Abstract
Aims and Objectives
To assess the effects of intensive follow‐up by primary care nurses on cardiovascular disease self‐management and compliance behaviours after myocardial infarction.
Background
Although cardiovascular disease prevention and cardiac rehabilitation take place in hospital settings, a nurse‐led approach is necessary in primary care during the first few months after a myocardial infarction. Therefore, it is important to assess self‐management of cardiovascular disease and levels of compliance with the prescribed diet, physical activity, and medication.
Design
The study used a multicentre, quasi‐experimental, pre‐post design without a control group.
Methods
Patients with acute coronary syndrome from 40 healthcare facilities were included in the study. A total of 212 patients participated in a programme including 11 interventions during the first 12–18 months after myocardial infarction. The following Nursing Outcomes Classification (NOC) outcomes were assessed at baseline and at the end of the intervention: Self‐management: Cardiac Disease (1617) and Compliance Behaviour: Prescribed Diet (1622), Compliance Behaviour: Prescribed Activity (1632), and Compliance Behaviour: Prescribed Medication (1623). Marjory Gordon's functional health patterns and a self‐care notebook were used in each intervention. Pre‐post intervention means were compared using Student's t‐tests for related samples. The results of the study are reported in compliance with the TREND Statement.
Results
A total of 132 patients completed the intervention. The indicators for each NOC outcome and the variations in scores before and after the intensive follow‐up showed a statistically significant improvement (p‐value = 0.000). Compliance Behaviour: Prescribed Diet (pre = 3.7; post = 4.1); Compliance Behaviour: Prescribed Activity (pre = 3.9; post = 4.3); Compliance Behaviour: Prescribed Medication (pre = 3.9; post = 4.7).
Conclusion
Intensive, immediate follow‐up after myocardial infarction improves compliance behaviours and self‐management of heart disease. A combined self‐care and family care approach should be encouraged to empower post‐myocardial infarction patients. To facilitate patients' self‐efficacy, the use of health education tools such as a cardiovascular self‐care notebook can also be helpful.
Relevance to Clinical Practice
This study highlights the benefits of intensive, protocolised, comprehensive patient follow‐up in primary care during the first few months after an acute myocardial infarction (AMI). Primary care nurses train patients in cardiovascular self‐care.
Patient or Public Contribution
Patients were not involved in either the design or the carrying out of the study. However, at the end of the study, they participated in an evaluation process about the utility of the research study and their satisfaction with it. This process was carried out using an ad hoc survey consisting of 10 questions assessing the nursing care and follow‐up inputs that were received.
Keywords: aftercare, myocardial infarction, primary care nursing, self‐care, self‐management, treatment adherence and compliance
What does this paper contribute to the wider global clinical community?
Follow‐up of post‐myocardial infarction patients by primary care nurses improves self‐management of heart disease and compliance with prescribed diet, physical activity, and medication during the first few months after an AMI.
The use of self‐care‐based health education tools increases empowerment and self‐efficacy among patients with chronic cardiovascular disease and their families.
1. INTRODUCTION
Individuals with coronary heart disease (CHD) are at high risk of recurrent events and mortality. Improving lifestyle‐related cardiovascular risk factors (CVRFs), such as maintaining a heart‐healthy diet, engaging in appropriate physical activity, and adhering to drug therapy, is associated with a significantly lower risk of recurrent events. Therefore, guidelines on secondary prevention and cardiac rehabilitation recommend lifestyle‐related interventions (Kotseva et al., 2019). Secondary Prevention and Cardiac Rehabilitation Programmes (SP‐CRPs) in hospital settings have decreased the risk of fatal and non‐fatal cardiovascular events and increased health‐related quality of life (Anderson et al., 2017). SP‐CRPs help to provide a deeper understanding of the chronic progression of the disease. They also enable and empower patients and their families to lead a heart‐healthy lifestyle (scheduled physical activity, heart‐healthy diet, psycho‐emotional support) and to adhere to the therapeutic plan and rigorously control risk factors (Pereira‐Rodríguez et al., 2020).
Self‐care behaviours and therapeutic cooperation from family members foster adherence to the therapeutic plan, which is crucial for mitigating the impact of the disease, reducing complications associated with chronic diseases, and improving quality of life (Duncan et al., 2016; Khalaf et al., 2021). Communication skills in interviews are important to enhance the self‐management of heart disease, boosting patients' self‐care skills and empowering them (Freier et al., 2020).
In the field of primary care, which is the secondary prevention of cardiovascular disease, individual and family care is provided, encouraging patients to take an active role in self‐managing their health‐disease process. The following would also be helpful: individualised counselling; family involvement in care delivery; intensive, protocolised follow‐up of the number of individual and family consultations; use of motivational communication to encourage shared decision‐making between patients and families; and a holistic approach to cardiovascular risk (Wood et al., 2008).
Taxonomies such as the Nursing Outcomes Classification (NOC) can help nurses to quantify and assess patients' conditions and reflect on potential problems to be prevented in chronic diseases. The NOC includes standardised terminology and criteria for describing and assessing the outcomes resulting from nursing interventions.
1.1. Background
The EUROASPIRE V study reports that the vast majority of patients with coronary heart disease have unhealthy habits in relation to diet, smoking, and a sedentary lifestyle, which negatively affect the management of the main CVRFs (Kotseva et al., 2019). However, patients with chronic cardiovascular disease have difficulty maintaining adherence and adherence levels fall considerably 6 months after discharge from hospital (Polsook et al., 2016; Zakeri et al., 2020). The reasons for this include inadequate information, lack of support from family and health professionals (who fail to take patients' needs into consideration), poor perceived self‐efficacy, beliefs, and low levels of patient understanding and motivation to learn about CHD prevention and management (Polsook et al., 2016; Zakeri et al., 2020).
A number of studies and clinical guidelines highlight the effectiveness of nurse‐led SP‐CRPs compared with the conventional approach. The reason for their effectiveness is that they focus on achieving healthier lifestyle changes and improved control of certain CVRFs in patients with established CHD and high‐risk individuals (Minneboo et al., 2017; Snaterse et al., 2016). It is crucial that SP‐CRPs are implemented as soon as possible after hospital discharge as they improve quality of life and reduce mortality and readmission rates (Türen & Enç, 2020). This involves a series of actions that promote adherence to medication, diet, and a follow‐up plan (Zakeri et al., 2020).
After acute coronary syndrome, adherence to behavioural advice on diet, exercise, prescribed medication, and smoking cessation is associated with a substantially lower risk of recurrent cardiovascular events (Chow et al., 2010). It has also been reported that the initiation, duration, and intensity of the intervention are correlated with a better prognosis and self‐management of the disease by patients. Therefore, it is advisable to carry out intensive follow‐up during the first year after hospital discharge (Khalaf et al., 2021; Moreno‐Palanco et al., 2011; Orozco‐Beltran et al., 2013), maintaining and reinforcing a good therapeutic relationship using new technologies (e.g. telephone, internet, videoconferencing). Several studies have demonstrated the effectiveness of primary care nurses in this type of intensive, protocolised follow‐up of post‐myocardial infarction patients due to their organisational set‐up and training (Snaterse et al., 2016).
The ability to develop care plans based on nursing theories and models is a prerequisite for nursing practice. One of the models most suited to primary care nursing is Dorothea Orem's theory of self‐care. She considers self‐care as a learned behaviour aiming to maintain health, recover from illness, and/or cope with the consequences of illness (Solano Villarrubia et al., 2015). Educational nursing interventions for patients that promote cardiovascular self‐care agency outside the hospital setting are ideal to improve CHD (Mohammadpour et al., 2015; Tok Yildiz & Kaşikçi, 2020). Moyra Allen's model and the University of Calgary model advocate families as therapeutic partners who can contribute to improving health and alleviating medical conditions (Thomas, 2018). Consequently, community nurses should consider the structure, development, and roles of the families of post‐myocardial infarction patients (Duncan et al., 2016; Hydzik et al., 2021). In addition, Marjory Gordon's functional health patterns help nurses to harmonise and systematise nursing care for patients with CHD (Mohammadpour et al., 2015; Tok Yildiz & Kaşikçi, 2020).
