Abstract
Background
Health evidence needs to be communicated and disseminated in a manner that is clearly understood by decision-makers. As an inherent component of health knowledge translation, communicating results of scientific studies, effects of interventions and health risk estimates, in addition to understanding key concepts of clinical epidemiology and interpreting evidence, represent a set of essential instruments to reduce the gap between science and practice. The advancement of digital and social media has reshaped the concept of health communication, introducing new, direct and powerful communication platforms and gateways between researchers and the public. The objective of this scoping review was to identify strategies for communicating scientific evidence in healthcare to managers and/or population.
Methods
We searched Cochrane Library, Embase®, MEDLINE® and other six electronic databases, in addition to grey literature, relevant websites from related organizations for studies, documents or reports published from 2000, addressing any strategy for communicating scientific evidence on healthcare to managers and/or population.
Results
Our search identified 24 598 unique records, of which 80 met the inclusion criteria and addressed 78 strategies. Most strategies focused on risk and benefit communication in health, were presented by textual format and had been implemented and somehow evaluated. Among the strategies evaluated and appearing to yield some benefit are (i) risk/benefit communication: natural frequencies instead of percentages, absolute risk instead relative risk and number needed to treat, numerical instead nominal communication, mortality instead survival; negative or loss content appear to be more effective than positive or gain content; (ii) evidence synthesis: plain languages summaries to communicate the results of Cochrane reviews to the community were perceived as more reliable, easier to find and understand, and better to support decisions than the original summaries; (iii) teaching/learning: the Informed Health Choices resources seem to be effective for improving critical thinking skills.
Conclusion
Our findings contribute to both the knowledge translation process by identifying communication strategies with potential for immediate implementation and to future research by recognizing the need to evaluate the clinical and social impact of other strategies to support evidence-informed policies.
Trial registration protocol is prospectively available in MedArxiv (doi.org/10.1101/2021.11.04.21265922).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12961-023-01017-2.
Keywords: Knowledge translation, Scientific communication, Evidence-based informed policy
Contributions to the literature
Communicating results of scientific studies, effects of interventions and health risk estimates, in addition to understanding key concepts of clinical epidemiology and interpreting evidence, account for a set of essential instruments to bridging the gap between science and practice.
There is still a lack of understanding about the exact types of strategies for communicating scientific evidence.
The findings of this manuscript, specifically the extensive and detailed list of strategies mapped out to communicate scientific evidence in health to managers and the population, may support the decision-making of stakeholders involved in the process of knowledge translation within the realms of evidence-informed policies.
Introduction
Within the context of evidence-informed policy (EIP), evidence syntheses should provide scientifically based information on health conditions, interventions, procedures, policies and programmes to meet the needs of health professionals, patients and public or private health managers. However, evidence obtained from scientific studies, especially from systematic reviews, other syntheses of multiple studies and clinical trials, is complex and often difficult for the general public to comprehend [1]. Health evidence needs to be communicated and disseminated in a manner that is clearly understood by decision-makers, especially in settings that demand rapid responses.
As an inherent component of health knowledge translation, communicating results of scientific studies, effects of interventions and health risk estimates, in addition to understanding key concepts of clinical epidemiology and interpreting evidence, represent a set of essential instruments to reduce the gap between science and practice. These needs have represented a challenge within the EIP worldwide.
Strategies for communication of evidence in health have the initial goal of increasing the understanding of the results of scientific research and should cover products, actions and approaches aligned to the needs of the manager (facing the demands for healthcare services) and the population (reliable information based on the best scientific evidence available) [2]. Nevertheless, the ultimate expected outcome of any effective communication, addressed to specific audiences, would be its clinical benefit (when considering individual health) and/or positive impact on health systems and organizations (when considering public health).
In this sense, expanding investment and improving skills in communication enables the identification of the best strategies to be used to overcome the barrier between evidence in health and managers and the population. Clear communication and active dissemination of health evidence to all relevant audiences in an understandable and accessible manner are essential to raise awareness of the importance of using scientific evidence, to support individual and population health-related decisions [1], and contribute to adherence to behaviours associated with positive health outcomes.
In the last decade, the advancement of digital and social media has reshaped the concept of health communication, introducing new, direct and powerful communication platforms and gateways between researchers and the public [2–4]. Various strategies such as plain language summaries and infographics have been devised and experimented for this purpose.
Some synthesis of strategies for communication of scientific evidence are available in the literature, including overviews of systematic reviews that address knowledge translation and general health communication strategies (for the population, health professionals and managers) [2, 5], systematic reviews restricted to communicating health benefits/risks [6–8] or teaching/learning strategies [9], narrative reviews [10, 11] and scoping reviews focused on communicating uncertainties [12]. No in-depth scoping review was identified with the objective of identify strategies for communicating scientific evidence on healthcare to managers and the population.
Thus, a mapping is necessary, through a scoping review, to identify the available strategies for communication of scientific evidence; the characteristics, barriers and facilitators for its implementation; the target audience and the context, as well as the gaps in the literature about its impact on healthcare. The results identified may constitute a valuable instrument for decision-making for sectors involved in promoting the use of scientific knowledge in decision-making processes related to the communication of evidence in the context of EIP.
Methods
Design and setting
This scoping review is a component of the project Apoio à Formulação e Implementação de Políticas Públicas de Saúde Informadas por Evidências (ESPIE), triennium 2021/2023, conducted at the Hospital Sírio-Libanês (São Paulo, Brazil), within the scope of the Programa de Apoio ao Desenvolvimento Institucional do Sistema Único de Saúde (PROADI-SUS), in partnership with the Department of Science and Technology of the Secretariat of Science, Technology, Innovation and Strategic Inputs of the Ministry of Health. This review was planned and conducted according to the recommendations of the Joanna Briggs Institute Manual for scoping reviews [13].
The report of the review followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses – extension for scoping reviews (PRISMA-ScR) [14]. The review protocol was planned and prospectively made available in the MedRxiv pre-prints database. [15]
Methods for engaging the community and other stakeholders in the review
Stakeholder consultation was carried out throughout the development of the protocol, with the aim of increasing the applicability of its results and supporting the communication and translation of its results to the community. To this end, the following stakeholders were informally consulted: consumers (managers, health professionals and patients), experts in ‘knowledge translation’ and ‘health communication’ and information specialists.
Criteria for inclusion of studies
The question of interest for this review was structured using the acronym PCC, which then guided the eligibility criteria as follows:
P (population, condition): health managers and the general population.
C (concept): strategies for communicating scientific evidence to health managers and/or the community. In this review, scientific evidence was considered as information obtained from the results of scientific studies and used to support or refute a health recommendation or the planning of health systems and policies. Thus, strategies were considered as those aiming to translate scientific and/or methodological information in a format/content geared to ensure the understanding of health managers and society of terms, criteria, tools and approaches related to scientific evidence in health. Any strategy focused on the communication of scientific evidence for this target audience was considered, including, for example, communication strategies to support health managers in decision-making, communications used during the organization of services and/or health systems, communication strategies to encourage the use of scientific evidence in the decision-making process, to increase access to health information from the perspective of the population, strategies for adapting the knowledge obtained by evidence to the local context, and so on. Studies on individual professional–patient communication (including diagnosis, communication of bad news and specific recommendations on individual therapy or prevention, among others) or specific to a particular health condition were not considered. Studies addressing the process of knowledge translation were included only when they reported, implemented and/or evaluated strategies for communication of scientific evidence as part of this process. Studies specifically addressing evidence dissemination and implementation strategies were not included.
C (context): individual or public health; within public, private or supplementary health systems; at any level of care (health unit, neighbourhood, municipality, state, region or country).
Any primary (descriptive or analytical) or secondary study design was considered.
Searching for studies
A broad and sensitive literature search was conducted using structured search strategies, with relevant descriptors and synonyms, for the following databases on 8 September 2021: Campbell Collaboration, Cochrane Library (via Wiley), Excerpta Medica dataBASE (Embase, via Elsevier), Biblioteca Virtual em Saúde (BVS), Epistemonikos, Health Evidence, Health Systems Evidence, Medical Literature Analysis and Retrieval System Online (MEDLINE, via PubMed) and PDQ-Evidence. A structured electronic search was conducted in the following grey literature bases on 24 February 2022: Opengrey (https://opengrey.eu), Thesis Commons (https://thesiscommons.org/) and Open Access Theses and Dissertations (https://oatd.org/).
Structured electronic searches were conducted on the following repositories of preprints on 24 February 2022: Europe PMC (https://europepmc.org/) and Open Science Preprints (https://osf.io/preprints/).
Additional unstructured searches were conducted on the following sources related to evidence-informed policy or health education on 27 February 2022: Agency for Healthcare Research and Quality AHRQ/EUA, Guidelines and Measures (www.guidelines.gov), Centre for Reviews and Dissemination (CRD), Service Delivery and Organisation (https://www.york.ac.uk/crd/research/service-delivery/), Cochrane Effective Practice and Organization of Care (EPOC) (https://epoc.cochrane.org/), EPPI-Centre (https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=56), Evidence Informed Policy and Practice in Education in Europe (EIPPEE) (http://www.eippee.eu/cms/Default.aspx?tabid=3179), European Observatory on Health Systems and Policies (https://eurohealthobservatory.who.int/), ECRAN Project. European Communication on Research Awareness Needs (http://www.ecranproject.eu/en), Evidence Informed Policy Networks (EVIPNet) (https://www.who.int/initiatives/evidence-informed-policy-network), Global Evaluation Initiative (https://www.globalevaluationinitiative.org/), Informed Health Choices (https://www.informedhealthchoices.org/), International Bibliography of the Social Sciences (IBSS) (https://about.proquest.com/en/products-services/ibss-set-c/), International Initiative for Impact Evaluation (3ie) (https://www.3ieimpact.org/), McMaster University's Health Forum (https://www.mcmasterforum.org/), Rx for Change (https://www.cadth.ca/rx-change), Supporting the use of Research Evidence (SURE) (https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/SURE-Guides-v2.1/Collectedfiles/sure_guides.html, The Alliance for Health Policy and Systems Research (https://ahpsr.who.int/) and What Works Centres (https://www.gov.uk/guidance/what-works-network).
Additional unstructured searches were conducted on the following sources related to health science communication on 24 February 2022: American Medical Writers Association (AMWA, https://www.amwa.org/), European Medical Writers Association (EMWA, https://www.emwa.org/) and International Society for Medical Publication Professionals (ISMPP, https://www.ismpp.org/). A manual search was performed in reference lists of relevant studies and through contact with experts in the field.
No language filter was applied. The search was restricted to the period from the year 2000 onwards, considering the advances and changes in the digital and social media that have occurred mainly in the last two decades. Full-length publications, abstracts presented at conferences and events, online reports, theses and dissertations were included. The structured search strategies are presented in Additional file 1.
Selecting studies
The study selection process was carried out in two phases using the Rayyan platform [16]. The first phase consisted of reading the titles and abstracts of all references retrieved by the search strategies and categorizing the studies into ‘potentially eligible’ or ‘eliminated’. The second phase consisted of reading in full the ‘potentially eligible’ studies to confirm their eligibility or exclude them in the second phase (the justifications for each exclusion in the second phase are presented). The two phases were conducted by two groups of independent researchers and inconsistencies in decisions to include or exclude studies were solved by a third researcher. The entire selection process is presented using a PRISMA flowchart.
Extracting data
Data on the of strategies identified and included in this review were extracted by two researchers independently and inconsistencies were solved by consulting a third researcher. The following data were collected for each included study: author, year of publication, type of publication (article/report, full text/ abstract), study design, name and description of the communication strategy, institution proposing the strategy and source of funding for the study. The following data were collected, when available, for each strategy identified:
Strategy main category and subcategories:
communication of risk/benefit: including the subcategories communication of health risks and benefits under different numerical or nominal formats, health communication with positive (benefits, gains) or negative (losses) words/terms, verbal versus visual communication of the effects of interventions, communicating health risks and benefits with bar charts or bar charts and histograms, strategies for communication of health evidence and strategies for communicating risks and benefits in health with different animated graphical presentations.
communication of uncertainty in health: including the subcategory communication of uncertainties about the effects of interventions on health.
teaching/learning: including the subcategories communication/learning of key concepts related to the effects of health interventions, communication/learning resources from the IHC initiative on key concepts of evidence for health, communication/learning of key concepts of health evidence, educational podcasts from the IHC initiative on key health evidence concepts, training for parliamentarians on scientific health evidence and inclusion of stakeholders in the working group for preparing comparative effectiveness summaries.
evidence synthesis frameworks using plain language: including the subcategories blogshots to communicate the results of systematic reviews, evidence synthesis summary template, plain language abstract, Cochrane plain language summaries, templates for plain language abstracts of systematic reviews, printed newsletters for communicating health evidence and systematic review summaries of evidence templates for policy-makers and health system managers.
guidelines for elaborating/evaluating communication products: including the subcategories guidelines for designing and evaluating health evidence communication products (CDC Clear Communication Index) and tool for evaluating the quality of health texts in plain language.
