Abstract
The increasing prevalence and burden of suicide have led to numerous studies to identify its risk factors. Cannabis is the most common illicit substance detected in suicide victims’ toxicology tests. This study aims to identify and appraise systematic reviews investigating suicidality after using cannabis and cannabinoids. Seven databases and two registries were searched without restrictions for systematic reviews investigating cannabis effects on suicidality. AMSTAR-2 was used for quality assessment and corrected covered area and citation matrix were used to determine overlap. Twenty-five studies were included, of which 24 were on recreational use and one was on therapeutic use. Only three of the studies on recreational use reported no effect or inconsistent results. Evidence generally showed a positive association between cannabis use and suicidal ideation and attempt among the general population, military veterans, and bipolar or major depression patients. A bidirectional causal association between cannabis and suicidal ideation was also mentioned. Moreover, a younger age of initiation, long-term use, and heavy consumption were reported to be associated with even worse suicidal outcomes. On the contrary, current evidence indicates that the therapeutic cannabis is safe. In conclusion, the literature supports the cannabis-suicidality association in recreational use but considers cannabidiol safe for treatment. Further studies with quantitative and interventional approaches are recommended.
Keywords: Marijuana, medicinal cannabis, self injury, substance use disorder, suicidal ideation, systematic review
Introduction
Psychiatric disorders and substance use, in particular, are important risk factors for suicide, especially in young people (Sher and Oquendo 2023), the same age group where suicide is a leading cause of death (Conner and Goldston 2007) and the same group where substance use is prevalent (Welty et al. 2019). The rate of suicidal behaviour in patients with substance use disorder has been reported to be as high as 45% (Ilgen et al. 2010).
Cannabis is the most common illicit substance, about five times more than any other substance, whose regular or heavy uses are also associated with an increased risk of using other illicit drugs (Fergusson et al. 2006; Sideli et al. 2020). Its use is high among adults and young people (Substance Abuse and Mental Health Services Administration 2010; Welty et al. 2019). Moreover, it is the most common illicit substance identified from toxicology tests of people who completed suicide (Darke et al. 2009). Apart from recreational consumption, it is used for therapeutic reasons, which has recently been in the spotlight (Collin et al. 2010; Smith et al. 2017).
The association between cannabis use and suicidal ideation or behaviour has been frequently reported in previous studies - although its nature is not fully understood. So far, numerous systematic reviews have investigated this link, each with its own partial and general aims. Yet, no study has aggregated, categorised, and documented the resulting information and appraised their methodology. This study is the first that systematically identified and evaluated systematic reviews investigating the effects of cannabis in any form for any purpose on suicidality in any type.
Materials and methods
This systematic review of systematic reviews was conducted following all relevant components of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, and its protocol was registered and published in the International Prospective Register of Systematic Reviews (PROSPERO) with the code CRD42022295679.
Search
Regarding the study aim, the following terms were applied to create the search string for obtaining systematic reviews (#1) evaluating the effects of cannabis (#2) use on suicidality (#3).
#1– ‘systematic review’ OR meta-analysis
#2– marijuana OR marihuana OR cannabi* (the wild-card term)
#3– suicid* (the wild-card term)
The intersection of these three formed the final search strategy. No MeSH-based terms were used. To obtain the needed information, AS searched Web of Science, Scopus, CINAHL Plus, PsycINFO, Embase, PubMed, and Cochrane Library electronic databases on 31 August 2022, without any restrictions on language, timespan, publication status, and document type. The searched string in each database is given in Supplementary Appendix 1, mentioning the specific fields of each.
Searching the registries of systematic reviews (PROSPERO and Research Registry), asking an expert, and reviewing the references of the included studies were additional sources. In order to consider their results, the two conditions of relevance and non-duplication were placed.
Eligibility
Duplicate citations were removed using EndNote 20. AS and AA performed the screening and full-text assessment independently, and any discrepancy was resolved in a discussion.
Inclusion criteria were as follows: (i) being a systematic review with or without meta-analysis; (ii) being published as a full paper in a peer-reviewed journal; (iii) using the mentioned search terms in the title, abstract, or keywords; (iv) investigating the effects of cannabis on suicidality; and (v) investigation of indexed publications on humans. In this study, the studies included in the included studies are called indexed publications.
The following criteria led to exclusion: (i) lack of clear distinction between preclinical and human studies (if both were included); (ii) being a conference or meeting abstract; (iii) lack of clear methodology reporting; (iv) including less than two indexed publications with necessitated characteristics. Item iv meant that at least two indexed publications on humans investigating suicidality after using cannabis must be included in an eligible study. In other words, including other substances or interventions was not an exclusion reason. No restrictions were placed on the type of cannabis use, whether recreational or therapeutic, and suicide type. Also, language was not a criterion for exclusion.
Data extraction
KP and AA independently and in parallel extracted data from the included studies - not indexed publications - using Review Manager 5.4. Through discussion, the discrepancies were brought to a consensus.
The following data were extracted from each included study: inclusion criteria and the approach of each of the included studies (interventional, observational, or both indexed publications), the number of indexed publications, the number of relevant indexed publications (i.e., investigating the main outcome of this study) and their first authors and publication years, the study type of each relevant indexed publication, the number of indexed publications investigating suicidal ideation/plan/attempt/completion, characteristics of participants enrolled, number of participants (in case of meta-analysis), male and female percentages (in case of meta-analysis), type of intervention or exposure, monotherapy or combination therapy (in interventional types), standardisation (in herbal types), dosage, control group characteristics, duration of follow-up, investigated outcomes, analysis results (in case of meta-analysis), how to assess the bias risk of indexed publications, limitations of the included studies, adverse events other than suicidality (in interventional types), final conclusion, and funding. A formal narrative synthesis was conducted. The primary outcome was the final conclusion of the effects of cannabis use (in any form) on suicidality (by any definition).
If needed, the corresponding authors of the included studies were contacted for additional data.
Quality assessment
AH and AA independently and in parallel reviewed the included studies to assess their quality. The second version of a measurement tool to assess systematic reviews (AMSTAR-2) was applied to appraise the quality of the included studies (Shea et al. 2017). This tool comprises seven major and nine minor items and categorises systematic reviews into four quality classes, including critically low (with more than one major flaw), low (with only one major flaw, irrespective of minor flaws), medium (without any major flaws and more than one minor flaw), and high (without any major flaws and with no or only one minor flaw).
