and 25% of men experiencing depressive symptoms, and 27.6% of women and 13.6% of men demonstrating anxiety. Among the 24 studies, only 3 compared the mental health of athletes versus nonathletes during the lockdown.11,27,48 Both Denerel et al 11 and Şenışık et al 48 found high rates of depression in athletes but acknowledged that these rates were lower than those in nonathletes. By contrast, Knowles et al 27 found that athletes experienced greater anxiety than nonathletes, although athletes and nonathletes possessed similar degrees of resilience.
Outside of the 32 studies, 1 study, by Leguizamo et al, 29 investigated the psychological effects of confinement in a cross–cultural sample of athletes from Europe, Asia, and America. They determined levels of depression, anxiety, and stress to be “relatively low,” although no direct comparison data were provided. The remaining 2 studies8,54 examined athlete mental health in the context of an intervention. Dauty et al 8 found that mental health remained stable during confinement when young elite soccer players were required to follow a home training program. Similarly, Washif et al 54 found that mental and emotional health, training motivation, and perceived stress improved when athletes participated in a quarantine training camp, effectively overcoming the adverse mental health consequences of lockdown.
Effect of Sex
Eighteen studies ## reported differences in mental health outcomes associated with sex. Of these, 14 studies a found higher rates of depression, anxiety, stress, fatigue, and/or neuroticism in female athletes. By contrast, male athletes were more likely to demonstrate increased resilience and emotional regulation.27,35 The remaining 4 studies7,19,24,40 reported adverse mental health outcomes associated with both male and female athletes. In the study of Pensgaard et al, 40 male athletes were more likely to suffer from gambling problems than their female counterparts (8.6% vs 1.3%), while female athletes were more likely to suffer from eating disorders than male athletes (8.8% vs 1.4%). Similarly, Håkansson et al 24 found increased gambling tendencies in male athletes and increased alcohol consumption in female athletes. In Costa et al, 7 male athletes scored higher on “catastrophizing” in team sports, whereas female athletes scored higher on catastrophizing in individual sports. And finally, in the study of Gouttebarge et al, 19 although female professional soccer players were more likely to experience anxiety (18.2% vs 15.5%) and depression (21.6% vs 12.9%) compared with their male counterparts, male players reported higher rates of suicidal ideation.
Effect of Type of Sport
Eight studies3,6,7,12,16,31,34,46 reported differences in mental health outcomes associated with the type of sport. Of these, 5 studies3,6,12,16,31 reported worse mental health outcomes associated with either individual or team sport athletes. Clemente-Suárez et al 6 found that Olympic and Paralympic individual sport athletes scored higher in agreeableness than team sport athletes. However, di Cagno et al 12 and Fiorilli et al 16 found that individual sport athletes also scored higher in stress and hyperarousal than team sport athletes, with statistically significant differences. In a study by McGuine et al 31 conducted on 13,002 American adolescent athletes, team sport athletes were characterized by the highest GAD-7 and PHQ-9 scores, as well as the highest prevalence of moderate to severe anxiety and moderate to severe depression; the opposite was true for individual sport athletes. Batalla-Gavalda et al 3 examined the mood states of Spanish youth athletes at several time points after lockdown. The team sports group demonstrated greater total mood disturbance, tension, depression, anger, and confusion than the individual sports group, with statistically significant differences at 6 weeks and 10 weeks after lockdown.
The remaining 3 studies7,34,46 reported adverse mental health outcomes associated with both individual and team sport athletes. Costa et al 7 found that nonelite team sport athletes had a stronger social identity but greater negative affectivity compared with individual sport athletes. Likewise, Melnyk et al 34 found that individual sports athletes possessed the highest psychological well–being (eg, motivation and self-esteem), whereas team sports athletes possessed the highest social well–being (eg, support from family and friends). And finally, in a study by Rubio et al, 46 team sport athletes had higher levels of somatic symptoms but exhibited quicker rates of adaptation compared with individual sports athletes.