Taxonomies such as the NOC can help nurses to quantify and assess patients' conditions and reflect on potential problems to be prevented in chronic diseases (Moorhead et al., 2018). The NOC includes standardised terminology and criteria for describing and assessing the outcomes resulting from nursing interventions. The NOC outcomes relating to self‐management of heart disease and adherence behaviours (diet, physical activity and prescribed medication) can be used as indicators to measure secondary cardiovascular prevention outcomes in primary care. Although they are a useful tool for improving communication between nurses and patients, their use in daily clinical practice should be further encouraged to improve the assessment of patients' self‐care.
The primary care model in Spain is based on healthcare facilities with a basic multidisciplinary team (family doctors, paediatricians and nurses) and, in some cases, additional support from physiotherapists and midwives. To optimise SP‐CRPs, in addition to the hospital model, new models such as those involving primary care are proposed to facilitate accessibility, rational allocation of healthcare resources, and prompt initiation of SP‐CRPs after the coronary event (Buckingham et al., 2016). Coordination between hospital SP‐CRP units and healthcare facilities to care for low‐ and medium‐risk patients is currently underway (Arrarte et al., 2020; Campuzano & de Tiedra, 2020). Primary care professionals should take a comprehensive, multidisciplinary approach to CHD, with early, intensive follow‐up immediately after hospital discharge.
To support cardiovascular self‐care, including self‐management and compliance behaviours, the availability of tools to facilitate follow‐up in primary care nurses' practices is crucial. The Madrid Society of Family and Community Nursing, or SEMAP (Sociedad Madrileña de Enfermería Familiar y Comunitaria), along with six Spanish nursing scientific societies, has published the Cuaderno del paciente en autocuidados cardiosaludables (Patient's Heart‐Healthy Self‐Care Notebook) (Lizcano Álvarez et al., 2012). A pilot test was carried out with 10 patients to verify its understandability and suitability as a health education tool. The aim of the notebook was to assist in the self‐management of CVRFs through self‐monitoring, increase patients' knowledge, make the follow‐up plan easier, and enhance communication between professionals in primary care and hospital settings. An added value of this document was that no such tool was available to support cardiovascular self‐care at the time of the study.
The study hypothesised that intensive, protocolised follow‐up with support from an educational tool such as the heart‐healthy self‐care notebook would improve cardiovascular disease self‐management and compliance behaviours in patients who have had a myocardial infarction.
1.2. Aims
The study objective was to assess cardiovascular disease self‐management and compliance behaviours to prescribed treatment among patients with acute coronary syndrome after intensive follow‐up by primary care nurses.
2. METHODS
2.1. Design
The study used a multicentre, quasi‐experimental, pre‐post design without a control group. The results of the study are reported in compliance with the Transparent Reporting of Evaluations with Non‐randomised Designs (TREND) statement (Des Jarlais et al., 2004) (see Appendix S1).
2.2. Setting and participants
The study was carried out from March 2017 to January 2019 in the nurses' offices of 40 primary care facilities in the city of Madrid, Spain.
The inclusion criteria were people who were
aged between 40 and 70 years old who had been diagnosed according to the International Classification of Primary Care (ICPC): K74 (Ischaemic heart disease with angina); K75 (Acute myocardial infarction); K76 (Ischaemic heart disease without angina) (WONKA International Classification Committee, 1998).
able to commit to attending nursing consultations during the study period and to sign the informed consent form.
The exclusion criteria were people who were
cognitively impaired;
unable to read or write in Spanish;
immobilised/unable to travel to the health facility;
suffering from a serious illness with a life expectancy of less than 1 year.
2.3. Participants and recruitment
Nurses were recruited on a voluntary basis. An invitation to participate was emailed to 320 primary care nurses. The Clinical Care Group (CCG) consisted of a total of 59 nurses.
A non‐probability purposive sampling method was used by selecting patients who: visited the nurses' offices at the primary care facilities; met the inclusion criteria; agreed to participate. Each nurse was required to select at least three patients for follow‐up. The study was completed by 53 nurses with a mean of 3.7 patients (1–9). The recruitment period lasted for 5 months (from February 2017 to June 2017).
To measure an unknown prevalence from a finite population (N = 3000), we used the proportion that maximises the variance of the sample proportion estimator (50%) and a 95% confidence level for a 5% level of accuracy. The necessary sample size was estimated to be 384 patients, reducing to 341 after correcting for a finite population. In the end, the study began with a sample of 212 patients (Figure 1).
FIGURE 1.
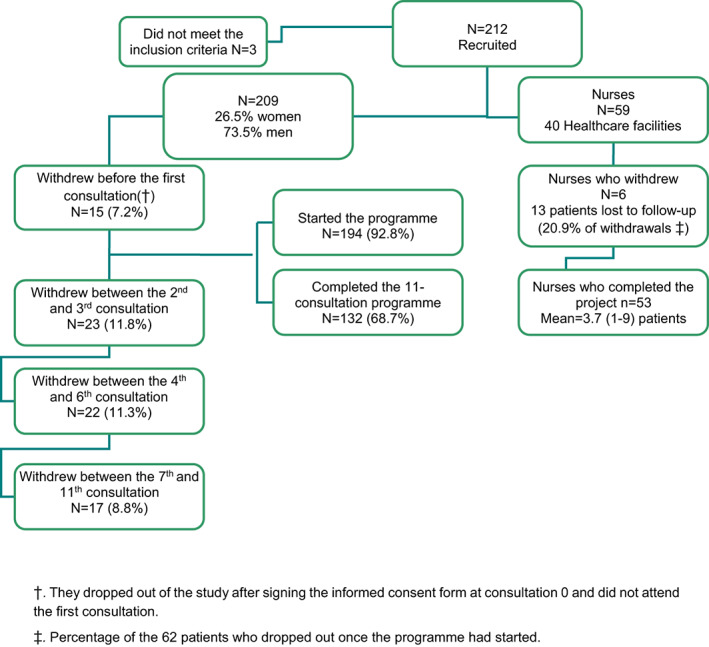
Flow chart showing the study population and recruited nurses.
2.4. Measurements
2.4.1. General information questionnaire
To harmonise the intervention and the use of the heart‐healthy self‐care notebook as far as possible, the nurses were trained to standardise data recording and intervention procedures using the Data Collection Manual (Manual de Recogida de Datos). The manual protocolised the steps to be followed in each nursing consultation, which were recorded on an ad‐hoc computer platform and in the patient's clinical record.
2.4.2. Variables
The following data were recorded: sociodemographic variables (age, sex, education level), clinical variables (blood pressure, diabetes, dyslipidaemia, obesity, tobacco use, previous heart disease according to the ICPC) and examination variables (mean blood pressure, BMI, abdominal circumference).
The outcome variables were the indicator scores for the following NOC outcomes: Self‐management: Cardiac Disease (1617); Compliance Behaviour: Prescribed Diet (1622); Compliance Behaviour: Prescribed Activity (1632); and Compliance Behaviour: Prescribed Medication (1623). Each indicator was assessed on a Likert scale ranging from 1 to 5: 1 (never demonstrated); 2 (rarely demonstrated); 3 (sometimes demonstrated); 4 (frequently demonstrated) and 5 (always demonstrated).
The Clinical Investigators Group (CIG), made up of eight primary care nurses with expertise in cardiovascular care, selected the indicators for each NOC outcome based on the following criteria: relevance to the primary care setting, estimated patient care time, concept clarity, and concept understandability (Table 1).
TABLE 1.
