Radiology is an integral component of any healthcare system and often plays a decisive role in the diagnosis and management of patients today. Radiology has undergone a complete metamorphosis in last 2–3 decades keeping pace with the ongoing revolution in digital, information, and communication technology. Advancement in hardware and software technology has led to the development of sophisticated equipment, and it may be digital radiography, ultrasonography, multi-detector computed tomography (MDCT), high-field magnetic resonance imaging (MRI) with better resolution, faster imaging, and overall, higher throughput. Last two decades have witnessed a significant rise in the utilization of radiology services (24 × 7), particularly CT scans, across the globe.1, 2, 3 Routine use of MDCT and high-field MRI with the ability to acquire thin section, high-resolution images, multiphasic, dynamic studies, and 3D imaging have led to the generation of unprecedented volume of data on a daily basis. On an average, today's radiologist has to analyze several hundreds to thousands of images including multi-planar reconstructions for every patient depending on the modality and type of cross-sectional imaging study performed before a report is generated. Thus, radiology today has become essentially a data-driven and data-intensive specialty. Whereas the data generation has been rising in geometric progression, the same needs to be reported upon by relatively finite or at best slowly increasing number of radiologists. Thus, there remains a dilemma of quantity vs quality and accountability. Such demand vs supply mismatch tends to put additional work pressure with resultant fatigue among the practicing radiologists with its potential consequences.4,5
With continued improvement in radiology workstation, the development of Digital Imaging and Communications in Medicine (DICOM) standard, Picture Archiving and Communication System (PACS), and Radiology Information System (RIS) have made a major impact and allowed clinicians to view digital images at their respective workplaces and store medical imaging data in a local server as desired. With the availability of high bandwidth internet connectivity capable of transmission of large volume of digital data, remote assessment and radiology reporting also known as teleradiology became feasible. Teleradiology has the inherent advantage of not being limited by geographic boundaries and time zone which has partially offset the problem of availability of radiologist at a particular location and also reduced turnaround time for radiology reporting. Although teleradiology has been widely practiced for more than two decades from now, it has its own share of pros and cons. Detailed deliberation about teleradiology is beyond the scope of this paper.
Image interpretation and reporting have long been considered the primary task of a radiologist. However, image interpretation radiology is a complex cognitive process and is prone to a wide variety of cognitive biases. Errors in diagnostic radiology are not uncommon and are mostly attributed to misses and misinterpretations.6, 7, 8 One of the contributing factors could be the large amount of data/number of images generated for each patient and viewed by a radiologist in a relatively limited timeframe.
Time and again, mankind has sought answer for the question, whether machines could carry out certain intellectual tasks which are normally expected to be performed by a human being. Soon, it was realized that machines do have the potential to carry out cognitive tasks, sometimes even better than a human being, provided the machine has been adequately prepared for that task. This led to the genesis of artificial intelligence (AI) in the late 1950s.9 AI can be simply defined as the capability of machines to perform cognitive tasks which are normally performed by humans. AI can mimic human intellect having the ability to learn and then solve a particular problem. During the initial days, AI was thought as more of an imagination and less probable. Since its inception, AI has gone through several ups and downs. With the availability of big medical data, internet of healthcare things, cloud computing, sophisticated machine learning (ML), and better algorithms, AI regained its momentum in the recent past in the field of healthcare, particularly, radiology. Today, with advancement in computing and information technology, AI is a fast-growing field and is a reality. AI holds great promise in many facets of radiology practice both in the interpretive as well as non-interpretive domains.10,11 It is time to examine in brief feasibility and utility of AI in the field of radiology.
