Abstract
Background/Aims
There is growing interest in whether Helicobacter pylori eradication (HPE) can affect body weight.
Methods
Data from 5 universities between January 2013 and December 2019 were analyzed retrospectively. H. pylori-positive subjects who had body weight measurements taken at least twice at intervals of 3 months or longer were included. Using propensity score (PS)-matched data, changes in body mass index (BMI) and the lipid profile after HPE were compared with the non-HPE group.
Results
Among 363 eligible patients, 131 HPE patients were PS-matched to 131 non-HPE patients. The median intervals between the measurements were 610 (range, 154-1250) days and 606 (range, 154-1648) days in the HPE and non-HPE groups, respectively. In both groups, the mean BMI increased (from 24.5 kg/m2 to 24.7 kg/m2 in the HPE group, and from 24.4 kg/m2 to 24.5 kg/m2 in the non-HPE group). The 2 groups did not show significantly different changes (P = 0.921). In the lowest baseline BMI quartile, the BMI increased after HPE by 1.23 (standard deviation [SD], 3.72) kg/m2 (P = 0.060), and the non-HPE group showed a decreased BMI at the time of follow-up (by −0.24 [SD, 5.25] kg/m2; P = 0.937) (between-group P = 0.214). Triglyceride levels increased after HPE (mean: 135 [SD, 78] to 153 [SD, 100] mg/dL; between-group P = 0.053).
Conclusion
The overall BMI change was not significantly different between the HPE and non-HPE groups, but patients with low BMI showed a tendency to gain weight after HPE. Triglyceride levels increased after HPE with marginal significance.
Keywords: Body mass index, Body weight, Helicobacter pylori, Lipids, Propensity score
Introduction
Several conflicting observational studies have reported associations between Helicobacter pylori infection and body weight. Some studies have observed an association between H. pylori infection and body mass index (BMI),1-3 whereas others have not.4 A proposed mechanism for body weight change is increased plasma levels of ghrelin after H. pylori eradication (HPE), which results in increased appetite,5-7 but the results regarding plasma ghrelin levels in previous studies are also conflicting.8-11
HPE therapy for patients with peptic ulcers is associated with weight gain.12,13 The effects of HPE in non-ulcer patients are less clear. A population-based randomized placebo-controlled study that analyzed the impact of HPE on body weight found that HPE was significantly associated with increased BMI.14 In a study among elderly people, HPE was significantly associated with elevated BMI.15 However, the presence of active ulcers was not controlled in the patients in these studies,14,15 and 1 study did not compare the HPE group with non-HPE controls.15
The purpose of this study is to analyze the impact of HPE on BMI. The secondary outcome is any change in the lipid profile after HPE. We collected data from 5 university hospitals that are affiliated with the Korean Society of Neurogastroenterology and Motility, and patients were propensity score (PS)-matched to account for measured and unmeasured confounding factors.
Materials and Methods
Study Population
Data were retrospectively collected from 5 university hospitals affiliated with the Korean Society of Neurogastroenterology and Motility. The 5 hospitals that participated in this study were Inje University Ilsan Paik Hospital, Catholic Kwandong University International St. Mary’s Hospital, Hallym University Chuncheon Sacred Heart Hospital, Ulsan University Gangneung Asan Hospital, and the Catholic University of Korea Eunpyung St. Mary’s Hospital. We analyzed adult patients’ data who participated in the general health screening program. Patients who tested positive on a general health screening for H. pylori infection using the rapid urease test, Warthin-Starry staining, or 13C-labeled urea breath test were included.