Effect of Level of Play
Ten studies b reported differences in mental health outcomes associated with level of play. Given the heterogeneity of study populations, the level of play was analyzed in relative rather than absolute terms (ie, more elite vs less elite rather than elite vs nonelite) and in reference to each study's population. Thus, all 10 studies were analyzed in a consistent manner, regardless of whether they evaluated amateur athletes, professional athletes, or some combination of amateur and professional athletes.
Of the 10 studies, poor mental health outcomes were associated with more elite athletes in 5 studies6,12,23,31,43 and less elite athletes in 1 study. 40 di Cagno et al 12 found that elite athletes showed significantly higher hyperarousal than amateur athletes, while Clemente-Suárez et al 6 found that professional athletes demonstrated significantly less agreeableness than nonprofessional athletes. In studies of adolescent athletes from Japan, the United States, and Spain, Hagiwara et al, 23 McGuine et al, 31 and Pons et al 43 all reported worse mental health outcomes in higher grade level students. In a study by McGuine et al, athletes in grade 12 were characterized by the highest GAD-7 and PHQ-9 scores, as well as the highest prevalence of moderate to severe anxiety and moderate to severe depression; by contrast, athletes in grade 9 had the lowest such scores and prevalence. Similarly, in a study by Hagiwara et al, fourth–year university students experienced a higher level of sports helplessness compared with first-, second-, and third–year students, and a significant positive correlation was identified between this helplessness and depression. The single study that associated worse mental health outcomes with less elite athletes was conducted by Pensgaard et al, 40 which described lower levels of anxiety and depression in Olympic and Paralympic athletes compared with elite and semi–elite athletes.
The remaining 4 studies7,16,47,51 reported adverse mental health outcomes associated with both more elite and less elite athletes. Costa et al 7 found that elite athletes possessed a stronger social identity but higher negative affectivity compared with nonelite athletes. Additionally, elite athletes were characterized by greater “acceptance” whereas nonelite athletes were more prone to self–blame. In the study of Ruffault et al, 47 higher–level athletes experienced worse anxiety while lower level athletes demonstrated less motivation. In a study by Vaughan et al, 51 athletes with more expertise scored higher on depression while athletes with less expertise scored higher on anxiety and stress. And finally, in a study by Fiorilli et al, 16 low–level athletes exhibited greater avoidance than middle–level athletes, who in turn displayed greater hyperarousal than high–level athletes.
Discussion
Throughout the COVID-19 pandemic, athletes around the world faced significant disruptions to their training and competition schedules. The present study sought to systematically review the published literature on the effect of the COVID-19 pandemic on the mental and emotional health of athletes. Overall, athletes reported worse mental health during lockdown, although these effects were attenuated by home training programs and quarantine training camps. Female sex and more elite levels of play were associated with an increased risk for poor mental health outcomes. The type of sport was associated with mixed results, with individual and team sports carrying different increased risks for poor mental and emotional health.
The findings of the present study are broadly consistent with those of the general population. Increased levels of depression, anxiety, and stress have been documented as a psychological consequence of the COVID-19 pandemic in nonathlete populations.4,44,52 The closure of fitness centers and training facilities has almost universally contributed to a decreased motivation to train and a diminished satisfaction with training.5,26 Female sex has also been implicated as a risk factor for worse mental health outcomes in nonathletes.4,44,52 This sex disparity may be attributed to the different emotional regulation processes between men and women, as well as to the disproportionate burden of the COVID-19 pandemic on female caregivers.22,53
The type of sport is a unique risk factor associated with athletes rather than the general population. It is well known that social interactions serve a protective role in mental health, and athletes who have remained connected to their coaches and the wider sports community during lockdown (either face–to–face or online via social media platforms) have reported greater mental well–being. 13 Although this observation would seem to imply that team sports are more protective than individual sports for mental and emotional health, our analysis yielded mixed results, suggesting that individual and team sports carry different risk and protective factors for mental health outcomes. It is possible that whereas team sport athletes may benefit from more regular social interactions, individual sport athletes may be more adapted and adjusted to solo training. Regardless of the type of sport, nearly all studies recommended the need for increased social interaction with coaches and the wider sports community during the COVID-19 pandemic.