Outcome indicators selected for each Nursing Outcomes Classification (NOC).
| NOC (1623): Compliance behaviour: prescribed medication | |
| Keeps a list of all medications with dose and frequency | |
| Obtains required medication | |
| Knows and informs health professional of all medication being taken (name, dosage, frequency, and how it is being taken) | |
| Takes all medication at intervals prescribed (assessed using the Morinsky‐Green test) | |
| Knows and monitors medication therapeutic effects (why and for what purpose it is being taken) | |
| Knows and monitors medication side effects | |
| NOC (1622): Compliance behaviour: prescribed diet | |
| Participates in setting achievable dietary goals with health professional | |
| Plans and prepares heart‐healthy meals consistent with activity and tastes | |
| Uses nutritional information on labels to guide selections | |
| Knows what food to eat when eating out | |
| Close relatives are aware of the agreed diet | |
| NOC (1632) Compliance behaviour: prescribed activity | |
| Identifies expected benefits of physical activity | |
| Identifies barriers to implement prescribed physical activity | |
| Sets achievable short‐term activity goals with health professional | |
| Participates in prescribed physical activity (3–5 days per week, 30–45 minutes per day, or 150 minutes per week with intensity specific to each patient) | |
| Knows and monitors target heart rate set by health professional | |
| Seeks external reinforcement for performance of health behaviours | |
| Identifies and reports symptoms experienced during activity to health professional | |
| NOC (1617): Self‐management: cardiac disease | |
| Dimension 1 | Uses effective weight control strategies |
| Self‐monitors CVRF parameters (blood pressure, weight, blood glucose, etc.) | |
| Follows recommended heart‐healthy diet | |
| Dimension 2 | Monitors symptom onset, severity, and frequency, and knows symptom relief strategy |
| Knows and accepts medical diagnosis | |
| Keeps appointments with health professional | |
| Has received pneumococcal conjugate vaccine (PCV13, PREvenar©) | |
| Dimension 3 | Practises self‐control to maintain smoking cessation |
| Avoids alcohol consumption or consumes less than 20 grams per day (men) or 10 grams per day (women), preferably red wine | |
| Adjusts daily routine to a heart‐healthy lifestyle | |
| Seeks information about cardiovascular health and participates in cardiovascular health decisions | |
| Dimension 4 | Has received annual influenza vaccine |
| Has received pneumococcal polysaccharide vaccine (PPSV23) | |
| Dimension 5 | Uses stress management strategies |
| Knows the most relevant analytical parameters (lipid, glycaemic, and renal profiles) and their normal levels and is able to interpret them | |
| Reduces weight by more than 5% per year (patients with a BMI > 25) | |
| Dimension 6 | Limits sodium intake to less than 5 grams per day |
| Limiting fat and cholesterol intake | |
2.5. Intervention and data collection procedures
The organisational structure (see Appendix S2) was nodal, consisting of three levels. The first level, the Technical Research Group (TRG), comprised the two principal investigators and two coordinators responsible for monitoring four nodes. The second level, the Clinical Research Group (CRG), comprised eight nurses, each responsible for another node made up of 7–8 nurses from the CCG.
Patients were recruited at nursing or medical consultations and given an appointment for the recruitment or ‘zero’ consultation. The study was explained to them and those interested signed the informed consent form. They were then issued with the heart‐healthy self‐care notebook and the NANDA‐I nursing diagnosis Readiness for Enhanced Health Management (00162) (Herdman & Kamitsuru, 2017) was recorded in their clinical history, as they had expressed a desire to improve the management of their illness over the forthcoming 12 months.
Eleven interventions were implemented during nursing consultations over a period of 12–18 months. Each consultation lasted approximately 30–60 min and was held every 15 to 45 days. Each intervention included protocolised actions (Figure 2).
FIGURE 2.

Structure of the follow‐up protocol used at the interventions.
In the last intervention, the final post‐intervention assessment of all outcome indicators was carried out. To minimise any bias caused by feeling observed and evaluated, which could influence the final assessment, the nurse could not see the assessment, or scores assigned to the indicators in the previous consultations.
The use of the self‐care notebook in nursing consultations consisted of several steps. At the beginning of each consultation, the patient's compliance with notebook use was assessed based on instructions given by the nurse. During each consultation, a section of the notebook corresponding to a particular functional pattern was explained to the patient. At the end of each consultation, the patient was instructed on the tasks to complete at home, for example, readings and self‐recording of measurements (blood pressure, weight, blood glucose, etc.).
2.6. Statistical analyses
To ascertain whether or not there was any variation between the pre‐ and post‐scores of the follow‐up intervention, means were compared using Student's t‐tests for related samples. To verify the reliability of the NOC outcome scales, Cronbach's alpha model for internal consistency was used, with ≥0.7 taken as an optimal value. To check the one‐dimensionality of the scales, an exploratory factor analysis was performed on each outcome.
Given the adequate sample size in each group (n > 30), the normality of the main variables can be assumed by applying the central limit theorem. The statistical significance threshold was set at 5% (α = 0.05). Data processing and analysis were performed using the SPSSv25 statistical package.
2.7. Ethical considerations
The study was approved by the Clinical Research Ethics Committee for the Ramón y Cajal Hospital (code 139/16) and followed the ethical principles set out in the Declaration of Helsinki (‘World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects’, 2013).
The data were handled anonymously and confidentially in compliance with Spanish law (Spanish Organic Law 15/1999 of 13 December on Personal Data Protection, and Spanish Law 14/2007 of 3 July on Biomedical Research). Participants signed an informed consent form after reading the project information sheet.
3. RESULTS
A total of 212 eligible patients were recruited, 3 of whom were excluded for failing to meet the inclusion criteria. The study began with a total of 209 patients. By the end of the study, each nurse had monitored a mean of 3.7 patients (range: 1–9). The intervention was completed by 132 patients (Figure 1). Table 2 shows their clinical characteristics.
TABLE 2.
Baseline demographic and clinical characteristics.
| Valid N | Percentage | Mean | Standard deviation | Median | ||
|---|---|---|---|---|---|---|
| Sex | Male | 97 | 73.5 | 81.66 | 10.92 | 83.00 |
| Female | 35 | 26.5 | 78.66 | 11.05 | 78.00 | |
| High blood pressure | No | 55 | 41.7 | 81.84 | 10.53 | 83.00 |
| Yes | 77 | 58.3 | 80.17 | 11.33 | 82.00 | |
| Tobacco use | Current smoker | 14 | 10.6 | 71.14 | 10.47 | 70.50 |
| Ex‐smoker | 58 | 43.9 | 80.53 | 10.87 | 82.00 | |
| Never smoked | 60 | 45.5 | 83.45 | 10.03 | 84.50 | |
| ICPC | K74 a | 47 | 35.6 | 80.70 | 11.68 | 83.00 |
| K75 b | 82 | 62.1 | 80.85 | 10.78 | 81.50 | |
| K76 c | 3 | 2.3 | 83.67 | 7.57 | 87.00 | |
| Dyslipidaemia | No | 46 | 34.8 | 81.46 | 10.76 | 82.50 |
| Yes | 86 | 65.2 | 80.55 | 11.16 | 82.50 | |
| Diabetes | No | 100 | 75.8 | 81.13 | 10.84 | 83.00 |
| Yes | 32 | 24.2 | 80.03 | 11.60 | 82.00 | |
| BMI | ||||||
| Normal 18.5–24.9 | Normal | 23 | 17.4 | 77.83 | 14.21 | 80.00 |
| Overweight 25–29.9 | Overweight | 68 | 51.5 | 82.26 | 10.60 | 84.50 |
| Obese I 30–34.9 | Obese I | 27 | 20.5 | 81.85 | 8.61 | 82.00 |
| Obese II 35–39.9 | Obese II | 14 | 10.6 | 77.14 | 10.22 | 74.50 |
| Abdominal circumference | 177 | 100 | 101.13 | 11.61 | 100 | |
| Mean blood pressure in the right arm | 191 | 100 | 103.95 | 10.81 | 104.2 | |
| Mean blood pressure in the left arm | 191 | 100 | 101.35 | 13.34 | 103.8 | |
Abbreviations: BMI, body mass index; ICPC, International Classification of Primary Care.
K74, Ischaemic heart disease with angina.
K75, Acute myocardial infarction.
K76, Ischaemic heart disease without angina.
The reliability of each outcome was measured using Cronbach's α: Compliance Behaviour: Prescribed Diet (0.822); Compliance Behaviour: Prescribed Activity (0.859); Compliance Behaviour: Prescribed Medication (0.683); Self‐Management: Cardiac Disease (0.760).
The exploratory factor analysis verified the one‐dimensionality of the three compliance behaviour outcomes. The outcome Self‐Management: Cardiac Disease displayed six dimensions (Table 1).
To analyse the pre‐post intervention scores, a Student's t‐test for related samples was used with each NOC outcome (taking the mean ratings of the indicators for each NOC outcome as the overall measure). The indicators for each NOC outcome and the variations in scores before and after the intensive follow‐up are presented below.