Data Collection and Outcome Measures
Height and weight were measured at enrollment and during follow-up at varying intervals. Upper endoscopic findings for active ulcers, ulcer scars, or non-ulcer gastritis at baseline were reviewed by physicians. Laboratory data including hemoglobin, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglyceride levels were collected. The hepatic steatosis index was calculated as follows16:
Hepatic steatosis index = 8 × alanine aminotransferase (ALT)/aspartate aminotransferase (AST) + BMI (if diabetes mellitus is present, +2; if the participant is female, +2)
Statistical Methods
To identify differences between the 2 PS-matched groups, within-group and between-group comparisons were made. To balance the differences between the HPE and non-HPE groups, PSs were generated using variables including baseline age, sex, the presence of an active peptic ulcer, and BMI. To compare the changes between the HPE and non-HPE groups (between-group comparisons), before-and-after change rates within the HPE and non-HPE groups were calculated and compared using the paired t test or the Wilcoxon signed-rank test, and comparisons were made between the HPE and non-HPE groups using the chi-square test or Fisher’s exact test for categorical data, and independent t test or Wilcoxon rank-sum test for continuous data. To compare the effects of HPE according to baseline BMI, we stratified patients by quartiles of baseline BMI and compared the between-group differences before and after HPE. For statistical analysis, SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata version 15.1 (Stata Corp., College Station, TX, USA) were used for analysis. The threshold for significance was P < 0.05.
Results
Baseline Characteristics
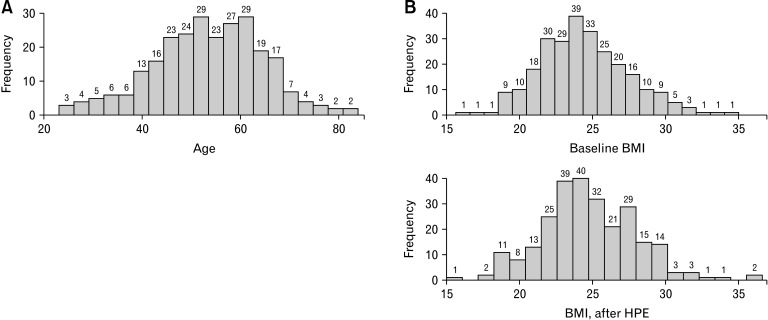
There were 195 patients in the HPE group and 168 in the non-HPE group before PS matching. The HPE group was older (median [range], 60 [23-87] vs 52 [25-84] years; P < 0.001) and contained more patients with active ulcers (n [%], 28 [14.4%] vs 13 [7.7%]; P = 0.047) than the non-HPE group (Table 1). After greedy matching with a caliper size of 0.33, 131 were selected in each group to create a PS-matched sample. Peptic ulcers were categorized as active (including healing ulcers) vs ulcer scars. The PS-matched groups showed no difference in median age (median [range], 55 [23-83] vs 54 [25-84] years) and proportion of patients with active ulcers (n [%], 12 [9.2%] vs 12 [9.2%]) in the HPE and non-HPE groups, respectively (Table 2). The distribution of baseline age and changes in BMI before and after HPE are shown in Figure. Baseline values in AST (mean 24.2 [95% CI, 22.4-26.1] vs 25.3 [95% CI, 23.5-27.1]; P = 0.423), ALT (mean 25.7 [95% CI, 21.9-29.5] vs 25.0 [95% CI, 22.0-28.0]; P = 0.793), and fasting blood glucose (mean 103.6 [95% CI, 98.8-108.4] vs 103.4 [95% CI, 96.9-109.9]; P = 0.953) were not different between HPE and non-HPE groups, respectively.
Table 1.
Baseline Characteristics Before Propensity Score-matching
| Characteristics | HPE (n = 195) | Non-HPE (n = 168) | P-value |
|---|---|---|---|
| Female | 93 (47.7) | 74 (44.1) | 0.487 |
| Age (yr) | 60 (23-87) | 52 (25-84) | < 0.001 |
| Interval between measurements (day) | 632 (105-1402) | 596 (150-1648) | 0.234 |
| Active ulcera | 28 (14.4) | 13 (7.7) | 0.047 |
| Eradication regimen | |||
| Triple therapy | 167 (85.6) | ||
| Quadruple therapy | 28 (14.4) | ||
| H. pylori test method | < 0.001 | ||
| Rapid urease test | 67 (38.9) | 19 (12.9) | |
| Warthin-Starry stain | 101 (58.7) | 128 (87.1) | |
| Urea-breath test | 4 (2.3) | 0 | |
| Site | < 0.001 | ||
| Inje University Ilsan Paik | 65 (33.3) | 68 (40.5) | |
| International St. Mary | 17 (8.7) | 69 (41.1) | |
| Hallym University Chuncheon Sacred Heart | 10 (5.1) | 0 (0.0) | |
| Gangneung Asan | 23 (11.8) | 21 (12.5) | |
| Eunpyung St. Mary | 80 (41.0) | 10 (6.0) |
aActive or healing ulcer vs ulcer scar or gastritis.
