Abstract
Introduction
Two group and save (G&S) samples are routinely collected from patients undergoing diagnostic laparoscopy and/or emergency appendicectomy. We aimed to identify the necessity of this practice by looking at the perioperative transfusion rates.
Methods
Data were obtained from our electronic theatre system for all patients who underwent emergency laparoscopic surgery (specifically diagnostic laparoscopy and/or laparoscopic appendicectomy) between January 2017 and December 2018. Records were reviewed for the number of G&S samples sent and perioperative transfusion rates.
Results
A total of 451 patients were included in the study. The numbers of procedures performed in 2017 and 2018 were 202 (44.8%) and 249 (55.2%), respectively. The total number of samples sent was 930. Only 786 (84.5%) samples were processed and the rest were rejected for various reasons. Of the 451 patients included in the study, 308 (68.3%) had two G&S samples sent, whereas 41 patients (9.1%) had only one G&S sample sent. Fifty-six (12.4%) and 20 (4.4%) patients had three and four G&S samples sent, respectively. Only two patients required transfusion perioperatively (0.4%), and the indication in both was irrelevant to the primary operation.
Conclusions
These results demonstrate a near-zero transfusion rate in this patient cohort. Omitting G&S is safe and potentially saves time and resources.
Keywords: Emergencies, Laparoscopy, Blood grouping and cross-matching
Introduction
Improving the quality of patient care while ensuring an efficient use of resources is critical in any healthcare system. Routine group and save (G&S) screening is one of the key avenues for investigation in this context. In the setting of preoperative workup, sampling may or may not be necessary.
G&S testing includes determining the ABO and RhD groups of the patient’s blood. It also includes screening of patient’s plasma for the presence of atypical antibodies. Centres across the UK have their in-house protocols regarding routine collection of G&S samples in both elective and emergency settings.1 The rationale behind this is based on the possibility of a major haemorrhage during surgery that will require an emergent blood transfusion. Nevertheless, previous studies have shown that the incidence of major blood loss is very low.2–4
Guidelines at our institution require all patients undergoing emergency laparoscopic surgery due to right iliac fossa (RIF) pain (namely diagnostic laparoscopies and/or appendicectomies) to have two G&S samples collected as part of their preoperative assessment. The aim of this study was to examine the necessity and cost-effectiveness of this practice by looking at the perioperative transfusion rates.
Methods
Data were retrieved from an electronic hospital coding system (known as Opera) covering a two-year period extending from 1 January 2017 to 31 December 2018. Data included information on all patients who underwent emergency laparoscopic surgery (specifically diagnostic laparoscopy and/or laparoscopic appendicectomy) during the specified period. Patients’ records were then reviewed retrospectively for: (1) whether G&S samples were sent for each patient, (2) numbers of samples sent, (3) numbers of samples rejected by the blood bank, and (4) reasons for rejection.
The rate of blood transfusion in this cohort of patients was subsequently investigated. Patients found to have been transfused perioperatively were further examined for indications (pre-existing medical conditions or operative injuries) and the timing of blood transfusion (intra- or perioperatively). Laparoscopic gynaecological procedures were excluded from the study. Data analysis was performed using SPSS software and data presented as percentages and frequencies.
Results
During the study period, a total of 451 patients underwent an emergency laparoscopic surgery due to RIF pain (diagnostic laparoscopy and/or laparoscopic appendicectomy). The mean age of patients in this cohort was 33.3 years (SD 15.3, median 30, range 7–85). See Table 1 for a distribution by age. The gender ratio was 42.6% female (n = 192) to 57.4% male (n = 259). The numbers of procedures performed in 2017 and 2018 were 202 (44.8%) and 249 (55.2%), respectively.
Table 1 .
