Abstract
Background:
Optimal infant feeding is critical for children’s growth and development during their first years of life. Plenty of evidence on ineffective breastfeeding techniques, yet the problem is still deep-rooted and requires further research in Ethiopia.
Objective:
To determine the proportion of ineffective breastfeeding techniques and associated factors among breastfeeding mothers who gave birth in the last 6 months in Sinan Woreda.
Design and methods:
A community-based cross-sectional study was conducted from March 10 to April 8, 2021 with a total of 389 samples. A computer-generated simple random sampling was used to select mothers. An observational checklist and interviewer-administered questionnaires were used. EpiData 4.2 for data entry and SPSS 25 for cleaning and analysis were used. Variables with a p-value < 0.05 and 95% confidence interval (CI) corresponding adjusted odds ratio (AOR) were used to identify factors of ineffective breastfeeding techniques.
Results:
The proportion of ineffective breastfeeding techniques was 66.8%. The mean (SD) age of mothers was 29.4 ± 5.95 years. No formal education [AOR: 5.88 (95% CI: (2.97, 11.65)], primipara [AOR: 4.34 (95% CI: 2.25, 8.36)], home delivery [AOR: 3.02 (95% CI: 1.12, 8.14)], not received breastfeeding counseling during antenatal care [AOR: 4.94 (95% CI: 1.83, 13.36)], breast problem [AOR: 2.62 (95% CI: 1.25, 5.48)], and breastfeeding experience [AOR: 1.82 (95% CI: 1.01, 3.28)] were statistically significant factors.
Conclusions:
The proportion of ineffective breastfeeding techniques 66.8% was unacceptable. Socio-demographic and maternal health care services were identified factors. Strengthening maternal care, improving health education and promotions, and designing appropriate strategies were required.
Keywords: Breastfeeding, techniques, mothers, Sinan Woreda, Ethiopia
Significant for public health.
Breastfeeding is crucial for a child’s growth and development, and it can also save many lives of children and mothers achieved only effective breastfeeding techniques were properly practiced. Breastfeeding techniques are a public health problem, it is still deep-rooted and needs further evidence to improve child and maternal health. The proportion of ineffective breastfeeding techniques was 66.8% which is high compared to various maternal programs that have been implemented nationwide. Women without formal education, primiparity, home delivery, not receiving breastfeeding counseling during ANC follow-up, breast problems, and breastfeeding experience were identified as associated factors of ineffective breastfeeding techniques. This study helps children, mothers, health care providers, policymakers, planners, and researchers to design effective strategies, bring behavioral changes, strengthen the maternal continuum of care, and improve the children’s and mothers’ current deep-rooted nutritional conditions which resulted in ineffective breastfeeding techniques.
Introduction
Optimal infant feeding is critical for children’s growth and development in their first few years of life. Exclusive breastfeeding for the first 6 months, followed by additional complementary feeding until the child is 2 years old.1–5 Breast milk is a perfect mix of vitamins, protein, fat, and antibodies which provides the ideal nutrition for infants.6–8 It is important for baby health, nutrition, and development, as well as improving brain learning readiness and protecting against common childhood illnesses such as necrotizing enterocolitis and sudden infant death syndromes.1,6,7,9,10 The World Health Organization (WHO) recommends that newborns be breastfed within an hour after birth.1,8 More than 820,000 children are lost due to common childhood illnesses, and 20,000 women are lost due to breast cancer, ovarian cancer, type 2 diabetes, and postnatal hemorrhage caused by Ineffective breastfeeding.1,3,11–14
The breastfeeding technique is an art, which is the combination of positioning, attachment, and suckling. Positioning is the technique in which the infant is held in relation to the mother’s body, attachment indicates whether the infant has adequate areola and breast tissue in the mouth, and suckling denotes the drawing of milk into the mouth from the nipple. Its also positioning describes how the baby’s body is close to the mother’s body, attachment defines how the baby’s mouth takes the breast, and suckling describes active sucking, latching, rooting, and audible swallowing.4,6,15,16 Inappropriate breastfeeding posture, wrong breast holding, mastitis, breast swelling, engorgement, cracked nipple, and breast abscess are the result of ineffective breastfeeding techniques. 8 Every year over 4.3 million infant deaths occur in the world before the age of 4 weeks. It accounts for around 33% of all deaths among under-five children and 500 newborns dying per hour as a result of improper breastfeeding.15,17
According to the evidence, 81.5% of mothers in Indonesia have good positioning and 77.8% have good attachment, 18 while 41.2% and 47.4% of mothers in India have correct attachment and positioning, respectively. 19 In Nigeria, the proportion of positioning, attachment, and suckling of breastfeeding techniques are 10.1%, 21.3%, and 23%, respectively. 2 Previous evidence in Areka town revealed that about 25.8% of mothers practiced good positioning. 4 Furthermore, the available evidence from different regions of Ethiopia, 52% in Gondar, 20 63.5% in Ari district, 15 and 56.6% in Harar 6 practiced ineffective breastfeeding techniques.