For this categorization, a new taxonomy was elaborated with an unstructured method, which is detailed in Additional file 2.
Target audience: health managers, population, both.
Type of strategy: language, content or format of the communication.
Health system and level of care for which the strategy was proposed or used (public or private health, primary or specialized care; others).
Approach to the strategy: textual communication (printed/online material), visual communication (graphic, illustrative with drawings), verbal communication (videos, podcasts) and others.
Strategy length: permanent or temporary.
Strategy status: proposed, implemented and not evaluated, or implemented and evaluated.
Costs for implementing the strategy (as predicted by the authors of the studies included).
Barriers and facilitators for implementing the strategy (as identified by the authors of the studies included).
For the scientific evidence communication strategies that were implemented and evaluated by the included studies, information on the results was collected. These strategies were subsequently classified, at the discretion of the reviewing authors, according to the feasibility of implementation, immediate or after the adoption of actions. This classification was performed considering facilities, costs, need for regulation or local policies, and regardless of the certainty of the available evidence.
The authors of the included studies could be contacted if additional information was needed.
Quality assessment/risk of bias of the included studies
As the aim of this scoping review is to map strategies presented in descriptive studies or to use pieces of analytical studies reporting strategies, no checklists or tools for assessing the methodological quality of the studies were applied, as recommended by the Joanna Briggs Institute for scoping reviews [13].
Synthesis and presentation of results
Strategies were classified using the categories determined based on the data described above. A narrative synthesis was presented using graphs and/or tables. Depending on the availability of information, descriptive statistics would be performed using Microsoft Excel® and/or STATA® software, but this was not undertaken due to the format and/or scarcity of the data presented.
Results
Search results
Structured searches in electronic databases resulted in 25 284 references and unstructured searches in additional sources retrieved 58 references, totaling 25 342 references. After removing 744 duplicates, 24 598 references were analyzed through titles and abstracts and 24 467 were eliminated for not meeting the eligibility criteria. Thus, in the second stage of the selection process, the full texts of 131 references were analyzed. Of these, 50 were excluded [17–66] and the reasons for exclusion are detailed in Additional file 3. One reference awaits classification because, despite a series of attempts, it was not possible to obtain the full paper and the abstract did not present enough information to allow confirmation of its eligibility [67].
At the end of the selection process, this review included 80 studies or documents (Fig. 1) [1, 2, 6–12, 68–138].
Fig. 1.
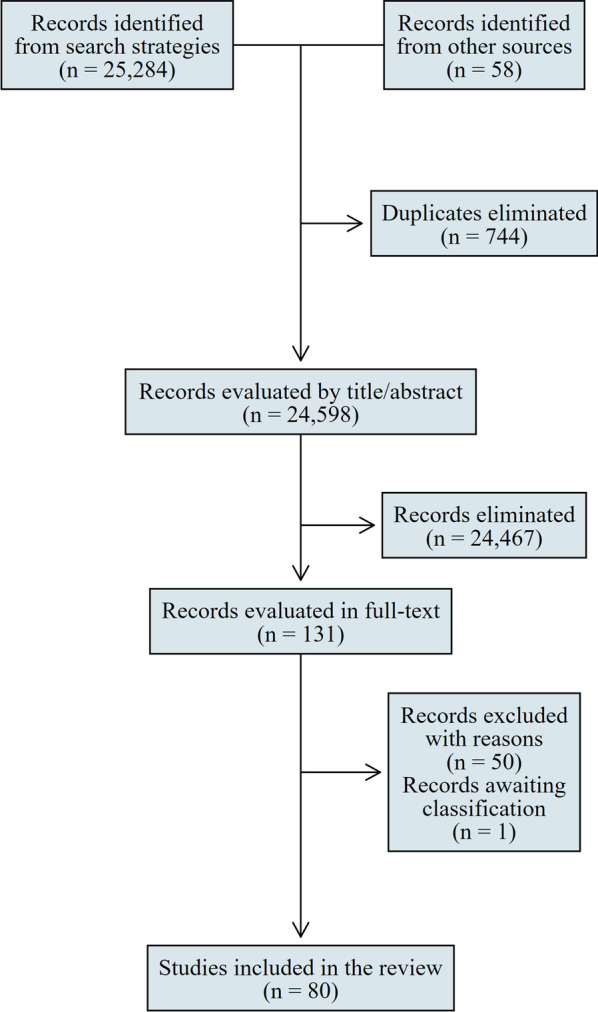
Flowchart of the study selection process
Characteristics of the included studies
The main characteristics of the included studies/documents are detailed in Additional file 4. Studies with a descriptive design were the most frequent (28.8%), followed by systematic reviews (16.3%) and case studies (13.8%). The studies were funded by governmental institutions or non-governmental initiatives, in the areas of health (research and assistance) and education.
Results of included studies
Seventy-eight strategies were identified in the included studies and are presented in Additional file 5. All of the studies had the ultimate or intermediate goal of improving the comprehension of health information. None of these strategies were proposed for a specific health system or level of healthcare, and they were implemented in different scenarios (including school settings) and on a continual basis. The costs associated with the strategies were not provided by any of the studies.
Table 1 presents the main results of the strategies for communicating scientific evidence that were implemented and, to some extent, evaluated, regardless of the method used to evaluate such results (experimental study, survey, and so on).
Table 1.
Main results of the strategies for communicating scientific evidence that were implemented and evaluated
| Communication of risk/benefit on health | |
|---|---|
| Subcategory | Main results |
| Communication of health risks and benefits under different numerical or nominal formats |
[Akl, 2011b] [7] This systematic review included 35 studies comparing the communication of health risks and benefits by natural frequency, percentages, relative risk reduction (RRR), absolute risk reduction (ARR) or number needed to treat (NNT). The main results are as follows Natural frequencies versus percentages: • comprehension: greater with natural frequencies than percentages (SMD 0.69; 95% CI 0.45–0.93; 642 participants; 7 comparisons; moderate-certainty evidence) RRR versus ARR: • comprehension: little or no difference between presentation formats (SMD 0.02; 95% CI −0.39 to 0.43; I [2] = 80%; 2 studies; moderate certainty evidence) • persuasiveness: greater with RRR (SMD 0.62; 95% CI 0.42–0.83; 15 studies; moderate-certainty evidence) RRR versus NNT: • comprehension: greater with RRR (SMD 0.73; 95% CI 0.43–1.04; 1 study; evidence certainty not evaluated) • persuasiveness: greater with RRR (SMD 0.65; 95% CI 0.51–0.80; 10 studies; moderate-certainty evidence) ARR versus NNT: • comprehension: greater with ARR (SMD 0.42; 95% CI 0.12–0.71; 1 study; moderate-certainty evidence) • persuasiveness: little or no difference between presentation formats (SMD 0.05; 95% CI −0.04 to 0.14; 10 studies; moderate-certainty evidence) |
|
[Büchter, 2014] [8] This systematic review included ten studies, and the main results (measured by a six-point Likert scale, suggesting small to moderate effects) were: • nominal presentation resulted in an overestimation of event risk • numerical presentation resulted in more accurate estimates, increased satisfaction with the information (MD 0.48; 95% CI 0.32–0.63; p < 0.00001; I [2] = 0%) and the probability of medication use | |
|
[Chapman, 2020] [2] This overview included 44 systematic reviews on strategies for health knowledge dissemination, including strategies for communicating health risks and benefits. The main results with sufficient evidence to be implemented were: Natural frequencies versus percentages: • comprehension (about outcomes of health intervention effects): greater with the use of natural frequencies than percentages RRR versus ARR: • comprehension: no difference between the formats • persuasiveness: higher with RRR RRR versus NNT: • comprehension: higher with RRR • persuasiveness: higher with RRR ARR versus NNT: • comprehension: higher with ARR • persuasiveness: little or no difference between the formats Numerical versus nominal (textual, printed) communication: • satisfaction: for reporting adverse event risk in printed materials, satisfaction was significantly higher with numerical communication | |
|
[Fortin, 2001] [85] This survey collected the opinion of 15 women about different ways of presenting risks related to hormone replacement therapy. The main results were: • 83% of the participants preferred bar to line graphs, survival curves and visual scales with facial expressions; • mortality estimates were preferred over 10 or 20 year survival • there was a preference for absolute risks over relative risks and NNT | |
|
[Ghosh, 2005] [88] This narrative review presented the following results about strategies for communication of risk for the population: • there was a preference for ARR over NNT • the ability to interpret graphs was limited • for the population aged 75 years and over, there was a preference for graphs over percentages | |
|
[Knapp, 2004] [96] This randomized controlled trial (RCT) included 120 participants taking simvastatin or atorvastatin after cardiac surgery or heart attack: 60 received a text communicating the risk of adverse events (constipation or pancreatitis) in nominal format, and 60 received the same text but with numerical reporting of the risks (for constipation, ‘common’ or 2.5%; for pancreatitis, ‘rare’ or 0.04%). The main results were: • estimated mean probability of constipation: 34.2% in the nominal communication group and 8.1% in the numerical communication group; for pancreatitis: 18% in the nominal communication group and 2.1% in the numerical communication group • nominal communication was associated with more negative perceptions of medications than equivalent numerical communication • nominal risk communication overrides the harm level and could lead patients to make inappropriate decisions about whether to use the medication | |
|
[Kristiansen, 2012] [98] This survey interviewed participants (general population) who were communicated about the risk of heart attack with the use of a hypothetical medication using the NNT. The results showed that: • the NNT did not communicate information about the proportion of patients who benefited from an intervention or the extent to which an adverse event was being prevented • 80% of participants agreed with the benefit of the medication, regardless of NNT • some people who disagreed with the benefit of the medication misinterpreted the NNT • the population may have difficulty understanding the meaning of NNT, and its use should be avoided for this target audience | |
|
[Lipkus, 2007] [100] The main results of this narrative review are presented below: Numerical risk communication: • people generally preferred numerical information over other formats (for example, nominal categories for probability: unlikely or very likely) • among numerical formats, natural frequencies were easier to understand • being consistent with using numerical formats, for example, not comparing percentages with probabilities or frequencies, facilitated understanding • using the same numerical denominator (for example, comparing 5 out of 100 with 15 out of 100) facilitated comparisons and reduced cognitive effort • in general, individuals more easily understood base-10 denominators (for example, 10, 100, 1000) • rounding numbers and avoiding decimals made it easier to comprehend (for example, it was easier to comprehend 30 than 29.6) • expressing a ratio as small numbers (for example, 1 in 10) led to fewer perceptions of the probability of events than the same ratio incorporating larger numbers (for example, 10 in 100) • specifying the relative risk and including the absolute risk were more comprehensive (for example, the risk of non-smokers getting the disease is 1%, while the risk of smokers is 10%, so smokers have a ten times higher risk of getting the disease than non-smokers) Nominal risk communication: • when nominal risk communication was the chosen format, using the main term and its variations added some objectivity and allowed comparisons (for example: likely, unlikely, very likely) Visual risk communication: • bar charts (histograms) were best suited for making comparisons, especially for subgroups (for example, comparing the magnitude of risk by ethnic group or sex) • line graphs (survival curves) were best suited to show trends over time and perhaps interactions between risk factors | |
|
[McCormack, 2013] [1] This systematic review included 61 studies about communication strategies. The main results are presented below Communication about benefits – effectiveness: • people who received non-numerical or factual communication about medication with a higher probability of benefit for myocardial infarction chose this medication more often than people who did not receive this communication (one study, low strength of evidence) • receiving additional non-numerical information about benefits had little effect on refusals of cancer screening tests, but receiving non-numerical information about harms significantly increased refusals to screening tests and significantly decreased satisfaction with the decision (one study, low strength of evidence) Communication about precision/imprecision: • risk communication with numerical point estimates versus reporting with 95% CI: studies showed varying results depending on the outcome, the range of the 95% CI and the presence or absence of comparative information on the population mean risk • numerical versus graphical communication of 95% CI regarding risk perception: uncertainty evidence (one study, insufficient strength of evidence) Communication about direct evidence: • choosing a cholesterol medication for which there was direct evidence of benefit was more frequent among people who received non-numerical communication or factual information with direct evidence encouraging the choice of the medication than those who did not receive this communication (one study, insufficient strength of evidence) | |
|
[Sheridan, 2003] [128] This RCT included 407 participants who were randomized to receive one of four formats of risk communication about the comparative effects of two medications: RRR (n = 97), ARR (n = 108), NNT (n = 100) or a combination of all three formats (n = 98). The main results were: • comprehension of the comparative effectiveness: higher in the RRR group (60% with RRR, 42% with ARR, 30% with NNT and 43% with the combination group; p = 0.001) • ability to calculate treatment effect from baseline disease risk: higher in the RRR group (21% with RRR, 17% with ARR, 6% with NNT and 7% with the combination; p = 0.004) • response on the effect calculation: 26% with RRR, 32% with ARR, 39% with NNT and 42% with the combination • greater difficulty with comparisons and estimates was observed in the subgroups of non-white, with some college education, females, persons with health problems or who had not previously discussed quantitative data with their physicians | |
|
[Trevena, 2006] [130] This systematic review included 10 systematic reviews of RCTs and 30 additional RCTs. The main results were: • more modern communication strategies (verbal, textual, visual and electronic offered by the provider) increased patient comprehension but were more likely to do so if they were structured, adapted and/or interactive • probabilistic information was best communicated as event rates (natural frequency) rather than nominal terms (for example, much, little) and measures of effect size (such as relative risk reduction) • figures such as cartoons or graphs (for example, vertical bar graphs) aided comprehension • value clarification exercises helped in individual decision-making | |