HPE, Helicobacter pylori (H. pylori) eradication.
Data are presented as n (%) or median (range).
Table 2.
Baseline Characteristics After Propensity Score-matching
| Characteristics | HPE (n = 131) | Non-HPE (n = 131) | P-value |
|---|---|---|---|
| Female | 64 (48.9) | 64 (48.9) | > 0.999 |
| Age (yr) | 55 (23-83) | 54 (25-84) | 0.637 |
| Interval between measurements (day) | 610 (156-1250) | 606 (154-1648) | 0.572 |
| Active ulcera | 12 (9.2) | 12 (9.2) | > 0.999 |
| Eradication regimen | |||
| Triple therapy | 114 (87.0) | ||
| Quadruple therapy | 17 (13.0) | ||
| H. pylori test method | < 0.001 | ||
| Rapid urease test | 52 (46.0) | 15 (12.9) | |
| Warthin-Starry stain | 59 (52.2) | 101 (87.1) | |
| Urea-breath test | 2 (1.8) | 0 (0.0) |
aActive or healing ulcer vs ulcer scar or gastritis.
HPE, Helicobacter pylori (H. pylori) eradication.
Data are presented as n (%) or median (range).
Figure.
Histogram of baseline age (A) and changes in body mass index (BMI) before and after Helicobacter pylori eradication (HPE) (B) among propensity score-matched data.
Changes in Body Mass Index and the Lipid Profile Among the Propensity Score-matched Groups
Table 3 shows within-group and between-group comparisons of variables related to BMI and the lipid profile among HPE and non-HPE patients. The mean BMI increased from 24.49 (SD, 2.79) kg/m2 to 24.66 (SD, 2.93) kg/m2 among HPE patients (P = 0.022), and from 24.39 (SD, 3.32) kg/m2 to 24.50 (SD, 3.63) kg/m2 among non-HPE patients (P = 0.083). The change in mean BMI (SD) after HPE was greater in HPE patients (0.72 kg/m2 [4.27]) than in non-HPE patients (0.42 kg/m2 [5.08]), but the difference was not statistically significant (P = 0.921). Other variables, including LDL cholesterol, HDL cholesterol, and total cholesterol, showed non-significant differences in the magnitude of change between HPE and non-HPE groups. Triglyceride levels increased after HPE (mean [SD] from 135 [78] mg/dL to 153 [100] mg/dL), whereas the non-HPE group showed no difference in triglyceride levels (mean [SD] from 128 [65] to 130 [65] mg/dL). The between-group P-value was marginally significant (P = 0.053).
Table 3.