Mother’s education level, family type, multiparous, place of delivery, lack of knowledge about breastfeeding techniques, and infrastructure were all known factors affecting ineffective breastfeeding techniques of attachment and positioning.4–6,15,18,20–22 Moreover, poor position, attachment, and suckling techniques were associated with mothers with breast lesions such as flat or inverted nipples, engorged breasts, fissures, parity, stretched breasts, neonatal jaundice, and length of hospital stay.18,20,23,24 There are plenty of studies have been conducted in Ethiopia to investigate ineffective breastfeeding techniques at the institutional level, which may not show the correct figure of ineffective breastfeeding techniques, there is a persistent observed problem among lactating women, community-based study recommendations from previous evidence, and insufficient evidence among mothers with children less than 6 months.4,6,15,20,25 This study helps children, mothers, health care providers, policymakers, planners, and researchers to design effective strategies, implement behavioral changes, improve children’s and mothers’ current deep-rooted nutritional conditions, and reduce child and maternal mortality and morbidity caused by ineffective breastfeeding techniques. Therefore, this study aims to determine the proportion of ineffective breastfeeding techniques and associated factors among breastfeeding mothers who gave birth in the last 6 months in Sinan Woreda.
Material and methods
Study design and eligibility criteria
A community-based cross-sectional study was conducted from March 10, 2021 to April 8, 2021. The study was conducted in Sinan Woreda, which is located in the East Gojjam Zone Amhara region. It is 292 km from Bahir Dar and 327 km from Addis Ababa the capital city of Ethiopia. According to the Sinan Woreda health office 2021 figures, the estimated total population is 123,322 with 28,680 males and 94,624 females. There are 19 kebeles in the woreda, and 4118 breastfeeding mothers were recorded. The source population includes all listed breastfeeding mothers who delivered during the last 6 months in Sinan woreda, regardless of the place of birth. Women who gave birth within the last 6 months and breastfed in selected kebele were included in this study; however, mothers who were sick, unable to breastfeed, whose infants were sick, as well as temporary residents in the selected kebele, were excluded.
Sample size determination and sampling procedure
The single population proportion formula was used to determine the sample size by using a 63.5% proportion of ineffective breastfeeding techniques in a study conducted in Ari District Southern Ethiopia, 2020. 15
This was calculated using the following assumptions of Za/2 95% confidence interval (CI) = 1.96, p = proportion of ineffective breastfeeding techniques = 63.5%, precision level (d) = 5%, and including 10% non-response rates, yielding 392 samples. All breastfeeding mothers were documented in each kebele health post. A simple random sampling procedure was used to select 8 kebeles from the woreda’s 19 kebeles. Then, the study participants were assigned to each kebele proportionally by size. All lists of breastfeeding mothers with Community Health Information System (CHIS) house codes in the selected kebeles were obtained from each health post. Finally, breastfeeding mothers who gave birth within the last 6 months with CHIS house codes to each kebeles were sorted and the sample of the study participant was selected by using a simple random computer-generating sampling technique.
Operational definitions
Ineffective breastfeeding technique: It was a composite variable comprising the three constructs (positioning, attachment, and suckling) such that lactating women with at least one of the constructs categorized as “poor” were considered as having ineffective breastfeeding techniques.6,15 This is categorized as an ineffective breastfeeding technique labeled as yes “1” and an effective breastfeeding technique labeled as no “0.”
Positioning: The technique in which the infant is held in relation to the mother’s body. It is categorized out of four (straight and slightly extended, close to the mother’s body, whole body supported, and baby facing toward the mother’s breast) criteria as good positioning: When at least three out of four criteria for infant positioning were fulfilled, average positioning: When any two of the four criteria were correct, and poor positioning: When only one or none criterion has been fulfilled.4,5,15 These three positioning categories merged into two categories by merging good and average positionings into good positioning labeled as “0” and poor positioning as it is labeled as “1.”
Attachment: It indicates whether the infant has enough areola and breast tissue in the mouth. It is categorized out of four (more areola is visible above the baby’s top lip, the baby’s mouth is wide open, the baby’s lower lip is turned outwards, and the baby’s chin is touching or almost touching the breast) criteria as a good attachment: when at least three out of four criteria have been fulfilled, average attachment: When any two of the four criteria have been fulfilled, and poor attachment: When only one or none out of four criteria have been fulfilled.4–6,15 These three attachment categories merged into two categories by merging good and average attachments into good attachments labeled as “0” and poor attachments as it is labeled as “1.”
Suckling: This is the drawing of milk into the mouth from the nipple. It is categorized from three (slow sucks, deep suckling, and sometimes pausing) criteria as a good suckling: At least two out of three criteria have been fulfilled, and poor suckling: Only one or none of three criteria has been fulfilled.6,15,20 Suckling was coded as “0” for good suckling and “1” for poor suckling.