The level of play is another unique risk factor associated with athletes rather than the general population. Although more elite athletes tended to demonstrate worse mental health outcomes, less elite athletes were not immune to these effects. This heterogeneity may be attributed to the fact that some studies divided their population into low–level and high–level athletes, while other studies included a third category of midlevel or midcareer athletes. Compared with low–level and high–level athletes, midlevel athletes may be particularly susceptible to the negative mental health effects of the COVID-19 pandemic. Fiorilli et al 16 proposed that midlevel athletes were most vulnerable to career instability. Unlike low–level athletes, midlevel athletes did not have as many years of competition ahead of them or as much flexibility to pursue a different career path; and unlike high–level athletes, they were also not well–enough established to live comfortably or retire. The uncertainty surrounding professional sports during the COVID-19 pandemic may sway some athletes toward a different career path that offers more long–term financial security. Abenza-Cano et al 1 found that although there were no differences in perceived athletic identity between current college athletes and those who attended college in 2015-2016, significantly fewer athletes during the COVID-19 period wished to continue playing sports after graduation.
There is some debate as to whether any of these statistically significant results are clinically significant in regard to necessitating widespread psychological interventions. Leguizamo et al 29 found that while elite athletes did experience depression, anxiety, and stress during the lockdown, they continued to demonstrate an “iceberg profile,” a set of personality traits characterized by high vigor, low tension, low depression, low anger, low fatigue, and low confusion. Historically, the iceberg profile has been recognized as a positive mood state in athletes associated with successful performance in sports. Leguizamo et al argued that because elite athletes continued to demonstrate an iceberg profile during the pandemic, they may be able to overcome mental health setbacks on their own without the need for professional assistance.
However, most athletes (and particularly those with 1 or more risk factors) will likely benefit from increased psychological support during the COVID-19 pandemic. Elliott et al 13 found that even if athletes were not able to meet with their coaches and teammates in person, a sense of connectedness was effectively established and maintained during lockdown via social media platforms, video conferencing, and online communication. Although these virtual formats did not replace the desire of athletes to connect in person, they served as vitally important substitutes in the absence of face–to–face interactions. Return to training has also been shown to offer numerous psychological benefits to athletes even when it did not limit detraining. Dauty et al 8 found that mental health remained stable during confinement when young elite soccer players were required to follow a home training program. Similarly, Washif et al 54 found that mental and emotional health, training motivation, and perceived stress improved when athletes participated in a quarantine training camp. Finally, access to mental health resources and professionals may offer additional psychological benefits to athletes. Early detection of symptoms suggestive of declining mental and emotional health can lead to prompt and more effective behavioral and cognitive therapy. 19 Thus, frequent check–ins and monitoring by coaches, parents, and medical personnel are critical to preventing further mental and emotional decline, as well as the manifestation of even more serious psychiatric diseases that may manifest later in life. 19 Given that athletes demonstrate different coping profiles, Pété et al 41 emphasized the need for a person–centered approach with individualized interventions. And even for elite athletes who continue to demonstrate an iceberg profile, the practice of adaptive coping strategies, such as cognitive restructuring, emotional calming, and psychological flexibility, can lead to less negative emotional states and better mental health outcomes.
