Abstract
Background:
Open kinetic chain (OKC) exercise is an effective method to improve muscle function during rehabilitation after anterior cruciate ligament reconstruction (ACLR); however, there is controversy about its use in the early phase of rehabilitation.
Purpose:
To determine (1) whether the use of OKC and closed kinetic chain (CKC) exercises improves quadriceps and hamstring strength in the early phase of rehabilitation after ACLR and (2) whether the early use of OKC exercise affects graft laxity at 3 and 6 months postoperatively in patients with a hamstring tendon graft.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This study included an intervention group that underwent OKC + CKC exercises (n = 51) and a control group that underwent CKC exercise only (n = 52). In the intervention group, OKC exercise for the quadriceps and hamstring was started at 4 weeks after ACLR. At 3 and 6 months postoperatively, isokinetic testing was performed to calculate the limb symmetry index (LSI) and the peak torque to body weight ratio (PT/BW) for the quadriceps and hamstring. Anterior knee laxity was measured by an arthrometer.
Results:
At 3 and 6 months postoperatively, quadriceps strength was higher in the intervention group than in the control group for the LSI (3 months: 76.14% ± 0.22% vs 46.91% ± 0.21%, respectively; 6 months: 91.05% ± 0.18% vs 61.80% ± 0.26%, respectively; P < .001 for both) and PT/BW (3 months: 1.81 ± 0.75 vs 0.85 ± 0.50 N·m/kg, respectively; 6 months: 2.40 ± 0.73 vs 1.39 ± 0.70 N·m/kg, respectively; P < .001 for both). There were similar findings regarding hamstring strength for the LSI (3 months: 86.13% ± 0.22% vs 64.26% ± 0.26%, respectively; 6 months: 91.90% ± 0.17% vs 82.42% ± 0.24%, respectively; P < .001 at three months, P = .024 at 6 months) and PT/BW (3 months: 1.09 ± 0.36 vs 0.67 ± 0.39 N·m/kg, respectively; 6 months: 1.42 ± 0.41 vs 1.07 ± 0.39 N·m/kg, respectively; P < .001 for both). No significant difference in laxity was observed between the intervention and control groups at 3 or 6 months.
Conclusion:
Early use of OKC exercise for both the quadriceps and the hamstring, in addition to conventional CKC exercise, resulted in better correction of quadriceps and hamstring strength deficits without increasing graft laxity.
Keywords: anterior cruciate ligament reconstruction, open kinetic chain, return to sport, strength recovery, graft laxity
After anterior cruciate ligament (ACL) reconstruction (ACLR), a long period of rehabilitation begins that is well-documented. There are consensus guidelines on the main steps to follow for rehabilitation according to 3 main phases. 27 It starts with the early phase, which includes the management of postoperative pain and other issues as well as the consequences of surgery. Then, the middle and late phases consist of the return-to-sport continuum, as proposed in the “reconstruction, rehabilitation and return-to-sport continuum after anterior cruciate ligament injury” (ACLR3–continuum). 36 Upon return to sport or in the longer term, a persistent strength deficit in the quadriceps is often observed and sometimes also in the hamstring, especially with the use of hamstring tendon grafts. Thus, muscle strengthening is a key element in rehabilitation after ACLR, and it is necessary to optimize rehabilitation to allow for a safe return to sport while respecting the biological (graft healing), physiological (ie, neuromuscular adaptations), and psychological challenges that the patient must face. 38
Open kinetic chain (OKC) exercise of the quadriceps early in the postoperative period is an effective method to improve muscle function; however, there is controversy regarding its use. According to the consensus guidelines, 27 this mode of strengthening can be utilized from the fifth postoperative week unless the graft is harvested from the semitendinosus, in which case the authors recommend against additional loads to the leg such as leg extension exercises. However, multiple studies have shown the absence of harm from this mode of contraction, even with this type of graft,9,10,45 as indicated by laxity measured using the KT-1000 arthrometer (MEDmetric). This type of measurement with the KT-1000 arthrometer or another evaluation that requires human action may introduce errors and be inaccurate. The GNRB arthrometer (Genourob), an automated tool to assess knee laxity, provides a more objective, reproducible, and less error-prone measurement of joint laxity.16,17,28,33,41
Few studies have been published that focus on hamstring strengthening during the early phase, especially after ACLR with a hamstring tendon graft. However, even if tenotomy is performed (semitendinosus tendon is fully harvested), healing and even regrowth may occur. 43 It therefore seems logical to offer early OKC exercise for the hamstring after the first stages of healing are complete. An isokinetic dynamometer is also very safe for both the evaluation and the strengthening of the knee extensor and flexor muscles. The isokinetic mode of OKC exercise, in addition to classic strengthening exercises for the quadriceps and hamstring, may both protect the graft (the action of the hamstring makes it possible to avoid anterior tibial drawer) and limit the onset of amyotrophy during the first phases of rehabilitation (early and middle).