| Health communication with positive (benefits, gains) or negative (losses) words/terms |
[Akl, 2011a] [6] This systematic review included 35 studies (16 342 participants from the general population) that compared communication of health attributes or effects of health interventions/exposures with positive (benefits, gains) or negative (losses) words/terms. The main results are below For communicating attributes: • comprehension (Likert scale): higher with negative words/terms; SMD −0.51; 95% CI −0.94 to −0, 22; 1 study; moderate effect size; low-certainty evidence • persuasiveness (measured as a hypothetical decision or intention or willingness to adopt an intervention, Likert scale): little or no difference with positive or negative words/terms; SMD 0.07; 95% CI −0.23 to 0.37; 11 studies; low-certainty evidence • behaviour (Likert scale): little or no difference with positive or negative words/terms; SMD 0.09; 95% CI −0.14 to 0.31; 1 study; moderate-certainty evidence For communicating the effects of interventions/exposition: • comprehension: no study evaluated the effect of communication as losses or gains on comprehension • persuasiveness (measured as a hypothetical decision or intention or willingness to adopt an intervention, Likert scale): for communication about treatment effects, persuasiveness was higher with words/terms signifying losses (SMD −0.50; 95% CI −1.04 to 0.04; 3 studies; moderate effect size; very low-certainty evidence) • behaviour (Likert scale): little or no difference with words/terms meaning gains or losses; SMD −0.06; 95% CI −0.15 to 0.03; 16 studies; low-certainty evidence |
|
[Edwards, 2001] [82] This narrative review concluded that there is a greater comprehension with the use of words/terms meaning losses versus words/terms meaning gains when communicating health risks and benefits (OR 1.18, 95% CI 1.01–1.38) | |
|
[Gallagher, 2013] [37] This systematic review included 94 studies comparing the communication of health outcome results with words/terms meaning gains or losses. In total, 189 measures of effect size were evaluated, and the main results were: • behaviour: reporting the results of effect size measures as gains was more effective for encouraging desirable behaviour than reporting the results as losses (p = 0.002), particularly for skin cancer prevention, smoking cessation and physical activity | |
|
[McCormack, 2013] [1] This systematic review included 61 studies on health communication strategies, and the main results on positive (benefits, gains) or negative terms were: • loss content communications associated with dichotomous (yes/no) narratives were more persuasive than (i) loss content communications associated with statistical information or (ii) gain content communications associated with narratives or statistical information (one study; insufficient strength of evidence) | |
| Verbal versus visual communication of the effects of interventions |
[Lopez, 2008] [102] This systematic review included five RCTs on contraceptive efficacy communication strategies. The main results were: • comprehension: higher in communication with sound slides than with the physician’s explanation (MD −19.00, 95% CI −27.52 to −10.48; one RCT) • correct answers: more frequent with efficacy communication using a category table compared to a numerical table (OR 2.42, 95% CI 1.43–4.12) and when compared to a category/numeric table (OR 2.58. 95% CI 1.5–4.42; one RCT) |
| Communicating health risks and benefits with bar charts or bar charts and histograms |
[Ghosh, 2008] [89] This RCT included 150 women: 74 were randomized to receive communication via bar charts (categoric bars) and 76 via bar charts and histograms (frequency diagrams, bars with a range of values). The main results were: • 72% of the women overestimated their risk of breast cancer before the interventions • the frequency of women who had improved comprehension of this risk was not different between the different communication strategies (42% versus 54%; p = 0.1) • for the subgroup that overestimated the risk before the interventions, improvements in the estimate accuracy were more frequent in those receiving communication with bar charts and frequency diagrams (19% versus> 9%, p = 0.004) |
| Strategies for communication of health evidence |
[Epstein, 2004] [83] This systematic review included eight studies, and the main results were: • the order of communicating the information and the outcomes may distort the comprehension of the population • when evidence was limited, using graphs or figures with human faces representing probabilities and vertical bar charts for comparative information were helpful • less-educated and older people preferred proportions to percentages and did not comprehend confidence intervals • the absolute risk was better comprehended than RRR • review authors suggested five aspects that should be considered when communicating scientific evidence to the population: comprehension of the experience and expectations of the patient (and their family members), building partnerships, providing evidence (including a balanced discussion of uncertainties), presenting recommendations informed by clinical judgment and patient preferences, and checking for comprehension and agreement |
|
[Grimshaw, 2012] [11] This narrative review presented some strategies for communicating health evidence divided into three groups Decision support strategies (to assist choices about health treatment options): • when compared with no strategy, decision support improved knowledge and risk accuracy perceptions, reduced the proportion of people who were passive in decision-making, resulted in a higher proportion of patients reaching informed decisions consistent with their values, reduced the number of people who remained undecided, reduced decision-making conflict and reduced choice for elective major surgery options favouring conservative options. Decision support did not impact satisfaction; however, further research is needed to clarify its effects on adherence to the chosen option, patient–professional communication, its cost-effectiveness and its impact on low-literate or developing populations (86 RCTs, 20 209 participants) Personalized risk communication (information focusing on a personal interest using, for example, epidemiological calculation methods for risk calculations): • personalized risk communication (textual, verbal or visual): increased uptake of screening tests for health conditions (weak evidence, consistent with a small effect; 22 RCT Communication before consultations (any intervention delivered before a medical visit to help the patient to clarify his/her doubts during consultations): • compared with control, communication before consultations increased questions asked during these consultations. Both verbal counselling and textual intervention produced similar effects on questions, but counselling increased patient satisfaction (33 RCT, 8244 participants) | |
| Strategies for communicating risks and benefits in health with different animated graphical presentations |
[Zikmund-Fisher, 2012] [137] This RCT included 4198 participants who were randomized to receive risk–benefit outcomes of health interventions based on ten different graphical presentations. Following this, participants were asked to choose the most effective and safest treatment. The probability of the participant choosing the ‘correct’ treatment with each type of graph was: • static grouped: OR 1 • static scattered: OR 0.59; 95% CI 0.38–0.91 • scatter, settles: OR 0.67; 95% CI 0.43–1.03 • grouped, built: OR 1.01; 95% CI 0.64–1.60 • scatter, built: OR 0.75; 95% CI 0.48–1.18 • scatter, built, settles: OR 0.80; 95% CI 0.51–1.26 • scatter, auto shuffles: OR 0.64; 95% CI 0.40–1.00 • scatter, auto shuffles, settles: OR 0.94; 95% CI 0.59–1.49 • scatter, user shuffles: OR 0.52; 95% CI 0.34–0.80 • scatter, user shuffles, settles: OR 0.81; 95% CI 0.52–1.27 After interpreting the results, the authors concluded that the proposed animated risk graphics showed no benefits over the traditional charts. In some cases, the animated graphs worsened the communication of risks and benefits of the intervention |
| Communication of uncertainty in health | |
|---|---|
| Subcategory | Main results |
| Communication of uncertainties about the effects of interventions on health |
[Büchter, 2020] [73] In this RCT, eight versions of a summary about the effects of medication for tinnitus were compared. The versions varied in degree, type and magnitude (number of reasons) of uncertainty. Overall, 1727 participants were randomized to receive one of these versions, and the following results were reported: • perception of treatment efficacy: no difference between the methods of presenting the degree and type of uncertainty; as to the method of presenting the magnitude of uncertainty, there was greater perception when two reasons were presented compared to three (p = 0.04) • certainty for judging the efficacy of treatment: no difference between the variation of showing the degree, type and magnitude of uncertainty • perception about the final body of evidence: the description of imprecision was associated with a greater perception of the limitations of the evidence than the general statement that more research is needed (p = 0.01) • quality of the text: no difference between the methods for presenting the degree, type and magnitude of uncertainty • the decision to use the medication: no difference between the methods for presenting the degree, type and magnitude of uncertainty |
| Evidence synthesis frameworks using plain language | |
|---|---|
| Subcategory | Main results |
| Blogshots to communicate the results of systematic reviews |
[Arienti, 2018] [69] This case study reported the experience of implementing five blogshots (infographics) to communicate the results of Cochrane reviews on rehabilitation in plain language. The results of accessing each blogshot were: • yoga: 2633 views, 67 interactions, 49 access to review • vocational rehabilitation: 2697 views, 67 interactions, 23 accesses to the full review • fatigue treatment: 1712 views, 76 interactions, 39 access to review • cardiovascular rehabilitation: 3419 views, 120 interactions, 51 accesses to full review (p = 0.12) |
| Evidence synthesis summary template |
[Hartling, 2018] [92] This survey collected information and opinions from managers on evidence synthesis summaries. The qualitative analysis of the results showed that: • decision-makers suggested a three-page summary with key messages, details on results, meaningful numbers/tables, and strength of evidence Detailed methods and contextual information were considered less important |
| Plain language abstract |
[Kerwer, 2021] [95] This descriptive study evaluated, through a survey, the opinion of 166 people about 12 original (scientific) abstracts and their respective plain language abstracts reporting the results of 12 different study designs. The main results showed that the plain language versions: • presented greater readability and allowed a correct comprehension of the corresponding information • were perceived as more reliable • were able to make the reader more confident about their ability to decide based on the content learned |
| Cochrane plain language summaries |
[Santesso, 2015] [124] This RCT included 143 participants from five countries (Canada, Norway, Argentina, Spain and Italy): 97 were randomized to receive the plain language summaries and 96 to receive the original abstract (scientific) of a Cochrane systematic review about the effects of vitamin C for the common cold. The main results were: • more participants in the plain language group comprehended the benefits and harms of treatment and the certainty of the evidence (53% versus 18%, p < 0.001). Comprehension occurred regardless of education level • more participants in the plain language group answered the requested questions correctly (p < 0.001) • reliability, accessibility, comprehensiveness and utility for helping decisions were more frequent among those who received plain language summaries |
| Templates for plain language abstracts of systematic reviews |
[Marquez, 2018] [103] In this survey, managers evaluated two new templates and one traditional template for summaries of systematic reviews through the System Usability Scale (SUS, a score < 68 is below average usability). The SUS score (standard deviation) was 55.7 (17.2) for the traditional template, 85.5 (8.0) for the new template 1 and 86.4 (11.5) for the new template 2 |
| Printed newsletters for communicating health evidence |
[Murthy, 2012] [108] This literature review identified interrupted time series assessing the dissemination of printed newsletters based on evidence from systematic reviews. The main results were: • reduced surgery rates for prominent ear correction in children younger than 10 years (mean annual decline: −10.1%, 95% CI −7.9 to −12.3) • reduced surgery rates for prominent ear correction in children younger than 15 years (mean quarterly decline: −0.044, 95% CI −0.080 to −0.011) |
| Systematic review summaries of evidence templates for policymakers and health system managers |
[Petkovic, 2016] [116] This systematic review included six studies assessing the use of evidence summaries by managers, and the main results showed that: • evidence summaries were more effortless to comprehend than full systematic reviews • it is unclear whether using abstracts increased the use of evidence derived from systematic reviews in decision-making • targeted and personalized messages have increased the number of evidence-based public health policies and programmes • there was little or no difference in the use of evidence summaries for decision-making regarding knowledge, comprehension or beliefs, perceived usefulness or usability • summary tables of findings with the certainty of evidence rating were considered easier to comprehend compared with full systematic reviews • reporting of study event rates and absolute differences were considered comprehensible |
| Guidelines for elaborating/evaluating communication products | |
|---|---|
| Subcategory | Main results |
| Guidelines for designing and evaluating health evidence communication products (CDC Clear Communication Index) |