Although most studies have focused on the negative effects of mandatory lockdowns and canceled competitions, a few qualitative studies have revealed more positive themes. The announcement that the 2020 Olympic Games would be officially postponed brought some Olympic athletes a sense of relief. 36 For those who were injured or who had not yet qualified for the 2020 Games, the extra time was seen as an opportunity for rest, recovery, and further performance enhancement. 36 For others, the postponement offered a welcome end to the “agonizing uncertainty and speculation about scheduled events.” 36 Moreover, the COVID-19 pandemic enabled many young athletes to reconnect with their families, both in adapting to life under lockdown and in finding the motivation to stay fit. 13 The forced period away from sports also encouraged some athletes to “recalibrate toward a deeper and more meaningful connection to sports, underpinned by the profound sense of enjoyment and fun that they first experienced when participating.” 13
Limitations
As expected, the majority of included studies were cross–sectional and limited in methodological quality, due in large part to the time sensitivity and resource constraints of the COVID-19 pandemic. Only 4 studies recruited participants via random sampling19,34,39,40; the remaining 31 studies utilized convenience sampling (23), c snowball sampling (5),7,12,16,35,46 or purposive sampling (2)14,51 or did not specify their sampling method (1). 49 These nonprobability sampling strategies are vulnerable to selection bias, in which the study participants do not generalize to the athlete population of interest. Additionally, only 5 studies19,20,30,45,49 directly compared athlete mental health before versus during/after lockdown. Among these 5 studies, 1 study 45 retrospectively collected pre-COVID-19 data, which are subject to recall bias, while another study 19 used pre-COVID-19 data from a different study population, which may not serve as an appropriate control. The remaining 30 studies lacked pre-COVID-19 mental health data entirely, which limited analysis but was understood to be a relatively unavoidable consequence of the pandemic.
The included studies were also characterized by significant heterogeneity. In particular, the ages of the study participants varied considerably; for example, Dauty et al 8 and Rubio et al 46 evaluated athletes with a mean age of 14.2 years and 35.8 years, respectively. Athletes at such different stages of their lives and careers undoubtedly faced different personal and professional stressors that affected their overall mental health. Furthermore, definitions of “elite” athletes also varied considerably, with some studies including only national- and international–level athletes and other studies including university- and regional–level athletes as well. This necessitated that the level of play be analyzed in relative rather than absolute terms (ie, more elite vs less elite rather than elite vs nonelite) to offer some consistency for comparison. Nevertheless, the present systematic review is the first to provide a comprehensive analysis of the effect of the COVID-19 pandemic on the mental and emotional health of athletes and the first to synthesize athlete–specific risk factors associated with poor mental health outcomes.
Conclusion
The effect of the COVID-19 pandemic on the mental and emotional health of athletes is complex and multifaceted. Increased social interactions with coaches and teammates, continued access to training facilities and mental health professionals, and active utilization of healthy coping mechanisms can improve mental health outcomes for athletes in the era of COVID-19.
Submitted November 14, 2021; accepted February 9, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: X.L. has received consulting fees from DePuy and FH Ortho and IP royalties from FH Ortho. J.D.K. has received educational support and compensation for services other than consulting from Arthrex and consulting fees from Heron Therapeutics and Flexion Therapeutics. R.L.P. has received educational support from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
An online CME course associated with this article is available for 1 AMA PRA Category 1 Credit™ at http://www.sportsmed.org/aossmimis/Members/Education/AJSM_Current_Concepts_Store.aspx. In accordance with the standards of the Accreditation Council for Continuing Medical Education (ACCME), it is the policy of The American Orthopaedic Society for Sports Medicine that authors, editors, and planners disclose to the learners all financial relationships during the past 12 months with any commercial interest (A ‘commercial interest’ is any entity producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients). Any and all disclosures are provided in the online journal CME area which is provided to all participants before they actually take the CME activity. In accordance with AOSSM policy, authors, editors, and planners’ participation in this educational activity will be predicated upon timely submission and review of AOSSM disclosure. Noncompliance will result in an author/editor or planner to be stricken from participating in this CME activity.
ORCID iDs: Lori Jia  https://orcid.org/0000-0001-7970-7081
https://orcid.org/0000-0001-7970-7081
Robert L. Parisien  https://orcid.org/0000-0002-7562-8375
https://orcid.org/0000-0002-7562-8375
References 3, 6-9, 11,12, 14, 16, 17, 19, 20, 23, 24, 26, 27, 29-31, 33-35, 38-40, 42, 43, 45-51, 54.
References 3, 6, 7, 9, 11, 12, 14, 16, 17, 19, 20, 23, 24, 26, 27, 30, 31, 33-35, 38-40, 42, 43, 45-51.