3.1. Compliance behaviour: Prescribed diet (1622)
Participates in setting achievable dietary goals with a health professional.
Plans and prepares heart‐healthy meals consistent with activity and tastes.
Uses nutritional information on labels to guide selections.
Knows what food to eat when eating out.
Close relatives are aware of the agreed diet.
The results show that the mean score rose significantly, by 0.45 points, suggesting that adherence to the prescribed diet throughout the pre‐post follow‐up improved by 0.45 points (Table 3).
TABLE 3.
Compliance behaviour: prescribed diet.
| Paired samples test | ||||||||
|---|---|---|---|---|---|---|---|---|
| Paired differences | t | df | Sig. (2‐tailed) | |||||
| Mean | Std. deviation | Std. error mean | 95% Confidence interval of the difference | |||||
| Lower | Superior | |||||||
| Pre–Post | 0.44697 | 0.83576 | 0.07274 | 0.30306 | 0.59087 | 6.144 | 131 | 0.000 |
| Paired samples statistics | ||||
|---|---|---|---|---|
| Mean | N | Std. deviation | Std. error mean | |
| Pre | 3.7008 | 132 | 0.67919 | 0.05912 |
| Post | 4.1477 | 132 | 0.76228 | 0.06635 |
3.2. Compliance behaviour: prescribed activity (1632)
Identifies expected benefits of physical activity.
Identifies barriers to implement prescribed physical activity.
Sets achievable short‐term activity goals with a health professional.
Participates in prescribed physical activity (3–5 days per week, 30–45 min per day, or 150 min per week with intensity specific to each patient).
Knows and monitors the target heart rate set by a health professional.
Seeks external reinforcement for the performance of health behaviours.
Identifies and reports symptoms experienced during activity to a health professional.
Similarly, the results show that the mean score rose significantly, by 0.33 points, suggesting that adherence to the prescribed physical activity throughout the pre‐post follow‐up improved by 0.33 points (Table 4).
TABLE 4.
Compliance behaviour: prescribed activity
| Paired samples test | t | df | Sig. (2‐tailed) | |||||
|---|---|---|---|---|---|---|---|---|
| Paired differences | ||||||||
| Mean | Std. deviation | Std. error mean | 95% Confidence interval of the difference | |||||
| Lower | Upper | |||||||
| Pre–Post | 0.33117 | 0.73425 | 0.06391 | 0.20474 | 0.45759 | 5.182 | 131 | 0.000 |
| Paired samples statistics | ||||
|---|---|---|---|---|
| Mean | N | Std. deviation | Std. error mean | |
| Pre | 3.9946 | 132 | 0.75292 | 0.06553 |
| Post | 4.3258 | 132 | 0.67315 | 0.05859 |
3.3. Compliance behaviour: prescribed medication (1623)
Keeps a list of all medication with dose and frequency.
Obtains required medication.
Knows and informs the health professional of all medication being taken (name, dosage, frequency, and how it is being taken).
Takes all medication at intervals prescribed (assessed using the Morinsky‐Green test).
Knows and monitors medication therapeutic effects (why and for what purpose it is being taken).
Knows and monitors medication side effects.
The results show that the mean score rose significantly, by 0.76 points, suggesting that adherence to the prescribed medication throughout the pre‐post follow‐up improved by 0.76 points (Table 5).
TABLE 5.
Compliance behaviour: prescribed medication.
| Paired samples test | ||||||||
|---|---|---|---|---|---|---|---|---|
| Paired differences | t | df | Sig. (2‐tailed) | |||||
| Mean | Std. deviation | Std. error mean | 95% Confidence interval of the difference | |||||
| Lower | Upper | |||||||
| Pre‐Post | 0.71645 | 0.62232 | 0.05417 | 0.60930 | 0.82360 | 13.227 | 131 | 0.000 |
| Paired samples statistics | ||||
|---|---|---|---|---|
| Mean | N | Std. deviation | Std. error mean | |
| Pre | 3.9848 | 132 | 0.59212 | 0.05154 |
| Post | 4.7013 | 132 | 0.37171 | 0.03235 |
3.4. Self‐management: cardiac disease (1617)
The results for the indicators (Table 1) show a variable increase in all dimensions of this outcome, with mean scores ranging from 0.25 to 0.9 points for Self‐management: Cardiac Disease. This further confirms the positive impact of the nurse‐led follow‐up intervention on post‐myocardial infarction patients (Table 6).
TABLE 6.
Self‐management: cardiac disease.
| Paired samples statistics | ||||||
|---|---|---|---|---|---|---|
| Mean | N | Std. deviation | Std. error mean | p‐Value, Student's t | ||
| Dimension 1 | SCD1_mean_pre | 3.6894 | 132 | 0.67072 | 0.05838 | 0.000 |
| SCD1_mean_post | 4.0581 | 132 | 0.76445 | 0.06654 | ||
| Dimension 2 | SCD2_mean_pre | 3.5473 | 132 | 0.57636 | 0.05017 | 0.000 |
| SCD2_mean_post | 4.1496 | 132 | 0.70971 | 0.06177 | ||
| Dimension 3 | SCD3_mean_pre | 3.8119 | 132 | 0.81400 | 0.07085 | 0.008 |
| SCD3_mean_post | 3.5278 | 132 | 1.05413 | 0.09175 | ||
| Dimension 4 | SCD4_mean_pre | 3.1061 | 132 | 1.80439 | 0.15705 | 0.000 |
| SCD4_mean_post | 3.9924 | 132 | 1.54449 | 0.13443 | ||
| Dimension 5 | SCD5_mean_pre | 3.2778 | 132 | 0.86558 | 0.07534 | 0.001 |
| SCD5_mean_post | 3.0000 | 132 | 0.84408 | 0.07347 | ||
| Dimension 6 | SCD6_mean_pre | 4.0265 | 132 | 0.75744 | 0.06593 | 0.000 |
| SCD6_mean_post | 4.2879 | 132 | 0.78905 | 0.06868 | ||
Abbreviation: SCD, self‐management: cardiac disease.
Table 7 presents a summary of the overall differential results throughout the pre‐post follow‐up of all outcomes.
TABLE 7.
Pre/post differences for all NOC outcomes.
| Pre | Post | Pre/post | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Difference in means (SD) | p‐Value (Student's t) | |
| CPD | 3.701 (0.679) | 4.148 (0.763) | 0.447 (0.836) | 0.000 |
| CPA | 3.995 (0.753) | 4.326 (0.673) | 0.332 (0.734) | 0.000 |
| CPM | 3.985 (0.592) | 4.703 (0.372) | 0.717 (0.622) | 0.000 |
| SCD1 | 3.690 (0.671) | 4.059 (0.765) | 0.369 (0.790) | 0.000 |
| SCD2 | 3.548 (0.577) | 4.150 (0.710) | 0.603 (0.839) | 0.000 |
| SCD3 | 3.812 (0.815) | 3.528 (1.055) | −0.285 (1.206) | 0.008 |
| SCD4 | 3.107 (1.805) | 3.993 (1.545) | 0.887 (1.531) | 0.000 |
| SCD5 | 3.278 (0.866) | 3.000 (0.845) | −0.278 (0.943) | 0.001 |
| SCD6 | 4.027 (0.758) | 4.288 (0.79) | 0.262 (0.840) | 0.000 |
Abbreviations: CPA, compliance behaviour: prescribed activity; CPD, compliance behaviour: prescribed diet; CPM, compliance behaviour: prescribed medication; SCD, self‐management: cardiac disease (1–6 dimensions); SD, standard deviation.
4. DISCUSSION
SP‐CRPs are known to reduce mortality, decrease cardiovascular complications, and improve patient quality of life, yet these programmes are underused (Kotseva et al., 2019). The implementation of SP‐CRP protocols in primary care is rare, continuity of care between hospital and primary care settings is critical to improve adherence (Arrarte et al., 2020). Primary care provides chronic cardiovascular patients with long‐term therapeutic relationships between themselves, their healthcare professionals, and their families, and continuous follow‐up, mutual trust, a better understanding of the disease, and improved adherence (Wang et al., 2018).