[Baur, 2014] [71] In this survey, 870 participants (general population) blindly assessed the quality of two versions of the same health evidence communication material: the original version and the version adjusted according to the CDC clear checklist items. Communication index for designing and evaluating health communication products (http://www.cdc.gov/healthcommunication/ClearCommunicationIndex/). The three assessed materials were: questions and answers about using thimerosal (preservative) in vaccines, a fact sheet on heart disease and a fact sheet on cell phone use and health. The results of the evaluations showed that: • on average, the original versions of the three materials scored less than 30% on the checklist, and the adjusted versions scored 90% or more • the adoption of the checklist increased the quality of health communication and evidence products for the population |
| Tool for evaluating the quality of health texts in plain language |
[Logullo, 2019] [101] In this study, the DISCERN tool was translated, culturally adapted and had its psychometric properties evaluated in Portuguese. The tool was applied in a validation study that used the plain language summary of a Cochrane systematic review. The main results were: • the Brazilian Portuguese version had excellent internal consistency and good reproducibility • age, sex and health literacy did not interfere with the score resulting from the application of the tool |
| Teaching/learning | |
|---|---|
| Subcategory | Main results |
| Communication/learning of key concepts related to the effects of health interventions |
[Cusack, 2018] [9] This systematic review included 24 studies (most at high or moderate risk of bias) on communication/learning strategies key concept effects of health interventions Strategies implemented inside and outside the school environment, single or multiple, were identified using different approaches such as discussion groups, printed material, online classes, and short- or long-term courses. The outcomes evaluated included: knowledge, skills, behaviour, confidence, perception of knowledge and/or skill, attitude and satisfaction. The main results observed were: • the effects of strategies on trust, attitude and behaviour were uncertain • improvements in the quality of studies, consistency of outcome measures, and longer-term evaluation of strategies are needed to improve reliability in estimating the effects of the strategies evaluated |
| Communication/learning resources from the IHC initiative on key concepts of evidence for health |
[Ikirezi, 2016] [94] This case study evaluated the feasibility of implementing communication/learning resources to support the comprehension and application of key concepts in the critical assessment of the evidence in health in a preschool in Rwanda. The main results observed in the qualitative analysis were: • the user experience was positive, as implementing the IHC features was considered beneficial, contextualized, reliable, feasible and desirable • the restricted time to use the resources was considered a barrier, while curiosity and a positive attitude towards the resources were facilitators • students and faculty suggested that IHC resources be distributed to other students at other schools so they could also benefit from the teachings and importance of making evidence-informed health choices |
|
[Mugisha, 2016] [107] This case study reported the experience of implementing communication/learning resources to support the comprehension and application of key concepts in the critical appraisal of the evidence in health in a primary school in Rwanda. The main results observed in the qualitative analysis were: • the use of IHC resources translated into Kinyarwanda was considered viable in Rwanda • it was essential to collect suggestions and ideas from participants to contextualize the IHC resources in the local scenario • children and teachers can be helpful in evaluating and reviewing primary school resources and contribute significantly to improving educational resources that would benefit ministries of education • the resources were considered useful, feasible, reliable and comprehensible by users | |
|
[Nsangi, 2017] [110] This cluster clinical trial included 120 schools that were randomized to receive learning resources (for example, teacher’s guides, exercise and textbooks, posters, songs and activities cards; intervention group, n = 60, 76 teachers and 6383 children) or not (control group, n = 60, 67 teachers and 4430 children). The main results were: • children's mean score on a test with two multiple-choice questions for each of the 12 key concepts in the material: 62.4% (SD 18.8) in the intervention group versus 43.1% (SD 15.2) in the control group (adjusted mean difference 20%; 95% CI 17.3–22.7; p < 0.00001) • the proportion of children with sufficient scores to pass the same test (≥ 13 of 24 correct answers): 69% (3967/5753) in the intervention group versus 27% (1186/4430) in the control group (adjusted difference of 50%; 95% CI 44–55) • the intervention was effective for children with different reading skills but was more effective in the subgroup of children with better reading skills | |
| Communication/learning of key concepts of health evidence |
[Nordheim, 2016] [109] This systematic review identified RCT and non-randomized studies comparing different educational strategies to acquire skills for the critical assessment of health evidence. The main results were: • active versus traditional teaching methodologies: capacity for basic knowledge about causality and association, randomization, epidemiology concepts and evidence-based medicine was 71% higher with active methods • educational strategy versus control: the ability to recognize that multiple outcomes can influence cancer research results were twice as high in the group that received an educational strategy • educational strategy with active methodology versus control: the comprehension of the need for comparative studies to make inferences about causality was 51% higher with the use of the educational strategy • fictional evidence reasoning simulation versus control group: reduction in the number of inappropriate responses, including personal beliefs and unsupported opinions, with the use of simulation |
| Educational podcasts from the IHC initiative on key health evidence concepts |
[Ringle, 2020] [118] This RCT included 250 American parents randomized to listen to the podcasts with evidence-based health content developed by the IHC initiative (intervention group, n = 128) or podcasts with general information (control group, n = 122). The main results were: • critical thinking skill: 53% of parents in the intervention group achieved a satisfactory score on the applied skill test (> 18 and 21) versus 26.2% in the control group • satisfaction with the podcast (scale 1–5): similar between groups (4.16 ± 0.93 versus 4.20 ± 0.85) • listening to the IHC podcast improved parents’ behaviour towards evidence-based practice and preference for evidence-based health information • podcasts are available at: https://www.informedhealthchoices.org/podcast-for-parents/ |
|
[Semakula, 2017; Semakula, 2020] [125, 126] This RCT included 675 parents of Ugandan elementary school students who were randomized to listen to podcasts with evidence-based health content (intervention group, n = 334) developed by the IHC initiative or podcasts with general health information used by the public service (control group, n = 341). The main initial and post-1 year results were: • mean critical thinking skill test score (two multiple-choice questions for each of nine key critical thinking concepts, 18 questions total): 67.8% (SD 19.6%) in the intervention group versus 52 .4% (SD 17.6%) in the control group (adjusted DM 15.5%; 95% CI 12.5–18.6%; p < 0.0001); after 1 year: 58.9% in the intervention group versus 52.6% in the control group (adjusted DM 6.7%; 95% CI 3.3–10.1%) • frequency of parents who achieved the minimum passing test score (at least 11 out of 18): 71% (203/288) in the intervention group versus 38% (103/273) in the control group (adjusted SD 34%; 95% CI 26–41%; p < 0·0001); after 1 year: 47.2% in the intervention group versus 39.5% in the control group (adjusted SD 9.8%; 95% CI 0.9–18.9%; p < 0.0001) • listening to the IHC initiative podcast improved parents’ ability to critically assess the information at baseline, but this ability declined substantially after 1 year | |
|
[Semakula, 2019b] [127] This descriptive study used design thinking methodology to develop podcasts on health evidence and presented users’ assessments of the podcasts. The main results were: • usefulness: IHC podcasts were considered useful tools that could help encourage critical thinking when publicized in the general media and specific contexts (for example, schools) • usability and comprehension: were considered satisfactory • credibility: considered satisfactory • desire to use: some participants asked if they could have access to all episodes. A non-governmental health communication organization and producers from the Uganda Broadcasting Corporation expressed their interest in broadcasting the podcasts on radio as part of their health communication programming | |
| Training for parliamentarians on scientific health evidence |
[Cockcroft, 2014] [78] In this case study, the authors reported the experience of training on scientific evidence in health for 36 of Botswana’s 54 elected parliamentarians. The training took place in two sessions (one theoretical and one practical workshop). It addressed the following topics: (i) initial concepts about scientific evidence (clinical trials, randomization, statistical significance, number needed to treat and bias) and the importance of control or comparators when evaluating the effects of interventions, (ii) how biases can distort results and reports, (iii) importance of evaluating the impact on public health and not just on individual health. The short-term qualitative assessment showed that: • feedback from Botswana parliamentarians were very favourable: they requested additional sessions to address the topics in more detail, and that training be offered to other decision-makers • after the training, one of the parliamentarians reported that the debate on updating the national human immunodeficiency virus (HIV) policy was more detailed and focused on evidence |
| Inclusion of stakeholders in the working group for preparing comparative effectiveness summaries |
[Balshem, 2011] [70] In this case study, the authors presented the process and results of including stakeholders (including managers) in preparing the summary ‘Medications to reduce the risk of primary breast cancer in women’. Stakeholders suggested that the conclusions of the summaries go beyond just saying that the evidence is insufficient and that further studies are needed. Instead, stakeholders indicated that the following issues be addressed in the summaries: • what evidence is available, and what can be learned from it? • what evidence tells us when and if an intervention is safe/harmful and effective/ineffective for relevant clinical outcomes? • what can we learn from the evidence from a study inferior to a randomized clinical trial? • what can patient records tell us about the safety of a treatment? • what evidence identifies the subpopulations most likely to benefit from its use? • what kind of evidence is needed to assess short-term and long-term effectiveness? • when is short-term evidence appropriate to be implemented? |
Regarding the target audience, 71.8% of the strategies were intended for the general population, 20.5% specifically for managers and 7.7% were applicable to both groups (Additional file 5).
According to the main category, communicating risks/benefits on health represented 29.5% of the strategies and encompassed different forms, nominal (categorical) or numerical (statistical), to communicate attributes or effects of health interventions or exposures. The 17 strategies in the ‘teaching/learning’ category, comprised structural actions in schools (many of them conducted by the IHC initiative), virtual environments (websites), and even in parliament (Table 1).
According to the status, more than half (52.6%) of the identified strategies had already been implemented and evaluated in some degree, 44.9% had already been implemented but not yet evaluated and 2.6% were merely proposed without any sort of implementation or evaluation (Additional file 5).
According to the delivery approach, 88.5% of the strategy had at least one textual component, 6.4% adopted an exclusively verbal approach of communication outreach and 2.6% a exclusively visual approach (Additional file 5).
As depicted in Additional file 5, the main barriers for implementing the proposed strategies are related to stakeholder time availability [73, 92, 107, 110], high speed of publication of new studies/growing volume of information [72, 77], language [76, 99, 104, 105, 121], conflicts of interest [78] and need for continuous update [97]. The main facilitator was online free access or social media access [2, 72, 97, 104, 105].
Discussion
This scoping review was developed to identify the evidence available on the strategies for communicating health scientific evidence to the public or managers, its characteristics and settings of implementation, as well as knowledge gaps. Overall, 80 studies, reports or other forms of information presentation were included which addressed 78 strategies. The most frequent strategies were those communicating risks and benefits in health, presenting textual delivery approach, implemented and, to some extent, evaluated. Although conclusions about effects are not the focus of a scoping review, among the strategies evaluated, those that appear to present some potential benefit are:
Risk/benefit communication: greater comprehension with natural frequencies than with percentages; greater comprehension with absolute risk than with relative risks and NNT; greater comprehension and behaviour change with numerical communication than with nominal communication; greater comprehension of mortality than of survival; communications with negative or loss content appear to be more useful for comprehension, satisfaction, and behaviour change than communications with positive or gain content; nominal communication can lead to overestimation of the risk of adverse events and can lead patients to make inappropriate decisions about whether or not to use a medication.