Thus, this study was designed to assess the association of OKC exercise for quadriceps and hamstring muscle strengthening with the accepted closed kinetic chain (CKC) exercise. The main objective was to compare the peak torque to body weight ratio (PT/BW) and the limb symmetry index (LSI) of the quadriceps and hamstring muscles at 3 and 6 months postoperatively between the 2 groups. The secondary objective was to compare the difference in laxity during rehabilitation (at 3 and 6 months) between a group of patients with an OKC + CKC exercise protocol (intervention group) and a group of patients rehabilitated only with CKC exercise (control group).
Methods
Study Design
The protocol for this study received ethics review board approval, and all included patients participated in agreement with the Declaration of Helsinki and provided written informed consent. The following baseline information was recorded for each participant regarding medical data (graft type, date of surgery, knee surgeon’s name) and demographic and sport-related data (age, weight, height, Tegner and Marx scores before ACL injury).
Participants
This study included 103 recreational athletes (33 women) who had undergone ACLR. Patients were included if (1) they had undergone ACLR using a hamstring autograft with semitendinous and gracilis tendons by 3 different knee surgeons (A.V., P.D., L.R.) (no extra procedures were performed), (2) their ACL injury occurred without contact during sports, (3) they were younger than 35 years and had a body mass index (BMI) <30 kg/m2, and (4) their activity level before the ACL injury was defined as a Tegner score 8 of ≥6 and a Marx score 19 of ≥6.
The exclusion criteria were (1) an existing or previous injury to the ipsilateral knee and (2) reconstruction for an iterative injury. Patients with meniscal repair and/or meniscectomy were not excluded, but patients with associated lesions (osteochondral lesions, multiple ligament injuries) other than meniscal injuries were excluded. There were 2 groups established: a control group (exclusively CKC exercise) and an intervention group (mixed OKC and CKC exercises). The intervention group underwent rehabilitation at 1 center, and the control group underwent rehabilitation at other centers. Each group was matched by sex, age, height, weight, BMI, Marx score, and Tegner score.
Rehabilitation Protocol
The rehabilitation protocols were overseen independently by 4 physical therapists who were experienced in ACL rehabilitation and who participated in the design of the rehabilitation programs but none of whom were authors of the study.. All the physical therapists were involved in the follow-up of the programs with regard to the assessment of the applied loads and the dosage of the individual exercises.
The control group followed a rehabilitation protocol after ACLR, 3 times per week, with muscle strengthening exclusively with CKC exercise initiated from the immediate postoperative phase, without any OKC exercise. The patients followed the same standardized rehabilitation protocol as different rehabilitation centers, as previously described by Quelard et al. 34 The intervention group followed a mixed protocol of OKC and CKC exercises for muscle strengthening of the quadriceps and hamstring. CKC exercise was initiated from the immediate postoperative phase, and OKC exercise was initiated from 4 weeks postoperatively (31.4 ± 7.6 days), as recommended by Perriman et al. 31 The introduction of OKC exercise was authorized if the patient presented a stroke test result of ≤1+, a range of motion between 0° and 110°, a single-leg rise without lag, and graft laxity at 134 N of <1.5 mm.13,33 Meniscal procedures did not modify ACL rehabilitation. 35
The OKC exercise protocol focused on the quadriceps and hamstring muscles. It was performed on an isokinetic machine with leg extension and seated leg curls. It included 10 sets of 8 repetitions in isokinetics at 60 deg/s (Figure 1A) as well as 8 sets of 8 repetitions, 3 times per week, for leg extension for the quadriceps (Figure 1B) and seated leg curls for the hamstring (Figure 1C). The contraction modalities were the same, regardless of the type of exercise, with 3 seconds of concentric contraction, 1 second of isometric contraction, and 3 seconds of eccentric contraction. 7 The load applied was 60% of the maximum resistance, reassessed weekly for the quadriceps and hamstring with a handheld dynamometer (microFET 2; Hoggan Scientific) at 90° of knee flexion with a strap. Both groups were assessed at 3 and 6 months postoperatively during follow-up with a clinical evaluation and an isokinetic muscle strength assessment for the quadriceps and hamstring. From 3 months onward, the interval was variable between each patient because time was not an absolute criterion and delays had to be individualized on the basis of other objective variables but were nevertheless without significant difference between the 2 groups.37,38
Figure 1.
