Abstract
Background
Combined atlas-axis fractures are rare occurrences with substantially higher rates of neurologic deficits compared with isolated injuries. Given the intricate anatomic relationship between the atlas and axis vertebra, variable fracture patterns may occur, warranting special considerations from surgeons.
Methods
A systematic search of PubMed and EMBASE was performed following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. Relevant studies on acute combined atlas-axis fractures that provided data on patient demographics, presentation (injury mechanism, neurologic deficits, fracture type), management, complications, and study conclusions were reviewed.
Results
A total of 22 articles published from 1977 to 2022, comprising 230 patients, were included in the final analysis. Thirty-seven of the 213 patients (17%) presented with neurologic deficits. The most common atlas injuries were posterior arch fractures (54/169 patients; 32%), combined posterior arch/anterior arch fractures (44/169 patients; 26%), and anterior arch fractures (43/169 patients; 25%). The most common axis injuries were type II odontoid fractures (115/175 patients; 66%). Of the 127 patients managed operatively (127/230 patients; 55%), 45 patients (35%) were treated with C1-C2 posterior spinal fusion, 33 patients (26%) were treated with odontoid screw fixation and anterior/posterior C1-C2 trans-articular screws, 16 patients (13%) were treated with occiputocervical fusion and 12 patients (9%) were treated with odontoid screw fixation alone.
Conclusions
Management strategies are generally based on the type of axis fracture as well as the condition of the transverse ligament. Patients with stable fractures can be successfully managed nonoperatively with a cervical collar or halo immobilization. Combined atlas-axis fractures with an atlantodental interval >5 mm, C1 lateral mass displacement >7 mm, C2-C3 angulation >11° or an MRI demonstrating a disrupted transverse ligament are suggestive of instability and are often successfully managed with surgical intervention. There is no consensus regarding surgical technique.
Keywords: Spine trauma, Cervical spine, Systematic review, Combined atlas axis fractures, Atlantoaxial fractures, Cervical fractures
Introduction
Combined atlas-axis fractures are rare occurrences that account for approximately 4% of all acute cervical spine injuries [1], [2], [3]. Neurologic deficits associated with combined fractures range from 12% to 34%, which are substantially higher than isolated injuries (0%–2%) [4], [5], [6]. Given the intricate anatomic relationship between the atlas and axis vertebra, variable fracture patterns may occur in the setting of cervical trauma. These combined patterns warrant special considerations from surgeons to formulate an optimal treatment plan.
While prior literature advocates that management strategies are generally based on axis fracture characteristics, more recent studies have described additional injury patterns that denote instability and warrant surgery [3,4,[7], [8], [9], [10]]. Furthermore, there are a multitude of patient factors that surgeons must consider, including age, activity level, and comorbidities, which may further complicate management decisions [3,4,7,8,11]. Additionally, there is no consensus in regards to specific surgical treatments, which include posterior cervical instrumented fusion, anterior/ posterior C1-C2 transarticular fixation and anterior odontoid fixation.
The purpose of this investigation is to systematically review the literature to provide clinicians management guidelines in the setting of acute combined atlas and axis fractures.
Methods
A systematic review was conducted according to preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines. The goal was to identify all studies discussing acute combined atlas and axis fractures. Two reviewers (NVM and ASK) independently conducted a literature search in June 2022 using PubMed (MEDLINE) and Ovid (EMBASE) databases. The following terms and Boolean operators were queried in each database: 1 (atlas OR C1 OR Jefferson) AND (axis OR C2 OR dens OR odontoid OR Hangman) AND (fractures); 2 (atlantoaxial) AND (fractures). After duplicates were screened, the search resulted in 1,290 articles in PubMed and EMBASE.
The 2 authors (NVM and ASK) independently examined all articles for inclusion in accordance with PRISMA guidelines as shown in the flow diagram (Fig. 1). First, the 1,290 titles were evaluated for relevance, resulting in 184 studies. Second, the remaining articles underwent further screening by abstract review and relevant references of the included studies were identified. Finally, 46 full text manuscripts were evaluated for inclusion and exclusion criteria for analysis. The main criteria for selection were articles within the aforementioned databases that were written in English, involved patient case studies and provided demographics/ management options specific to combined atlas-axis fractures. Studies in which combined atlas-axis fractures were pooled with isolated cervical injuries were excluded. No time frame was identified regarding publication date. The reviewing authors independently filtered through resulting articles and any discrepancies were coreviewed.
Fig. 1.
PRISMA for the systematic review of combined atlas-axis fractures preferred reporting items for systematic reviews and meta-analyses (PRISMA) demonstrating search and selection criteria for the systematic review of the literature on acute combined atlas and axis fractures.
Using the mentioned inclusion and exclusion criteria, a thorough appraisal of the remaining articles was performed. The following data were extracted from the included articles: patient demographics (age, sex, comorbidities), presentation (injury mechanism, presence of neurologic deficits, atlas/axis fracture type), management, complications, conclusions, and secondary measures. Of the 1,290 articles found in the original search, a total of 22 articles were included in the review. A pooled data analysis was not conducted due to variability in the reported outcomes among included studies.
Results
The 22 articles identified during our literature review were published from 1977 to 2022, totaling 230 patients. A description of each article is presented in Table 1 [1,4,8,9,[11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]]. There were 12 case series, 7 case reports, and 3 retrospective reviews. There were no prospective studies.
Table 1.