Change of Body Mass Index and Lipid Profile Among Propensity Score-matched Helicobacter pylori Eradicated and non-Helicobacter pylori Eradicated Patients
| Characteristics | HPE (n = 131) | Within-group P-value |
Non-HPE (n = 131) | Within-group P-value |
Between-group P-value |
|---|---|---|---|---|---|
| BMI (kg/m2) | |||||
| Initial | 24.49 (2.79) | 24.39 (3.32) | 0.174 (T) | ||
| Follow-up | 24.66 (2.93) | 24.50 (3.63) | |||
| Change | 0.72 (4.27) | 0.022 (S) | 0.42 (5.08) | 0.083 (S) | 0.921 (W) |
| Hemoglobin (g/dL), mean | |||||
| Initial | 14.37 (4.06) | 14.35 (1.61) | 0.983 (T) | ||
| Follow-up | 14.12 (1.50) | 14.27 (1.56) | |||
| Change | 0.16 (9.87) | 0.784 (S) | –0.16 (5.98) | 0.695 (S) | 0.599 (W) |
| C-reactive protein (mg/dL) | |||||
| Initial | 0.32 (0.52) | 0.17 (0.35) | 0.307 (T) | ||
| Follow-up | 0.44 (0.92) | 0.27 (0.66) | |||
| Change | 2.90 (63.57) | 0.877 (P) | 81.33 (201.78) | 0.418 (P) | 0.439 (T) |
| Total cholesterol (mg/dL) | |||||
| Initial | 186.68 (37.39) | 193.59 (36.43) | 0.149 (T) | ||
| Follow-up | 182.68 (36.60) | 191.20 (40.81) | |||
| Change | –1.91 (14.71) | 0.250 (P) | –0.06 (14.58) | 0.866 (S) | 0.710 (W) |
| HDL cholesterol (mg/dL) | |||||
| Initial | 49.63 (21.87) | 42.84 (21.56) | 0.398 (T) | ||
| Follow-up | 48.36 (49.34) | 46.46 (49.83) | |||
| Change | –38.77 (169.59) | 0.027 (S) | –4.82 (137.88) | 0.475 (S) | 0.438 (W) |
| LDL cholesterol (mg/dL) | |||||
| Initial | 112.10 (34.53) | 119.55 (32.50) | 0.152 (T) | ||
| Follow-up | 110.37 (34.39) | 113.13 (31.26) | |||
| Change | 0.75 (28.06) | 0.823 (S) | –1.87 (17.30) | 0.147 (S) | 0.497 (W) |
| Triglycerides (mg/dL) | |||||
| Initial | 135.47 (78.42) | 128.92 (65.62) | 0.697 (T) | ||
| Follow-up | 153.47 (100.16) | 130.13 (64.25) | |||
| Change | 20.56 (63.98) | 0.009 (S) | 5.74 (38.00) | 0.456 (S) | 0.053 (W) |
| Hepatic steatosis index | |||||
| Initial | 33.94 (24.32-45.64) | 32.84 (19.42-52.66) | 0.050 (T) | ||
| Follow-up | 34.17 (25.29-49.30) | 32.88 (22.70-46.55) | |||
| Change | –0.22 (9.12) | 0.816 (P) | 0.47 (8.25) | 0.579 (P) | 0.585 (T) |
HPE, Helicobacter pylori (H. pylori) eradication; BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein; PS, propensity score.
Between-group P-value: categorical data, chi-square test (C) or Fisher exact test (F); continuous data, independent t test (T) or Wilcoxon rank-sum test (W); within-group P-value, paired t test (P) or Wilcoxon signed-rank test (S). A P < 0.05 was considered statistically significant.
Data are presented as mean (SD) or median (range).
Change in Body Mass Index According to Baseline Body Mass Index Quartiles
In the lowest baseline BMI quartile group, the BMI increased after HPE with marginal significance (1.23 [SD, 3.72] kg/m2, P = 0.060), and the non-HPE group showed a decreased BMI after HPE (–0.24 [SD, 5.25] kg/m2, P = 0.937). However, the between-group difference was not significant (P = 0.214). BMI increased in all other quartiles after HPE, although the between-group differences were not significant (Table 4).
Table 4.