(A) Isokinetic machine for the quadriceps and hamstring muscles. (B) Seated leg curl for the hamstring. (C) Leg extension for the quadriceps.
Assessment Protocol
The principal investigator (F.F.), who performed all measurements, was not informed of group assignment. At 3 months (102.3 ± 18.9 days) and 6 months (203.4 ± 42.2 days), all participants underwent an isokinetic muscle strength assessment for the quadriceps and hamstring and a graft laxity assessment with a GNRB arthrometer. The muscle strength assessment was performed using a Humac Norm isokinetic dynamometer (Version 15.000.0273; Computer Sports Medicine), and data were collected using the computer software interface attached to the machine. Before carrying out the isokinetic assessment, each participant had a standardized warm-up with 10 minutes of walking on a treadmill at 5 km/h. The objective of this assessment was to measure the PT/BW for the quadriceps and hamstring during knee extension and flexion movements, allowing interpatient comparison, and for both legs to analyze the variation in intrapatient strength. Symmetry was expressed as percentages by the LSI, which was calculated as the PT/BW of the injured limb divided by the PT/BW of the uninjured limb, multiplied by 100.26,46
The positioning of the participants on the isokinetic dynamometer was individually adjusted to ensure correct alignment of the anatomic axis of the knee joint with the axis of rotation of the lever arm during movements. The trunk and thigh of the limb tested were strapped to minimize body movements. Once the warm-up was completed and the positioning adjusted on the machine, each of the participants performed 1 series of 4 knee extensions and flexions at 60 deg/s ranging from 0° to 100°. The series was performed first on the operated limb and then on the nonoperated limb.
The angular range chosen and the angular velocity corresponded to standards in the literature in terms of isokinetic assessments for the quadriceps and hamstring in the context of follow-up after ACLR.14,39 These were justified, as the maximum torque values measured were obtained at between 0 and 60 deg/s. An assessment at a higher angular velocity would not only decrease PT/BW values but also decrease the sensitivity of a comparison of the PT/BW between the 2 legs or between 2 distinct groups, thus biasing decision making within the framework of return to sport. 38
After the isokinetic muscle strength assessment for the quadriceps and hamstring, the graft laxity assessment with the GNRB arthrometer was performed (Figure 2). After having immobilized the distal extremities of the femur (tightening at 10 N compared with the contralateral side) and of the tibia (the base-foot distance indicated is noted for the reproducibility between measurements), 3 successive thrusts were carried out.13,16,17,28,41 The data were collected at 134 N.13,28,33,41 The laxity assessment had moderate to good intratester reliability (intraclass correlation coefficient [ICC], 0.72-0.83) and good intertester reliability (ICC, 0.76-0.81), and test-retest repeatability also demonstrated good reliability (ICC, 0.77-0.83).13,28,33,42 The calculated standard errors of measurement for intrarater reliability, interrater reliability, and test-retest repeatability ranged from 0.48 to 0.62 mm. The minimal detectable change at 134 N was 2.1 mm/N. 42 The minimal detectable change can be a clinically significant metric when looking to compare the smallest amount of change between testing sessions of 1 limb. 42
Figure 2.

Positioning of the leg segment during the assessment with a GNRB arthrometer.