Description of articles
| Author | Year | Title | Journal | Type of article (case report, case series, etc.) | Level of evidence |
|---|---|---|---|---|---|
| Lipson [12] | 1977 | Fractures of the atlas associated with fractures of the odontoid process and transverse ligament ruptures | The Journal of Bone and Joint Surgery | Case Series | IV |
| Esses [13] | 1981 | Fracture of the atlas associated with fracture of the odontoid process | Injury | Case Report | IV |
| Deen [14] | 1989 | Combination Jefferson Fracture of C1 and Type II Odontoid Fracture Requiring Surgery: Report of Two Cases | Neurosurgery | Case Series | IV |
| Dickman [4] | 1989 | Neurosurgical management of acute atlas-axis combination fractures | Journal of Neurosurgery | Case Series | IV |
| Guiot [1] | 1999 | Complex atlantoaxial fractures | Journal of Neurosurgery | Retrospective Review | III |
| Vieweg [15] | 2000 | Differential treatment in acute upper cervical spine injuries: a critical review of a single-institution series | Surgical Neurology | Retrospective Review | III |
| Tannoury [16] | 2004 | Multiple Unstable Cervical Fractures With Cord Compromise Treated Nonoperatively A Case Report | Spine | Case Report | IV |
| Agrillo [17] | 2006 | Acute combination fracture of atlas and axis: “triple” anterior screw fixation in a 92-year-old man | Surgical Neurology | Case Report | IV |
| Aicha [18] | 2009 | Surgical management of a combined fracture of the odontoid process with an atlas posterior arch disruption: a review of four cases | Orthopaedics and Traumatology: Surgery & Research | Case Series | IV |
| Q Dean [19] | 2010 | Minimally invasive technique of triple anterior screw fixation for an acute combination atlas-axis fracture: case report and literature review | Spinal Cord | Case Report | IV |
| Wu [20] | 2012 | Management of acute combination atlas-axis fractures with percutaneous triple anterior screw fixation in elderly patients | Orthopaedics & Traumatology: Surgery & Research | Case Series | IV |
| Liu [21] | 2014 | Management of combination fractures of the atlas and axis: a report of four cases and literature review | International Journal of Clinical and Experimental Medicine | Case Series | IV |
| Malagelada [22] | 2015 | Combined Type II Odontoid Fracture With Axis Anterior Arch Fracture: A Case Report in an Elderly Patient | Geriatric Orthopaedic Surgery & Rehabilitation | Case Report | IV |
| Pawar [11] | 2015 | Combined Type II Odontoid Fracture with Jefferson's Fracture Treated with Temporary Internal Fixation | Asian Spine Journal | Case Report | IV |
| Lin [23] | 2016 | Management of combined atlas-axis fractures: a review of forty one cases | International Orthopaedics | Case Series | IV |
| DiDomenico [8] | 2017 | Management of acute combined fractures of the atlas and axis: A retrospective study of two trauma centers | Journal of Craniovertebral Junction and Spine | Retrospective Review | III |
| Josten [24] | 2018 | Odontoid fractures in combination with C1 fractures in the elderly treated by combined anterior odontoid and transarticular C1/2 screw fixation | Archives of Orthopaedic and Trauma Surgery | Case Series | IV |
| Dagtekin [25] | 2018 | Management of occipitocervical junction and upper cervical trauma | Journal of Craniovertebral Junction and Spine | Case Series | IV |
| Takami [26] | 2018 | Combined Fractures Involving the Odontoid and Unilateral Superior Articular Processes of the Axis: A Report of Three Cases and Literature Review | Journal of Orthopaedic Case Reports | Case Series | IV |
| Zhao [9] | 2019 | Management of Combined Atlas Fracture with Type II Odontoid Fracture: A Review of 21 Cases | Indian Journal of Orthopaedics | Case Series | IV |
| Kolz [27] | 2021 | C1 and C2 fractures above a previous fusion treated with internal fixation without fusion | The Journal of Bone and Joint Surgery Case Connector | Case Report | IV |
| Verma [28] | 2022 | Use of Intraoperative Imaging to Preserve C1-C2 Mobility in Complex Atlas-Hangman Fractures | Neurology India | Case Series | IV |
Most patients were male (121/207 patients; 58%), although 3 studies did not report gender [15,18,25]. The mean age of 221 patients with reported data was 58 years. Only 2 studies reported on comorbidities, which included hypertension, myocardiopathy, diabetes, cerebrovascular accident, hypothyroidism, and smoking [8,22]. Thirty-seven of the 213 patients (17%) presented with neurologic deficits, which is consistent with previously reported data [4], [5], [6]. The most common mechanism of injury was fall (118/203 patients; 58%), followed by motor vehicle accidents (65/203 patients; 32%). The demographics, neurologic deficits, and mechanism of injury of included articles are presented in Table 2.
Table 2.
Study demographics
| Reference | Patients (#) | Mean age (SD) | Sex (male) | Comorbidities | Neurologic deficits? | Mechanism |
|---|---|---|---|---|---|---|
| Lipson et al. [12], The Journal of Bone and Joint Surgery, 1977 | 4 | 54.25 (21–71) | 2/4 (50%) | Not Reported | 0/4 (0%) | Fall 3/4 (75%), MVC 1/4 (25%) |
| Esses et al. [13], Injury, 1981 | 1 | 34 | 1/1 (100%) | Not Reported | 1/1 (100%) | Miscellaneous 1/1 (100%) |
| Deen et al. [14], Neurosurgery, 1989 | 2 | 69 | 2/2 (100%) | Not Reported | 0/2 (0%) | Bicycle Accident 1/2 (50%), MCC 1/2 (50%) |
| Dickman et al. [4], Journal of Neurosurgery, 1989 | 25 | 40 (14–82) | 16/25 (64%) | Not Reported | 3/25 (12%) | MVC 13/25 (52%), Fall 7/25 (28%), MCC 2/25 (8%), Miscellaneous 3/25 (12%) |
| Guiot et al. [1], Journal of Neurosurgery, 1999 | 10 | 57 (20–74) | 6/10 (60%) | Not Reported | 3/10 (30%) | Fall 7/10 (70%), MVC 2/10 (20%), Miscellaneous 1/10 (10%) |
| Vieweg et al. [15], Surgical Neurology, 2000 | 10 | 58 (52–79) | Not Reported | Not Reported | Not Reported | Not Reported |
| Tannoury et al. [16], Spine, 2004 | 1 | 17 | 1/1 (100%) | Not Reported | 1/1 (100%) | MVC 1/1 (100%) |
| Agrillo et al. [17], Surgical Neurology, 2006 | 1 | 92 | 1/1 (100%) | Not Reported | 1/1 (100%) | Fall 1/1 (100%) |
| Aicha et al. [18], Orthopaedics and Traumatology: Surgery & Research, 2009 | 4 | 64.5 (20–87) | Not Reported | Not Reported | 2/4 (50%) | Bicycle Accident 2/4 (50%), Fall 1/4 (25%), MVC 1/4 (25%) |
| Q Dean et al. [19], Spinal Cord, 2010 | 1 | 39 | 1/1 (100%) | Not Reported | 0/1 (0%) | Fall 1/1 (100%) |
| Wu et al. [20], Orthopaedics & Traumatology: Surgery & Research, 2012 | 7 | 72.4 (65–84) | 6/7 (85.7%) | Not Reported | Not Reported | Not Reported |
| Liu et al. [21], International Journal of Clinical and Experimental Medicine, 2014 | 4 | 42.75 (18–59) | 3/4 (75%) | Not Reported | 0/4 (0%) | Fall 2/4 (50%), MVC 2/4 (50%) |
| Malagelada et al. [22], Geriatric Orthopaedic Surgery & Rehabilitation, 2015 | 1 | 92 | 1/1 (100%) | HTN, myocardiopathy, CVA | 0/1 (0%) | Fall 1/1 (100%) |
| Pawar and O'Leary [11], Asian Spine Journal, 2015 | 1 | 18 | 1/1 (100%) | Not Reported | 0/1 (0%) | MVC 1/1 (100%) |
| Lin et al. [23], International Orthopaedics, 2016 | 41 | 50.9 (24–78 years) | 28/41 (68%) | Not Reported | 7/41 (17%) | MVC 23/41 (56%), Fall 14/41 (34%), Miscellaneous 4/41 (10%) |
| DiDomenico et al. [8], Journal of Craniovertebral Junction and Spine, 2017 | 48 | 75.6 | 16/48 (33%) | HTN 24/48 (50%), Hypothyroidism 10/48 (20.8%), Type II DM 5/48 (10.4%), Smoking 10/48 (10.4%) | 6/48 (12.5%) | Fall 41/48 (84.5%), MVC 5/48 (10.4%), Miscellaneous 2/48 (4.2%) |
| Josten et al. [24], Archives of Orthopaedic and Trauma Surgery, 2018 | 23 | 84.6 (73–94) *Inclusion criteria age >70* |
9/23 (34.8%) | Not Reported | 0/23 (0%) | Fall 23/23 (100%) |
| Dagtekin et al. [25], Journal of Craniovertebral Junction and Spine, 2018 | 9 | Not Reported | Not Reported | Not Reported | 0/9 (9%) | Not Reported |
| Takami et al. [26], Journal of Orthopaedic Case Reports, 2018 | 3 | 77.7 (65–87) | 1/3 (33.3%) | Not Reported | 0/3 (0%) | Fall 2/3 (66.7%), MVC 1/3 (33.3%) |
| Zhao et al. [9], Indian Journal of Orthopaedics, 2019 | 23 | 52.4 (24–72) | 16/23 (69.6 %) | Not Reported | 9/23 (39.1%) | MVC 12/23 (52.2%), Fall 8/23 (34.8%), Miscellaneous 3/23 (13%) |
| Kolz et al. [27], The Journal of Bone and Joint Surgery Case Connector, 2021 | 1 | 71 | 0/1 (0%) | Not Reported | 0/1 (0%) | Not Reported |
| Verma et al. [28], Neurology India, 2022 | 10 | 47.7 (23–81) | 10/10 (100%) | Not Reported | 4/10 (40%) | Fall 7/10 (70%), MVC 3/10 (30%) |
MVC, motor vehicle collision; MCC, motorcycle collision; HTN, hypertension; CVA, cerebrovascular attack; DM, diabetes.