Slow suckling: Suckling rhythm of about one suck per second. 20
Deep suckling: The baby’s cheeks should not draw inward and are rounded during a suckling, evidenced by visible or audible swallowing after every one or two sucks. 20
Sometimes pausing: The baby pauses for a few seconds, allowing the ducts to fill up with milk again. 26
Data collection tools, procedures, and quality control
The questionnaires were prepared in English, translated into Amharic, and back-translated to English to maintain consistency. The tool was adapted from different previous studies and WHO guidelines.4,6,15,20,27,28 A standard observational checklist and an interviewer-administered questionnaire were used collected data. To assess the mother and baby’s position, infant’s mouth attachment, and suckling, the WHO B-R-E-A-S-T-Feed observational checklist was used.27,28 The tool includes socio-demographic and economic, maternal, obstetrical, and neonatal characteristics. Data collectors observed the breastfeeding process for 5 min and recorded the mother and infant’s positioning, attachment to the breast, and effective suckling using the WHO B-R-E-A-S-T Feed observation checklist. It was done by asking the mother to put her infant to the breast and feed it if the infant had not been fed in the previous hour. If the infant had been fed within the last previous hour, then the mother was kindly asked when the infant would have the next feed, and the observation assessment took place when the baby was ready to feed.15,28,29 Eight BSc midwife data collectors and two master public health professional supervisors participated. The tool was previously conducted in the Ethiopian local (Amharic) language.4,6,15,20 To ensure data quality, the questionnaires were carefully designed and used a standard observational checklist, 5% of samples were pre-tested outside of the study setting, data collectors and supervisors were trained, and continuous supervision was held throughout the data collection period.
Data processing and analysis
Data were entered using EpiData version 4.2 and exported to SPSS version 25 for cleaning and analysis. Bivariable and multivariable logistic regression analysis was used to identify the most important variables that have been associated with ineffective breastfeeding techniques. In bivariable logistic regression analysis variables with a p-value ≤ 0.25 were selected for multivariable logistic regression analysis. The Hosmer-Lemeshow test was used to assess the model goodness-of-fit. Descriptive statistics are presented by texts, mean, standard deviation (SD), frequency tables, and figures. In multivariable logistic regression, variables with a p-value < 0.05 and 95% confidence interval (CI) corresponding adjusted odds ratio (AOR) were used to identify factors of ineffective breastfeeding techniques.
Results
Socio-demographic and economic characteristics
In this study, 389 respondents participated with a 99.2% response rate. The mean (SD) age of breastfeeding mothers was 29.4 ± 5.95 years, and (38.3%) of respondents were between the age of 26 and 30. This study’s participants were Amhara nationality and orthodox Christian religion followers. Three-fourths (75.6%) of the study participants lived in rural residents and nearly half (49.4%) of the mothers had no formal education (Table 1).
Table 1.
Socio-demographic and economic characteristics of breastfeeding mothers who gave birth in the last 6 months in Sinan Woreda, 2021 (n = 389).
| Characteristics | Frequency (N) | Percent (%) |
|---|---|---|
| Residence | ||
| Urban | 95 | 24.4 |
| Rural | 294 | 75.6 |
| Age | ||
| <20 years | 55 | 14.2 |
| 20–25 years | 88 | 22.6 |
| 26–30 years | 149 | 38.3 |
| >30 years | 97 | 24.9 |
| Monthly income | ||
| ≤500 birr | 52 | 13.3 |
| 501–1000 birr | 108 | 27.8 |
| ≥1001 birr | 229 | 58.9 |
| Family size | ||
| <5 children | 91 | 23.4 |
| ≥5 children | 298 | 76.6 |
| Marital status | ||
| Single | 6 | 1.5 |
| Married | 361 | 92.8 |
| Divorced | 15 | 3.9 |
| Widow | 7 | 1.8 |
| Education level | ||
| No formal education | 192 | 49.4 |
| Primary education (grades 1–8) | 119 | 30.6 |
| Secondary and above education (grades 9 and above) | 78 | 20.0 |
| Occupation status | ||
| Farmer | 290 | 74.6 |
| Employed | 79 | 20.3 |
| Daily laborer | 20 | 5.1 |
Maternal obstetric and infant characteristics
In this finding, the majority (87.7%) had received Antenatal Care (ANC) follow-up services, 294 (75.6%) had received Postnatal Care (PNC) services, and about 279 (71.7%) had received breastfeeding techniques counseling after delivery. Forty-three (11.1%) and 20 (5.1%) ever had a stillbirth and neonatal death, respectively in this study. Whereas more than two-thirds (70%) of pregnant women were delivered at health centers during this pregnancy. Almost all 389 (99.7%) mothers had singletons delivery, 268 (68.9%) had female sex, and 332 (85.3%) had 42 and above day-old infants (Table 2).
Table 2.
Maternal obstetric and infant characteristics of breastfeeding mothers who gave birth in the last 6 months in Sinan Woreda, 2021 (n = 389).
| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Parity | ||
| Multipara | 240 | 61.7 |
| Primipara | 149 | 38.3 |
| Pregnancy status | ||
| Unplanned | 285 | 73.3 |
| Planned | 104 | 26.7 |
| ANC follow-up | ||
| No | 48 | 12.3 |
| Yes | 341 | 87.7 |
| ANC follow-up (341) | ||
| First | 15 | 4.4 |
| Second | 75 | 21.6 |
| Third | 86 | 24.5 |
| Fourth | 165 | 43.1 |
| BFT counseling during ANC | ||
| No | 83 | 21.3 |
| Yes | 306 | 78.7 |
| Place of delivery | ||
| Home | 53 | 13.6 |
| Hospital | 64 | 16.4 |
| Health center | 272 | 70.0 |
| Mode of delivery | ||
| Cesarean section | 59 | 15.2 |
| Instrument | 133 | 34.2 |
| Spontaneous vaginal | 197 | 50.6 |
| Ever had stillbirth | ||
| No | 346 | 88.9 |
| Yes | 43 | 11.1 |
| Ever had a neonatal death | ||
| No | 369 | 94.9 |
| Yes | 20 | 5.1 |
| BFT counseling after delivery | ||
| No | 110 | 28.3 |
| Yes | 279 | 71.7 |
| PNC follow-up | ||
| No | 95 | 24.4 |
| Yes | 294 | 75.6 |
| PNC follow-up (294) | ||
| First | 201 | 51.7 |
| Second | 55 | 14.1 |
| Third | 38 | 9.8 |
| Infant birth weight | ||
| Very low weight | 10 | 2.0 |
| Low weight | 30 | 8.0 |
| Normal weight | 292 | 75.0 |
| Microsomal | 4 | 1.0 |
| Unknown | 53 | 14.0 |
| Infant age | ||
| <42 days | 57 | 14.7 |
| ≥42 days | 332 | 85.3 |
| Sex of infant | ||
| Male | 121 | 31.1 |
| Female | 268 | 68.9 |
| Colostrum feeding | ||
| No | 128 | 32.9 |
| Yes | 261 | 67.1 |
| Prelacteal feeding | ||
| No | 372 | 95.6 |
| Yes | 17 | 4.4 |
| Skin-to-skin contact | ||
| <60 min | 275 | 70.7 |
| ≥60 min | 114 | 29.3 |
BFT: breastfeeding techniques.
Breastfeeding and other infant feeding-related characteristics
More than two-thirds 274 (70.4%) of lactating mothers had information about breastfeeding techniques. Two hundred forty (61.7%) of mothers had breastfeeding experience and among those more than two-thirds 168 (68.7%) of them have more than 3 years of experience. The majority of breastfeeding mothers 312 (80.2%) reported no breast problems, and 284 (73.0%) had not started complementary feeding for their recent child (Table 3).
Table 3.
Breastfeeding and other infant feeding-related characteristics of mothers who gave birth in the last 6 months in Sinan Woreda, 2021 (n = 389).
| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Information about breastfeeding techniques | ||
| No | 115 | 29.6 |
| Yes | 274 | 70.4 |
| Breastfeeding experience | ||
| No | 149 | 38.3 |
| Yes | 240 | 61.7 |
| Duration of breastfeeding experience (240) | ||
| <1 year | 15 | 6.3 |
| 1–2 years | 60 | 25 |
| >3 years | 165 | 68.7 |
| Breast problems | ||
| No | 312 | 80.2 |
| Yes | 77 | 19.8 |
| Started complementary feeding | ||
| No | 284 | 73.0 |
| Yes | 105 | 27.0 |
| Handwashing before breastfeeding | ||
| No | 200 | 50.9 |
| Yes | 189 | 49.1 |
| Breastfeeding frequency per day | ||
| ≤7 times | 42 | 10.8 |
| 8–12 times | 277 | 71.2 |
| >12 times | 70 | 18.0 |
The proportion of ineffective breastfeeding techniques
In this study, the proportion of ineffective breastfeeding techniques was 66.8% (95% CI: 62, 71). This finding revealed that 40.4% had a poor position, 40.1% had a poor attachment, and 25.2% had poor suckling breastfeeding techniques. Whereas more than one-fourth of breastfeeding mothers practiced average positioning and attachments (Figure 1).
Figure 1.
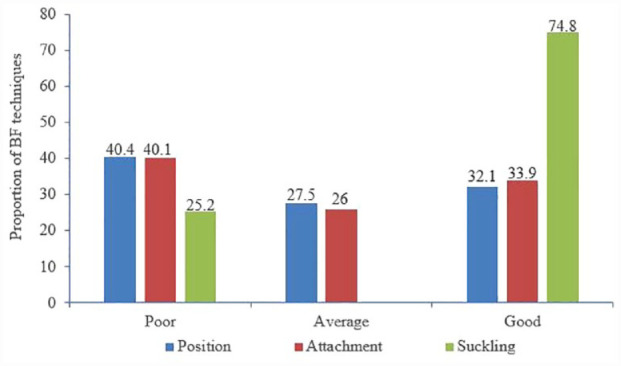
Proportion of breastfeeding techniques among breastfeeding mothers who gave birth in the last 6 months in Sinan Woreda, 2021.
Factors associated with ineffective breastfeeding techniques
In the multivariable logistic regression analysis, the Hosmer-Lemeshow test statistics were 13.65 with a p-value of 0.091. Education level, parity, place of delivery, breastfeeding techniques counseling during ANC follow-up, breast problems, and breastfeeding experience were identified as associated factors of ineffective breastfeeding techniques. The odds of ineffective breastfeeding techniques were 5.88 times higher among women who have no formal education compared to women who have secondary and above education levels [AOR: 5.88 (95% CI: 2.97, 11.65)]. Primipara breastfeeding mothers were more than four times more likely to practice ineffective breastfeeding techniques compared to multipara breastfeeding mothers [AOR: 4.34 (95% CI: 2.25, 8.36)]. Breastfeeding mothers who had home delivery were 3 times more likely to practice ineffective breastfeeding techniques compared to mothers who had health center delivery [AOR: 3.02 (95% CI: 1.12, 8.14)]. Similarly, mothers who have not received breastfeeding techniques counseling during ANC follow-up were nearly 5 times more likely to practice ineffective breastfeeding techniques compared to mothers who have received breastfeeding counseling during ANC follow-up [AOR: 4.94 (95% CI: 1.83, 13.36)]. Moreover, breastfeeding mothers who had breast problems were 2.62 times more likely to practice ineffective breastfeeding techniques compared to counterparts breastfeeding mothers who had no breast problems [AOR: 2.62 (95% CI: 1.25, 5.48)]. Finally, the odds of ineffective breastfeeding were 1.82 times higher among women who have no breastfeeding experience compared to women who have breastfeeding experience [AOR: 1.82 (95% CI: 1.01, 3.28)] (Table 4).