Statistical Analysis
Statistical analysis and calculation of means and standard deviations were performed with R software (Version 1.2.5033; RStudio) after exporting the data to Excel (Microsoft Version 16.61). All variables were normally distributed (Shapiro-Wilk normality test). A P value of <.05 was used to identify statistical significance. To compare the characteristics between patient groups, the unpaired t test was used for continuous variables, and the chi-square test was used for categorical variables. For measurements of the LSI, the PT/BW, and graft laxity (anterior displacement of the tibia), t tests were used for independent-samples group comparisons. The effect size was reported as the Cohen d, with values of 0.2, 0.5, and 0.8 interpreted as small, medium, and large effects, respectively. 23
Results
Patient Characteristics
The mean age of the 103 study patients was 30.1 ± 9.3 years. A complete summary of patient data is presented in Table 1. No statistically significant differences were observed between the 2 groups for the variables of sex, age, height, weight, BMI, and Tegner and Marx scores (Table 1).
Table 1.
Characteristics of Patients (N = 103) a
| Intervention Group (n = 51) | Control Group (n = 52) | P | Cohen d | |
|---|---|---|---|---|
| Age, y | 26.3 ± 5.3 | 30.5 ± 10.2 | .71 | 0.22 |
| Male sex, n | 34 | 36 | .94 | NA |
| Height, cm | 173.0 ± 9.0 | 174.0 ± 8.0 | .94 | 0.11 |
| Weight, kg | 74.0 ± 13.5 | 73.1 ± 10.9 | .96 | 0.07 |
| BMI, kg/m2 | 24.6 ± 3.5 | 24.4 ± 3.2 | .96 | 0.05 |
| Tegner score b | 7.5 ± 1.0 | 7.0 ± 2.0 | .82 | 0.31 |
| Marx score c | 13.5 ± 3.0 | 10.2 ± 3.3 | .46 | 1.04 |
a Data are reported as mean ± SD unless otherwise indicated. BMI, body mass index; NA, not applicable.
b All Tegner scores were between 6 and 10.
c All Marx scores were between 6 and 16.
Tables 2 and 3 present comparisons between the groups for the LSI and PT/BW, respectively. At 3 months, significant differences of 29.2% in the LSI for the quadriceps (P < .001; Cohen d = –1.3) and of 21.8% in the LSI for the hamstring (P < .001; Cohen d = –0.9) were observed, favoring the intervention group. At 6 months, similar results were observed, with significant differences of 29.2% in the LSI for the quadriceps (P < .001; Cohen d = –1.2) and of 9.5% in the LSI for the hamstring (P = .024; Cohen d = –0.4), also favoring the intervention group.
Table 2.
Limb Symmetry Index (%) a
| Intervention Group (n = 51) | Control Group (n = 52) | P | Cohen d | |
|---|---|---|---|---|
| Quadriceps strength | ||||
| 3 mo | 76.14 ± 0.22 | 46.91 ± 0.21 | <.001 | –1.3 |
| 6 mo | 91.05 ± 0.18 | 61.80 ± 0.26 | <.001 | –1.2 |
| Hamstring strength | ||||
| 3 mo | 86.13 ± 0.22 | 64.26 ± 0.26 | <.001 | –0.9 |
| 6 mo | 91.90 ± 0.17 | 82.42 ± 0.24 | .024 | –0.4 |
a Data are reported as mean ± SD. Boldface P values indicate a statistically significant difference between groups (P < .05).
Table 3.
Peak Torque to Body Weight Ratio (N·m/kg) a
| Intervention Group (n = 51) | Control Group (n = 52) | P | Cohen d | |
|---|---|---|---|---|
| Quadriceps strength | ||||
| Operated side at 3 mo | 1.81 ± 0.75 | 0.85 ± 0.50 | <.001 | –1.5 |
| Nonoperated side at 3 mo | 2.36 ± 0.62 | 1.81 ± 0.56 | <.001 | –1.0 |
| Operated side at 6 mo | 2.40 ± 0.73 | 1.39 ± 0.70 | <.001 | –1.3 |
| Nonoperated side at 6 mo | 2.62 ± 0.59 | 2.24 ± 0.52 | <.001 | –0.8 |
| Hamstring strength | ||||
| Operated side at 3 mo | 1.09 ± 0.36 | 0.67 ± 0.39 | <.001 | –0.9 |
| Nonoperated side at 3 mo | 1.29 ± 0.36 | 1.08 ± 0.40 | .005 | –0.5 |
| Operated side at 6 mo | 1.42 ± 0.41 | 1.07 ± 0.39 | <.001 | –0.6 |
| Nonoperated side at 6 mo | 1.55 ± 0.38 | 1.32 ± 0.42 | .005 | –0.5 |
a Data are reported as mean ± SD. Boldface P values indicate a statistically significant difference between groups (P < .05).