The most common atlas injuries were posterior arch fractures (54/169 patients; 32%), combined posterior arch/ anterior arch fractures (44/169 patients; 26%), and anterior arch fractures (43/169 patients; 25%). Of note, 4 studies consisting of 61 patients did not specify the type of atlas injury [13,15,23,25]. The most common axis injuries were type II odontoid fractures (115/175 patients; 66%). Three studies consisting of 55 patients were excluded due to no specification of the type of axis fracture or having type II odontoid fractures as part of the inclusion criteria [9,24,25].
Of the 230 patients, 103 underwent nonoperative management (45%). Nonoperative management consisted of a cervical collar or halo vest. Of the 127 patients managed operatively, 45 patients (35%) were treated with C1-C2 posterior spinal fusion, 33 patients (26%) were treated with odontoid screw fixation and anterior/posterior C1-C2 transarticular screws, 16 patients (13%) were treated with occiputocervical fusion and 12 patients (9%) were treated with odontoid screw fixation alone. Of note, one study of 23 patients only assessed patients treated with odontoid screw fixation and anterior C1-C2 transarticular screws [24]. The fracture type, management, complications and study conclusions are presented in Table 3.
Table 3.
Fracture type and management
| Reference | C1 (atlas) fracture type | C2 (axis) fracture type | Treatment | ADI | C2-C3 angulation | Length of stay (days) | Complication (s) | Follow-up (months) | Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| Lipson et al. [12], The Journal of Bone and Joint Surgery, 1977 | Posterior Arch 3/4 (75%) Lateral Mass 1/4 (25%) |
Type II Odontoid 4/4 (100%) | Operative 3/4 (75%): OCF Nonoperative 1/4 (25%): Halo Vest |
Not Reported | Not Reported | Not Reported | None 0/4 (0%) | 27.75 | Staged treatment is recommended with halo immobilization until atlas fracture is healed and then posterior cervical fusion if late atlantoaxial instability |
| Esses et al. [13], Injury, 1981 | Not Reported | Type II Odontoid 1/1 (100%) | Nonoperative 1/1 (100%): C-Collar | Not Reported | Not Reported | Not Reported | None 0/1 (0%) | 4 | Cervical collar immobilization is a valid treatment option in stable, nondisplaced Jefferson-Type II odontoid fractures |
| Deen et al. [14], Neurosurgery, 1989 | Anterior + Posterior Arch 2/2 (100%) | Type II Odontoid 2/2 (100%) |
Operative 2/2 (100%): OCF |
Not Reported | Not Reported | 14 | None 0/2 (0%) | 6 | Posterior cervical fusion indicated in the setting of early or late atlantoaxial instability |
| Dickman et al. [4], Journal of Neurosurgery, 1989 | Multiple Ring Fractures 10/25 (40%), Posterior Arch Fracture 7/25 (28%), Unilateral Ring 6/25 (24%), Lateral Mass 2/25 (8%) | Type II Odontoid 10/25 (40%) Type III Odontoid 5/25 (20%) Hangman 3/25 (12%) Miscellaneous C2 7/25 (28%) |
Nonoperative 21/25 (84%): Halo Vest 18/25 (72%), SOMI Brace 2/25 (8%) Operative 4/25 (16%): C1-C2 PSF 3/25 (12%), OCF 1/25 (4%) |
Not Reported | Not Reported | Not Reported | Nonoperative: Neck Pain 3/21 (14.3%) Operative: Neck Pain 3/4 (75%) |
41 | Operative management based on C2 fracture type, displaced odontoid fractures (>5 mm); Occiput fixation indicated in multiple C1 ring fractures |
| Guiot et al. [1], Journal of Neurosurgery, 1999 | Anterior Arch 2/10 (20%) Posterior Arch 2/10 (20%) Anterior + Posterior Arch 6/10 (60%) |
Type II Odontoid 9/10 (90%) Type III Odontoid/Hangman 1/10 (10%) |
Operative 10/10 (100%): Odontoid screw 6/10 (60%), Posterior transarticular C1-C2 screws 2/10 (20%), Odontoid and anterior transarticular C1-C2 screws 1/10 (10%), Odontoid screw and C2 pedicle screws 1/10 (10%) | Not Reported | Not Reported | Not Reported | None 0/10 (0%) | 28.5 | Odontoid screw fixation preserves motion but requires an intact transverse ligament; C1-C2 transarticular fixation is indicated in transverse ligament injuries |
| Vieweg et al. [15], Surgical Neurology, 2000 | Not Reported | Type II Odontoid 5/10 (50%) Type III Odontoid 1/10 (10%) Hangman 2/10 (20%) Complex 2/10 (20%) |
Nonoperative 2/10 (20%): Halo Vest Operative 8/10 (80%): Odontoid screw 5/8 (63%), C1-C2 PSF 2/8 (25%), OCF 1/8 (12.5%) |
Not Reported | Not Reported | Not Reported | None 0/10 (0%) | 10 | Operative management based on C2 fracture type and atlantoaxial instability |
| Tannoury et al. [16], Spine, 2004 | Posterior Arch 1/1 (100%) | Atypical traumatic spondylolisthesis of C2 1/1 (100%) | Nonoperative 1/1 (100%) Halo Vest, C-Collar | Not Reported | Not Reported | 14 | None 0/1 (0%) | 12 | Halo immobilization is a valid treatment option in complex cervical fractures |
| Agrillo et al. [17], Surgical Neurology, 2006 | Posterior Arch 1/1 (100%) | Type II Odontoid 1/1 (100%) | Operative 1/1 (100%): Odontoid and anterior bilateral transarticular C1-C2 screws | Not Reported | Not Reported | Not Reported | Operative 1/1 (100%): Pneumonia | 6 | Anterior odontoid and transarticular C1-C2 fixation is a valid treatment option in elderly patients |
| Aicha et al. [18], Orthopaedics and Traumatology: Surgery & Research, 2009 | Posterior Arch 4/4 (100%) | Type II Odontoid 4/4 (100%) | Operative 4/4 (100%): Posterior transarticular C1-C2 screw 2/4 (50%), OCF 1/4 (25%), Odontoid screw 1/4 (25%) | Not Reported | Not Reported | Not Reported | Operative: Death 2/4 (50%) | 10.5 | Operative management based on C2 fracture type, displaced odontoid fractures and atlantoaxial instability; C1 wiring should be avoided with posterior arch discontinuity |
| Q Dean et al. [19], Spinal Cord, 2010 | Anterior + Posterior Arch 1/1 (100%) | Type II Odontoid 1/1 (100%) | Operative 1/1 (100%): Odontoid and anterior transarticular C1-C2 screws 1/1 (100%) | Not Reported | Not Reported | 4 | None 0/1 (0%) | 24 | Anterior odontoid and transarticular C1-C2 fixation is a valid treatment option |