Distribution by age
| Patient age | n |
|---|---|
| 1–20 | 70 |
| 21–40 | 266 |
| 41–60 | 83 |
| 61–80 | 29 |
| 81–100 | 3 |
n, number of patients in each age group
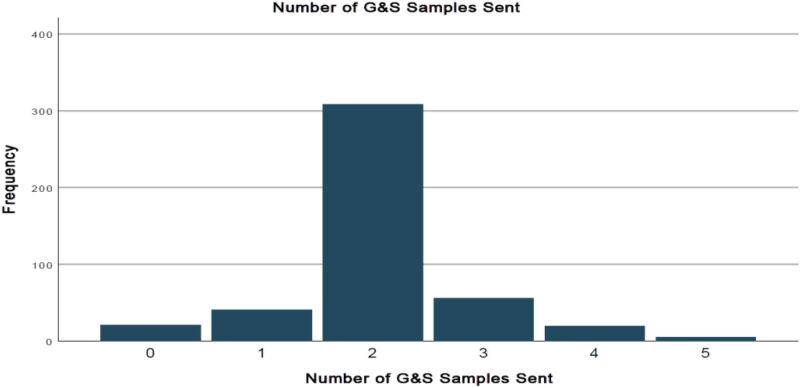
The total number of G&S samples sent was 930, of which 786 (84.5%) were processed and the rest (n = 144, 15.4%) were rejected by the blood bank for various reasons (highlighted in Table 2). Of the 451 patients included in the study, 308 (68.3%) had two G&S samples sent, whereas 41 patients (9.1%) had only one G&S sample sent. Fifty-six (12.4%) and 20 (4.4%) patients had three and four G&S samples sent, respectively (Figure 1).
Table 2 .
Reason for rejection of sample
| Reason | n |
|---|---|
| Inaccurate or missing details | 42 |
| Valid sample already available | 32 |
| Samples sent at the same time | 35 |
| Insufficient/haemolysed/clotted sample | 8 |
| Using pre-printed labels | 6 |
| Missing/unclear reason | 2 |
n, number of times the reason was mentioned
Figure 1 .
Number of group and save (G&S) samples sent
Of the 451 patients, only two required transfusion of packed red blood cells perioperatively, representing an overall transfusion rate of 0.4%, and the indication for transfusion in both patients was not directly due to operative complication. Patient 1 had Von Willebrand disease requiring a planned transfusion of blood and platelets following a discussion with the haematology specialists. Patient 2 had rectal bleeding at day 3 postoperatively. A gastroscopy in this patient demonstrated a duodenal ulcer and rectal and sigmoid polyps.
Discussion
National guidance
Valid G&S samples are often required in UK hospitals prior to surgery to ensure that cross-matched blood can be made available in case of a major perioperative haemorrhage. However, G&S screening is not considered part of routine preoperative testing for elective surgery in the most recent National Institute for Health and Care Excellence (NICE) guidelines (2016).5 There is currently no consensus or national guidance in the UK regarding routine G&S screening for patients undergoing emergency laparoscopic surgery.1
Evidence of safety
Several studies have previously reported very low rates of blood transfusion in laparoscopic general surgical operations. Ghirardo et al, reported a transfusion rate of 0.16% (n = 1) for laparoscopic appendicectomy in a sample of 613 patients.2 A similar study performed at University College London Hospitals NHS Foundation Trust (UCLH) in 2016 covering elective day-case laparoscopic operations reported a perioperative transfusion rate of 0.18% (n = 1). This patient was transfused to optimise pre-existing anaemia following a staging laparoscopy for an upper gastrointestinal cancer.6
Potential futility of sampling
The main factor requiring emergency blood transfusion in laparoscopic surgery is vascular injury during trocar insertion. However, the risk of major bleeding when accessing the peritoneal cavity has been reported at very low rates (0.02–0.04% for intra-abdominal vessels and 0.25–0.6% for abdominal wall vessels).1 Nevertheless, cross-matched blood would not be available immediately and the urgency of blood transfusion means that O-negative blood would most likely be used while a formal cross-match could be determined.7 In any case, immediate management in such a scenario would focus on operative measures to control the bleeding, such as the conversion to an open procedure or laparotomy.6
Individual risk assessment
The requirement for blood transfusion often relates to the presence of a pre-existing medical issue such as anaemia or anticoagulation therapy rather than the surgery itself.2 This fact supports that G&S testing should be done selectively and on an individualised basis.
Potential resource savings
At our institution, the cost of processing a single G&S sample is £12. When applying this figure to the total number of samples processed in our cohort, the cost would have been £9,432. In 2018–2019, 49,279 appendicectomies were performed in the NHS. Accordingly, the total cost if two G&S samples were processed for each patient in this cohort would have been £1,182,696.8 Moreover, it is estimated that each G&S sample takes at least 35–45 minutes to process and the time spent by staff on this can be as high as 55% of a normal working day.9,10
Our study has led UCLH to omit the requirement for routine G&S testing for patients investigated for RIF pain. Other studies have reached similar conclusions resulting in the immediate elimination of this practice in several other procedures without risking patient safety or reducing the quality of patient care.3,4,11–14
Conclusions
Our results show that omitting routine preoperative G&S testing for patients undergoing emergency diagnostic laparoscopy or laparoscopic appendicectomy is safe and clinically appropriate. We believe that eliminating this practice or implementing it on an individualised risk assessed basis would lead to substantial workload reduction and financial savings across healthcare systems.