References
- 1.Abenza-Cano L, Leiva-Arcas A, Vaquero-Cristóbal R, et al. Effect of coronavirus disease 2019 (COVID-19) on elite spanish student-athletes’ perception of the dual career. Front Psychol. 2020;11:620042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aschburner S. Coronavirus pandemic causes NBA to suspend season after player tests positive. Updated March12, 2020. Accessed July 1, 2021. https://www.nba.com/news/coronavirus-pandemic-causes-nba-suspend-season
- 3.Batalla-Gavalda A, Cecilia-Gallego P, Revillas-Ortega F, Beltran-Garrido JV. Variations in the mood states during the different phases of COVID-19’s lockdown in young athletes. Int J Environ Res Public Health. 2021;18(17):9326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bu F, Bone JK, Mitchell JJ, Steptoe A, Fancourt D. Longitudinal changes in physical activity during and after the first national lockdown due to the COVID-19 pandemic in England. Sci Rep. 2021;11(1):17723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clemente-Suárez VJ, Fuentes-García JP, de la Vega Marcos R, Martínez Patiño MJ. Modulators of the personal and professional threat perception of Olympic athletes in the actual COVID-19 crisis. Front Psychol. 2020;11:1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa S, Santi G, di Fronso S, et al. Athletes and adversities: athletic identity and emotional regulation in time of COVID-19. Sport Sci Health. 2020;16(4):609-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dauty M, Menu P, Fouasson-Chailloux A. Effects of the COVID-19 confinement period on physical conditions in young elite soccer players. J Sports Med Phys Fitness. 2021;61(9):1252-1257. [DOI] [PubMed] [Google Scholar]
- 9.Davila-Torres DM, Vilcas-Solís GE, Rodríguez-Vásquez M, Calizaya-Milla YE, Saintila J. Eating habits and mental health among rugby players of the Peruvian pre–selection during the second quarantine due to the COVID-19 pandemic. SAGE Open Med. 2021;9:20503121211043718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Albuquerque Freire L, Tannure M, Sampaio M, et al. COVID-19-related restrictions and quarantine COVID-19: effects on cardiovascular and yo–yo test performance in professional soccer players. Front Psychol. 2020;11:589543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Denerel N, Şenışık S, Köyağasıoğlu O, Çiğdem S, Tunç S. Effects of long–duration home isolation linked to the COVID-19 pandemic on mental health of adolescent athletes. Pediatr Exerc Sci. 2021;33(4):170-176. [DOI] [PubMed] [Google Scholar]
- 12.di Cagno A, Buonsenso A, Baralla F, et al. Psychological impact of the quarantine–induced stress during the coronavirus (COVID-19) outbreak among Italian athletes. Int J Environ Res Public Health. 2020;17(23):8867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elliott S, Drummond MJ, Prichard I, et al. Understanding the impact of COVID-19 on youth sport in Australia and consequences for future participation and retention. BMC Public Health. 2021;21(1):448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Facer-Childs ER, Hoffman D, Tran JN, Drummond SPA, Rajaratnam SMW. Sleep and mental health in athletes during COVID-19 lockdown. Sleep. 2021;44(5):ZSAA261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fikenzer S, Fikenzer K, Laufs U, et al. Impact of COVID-19 lockdown on endurance capacity of elite handball players. J Sports Med Phys Fitness. 2021;61(7):977-982. [DOI] [PubMed] [Google Scholar]
- 16.Fiorilli G, Grazioli E, Buonsenso A, et al. A national COVID-19 quarantine survey and its impact on the Italian sports community: implications and recommendations. PLoS One. 2021;16(3):e0248345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garver MJ, Gordon AM, Philipp NM, Huml MR, Wakeman AJ. Change-event steals “athlete” from “college athlete”: perceived impact and depression, anxiety, and stress. J Multidiscip Healthc. 2021;14:1873-1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gössling S, Scott D, Hall CM. Pandemics, tourism and global change: a rapid assessment of COVID-19. J Sustain Tour. 2021;29(1):1-20. [Google Scholar]