Table 4.
Bivariable and multivariable analysis of ineffective breastfeeding techniques and associated factors among mothers who gave birth in the last 6 months in Sinan Woreda, 2021 (n = 389).
| Variables | Ineffective BFT | COR with 95% CI | AOR with 95% CI | p-Value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Residence | |||||
| Urban | 54 | 41 | 1 | 1 | |
| Rural | 206 | 88 | 1.77 (1.10, 2.86) | 1.54 (0.77, 3.07) | 0.21 |
| Age | |||||
| <20 years | 40 | 15 | 1.64 (0.80, 3.38) | 0.68 (0.27, 1.69) | 0.40 |
| 20–25 years | 62 | 26 | 1.47 (0.79, 2.72) | 0.80 (0.35, 1.82) | 0.59 |
| 26–30 years | 98 | 51 | 1.18 (0.69, 2.01) | 0.92 (0.48, 1.75) | 0.80 |
| >30 years | 60 | 37 | 1 | 1 | |
| Monthly income | |||||
| ≤500 birr | 37 | 15 | 1.40 (0.73–2.71) | 0.83 (0.37, 1.87) | 0.65 |
| 501–1000 birr | 77 | 31 | 1.41 (0.86–2.32) | 1.05 (0.57, 1.93) | 0.86 |
| ≥1001 birr | 146 | 83 | 1 | 1 | |
| Education level | |||||
| No formal education | 155 | 37 | 4.41 (2.49, 7.80) | 5.88 (2.97, 11.65)* | 0.001 |
| Primary education | 67 | 52 | 1.36 (0.76, 2.40) | 1.59 (0.80, 3.17) | 0.18 |
| Secondary and above education | 38 | 40 | 1 | 1 | |
| Occupation | |||||
| Farmer | 198 | 92 | 1 | 1 | |
| Employed | 47 | 32 | 0.68 (0.40, 1.14) | 0.71 (0.36, 1.42) | 0.33 |
| Daily laborer | 15 | 5 | 1.39 (0.49, 3.95) | 1.75 (0.49, 6.23) | 0.39 |
| Parity | |||||
| Primiparity | 118 | 31 | 2.62(1.64, 4.21) | 4.34 (2.25, 8.36)* | 0.001 |
| Multi parity | 142 | 98 | 1 | 1 | |
| Place of delivery | |||||
| Home | 46 | 7 | 3.88 (1.69, 8.92) | 3.02 (1.12, 8.14) | 0.029 |
| Hospital | 43 | 21 | 1.21 (0.68, 2.15) | 1.10 (0.55, 2.18) | 0.78 |
| Health center | 171 | 101 | 1 | 1 | |
| ANC follow-up | |||||
| No | 43 | 5 | 4.91 (1.89, 12.73) | 0.77 (0.18, 3.20) | 0.72 |
| Yes | 217 | 124 | 1 | 1 | |
| BFT counseling during ANC | |||||
| No | 72 | 11 | 4.11 (2.09, 8.07) | 4.94 (1.83, 13.36) | 0.002 |
| Yes | 188 | 118 | 1 | 1 | |
| Breast problem | |||||
| No | 196 | 116 | 1 | 1 | |
| Yes | 64 | 13 | 2.91 (1.54, 5.52) | 2.62 (1.25, 5.48) | 0.011 |
| Breastfeeding experience | |||||
| No | 118 | 31 | 2.63 (1.64, 4.21) | 1.82 (1.01, 3.28) | 0.045 |
| Yes | 142 | 98 | 1 | 1 | |
p-Value = <0.001, BFT: breastfeeding techniques.
Discussion
This study assessed ineffective breastfeeding techniques and associated factors among mothers who have children less than 6 months. Suboptimal infant and young child feed resulted in a variety of health problems including undernutrition, stunting, wasting, and micronutrient deficiencies. Undernutrition is a major public health problem in low and middle-income countries. To prevent this problem, early initiation of breastfeeding within 1 h of birth, exclusive breastfeeding in the first 6 months of life, and breastfeeding with additional complementary feeding until 2 years of life are pivotal roles in child health, growth, and development.2–5,8,14,20,27 Ineffective breastfeeding technique due to improper positioning, attachment, and suckling resulted in insufficient intake of breast milk, early weaning, and poor child development leading to suffering common childhood illnesses and deaths.6,14,15,20 In this study, the overall proportion of ineffective breastfeeding techniques was 66.8% (95% CI: 62%, 71%). This finding is similar to studies conducted 63.5% in the Ari district, Southern Ethiopia. 15 This finding is higher than previously reported evidence, 52% Gondar, 20 56.6% Harar, 6 20.1% Arba Minch, 25 and 42.8% India. 24 In most of the previous studies, participants were included for less than 2 years and conducted in institution-based settings which may underestimate the proportion of ineffective breastfeeding techniques.6,15,20,24,25 This discrepancy might be due to the difference in the counseling services, health education dissemination, breastfeeding techniques demonstrations during pregnancy, and postnatal care services. In addition, it might be due to socio-cultural, study population, and period variations across the studies.