Overlap
As a representation of overlap in the included studies, the corrected covered area (CCA) was calculated according to the formula provided by Pieper et al. Also, the same overlap thresholds in the interpretation of results were used (0–5%: slight, 6–10%: moderate, 11–15%: high, and >15%: very high) (Pieper et al. 2014). In addition, pairwise CCA tables were designed to address the overlap between every two reviews. A citation matrix was also provided to represent overlap visually (Thabet et al. 2021).
Results
Search and selection
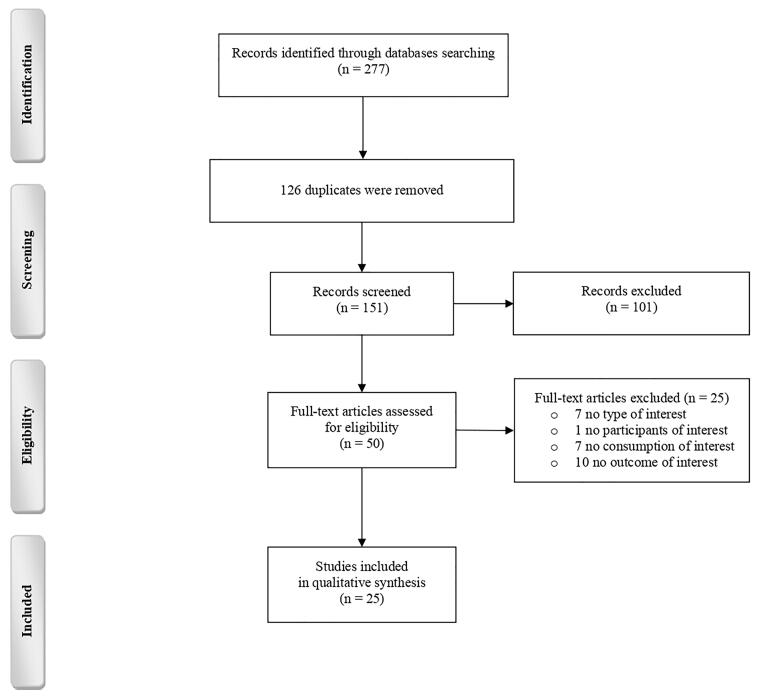
Figure 1 depicts the information flow diagram through different phases of the study. A total of 277 citations were obtained from electronic databases, the breakdown of which is reported in Supplementary Appendix 1. After removing duplicates, 101 studies were excluded in the screening phase because they were editorials, conference abstracts, study protocols, non-systematic reviews, or erratum of systematic reviews or did not clearly address the topic of interest. In addition, another 25 studies were excluded in the full-text assessment phase, the reasons for which are given in Supplementary Appendix 2.
Figure 1.
Flow diagram of the study.
As shown in Table 1, the included studies were published between 2004 and 2022, with twelve reviews conducting meta-analyses. A wide range of participants, including the general population, adolescents and early adult populations, military veterans, and patients with bipolar disorder (BD), major depressive disorder (MDD), substance use disorder, and epileptic disorder, were studied in the reviews. The number of eligible publications in each review ranged from two to 37, with controlled or uncontrolled observational studies being the most prevalent. Randomised clinical trials were only included in two reviews. Outcomes, i.e., suicidal ideation and behaviours, were evaluated using various methods such as questionnaires, direct interviews, and medical record inquiries.
Table 1.
Characteristics of the included studies.
| Study | Interventional /Observational (I, O, I/O) | Total number of studies (any existing irrelevant study included) | Relevant studies (study designs) | Number of studies on suicide ideation/attempt/ (unspecified) | Included population (number of participants) | Intervention (or exposure) | Control | Outcome | Effect direction (I (intervention) or C), and effect size (if meta-analysis) | Limitations | Funding | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Carvalho et al. 2022) | O | 22 | 22 (22 Coh) | 15/18 | Only populations with specific psychiatric disorders were excluded. | Cannabis use | NR | NR | NR | Not including a meta-analysis of the selected articles, only outcomes associated with suicidal behaviour were analysed, restricting the observations about outcomes such as depression, no studies regarding synthetic cannabinoids were included, and studies from developed and English-speaking countries were over-represented. | None | The relationship between cannabis use and suicidal behaviour is both complex and controversial, with no clear consensus in the literature. The existence of numerous confounding variables, such as the difficulty in accurately measuring cannabis use and the intensity of suicidal behaviour make it difficult to establish a causal relationship. Moreover, these variables are unlikely to be responsible for the entire association found. |
| (Fresán et al. 2022) | O | 20 | 20 (13 CS, 5 longitudinal, 1 retrospective, 1 Coh) | 12/16 | Young individuals aged 11–21 years (316,645) | Cannabis smoking | Non-cannabis smoker adolescents | Suicide attempt, ideation, or planning | Suicide ideation: OR: 2.04, 95%CI: 1.64–2.53, Z p value: <0.001, I2: 94.88%; suicide attempt: OR: 2.33, 95%CI: 1.78–3.05, Z p value: <0.0001, I2 = 97.12%; suicide plan: OR: 1.674, 95%CI: 1.554–1.804, Z p value: 0.000, I2: 92.609 | Low number of included studies, no evaluation for other endophenotypes such as gender and age of cannabis use onset, and unspecific definition for cannabis use. | None | Young individuals who smoke cannabis show a higher risk of presenting suicidal ideation, suicide planning or suicide attempts. Young individuals in France, USA, and Canada, who smoke cannabis showed a greater association with suicide behaviours. |
| (Tourjman et al. 2023) | O | 56 | 10 (9 retrospective, 1 meta-analysis) | 1/5/(4) | BD and MDD patients | NR | NR | NR | NR | Retrospective study designs, unclear definitions for cannabis use and suicidality, and undetermined cannabis content in included studies. | Multiple funding sources were reported. | CU is associated with increased suicidality in both BD and MDD, which may represent a correlation of CU with suicidality. |
| (Armoon et al. 2021) | O | 48 | 10 (10 CS) | 7/5 | SUD patients (IDU and DU) | CUD | NR | Suicide attempt | Suicide ideation: OR: 1.71, 95%CI: 1.37–2.14; suicide attempt: 2.01, 95%CI: 1.01–4.01 |
Low number of included studies, high heterogeneity, studies were mostly CS, and the gender groups were not separated. | None | Cannabis abuse was detected as a risk factor associated with suicidal ideations in SUD population. |
| (Bahji et al. 2021) | O | 48 | NR | NR | BD patients | CUD | BD patients without CUD | Lifetime suicide attempts | OR: 2.74, 95%CI: 1.39–5.39, k = 6, I2 = 89.1% | High heterogeneity, imprecision, and publication bias. Polysubstance use may have confounded the assessment of CUD effects. | NR | CUD comorbidity affects up to one quarter of all BD patients and may be associated with adverse effects in the course of BD, such as suicide attempts. |
| (Chiappini et al. 2021) | O | 16 | 13 (3 case report, 8 retrospective, 1 Coh, 1 case-control) | 2/12 | NS | Synthetic cannabinoid use | NR | Suicidality | NR | A limited number of studies were included, probable publication bias, mostly no reliable measure of consumed drug is available, and concentrations could not be established. | None | Although the long-term risks of synthetic cannabinoids are still unclear, some studies suggest the possibility of inducing chronic psychotic symptoms and worsening underlying psychiatric illness. Also, the toxic effects of synthetic cannabinoids appear more severe and diverse than those associated with cannabis. |