For this reason, it is important that intensive, comprehensive follow‐up is carried out during the first months after the event to improve CVRFs and morbidity and mortality rates. As in previous studies, it has been observed that better results are obtained in this period, enabling patients to improve some of their CVRFs (Huang et al., 2017; Jafari et al., 2020; Nurmeksela et al., 2021; Ruiz‐Bustillo et al., 2019), their self‐efficacy (Polsook et al., 2016), and their levels of empowerment (Lei et al., 2018). Kim et al. confirmed that it is essential to periodically monitor the direct effect of self‐care compliance on changes to left ventricular ejection fraction in outpatients after AMI. They concluded that counselling and education could improve disease awareness and self‐efficacy among patients with low self‐management compliance (Kim et al., 2021).
Studies conducted in primary care settings similar to our own have also reported good results (Brotons et al., 2011; Khalaf et al., 2021; Moreno‐Palanco et al., 2011), but none have been identified using this type of protocolised follow‐up in 11 nursing consultations over such a short period of time. By contrast, one trial (Kennedy et al., 2014) failed to demonstrate the involvement of primary care nurses in patient self‐care, despite them playing a key role in comprehensive care and adherence to the therapeutic regimen (Tharani et al., 2021).
Our study provides evidence of the importance of individualised nursing education focused on self‐care for cardiovascular prevention. Like other studies and meta‐analyses (Baptiste et al., 2016), this approach improves mortality rates and reduces readmissions due to cardiovascular disease. The data from our study confirm that improved self‐care are associated with nurse‐led follow‐up, corroborating other studies such as the RESPONSE 2 trial (Minneboo et al., 2017), which assessed the effect of comprehensive primary care nursing programmes on lifestyle. Unlike other studies (Pajk et al., 2020; Wood et al., 2008), in which nurses devoted all of their clinical care time to the research study, our protocol allows them to incorporate intensive follow‐up into their regular care activities. Another trial has found that nursing interventions increase knowledge and improve self‐care behaviour among patients compared with traditional medical education (Oh & Hwang, 2021).
Another key aspect of our research is the proposal of a follow‐up protocol to standardise care for patients and their families through the assessment of Gordon's functional health patterns. Türen et al. linked this model to improved quality of life and survival rates in patients with heart failure during the first 30 days after admission (Türen & Enç, 2020). Partner involvement in the early stages of AMI also influences lifestyle improvement (Minneboo et al., 2017). As a result, the family consultation at the end of the programme is of particular note. Nurses, patients, and families felt that this was a positive experience. At the consultation, the family receives the nurse's full attention and care, as they are viewed as a therapeutic partner in any chronic disease. In their mixed methods research with 740 families, Jeemon et al. observed that it was important for the family unit to be informed about and involved in heart‐healthy lifestyles (Jeemon et al., 2017). In addition, brief educational interventions with families in primary care settings improve CVRFs (Duncan et al., 2016). This suggests that during the first months after an AMI, family relationships can become dysfunctional so a family approach is essential (Hydzik et al., 2021). Once our study was complete, the need for another family session at the second consultation in the protocol was assessed.
The use of NOC outcomes makes it possible to assess the management of the therapeutic regimen in individuals with chronic conditions with adequate validity while offering new approaches to address this problem (Morilla‐Herrera et al., 2011). Outcomes in heart disease self‐management and compliance behaviour are crucial, which is why our study measured them and identified an improvement in outcome indicators by patients, particularly in terms of adherence to diet and physical activity. It should also be noted that, to achieve these outcome indicators, trials with different methodologies from ours (Köhler et al., 2020; Zakeri et al., 2020) stress the importance of nurse‐led educational programmes, including group education.
Another important, widely studied aspect in post‐myocardial infarction patients is compliance with prescribed medication. Our results show an improvement in this behaviour. Despite not exploring the type of medication, other studies measuring adherence to statins, antihypertensives, etc., highlight the importance of this intervention being implemented in primary care (Kavita et al., 2020; Sotorra‐Figuerola et al., 2021; Zafeiropoulos et al., 2021) and in the first year after infarction (Khalaf et al., 2021). Another clinical trial in secondary prevention showed that a 12‐week nursing intervention after AMI in the community setting improved self‐management of the disease, adherence to medication, and physical activity. This study, unlike ours, took less of an individual approach and relied more on group and telephone management (Shen et al., 2021). That said, our findings show an improvement in the self‐management of heart disease and the level of compliance with the therapeutic regimen in terms of diet, physical activity, and prescribed medication.
The use of the ad‐hoc notebook was an important aspect of this study. Providing support using this type of educational material was found to help patients to monitor their CVRFs and health professionals to communicate, enhancing empowerment and self‐efficacy among patients and their families. Several studies agree on the usefulness of guidelines for patient self‐management and improvement of primary care nurses' skills in cardiovascular care (Kennedy et al., 2014).
Potential limitations of the results include patient attrition. We believe that the study dropout rate after an intensive follow‐up of 11 consultations and more than 1 year is acceptable compared with similar studies, where the number of follow‐up consultations was lower (Brotons et al., 2011; Minneboo et al., 2017; Moreno‐Palanco et al., 2011). One‐fifth of the patients who withdrew from the study were assigned to nurses who did not complete the study. We believe that patients and nurses alike displayed strong adherence to the study. Another limitation was the voluntary nature of nurses' participation, which could lead to patient selection bias. Neither the professionals nor the patients could be blinded. In routine clinical practice, it was not feasible for an external evaluator from outside the care unit to perform the initial and final assessments of the variables. To increase concordance and objectivity, and to improve external validity, nurses were trained in the intervention protocol and the data collection manual. The NOC indicators and items selected for the study are pending validation in terms of accuracy, significance, and utility.
In view of the above and based on their professional experience and previously published studies (Lizcano Álvarez, 2021), the authors believe that primary care nurses are a key component in a protocolised approach to secondary cardiovascular prevention and that continuity of care must be improved alongside hospital cardiac rehabilitation units. This study could help to improve the management of post‐myocardial infarction patients during the first months after an AMI.
The relevance of this study and its impact on clinical practice lies in the fact that it aims to empower chronic post‐myocardial infarction patients and their families during the first few months after an AMI using a protocolised, intensive, comprehensive nursing intervention.
5. CONCLUSIONS
Intensive, comprehensive, protocolised follow‐up of AMI patients by community‐based primary care nurses could improve self‐management of heart disease and adherence to diet, physical activity, and prescribed medication.
To improve both patient and family empowerment and self‐efficacy, this study highlights the importance of gearing cardiovascular nursing care towards patient self‐care training and family engagement. The use of an educational tool, such as a self‐care notebook, improves adherence and enhances the therapeutic relationship.
Further clinical trials are needed to assess improvements in health outcomes by measuring lifestyle‐related CVRFs and to test the level of adherence and self‐efficacy in the longer term. Finally, healthcare institutions should supply protocols and educational materials to primary care facilities to improve secondary cardiovascular prevention.
AUTHOR CONTRIBUTIONS
All authors have met the criteria for authorship as established by the Nursing Open Journal and the Wiley Editing Services and all authors are in agreement with the content of the manuscript. ALA and LCJ: conceptualization; study design; writing – original draft preparation. ATS, BCZ, AAC and MGCE: data analysis and writing – review and editing. All authors were involved in editing and approving the final version of the manuscript.
FUNDING INFORMATION
This project was awarded the 1st National Prize for Best Research Project in Nursing by the Gregorio Marañón General University Hospital in Madrid in 2017.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest to declare.
ETHICS STATEMENT
The study was approved by the Clinical Research Ethics Committee for the Ramón y Cajal Hospital (code 139/16) and followed the ethical principles set out in the Declaration of Helsinki. Participants signed an informed consent form after reading the project information sheet.
Supporting information
Appendix S1
Appendix S2
ACKNOWLEDGMENTS
The authors would like to thank all participants, patients and the primary care teams involved, Clinical Research and Care Group of the Cardiovascular Nursing in Primary Care Network (REccAP) and the Madrid Society of Family and Community Nursing (SEMAP) for making this study possible.
Investigators and Collaborators of Clinical Research and Care Group of the Cardiovascular Nursing in Primary Care Network (REccAP).