Changes in Body Mass Index Among Propensity Score-matched Helicobacter pylori Eradicated and non-Helicobacter pylori Eradicated Patients According to the Baseline Body Mass Index Quartiles
| Groups | HPE (n = 131) | non-HPE (n = 131) |
|---|---|---|
| BMI Q1 (kg/m2) | ||
| Initial | ||
| n | 33 | 39 |
| Range | 17.47-22.51 | 15.61-22.51 |
| Mean (SD) | 21.09 (1.24) | 20.80 (1.40) |
| Between-group P-value | 0.340 (W) | |
| Follow-up | ||
| n | 33 | 39 |
| Range | 18.07-24.24 | 15.01-23.21 |
| Mean (SD) | 21.35 (1.44) | 20.75 (1.73) |
| Between-group P-value | 0.207 (W) | |
| Change | ||
| n | 33 | 39 |
| Mean (SD) | 1.23 (3.72) | –0.24 (5.25) |
| Within-group P-value | 0.066 (P) | 0.937 (S) |
| Between-group P-value | 0.214 (W) | |
| BMI Q2 (kg/m2) | ||
| Initial | ||
| n | 33 | 35 |
| Range | 22.52-24.35 | 22.64-24.35 |
| Mean (SD) | 23.42 (0.58) | 23.57 (0.51) |
| Between-group P-value | 0.244 (W) | |
| Follow-up | ||
| n | 33 | 35 |
| Range | 18.99-24.96 | 19.83-26.79 |
| Mean (SD) | 23.61 (1.12) | 23.71 (1.27) |
| Between-group P-value | 0.980 (W) | |
| Change | ||
| n | 33 | 35 |
| Mean (SD) | 0.83 (4.71) | 0.58 (4.76) |
| Within-group P-value | 0.050 (S) | 0.184 (S) |
| Between-group P-value | 0.956 (W) | |
| BMI Q3 (kg/m2) | ||
| Initial | ||
| n | 34 | 27 |
| Range | 24.46-26.56 | 24.43-26.56 |
| Mean (SD) | 25.41 (0.62) | 25.42 (0.62) |
| Between-group P-value | 0.967 (T) | |
| Follow-up | ||
| n | 34 | 27 |
| Range | 23.12-29.79 | 22.84-29.26 |
| Mean (SD) | 25.55 (1.47) | 25.72 (1.46) |
| Between-group P-value | 0.651 (T) | |
| Change | ||
| n | 34 | 27 |
| Mean (SD) | 0.53 (4.85) | 1.21 (5.44) |
| Within-group P-value | 0.531 (P) | 0.259 (P) |
| Between-group P-value | 0.607 (T) | |
| BMI Q4 (kg/m2) | ||
| Initial | ||
| n | 31 | 30 |
| Range | 26.70-31.25 | 26.64-35.01 |
| Mean (SD) | 28.25 (1.32) | 29.08 (2.06) |
| Between-group P-value | 0.130 (W) | |
| Follow-up | ||
| n | 31 | 30 |
| Range | 25.21-33.68 | 23.05-36.63 |
| Mean (SD) | 28.33 (1.75) | 29.20 (2.73) |
| Between-group P-value | 0.139 (W) | |
| Change | ||
| n | 31 | 30 |
| Mean (SD) | 0.27 (3.75) | 0.37 (5.01) |
| Within-group P-value | 0.691 (P) | 0.228 (S) |
| Between-group P-value | 0.579 (W) |
HPE, Helicobacter pylori eradication; BMI, body mass index; Q1-4, quartile 1-4; SD, standard deviation.
Between-group P-value: categorical data, chi-square test (C) or Fisher exact test (F); continuous data, independent t test (T) or Wilcoxon rank-sum test (W); within-group P-value: paired t test (P) or Wilcoxon signed-rank test (S).
Change in Body Mass Index According to Age and Sex
The BMI change among males (mean 0.50 [SD 4.13] vs 0.89 [4.99], P = 0.632) and females (mean 0.75 [SD 4.36] vs 0.01 [SD 5.06], P = 0.377) were not significantly different between HPE and non-HPE groups, respectively. The interaction effect between sex and HPE was not significant (P = 0.330). When we categorized by patient aged 60 years, there was also no significant difference in BMI change between HPE and non-HPE groups. The BMI change among elderly > 60 years was a mean of 0.18 [SD 3.31], and a mean of –0.40 [SD 7.02], in HPE and non-HPE groups, respectively (P = 0.626). In patients below 60 years, the BMI change was a mean of 0.85 [SD 4.62], and a mean of 0.85 [SD 3.81], in HPE and non-HPE groups, respectively (P = 0.997). The interaction effect between age and HPE was not significant (P = 0.639).
Discussion
In this study, we compared the changes in BMI and the lipid profile between HPE and non-HPE groups. BMI and lipid markers increased in both the HPE and non-HPE groups, and the magnitudes of change were not significantly different between the groups. We performed a PS-matched analysis to account for the variables that could potentially bias the results, such as the presence of active ulcer17 and baseline age.18 A stratified analysis by quartiles of baseline BMI was performed to test the difference in BMI change in HPE and non-HPE groups.