Educational status of mothers was associated with ineffective breastfeeding technique: Breastfeeding mothers who have no formal education were 5.88 times more likely to practice ineffective breastfeeding techniques compared to mothers who have attended secondary and above education level. This is similar to previous evidence in Ethiopia and India.5,6,24,30 Maternal education improves awareness, knowledge, attitude, and practice toward breastfeeding techniques, easy-to-adopt instructions, and behavioral change through health professionals’ health education, promotion, and counseling service.5,31 This may affect mothers’ ability to give more emphasis on instruction, guidance, and support from maternal and child health care providers in order to practice successful breastfeeding techniques.
Mothers who have primiparity was a statistically significant factor for ineffective breastfeeding technique: Primiparity mothers were more than fourfold times more likely to practice ineffective breastfeeding technique compared to their counterparts of multiparity breastfeeding mothers. This is consistent with previous studies conducted in different regions of Ethiopia, Libya, Italy, and India.4,7,15,20,23,24,32–35 Unlike primipara breastfeeding mothers, multiparous breastfeeding women have adequate knowledge and experience in infant care and are well familiar with breastfeeding techniques from their previous pregnancies.4,15,20 This could be due to a lack of access to regular counseling, skills, exposure, and experience with breastfeeding techniques.
Place of delivery was associated with ineffective breastfeeding technique: Women who had home delivery were three times more likely to practice ineffective breastfeeding techniques compared to mothers who had health center delivery. This finding is supported by previous studies conducted in Ethiopia. 15 The possible reason is that women who gave birth in the health centers are more likely to receive support and be exposed to early initiation, counseling, guidance, and frequent follow-up by healthcare professionals, which may improve the well functioning of effective breastfeeding techniques. 36
Similarly, breastfeeding techniques counseling during ANC follow-up was identified factor for ineffective breastfeeding techniques. Lactating mothers who have not received breastfeeding techniques counseling during ANC follow-up were nearly 5 times more likely to practice ineffective breastfeeding techniques compared to those who have received counseling during ANC follow-up. This evidence is similar to previous findings reported in Ethiopia and India.15,20,34,37 Breastfeeding counseling for pregnant women helps to know the benefit of breastfeeding, allowing mothers and their neonates to initiate within 1 hour of birth, avoiding unnecessary separation from their neonates or maintaining dyad, enabling caring and positive relationships through maintaining skin-skin contact, and promoting and continue effective breastfeeding techniques.14,38–40 ANC services include risk identification, prevention and management of pregnancy-related or concurrent diseases, health education and promotion related to pregnancy danger signs, birth preparedness, and effective breastfeeding practices. 41 This improves maternal knowledge and infant care, encourages early initiation of breastfeeding practice, and inquires about immediate postnatal services, all of which may increase the likelihood of practicing effective breastfeeding techniques.
In addition, breast problem was a statistically identified factor for ineffective breastfeeding technique: Those mothers who had breast problem was more than two and half times more likely to practice ineffective breastfeeding techniques compared to mothers who had no breast problem. This study finding was consistent with findings revealed in the different regions of Ethiopia, Libya, and India.6,15,20,23,42 Improper breastfeeding techniques may cases uncomfortable and painful for the mother resulting in damage to the skin of the nipple, cracking, sore nipples, fissures, engorged, and blocked ducts, or mastitis.8,35,43 This could be the reason for the difficulties in maintaining proper position, attachment, and suckling, resulting in ineffective breastfeeding techniques practiced.
Finally, breastfeeding experience was a statistically significant factor for ineffective breastfeeding techniques: Mothers who have no breastfeeding experience have 1.82 times more likely to practice ineffective breastfeeding techniques compared to mothers who have breastfeeding experience. This finding is supported by previous findings conducted in Ethiopia and Italy.6,7 The possible explanations include the acquired skills, sufficient knowledge of the benefits of breastfeeding for both the infant and mother, the benefits of breast milk, establishment and maintenance of mother-to-child relationships, and access to support and guidance from previous birth experiences.
Strength of the study
This study was conducted community-based in order to overcome the previous finding limitations and be able to generalize the findings to the community. The proportion of ineffective breastfeeding techniques using a standardized observational checklist and interviewer-administered questionnaires ensures the quality of the finding.
Limitations of the study
Observer bias and the Hawthorne effect might be present during data collection, to minimize this bias the data collectors were recruited those who had data collection experience, were well-trained and qualified to collect data using standardized tools, and each study participant was observed privately to maintain confidentiality. Due to the limitation of the cross-sectional design, it does not demonstrate causal inference.
Conclusions
In this study, the proportion of ineffective breastfeeding techniques was 66.8% which is unacceptable high for the established robust maternal programs nationally. Women with no formal education, primipara, home delivery, have not received breastfeeding techniques counseling during ANC follow-up, breast problems, and breastfeeding experience were identified as statistically significant factors for ineffective breastfeeding techniques. Strengthening the maternal continuum of care, and improving health education and promotion to increase awareness about ANC follow-up, the benefits of institutional delivery, and early treatment and management of breast problems at the community level requires priorities. Further prospective studies are required to ensure the antecedence of causality factors. Policymakers and planners should be focused on addressing this deep-rooted problem by designing appropriate strategies and interventions to improve ineffective breastfeeding practices and assure national child and maternal health.