| Wu et al. [20], Orthopaedics & Traumatology: Surgery & Research, 2012 | Anterior Arch 2/7 (28.6%) Anterior + Posterior Arch 5/7 (71.4%) |
Type II Odontoid 6/7 (85.7%) Type I Odontoid 1/7 (14.3%) |
Operative 7/7 (100%): Odontoid and anterior transarticular C1-C2 screws 7/7 (100%) |
Not Reported | Not Reported | Not Reported | None 0/7 (0%) | 13.1 | Anterior odontoid and transarticular C1-C2 fixation is a valid treatment option in elderly patients |
| Liu et al. [21], International Journal of Clinical and Experimental Medicine, 2014 | Posterior Arch 2/4 (50%) Anterior + Posterior Arch 2/4 (50%) |
Type II Odontoid 3/4 (75%) Hangman Fracture 1/4 (25%) |
Nonoperative 1/4 (25%): Plaster immobilization Operative 3/4 (75%): Odontoid screw + C1-C2 pedicle screws 2/3 (66.7%), OCF 1/3 (33.3%) |
Not Reported | Not Reported | Not Reported | None 0/4 (0%) | 11.5 | Operative recommended in transverse ligament injuries, displaced odontoid fractures (>5 mm) and C2-C3 angulation >11° |
| Malagelada et al. [22], Geriatric Orthopaedic Surgery & Rehabilitation, 2015 | Anterior Arch 1/1 (100%) | Type II Odontoid 1/1 (100%) | Nonoperative 1/1 (100%): C-collar | Not Reported | Not Reported | 2 | None 0/1 (0%) | 12 | In elderly patients, cervical collar immobilization of C1 anterior arch and Type II odontoid fractures can lead to fibrous nonunion with good functional outcomes |
| Pawar and O'Leary [11], Asian Spine Journal, 2015 | Anterior + Posterior Arch 1/1 (100%) | Type II Odontoid 1/1 (100%) | Operative 1/1 (100%): C1-C2 temporary internal fixation (Left C1 lateral mass and C2 pedicle screws) | Not Reported | Not Reported | Not Reported | None 0/1 (0%) | 12 | C1-C2 temporary internal fixation is a valid treatment option in young patients since it preserves cervical motion |
| Lin et al. [23], International Orthopaedics, 2016 | Not Reported | Type II Odontoid 19/41 (46%) Type III Odontoid 7/41 (17%) Hangman 4/41 (10%) Miscellaneous C2 11/41 (27%) |
Nonoperative 22/41 (53.7%): Halo Vest 19/22 (86.3%), C-Collar 3/22 (13.6%) Operative 19/41 (46.3%): C1-C2 PSF 12/19 (63.2%), C1-C3 PSF 4/19 (21.1%), C2-C3 PSF 1/19 (5.2%), OCF 2/19 (10.5%) |
All Type II/ III Odontoid fractures with ADI >5 mm or LMD >7 mm 16/26 (61.5%) managed operatively | All fractures with C2-C3 angulation >11° 5/41 (12.2%) managed operatively | Not Reported | Nonoperative 2/22 (9%): 1 nonunion, 1 pinsite infection Operative 3/19 (7%): 1 wound infection, 1 hematoma, 1 screw malposition |
19.3 (12–45) | Operative management based on C2 fracture type, atlantoaxial instability (ADI >5 mm, LMD >7 mm) and C2-C3 angulation >11° |
| DiDomenico et al. [8], Journal of Craniovertebral Junction and Spine, 2017 | Anterior Arch 15/48 (31.3%) Posterior Arch 17/48 (35.4%) Anterior + Posterior Arch 16/48 (33.3%) |
Type II Odontoid 35/48 (72.9%) Type III Odontoid 4/48 (8.3%) Hangman 2/48 (4.2%) Miscellaneous C2 1/48 (2.1%) |
Nonoperative 29/48 (60.4%): C-Collar, Halo Vest Operative 19/48 (39.6%): C1-C2 PSF 10 |
Nonoperative: 1.78 mm Operative: 1.94 mm (p=.58) |
Nonoperative: 6.06° Operative: 7.81° (p=.28) |
Nonoperative: 7.2 Operative: 13.5 (p=.001) |
Operative 3/19 (15.8%): 1 vertebral artery injury, 1 intra-op pneumothorax, 1 aspiration pneumonia |
10 | Operative management performed more frequently in the setting of Jefferson fractures |
| Josten et al. [24], Archives of Orthopaedic and Trauma Surgery, 2018 | Anterior Arch 13/23 (56.5%) Posterior Arch 5/23 (21.7%) Anterior + Posterior Arch 5/23 (21.7%) |
Type II Odontoid 23/23 (100%) *Inclusion criteria* |
Operative 23/23 (100%): Odontoid and anterior transarticular C1-C2 screws *Inclusion criteria* |
Not Reported | Not Reported | 15.7 | Operative 13/23 (56.5%): 6 dysphagia, 3 pneumonia, 3 screw loosening, 1 pleura effusion | Not Reported | Anterior odontoid and transarticular C1-C2 fixation is a valid treatment option in elderly patients but with high rates of dysphagia |
| Dagtekin et al. [25], Journal of Craniovertebral Junction and Spine, 2018 | Not Reported | Not Reported | Nonoperative 9/9 (100%): Halo Vest or C-Collar | Not Reported | Not Reported | Not Reported | None 0/9 (0%) | Not Reported | Operative management recommended in displaced Type II odontoid fractures (>6 mm, transverse ligament injuries and unstable Hangman's fracture |
| Takami et al. [26], Journal of Orthopaedic Case Reports, 2018 | Lateral mass + Superior Articular Process 3/3 (100%) | Type III Odontoid 3/3 (100%) | Nonoperative 1/3 (33.%): Halo Vest Operative 2/3 (66.7%): C1-C2 PSF 1/2 (50%), C1-C3 PSF 1/2 (50%) |
Not Reported | Not Reported | Not Reported | Nonoperative 1/3 (33%): Torticollis | 18 | Operative management recommended in C1 lateral mass and C2 superior articular process fractures |
| Zhao et al. [9], Indian Journal of Orthopaedics, 2019 | Anterior Arch 8/23 (34.8%) Posterior Arch 8/23 (34.8%) Anterior + Posterior Arch 3/23 (13.0%) Lateral mass 4/23 (17.4%) |
Type II Odontoid 23/23 (100%) *Inclusion criteria* |
Nonoperative 13/23 (56.5%): Halo Vest 10/13 (76.9%), C-Collar 3/13(23.1%) Operative 10/23 (43.5%): C1-C2 PSF 8/10 (80%), OCF 2/10 (20%) |
Not Reported | Not Reported | Not Reported | Nonoperative 2/13 (9%): 1 nonunion, 1 pinsite infection Operative 2/10 (20%): 1 occipital cervical pain, 1 CSF leak |
23.9 (1542) | Operative management based on C1 fracture type and atlantoaxial instability (ADI >5 mm, LMD >7 mm) |
| Kolz et al. [27], The Journal of Bone and Joint Surgery Case Connector, 2021 | Lateral Mass 1/1 (100%) | Type II Odontoid 1/1 (100%) | Operative 1/1 (100%): C1-C4 temporary internal fixation | Not Reported | Not Reported | Not Reported | None 0/1 (0%) | Not reported | Temporary internal fixation is a valid treatment option in elderly patients with a prior cervical fusion |
| Verma et al. [28], Neurology India, 2022 | Anterior Arch 2/10 (20%) Posterior Arch 4/10 (40%) Anterior + Posterior Arch 3/10 (30%) Lateral Mass 1/10 (10%) |