Similar results were observed in the comparison of the PT/BW, with a significant difference at 3 months of 0.96 N·m/kg in relative quadriceps strength (1.81 ± 0.75 vs 0.85 ± 0.50 N·m/kg, respectively; P < .001; Cohen d = –1.5) and 0.42 N·m/kg in relative hamstring strength (1.09 ± 0.36 vs 0.67 ± 0.39 N·m/kg, respectively; P < .001; Cohen d = –0.9), favoring the intervention group. These significantly higher strength values in the intervention group were also present at 6 months, with a between-group difference in quadriceps strength of 1.01 N·m/kg (P < .001; Cohen d = –1.3) and in hamstring strength of 0.35 N·m/kg (P < .001; Cohen d = –0.6).
Graft Laxity
As shown in Figure 3A, laxity was substantially the same at 3 months between the 2 groups (0.38 ± 1.19 vs 0.38 ± 1.90 mm, respectively; P = .98; Cohen d = 0.005). However, at 6 months (Figure 3B), laxity was increased in the control group versus the intervention group (0.58 ± 1.65 vs 0.44 ± 1.20 mm, respectively; P = .62; Cohen d = 0.09). Yet, in both groups, the results were not significant at 3 and 6 months.
Figure 3.
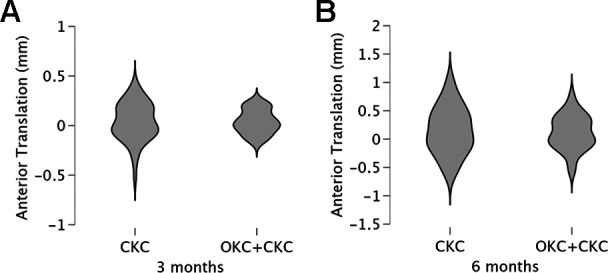
Comparison of laxity at (A) 3 and (B) 6 months in the intervention and control groups (the width of the plots indicates the frequency with which these values occur). CKC, closed kinetic chain; OKC, open kinetic chain.
Discussion
The results show that the rehabilitation program that combined CKC exercise with early OKC exercise for the quadriceps and hamstring seemed to lead to significantly higher quadriceps and hamstring strength at 3 and 6 months on isokinetic testing compared with a rehabilitation program exclusively carried out with CKC exercise. Muscle assessments have shown that OKC exercise with resistance is more effective than CKC exercise alone for quadriceps and hamstring strength recovery. There was no significant increased graft laxity with combined CKC and OKC exercises.
Consistent with these results, other studies have shown that OKC exercise with CKC exercise significantly improved quadriceps strength.1,4,11,29 However, this study highlights the benefits of OKC exercise on the hamstring strength symmetry index. For return to sport, the hamstring strength symmetry index is a decisive value37,38 and was not considered by previous researchers. Also, Grondin et al 12 showed that the hamstring strength symmetry index could be added to slightly increase the prediction of return to running. In addition, Krzeminska and Czamara 18 highlighted that restoring the hamstring strength symmetry index and hamstring/quadriceps ratio can reduce the risk factor for ACL graft ruptures. As with Kang et al 15 and Morrissey et al, 30 the increase in applied and controlled loads to the quadriceps and hamstring showed similar effects to those in our intervention group. Quadriceps and hamstring muscle function after an ACL injury appear to be critical factors in a patient’s ability to cope with the injury process. 46 Therefore, it is very important to recover strength in the quadriceps and hamstring. These results support the theory that progressive training of the quadriceps and hamstring with OKC exercise facilitates the recovery of muscle strength at different times for return to sport.