Evidence synthesis templates and other plain language documents: plain language summaries to communicate the results of Cochrane systematic reviews to the population were perceived to be more reliable, easier to find and understand, and better to support decisions than the original summaries.
Teaching/learning: the IHC initiative’s resources for communication and learning of key health evidence concepts appear to be effective in improving critical thinking skills in health immediately after their use; however, these effects were not observed after 1 year; theoretical–practical training for parliamentarians on scientific evidence in health seems to be a strategy with potential to raise awareness and improve the comprehension of this subgroup of managers on health-related evidence.
The main strengths of this scoping review involve a broad (across multiple sources of information) and sensitive (search strategies including also synonyms and free terms) search. As shown in Fig. 1, 24 598 references were screened in the first phase by reading titles and abstracts. Other features that endow methodological robustness are: the availability of a prospectively developed protocol, the selection and extraction of data in a duplicative and independent mode, and the adoption of methods recommended by the Joanna Briggs Institute Manual for scoping reviews [13].
One strength was the identification of communication strategies that used structuring learning approaches to continuously and progressively build a more favourable scenario for the population and managers to receive communication products. In this respect, the IHC initiative (https://www.informedhealthchoices.org/) and the ECRAN project (http://ecranproject.eu/) were particularly noteworthy.
For the categorization of communication strategies, different taxonomies have been identified in the literature that could be somewhat adapted for use in this scoping review [1, 99, 139, 140]. These taxonomies covered health communication in a broad sense, including mainly guidance on diagnostic, prophylactic and therapeutic conducts, many of them focusing on the individual and on the professional–patient relationship. Others had as the target audience mainly managers and health professionals, while others involved the whole process of knowledge translation and/or evidence implementation.
The particularities of health communication strategies with a specific focus on scientific evidence difficult reproducible and consistent adaptations from these aforementioned taxonomic tools. Thus, while conducting this scoping review, the authors developed, by means of an unstructured method, a proposal for a particular taxonomy for this scenario (Additional file 2). Although innovative, and having fulfilled its role within this scoping review, the proposed taxonomy has been applied for the first time and has not been formally evaluated, so limitations may be identified throughout its use hereafter.
When planning this review (protocol phase), there was no nominal definition of possible strategies. Along the construction of the search strategies, the term ‘risk communication’ and its synonyms were not used, but instead, less specific terms were used to sensitize the search. However, throughout the study selection process, a considerable number of studies specific to risk communication were identified. Thus, although 29.9% of the communication strategy included were specific to risk communication and health benefits, it is not possible to rule out that studies targeting this approach were not retrieved.
Another concern was that despite a number of different attempts (including messages to the authors, contacting experts and searching international libraries) it was not possible to obtain the full text of one of the identified studies [67]. The reading of the abstract did not allow us to confirm or refute the adequacy to the eligibility criteria and therefore this study remained as ‘awaiting classification’.
Some studies addressed combined strategies and it was not possible to quantify the exact number of different strategies addressed in the 78 strategies identified given a high rate of overlap of their components. To mitigate this shortcoming, we have chosen to present a detailed (and therefore longer than we would have preferred) table describing each strategy (Additional file 5).
Although 52.6% of the identified strategy were implemented and evaluated, much of these evaluations were characterized by opinions and satisfaction surveys. Few were evaluated through comparative studies capable of estimating their efficacy with more certainty and less bias. Additionally, the studies showed that most of the outcomes evaluated were limited to assessing comprehension, persuasion and customer satisfaction; few studies assessed health behaviour change, and none considered clinical outcomes.
Part of the strategies categorized as teaching/learning have been implemented and evaluated in African countries such as Rwanda [94], Uganda [110, 125, 126] and Botswana [78] which allowed us to evaluate the impact of these strategies, customer experience, barriers and facilitators in settings with limited financial and social resources.
As implications for practice, the identification of communication strategies that have been implemented and evaluated (Table 1) can support social, academic, governmental or non-governmental actions. Considering aspects such as feasibility, costs, need for regulation or local policies, regardless of the certainty of the available evidence, this review identified strategies that have already been evaluated in some way and that are potentially implementable in resource-scarce settings.
Strategies for communicating health risks and benefits, including attribute results and effects of interventions and exposures on health outcomes, were evaluated by studies with appropriate designs, with reliable results that could be implemented. An example is the benefit of communication using absolute frequencies and standardized decimal denominators (20 people out of 100 people using this drug might get diarrhea) rather than relative risk or NNT.
The elaboration and dissemination of communication products in parallel with scientific publications, and aimed at different audiences, is a reality (as exemplified by Cochrane’s plain language summary). This approach could be replicated and adopted by other organizations or scientific publishers, using results from reviews such as this one. In the same direction, the Brazilian Ministry of Health, in a recent initiative in partnership with the Escola Nacional de Administração (ENAP, National School of Administration), is producing prototype products for communicating scientific evidence in accessible language using design thinking methodology [141, 142].
As implications for forthcoming research, this scoping review identified a number of knowledge gaps that still need to be addressed by studies with appropriate designs and methods. These gaps include evidence on (i) the efficacy of communication strategies on outcome measures, such as behaviour change and clinical benefits related to the control or prevention of health conditions, (ii) the costs associated with implementing the strategies, (iii) effects of the strategies for low-income, lower sociocultural and/or resource-poor populations, and (iv) effects of the strategies for subgroups such as the elderly, adolescents and children.
Conclusions
This scoping review identified 80 studies, reports or other documents that addressed 78 strategies for communicating scientific health evidence to the population and/or managers. Some of these strategies have been implemented and evaluated, and may have some benefit in improving these audiences’ comprehension of evidence concepts and promoting behaviour change. The findings of this review have important potential for applicability in the area of evidence-informed policy, with direct application or adaptation of identified strategies to improve the communication of scientific evidence on healthcare to managers and the population. Future efforts are needed to evaluate the effects of evidence communication strategies on relevant clinical outcomes, identify the most appropriate strategies for different settings and contexts, and promote the use of those strategies that show benefits for individual or public health and health systems.
Supplementary Information
Additional file 1. Strategies of electronic and structured searches.
Additional file 2. Proposed taxonomy to categorize strategies for communicating scientific evidence in health to the population/managers.
Additional file 3. Studies/documents excluded and reasons for exclusions after reading the full text (second phase of the selection process).
Additional file 4. Main characteristics of included studies.
Additional file 5. Main characteristics of the identified strategies or sets of strategies for communicating scientific evidence.
Acknowledgements
We thank Daniela Fortunato Rêgo, Aurelina Aguiar de Lima, Keitty Regina Cordeiro de Andrade, Luciana Hentzy Moraes, Marina Melo Arruda Marinho, Roberta Borges Silva, Sarah Dos Santos Conceição e Virginia Kagure Wachira from Departamento de Ciência e Tecnologia da Secretaria de Ciência, Tecnologia, Inovação e Insumos Estratégicos (Decit/Sctie), Brazilian Ministry of Health.
Author contributions
Conceptualization: RR, ALCM, RLP. Writing – original draft: RLP, COCL, ALCM, RCMP. Writing review and editing: RR, DMMR, JOMB, MLTM, RG, SFS. Supervision: RR, DMMR, JOMB, MLTM, RG, SFS. Project administration: RR, DMMR, JOMB, MLTM, RG, SFS. Final approval: all authors.
Funding
Programa de Apoio ao Desenvolvimento Institucional do Sistema Único de Saúde (PROADI-SUS), Brazilian Ministry of Health.
Availability of data and materials
All relevant data is presented as supplementary files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rachel Riera, Email: rachelriera@hotmail.com.
Carolina de Oliveira Cruz Latorraca, Email: caru.pepm@yahoo.com.br.
Roberta Carreira Moreira Padovez, Email: roberta.carreira@gmail.com.
Rafael Leite Pacheco, Email: rleitepacheco@hotmail.com.
Davi Mamblona Marques Romão, Email: davi@veredas.org.
Jorge Otávio Maia Barreto, Email: jorgeomaia@hotmail.com.
Maria Lúcia Teixeira Machado, Email: mluciatmachado@gmail.com.
Romeu Gomes, Email: romeu.gomes@hsl.org.br.
Silvio Fernandes da Silva, Email: fernandessilvio90@gmail.com.
Ana Luiza Cabrera Martimbianco, Email: analuizacabrera@hotmail.com.
References
- 1.McCormack L, Sheridan S, Lewis M, Boudewyns V, Melvin CL, Kistler C, Lux LJ, Cullen K, Lohr KN. Communication and dissemination strategies to facilitate the use of health-related evidence. Evid Rep Technol Assess (Full Rep) 2013;213:1–520. doi: 10.23970/ahrqepcerta213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chapman E, Haby MM, Toma TS, de Bortoli MC, Illanes E, Oliveros MJ, Barreto JOM. Knowledge translation strategies for dissemination with a focus on healthcare recipients: an overview of systematic reviews. Implement Sci. 2020;15(1):14. doi: 10.1186/s13012-020-0974-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brownell SE, Price JV, Steinman L. Science communication to the general public: why we need to teach undergraduate and graduate students this skill as part of their formal scientific training. J Undergrad Neurosci Educ. 2013;12:E6–E10. [PMC free article] [PubMed] [Google Scholar]
- 4.Fontaine G, Lavallée A, Maheu-Cadotte MA, Bouix-Picasso J, Bourbonnais A. Health science communication strategies used by researchers with the public in the digital and social media ecosystem: a systematic scoping review protocol. BMJ Open. 2018;8(1):e019833. doi: 10.1136/bmjopen-2017-019833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chapman E, Pantoja T, Kuchenmüller T, Sharma T, Terry RF. Assessing the impact of knowledge communication and dissemination strategies targeted at health policy-makers and managers: an overview of systematic reviews. Health Res Policy Syst. 2021;19(1):140. doi: 10.1186/s12961-021-00780-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, Costiniuk C, Blank D, Schünemann H. Framing of health information messages. Cochrane Database Syst Rev. 2011;12:CD006777. doi: 10.1002/14651858.CD006777.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, Costiniuk C, Blank D, Schünemann H. Using alternative statistical formats for presenting risks and risk reductions. Cochrane Database Syst Rev. 2011;2011(3):CD006776. doi: 10.1002/14651858.CD006776.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Büchter RB, Fechtelpeter D, Knelangen M, Ehrlich M, Waltering A. Words or numbers? Communicating risk of adverse effects in written consumer health information: a systematic review and meta-analysis. BMC Med Inform Decis Mak. 2014;14:76. doi: 10.1186/1472-6947-14-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cusack L, Del Mar CB, Chalmers I, Gibson E, Hoffmann TC. Educational interventions to improve people's understanding of key concepts in assessing the effects of health interventions: a systematic review. Syst Rev. 2018;7(1):68. doi: 10.1186/s13643-018-0719-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burkiewicz JS, Vesta KS, Hume AL. Improving effectiveness in communicating risk to patients. Consult Pharm. 2008;23(1):37–43. doi: 10.4140/tcp.n.2008.37. [DOI] [PubMed] [Google Scholar]
- 11.Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50. doi: 10.1186/1748-5908-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medendorp NM, Stiggelbout AM, Aalfs CM, Han PKJ, Smets EMA, Hillen MA. A scoping review of practice recommendations for clinicians' communication of uncertainty. Health Expect. 2021;24(4):1025–1043. doi: 10.1111/hex.13255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil, H. Chapter 11: Scoping Reviews (2020 version). In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis, JBI, 2020. https://jbi-global-wiki.refined.site/space/MANUAL/4687833/11.1+Introduction+to+Scoping+reviews. Acessed 16 Sep 2022.
- 14.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 15.Martimbianco ALC, Pacheco RL, Bagattini AM, Padovez RFCM, Riera R. Strategies for communicating health evidence to health policymakers and the population. Scoping review protocol. medRxiv 2021.11.04.21265922; doi: 10.1101/2021.11.04.21265922. https://www.medrxiv.org/content/10.1101/2021.11.04.21265922v1.article-info. Accessed 16 Sep 2022.