Type II Odontoid 9/10 (90%) Type I Odontoid 1/10 (10%) |
Nonoperative 1/10 (10%): C-Collar Operative 9/10 (90%): C2 pedicle + C3 lateral mass screws 5/9 (55.6%) OCF 3/9 (33.3%), Posterior transarticular C1-C2 screws 1/9 (11.1%) |
Not Reported | Not Reported | Not Reported | None 0/10 (0%) | 28.7 | Intraoperative CT navigation systems allows for more accurate C2 pedicle screw placement and can preserve C1-C2 rotation by avoiding C1 instrumentation in certain fracture patterns |
ADI, atlantodental interval; OCF, occiputocervical fusion; SOMI, sternal occipital mandibular immobilizer; PSF, posterior spinal fusion; LMD, lateral mass displacement.
Discussion
Management of combination C1-type II odontoid fractures
Similarly to isolated type II odontoid fractures, management strategies involving those in combination with C1 fractures are controversial and require clinicians to consider a multitude of factors. Options include semirigid immobilization (cervical collar), rigid immobilization (halo vest), occiputocervical fusion, posterior C1-C2 fusion, temporary C1-C2 fixation, anterior/ posterior C1-C2 transarticular fixation and anterior odontoid fixation.
Many studies have described semirigid immobilization via a cervical collar as a conservative treatment modality in the setting of combination fractures [3,4]. However, clinicians must note that compared with rigid halo immobilization, cervical collars have decreased union rates and should therefore be reserved for stable fractures in patients without risk factors for nonunion, which include age >40 years, delays in treatment, and smoking [3,11,29,30].
Although halo immobilization provides a rigid external fixation, there are numerous disadvantages. Compared with cervical collars, halo vests are invasive and require a long treatment period with complications of pin loosening, pin site infections and loss of fracture reduction [3,11,23]. Their role in the elderly population is particularly controversial based on the significant morbidity.
Tashjian et al. conducted a retrospective review of 78 elderly patients with odontoid fractures, of which 9 patients had combined C1 fractures [31]. Despite no differences in injury severity or baseline comorbidities from those treated with cervical orthosis or surgery, halo vest immobilization was associated with increased mortality (42% compared with 20%, p=.03) and major complications (66% compared 36%, p=.003) [31].
On the contrary, more recent studies have demonstrated overall successful outcomes with halo vests. Lin et al. conducted a retrospective review of combined atlas-axis fractures, where among the nonoperative patients, 19 of the 22 patients (86.3%) were treated with halo vests, with 2 reported complications (1 nonunion and 1 pin site infection)[23]. Zhao et al. conducted a similar review of combined C1-type II odontoid fractures, where 10 out of the 13 nonoperative patients (76.9%) were placed in halo immobilization with 2 complications (1 nonunion and 1 pin site infection)[9].
In the setting of atlantoaxial instability, surgical intervention is indicated for management of C1-type II odontoid fractures. As the primary stabilizer of the atlantoaxial junction, the transverse ligament must be evaluated by clinicians when determining instability [3].
In 1989, Dickman et al. reported one of the earliest retrospective reviews of combined atlas-axis fractures in literature, which consisted of 25 patients [4]. Of these, 20 patients (80%) were initially treated with rigid immobilization for a median duration of 12 weeks [4]. Four patients underwent initial surgical management (occiput-C2 fusion or C1-C2 fusion) due to an atlantodental interval (ADI) >6 mm on presentation [4]. Of note, 1 patient with an ADI of 5 mm who was initially treated with halo immobilization developed a nonunion and subsequently underwent C1-C2 fusion [4]. Based on his findings, Dickman et al. proposed that combination C1-type II odontoid fractures with an ADI >5 mm suggests atlantoaxial instability and should be considered for early surgical intervention [4]. Several studies following Dickman et al. have corroborated that an ADI >5 mm suggests injury to the transverse ligament, and therefore warrants surgery [4,8,9,11,23].
Initially described by Spence et al. another radiographic parameter of potential transverse ligament injury is if the C1 lateral mass displacement is >7 mm [32]. However, recent radiographic and cadaveric studies have questioned the validity of the “rule of Spence” in assessing transverse ligament injuries and should therefore be reserved as only an adjunct in management [33,34]. Ultimately, magnetic resonance imaging (MRI) should be obtained to evaluate transverse ligament competency.
In addition to atlantoaxial instability, surgery is warranted in type II odontoid fracture patterns at risk for nonunion [35]. These include patients with a fracture gap >2 mm, posterior displacement >5 mm, angulation >11° and highly comminuted fractures [35,36].
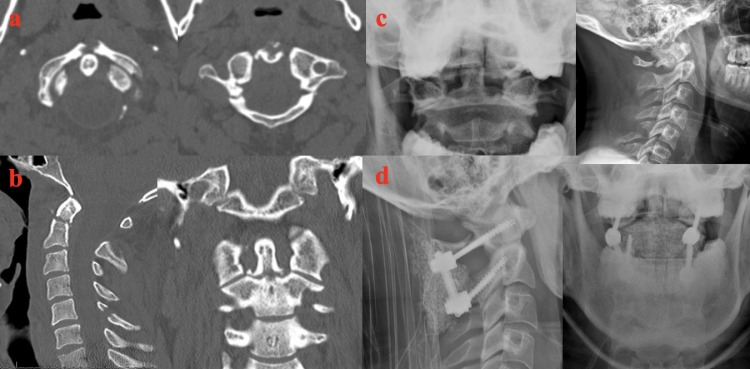
Several surgical techniques have been described in the treatment of combined C1-type II odontoid fractures. Lin et al. [23], DiDomenico et al. [8] and Zhao et al. [9] have reported a combined total of 39 patients treated with posterior C1-C2 fusion and 4 patients treated with occiputocervical fusion. These authors advocate for posterior cervical fusion as it offers immediate stabilization with high rates of fusion, allows for appropriate reduction in the setting of atlantoaxial dislocations and presents less risk of vertebral artery injury compared with trans-articular screws [9,23]. A case of a 30-year-old male who sustained an anterior/ posterior C1 arch fracture, type II odontoid fracture (as well as a C5 spinous process and right C6 facet fracture) after diving into a shallow pool managed with a posterior C1-C2 fusion is presented in Fig. 2.