Lead Clinical Investigators Group, REccAP:
Cristina Gómez Menor; José Dionisio Benito; Lobato; Juana Mª Gómez Puente; Laura López Köllmer; Sergio Belmonte Sánchez; Teresa Villar Espejo; Laura Iglesias Rus; Gemma Ferrero García, Milagros Rico Blazquez, María Gálvez Fernandez.
Clinical Investigators at primary care facilities:
Adoración Ortega Temiño, Ángeles Álvarez Hermida, Carmen Yegler Velasco, Carolina Guerrero Mártir, Carolina Regacho Ramírez, Encarnación Tornay Muñoz, Eva María Rey Camacho, Eva Molina Alén, Inmaculada Moreno Gª‐Herrera, Leonor Molina Alameda, Leticia Gómez Chacón, Mª Ángeles de Francisco Casado, Mª Beatriz Pérez Vallejo, Mª del Mar Garcia Navarro, Mª José Barras Bermejo, Mª Rosario Campo Martínez, Mª Sonsoles Molina Herráez, Maria Belén Pose García, Maria Luisa Merino Cuesta, Mónica Costumero García, Montserrat Jurado Sueiro, Rosa Cayetano Díaz, Rosa Mª Martínez Ortega, Sagrario Sancha Canales, Vanesa Gonzalez Alonso, Ana Rosa León Casquete, Arancha Martin Belinchón, Aránzazu Ramos Martín, Irene Díaz Jimenez, Mª José Muñoz Cátedra, Adoración Ortega Temiño, Ana Isabel Palacios Calle, Ana María Polo González, Amalia Domínguez González, Concepción Espariz Campano, Esther Blázquez Hernández, Mª Pilar Escudero Socorro, Mª Sandra Hernández Rodríguez, Margarita Ortiz Sánchez, Margarita Vázquez Asenjo, Nieves López Yunquera, Olga Brezo García del Pino, Tania Casasola Gutierrez.
Lizcano‐Álvarez, Á. , Carretero‐Julián, L. , Talavera‐Saez, A. , Cristóbal‐Zárate, B. , Cid‐Expósito, M.‐G. , Alameda‐Cuesta, A. , & (2023). Intensive nurse‐led follow‐up in primary care to improve self‐management and compliance behaviour after myocardial infarction. Nursing Open, 10, 5211–5224. 10.1002/nop2.1758
See Acknowledgments for REccAP Group.
Contributor Information
María‐Gema Cid‐Expósito, Email: gema.cid@urjc.es.
REccAP Group (Red de Enfermería de Cuidados Cardiovasculares en Atención Primaria):
Cristina Gómez Menor, José Dionisio Benito, Juana Mª Gómez Puente, Laura López Köllmer, Sergio Belmonte Sánchez, Teresa Villar Espejo, Laura Iglesias Rus, Gemma Ferrero García, Milagros Rico Blazquez, María Gálvez Fernandez, Adoración Ortega Temiño, Ángeles Álvarez Hermida, Carmen Yegler Velasco, Carolina Guerrero Mártir, Carolina Regacho Ramírez, Encarnación Tornay Muñoz, Eva María Rey Camacho, Eva Molina Alén, Inmaculada Moreno Gª‐Herrera, Leonor Molina Alameda, Leticia Gómez Chacón, Mª Ángeles de Francisco Casado, Mª Beatriz Pérez Vallejo, María del Mar del García Navarro, Mª José Barras Bermejo, Mª Rosario Campo Martínez, Mª Sonsoles Molina Herráez, Maria Belén Pose García, Maria Luisa Merino Cuesta, Mónica Costumero García, Montserrat Jurado Sueiro, Rosa Cayetano Díaz, Rosa Mª Martínez Ortega, Sagrario Sancha Canales, Vanesa Gonzalez Alonso, Ana Rosa León Casquete, Arancha Martín Belinchón, Aránzazu Ramos Martín, Irene Díaz Jimenez, Mª José Muñoz Cátedra, Ana Isabel Palacios Calle, Ana María Polo González, Amalia Domínguez González, Concepción Espariz Campano, Esther Blázquez Hernández, Mª Pilar Escudero Socorro, Mª Sandra Hernández Rodríguez, Margarita Ortiz Sánchez, Margarita Vázquez Asenjo, Nieves López Yunquera, Olga Brezo del García Pino, and Tania Casasola Gutierrez
DATA AVAILABILITY STATEMENT
The data underlying this article will be shared on reasonable request to the corresponding author.
REFERENCES
- Anderson, L. , Brown, J. P. R. , Clark, A. M. , Dalal, H. , Rossau, H. K. , Bridges, C. , & Taylor, R. S. (2017). Patient education in the management of coronary heart disease. Cochrane Database of Systematic Reviews, 6(6), CD008895. 10.1002/14651858.CD008895.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrarte, V. , Campuzano, R. , de Tiedra, C. , Manjón, T. , Alarcón, J. A. , Fernández, R. , Calderón, A. , Castro, A. , Valle, A. , Meroño, O. , Obaya, J. C. , & Lasa, M. (2020). Expert consensus on the coordination of cardiac rehabilitation between cardiology departments and primary care. The RehaCtivAP project. Revista Espanola de Cardiologia Suplementos, 20, 15–21. 10.1016/S1131-3587(20)30020-0 [DOI] [Google Scholar]
- Baptiste, D. L. , Davidson, P. , Groff Paris, L. , Becker, K. , Magloire, T. , & Taylor, L. A. (2016). Feasibility study of a nurse‐led heart failure education program. Contemporary Nurse, 52(4), 499–510. 10.1080/10376178.2016.1229577 [DOI] [PubMed] [Google Scholar]
- Brotons, C. , Soriano, N. , Moral, I. , Rodrigo, M. P. , Kloppe, P. , Rodríguez, A. I. , González, M. L. , Ariño, D. , Orozco, D. , Buitrago, F. , Pepió, J. M. , & Borrás, I. (2011). Randomized clinical trial to assess the efficacy of a comprehensive programme of secondary prevention of cardiovascular disease in general practice: The PREseAP study. Revista Española de Cardiología, 64(1), 13–20. 10.1016/j.rec.2010.06.007 [DOI] [PubMed] [Google Scholar]
- Buckingham, S. A. , Taylor, R. S. , Jolly, K. , Zawada, A. , Dean, S. G. , Cowie, A. , Norton, R. J. , & Dalal, H. M. (2016). Home‐based versus centre‐based cardiac rehabilitation: Abridged Cochrane systematic review and meta‐analysis. Open Heart, 3(2), e000463. 10.1136/openhrt-2016-000463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campuzano, R. , & de Tiedra, C. (2020). Coordination of hospital cardiac rehabilitation units with primary care. Encouraging the creation of community units. Revista Espanola de Cardiologia Suplementos, 20, 13–14. 10.1016/S1131-3587(20)30019-4 [DOI] [Google Scholar]
- Chow, C. K. , Jolly, S. , Rao‐Melacini, P. , Fox, K. A. A. , Anand, S. S. , & Yusuf, S. (2010). Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation, 121(6), 750–758. 10.1161/CIRCULATIONAHA.109.891523 [DOI] [PubMed] [Google Scholar]
- Des Jarlais, D. C. , Lyles, C. , & Crepaz, N. (2004). Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. American Journal of Public Health, 94(3), 361–366. 10.2105/AJPH.94.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan, S. , Goodyear‐Smith, F. , McPhee, J. , Zinn, C. , Grøntved, A. , & Schofield, G. (2016). Family‐centered brief intervention for reducing obesity and cardiovascular disease risk: A randomized controlled trial. Obesity, 24(11), 2311–2318. 10.1002/oby.21602 [DOI] [PubMed] [Google Scholar]
- Freier, C. , Heintze, C. , & Herrmann, W. J. (2020). Prescribing and medical non‐adherence after myocardial infarction: Qualitative interviews with general practitioners in Germany. BMC Family Practice, 21(1), 1–11. 10.1186/s12875-020-01145-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herdman, T. H. , & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions and classification 2018–2020 (11th ed.). Thieme. [Google Scholar]
- Huang, Y. J. , Parry, M. , Zeng, Y. , Luo, Y. , Yang, J. , & He, G. P. (2017). Examination of a nurse‐led community‐based education and coaching intervention for coronary heart disease high‐risk individuals in China. Asian Nursing Research, 11(3), 187–193. 10.1016/j.anr.2017.07.004 [DOI] [PubMed] [Google Scholar]