- 16.Ouzanni M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adam T, Moat KA, Ghaffar A, Lavis JN. Towards a better understanding of the nomenclature used in information-packaging efforts to support evidence-informed policymaking in low- and middle-income countries. Implement Sci. 2014;9:67. doi: 10.1186/1748-5908-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.AHRQ. Environmental scan of patient safety education and training programs. (Prepared by American Institutes for Research, under contract HHSA290200600019i). AHRQ Publication No. 13–0051- EF. Rockville, MD: Agency for Healthcare Research and Quality; June 2013. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/final-reports/environmental-scan-programs/envptscan.pdf. Accessed 16 Sep 2022.
- 19.Alkhaldi M, Meghari H, Jillson IA, Alkaiyat A, Tanner M. State of research quality and knowledge transfer and translation and capacity strengthening strategies for sound health policy decision-making in Palestine. Int J Public Health. 2021;66:620425. doi: 10.3389/ijph.2021.620425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armstrong R, Waters E, Roberts H, Oliver S, Popay J. The role and theoretical evolution of knowledge translation and exchange in public health. J Public Health (Oxf) 2006;28(4):384–389. doi: 10.1093/pubmed/fdl072. [DOI] [PubMed] [Google Scholar]
- 21.Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan. Implement Sci. 2013;8:121. doi: 10.1186/1748-5908-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ashcraft LE, Quinn DA, Brownson RC. Strategies for effective dissemination of research to United States policymakers: a systematic review. Implement Sci. 2020;15(1):89. doi: 10.1186/s13012-020-01046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austvoll-Dahlgren A, Nsangi A, Semakula D. Interventions and assessment tools addressing key concepts people need to know to appraise claims about treatment effects: a systematic mapping review. Syst Rev. 2016;5(1):215. doi: 10.1186/s13643-016-0389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barac R, Stein S, Bruce B, Barwick M. Scoping review of toolkits as a knowledge translation strategy in health. BMC Med Inform Decis Mak. 2014;14:121. doi: 10.1186/s12911-014-0121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bastian H, Kaiser T, Matschewsky S. Förderung allgemeiner Gesundheits- und Wissenschaftskenntnisse mittels Bürger- und Patienteninformation: Die Rolle des IQWiG [Promotion of general health and scientific literacy via consumer and patient information: the role of the IQWiG] Z Arztl Fortbild Qualitatssich. 2005;99(6):379–385. [PubMed] [Google Scholar]
- 26.Bastian H. Health literacy and patient information: developing the methodology for a national evidence-based health website. Patient Educ Couns. 2008;73(3):551–556. doi: 10.1016/j.pec.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 27.Campbell A, Louie-Poon S, Slater L, Scott SD. Knowledge translation strategies used by healthcare professionals in child health settings: an updated systematic review. J Pediatr Nurs. 2019;47:114–120. doi: 10.1016/j.pedn.2019.04.026. [DOI] [PubMed] [Google Scholar]
- 28.Carman KL, Workman TA. Engaging patients and consumers in research evidence: applying the conceptual model of patient and family engagement. Patient Educ Couns. 2017;100(1):25–29. doi: 10.1016/j.pec.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Carvalho IA, Byles J, Aquah C, Amofah G, Biritwum R, Panisset U, et al. Informing evidence-based policies for ageing and health in Ghana. Bull World Health Organ. 2015;93(1):47–51. doi: 10.2471/BLT.14.136242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Colquhoun HL, Helis E, Lowe D, Belanger D, Hill S, Mayhew A, et al. Development of training for medicines-oriented policymakers to apply evidence. Health Res Policy Syst. 2016;14(1):57. doi: 10.1186/s12961-016-0130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crowley M, Scott JTB, Fishbein D. Translating prevention research for evidence-based policymaking: results from the research-to-policy collaboration pilot. Prev Sci. 2018;19(2):260–270. doi: 10.1007/s11121-017-0833-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erismann S, Pesantes MA, Beran D, Leuenberger A, Farnham A, Berger Gonzalez de White M, et al. How to bring research evidence into policy? Synthesizing strategies of five research projects in low-and middle-income countries. Health Res Policy Syst. 2021;19(1):29. doi: 10.1186/s12961-020-00646-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evans I, Thornton H, Chalmers I, Glasziou P. Avaliação de tratamentos de saúde—identificando evidências científicas para oferecer sempre o melhor para a saúde 2a. ed. – Barueri, SP: Minha Editora, 2016.
- 34.FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and other Tools) Resource [Internet]. Silver Spring (MD): Food and Drug Administration (US); Co-published by National Institutes of Health (US), Bethesda (MD). 2016. https://www.ncbi.nlm.nih.gov/books/NBK326791/. Accessed 16 Sep 2022. [PubMed]
- 35.Fadlallah R, El-Jardali F, Nomier M, et al. Using narratives to impact health policy-making: a systematic review. Health Res Policy Syst. 2019;17(1):26. doi: 10.1186/s12961-019-0423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fervers B, Leichtnam-Dugarin L, Carretier J, Delavigne V, Hoarau H, Brusco S, et al. The SOR SAVOIR PATIENT project—an evidence-based patient information and education project. Br J Cancer. 2003;89(Suppl 1):S111–S116. doi: 10.1038/sj.bjc.6601093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7. [DOI] [PubMed] [Google Scholar]
- 38.Genova J. Reintroducing communication as a strategy in printed evidence-based medical materials. Model to assess effectiveness. 2012. doi: 10.20381/ruor-6190. https://ruor.uottawa.ca/handle/10393/23497. Accessed 16 Sep 2022.
- 39.Glenton C, Santesso N, Rosenbaum S, Nilsen ES, Rader T, Ciapponi A, Dilkes H. Presenting the results of cochrane systematic reviews to a consumer audience: a qualitative study. Med Decis Making. 2010;30(5):566–577. doi: 10.1177/0272989X10375853. [DOI] [PubMed] [Google Scholar]
- 40.Gudi SK, Tiwari KK, Panjwani K. Plain-language summaries: an essential component to promote knowledge translation. Int J Clin Pract. 2021;75(6):e14140. doi: 10.1111/ijcp.14140. [DOI] [PubMed] [Google Scholar]
- 41.Han PK. Conceptual, methodological, and ethical problems in communicating uncertainty in clinical evidence. Med Care Res Rev. 2013;70(1 Suppl):14S–36S. doi: 10.1177/1077558712459361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hesse BW, Johnson LE, Davis KL. Extending the reach, effectiveness, and efficiency of communication: evidence from the centers of excellence in cancer communication research. Patient Educ Couns. 2010;81(Suppl):S1–5. doi: 10.1016/j.pec.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hibbard JH. Patient activation and the use of information to support informed health decisions. Patient Educ Couns. 2017;100(1):5–7. doi: 10.1016/j.pec.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Hupert J. Translating best evidence into best care. J Pediatr. 2017;190(11):287–290. doi: 10.1016/j.jpeds.2017.08.050. [DOI] [PubMed] [Google Scholar]
- 45.Jirjis J, Weiss JB, Giuse D, Rosenbloom ST. A framework for clinical communication supporting healthcare delivery. AMIA Annu Symp Proc. 2005;2005:375–379. [PMC free article] [PubMed] [Google Scholar]
- 46.Kelechi TJ, Naccarato MK. Knowledge translation: summarizing and synthesizing the evidence for WOC best practices. J Wound Ostomy Continence Nurs. 2010;37(2):132–136. doi: 10.1097/WON.0b013e3181cf886c. [DOI] [PubMed] [Google Scholar]
- 47.LaRocca R, Yost J, Dobbins M, Ciliska D, Butt M. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. 2012;12:751. doi: 10.1186/1471-2458-12-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lavis JN, Panisset U. EVIPNet Africa's first series of policy briefs to support evidence-informed policymaking. Intern J Technology Assess Health Care. 2010;26:229–232. doi: 10.1017/S0266462310000206. [DOI] [PubMed] [Google Scholar]
- 49.Moat KA, Lavis JN. Supporting the use of research evidence in the Americas through an online "one-stop shop": the EVIPNet VHL. Cad Saude Publica. 2014;30(12):2697–2701. doi: 10.1590/0102-311X00110214. [DOI] [PubMed] [Google Scholar]
- 50.Nair-Bedouelle S. Science journalism needed now, more than ever. 2021. https://cdn.who.int/media/docs/default-source/epi-win/1_science-journalism-needed-now_s.-nair-bedouelle.pdf?sfvrsn=eaaae174_4. Accessed 16 Sep 2022.
- 51.O'Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Health Commun. 2007;12(7):623–644. doi: 10.1080/10810730701615198. [DOI] [PubMed] [Google Scholar]
- 52.O'Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Commun. 2009;59:296–316. doi: 10.1111/j.1460-2466.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 53.O'Keefe DJ, Wu D. Gain-framed messages do not motivate sun protection: a meta-analytic review of randomized trials comparing gain-framed and loss-framed appeals for promoting skin cancer prevention. Int J Environ Res Public Health. 2012;9(6):2121–2133. doi: 10.3390/ijerph9062121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oxman M, Habib L, Jamtvedt G, Kalsnes B, Molin M. Using claims in the media to teach essential concepts for evidence-based healthcare. BMJ Evid Based Med. 2021;26(5):234–236. doi: 10.1136/bmjebm-2020-111390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pettman TL, Armstrong R, Jones K, Waters E, Doyle J. Cochrane update: building capacity in evidence-informed decision-making to improve public health. J Public Health (Oxf) 2013;35(4):624–627. doi: 10.1093/pubmed/fdt119. [DOI] [PubMed] [Google Scholar]
- 56.Rapport F, Clay-Williams R, Churruca K, Shih P, Hogden A, Braithwaite J. The struggle of translating science into action: Foundational concepts of implementation science. J Eval Clin Pract. 2018;24(1):117–126. doi: 10.1111/jep.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sachs L. Kommunikativa problem i den evidensbaserade medicinen [Communication problems in evidence-based medicine] Lakartidningen. 2002;99(8):757–762. [PubMed] [Google Scholar]
- 58.Semakula D, Nsangi A, Oxman A, Glenton C, Lewin S, Rosenbaum S, Oxman M, Kaseje M, Austvoll-Dahlgren A, Rose CJ, Fretheim A, Sewankambo N. Informed Health Choices media intervention for improving people's ability to critically appraise the trustworthiness of claims about treatment effects: a mixed-methods process evaluation of a randomised trial in Uganda. BMJ Open. 2019;9(12):e031510. doi: 10.1136/bmjopen-2019-031510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sim I, Sanders GD, McDonald KM. Evidence-based practice for mere mortals: the role of informatics and health services research. J Gen Intern Med. 2002;17(4):302–308. doi: 10.1046/j.1525-1497.2002.10518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sofaer S, Hibbard J. Best practices in public reporting no. 2: maximizing consumer understanding of public comparative quality reports: effective use of explanatory information. Rockville, MD: Agency for Healthcare Research and Quality; June 2010. AHRQ Publication No. 10–0082–1-EF. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/public-reporting/report-2-public-reporting.pdf. Accessed 16 Sep 2022.
- 61.Solomon ED, Mozersky J, Wroblewski MP, Baldwin K, Parsons MV, Goodman M, et al. Understanding the use of optimal formatting and plain language when presenting key information in clinical trials. J Empir Res Hum Res Ethics. 2022;17(1–2):177–192. doi: 10.1177/15562646211037546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Teichmann L, Nossek S, Bridgman A, Loewen PJ, Owen T, Ruths D, et al. Public health communication and engagement on social media during the COVID-19 pandemic. Media Ecosystem Observatory. Centre for Media, Technology and Democracy;2020. https://www.mediatechdemocracy.com/work/meo-public-health-communication-and-engagement-on-social-media-during-the-covid-19-pandemic. Accessed 16 Sep 2022.
- 63.The SURE Collaboration. SURE guides for preparing and using evidence-based policy briefs: informing and engaging stakeholders. Versão 2.1. The SURE Collaboration, 2011. www.evipnet.org/sure. Accessed 27 Jul 2022.