At 3 and 6 months, most patients had started running, jumping, agility exercises, and specific sport activities, which may have influenced the results in the 2 groups as well. In the control group, the LSI for the quadriceps and the LSI for the hamstring were far from recommended values at 3 37 and 6 months,22,32 while those in the intervention group were close. Indeed, at 3 and 6 months, a difference of 29.2% was noted in the LSI for the quadriceps and of 21.8% and 9.5% in the LSI for the hamstring at 3 and 6 months, respectively. Similar differences in the PT/BW were observed at 3 and 6 months for quadriceps and hamstring strength. However, analysis of the results showed moderate effect sizes for the LSI and PT/BW of the hamstring at 6 months after ACLR.
Beynnon et al2,3 found that CKC and OKC exercises produced similar ACL strain forces, and in the present study, there was no significant difference in tibial translation between the groups at 3 or 6 months. These findings are consistent with previous studies that showed that both CKC and OKC exercises can be safely implemented in an ACL rehabilitation program in the early phase without restricting the range of motion.1,4,25,29,30,40 However, Heijne and Werner 13 concluded that the early introduction of OKC exercise of the quadriceps engendered greater anterior translation after ACLR with a hamstring tendon graft compared with a bone–patellar tendon–bone graft. However, their rehabilitation protocol of OKC exercise did not include strengthening sessions on an isokinetic machine with seated leg curls but only leg extension on a quadriceps machine. Therefore, the 2 protocols are not comparable, which may explain the differences in the LSI and graft laxity between the 2 studies. Contrary to Heijne and Werner, 13 early OKC exercise for hamstring strengthening was introduced in a concentric contraction mode. This mode of exercise could have had a role in less anterior tibial translation. Indeed, Blackburn et al5,6 showed that isometric concentric strengthening increases hamstring stiffness and that stiffness decreases anterior tibial translation. Joint compression increases, which lead to joint stiffening, improve joint stability in the anterior position20,21,24,44 and reduce graft strain.
Limitations
In this study, standardization and compliance of the control group could not be controlled. The intervention group was derived from the same rehabilitation center and underwent rehabilitation after ACLR according to the same standardized protocol. The patients in the control group underwent their rehabilitation at other centers, according to Quelard et al. 34 However, it was not possible to randomize and perform blinded testing on the patients of the 2 groups and the evaluators. In addition, the time from injury to surgery, the time from surgery to strength testing, meniscal procedures, sex, mechanisms of injury, and rehabilitation before surgery may be parameters that influence the initial and final strength assessments.
Conclusion
The current results indicated the potential benefits of early OKC exercise at 6 months postoperatively. This study is consistent with previous literature that examined similar protocols and supports current recommendations that OKC exercise should be introduced at an early stage. These results highlight several perspectives that would be interesting to consider in the future, particularly by linking with psychological parameters that are also involved in the decision-making process as patients progress toward recovery.
Acknowledgment
The authors thank Saphia Issaouni, Elodie Boisselier, Cindy Lelievre, Sandra Domrane, Alexandra Maggio, Illéna Maggio, Christelle Zerrougui, Salima Loeillet, and all team members at Clinique de Domont.
Footnotes
Final revision submitted February 4, 2023; accepted March 9, 2023.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Clinique de Domont (No. PCE-06.18-038).