| (Escelsior et al. 2021) | O | 37 | 9 (3 CS, 4 Coh, 2 case report) | 0/0/(9) | NS | Cannabis use | NR | Self-harm indicated by: Direct question, Suicidal Behaviours Questionnaire-Revised, or Clinical data | CS: OR: 1.569,95%CI: 1.167–2.108; longitudinal: OR: 2.569, 95%CI: 2.207–3.256 |
Less than a third of included studies had a Coh design, while the vast majority were CS or anecdotical reports, and few other studies have open label or case-control design. Results of the meta-analysis of CS studies, in particular, were affected by publication bias; thus, may not generalise broadly. Moreover, few studies were able to robustly control for the presence of confounding factors, most notably polysubstance use. | None | Cannabis use is significantly associated with self-injurious behaviours both at the CS and longitudinal level. |
| (Klein et al. 2021) | I | 19 | 2 (2 RCT) | 2/2 | Epileptic patients (291) | Cannabidiol treatment | Epileptic patients receiving placebo | Suicidal Ideation or attempt (based on C-SSRS). | Suicidal ideation: risk ratio: 0.98, 95%CI: 0.06-15.49; suicidal attempt: risk ratio: 0.98, 95%CI: 0.06–15.49 |
Limited sample size, cannabidiol was mostly tested in children, who have lower suicide risks, insufficient data to evaluate whether ASMs affect suicidality in high-risk individuals, and suicidality was analysed based on non-standardised reports of adverse events. | Multiple funding sources were reported. | Cannabidiol had no associated suicidality. |
| (Rioux et al. 2021) | O | 25 | 5 (3 prospective, 2 longitudinal) | 3/5 | Youth aged 25 or younger (7644) | CUD | Youth without SUD | Suicidal ideation, attempt, or general behaviour (based on interviewing adolescent, interview parent, or self-report). | SPDH: OR: 3.20, 95%CI: 1.42–7.20; SSUDH: OR: 3.31, 95%CI: 1.40–7.79 |
Some moderation analyses did not include all studies, and were thus underpowered. Over half of the studies for the SPDH and a fourth of the studies for the SSUDH were of poor quality according to the Newcastle Ottawa criteria. The majority of studies were from the western world and there were no studies from South America and Africa. | NR | SUDs and suicidality in youth likely influence each other, an effect that was significant for alcohol and drugs, as well as suicidal ideation and attempts. |
| (Turna and MacKillop 2021) | I/O | 86 | 5 (3 CS, 1 longitudinal, 1 meta-analysis) | 1/5 | Military veterans (4866930) | Cannabis dependence or CUD | Veterans without CUD | Suicidal injury, ideation, attempt, or completion | NR | Female population was under represented, very few studies on suicidal behaviour were included, and veterans from other nations were not included. | Michael G. DeGroote Centre for Research | CUD is associated with suicidal behaviour in military veterans. |
| (Campeny et al. 2020) | I/O | 44 | 4 (4 systematic review) | 3/3 | NS | Cannabis use | Non-cannabis users | NR | NR | All recent articles were not possibly included, most studies did not provide results by gender, and dose and frequency of cannabis use were not determined in all studies. | Multiple funding sources were reported. | Cannabis use has an impact on suicidal behaviour. |
| (Schmidt et al. 2020) | O | 12 | 12 (7 CS, 3 longitudinal, 1 review, 1 letter) | 6/11/(2) | Adolescents aged 13-18 years | Cannabis use | Non-cannabis users | NR | NR | Low number of included studies and probable publication, interpretation, and dissemination bias. | NR | Cannabis use is associated with suicidal behaviour in adolescents. |
| (Bartoli et al. 2019) | O | 13 (11 quantitative synthesis) | 13 (11 CS, 2 Coh) | 0/13 | BD patients (6375) | CUD | BD patients without CUD | Suicide attempts | OR for CS association between CUD and suicide attempts: 1.35, 95%CI: 1.08–1.70 | Due to the CS design of included studies, causal inferences could not be explored and number of studies reporting prospective data was not enough for a meta-analysis. | None | The meta-analysis estimated a weak but noteworthy association between cannabis use disorder and suicidal attempts in subjects with BD. |
| (Gobbi et al. 2019) | O | 35 (11 quantitative synthesis) | 8 (6 prospective cohort in meta-analysis) | 6/6 | Adolescents | Cannabis use | Non-cannabis users | Questionnaires and/or standardised interview assessment or scales | Suicidal ideation: OR: 1.50, 95%CI: 1.11–2.03; suicidal attempt: OR: 3.46, 95%CI: 1.53–7.84 |
Analyses made in the included longitudinal studies did not allow causal inferences. Exact quantity of cannabis consumed was not determined. Potency of cannabis may vary across geographic locations. | Multiple funding sources were reported. | Cannabis use in adolescence had a significant association with suicidal ideation or attempts. |
| (Karanikola et al. 2019) | O | 20 | 4 (4 CS) | 2/3 | School students | Illegal cannabis use | Non-cannabis users | NR | NR | Majority of studies were CS, students were of a wide age range, confounding risk factors were not included in some studies, and lack of consistency in the frequency and severity of substance use. | Partially funded by Cyprus University of Technology. | It is possible that female school students are more vulnerable to the adverse effects of cannabis use on suicidal behaviour, or female school students use cannabis as a self-regulatory coping strategy against suicidality more frequently than males. |
| (Pinto et al. 2019) | O | 53 | 6 (6 CS) | 0/6 | BD patients | Cannabis use and CUD | Non-cannabis user BD patients | Suicide attempts | Suicide attempt: ES: 1.37, 95%CI: 1.11-1.67 |
Only CS studies were included (risk of memory bias) and heterogeneity among studies. | Multiple funding sources were reported. | Cannabis use and CUD, as prevalent comorbidities in BD patients, are correlated with negative clinical correlates such as suicide. |
| (Breet et al. 2018) | O | 108 | 10 (1 on cannabis with mandrax as well) | 6/8 | Populations from low- and middle-income countries | Pathological and non-pathological cannabis use | Non-users | Suicide ideation and behaviour | NR | Probable publication bias (only English studies from 2006 to 2016 + null studies usually unpublished). | Medical Research Council and the National Research Foundation (NRF) | Substance use is associated with increased risk of suicide ideation and behaviour. Although contradicting results were present, most of the studies showed a positive association between cannabis use and suicidality. |