H. pylori colonization is almost always associated with chronic active gastritis, which exerts various effects, such as interfering with gastric hormone regulation, including ghrelin and leptin. H. pylori eradication increases serum ghrelin levels,5,8-10,19 which increases body weight by increasing the appetite and food intake.20 Several epidemiological studies focusing on the correlation between H. pylori colonization and BMI and obesity have shown contrasting results.1,2,13,15,21-25 A study from the Netherlands showed no evidence supporting a clinically relevant association between H. pylori and BMI/obesity, but a small negative association with obesity was present.25 In a prospective randomized study of 1558 H. pylori-infected patients conducted in 2011, the BMI increased significantly after 6 months following randomization to H. pylori eradication therapy.14 A meta-analysis from Japan reported increased HDL cholesterol and triglyceride levels after HPE, with no or little change in LDL cholesterol levels.26 Our data showed no difference in HDL, LDL, and total cholesterol levels between the HPE and non-HPE groups, but triglyceride levels increased after HPE with marginal significance (P = 0.053). The reasons for these changes are unclear, but reductions in hepatic lipase and cholesterol ester transfer protein caused by the suppression of inflammation following HPE, or a reduction in lipoprotein lipase activity due to insulin resistance could have led to an increase in triglyceride levels following HPE.27-29
To compare the BMI changes in extremes of baseline BMI, we conducted a subgroup analysis by quartiles of baseline BMI. In patients with the lowest baseline BMI, the HPE group showed an increase in BMI, whereas the non-HPE group showed a decrease in BMI (mean [SD] changes, 1.23 [3.72] kg/m2 vs –0.24 [5.25] kg/m2, respectively; P = 0.214). The HPE patients in this subgroup showed an increased BMI with marginal significance (P = 0.060). Since the number of participants in this subgroup was insufficient (33 and 39 patients in each HPE and non-HPE group, respectively), the difference between the HPE and non-HPE groups was not significant. There is a definite need for a more focused analysis in the future, especially among patients showing sarcopenia or cachexia. Considering a Chinese study of elderly individuals,15 HPE therapy could prevent further weight loss in those with sarcopenia or frailty. Among patients with the highest baseline BMI, the change in BMI after HPE was minimal (mean change [SD], 0.27 [3.75], P = 0.691). Obese patients with H. pylori infections should not be discouraged from receiving eradication therapy.
We also performed stratified analyses for baseline age and sex and tested for the interaction effects. In a recent study in Korea, the HDL levels increased, and LDL levels decreased after eradication in females, whereas BMI, but not HDL, increased in male subjects.30 It was suggested that the sex hormones could have caused differences in sex, but the exact mechanisms remained unknown. Our study showed no difference in sex and baseline age between HPE and non-HPE groups, and the interaction effects were also not significant. Perhaps a more detailed prospective analysis on this subject with a larger sample is required.
This study has some limitations. First, the follow-up time was not controlled and was different for every patient. Most of our data came from routine health-screening participants, which is usually carried out at 2-year intervals in Korea; hence the median interval between weight measurements (ie, after HPE in patients who underwent HPE) was 632 days. It is possible that HPE could have had a shorter-term effect on BMI that was not captured in this study. Second, as this was a retrospective study, there is a chance of bias, even after PS matching. There was also a chance of inaccurate measurements of body weight, and the treatment success rate of HPE is unknown. In addition, the baseline prevalence of dyslipidemia or diabetes was not considered into account. Third, the number of participants in our study was relatively small. Despite these limitations, this study combined the treatment results of various centers in Korea on weight change after HPE. In particular, HPE could promote weight gain in the underweight population.
In conclusion, the BMI and lipid profile did not show a significant difference between HPE and non-HPE groups among H. pylori-positive patients. Patients with low BMI showed a tendency to gain weight after HPE. In addition, there was a tendency among H. pylori-eradicated patients to show increased triglyceride levels. Further studies with a prospective design and fixed follow-up BMI measurement schedules are required.