- 64.Thissen P. Developing evaluation capacity: a conversation with the head of Global Evaluation Initiative. 2019. https://www.3ieimpact.org/blogs/developing-evaluation-capacity-conversation-head-global-evaluation-initiative. Accessed 16 Sep 2022.
- 65.Yost J, Ganann R, Thompson D, Aloweni F, Newman K, Hazzan A, et al. The effectiveness of knowledge translation interventions for promoting evidence-informed decision-making among nurses in tertiary care: a systematic review and meta-analysis. Implement Sci. 2015;10:98. doi: 10.1186/s13012-015-0286-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.YousefiNooraie R, Kwan BM, Cohn E, AuYoung M, Clarke Roberts M, Adsul P, et al. Advancing health equity through CTSA programs: opportunities for interaction between health equity, dissemination and implementation, and translational science. J Clin Transl Sci. 2020;4(3):168–175. doi: 10.1017/cts.2020.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nannini A, Houde SC. Translating evidence from systematic reviews for policy makers. J Gerontol Nurs. 2010;36(6):22–26. doi: 10.3928/00989134-20100504-02. [DOI] [PubMed] [Google Scholar]
- 68.Antonopoulou V, Chadwick P, McGee O, Sniehotta FF, Lorencatto F, Meyer C, O’Donnell A, Lecouturier J, Kelly M, Michie S. Research engagement with policy makers: a practical guide to writing policy briefs. National Institute for Health Research (NIHR) [Policy Research Unit in Behavioural Science. 2021. https://research.ncl.ac.uk/behscipru/outputs/guidetowritingpolicybriefs/. Accessed 16 Sep 2022.
- 69.Arienti C, Gimigliano F, Ryan-Vig S, Kiekens C, Negrini S. Cochrane rehabilitation blogshots: a modern method to spread cochrane evidence. Eur J Phys Rehabil Med. 2018;54(3):466–468. doi: 10.23736/S1973-9087.18.05313-3. [DOI] [PubMed] [Google Scholar]
- 70.Balshem H, Curtis P, Joplin L, Justman RA, Rosenberg AB. Stakeholder involvement in improving comparative effectiveness reviews: AHRQ and the effective health care program (Prepared by the AHRQ Effective Health Care Program Product Development Work Group under Contract No. HHSA 290–2007-10057-I). AHRQ Publication No. 11-EHC079-EF. Rockville, MD: Agency for Healthcare Research and Quality. September 2011. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/stakeholder-engagement_research.pdf. Accessed 16 Sep 2022.
- 71.Baur C, Prue C. The CDC clear communication index is a new evidence-based tool to prepare and review health information. Health Promot Pract. 2014;15(5):629–637. doi: 10.1177/1524839914538969. [DOI] [PubMed] [Google Scholar]
- 72.Bireme. Boletim BIREME n° 50. Mapa de Evidências: traduzindo o conhecimento para aproximar a ciência da gestão em saúd, 5 dezembro, 2020. https://boletin.bireme.org/pt/2020/12/05/mapa-de-evidencias-traduzindo-o-conhecimento-para-aproximar-a-ciencia-da-gestao-em-saude-2/. Accessed 16 Sep 2022.
- 73.Büchter RB, Betsch C, Ehrlich M, Fechtelpeter D, Grouven U, Keller S, et al. Communicating uncertainty in written consumer health information to the public: parallel-group, web-based randomized controlled trial. J Med Internet Res. 2020;22(8):e15899. doi: 10.2196/15899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Busert LK, Mütsch M, Kien C, Flatz A, Griebler U, Wildner M, et al; Cochrane Public Health Europe. Facilitating evidence uptake: development and user testing of a systematic review summary format to inform public health decision-making in German-speaking countries. Health Res Policy Syst. 2018;16(1):59. 10.1186/s12961-018-0307-z. [DOI] [PMC free article] [PubMed]
- 75.Carroll C, Cooke J, Booth A, Beverley C. Bridging the gap: the development of knowledge briefings at the health and social care interface. Health Soc Care Community. 2006;14(6):491–498. doi: 10.1111/j.1365-2524.2006.00637.x. [DOI] [PubMed] [Google Scholar]
- 76.Castle JC, Chalmers I, Atkinson P, Badenoch D, Oxman AD, Austvoll-Dahlgren A, et al. Establishing a library of resources to help people understand key concepts in assessing treatment claims—the "Critical thinking and Appraisal Resource Library" (CARL). PLoS One. 2017;12(7):e0178666. 10.1371/journal.pone.0178666. [DOI] [PMC free article] [PubMed]
- 77.Chambers D, Wilson PM, Thompson CA, Hanbury A, Farley K, Light K. Maximizing the impact of systematic reviews in health care decision making: a systematic scoping review of knowledge-translation resources. Milbank Q. 2011;89(1):131–156. doi: 10.1111/j.1468-0009.2011.00622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cockcroft A, Masisi M, Thabane L, Andersson N. Science communication. Legislators learning to interpret evidence for policy. Science. 2014;345(6202):1244–1245. doi: 10.1126/science.1256911. [DOI] [PubMed] [Google Scholar]
- 79.Davidson B. Storytelling and evidence-based policy: lessons from the grey literature. Palgrave Commun. 2017;3:17093. doi: 10.1057/palcomms.2017.93. [DOI] [Google Scholar]
- 80.Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, Bowman M. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 81.Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman JL, Ewigman B, Bowman M. Simplifying the language of evidence to improve patient care: Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. J Fam Pract. 2004;53(2):111–120. [PubMed] [Google Scholar]
- 82.Edwards A, Elwyn G, Covey J, et al. Presenting risk information—a review of the effects of ‘framing’ and other manipulations on patient outcomes. J Health Commun. 2001;6(1):61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- 83.Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA. 2004;291(19):2359–2366. doi: 10.1001/jama.291.19.2359. [DOI] [PubMed] [Google Scholar]
- 84.European Research Area Network for Environment and Health (ERA-ENVHEALTH). Improving knowledge transfer a checklist for researchers. 2019. https://www.era-learn.eu/network-information/networks/era-envhealth. Accessed 16 Sep 2022.
- 85.Fortin JM, Hirota LK, Bond BE, O'Connor AM, Col NF. Identifying patient preferences for communicating risk estimates: a descriptive pilot study. BMC Med Inform Decis Mak. 2001;1:2. doi: 10.1186/1472-6947-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Freeman A, Kerr J, Recchia G, Ellermann C. Communicating risks and evidence in a public health emergency. WHO EPI-WIN Webinar—Science Communication. 2021. https://www.who.int/news-room/events/detail/2021/09/14/default-calendar/communicating-risks-and-evidence-in-a-public-health-emergency. Accessed 16 Sep 2022.
- 87.Freeman A. Trustworthy and useful evidence communication, evidence communication tick-list. Opening panel presentations. WHO global conference on communicating science during health emergencies. https://cdn.who.int/media/docs/default-source/epi-win/4_trustworthy-useful-evidence-communication_a-freeman.pdf?sfvrsn=15516667_4. Acessed 27 Jul 2022.
- 88.Ghosh AK, Ghosh K. Translating evidence-based information into effective risk communication: current challenges and opportunities. J Lab Clin Med. 2005;145(4):171–180. doi: 10.1016/j.lab.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 89.Ghosh K, Crawford BJ, Pruthi S, Williams CI, Neal L, Sandhu NP, Johnson RE, Wahner-Roedler D, Britain MK, Cha SS, Ghosh AK. Frequency format diagram and probability chart for breast cancer risk communication: a prospective, randomized trial. BMC Womens Health. 2008;8:18. doi: 10.1186/1472-6874-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gigerenzer G, Gaissmaier W, Kurz-Milcke E, et al. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest. 2007;8(2):53–96. doi: 10.1111/j.1539-6053.2008.00033.x. [DOI] [PubMed] [Google Scholar]
- 91.Glenton C, Rosenbaum S, Fønhus MS. Checklist and Guidance for disseminating findings from Cochrane intervention reviews. Cochrane, 2019. https://training.cochrane.org/online-learning/knowledge-translation/how-sharecochrane-evidence/dissemination-essentials-checklist. Accessed 16 Sep 2022.
- 92.Hartling L, Gates A, Pillay J, Nuspl M, Newton AS. Development and usability testing of EPC evidence review dissemination summaries for health systems decisionmakers. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018. Report No.: EHC027-EF. [PubMed]
- 93.Informed Healthcare Choices Group. Supporting informed healthcare choices in low-income countries—final report. IHC Update 9 January 2018. https://www.informedhealthchoices.org/wp-content/uploads/2016/08/IHC-Update-9-January-2018.pdf. Accessed 27 Jul 2022.
- 94.Ikirezi A. A qualitative study exploring the suitability of Informed Health Choices resources translated into Kinyarwanda for use in primary schools: Case of Remera Protestant Primary School in Kigali city. A dissertation submitted in partial fulfilment of the requirements for the degree of Master of Public Health in the College of Medicine and Health Sciences, University of Rwanda, 2016. https://www.informedhealthchoices.org/wp-content/uploads/2019/12/IKIREZI-ALINE_masters-thesis_UofRwanda_2019.pdf. Accessed 16 Sep 2022.
- 95.Kerwer M, Chasiotis A, Stricker J, Günther A, Rosman T. Straight from the scientist’s mouth—plain language summaries promote laypeople’s comprehension and knowledge acquisition when reading about individual research findings in Psychology. Collabra: Psychology. 2021;7(1):18898. doi: 10.1525/collabra.18898. [DOI] [Google Scholar]
- 96.Knapp P, Raynor DK, Berry DC. Comparison of two methods of presenting risk information to patients about the side effects of medicines. Qual Saf Health Care. 2004;13(3):176–180. doi: 10.1136/qhc.13.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krause LK, Schwartz L, Woloshin S, Oxman A. Interactive tools to teach the public to be critical consumers of information about health care: what’s out there? Abstracts of the 19th Cochrane Colloquium, Madrid, Spain, 2011, 157. https://www.informedhealthchoices.org/wp-content/uploads/2016/08/4Da-Krause-Interactive-Tools-Poster.pdf. Accessed 16 Sep 2022.
- 98.Kristiansen IS, Gyrd-Hansen D, Nexøe J, Nielsen JB. Number needed to treat: easily understood and intuitively meaningful? Theoretical considerations and a randomized trial. J Clin Epidemiol. 2002;55(9):888–892. doi: 10.1016/s0895-4356(02)00432-8. [DOI] [PubMed] [Google Scholar]
- 99.Lavis JN, Catallo C, Permanand G, Zierler A, BRIDGE Study Team: BRIDGE Summary 1: communicating clearly: enhancing information-packaging mechanism sto support knowledge brokering in European Health Systems. Brussels, Belgium: European Observatory on Health Systems and Policies; 2013. RefT ype: Report. https://www.euro.who.int/__data/assets/pdf_file/0005/195233/Obs-Policy-Summary-7,-Communicating-clearly.pdf. Accessed 16 Sep 2022.
- 100.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making. 2007;27(5):696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 101.Logullo P, Torloni MR, Latorraca CdOC, Riera R. The Brazilian Portuguese version of the DISCERN Instrument: translation procedures and psychometric properties. Value Health Reg Issues. 2019;20:172–179. doi: 10.1016/j.vhri.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 102.Lopez LM, Steiner MJ, Grimes DA, Schulz KF. Strategies for communicating contraceptive effectiveness. Cochrane Database Syst Rev. 2008;(2):CD006964. 10.1002/14651858.CD006964.pub2. Update in: Cochrane Database Syst Rev. 2013;4:CD006964. [DOI] [PubMed]
- 103.Marquez C, Johnson AM, Jassemi S, Park J, Moore JE, Blaine C, et al. Enhancing the uptake of systematic reviews of effects: what is the best format for health care managers and policy-makers? A mixed-methods study. Implement Sci. 2018;13(1):84. doi: 10.1186/s13012-018-0779-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Moberg J, Austvoll-Dahlgren A, Treweek S, Badenoch D, Layfield R, Harbour R, et al. The plain language glossary of evaluation terms for informed treatment choices (GET-IT) at www.getitglossary.org’. Research for All. 2018;2(1):106–121. 10.18546/RFA.02.1.10.