| (Tait et al. 2016) | O | 106 | 5 | 1/0/(4) | NS | Any synthetic cannabinoid use | – | Self-injury | NR | Differences among compounds in the class were difficult to assess, and many of the cases depended upon self-report of the patients. | Multiple funding sources were reported. | Use of synthetic cannabinoids was associated with suicidality in some cases. |
| (Borges et al. 2016) | O | 44 | 44 | 13/36 | General (NS) | Acute /chronic cannabis use | General | Suicide ideation, attempt, and completion | Any cannabis use and suicide ideation: OR: 1.43, 95%CI: 1.13–1.83; heavy cannabis use and suicide ideation: OR: 2.53, 95%CI: 1.00–6.39; any cannabis use and suicide attempt: OR: 2.23, 95%CI:1.24–4.00; heavy cannabis use and suicide attempt: OR: 3.20, 95%CI:1.72–5.94 |
Heterogenous measurements of cannabis exposure and lack of systematic control for known risk factors. | NR | There is lack of evidence showing that acute cannabis use increases imminent risk for suicidality. The evidence tends to support that chronic cannabis use can predict suicidality. |
| (Schaffer et al. 2015 | O | 34 | 4 | 0/4 | BD patients aged more than 13 | Any cannabis use | BD patients | Suicide attempt / death | Any cannabis use and suicide attempts: OR: 1.29, 95%CI: 0.85–1.94 |
Number of studies included regarding cannabis use was limited. | Brenda Smith Bipolar Disorder Research Fund Sunnybrook Health Sciences Centre University of Toronto |
Cannabis use was not associated with suicide attempts in BD patients. |
| (Carrà et al. 2014) | O | 29 | 4 | 0/4 | BD patients (3,439) | CUD | BD patients without CUD | Suicide attempt | OR for association between CUD and suicide attempt in BD patients: 1.44, 95%CI: 1.07–1.94 |
Limited number of included studies on cannabis use, the effects of the number and the type of suicide attempts was not investigated, the studies included were mainly CS, only the presence or absence of a suicide attempt and not the number of suicide attempts was investigated, and information on the type of suicide attempt was not presented. | None | Cannabis use can have serious consequences in terms of suicide attempts for individuals with BD. |
| (Serafini et al. 2012) | O | 45 | 45 (4 review, 22 CS, 11 retrospective, 6 longitudinal, 1 pilot, 1 case report) | 23/36/(4) | General population | Cannabis use | NR | Suicidal behaviour | NR | Due to the high heterogeneity of individual data, a meta-analysis was not performed. | NR | Cannabis use was a relevant but not a robust risk factor associated with both suicidal attempts and behaviours in psychotic and non-psychotic samples. Cannabis use cannot be identified as the only causal risk factor involved in increasing suicidal risk in psychosis. |
| (Calabria et al. 2010) | O | 19 | 4 (2 case-control, 2 Coh) | 2/4 | NS | Heavy or light cannabis use | NR | Suicidal behaviour | – | Limited sample size, diverse exposure and outcome measures, and potential confounding variables that are strongly related to suicide were not controlled for (namely, depression and alcohol use). | NR | Association of cannabis use and suicidal behaviour was significant, but of uncertain interpretation because potential confounding variables that are strongly related to suicide were not controlled for (namely, depression and alcohol use). |
| (Moore et al. 2007) | O | 35 | 8 (8 Coh) | 8/5 | NS | Ever used before 16, used more than 40 occasions, cannabis misuse disorder | NR | Suicide ideation or attempt | – | Including only observational studies, limited sample size, and excluding populations with comorbid mental illnesses or SUDs. | Multiple funding sources were reported. | A consistent association between cannabis use and psychotic symptoms, including disabling psychotic disorders, was found. The possibility that this association results from confounding factors or bias could not be ruled out. |
| (Macleod et al. 2004) | O | 48 | 4 (2 longitudinal, 2 follow up) | 4/2 | General population aged less than 15 | Cannabis use | NR | Report of suicidal thoughts | NR | Limited sample size and including outdated studies. | UK Department of Health, Drug Misuse Research Initiative | No strong evidence was found to suggest that use of cannabis in itself has important consequences for psychological or social health. |
BD: bipolar disorder; CI: confidence interval; Coh: cohort; CS: cross-sectional; C-SSRS: Columbia Suicidality Severity Rating Scale; CU: cannabis use; CUD: cannabis use disorder; DU: drug user; ES: effect size; IDU: injection drug user; MDD: major depressive disorder; NR: not reported; NS: not specified; OR: odds ratio; RCT: randomised controlled trial; SPDH: secondary psychiatric disorder hypothesis; SSUDH: secondary substance use disorder hypothesis; SUD: substance use disorder.
Methodological quality
As depicted in Supplementary Appendix 3, all included studies had at least one major flaw; consequently, no high-quality nor medium-quality reviews were found based on the AMSTAR-2. Twenty reviews were critically low quality, and the other five were low quality. Only four studies provided a list of excluded studies (Item 7; major flaw); none were among the five studies with a published protocol before conducting the study (Item 2; major flaw). Nine studies did not assess the risk of bias (Item 9; major flaw), and 11 did not include it in their interpretation (Item 13; major flaw). Additionally, no reviews reported the funding sources of the included studies (Item 10; minor flaw).
Overlap
Regardless of the exact definition (attempt or ideation), suicidality was reported in 25 studies, one of which did not provide the included publications (Bahji et al. 2021). Hence, the overlap was calculated in 24 studies with a total of 191 indexed publications. The overlap of included studies was slight, with a CCA of 1.82%. A visual representation of the overlap is demonstrated in the citation matrix (Supplementary Appendix 4) and pairwise CCA table (Supplementary Appendix 5).