Funding Statement
Financial support: None.
Footnotes
Conflicts of interest: None.
Author contributions: Jong Wook Kim designed the study and analyzed the data, drafted the manuscript, tables, and figures, and approved the final version to be published; Myong Ki Baeg analyzed the data, revised the manuscript, and approved the final version; Chang Seok Bang and Jong-Kyu Park analyzed the data and approved the final version; and Jung-Hwan Oh analyzed the data, revised the draft, tables, and figures, and approved the final version.
References
- 1.Kopacova M, Bures J, Koupil I, et al. Body indices and basic vital signs in Helicobacter pylori positive and negative persons. Eur J Epidemiol. 2007;22:67–75. doi: 10.1007/s10654-006-9090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenstock SJ, Jorgensen T, Andersen LP, Bonnevie O. Association of Helicobacter pylori infection with lifestyle, chronic disease, body-indices, and age at menarche in Danish adults. Scand J Public Health. 2000;28:32–40. doi: 10.1177/140349480002800107. [DOI] [PubMed] [Google Scholar]
- 3.Russo A, Eboli M, Pizzetti P, et al. Determinants of Helicobacter pylori seroprevalence among Italian blood donors. Eur J Gastroenterol Hepatol. 1999;11:867–873. doi: 10.1097/00042737-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Cho I, Blaser MJ, Francois F, et al. Helicobacter pylori and overweight status in the United States: data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2005;162:579–584. doi: 10.1093/aje/kwi237. [DOI] [PubMed] [Google Scholar]
- 5.Nwokolo CU, Freshwater DA, O'Hare P, Randeva HS. Plasma ghrelin following cure of Helicobacter pylori. Gut. 2003;52:637–640. doi: 10.1136/gut.52.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Francois F, Roper J, Joseph N, et al. The effect of H. pylori eradication on meal-associated changes in plasma ghrelin and leptin. BMC Gastroenterol. 2011;11:37. doi: 10.1186/1471-230X-11-37.f91deee1ce194406881b6ae589f393ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prinz P, Stengel A. Control of food intake by gastrointestinal peptides: mechanisms of action and possible modulation in the treatment of obesity. J Neurogastroenterol Motil. 2017;23:180–196. doi: 10.5056/jnm16194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osawa H, Kita H, Ohnishi H, et al. Changes in plasma ghrelin levels, gastric ghrelin production, and body weight after Helicobacter pylori cure. J Gastroenterol. 2006;41:954–961. doi: 10.1007/s00535-006-1880-4. [DOI] [PubMed] [Google Scholar]
- 9.Osawa H, Nakazato M, Date Y, et al. Impaired production of gastric ghrelin in chronic gastritis associated with Helicobacter pylori. J Clin Endocrinol Metab. 2005;90:10–16. doi: 10.1210/jc.2004-1330. [DOI] [PubMed] [Google Scholar]
- 10.Pacifico L, Anania C, Osborn JF, et al. Long-term effects of Helicobacter pylori eradication on circulating ghrelin and leptin concentrations and body composition in prepubertal children. Eur J Endocrinol. 2008;158:323–332. doi: 10.1530/EJE-07-0438. [DOI] [PubMed] [Google Scholar]
- 11.Nweneka CV, Prentice AM. Helicobacter pylori infection and circulating ghrelin levels - a systematic review. BMC Gastroenterol. 2011;11:7. doi: 10.1186/1471-230X-11-7.e71cf1e1224e4a3faf2bacbdc538c283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujiwara Y, Higuchi K, Arafa UA, et al. Long-term effect of Helicobacter pylori eradication on quality of life, body mass index, and newly developed diseases in Japanese patients with peptic ulcer disease. Hepatogastroenterology. 2002;49:1298–1302. [PubMed] [Google Scholar]