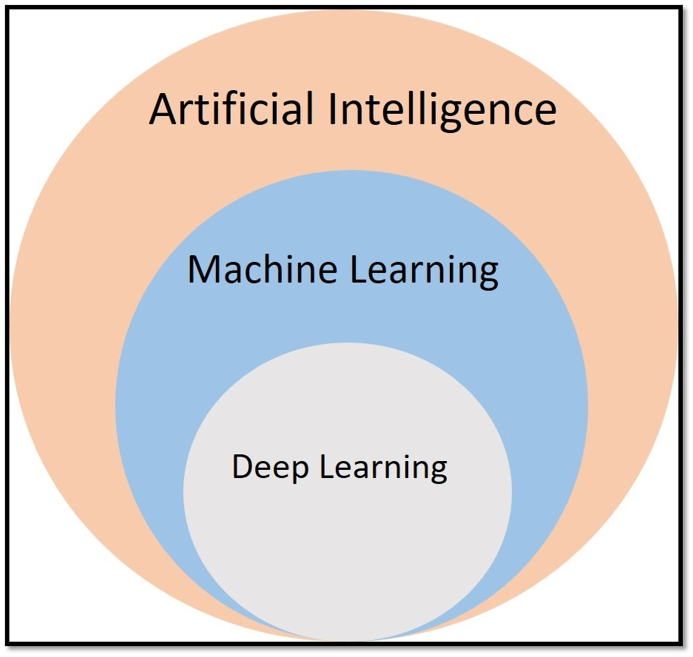
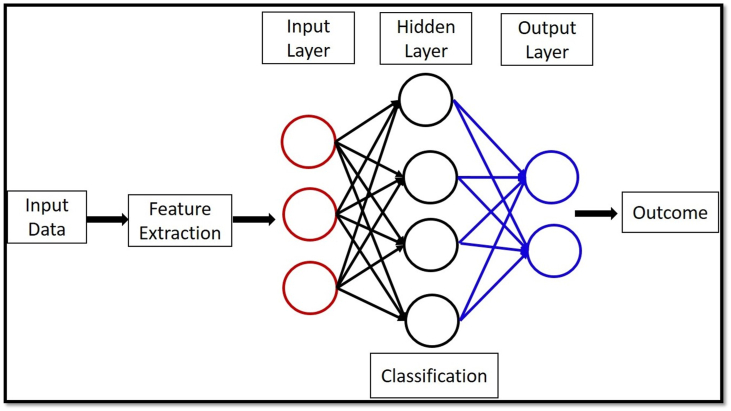
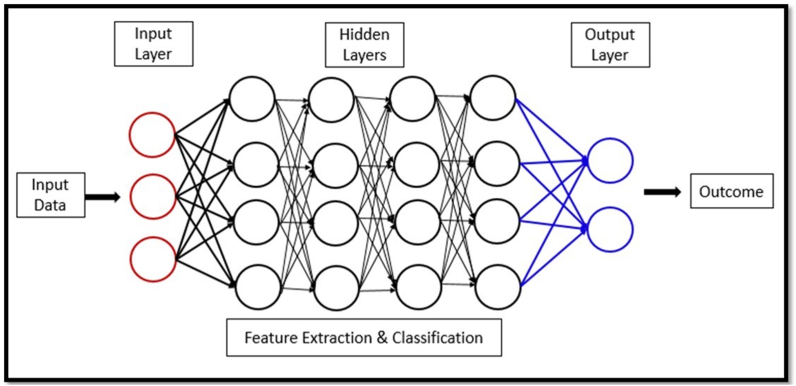
At the beginning, it is pertinent to understand the fundamental principles and key concepts of AI before deliberating on the relevance of AI in radiology. Broadly speaking, AI encompasses two main subfields: (a) traditional ML and (b) human brain-inspired deep learning (DL) (Fig. 1).12 In simple terms, ML means the ability of computers to learn without being explicitly programmed. ML involves the application of an algorithm to a set of data that is already trained by human intervention through data manipulation to make a prediction.12 ML algorithms work on the set of available inputs for desirable outputs (Fig. 2). In radiology, image data form the common input. Performance of ML improves with experience. ML can be supervised or unsupervised depending on whether the input data are labeled/organized or not. A third category namely reinforcement learning is also described where learning is based on repeated trial and error.9 DL, on the other hand, is a sophisticated and mathematically complex outgrowth of ML where there is minimal human intervention. DL systems consist of multiple hidden layers configured structurally as well as functionally much like the neural networks of human brain (Fig. 3). By virtue of multiple layers of artificial neural network (ANN), DL systems are independently capable of extracting relevant features from the given data and producing high-value output.9 There are various types of ANN available today. Convolutional neural network (CNN) is the mostly widely used ANN in radiology practice. Further details of structure and functioning of AI are beyond the scope of the paper.
Fig. 1.
Basic components of artificial intelligence (AI) (modified from Nair et al. Ref 12).
Fig. 2.
Outline of machine learning (ML) (modified from Nair et al. Ref 12).
Fig. 3.
Outline of deep learning (DL) (modified from Nair et al. Ref 12).