Suicidal ideation
Cannabis effects on suicidal ideation were investigated in 18 studies, six of which included quantitative syntheses. Sixteen studies had critically low quality based on the AMSTAR-2 checklist.
Meta-analyses indicated significant associations between cannabis use and the risk of suicidal ideation in the general population, adolescents, and substance use disorder patients. A bidirectional association (Rioux et al. 2021) and a higher risk for heavy users (Borges et al. 2016) were also reported. A meta-analysis on epileptic patients (Klein et al. 2021) was the only one suggesting opposing results; however, it acquired wide confidence intervals (CIs) (risk ratio: 0.98, CI: 0.06–15.49).
This association was supported by most qualitative reviews in the general population, adolescents, military veterans, and MDD and BD patients. Additionally, a possible association between suicidal ideation and synthetic cannabinoids was reported (Chiappini et al. 2021). However, two studies described nonconclusive results, primarily due to insufficient control for potential confounding variables (Calabria et al. 2010; Carvalho et al. 2022). Only one review reported no firm evidence of important psychological health consequences (including suicidality) following cannabis use (Macleod et al. 2004).
Suicidal attempt
Twenty-three reviews investigated the effects of cannabis on suicidal attempts, with 11 including meta-analysis in their report. Only five studies were of low quality when assessed by the AMSTAR-2 checklist.
Meta-analyses indicated significant associations between cannabis use and suicidal attempts in the general population and adolescent users. Similar results were also obtained from most studies on BD patients, although two out of five studies concluded non-significant associations (Schaffer et al. 2015; Pinto et al. 2019). A high odds ratio (OR) of 3.20 (CI: 1.72–5.94) for heavy cannabis uses and suicidal attempts in the general population was suggestive of a dose-response relationship (Borges et al. 2016). In contrast, a study regarding cannabidiol use on epileptic patients did not report a significant relationship (Klein et al. 2021).
Studies with qualitative synthesis backed these findings. Reviews on the general population, adolescents, and military veterans mostly favoured the cannabis-suicidal attempt association. Only one was concerned with synthetic cannabinoids (Chiappini et al. 2021). Several studies could not confirm a robust association, mostly due to insufficient control of confounding factors (Macleod et al. 2004; Calabria et al. 2010; Carvalho et al. 2022). Cannabis use in military veterans and BD and MDD patients was also associated with suicidal attempts, though the evidence for MDD was less consistent.
Unspecified suicidality
Two of the reviews were not easily categorizable. One study on synthetic cannabinoids reported some patients with suicidality after using synthetic cannabis without a clear conclusion on the association (Tait et al. 2016). The other study found a significant association between cannabis use and self-injurious behaviours, regardless of intent, indicating a higher likelihood of self-injurious behaviours among cannabis users than non-users (Escelsior et al. 2021).
Mediating factors
Gender
While some studies found no significant gender difference in the effects of cannabis on suicidality (Bartoli et al. 2019; Fresán et al. 2022), others demonstrated a predominance in males (Karanikola et al. 2019; Turna and MacKillop 2021) or females (Tourjman et al. 2023). Such opposing results limit a robust conclusion.
Age
One review on adolescents reported that suicidal attempts and ideations had higher ORs in both genders who started cannabis use before the age of 13 compared to older counterparts (Karanikola et al. 2019). Additionally, a meta-regression revealed that age was negatively associated with the suicide attempt (Fresán et al. 2022). Overall, the literature suggests that younger cannabis users are at higher risk of suicidal behaviours (Gobbi et al. 2019).
Duration of use
Although acute and long-term effects of cannabis use on suicidality were not compared in most reviews, studies attempting this comparison support the hypothesis that cannabis effects on suicidality are duration-dependent, as chronic cannabis use may predict suicidality (Borges et al. 2016; Escelsior et al. 2021).
Co-occurring illnesses
Cannabis consumption may increase the severity of co-occurring psychiatric illnesses like BD and MDD. Increased depressive or psychotic symptoms may mediate the effects of cannabis on suicidality in these individuals (Tourjman et al. 2023, Bahji et al. 2021). Psychotic and non-psychotic cannabis consumers are 2.6 and 1.7 times more likely to attempt suicide, respectively (Serafini et al. 2012). Still, many studies show a stable association between suicidal behaviour and cannabis consumption, even after adjusting for psychiatric illnesses (Turna and MacKillop 2021; Serafini et al. 2012).
In addition, cannabis users may consume alcohol or other drugs, which may affect suicidal behaviour. It is markedly important since the risk of alcohol and substance use disorders increases with cannabis use (Tourjman et al. 2023). Nevertheless, most studies controlling their outcomes for alcohol or non-cannabis substance use disorders have demonstrated a stable association between cannabis use and suicidal behaviour (Carvalho et al. 2022; Turna and MacKillop 2021; Borges et al. 2016).
Interestingly, the effects of cannabis consumption on depression showed a higher susceptibility in females (Gobbi et al. 2019), suggesting different mediating mechanisms for suicidal behaviours in males and females.
Others
Valuable evidence exists for other factors, such as impulsivity, history of childhood sexual abuse, post-traumatic stress disorder (PTSD), combat exposure in military veterans, and non-cannabis substance use disorders. Most studies did not adjust their final results based on these covariates; however, cannabis use was associated with suicidal behaviours even after adjusting for these covariates in one study (Turna and MacKillop 2021).
An effect for cannabis intoxication was not reported in the included reviews, while one argued that synthetic cannabinoids are more potent in causing toxic effects (Chiappini et al. 2021).
Cross-sectional versus longitudinal data
A meaningful association between cannabis use and suicidal attempts was reported using cross-sectional data on BD patients, while the number of longitudinal studies was insufficient for a meta-analysis (Bartoli et al. 2019). In addition, all cross-sectional and longitudinal studies in a qualitative synthesis favoured an increased risk of prospective suicidal behaviour in non-psychotic samples (Serafini et al. 2012). Overall, the direction of the cannabis-suicidality association was similar in cross-sectional and longitudinal studies, while comparing the effect sizes was not feasible applying the current data.
Discussion
Many included studies indicated that cannabis increases the risk of suicidal ideation or attempt. No definite pathway clarifies this relationship, but two probable mechanisms are closer to the truth: neurophysiological (direct) and social (indirect). The direct mechanism acts on the serotonin pathway and induces depressive disorders through tetrahydrocannabinol (Degenhardt et al. 2003). Another possible direct mechanism is acute cannabis intoxication and subsequent cognitive impairment (Whitlow et al. 2004), similar to a schizophrenic patient (Solowij and Michie 2007). The indirect pathway is mainly due to associations between cannabis use and behavioural problems like educational failures (Lynskey and Hall 2000) and psychosocial adjustments (Fergusson et al. 2002).