- Hydzik, P. , Kolarczyk, E. , Kustrzycki, W. , Kubielas, G. , Kałużna‐oleksy, M. , Szczepanowski, R. , & Uchmanowicz, B. (2021). Readiness for discharge from hospital after myocardial infarction: A cross‐sectional study. International Journal of Environmental Research and Public Health, 18(13), 6937. 10.3390/ijerph18136937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafari, F. , Shahriari, M. , Sabouhi, F. , Khosravi‐Farsani, A. , & Eghbali‐Babadi, M. (2020). The effect of a lifestyle management educational program on blood pressure, heart rate, and body mass index in patients with hypertension. ARYA Atherosclerosis, 16(1), 7–15. 10.22122/arya.v16i1.1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeemon, P. , Harikrishnan, S. , Sanjay, G. , Sivasubramonian, S. , Lekha, T. R. , Padmanabhan, S. , Tandon, N. , & Prabhakaran, D. (2017). A PROgramme of lifestyle intervention in families for cardiovascular risk reduction (PROLIFIC study): Design and rationale of a family based randomized controlled trial in individuals with family history of premature coronary heart disease. BMC Public Health, 17(1), 10. 10.1186/s12889-016-3928-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavita, Thakur, J. S. , Vijayvergiya, R. , & Ghai, S. (2020). Task shifting of cardiovascular risk assessment and communication by nurses for primary and secondary prevention of cardiovascular diseases in a tertiary health care setting of Northern India. BMC Health Services Research, 20(1), 10. 10.1186/s12913-019-4864-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, A. , Rogers, A. , Bowen, R. , Lee, V. , Blakeman, T. , Gardner, C. , Morris, R. , Protheroe, J. , & Chew‐Graham, C. (2014). Implementing, embedding and integrating self‐management support tools for people with long‐term conditions in primary care nursing: A qualitative study. International Journal of Nursing Studies, 51(8), 1103–1113. 10.1016/J.IJNURSTU.2013.11.008 [DOI] [PubMed] [Google Scholar]
- Khalaf, K. , Johnell, K. , Austin, P. C. , Tyden, P. , Midlöv, P. , Perez‐Vicente, R. , & Merlo, J. (2021). Low adherence to statin treatment during the 1st year after an acute myocardial infarction is associated with increased 2nd‐year mortality risk – An inverse probability of treatment weighted study on 54 872 patients. European Heart Journal – Cardiovascular Pharmacotherapy, 7(2), 141–147. 10.1093/ehjcvp/pvaa010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köhler, A. K. , et al. (2020). The effect of problem‐based learning after coronary heart disease – A randomised study in primary health care (COR‐PRIM). BMC Cardiovascular Disorders, 20(1), 1–11. 10.1186/s12872-020-01647-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. H. , Hwang, S. Y. , Shin, J. H. , & Lim, Y. H. (2021). Self‐care and related factors associated with left ventricular systolic function in patients under follow‐up after myocardial infarction. European Journal of Cardiovascular Nursing, 20(1), 5–13. 10.1177/1474515120923201 [DOI] [PubMed] [Google Scholar]
- Kotseva, K. , De Backer, G. , De Bacquer, D. , Rydén, L. , Hoes, A. , Grobbee, D. , Maggioni, A. , Marques‐Vidal, P. , Jennings, C. , Abreu, A. , Aguiar, C. , Badariene, J. , Bruthans, J. , Castro Conde, A. , Cifkova, R. , Crowley, J. , Davletov, K. , Deckers, J. , De Smedt, D. , … Wood, D. (2019). Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European Society of Cardiology ESC‐EORP EUROASPIRE V registry. European Journal of Preventive Cardiology, 26(8), 824–835. 10.1177/2047487318825350 [DOI] [PubMed] [Google Scholar]
- Lei, H. , Yang, J. , Kong, L. , Liu, N. , Liu, S. , Yu, N. , Peng, Y. , Wen, Y. , & Tang, J. (2018). Correlations among psychological resilience, self‐efficacy, and negative emotion in acute myocardial infarction patients after percutaneous coronary intervention. Frontiers in Psychiatry, 9, 1. 10.3389/fpsyt.2018.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lizcano Álvarez, Á. , Espejo, M. T. V. , Rodríguez, E. D. , Pérez González, M. J. , García, A. O. , Miranda Camarero, M. V. , Fuster, M. A. , Quirós, E. R. , Castrillo, M. S. , & González, M. D. (2012). Cuaderno del Paciente en autocuidados cardiosaludables. Sociedad de Enfermería Madrileña de Atención Primaria (SEMAP). https://semap.org/wp‐content/uploads/2018/06/Cuaderno_Paciente_Autocuidados_Final.pdf [Google Scholar]
- Lizcano Álvarez, Á. , Villar Espejo, T. , López Köllmer, L. , Gómez Menor, C. , Ledesma Rodríguez, R. , & Fernández Zarataín, G. (2021). The efficacy of an integrated care training program for primary care nurses for the secondary prevention of cardiovascular risk. Enfermeria Clinica, 31(5), 303–312. 10.1016/j.enfcle.2020.10.009 [DOI] [PubMed] [Google Scholar]
- Minneboo, M. , Lachman, S. , Snaterse, M. , Jørstad, H. T. , ter Riet, G. , Boekholdt, S. M. , Scholte op Reimer, W. J. M. , Peters, R. J. G. , Riezebos, R. K. , van Liebergen, R. A. M. , van der Spank, A. , van Dantzig, J. M. , de Milliano, P. A. R. , van Hessen, M. W. J. , Kragten, J. A. , Jaarsma, W. , den Hartog, F. R. , Bartels, G. L. , Aengevaeren, W. R. M. , … de Vries, C. J. (2017). Community‐based lifestyle intervention in patients with coronary artery disease: The RESPONSE‐2 trial. Journal of the American College of Cardiology, 70(3), 318–327. 10.1016/j.jacc.2017.05.041 [DOI] [PubMed] [Google Scholar]
- Mohammadpour, A. , Rahmati Sharghi, N. , Khosravan, S. , Alami, A. , & Akhond, M. (2015). The effect of a supportive educational intervention developed based on the Orem's self‐care theory on the self‐care ability of patients with myocardial infarction: A randomised controlled trial. Journal of Clinical Nursing, 24(11–12), 1686–1692. 10.1111/jocn.12775 [DOI] [PubMed] [Google Scholar]
- Moorhead, S. , Swanson, E. , Johnson, M. , & Maas, M. (2018). Nursing outcomes classification (NOC) (6th ed.). Elsevier. [Google Scholar]
- Moreno‐Palanco, M. A. , Ibáñez‐Sanz, P. , Ciria‐de Pablo, C. , Pizarro‐Portillo, A. , Rodríguez‐Salvanés, F. , & Suárez‐Fernández, C. (2011). Impact of comprehensive and intensive treatment of risk factors concerning cardiovascular mortality in secondary prevention: MIRVAS study. Revista Española de Cardiología, 64(3), 179–185. 10.1016/j.rec.2010.07.002 [DOI] [PubMed] [Google Scholar]
- Morilla‐Herrera, J. C. , Morales‐Asencio, J. M. , Fernández‐Gallego, M. C. , Berrobianco Cobos, E. , & Delgado Romero, A. (2011). Utility and validity of indicators from the nursing outcomes classification as a support tool for diagnosing ineffective self health management in patients with chronic conditions in primary health care. Anales Del Sistema Sanitario de Navarra, 34(1), 51–61. 10.4321/s1137-66272011000100006 [DOI] [PubMed] [Google Scholar]
- Nurmeksela, A. , Vuokko, R. P. , Kettunen, T. , Laukkanen, J. , & Peltokoski, J. (2021). Nurse‐led counseling for coronary artery disease patients: A 1‐year follow‐up study. Nursing & Health Sciences, 23, 678–687. 10.1111/nhs.12852 [DOI] [PubMed] [Google Scholar]