Acknowledgments
We would like to thank Debre Markos University College of Health Science for providing ethical clearance, data collectors, supervisors, all selected kebeles health posts health extension workers, and community leaders for their support, guidance, and help to retrieve this data.
Footnotes
Authors’ contributions: Conceptualization: KA. Formal analysis: KA TE WA DBK ATT GG TDT. Development or design of methodology: KA TE MD TA GG AA. Entering data into computer software: KA ATT DBK AA TE WA. Supervision and validation: MD AA TE TDT. Writing original draft: KA TE WA ATT TA TDT. Writing review & editing: KA WA TE ATT MD DBK AA. All authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement and consent to participate: This study was approved by the Debre Markos University, College of Health Science ethical review committee (HSC/R/C/Ser/Co/242/11/13). Written informed consent was obtained from each study participant before starting the interview and observations. The information given was maintained strictly confidential and used for this study purpose only. All procedures were carried out in accordance with relevant guidelines and regulations.
Consent for publication: Not applicable.
ORCID iDs: Alehegn Aderaw Alamneh  https://orcid.org/0000-0002-1689-7356
https://orcid.org/0000-0002-1689-7356
Animut Takele Telayneh  https://orcid.org/0000-0002-8707-4963
https://orcid.org/0000-0002-8707-4963
Data availability: The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1.Gupta A, Suri S, Dadhich JP, et al. The world breastfeeding trends initiative: Implementation of the global strategy for infant and young child feeding in 84 countries. J Public Health Policy 2019; 40(1): 35–65. [DOI] [PubMed] [Google Scholar]
- 2.Lawan U, Sani A, Amole G, et al. Age-appropriate feeding practices and nutritional status of infants attending child welfare clinic at a teaching hospital in Nigeria. J Fam Community Med 2014; 21(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haileamlak A. Appropriate infant and young child feeding. Ethiop J Health Sci 2019; 29(2): 151–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degefa N, Tariku B, Bancha T, et al. Breast Feeding Practice: positioning and attachment during Breast Feeding among lactating mothers visiting health facility in Areka Town, Southern Ethiopia. Int J Pediatr 2019; 2019: 8969432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parashar M, Singh S, Kishore J, et al. Breastfeeding attachment and positioning technique, practices, and knowledge of related issues among mothers in a resettlement colony of Delhi. ICAN Infant Child Adolesc Nutr 2015; 7(6): 317–322. [Google Scholar]
- 6.Tiruye G, Mesfin F, Geda B, et al. Breastfeeding technique and associated factors among breastfeeding mothers in Harar city, Eastern Ethiopia. Int Breastfeed J 2018; 13(1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colombo L, Crippa BL, Consonni D, et al. Breastfeeding determinants in healthy term newborns. Nutrients 2018; 10(1): 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization, 2009. [PubMed] [Google Scholar]
- 9.AffifaTanny S, Mamun A, Sabiruzzaman M, et al. Factors influencing exclusive breastfeeding practice in Bangladesh: Multiple logistic regression analysis. In: 7th International Conference on Data Science & SDGs, Dept. of Statistics, University of Rajshahi, Bangladesh, 2019, pp.191–200. [Google Scholar]
- 10.Rudrappa S, Nagaraju H, Raju Y, et al. To study the knowledge, attitude, and practice of breastfeeding among postnatal mothers in a tertiary care center of South India. Indian J Child Health 2020; 07: 113–116. [Google Scholar]
- 11.Moraes BA, Strada JKR, Gasparin VA, et al. Breastfeeding in the first six months of life for babies seen by lactation consulting. Revista Latino-Americana de Enfermagem 2021; 29: e3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Del Ciampo LA, Del Ciampo IRL. Breastfeeding and the benefits of lactation for women’s health. Rev Bras Ginecol Obstet 2018; 40(6): 354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chouhan Y, Siddharth R, Sakalle S, et al. A cross-sectional study to assess breastfeeding positioning and attachment among mother-infant pairs in Indore. Ann Commun Health 2020; 8(3): 31–36. [Google Scholar]
- 14.World Health Organization. Protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: the revised Baby-friendly Hospital initiative: 2018 implementation guidance: frequently asked questions. Geneva: World Health Organization, 2020. [Google Scholar]
- 15.Yilak G, Gebretsadik W, Tadesse H, et al. Prevalence of ineffective breastfeeding technique and associated factors among lactating mothers attending public health facilities of South Ari district, southern Ethiopia. PLoS One 2020; 15(2): e0228863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mulder PJ. A concept analysis of effective breastfeeding. J Obstet Gynecol Neonat Nurs 2006; 35(3): 332–339. [DOI] [PubMed] [Google Scholar]
- 17.Langton CR, Whitcomb BW, Purdue-Smithe AC, et al. Association of parity and breastfeeding with risk of early natural menopause. JAMA Netw Open 2020; 3(1): e1919615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rinata E, Sari PA. Breastfeeding practices [Positioning, attachment/latch- on and effective suckling. SEAJOM: Southeast Asia J Midwif 2019; 3(2): 1–6. [Google Scholar]