A group of neuro-pharmacological and genetic mechanisms is implicated in cannabis use, MDD, and suicidal ideation or attempt. A study on twins who differed in their cannabis use or when they started using it found that cannabis use increased the risk of suicidal ideation and attempts among users, but cannabis dependence was associated only with elevated risks of MDD in dizygotic twins compared to monozygotic twins (Lynskey et al. 2004). These findings indicated that in addition to genetic processes, environmental factors are also influential in cannabis complications. Another study showed that the incidence of depressive disorders caused by cannabis would occur in the presence of the 5-HTTLPR genotype (Otten and Engels 2013), while other studies showed that NCAM1, CADM2, SCOC, and KCNT2 genes were related to cannabis use over the life (Stringer 2016). Additionally, the role of chromosome 21 in cannabis use and the role of a pleiotropy localised to a region on chromosome 11q23 in a genetic correlation between cannabis use and MDD have been shown in Mexican Americans (Hodgson et al. 2017).
Various studies observed gender differences in the cannabis-suicidality association; however, the findings were insufficient for a definitive conclusion. Some findings indicated that females are more vulnerable to the suicidal effects of cannabis (Karanikola et al. 2019) because social pressures have a greater impact on suicidal behaviours among women who consume cannabis. Moreover, hormonal changes and menstrual cycles can put women at greater risk (Chapman et al. 2017). Also, the politics of legalising cannabis use has caused the growth of cannabis use among females to be higher than that of males (Shi et al. 2015).
The effects of age are undeniable in the cannabis-suicidality association. Younger cannabis use onset is associated with a higher prevalence of suicidal ideation and attempts. On the other hand, using cannabis during adolescence increases the risk of suicide in adulthood. Of course, cannabis consumption is higher in adolescents than adults (Fergusson et al. 2002). Regarding the pathophysiology, studies suggested different possible causes. The first reason is that people are probably more vulnerable to the toxic effects of drugs during puberty, so they have fewer inhibitory mechanisms and, at the same time, higher impulsivity (De Wit 2009). On the other hand, teenagers who pursue illegal drugs probably have greater problems in school and interpersonal relationships (Conner and Goldston 2007). Although the prevalence of depression is higher in this group, and also depression has an important effect on the occurrence of suicidal ideations or attempts, studies have shown that the relationship between cannabis use and suicide can be independent of depression (Weeks and Colman 2017). So, decision makers need to pay more attention to cannabis use in schools, especially among females.
Most studies on the therapeutic effects of cannabis have also investigated its side effects as a secondary outcome. These studies indicated that following the therapeutic use of cannabis, the risk of suicidality is lower than that of recreational use (Collin et al. 2010; Smith et al. 2017). The entry of higher doses into the body following recreational consumption than therapeutic use can explain this difference.
Acute cannabis use (less than 24 h) may even protect against suicide (Bagge and Borges 2017), probably due to the euphoria caused by using. However, following the onset of withdrawal symptoms of cannabis, suicidal ideation and attempt increase (Rudd et al. 2006; Crean et al. 2011). Nevertheless, many studies indicated that chronic cannabis use is associated with an increased risk of suicide (Fergusson et al. 2002; Kung et al. 2003).
A point to consider is the effect of legalising the recreational use of cannabis in some countries. The results of studies in this field are heterogeneous as suicide deaths following cannabis use decreased from 20 to 40 years old in a study (Mark Anderson et al. 2015), but deaths among teenagers and early adults in Washington state increased in another (Doucette et al. 2021).
Limitations
Despite the significant advantages of this study, including the recentness of the search, comprehensiveness, and precise and clear categorisation, some limitations need to be mentioned and explained. The first limitation is the heterogeneity, which was predictable due to the comprehensiveness. In other words, in this study, there was no restriction for indexed publications, and also, systematic reviews that investigated the primary outcome of this study as a ‘secondary’ outcome and included a small number of related indexed publications were included. Second, the quality of studies during synthesis and interpreting the results was not a decisive item, which of course, was because none of the included studies were of high quality according to the AMSTAR-2, as described earlier.
Conclusion
This study comprehensively included previous systematic reviews, each of which had smaller aims and scopes, and reviewed the evidence of the cannabis-suicide association. Cannabis use was associated with a higher rate of suicidal ideation and attempts in various populations, including BD and MDD patients, military veterans, and the general population. Evidence for a causal relationship was mentioned in one study for suicidal ideation. Additionally, some studies showed that heavy and long-term cannabis use was associated with worse suicidal outcomes. There was no robust consensus in the literature on gender differences. The overall qualities of the included systematic reviews were critically low to low, and their overlap was slight. Not publishing a protocol before conducting the review, not justifying the exclusions, and not considering the risk of bias in interpreting the results were the most important methodological flaws of the included studies. As a result, further high-quality studies with quantitative and interventional approaches are required to draw a more robust conclusion.
Supplementary Material
Acknowledgments
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
AS: conceptualisation, project administration, supervision, methodology, protocol registration, software, data curation, writing – original draft, writing – review and editing. AA: supervision, software, data curation, writing – original draft, writing – review and editing. KP: data curation, investigation, writing – original draft, writing – review and editing. AH: data curation, investigation, writing – original draft. HA: writing – original draft, writing – review and editing. All authors approved the final version of the manuscript and had accountability for all work aspects.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
No data were created or analysed except as fully presented in the full text and appendices.