Human eyes can detect, extract, and analyze only a small portion of the total information available in the digital images, especially when the number of images and data volume is high. In radiology, ML has been in use for more than two decades. Examples are image-based approach like automatic calculation of coronary artery calcium score, computer-aided diagnosis (CAD) of breast lesions, and microcalcifications in mammography. Such image-based ML help extracting specific features of lesions, image segmentation, and classify them for decision-making.13 Advances in ML and DL algorithms have enabled greater rates of lung nodule detection and characterization. CNNs are usually able to comment on the presence or absence of disease and also extract relevant data from previous studies for a meaningful comparative reporting by the radiologist. Computer vision is a sub-field of AI that has the ability to derive meaningful information from digital images much like the human eye and brain.13
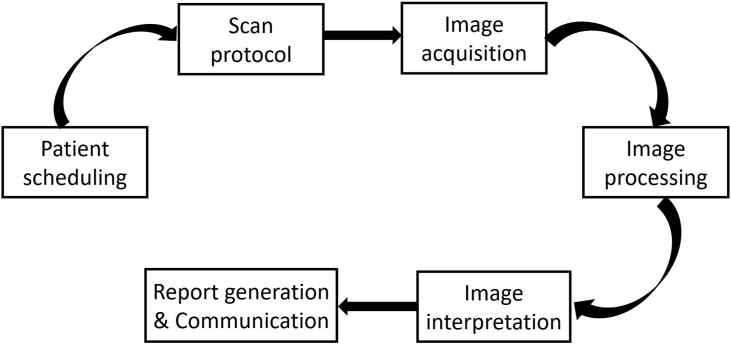
Today, AI has an established role in emergency radiology14 in the detection and diagnosis of (a) stroke and large vessel occlusion, (b) intracranial hemorrhage, (c) spine/bony injury, (d) pneumothorax, (e) pulmonary thromboembolism, (f) pneumoperitoneum, (g) intra-abdominal bleed, etc. Besides image interpretation (lesion detection, characterization, response to treatment, automated follow-up, etc), many AI algorithms are already in use or have potential use for various non-interpretive tasks in day-to-day radiology workflow which includes but not limited to (a) patient scheduling (suitable resource allocation), (b) selecting right scan protocol, (c) image acquisition (optimization of image quality, radiation dose, image noise, contrast dose, reduced scanning time, etc), (d) image processing (post-processing, quantitative analysis, automated anatomic labeling, hanging protocols, etc), (e) report generation and communication with clinicians and patients (natural language processing, computer-assisted structured reporting, follow-up recommendations, etc) (Fig. 4).10,11,14,15 Multiple studies have shown that AI has the capability to triage and direct radiologists/clinicians attention to life-threatening conditions, improve consistency of performance, reduce intra or inter observer variability, and help creating standardized reporting workflow among many others. AI can be of great help in linking various imaging and laboratory reports of patients which is an essential routine but time-consuming process for the radiologist.
Fig. 4.
Role of AI in radiology workflow management.
Although AI has many established and many more prospective applications in radiology, the widespread utility of AI in day-to-day clinical radiology practice is rather limited at this time. There are multiple barriers to the effective development and successful implementation of AI in routine radiology practice as summarized below: (a) development of AI in radiology needs huge amount of authentic and validated training data covering the normal and broad spectrum of abnormal anatomy in various disease processes. Procuring, labeling, and training AI with such amount of data with the requisite quality is an extremely tedious task. Currently, most training data are obtained from limited number of institutions with the resultant lack of generalizability of such data and accuracy of results therefrom. (b) Validation of AI algorithm outputs in diverse clinical/radiological scenario by subject experts is another challenging task and is a major hindrance for the widespread acceptance and application of AI as on date. (c) Most current AI applications are narrow/weak, that is, they are good at performing a specific task for which they are trained but are not appropriate for other tasks as humans can perform. Besides, currently available AI applications are not fully capable of performing subjective associations as is commonly done by an expert radiologist. (d) Lack of transparency and trustworthiness: most radiologists are not aware about how a particular AI algorithm works. Also, there is the perception among the medical fraternity that AI algorithms are unable to give more accurate diagnosis than a radiologist. If a radiologist over-relies on AI for clinical decision-making, there will be a distinct possibility of “automation bias.” Besides, there is fear that any error that occurs during the training of AI-related data may get propagated and potentially magnified during real-life applications. (e) Lack of robust clinical proof about the effectiveness of AI algorithms in real-life scenario. (f) Misc issues: (i) Ethical issues and regulatory compliance; (ii) Data ownership, privacy, and intellectual property rights; (iii) Cyber security and data protection; (iv) Conflicts of interest; (v) Need for integration into radiology practice by multiple stakeholders for multiple imaging modalities.12,13
Conclusion
AI has traveled a long way and has been constantly evolving. AI is a reality in clinical radiology today and is going to stay with us. Radiology workflow in day-to-day practice will be immensely benefitted from the newer-generation AI applications. AI tools will help radiologists to reduce time spent on essential but repetitive non-interpretive tasks and thereby enable them to spend more time for higher cognitive tasks of accurate interpretation and diagnosis which is the most important aspect of radiology practice. Current limitations and impediments of widespread implementation of AI in radiology need to be addressed by all stakeholders in the near future. Radiologists need to embrace AI with a clear understanding of pros and cons and use optimally to benefit radiology fraternity as well as patients in general. AI should be used as a “decision support tool” and not a “decision-maker.” As on date, it is going to be “AI-augmented radiology” rather than “AI replacing radiologists.”