- 19.Gouttebarge V, Ahmad I, Mountjoy M, Rice S, Kerkhoffs G. Anxiety and depressive symptoms during the COVID-19 emergency period: a comparative cross–sectional study in professional football. Clin J Sport Med. 2022;32(1):21-27. [DOI] [PubMed] [Google Scholar]
- 20.Graupensperger S, Benson AJ, Kilmer JR, Evans MB. Social (un)distancing: teammate interactions, athletic identity, and mental health of student–athletes during the COVID-19 pandemic. J Adolesc Health. 2020;67(5):662-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grazioli R, Loturco I, Baroni BM, et al. Coronavirus disease-19 quarantine is more detrimental than traditional off–season on physical conditioning of professional soccer players. J Strength Cond Res. 2020;34(12):3316-3320. [DOI] [PubMed] [Google Scholar]
- 22.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. JPers Soc Psychol. 2003;85(2):348-362. [DOI] [PubMed] [Google Scholar]
- 23.Hagiwara G, Tsunokawa T, Iwatsuki T, Shimozono H, Kawazura T. Relationships among student-athletes’ identity, mental health, and social support in Japanese student–athletes during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(13):7032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Håkansson A, Jönsson C, Kenttä G. Psychological distress and problem gambling in elite athletes during COVID-19 restrictions: a web survey in top leagues of three sports during the pandemic. Int J Environ Res Public Health. 2020;17(18):6693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.IOC. Joint Statement from the International Olympic Committee and the Tokyo 2020Organising Committee. Updated March 24, 2020. Accessed July 1, 2021. https://olympics.com/ioc/news/joint-statement-from-the-international-olympic-committee-and-the-tokyo-2020-organising-committee
- 26.Jagim AR, Luedke J, Fitzpatrick A, et al. The impact of COVID-19-related shutdown measures on the training habits and perceptions of athletes in the United States: a brief research report. Front Sports Act Living. 2020;2:623068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knowles C, Shannon S, Prentice G, Breslin G. Comparing mental health of athletes and non–athletes as they emerge from a COVID-19 pandemic lockdown. Front Sports Act Living. 2021;3:612532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Korkmaz S, Aslan CS, Eyuboğlu E, et al. Impact of detraining process experienced during the COVID-19 pandemic on the selected physical and motor features of football players. Prog Nutr. 2020;22(2)(suppl 2):e2020029. [Google Scholar]
- 29.Leguizamo F, Olmedilla A, Núñez A, et al. Personality, coping strategies, and mental health in high–performance athletes during confinement derived from the COVID-19 pandemic. Front Public Health. 2020;8:561198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martínez-González N, Atienza FL, Tomás I, Duda JL, Balaguer I. The impact of coronavirus disease 2019 lockdown on athletes’ subjective vitality: the protective role of resilience and autonomous goal motives. Front Psychol. 2020;11:612825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuine TA, Biese KM, Petrovska L, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13 000 athletes. J Athl Train. 2020;56(1):11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehrsafar AH, Gazerani P, Moghadam Zadeh A, Jaenes Sánchez JC. Addressing potential impact of COVID-19 pandemic on physical and mental health of elite athletes. Brain Behav Immun. 2020;87:147-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mehrsafar AH, Moghadam Zadeh A, Gazerani P, et al. Mental health status, life satisfaction, and mood state of elite athletes during the COVID-19 pandemic: a follow–up study in the phases of home confinement, reopening, and semi–lockdown condition. Front Psychol. 2021;12:630414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Melnyk YB, Stadnik AV, Pypenko IS, Kostina VV, Yevtushenko DO. Impact of COVID-19 on the social and psychological state of athletes. J Sports Med Phys Fitness. 2022;62(2):297-299. [DOI] [PubMed] [Google Scholar]