References
- Armoon B, SoleimanvandiAzar N, Fleury M-J, Noroozi A, Bayat A-H, Mohammadi R, Ahounbar E, Fattah Moghaddam L.. 2021. Prevalence, sociodemographic variables, mental health condition, and type of drug use associated with suicide behaviors among people with substance use disorders: a systematic review and meta-analysis. J Addict Dis. 39(4):550–569. doi: 10.1080/10550887.2021.1912572. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Borges G.. 2017. Acute substance use as a warning sign for suicide attempts: a case-crossover examination of the 48 hours prior to a recent suicide attempt. J Clin Psychiatry. 78(06):691–696. doi: 10.4088/JCP.15m10541. [DOI] [PubMed] [Google Scholar]
- Bahji A, Danilewitz M, Vazquez G, Patten S.. 2021. The prevalence of cannabis use disorder comorbidity in individuals with bipolar disorder: a systematic review and meta-analysis. Canadian J Addict. 12(3):22–38. doi: 10.1097/CXA.0000000000000123. [DOI] [Google Scholar]
- Bartoli F, Crocamo C, Carrà G.. 2019. Cannabis use disorder and suicide attempts in bipolar disorder: a meta-analysis. Neurosci Biobehav Rev. 103:14–20. doi: 10.1016/j.neubiorev.2019.05.017. [DOI] [PubMed] [Google Scholar]
- Borges G, Bagge CL, Orozco R.. 2016. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 195:63–74. doi: 10.1016/j.jad.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Breet E, Goldstone D, Bantjes J.. 2018. Substance use and suicidal ideation and behaviour in low- and middle-income countries: a systematic review. BMC Public Health. 18(1). doi: 10.1186/s12889-018-5425-6. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5425-6#citeas [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabria B, Degenhardt L, Hall W, Lynskey M.. 2010. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 29(3):318–330. doi: 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- Campeny E, López-Pelayo H, Nutt D, Blithikioti C, Oliveras C, Nuño L, Maldonado R, Florez G, Arias F, Fernández-Artamendi S, et al. 2020. The blind men and the elephant: systematic review of systematic reviews of cannabis use related health harms. Eur Neuropsychopharmacol. 33:1–35. doi: 10.1016/j.euroneuro.2020.02.003. [DOI] [PubMed] [Google Scholar]
- Carrà G, Bartoli F, Crocamo C, Brady KT, Clerici M.. 2014. Attempted suicide in people with co-occurring bipolar and substance use disorders: systematic review and meta-analysis. J Affect Disord. 167:125–135. doi: 10.1016/j.jad.2014.05.066. [DOI] [PubMed] [Google Scholar]
- Carvalho JV, Souza LS, Moreira EC.. 2022. Association between cannabis use and suicidal behavior: a systematic review of cohort studies. Psychiatry Res. 312:114555. doi: 10.1016/j.psychres.2022.114555. [DOI] [PubMed] [Google Scholar]
- Chapman C, Slade T, Swift W, Keyes K, Tonks Z, Teesson M.. 2017. Evidence for sex convergence in prevalence of cannabis use: a systematic review and meta-regression. J Stud Alcohol Drugs. 78(3):344–352. doi: 10.15288/jsad.2017.78.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiappini S, Mosca A, Miuli A, Santovito MC, Orsolini L, Corkery JM, Guirguis A, Pettorruso M, Martinotti G, Di Giannantonio M, et al. 2021. New psychoactive substances and suicidality: a systematic review of the current literature. Medicina. 57(6):580. doi: 10.3390/medicina57060580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin C, Ehler E, Waberzinek G, Alsindi Z, Davies P, Powell K, Notcutt W, O'Leary C, Ratcliffe S, Nováková I, et al. 2010. A double-blind, randomized, placebo-controlled, parallel-group study of Sativex, in subjects with symptoms of spasticity due to multiple sclerosis. Neurol Res. 32(5):451–459. doi: 10.1179/016164109X12590518685660. [DOI] [PubMed] [Google Scholar]
- Conner KR, Goldston DB.. 2007. Rates of suicide among males increase steadily from age 11 to 21: developmental framework and outline for prevention. Aggres Violent Behav. 12(2):193–207. doi: 10.1016/j.avb.2006.07.002. [DOI] [Google Scholar]
- Crean RD, Crane NA, Mason BJ.. 2011. An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. 5(1):1–8. doi: 10.1097/ADM.0b013e31820c23fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Duflou J, Torok M.. 2009. Toxicology and circumstances of completed suicide by means other than overdose. J Forensic Sci. 54(2):490–494. doi: 10.1111/j.1556-4029.2008.00967.x. [DOI] [PubMed] [Google Scholar]
- De Wit H. 2009. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol. 14(1):22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M.. 2003. Exploring the association between cannabis use and depression. Addiction. 98(11):1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- Doucette ML, Borrup KT, Lapidus G, Whitehill JM, McCourt AD, Crifasi CK.. 2021. Effect of Washington State and Colorado’s cannabis legalization on death by suicides. Prev Med. 148:106548. doi: 10.1016/j.ypmed.2021.106548. [DOI] [PubMed] [Google Scholar]
- Escelsior A, Belvederi Murri M, Corsini GP, Serafini G, Aguglia A, Zampogna D, Cattedra S, Nebbia J, Trabucco A, Prestia D, et al. 2021. Cannabinoid use and self-injurious behaviours: a systematic review and meta-analysis. J Affect Disord. 278:85–98. doi: 10.1016/j.jad.2020.09.020. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ.. 2006. Cannabis use and other illicit drug use: testing the cannabis gateway hypothesis. Addiction. 101(4):556–569. doi: 10.1111/j.1360-0443.2005.01322.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Swain‐Campbell N.. 2002. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 97(9):1123–1135. doi: 10.1046/j.1360-0443.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- Fresán A, Dionisio-García DM, González-Castro TB, Ramos-Méndez M, Castillo-Avila RG, Tovilla-Zárate CA, Juárez-Rojop IE, López-Narváez ML, Genis-Mendoza AD, Nicolini H.. 2022. Cannabis smoking increases the risk of suicide ideation and suicide attempt in young individuals of 11–21 years: a systematic review and meta-analysis. J Psychiatr Res. 153:90–98. doi: 10.1016/j.jpsychires.2022.06.053. [DOI] [PubMed] [Google Scholar]
- Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, Ware M, Marmorstein N, Cipriani A, Dendukuri N, et al. 2019. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 76(4):426. doi: 10.1001/jamapsychiatry.2018.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgson K, Almasy L, Knowles EEM, Kent JW, Curran JE, Dyer TD, Göring HHH, Olvera RL, Woolsey MD, Duggirala R, et al. 2017. The genetic basis of the comorbidity between cannabis use and major depression. Addiction. 112(1):113–123. doi: 10.1111/add.13558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Burnette ML, Conner KR, Czyz E, Murray R, Chermack S.. 2010. The association between violence and lifetime suicidal thoughts and behaviors in individuals treated for substance use disorders. Addict Behav. 35(2):111–115. doi: 10.1016/j.addbeh.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Karanikola M, Zisimou P, Nystazaki M, Koutrouba A, Severinsson E.. 2019. Association between illegal use of substances and suicidal behavior in school students: an integrative review of empirical data. J Child Adolesc Psychiatr Nurs. 32(2):80–101. doi: 10.1111/jcap.12228. [DOI] [PubMed] [Google Scholar]