- 19.Shrivastava P, Saha I, Nandy S. A study on feeding practice of under 6 months infants attending the nutrition clinic of a tertiary care hospital of West Bengal, India. Epidemiol Biostat Public Health 2013; 10(4): 7. [Google Scholar]
- 20.Safayi BL, Assimamaw NT, Kassie DG. Breastfeeding technique and associated factors among lactating mothers visiting Gondar town health facilities, Northwest Ethiopia: Observational method. Ital J Pediatr 2021; 47: 206–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rahim F, Muhammad J, Ali S, et al. Breastfeeding practices in neonatal units. J Med Sci 2014; 22: 159–163. [Google Scholar]
- 22.Khasawneh W, Kheirallah K, Mazin M, et al. Knowledge, attitude, motivation, and planning of breastfeeding: a cross-sectional study among Jordanian women. Int Breastfeed J 2020; 15(1): 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal RC, Banginwar AS, Ziyo F, et al. Breastfeeding practices: positioning, attachment (latch-on) and effective suckling – A hospital-based study in Libya. J Fam Community Med 2011; 18(2): 74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagendra K, Shetty PN, Rudrappa S, et al. Evaluation of breast feeding techniques among postnatal mothers and effectiveness of intervention: Experience in a tertiary care centre. Sri Lanka J Child Health 2017; 46(1): 39. [Google Scholar]
- 25.Tamiru D, Jisha H. Breastfeeding skills in Arba Minch Zuria: the positioning and attachment initiatives. Int J Nurs Midwifery 2017; 9(4): 46–52. [Google Scholar]
- 26.World Health Organization. Session 2 the physiological basis of breastfeeding: infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization, 2009. [PubMed] [Google Scholar]
- 27.World Health Organization. Breastfeeding counseling: A training course. Geneva: World Health Organization, 1993. [Google Scholar]
- 28.World Health Organization. Baby-friendly hospital initiative: revised, updated, and expanded for integrated care. Geneva: World Health Organization, 2009. [PubMed] [Google Scholar]
- 29.Gove S. Integrated management of childhood illness by outpatient health workers: Technical basis and overview. The WHO working group on guidelines for integrated management of the sick child. Bull World Health Organ 1997; 75: 7. [PMC free article] [PubMed] [Google Scholar]
- 30.Dasgupta U, Mallik S, Bhattacharyya K, et al. Breastfeeding practices: positioning, attachment, and effective suckling a hospital-based study in West Bengal/Kolkata. Indian J Matern Child Health 2013; 15: 1–11. [Google Scholar]
- 31.Awoke S, Mulatu B. Determinants of exclusive breastfeeding practice among mothers in Sheka Zone, Southwest Ethiopia: A cross-sectional study. Public Health Practice 2021; 2: 100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prajapati A, Chandwani H, Rana B, et al. A community based assessment study of positioning, attachment and suckling during breastfeeding among 0-6 months aged infants in rural area of Gandhinagar district, Gujarat, India. Int J Community Med Public Health 2016; 3(7): 1921–1926. [Google Scholar]
- 33.Davra K, Chavda P, Pandya C, et al. Breastfeeding position and attachment practices among lactating mothers: an urban community-based cross-sectional study from Vadodara city in western India. Clin Epidemiol Glob Health 2022; 15: 101009. [Google Scholar]
- 34.Sindhuri R, Nancy S, Arunagirinathan A, et al. Breastfeeding positioning and attachment among postnatal mothers: A mixed methods study in a tertiary care hospital in Puducherry, South India. Indian J Commun Med 2022; 47(1): 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joshi H, Magon P, Raina S. Effect of mother–infant pair's latch-on position on child's health: A lesson for nursing care. J Fam Med Prim Care 2016; 5(2): 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cozma-Petruţ A, Filip L, Banc R, et al. Breastfeeding practices and determinant factors of exclusive breastfeeding among mothers of children aged 0-23 months in northwestern Romania. Nutrients 2021; 13(11): 3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choudhary P, Bapna D, Jain A, et al. Association of breastfeeding counseling with infant breastfeeding practices among lactating mothers of rural area of Haryana: A cross-sectional study. Int J Prev Curat Commun Med 2020; 6(4): 1–8. [Google Scholar]
- 38.World Health Organization. Implementation guidance: protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. Geneva: World Health Organization, 2018. [Google Scholar]
- 39.McFadden A, Siebelt L, Marshall JL, et al. Counselling interventions to enable women to initiate and continue breastfeeding: A systematic review and meta-analysis. Int Breastfeed J 2019; 14(1): 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Federal Democratic Republic of Ethiopia. Ministry of Health: Antenatal care, part 2 blended learning module for the health extension Program. Addis Ababa: Ministry of Health, 2008. [Google Scholar]
- 41.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization, 2016. [PubMed] [Google Scholar]
- 42.Aswathaman N, Sajjid M, Kamalarathnam CN, et al. Assessment of breastfeeding position and attachment (ABPA) in a tertiary care centre in Chennai, India: an observational descriptive cross-sectional study. Int J Contemp Pediatr 2018; 5: 2209–2216. [Google Scholar]
- 43.Puapornpong P, Paritakul P, Suksamarnwong M, et al. Nipple pain incidence, the predisposing factors, the recovery period after care management, and the exclusive breastfeeding outcome. Breastfeed Med 2017; 12(3): 169–173. [DOI] [PubMed] [Google Scholar]