Acknowledgements
Study design: SA, TT and IR; data collection: SA and TT; data analysis and manuscript writing: SA; manuscript revision and supervision: IR. Special thanks to Mr Khaled Dawas, the head of Upper Gastrointestinal Surgery Department at the UCLH for supporting this project. The abstract of this paper was presented by Dr Said Alyacoubi at international meetings organised by the Association of Surgeons in Training (ASiT) and the Association of Surgeons of Great Britain and Ireland (ASGBI) during 2020.
References
- 1.Barrett-Lee J, Vatish J, Vazirian-Zadeh M, Waterland P. Routine blood group and antibody screening prior to emergency laparoscopy. Ann R Coll Surg Engl 2018; 100: 322–325. 10.1308/rcsann.2018.0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghirardo SF, Mohan I, Gomensoro A, Chorost MI. Routine preoperative typing and screening: a safeguard or a misuse of resources. J Soc Laparoendosc Surg 2010; 14: 395–398. 10.4293/108680810X12924466007241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Usal H, Nabagiez J, Sayad P, Ferzli GS. Cost effectiveness of routine type and screen testing before laparoscopic cholecystectomy. Surg Endosc 1999; 13: 146–147. 10.1007/s004649900925 [DOI] [PubMed] [Google Scholar]
- 4.Ransom SB, McNeeley SG, Hosseini RB. Cost-effectiveness of routine blood type and screen testing before elective laparoscopy. Obstet Gynecol 1995; 86: 346–348. 10.1016/0029-7844(95)00187-V [DOI] [PubMed] [Google Scholar]
- 5.NICE. Routine preoperative tests for elective surgery. NICE Guidel. https://www.nice.org.uk/guidance/ng45 (cited February 2021) [Google Scholar]
- 6.Thomson PM, Ross J, Mukherjee S, Mohammadi B. Are routine blood group and save samples needed for laparoscopic day case surgery? World J Surg 2016; 40: 1295–1298. 10.1007/s00268-016-3463-8 [DOI] [PubMed] [Google Scholar]
- 7.Hamza N, Pereira M, Gilliam A. Routine ‘group and save’ is unnecessary on the day of surgery for elective laparoscopic cholecystectomy. Bull R Coll Surg Engl 2015; 97: E1–E4. 10.1308/147363515X14272809071167 [DOI] [Google Scholar]
- 8.NHS Digital. Hospital admitted patient care activity 2018–19: procedures and interventions. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2018-19 (cited February 2021)
- 9.Parker S, Mahawar K, Balupuri Set al. Routine group and save unnecessary for gastric band surgery: a retrospective case review audit of 1018 bariatric patients. Clin Obes 2012; 2: 73–77. 10.1111/j.1758-8111.2012.00043.x [DOI] [PubMed] [Google Scholar]
- 10.Malik H, Bishop H, Winstanley J. Audit of blood transfusion in elective breast cancer surgery - Do we need to group and save pre-operatively? Ann R Coll Surg Engl 2008; 90: 472–473. 10.1308/003588408X301091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ransom SB, Fundaro G, Dombrowski MP. Cost-effectiveness of routine blood type and screen testing for cesarean section. J Reprod Med Obstet Gynecol. 1999; 44: 592–594. [PubMed] [Google Scholar]
- 12.Ransom SB, McNeeley SG, Malone J. A cost-effectiveness evaluation of preoperative type-and-screen testing for vaginal hysterectomy. Am J Obstet Gynecol 1996; 175: 1201–1203. 10.1016/s0002-9378(96)70028-5 [DOI] [PubMed] [Google Scholar]
- 13.Ransom SB, Fundaro G, Dombrowski MP. The cost-effectiveness of routine type and screen admission testing for expected vaginal delivery. Obstet Gynecol 1998; 92: 493–495. 10.1016/S0029-7844(98)00288-9 [DOI] [PubMed] [Google Scholar]
- 14.Lin JS, Chen YJ, Tzeng CHet al. Revisiting of preoperative blood ordering policy - A single institute’s experience in Taiwan. J Chinese Med Assoc. 2006; 69: 507–511. 10.1016/S1726-4901(09)70319-3 [DOI] [PubMed] [Google Scholar]