Fig. 2.
Case presentation of combined Jefferson fracture and type II odontoid fracture. A 30-year-old male was transferred from a tertiary trauma after sustaining a neck injury while diving into a shallow pool. (A and B) He was found to have an anterior and bilateral posterior arch fractures of C1 and a type II odontoid fracture (as well as a C5 spinous process fracture and a right C6 facet fracture). The atlantodental interval (ADI) and lateral mass displacement (LMD) were measured at 2 mm and 6 mm, respectively. On presentation, patient exhibited 5/5 strength but reported transient numbness in his bilateral extremities which resolved spontaneously. He was initially mobilized in a Miami-J with thoracic extension. (C) Upright radiographs were obtained which revealed interval displacement of the odontoid fracture with extension angulation of 40° and gapping measuring 6 mm. (D) Due to risk of nonunion, patient underwent a posterior C1-C2 fusion with postoperative radiographs demonstrating significantly improved atlantoaxial alignment.
Due to significantly restricted motion, occiputocervical fusion should be reserved as a last resort in the setting of C1 pedicle bony defects, comminuted C1 posterior arch fractures or risk of potential vertebral artery injuries [3,9,23]. As a motion-preserving alternative, Pawar and O'Leary [11] and Kolz et al. [27] reported 2 respective cases in which combined C1-type II odontoid fractures were managed with temporary internal fixation followed by hardware removal. The former study involved an 18-year-old male, while the latter was a 71-year-old female who previously underwent a C2-T2 anterior-posterior fusion for cervical spondylosis [11,27]. The authors advocate that in the setting of an intact transverse ligament, temporary internal fixation is a viable alternative in certain patient populations in order to preserve postoperative motion [11,27].
Josten et al. [24], Guiot et al. [1,20], Vieweg et al. [15], and Wu et al. [20] successfully managed a combined 31 patients with an odontoid and anterior C1-C2 transarticular screws, 6 patients with an isolated odontoid screw and 2 patients with a posterior C1-C2 transarticular screw. While isolated anterior odontoid screws allow for maintenance of rotational motion of the atlantoaxial joint, indications should be limited to anterior oblique fracture patterns with minimal displacement and intact transverse ligaments [1,11,24]. With concomitant atlantoaxial instability, C1-C2 transarticular fixation is indicated with multiple described techniques in literature, including Uehara et al. [37] and Wu et al. [20]. These techniques offer significantly less tissue dissection compared with open posterior fusions, while providing adequate atlantoaxial stability [20,24]. Furthermore, Josten et al. noted that although high rates of postoperative dysphagia occurred in the elderly with anterior transarticular fixation, the majority of cases resolved with conservative care and remains a viable option in the elderly population [24]. It must be noted, however, that the course of the vertebral arteries must be carefully evaluated and may necessitate other treatment options in certain anatomic variations [24].
In summary, treatment options include external orthosis via cervical collars or halo immobilization and surgery. There is no optimal surgical technique in the treatment of combination C1-type II odontoid fractures. Clinicians must be cognizant of fracture patterns suggestive of atlantoaxial instability and nonunion to help guide management when treating patients.
Management of combination C1-type III odontoid fractures
In comparison to type II odontoid fractures, C1-type III odontoid fractures are less frequently reported in the literature. Nevertheless, external orthosis with cervical collars or halo vests has been described as an effective management strategy in a majority of cases. Dickman et al. [4], Lin et al. [23], and DiDomenico et al. [8] reported a combined 16 cases of combined type III odontoid fractures with 13/16 patients (81.3%) managed successfully without surgery. Those that were managed operatively exhibited atlantoaxial instability, with an ADI >5 mm or LMD >7 mm [8,23].
Management of combination C1-Hangman fractures
Combination C1-Hangman fractures are generally managed successfully with external orthosis. However, clinicians must be cognizant of particular fracture characteristics that may denote instability. For instance, Lin et al. [23] and Fielding et al. [38] reported combination injuries and noted that C2-C3 angulation >11° suggests instability and warrants surgery. These findings are consistent with prior literature on isolated Hangman fractures, which also describe instability with C2 anterior translation >6 mm and >2 mm movement on flexion/ extension radiographs [39,40].
Additionally, due to suboptimal healing rates with nonoperative care, surgical stabilization is recommended in Levine and Edwards type IIa (flexion-distraction with severe angulation) and III (flexion-compression with bilateral facet dislocations) injuries [39,41]. Operative cases in combination C1-Hangman fractures have been performed with posterior cervical stabilization and fusion in reported literature [15,23,38].
Management of combination C1-miscellaneous C2 body fractures
The management of combination C1-miscellaneous C2 body fractures is nonoperative in the majority of cases. Outcomes have been described by Dickman et al. [4] and Lin et al. [23] with a combined 16 cases successfully treated via rigid (halo vest or sterno-occopital mandibular immobilizer) or semirigid (cervical collar) immobilization.
C1 fracture considerations
Although most literature on combined fractures asserts that operative management is generally based on C2 fracture characteristics, clinicians must be cognizant of C1 fracture patterns that also suggest instability. As with any atlantoaxial injury, the integrity of the transverse ligament must be closely evaluated as it is the key structure that prevents anterior translation of the axis. As previously discussed, C1 lateral mass displacement >7 mm may indicate a transverse ligament injury and should be confirmed with an MRI [32], [33], [34].
DiDomenico et al. conducted a retrospective review of 48 cases of combined atlas-axis fractures, of which 16/48 (33.3%) patients sustained bilateral anterior and posterior arch (Jefferson) fractures, 15/48 (31.3%) patients sustained anterior arch fractures and 17/48 (29.2%) patients sustained posterior arch fractures [8]. He noted that patients with C1 Jefferson fractures tended to be managed more frequently with surgery when comparing those with anterior or posterior arch fractures (p=.030) [8].
Nevertheless, consistent with literature on isolated atlas fractures, Guiot et al. [1] and several studies have described successful cervical collar immobilization in stable Jefferson, anterior arch, posterior arch or lateral mass fractures in combined patterns [9,42]. With atlantoaxial instability, surgical techniques have included occiputocervical fusion, posterior C1-C2 fusion and anterior/posterior transarticular fixation [1,9,15].