- 13.Kamada T, Hata J, Kusunoki H, et al. Eradication of Helicobacter pylori increases the incidence of hyperlipidaemia and obesity in peptic ulcer patients. Dig Liver Dis. 2005;37:39–43. doi: 10.1016/j.dld.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Lane JA, Murray LJ, Harvey IM, Donovan JL, Nair P, Harvey RF. Randomised clinical trial: Helicobacter pylori eradication is associated with a significantly increased body mass index in a placebo-controlled study. Aliment Pharmacol Ther. 2011;33:922–929. doi: 10.1111/j.1365-2036.2011.04610.x. [DOI] [PubMed] [Google Scholar]
- 15.Maruyama M, Kamimura K, Hoshiyama A, et al. Effect of Helicobacter pylori eradication on elder cases: observational study in community-based medicine. World J Clin Cases. 2017;5:412–418. doi: 10.12998/wjcc.v5.i12.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JH, Kim D, Kim HJ, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:503–508. doi: 10.1016/j.dld.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician. 2007;76:1005–1012. doi: 10.5772/18607. [DOI] [PubMed] [Google Scholar]
- 18.Ali S, Garcia JM. Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options - a mini-review. Gerontology. 2014;60:294–305. doi: 10.1159/000356760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osawa H. Ghrelin and Helicobacter pylori infection. World J Gastroenterol. 2008;14:6327–6333. doi: 10.3748/wjg.14.6327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes Rev. 2007;8:21–34. doi: 10.1111/j.1467-789X.2006.00270.x. [DOI] [PubMed] [Google Scholar]
- 21.Lender N, Talley NJ, Enck P, et al. Review article: associations between Helicobacter pylori and obesity--an ecological study. Aliment Pharmacol Ther. 2014;40:24–31. doi: 10.1111/apt.12790. [DOI] [PubMed] [Google Scholar]
- 22.Lim SH, Kim N, Kwon JW, et al. Positive association between Helicobacter pylori infection and metabolic syndrome in a Korean population: a multicenter nationwide study. Dig Dis Sci. 2019;64:2219–2230. doi: 10.1007/s10620-019-05544-3. [DOI] [PubMed] [Google Scholar]
- 23.Pundak OY, Topf Olivestone C, Hofi L, Kori M. Lack of association between Helicobacter pylori infection and childhood overweight/obesity. Helicobacter. 2020;25:e12728. doi: 10.1111/hel.12728. [DOI] [PubMed] [Google Scholar]
- 24.Xu X, Li W, Qin L, Yang W, Yu G, Wei Q. Relationship between Helicobacter pylori infection and obesity in Chinese adults: a systematic review with meta-analysis. PLoS One. 2019;14:e0221076. doi: 10.1371/journal.pone.0221076.22637b2ac590473286a0d1020c1bb4f4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.den Hollander WJ, Broer L, Schurmann C, et al. Helicobacter pylori colonization and obesity - a Mendelian randomization study. Sci Rep. 2017;7:14467. doi: 10.1038/s41598-017-14106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watanabe J, Hamasaki M, Kotani K. The effect of Helicobacter pylori eradication on lipid levels: a meta-analysis. J Clin Med. 2021;10:904. doi: 10.3390/jcm10050904.6e1bca08938a43ceb7b9461c22f62899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dongiovanni P, Stender S, Pietrelli A, et al. Causal relationship of hepatic fat with liver damage and insulin resistance in nonalcoholic fatty liver. J Intern Med. 2018;283:356–370. doi: 10.1111/joim.12719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kar D, Gillies C, Zaccardi F, et al. Relationship of cardiometabolic parameters in non-smokers, current smokers, and quitters in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2016;15:158. doi: 10.1186/s12933-016-0475-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kolovou GD, Anagnostopoulou KK, Kostakou PM, Mikhailidis DP. Cholesterol ester transfer protein (CETP), postprandial lipemia and hypolipidemic drugs. Curr Med Chem. 2009;16:4345–4360. doi: 10.2174/092986709789712853. [DOI] [PubMed] [Google Scholar]
- 30.Park J, Kim N, Kim WS, et al. Long-term effects of the eradication of Helicobacter pylori on metabolic parameters, depending on sex, in South Korea. Gut Liver. 2022;17:58–68. doi: 10.5009/gnl210588. [DOI] [PMC free article] [PubMed] [Google Scholar]