References
- 1.Andersson D, Samuelsson K, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy. 2009;25(6):653–685. [DOI] [PubMed] [Google Scholar]
- 2.Beynnon BD, Johnson RJ, Fleming BC, et al. Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am. 2002;84(9):1503–1513. [DOI] [PubMed] [Google Scholar]
- 3.Beynnon BD, Johnson RJ, Fleming BC, Stankewich CJ, Renström PA, Nichols CE. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension: a comparison of an open and a closed kinetic chain exercise. Am J Sports Med. 1997;25(6):823–829. [DOI] [PubMed] [Google Scholar]
- 4.Bieler T, Aue Sobol N, Andersen LL, et al. The effects of high-intensity versus low-intensity resistance training on leg extensor power and recovery of knee function after ACL-reconstruction. Biomed Res Int. 2014;2014:278512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blackburn JT, Norcross MF. The effects of isometric and isotonic training on hamstring stiffness and anterior cruciate ligament loading mechanisms. J Electromyogr Kinesiol. 2014;24(1):98–103. [DOI] [PubMed] [Google Scholar]
- 6.Blackburn JT, Norcross MF, Padua DA. Influences of hamstring stiffness and strength on anterior knee joint stability. Clin Biomech. 2011;26(3):278–283. [DOI] [PubMed] [Google Scholar]
- 7.Brinlee AW, Dickenson SB, Hunter-Giordano A, Snyder-Mackler L. ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health. 2022;14(5):770–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. 2011;63(suppl 11):S208–S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Escamilla RF, Fleisig GS, Zheng N, Barrentine SW, Wilk KE, Andrews JR. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med Sci Sports Exerc. 1998;30(4):556–569. [DOI] [PubMed] [Google Scholar]
- 10.Fleming BC, Oksendahl H, Beynnon BD. Open- or closed-kinetic chain exercises after anterior cruciate ligament reconstruction? Exerc Sport Sci Rev. 2005;33(3):134–140. [DOI] [PubMed] [Google Scholar]
- 11.Fukuda TY, Fingerhut D, Moreira VC, et al. Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized controlled clinical trial. Am J Sports Med. 2013;41(4):788–794. [DOI] [PubMed] [Google Scholar]
- 12.Grondin J, Crenn V, Gernigon M, et al. Relevant strength parameters to allow return to running after primary anterior cruciate ligament reconstruction with hamstring tendon autograft. Int J Environ Res Public Health. 2022;19(14):8245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):402–414. [DOI] [PubMed] [Google Scholar]
- 14.Impellizzeri FM, Bizzini M, Rampinini E, Cereda F, Maffiuletti NA. Reliability of isokinetic strength imbalance ratios measured using the Cybex NORM dynamometer. Clin Physiol Funct Imaging. 2008;28(2):113–119. [DOI] [PubMed] [Google Scholar]
- 15.Kang H, Jung J, Yu J. Comparison of strength and endurance between open and closed kinematic chain exercises after anterior cruciate ligament reconstruction: randomized control trial. J Phys Ther Sci. 2012;24(10):1055–1057. [Google Scholar]
- 16.Klasan A, Putnis SE, Kandhari V, Oshima T, Fritsch BA, Parker DA. Healthy knee KT1000 measurements of anterior tibial translation have significant variation. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2177–2183. [DOI] [PubMed] [Google Scholar]
- 17.Klasan A, Putnis SE, Kandhari V, Oshima T, Parker DA. Anterior knee translation measurements after ACL reconstruction are influenced by the type of laximeter used. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3639–3646. [DOI] [PubMed] [Google Scholar]
- 18.Krzeminska K, Czamara A. Diagnostic value of the hamstring to quadriceps ratio in monitoring of the effectiveness of supervised 6-month physiotherapy in males after anterior cruciate ligament reconstruction (ACLR). Acta Bioeng Biomech. 2020;22(4):31–39. [PubMed] [Google Scholar]
- 19.Kuenze C, Cadmus-Bertram L, Pfieffer K, et al. Relationship between physical activity and clinical outcomes after ACL reconstruction. J Sport Rehabil. 2019;28(2):180–187. [DOI] [PubMed] [Google Scholar]
- 20.Kvist J, Gillquist J. Anterior positioning of tibia during motion after anterior cruciate ligament injury. Med Sci Sports Exerc. 2001;33(7):1063–1072. [DOI] [PubMed] [Google Scholar]
- 21.Kvist J, Good L, Tagesson S. Changes in knee motion pattern after anterior cruciate ligament injury: a case report. Clin Biomech. 2007;22(5):551–556. [DOI] [PubMed] [Google Scholar]
- 22.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 23.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4. doi:doi.org/10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SLY. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32(4):395–400. [DOI] [PubMed] [Google Scholar]