Combined atlas-axis fractures in adolescents
We did not use age in our exclusion criteria. Therefore, we captured available data related to adolescents. Four of our studies included patients 19 years or younger. Dickman et al. included patients as young as 14 in their study, but the authors did not provide age-specific [4]. Liu et al. provided one case report of an 18-year-old patient, but this patient refused surgery and was lost to follow-up [21]. Two of the included studies have usable data regarding combined injuries in adolescents. Tannoury et al. is a case report of a 17-year-old male who was involved in a high-speed rollover motor vehicle accident, sustaining a posterior arch fracture of the atlas, atypical traumatic spondylolisthesis of the axis, bilateral pedicle fractures of C3, 80% anterior subluxation of C3 on C4, a burst fracture of C6, and compression fractures of C7 and [16]. The patient had significant motor weakness on presentation. He was treated with cervical traction for 1 week, followed by 9 weeks in a halo vest, followed by an additional 4 weeks in a hard cervical collar. At 4 months after injury, the patient had regained most of his motor function. Finally, Pawar and O'Leary described the case of an 18-year-old male involved in a rollover motor vehicle accident, sustaining a type II odontoid fracture and anterior and posterior arch fractures of the atlas with an unstable left lateral mass of [11]. The patient had no neurologic deficits and MRI demonstrated an intact transverse ligament. The patient was treated with temporary unilateral internal fixation with lateral mass fixation of C1 and pedicle fixation of C2 without fusion to preserve his range-of-motion. CT revealed complete healing by 6 months. The hardware was removed at 9 months. At 1 year, the patient had full cervical range-of-motion. The lack of data on combined injuries in adolescent patients underscores the need for further research in this patient population. These 2 cases demonstrate that these fractures can be treated without fusion or even without surgery in adolescents, even in the setting of concomitant multilevel injuries and motor weakness.
Conclusions
There were a few limitations to this systematic review. The primary limitation was that the level of evidence in the published literature on combined atlas-axis fractures is low, as most studies were case series. Second, the heterogeneity of the data in the reviewed studies made it difficult for the authors to directly compare the studies. Because of these limitations, the authors opted to do a systematic review of the literature rather than a meta-analysis. While there has been several recent studies on combined patterns, this review highlights the lack of prospective and comparison data on different management strategies.
In summary, combined atlas-axis fractures are rare occurrences with substantially higher rates of neurologic deficits compared with isolated injuries. Management strategies are generally based on the type of axis fracture as well as the condition of the transverse ligament, which provides atlantoaxial stability. The majority of patients can be successfully managed with external orthosis via cervical collars or halo immobilization.
Combined atlas-axis fractures with an atlantodental interval >5 mm, C1 lateral mass displacement >7 mm, C2-C3 angulation >11° or MRI findings demonstrating a disrupted transverse ligament are suggestive of instability and often successfully managed with surgical intervention. Additionally, surgery is warranted in setting of potential nonunion with an odontoid fracture gap >2 mm, posterior displacement >5 mm, angulation >11°, highly comminuted fractures or in patients with certain risk factors.
There is no consensus in regards to specific surgical treatments, which include occiputocervical fusion, posterior C1-C2 fusion, temporary C1-C2 fixation, anterior/ posterior C1-C2 transarticular fixation and anterior odontoid fixation. Ultimately, future prospective studies would provide clinicians with more well-defined strategies to optimize patient outcomes.
Funding
Neil V Mohile, Alexander S Kuczmarski, Arya Minaie, Alina Syros, Joseph S Geller, and Motasem Al Maaieh declare no grants, technical support, or corporate support.
Declarations of competing interests
Neil V. Mohile, Alexander S. Kuczmarski, Arya Minaie, Alina Syros, Joseph S. Geller and Motasem Al Maaieh declare that they have no conflicting or competing interests.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: NVM: Nothing to disclose. ASK: Nothing to disclose. AM: Nothing to disclose. AS: Nothing to disclose. JSG: Nothing to disclose. MAM: Nothing to disclose.
References
- 1.Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. 1999;91(2 suppl):139–143. doi: 10.3171/spi.1999.91.2.0139. [DOI] [PubMed] [Google Scholar]
- 2.Gleizes V, Jacquot FP, Signoret F, Feron JM. Combined injuries in the upper cervical spine: clinical and epidemiological data over a 14-year period. Eur Spine J. 2000;9(5):386–392. doi: 10.1007/s005860000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryken TC, Hadley MN, Aarabi B, et al. Management of acute combination fractures of the atlas and axis in adults. Neurosurgery. 2013;72(suppl 2):151–158. doi: 10.1227/NEU.0b013e318276ee55. [DOI] [PubMed] [Google Scholar]
- 4.Dickman CA, Hadley MN, Browner C, Sonntag VK. Neurosurgical management of acute atlas-axis combination fractures. A review of 25 cases. J Neurosurg. 1989;70(1):45–49. doi: 10.3171/jns.1989.70.1.0045. [DOI] [PubMed] [Google Scholar]
- 5.Fujimura Y, Nishi Y, Chiba K, Kobayashi K. Prognosis of neurological deficits associated with upper cervical spine injuries. Paraplegia. 1995;33(4):195–202. doi: 10.1038/sc.1995.44. [DOI] [PubMed] [Google Scholar]
- 6.Kesterson L, Benzel E, Orrison W, Coleman J. Evaluation and treatment of atlas burst fractures (Jefferson fractures) J Neurosurg. 1991;75(2):213–220. doi: 10.3171/jns.1991.75.2.0213. [DOI] [PubMed] [Google Scholar]
- 7.Hadley MN, Walters BC, Grabb PA, et al. Management of combination fractures of the atlas and axis in adults. Neurosurgery. 2002;50(3 suppl):S140–S147. doi: 10.1097/00006123-200203001-00022. [DOI] [PubMed] [Google Scholar]
- 8.DiDomenico J, Abode-Iyamah K, Khanna R, et al. Management of acute combined fractures of the atlas and axis: a retrospective study of two trauma centers. J Craniovertebr Junction Spine. 2017;8(4):311–315. doi: 10.4103/jcvjs.JCVJS_53_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao ZS, Wu GW, Lin J, et al. Management of combined atlas fracture with type II odontoid fracture: a review of 21 cases. Indian J Orthop. 2019;53(4):518–524. doi: 10.4103/ortho.IJOrtho_249_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imura T, Inoue G, Nakazawa T, Saito W, Takaso M. Surgical treatment of an atlantoaxial fracture after a delayed diagnosis in a comatose patient. Eur Spine J. 2015;24(suppl 4):S623–S627. doi: 10.1007/s00586-015-3907-0. [DOI] [PubMed] [Google Scholar]