- Oh, Y. H. , & Hwang, S. Y. (2021). Individualized education focusing on self‐management improved the knowledge and self‐management behaviour of elderly people with atrial fibrillation: A randomized controlled trial. International Journal of Nursing Practice, 27(4), e12902. 10.1111/IJN.12902 [DOI] [PubMed] [Google Scholar]
- Orozco‐Beltran, D. , Ruescas‐Escolano, E. , Navarro‐Palazón, A. I. , Cordero, A. , Gaubert‐Tortosa, M. , Navarro‐Perez, J. , Carratalá‐Munuera, C. , Pertusa‐Martínez, S. , Soler‐Bahilo, E. , Brotons‐Muntó, F. , Bort‐Cubero, J. , Nuñez‐Martinez, M. A. , Bertomeu‐Martinez, V. , & Gil‐Guillen, V. F. (2013). Effectiveness of a new health care organization model in primary care for chronic cardiovascular disease patients based on a multifactorial intervention: The PROPRESE randomized controlled trial. BMC Health Services Research, 13(1), 1–9. 10.1186/1472-6963-13-293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajk, A. , Wolfshaut‐Wolak, R. , Doryska, A. , Jankowski, P. , Fornal, M. , Grodzicki, T. , Jennings, C. , KaweckaJaszcz, K. , Kotseva, K. , Pajk, K. , & Wood, D. (2020). Longitudinal effects of a nurse‐managed comprehensive cardiovascular disease prevention program for hospitalized coronary heart disease patients and primary care high‐risk patients. Kardiologia Polska, 78(5), 429–437. 10.33963/KP.15273 [DOI] [PubMed] [Google Scholar]
- Pereira‐Rodríguez, J. E. , Peñaranda‐Florez, D. G. , Pereira‐Rodríguez, R. , Velásquez‐Badillo, X. , Quintero‐Gómez, J. C. , Santamaría‐Pérez, K. N. , Sanchez‐Cajero, O. A. , & Avendaño‐Aguilar, J. A. (2020). Consenso mundial sobre las guías de intervención para rehabilitación cardiaca. Revista Cubana de Cardiologia y Cirugia Cardiovascular, 26(1), 429–437. [Google Scholar]
- Polsook, R. , Aungsuroch, Y. , & Thongvichean, T. (2016). The effect of self‐efficacy enhancement program on medication adherence among post‐acute myocardial infarction. Applied Nursing Research, 32, 67–72. 10.1016/j.apnr.2016.05.002 [DOI] [PubMed] [Google Scholar]
- Ruiz‐Bustillo, S. , Ivern, C. , Badosa, N. , Farre, N. , Marco, E. , Bruguera, J. , Cladellas, M. , Enjuanes, C. , Cainzos‐Achirica, M. , Marti‐Almor, J. , & Comin‐Colet, J. (2019). Efficacy of a nurse‐led lipid‐lowering secondary prevention intervention in patients hospitalized for ischemic heart disease: A pilot randomized controlled trial. European Journal of Cardiovascular Nursing, 18(5), 366–374. 10.1177/1474515119831511 [DOI] [PubMed] [Google Scholar]
- Shen, Q. , He, P. , Wen, M. , Yu, J. , Chen, Y. , Li, J. , & Ouyang, X. (2021). Secondary prevention of coronary heart disease: The effect of a nursing intervention using Cox's interaction model of client health behaviour. Journal of Advanced Nursing, 77(10), 4104–4119. 10.1111/jan.14930 [DOI] [PubMed] [Google Scholar]
- Snaterse, M. , Dobber, J. , Jepma, P. , Peters, R. J. G. , Ter Riet, G. , Boekholdt, S. M. , Buurman, B. M. , & Reimer, W. J. M. S. (2016). Effective components of nurse‐coordinated care to prevent recurrent coronary events: A systematic review and meta‐analysis. Heart, 102(1), 50–56. 10.1136/heartjnl-2015-308050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solano Villarrubia, C. , González Castellanos, L. , González Villanueva, P. , Infantes Rodríguez, J. , Infantes Rodríguez, S. M. , Robledo, E. M. , Torrecilla Abril, M. , & Rico Blázquez, R. (2015). El autocuidado en las personas con enfermedad crónica. Cuadernos de enfermeria familiar y comunitaria II. SEMAP (Sociedad Madrileña de Enfermería Familiar y Comunitaria). https://semap.org/wp‐content/uploads/2015/12/El‐atouidado‐en‐las‐personas‐con‐enfermedad‐cronica‐2015.pdf [Google Scholar]
- Sotorra‐Figuerola, G. , Ouchi, D. , Giner‐Soriano, M. , & Morros, R. (2021). Impact of adherence to drugs for secondary prevention on mortality and cardiovascular morbidity: A population‐based cohort study. IMPACT study. Pharmacoepidemiology and Drug Safety, 1250–1257. 10.1002/pds.5261 [DOI] [PubMed] [Google Scholar]
- Tharani, A. , Van Hecke, A. , Ali, T. S. , & Duprez, V. (2021). Factors influencing nurses’ provision of self‐management support for patients with chronic illnesses: A systematic mixed studies review. International Journal of Nursing Studies, 120, 103983. 10.1016/j.ijnurstu.2021.103983 [DOI] [PubMed] [Google Scholar]
- Thomas, C. D. (2018). Nursing models related to the community‐and the family‐oriented preventive care. Revista Cubana de Enfermeria, 34(4), e2318. [Google Scholar]
- Tok Yildiz, F. , & Kaşikçi, M. (2020). Impact of training based on Orem's theory on self‐care agency and quality of life in patients with coronary artery disease. Journal of Nursing Research, 28(6), e125. 10.1097/JNR.0000000000000406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Türen, S. , & Enç, N. (2020). A comparison of Gordon's functional health patterns model and standard nursing care in symptomatic heart failure patients: A randomized controlled trial. Applied Nursing Research, 53, 151247. 10.1016/j.apnr.2020.151247 [DOI] [PubMed] [Google Scholar]
- Wang, A. , Pollack, T. , Kadziel, L. A. , Ross, S. M. , Mchugh, M. , Jordan, N. , & Kho, A. N. (2018). Impact of practice facilitation in primary care on chronic disease care processes and outcomes: A systematic review. Journal of General Internal Medicine, 33(11), 1968–1977. 10.1007/s11606-018-4581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WONKA International Classification Committee . (1998). International classification of primary care (ICPC‐2) (2nd ed.). Oxford University Press. [Google Scholar]
- Wood, D. A. , Kotseva, K. , Connolly, S. , Jennings, C. , Mead, A. , Jones, J. , Holden, A. , De Bacquer, D. , Collier, T. , De Backer, G. , Faergeman, O. , Buxton, M. J. , Graham, I. , Howard, A. , Logstrup, S. , McGee, H. , Mioulet, M. , Smith, K. , Thompson, D. , … King, H. (2008). Nurse‐coordinated multidisciplinary, family‐based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: A paired, cluster‐randomised controlled trial. The Lancet, 371(9629), 1999–2012. 10.1016/S0140-6736(08)60868-5 [DOI] [PubMed] [Google Scholar]
- World Medical Association . (2013). World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- Zafeiropoulos, S. , Farmakis, I. , Kartas, A. , Arvanitaki, A. , Pagiantza, A. , Boulmpou, A. , Tampaki, A. , Kosmidis, D. , Nevras, V. , Markidis, E. , Papadimitriou, I. , Vlachou, A. , Arvanitakis, K. , Miyara, S. J. , Ziakas, A. , Molmenti, E. P. , Kassimis, G. , Zanos, S. , Karvounis, H. , & Giannakoulas, G. (2021). Reinforcing adherence to lipid‐lowering therapy after an acute coronary syndrome: A pragmatic randomized controlled trial. Atherosclerosis, 323, 37–43. 10.1016/j.atherosclerosis.2021.03.013 [DOI] [PubMed] [Google Scholar]
- Zakeri, M. A. , Khoshnood, Z. , Dehghan, M. , & Abazari, F. (2020). The effect of the continuous care model on treatment adherence in patients with myocardial infarction: A randomised controlled trial. Journal of Research in Nursing, 25(1), 54–65. 10.1177/1744987119890666 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