Disclosure of competing interest
The author has none to declare.
References
- 1.Bruls R.J.M., Kwee R.M. Workload for radiologists during on-call hours: dramatic increase in the past 15 years. Insights Imaging. 2020;11:121. doi: 10.1186/s13244-020-00925-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dan Lantsman C., Barash Y., Klang E., Guranda L., Konen E., Tau N. Trend in radiologist workload compared to number of admissions in the emergency department. Eur J Radiol. 2022;149 doi: 10.1016/j.ejrad.2022.110195. [DOI] [PubMed] [Google Scholar]
- 3.Winder M., Owczarek A.J., Chudek J., Pilch-Kowalczyk J., Baron J. Are we overdoing it? Changes in diagnostic imaging workload during the years 2010-2020 including the impact of the SARS-CoV-2 pandemic. Healthcare (Basel) 2021;9(11):1557. doi: 10.3390/healthcare9111557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor-Phillips S., Stinton C. Fatigue in radiology: a fertile area for future research. Br J Radiol. 2019;92(1099) doi: 10.1259/bjr.20190043. Epub 2019 May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stec N., Arje D., Moody A.R., Krupinski E.A., Tyrrell P.N. A systematic review of fatigue in radiology: is it a problem? Am J Roentgenol. 2018;210:799–806. doi: 10.2214/AJR.17.18613. [DOI] [PubMed] [Google Scholar]
- 6.Busby L.P., Courtier J.L., Glastonbury C.M. Bias in radiology: the how and why of misses and misinterpretations. Radiographics. 2018;38(1):236–247. doi: 10.1148/rg.2018170107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Itri J.N., Tappouni R.R., McEachern R.O., Pesch A.J., Patel S.H. Fundamentals of diagnostic error in imaging. Radiographics. 2018;38(6):1845–1865. doi: 10.1148/rg.2018180021. [DOI] [PubMed] [Google Scholar]
- 8.Pinto A., Brunese L. Spectrum of diagnostic errors in radiology. World J Radiol. 2010;2(10):377–383. doi: 10.4329/wjr.v2.i10.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pérez Del Barrio A., Menéndez Fernández-Miranda P., Sanz Bellón P., Lloret Iglesias L., Rodríguez González D. Artificial Intelligence in Radiology: an introduction to the most important concepts. Radiologia (Engl Ed). 2022;64(3):228–236. doi: 10.1016/j.rxeng.2022.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Richardson M.L., Garwood E.R., Lee Y., et al. Noninterpretive uses of artificial intelligence in radiology. Acad Radiol. 2021;28(9):1225–1235. doi: 10.1016/j.acra.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Ranschaert E., Topff L., Pianykh O. Optimization of radiology workflow with artificial intelligence. Radiol Clin North Am. 2021;59(6):955–966. doi: 10.1016/j.rcl.2021.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Nair A.V., Ramanathan S., Sathiadoss P., Jajodia A., Blair Macdonald D. Barriers to artificial intelligence implementation in radiology practice: what the radiologist needs to know. Radiologia (Engl Ed). 2022;64(4):324–332. doi: 10.1016/j.rxeng.2022.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Martín Noguerol T., Paulano-Godino F., Martín-Valdivia M.T., Menias C.O., Luna A. Strengths, weaknesses, opportunities, and threats analysis of artificial intelligence and machine learning applications in radiology. J Am Coll Radiol. 2019;16(9 Pt B):1239–1247. doi: 10.1016/j.jacr.2019.05.047. [DOI] [PubMed] [Google Scholar]
- 14.Al-Dasuqi K., Johnson M.H., Cavallo J.J. Use of artificial intelligence in emergency radiology: an overview of current applications, challenges, and opportunities. Clin Imag. 2022;89:61–67. doi: 10.1016/j.clinimag.2022.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Kapoor N., Lacson R., Khorasani R. Workflow applications of artificial intelligence in radiology and an overview of available tools. J Am Coll Radiol. 2020;17(11):1363–1370. doi: 10.1016/j.jacr.2020.08.016. [DOI] [PubMed] [Google Scholar]