- 11.Pawar AY, O'Leary PF. Combined type II odontoid fracture with Jefferson's fracture treated with temporary internal fixation. Asian Spine J. 2015;9(6):966–970. doi: 10.4184/asj.2015.9.6.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lipson SJ. Fractures of the atlas associated with fractures of the odontoid process and transverse ligament ruptures. J Bone Joint Surg Am. 1977;59(7):940–943. [PubMed] [Google Scholar]
- 13.Esses S, Langer F, Gross A. Fracture of the atlas associated with fracture of the odontoid process. Injury. 1981;12(4):310–312. doi: 10.1016/0020-1383(81)90207-2. [DOI] [PubMed] [Google Scholar]
- 14.Deen HG, Tolchin S. Combination Jefferson fracture of C1 and type II odontoid fracture requiring surgery: report of two cases. Neurosurgery. 1989;25(2):293–297. doi: 10.1097/00006123-198908000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Vieweg U, Meyer B, Schramm J. Differential treatment in acute upper cervical spine injuries: a critical review of a single-institution series. Surg Neurol. 2000;54(3):203–210. doi: 10.1016/s0090-3019(00)00301-3. discussion 210-201. [DOI] [PubMed] [Google Scholar]
- 16.Tannoury TY, Zmurko MG, Tannoury CA, Anderson DG, Chan DP. Multiple unstable cervical fractures with cord compromise treated nonoperatively: a case report. Spine (Phila Pa 1976) 2004;29(11):E234–E238. doi: 10.1097/00007632-200406010-00024. [DOI] [PubMed] [Google Scholar]
- 17.Agrillo U, Mastronardi L. Acute combination fracture of atlas and axis: "triple" anterior screw fixation in a 92-year-old man: technical note. Surg Neurol. 2006;65(1):58–62. doi: 10.1016/j.surneu.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 18.Ben Aicha K, Laporte C, Akrout W, Atallah A, Kassab G, Jegou D. Surgical management of a combined fracture of the odontoid process with an atlas posterior arch disruption: a review of four cases. Orthop Traumatol Surg Res. 2009;95(3):224–228. doi: 10.1016/j.otsr.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 19.Dean Q, Jiefu S, Jie W, Yunxing S. Minimally invasive technique of triple anterior screw fixation for an acute combination atlas-axis fracture: case report and literature review. Spinal Cord. 2010;48(2):174–177. doi: 10.1038/sc.2009.108. [DOI] [PubMed] [Google Scholar]
- 20.Wu AM, Wang XY, Chi YL, et al. Management of acute combination atlas-axis fractures with percutaneous triple anterior screw fixation in elderly patients. Orthop Traumatol Surg Res. 2012;98(8):894–899. doi: 10.1016/j.otsr.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Liu C, Kuang L, Wang L, Tian J. Management of combination fractures of the atlas and axis: a report of four cases and literature review. Int J Clin Exp Med. 2014;7(8):2074–2080. [PMC free article] [PubMed] [Google Scholar]
- 22.Malagelada F, Tibrewal S, Lucar GA, Jeyaseelan L, Fahmy A, Gonzalez JS. Combined type II odontoid fracture with axis anterior arch fracture: a case report in an elderly patient. Geriatr Orthop Surg Rehabil. 2015;6(1):37–41. doi: 10.1177/2151458514554083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin B, Wu J, Chen ZD, Zeng W, Liu Q, Dai L. Management of combined atlas-axis fractures: a review of forty one cases. Int Orthop. 2016;40(6):1179–1186. doi: 10.1007/s00264-015-3076-0. [DOI] [PubMed] [Google Scholar]
- 24.Josten C, Jarvers JS, Glasmacher S, Spiegl UJ. Odontoid fractures in combination with C1 fractures in the elderly treated by combined anterior odontoid and transarticular C1/2 screw fixation. Arch Orthop Trauma Surg. 2018;138(11):1525–1531. doi: 10.1007/s00402-018-3013-y. [DOI] [PubMed] [Google Scholar]
- 25.Dagtekin A, Avci E, Hamzaoglu V, et al. Management of occipitocervical junction and upper cervical trauma. J Craniovertebr Junct Spine. 2018;9(3):148–155. doi: 10.4103/jcvjs.JCVJS_72_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takami M, Yamada H, Yukawa Y, Kudo Y. Combined fractures involving the odontoid and unilateral superior articular processes of the axis: a report of three cases and literature review. J Orthop Case Rep. 2018;8(2):3–8. doi: 10.13107/jocr.2250-0685.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kolz JM, Hobson SL, Currier BL, Nassr AN. C1 and C2 fractures above a previous fusion treated with internal fixation without fusion: a case report. JBJS Case Connect. 2021;11(2) doi: 10.2106/JBJS.CC.20.00672. [DOI] [PubMed] [Google Scholar]
- 28.Verma S, Singh PK, Agrawal M, et al. Use of intraoperative imaging to preserve C1-C2 mobility in complex Atlas-Hangman fractures. Neurol India. 2022;70(1):209–214. doi: 10.4103/0028-3886.336335. [DOI] [PubMed] [Google Scholar]
- 29.Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976) 2013;38(11):881–886. doi: 10.1097/BRS.0b013e31828314ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schroeder GD, Kepler CK, Kurd MF, et al. A systematic review of the treatment of geriatric type II odontoid fractures. Neurosurgery. 2015;77(suppl 4):S6–14. doi: 10.1227/NEU.0000000000000942. [DOI] [PubMed] [Google Scholar]
- 31.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 32.Spence KF, Jr., Decker S, Sell KW. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am. 1970;52(3):543–549. [PubMed] [Google Scholar]
- 33.Woods RO, Inceoglu S, Akpolat YT, Cheng WK, Jabo B, Danisa O. C1 lateral mass displacement and transverse atlantal ligament failure in Jefferson's fracture: a biomechanical study of the "rule of spence". Neurosurgery. 2018;82(2):226–231. doi: 10.1093/neuros/nyx194. [DOI] [PubMed] [Google Scholar]
- 34.Radcliff KE, Sonagli MA, Rodrigues LM, Sidhu GS, Albert TJ, Vaccaro AR. Does C(1) fracture displacement correlate with transverse ligament integrity? Orthop Surg. 2013;5(2):94–99. doi: 10.1111/os.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31(11 suppl):S53–S60. doi: 10.1097/01.brs.0000217941.55817.52. discussion S61. [DOI] [PubMed] [Google Scholar]
- 36.Hsu WK, Anderson PA. Odontoid fractures: update on management. J Am Acad Orthop Surg. 2010;18(7):383–394. doi: 10.5435/00124635-201007000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Uehara M, Takahashi J, Hirabayashi H, et al. Computer-assisted C1-C2 transarticular screw fixation "Magerl technique" for atlantoaxial instability. Asian Spine J. 2012;6(3):168–177. doi: 10.4184/asj.2012.6.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fielding JW, Francis WR, Jr., Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. Clin Orthop Relat Res. 1989;(239):47–52. [PubMed] [Google Scholar]
- 39.Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman's fractures. Eur Spine J. 2006;15(3):257–269. doi: 10.1007/s00586-005-0918-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coric D, Wilson JA, Kelly DL., Jr. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85(4):550–554. doi: 10.3171/jns.1996.85.4.0550. [DOI] [PubMed] [Google Scholar]
- 41.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67(2):217–226. [PubMed] [Google Scholar]
- 42.Alker GJ, Oh YS, Leslie EV, Lehotay J, Panaro VA, Eschner EG. Postmortem radiology of head neck injuries in fatal traffic accidents. Radiology. 1975;114(3):611–617. doi: 10.1148/114.3.611. [DOI] [PubMed] [Google Scholar]