- 105.Moretti A, Gimigliano F, Arienti C, Pollet J, Kiekens C, Negrini S. The cochrane rehabilitation eBook: a knowledge translation tool to transfer evidence to different rehabilitation audiences. Eur J Phys Rehabil Med. 2018;54(5):808–810. doi: 10.23736/S1973-9087.18.05406-0. [DOI] [PubMed] [Google Scholar]
- 106.Mosconi P, Antes G, Barbareschi G, Burls A, Demotes-Mainard J, Chalmers I, Colombo C, Garattini S, Gluud C, Gyte G, Mcllwain C, Penfold M, Post N, Satolli R, Valetto MR, West B, Wolff S. A European multi-language initiative to make the general population aware of independent clinical research: the European Communication on Research Awareness Need project. Trials. 2016;17:19. doi: 10.1186/s13063-015-1146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mugisha M. Piloting primary school teaching resources for informed health care choices in an urban school in Kigali, Rwanda: a qualitative study. A dissertation submitted in partial fulfilment of the requirements for the degree of Master of Public Health in the College of Medicine and Health Sciences, University of Rwanda, 2016. https://www.informedhealthchoices.org/wp-content/uploads/2016/08/IHC_Dissertation_final_Printed_Version_Library_20160728.pdf. Accessed September 16, 2022.
- 108.Murthy L, Shepperd S, Clarke MJ, Garner SE, Lavis JN, Perrier L, et al. Interventions to improve the use of systematic reviews in decision-making by health system managers, policy makers and clinicians. Cochrane Database of Syst Rev. 2012 doi: 10.1002/14651858.CD009401.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nordheim LV, Gundersen MW, Espehaug B, Guttersrud Ø, Flottorp S. Effects of school-based educational interventions for enhancing adolescents abilities in critical appraisal of health claims: a systematic review. PLoS ONE. 2016;11(8):e0161485. doi: 10.1371/journal.pone.0161485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nsangi A, Semakula D, Oxman AD, Austvoll-Dahlgren A, Oxman M, Rosenbaum S, Morelli A, Glenton C, Lewin S, Kaseje M, Chalmers I, Fretheim A, Ding Y, Sewankambo NK. Effects of the Informed Health Choices primary school intervention on the ability of children in Uganda to assess the reliability of claims about treatment effects: a cluster-randomised controlled trial. Lancet. 2017;390(10092):374–388. doi: 10.1016/S0140-6736(17)31226-6. [DOI] [PubMed] [Google Scholar]
- 111.Ongolo-Zogo P, Lavis JN, Tomson G, Sewankambo NK. Initiatives supporting evidence informed health system policymaking in Cameroon and Uganda: a comparative historical case study. BMC Health Serv Res. 2014;14:612. doi: 10.1186/s12913-014-0612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Oxman AD, Glenton C, Flottorp S, Lewin S, Rosenbaum S, Fretheim A. Development of a checklist for people communicating evidence-based information about the effects of healthcare interventions: a mixed methods study. BMJ Open. 2020;10(7):e036348. doi: 10.1136/bmjopen-2019-036348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Oxman AD, García LM. Comparison of the Informed Health Choices Key Concepts Framework to other frameworks relevant to teaching and learning how to think critically about health claims and choices: a systematic review [version 1; peer review: 3 approved]. FResearch 2020; 9:164. 10.12688/f1000research.21858.1. [DOI] [PMC free article] [PubMed]
- 114.Paling J. Strategies to help patients understand risks. BMJ. 2003;327(7417):745–748. doi: 10.1136/bmj.327.7417.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Parmelli E, Amato L, Saitto C, Davoli M; Gruppo di Lavoro "DECIDE Italia. DECIDE: uno strumento per rendere trasparenti i criteri utilizzati per le decisioni in sanità [DECIDE: developing and evaluating communication strategies to support informed decisions and practice based on evidence]. Recenti Prog Med. 2013;104(10):522–31. doi: 10.1701/1349.14997. [DOI] [PubMed]
- 116.Petkovic J, Welch V, Jacob MH, Yoganathan M, Ayala AP, Cunningham H, et al. The effectiveness of evidence summaries on health policymakers and health system managers use of evidence from systematic reviews: a systematic review. Implement Sci. 2016;11:1–14. doi: 10.1186/s13012-016-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Prictor M, Hill S. Cochrane consumers and communication review group: leading the field on health communication evidence. J Evid Based Med. 2013;6(4):216–220. doi: 10.1111/jebm.12066. [DOI] [PubMed] [Google Scholar]
- 118.Puljak L. Using social media for knowledge translation, promotion of evidence-based medicine and high-quality information on health. J Evid Based Med. 2016;9(1):4–7. doi: 10.1111/jebm.12175. [DOI] [PubMed] [Google Scholar]
- 119.Ringle VA. Developing and testing the effects of an educational podcast to improve critical appraisal of healthcare claims. Doctoral dissertation, University of Miami. 2020. https://www.informedhealthchoices.org/wp-content/uploads/2021/08/MoraRingleDissertation2020.pdf. Accessed 16 Sep 2022.
- 120.Robinson EJ, Kerr CE, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, Beck SR, Rowley MG. Lay public's understanding of equipoise and randomisation in randomised controlled trials. Health Technol Assess. 2005;9(8):1–192, iii–iv. doi: 10.3310/hta9080. [DOI] [PubMed] [Google Scholar]
- 121.Rosenbaum SE, Glenton C, Wiysonge CS, Abalos E, Mignini L, Young T, Althabe F, Ciapponi A, Marti SG, Meng Q, Wang J, la Hoz Bradford AM, Kiwanuka SN, Rutebemberwa E, Pariyo GW, Flottorp S, Oxman AD. Evidence summaries tailored to health policy-makers in low- and middle-income countries. Bull World Health Organ. 2011;89(1):54–61. doi: 10.2471/BLT.10.075481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ryan G, Sfar-Gandoura H. Disseminating research information through Facebook and Twitter (DRIFT): presenting an evidence-based framework. Nurse Res. 2018 doi: 10.7748/nr.2018.e1562. [DOI] [PubMed] [Google Scholar]
- 123.Santesso N, Maxwell L, Tugwell PS, Wells GA, O'connor AM, Judd M, et al. Knowledge transfer to clinicians and consumers by the Cochrane Musculoskeletal Group. J Rheumatol. 2006;33(11):2312–2318. [PubMed] [Google Scholar]
- 124.Santesso N, Rader T, Nilsen ES, Glenton C, Rosenbaum S, Ciapponi A, et al. A summary to communicate evidence from systematic reviews to the public improved understanding and accessibility of information: a randomized controlled trial. J Clin Epidemiol. 2015;68(2):182–190. doi: 10.1016/j.jclinepi.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 125.Semakula D, Nsangi A, Oxman AD, Oxman M, Austvoll-Dahlgren A, Rosenbaum S, Morelli A, Glenton C, Lewin S, Kaseje M, Chalmers I, Fretheim A, Kristoffersen DT, Sewankambo NK. Effects of the Informed Health Choices podcast on the ability of parents of primary school children in Uganda to assess claims about treatment effects: a randomised controlled trial. Lancet. 2017;390(10092):389–398. doi: 10.1016/S0140-6736(17)31225-4. [DOI] [PubMed] [Google Scholar]
- 126.Semakula D, Nsangi A, Oxman AD, Oxman M, Austvoll-Dahlgren A, Rosenbaum S, et al. Effects of the Informed Health Choices podcast on the ability of parents of primary school children in Uganda to assess the trustworthiness of claims about treatment effects: one-year follow up of a randomised trial. Trials. 2020;21(1):187. doi: 10.1186/s13063-020-4093-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Semakula D, Nsangi A, Oxman M, et al. Development of mass media resources to improve the ability of parents of primary school children in Uganda to assess the trustworthiness of claims about the effects of treatments: a human-centred design approach. Pilot Feasibility Stud. 2019;5:155. doi: 10.1186/s40814-019-0540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sheridan SL, Pignone MP, Lewis CL. A randomized comparison of patients' understanding of number needed to treat and other common risk reduction formats. J Gen Intern Med. 2003;18(11):884–892. doi: 10.1046/j.1525-1497.2003.21102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.The SHARE Approach—Communicating numbers to your patients: a reference guide for health care providers. Content last reviewed September 2020. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tool/resource-5.html.
- 130.Trevena LJ, Davey HM, Barratt A, Butow P, Caldwell P. A systematic review on communicating with patients about evidence. J Eval Clin Pract. 2006;12(1):13–23. doi: 10.1111/j.1365-2753.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- 131.West African Health Organization (WAHO). Regional evidence-based policy making guidance for ECOWAS countries: process of evidence use in policymaking. Bobo Dioulasso: WAHO, 2021.45 p. 10. 31219/osf.io/xtu4v. https://osf.io/xtu4v/. Accessed 16 Sep 2022.
- 132.Welch VA, Petticrew M, O'Neill J, Waters E, Armstrong R, Bhutta ZA, et al. Health equity: evidence synthesis and knowledge translation methods. Syst Rev. 2013;2:43. doi: 10.1186/2046-4053-2-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wickremasinghe D, Kuruvilla S, Mays N, Avan BI. Taking knowledge users' knowledge needs into account in health: an evidence synthesis framework. Health Policy Plan. 2016;31(4):527–537. doi: 10.1093/heapol/czv079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Woloshin S, Schwartz LM, Ellner A. Making sense of risk information on the web. BMJ. 2003;327(7417):695–696. doi: 10.1136/bmj.327.7417.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Woloshin S, Schwartz LM, Welch HG. Know your chances. Understanding Health Statistics. Berkeley (CA): University of California Press; 2008. ISBN-13: 978-0-520-25222-6. [PubMed]
- 136.Woolf SH, Purnell JQ, Simon SM, Zimmerman EB, Camberos GJ, Haley A, et al. Translating evidence into population health improvement: strategies and barriers. Annu Rev Public Health. 2015;18(36):463–482. doi: 10.1146/annurev-publhealth-082214-110901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zikmund-Fisher BJ, Witteman HO, Fuhrel-Forbis A, Exe NL, Kahn VC, Dickson M. Animated graphics for comparing two risks: a cautionary tale. J Med Internet Res. 2012;14(4):e106. doi: 10.2196/jmir.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zikmund-Fisher BJ. The right tool is what they need, not what we have: a taxonomy of appropriate levels of precision in patient risk communication. Med Care Res Rev. 2013;70(1 Suppl):37S–49S. doi: 10.1177/1077558712458541. [DOI] [PubMed] [Google Scholar]
- 139.Effective Practice and Organisation of Care (EPOC). EPOC Taxonomy; 2015. https://epoc.cochrane.org/epoc-taxonomy. Accessed 27 Jul 2022.
- 140.Willis N, Hill S, Kaufman J, Lewin S, Kis-Rigo J, De Castro Freire SB, Bosch-Capblanch X, Glenton C, Lin V, Robinson P, Wiysonge CS. "Communicate to vaccinate": the development of a taxonomy of communication interventions to improve routine childhood vaccination. BMC Int Health Hum Rights. 2013;13:23. doi: 10.1186/1472-698X-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Escola Nacional de Administração (Enap). Enap ajuda Ministério da Saúde a aperfeiçoar a comunicação de evidências. Notícia publicada em 2 de julho de 2021. https://www.enap.gov.br/pt/acontece/noticias/enap-ajuda-ministerio-da-saude-a-aperfeicoar-a-comunicacao-de-evidencias. Accessed 16 Sep 2022.
- 142.Ministério da Saúde (Brasil). Ministério da Saúde conclui projeto de comunicação de evidências científicas Notícia publicada em 5 de julho de 2021. https://www.ismep.com.br/ministerio-da-saude-conclui-projeto-de-comunicacao-de-evidencias-cientificas/. Accessed 16 Sep 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Strategies of electronic and structured searches.
Additional file 2. Proposed taxonomy to categorize strategies for communicating scientific evidence in health to the population/managers.
Additional file 3. Studies/documents excluded and reasons for exclusions after reading the full text (second phase of the selection process).
Additional file 4. Main characteristics of included studies.
Additional file 5. Main characteristics of the identified strategies or sets of strategies for communicating scientific evidence.
Data Availability Statement
All relevant data is presented as supplementary files.