- 25.Liu H, Lu W, Liang D, et al. Effect of isokinetic training of thigh muscle group on graft remodeling after anterior cruciate ligament reconstruction. Chin J Reconstr Surg. 2019;33(9):1088–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining “successful outcome” after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melick NV, van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506–1515. [DOI] [PubMed] [Google Scholar]
- 28.Michel E, Jordan E, Canovas F, Bouchdoug K, Dagneaux L, Gaillard F. Influence of residual anterior laxity on functional outcomes after anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res. 2022;108(3):103264. [DOI] [PubMed] [Google Scholar]
- 29.Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8(6):337–342. [DOI] [PubMed] [Google Scholar]
- 30.Morrissey MC, Perry MC, King JB. Is knee laxity change after ACL injury and surgery related to open kinetic chain knee extensor training load? Am J Phys Med Rehabil. 2009;88(5):369–375. [DOI] [PubMed] [Google Scholar]
- 31.Perriman A, Leahy E, Semciw AI. The effect of open- versus closed-kinetic-chain exercises on anterior tibial laxity, strength, and function following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2018;48(7):552–566. [DOI] [PubMed] [Google Scholar]
- 32.Pietrosimone B, Lepley AS, Harkey MS, et al. Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc. 2016;48(9):1671–1677. [DOI] [PubMed] [Google Scholar]
- 33.Pouderoux T, Muller B, Robert H. Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1979–1988. [DOI] [PubMed] [Google Scholar]
- 34.Quelard B, Rachet O, Sonnery-Cottet B, Chambat P. Rééducation postopératoire des greffes du ligament croisé antérieur. EMC - Kinésithérapie - Médecine Physique - Réadaptation. 2010;6(3):1–16. [Google Scholar]
- 35.Rambaud AJ, Neri T, Dingenen B, et al. The modifying factors that help improve anterior cruciate ligament reconstruction rehabilitation: a narrative review. Ann Phys Rehabil Med. 2022;65(4):101601. [DOI] [PubMed] [Google Scholar]
- 36.Rambaud AJ, Neri T, Edouard P. Reconstruction, rehabilitation and return-to-sport continuum after anterior cruciate ligament injury (ACLR3-continuum): call for optimized programs. Ann Phys Rehabil Med. 2022;65(4):101470. [DOI] [PubMed] [Google Scholar]
- 37.Rambaud AJM, Ardern CL, Thoreux P, Regnaux JP, Edouard P. Criteria for return to running after anterior cruciate ligament reconstruction: a scoping review. Br J Sports Med. 2018;52(22):1437–1444. [DOI] [PubMed] [Google Scholar]
- 38.Rambaud AJM, Semay B, Samozino P, et al. Criteria for return to sport after anterior cruciate ligament reconstruction with lower reinjury risk (CR’STAL study): protocol for a prospective observational study in France. BMJ Open. 2017;7(6):e015087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reichard LB, Croisier JL, Malnati M, Katz-Leurer M, Dvir Z. Testing knee extension and flexion strength at different ranges of motion: an isokinetic and electromyographic study. Eur J Appl Physiol. 2005;95(4):371–376. [DOI] [PubMed] [Google Scholar]
- 40.Ross MD, Denegar CR, Winzenried JA. Implementation of open and closed kinetic chain quadriceps strengthening exercises after anterior cruciate ligament reconstruction. J Strength Cond Res. 2001;15(4):466–473. [PubMed] [Google Scholar]
- 41.Saravia A, Cabrera S, Molina CR, Pacheco L, Muñoz G. Validity of the Genourob arthrometer in the evaluation of total thickness tears of anterior cruciate ligament. J Orthop. 2020;22:203–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith K, Miller N, Laslovich S. The reliability of the GNRB knee arthrometer in measuring ACL stiffness and laxity: implications for clinical use and clinical trial design. Int J Sports Phys Ther. 2022;17(6):1016–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tadokoro K, Matsui N, Yagi M, Kuroda R, Kurosaka M, Yoshiya S. Evaluation of hamstring strength and tendon regrowth after harvesting for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(7):1644–1650. [DOI] [PubMed] [Google Scholar]
- 44.Tagesson S, Öberg B, Good L, Kvist J. A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med. 2008;36(2):298–307. [DOI] [PubMed] [Google Scholar]
- 45.Wilk KE, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR, Boyd ML. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med. 1996;24(4):518–527. [DOI] [PubMed] [Google Scholar]
- 46.Williams GN, Snyder-Mackler L, Barrance PJ, Buchanan TS. Quadriceps femoris muscle morphology and function after ACL injury: a differential response in copers versus non-copers. J Biomech. 2005;38(4):685–693. [DOI] [PubMed] [Google Scholar]