- 35.Mon-López D, de la Rubia Riaza A, Hontoria Galán M, Refoyo Roman I. The impact of covid-19 and the effect of psychological factors on training conditions of handball players. Int J Environ Res Public Health. 2020;17(18):6471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oblinger-Peters V, Krenn B. “Time for recovery” or “utter uncertainty”? The postponement of the Tokyo 2020 Olympic Games through the eyes of Olympic athletes and coaches. A qualitative study. Front Psychol. 2020;11:610856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Osburn S. NCAA cancels remaining winter and spring championships. Updated March12, 2020. Accessed July 1, 2021. https://www.ncaa.org/about/resources/media-center/news/ncaa-cancels-remaining-winter-and-spring-championships
- 38.Ozen G, Koc H, Aksoy C. Health anxiety status of elite athletes in COVID-19 social isolation period. Bratisl Lek Listy. 2020;121(12):888-893. [DOI] [PubMed] [Google Scholar]
- 39.Parm Ü, Aluoja A, Tomingas T, Tamm AL. Impact of the COVID-19 pandemic on Estonian elite athletes: survey on mental health characteristics, training conditions, competition possibilities, and perception of supportiveness. Int J Environ Res Public Health. 2021;18(8):6471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pensgaard AM, Oevreboe TH, Ivarsson A. Mental health among elite athletes in Norway during a selected period of the COVID-19 pandemic. BMJ Open Sport Exerc Med. 2021;7(1):e001025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pété E, Leprince C, Lienhart N, Doron J. Dealing with the impact of the COVID-19 outbreak: are some athletes’ coping profiles more adaptive than others? Eur J Sport Sci. 2022;22(2):237-247. doi: 10.1080/17461391.2021.1873422 [DOI] [PubMed] [Google Scholar]
- 42.Pillay L, Janse van Rensburg DCC, Jansen van Rensburg A, et al. Nowhere to hide: the significant impact of coronavirus disease 2019 (COVID-19) measures on elite and semi–elite South African athletes. J Sci Med Sport. 2020;23(7):670-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pons J, Ramis Y, Alcaraz S, et al. Where did all the sport go? Negative impact of COVID-19 lockdown on life–spheres and mental health of Spanish young athletes. Front Psychol. 2020;11:611872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roberts RJ, Lane AM. Mood responses and regulation strategies used during COVID-19 among boxers and coaches. Front Psychol. 2021;12:624119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rubio VJ, Sánchez-Iglesias I, Bueno M, Martin G. Athletes’ psychological adaptation to confinement due to COVID-19: a longitudinal study. Front Psychol. 2020;11:613495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruffault A, Bernier M, Fournier J, Hauw N. Anxiety and motivation to return to sport during the French COVID-19 lockdown. Front Psychol. 2020;11:610882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Şenışık S, Denerel N, Köyağasıoğlu O, Tunç S. The effect of isolation on athletes’ mental health during the COVID-19 pandemic. Phys Sportsmed. 2021;49(2):187-193. [DOI] [PubMed] [Google Scholar]
- 49.Simons C, Martin LA, Balcombe L, Dunn PK, Clark RA. Mental health impact on at–risk high-level athletes during COVID-19 lockdown: a pre-, during and post–lockdown longitudinal cohort study of adjustment disorder. J Sci Med Sport. 2021;24(4):329-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soares LL, Leite LB, Guilherme LQ, et al. Anxiety, sleep quality and mood in elite athletes during the COVID-19 pandemic: a preliminary study. Published online April 19, 2021. J Sports Med Phys Fitness. 2021;10.23736/S0022-4707.21.12276-5 [DOI] [PubMed] [Google Scholar]
- 51.Vaughan RS, Edwards EJ, MacIntyre TE. Mental health measurement in a post Covid-19 world: psychometric properties and invariance of the DASS-21 in athletes and non-athletes. Front Psychol. 2020;11:590559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wade M, Prime H, Johnson D, et al. The disparate impact of COVID-19 on the mental health of female and male caregivers. Soc Sci Med. 2021;275:113801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Washif JA, Mohd Kassim SFA, Lew PCF, Chong CSM, James C. Athlete’s perceptions of a “quarantine” training camp during the COVID-19 lockdown. Front Sports Act Living. 2020;2:622858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.WHO. Coronavirus (COVID-19) dashboard. Updated January15, 2022. Accessed January 15, 2022. https://covid19.who.int/