- Klein P, Devinsky O, French J, Harden C, Krauss GL, McCarter R, Sperling MR.. 2021. Suicidality risk of newer antiseizure medications: a meta-analysis. JAMA Neurol. 78(9):1118–1127. doi: 10.1001/jamaneurol.2021.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kung H-C, Pearson JL, Liu X.. 2003. Risk factors for male and female suicide decedents ages 15–64 in the United States. Soc Psychiatry Psychiatr Epidemiol. 38(8):419–426. doi: 10.1007/s00127-003-0656-x. [DOI] [PubMed] [Google Scholar]
- Lynskey M, Hall W.. 2000. The effects of adolescent cannabis use on educational attainment: a review. Addiction. 95(11):1621–1630. doi: 10.1046/j.1360-0443.2000.951116213.x. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Glowinski AL, Todorov AA, Bucholz KK, Madden PA, Nelson EC, Statham DJ, Martin NG, Heath AC.. 2004. Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for cannabis dependence and early-onset cannabis use. Arch Gen Psychiatry. 61(10):1026–1032. doi: 10.1001/archpsyc.61.10.1026. [DOI] [PubMed] [Google Scholar]
- Macleod J, Oakes R, Copello A, Crome L, Egger M, Hickman M, Oppenkowski T, Stokes-Lampard H, Smith GD.. 2004. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 363(9421):1579–1588. doi: 10.1016/S0140-6736(04)16200-4. [DOI] [PubMed] [Google Scholar]
- Mark Anderson D, Hansen B, Rees DI.. 2015. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 17(2):495–528. doi: 10.1093/aler/ahv002. [DOI] [Google Scholar]
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G.. 2007. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review [Article]. Lancet. 370(9584):319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Otten R, Engels RC.. 2013. Testing bidirectional effects between cannabis use and depressive symptoms: moderation by the serotonin transporter gene. Addict Biol. 18(5):826–835. doi: 10.1111/j.1369-1600.2011.00380.x. [DOI] [PubMed] [Google Scholar]
- Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M.. 2014. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 67(4):368–375. doi: 10.1016/j.jclinepi.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Pinto JV, Medeiros LS, Santana da Rosa G, Santana de Oliveira CE, Crippa JAS, Passos IC, Kauer-Sant’Anna M.. 2019. The prevalence and clinical correlates of cannabis use and cannabis use disorder among patients with bipolar disorder: a systematic review with meta-analysis and meta-regression. Neurosci Biobehav Rev. 101:78–84. doi: 10.1016/j.neubiorev.2019.04.004. [DOI] [PubMed] [Google Scholar]
- Rioux C, Huet A-S, Castellanos-Ryan N, Fortier L, Le Blanc M, Hamaoui S, Geoffroy M-C, Renaud J, Seguin JR.. 2021. Substance use disorders and suicidality in youth: a systematic review and meta-analysis with a focus on the direction of the association. PLOS One. 16(8):e0255799. doi: 10.1371/journal.pone.0255799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd MD, Berman AL, Joiner TE, Jr Nock MK, Silverman MM, Mandrusiak M, Van Orden K, Witte T.. 2006. Warning signs for suicide: theory, research, and clinical applications. Suicide Life Threat Behav. 36(3):255–262. doi: 10.1521/suli.2006.36.3.255. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Isometsä ET, Tondo L, D HM, Turecki G, Reis C, Cassidy F, Sinyor M, Azorin JM, Kessing LV, et al. 2015. International Society for Bipolar Disorders Task Force on Suicide: meta-analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar Disord. 17(1):1–16. doi: 10.1111/bdi.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt K, Tseng I, Phan A, Fong T, Tsuang J.. 2020. A systematic review: adolescent cannabis use and suicide. Addict Disord Treat. 19(3):146–151. doi: 10.1097/ADT.0000000000000196. [DOI] [Google Scholar]
- Serafini G, Pompili M, Innamorati M, Rihmer Z, Sher L, Girardi P.. 2012. Can cannabis increase the suicide risk in psychosis? A critical review. Curr Pharm Des. 18(32):5165–5187. doi: 10.2174/138161212802884663. [DOI] [PubMed] [Google Scholar]
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. 2017. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both BMJ 2017; 358 :j4008 doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L, Oquendo MA.. 2023. Suicide: An Overview for Clinicians. Medical Clinics of North America. 107(1):119–130. https://www.sciencedirect.com/science/article/abs/pii/S0025712522000402?via%3Dihub [DOI] [PubMed]
- Shi Y, Lenzi M, An R.. 2015. Cannabis liberalization and adolescent cannabis use: a cross-national study in 38 countries. PLOS One. 10(11):e0143562. doi: 10.1371/journal.pone.0143562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sideli L, Quigley H, La Cascia C, Murray RM.. 2020. Cannabis use and the risk for psychosis and affective disorders. J Dual Diagn. 16(1):22–42. doi: 10.1080/15504263.2019.1674991. [DOI] [PubMed] [Google Scholar]
- Smith PA, Slaven M, Shaw E, Chow E, Wolt A.. 2017. Medical cannabis use in military and police veterans diagnosed with post-traumatic stress disorder (PTSD). J Pain Manag. 10(4):397–405. [Google Scholar]
- Solowij N, Michie PT.. 2007. Cannabis and cognitive dysfunction: parallels with endophenotypes of schizophrenia? J Psychiat Neurosci. 32(1):30–52. [PMC free article] [PubMed] [Google Scholar]
- Stringer S, Minică CC, Verweij KJ, Mbarek H, Bernard M, Derringer J, van Eijk KR, Isen JD, Loukola A, Maciejewski DF et al. 2016. Genome-wide association study of lifetime cannabis use based on a large metaanalytic sample of 32 330 subjects from the International Cannabis Consortium. Transl Psychiatry. 6(3):e769. eng. https://pubmed.ncbi.nlm.nih.gov/27023175/ [DOI] [PMC free article] [PubMed]
- Substance Abuse and Mental Health Services Administration. 2010. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No. SMA 10-4586Findings). Rockville, MD. [Google Scholar]
- Tait RJ, Caldicott D, Mountain D, Hill SL, Lenton S.. 2016. A systematic review of adverse events arising from the use of synthetic cannabinoids and their associated treatment. Clin Toxicol. 54(1):1–13. doi: 10.3109/15563650.2015.1110590. [DOI] [PubMed] [Google Scholar]
- Thabet P, Joshi A, MacDonald E, Hutton B, Cheng W, Stevens A, Kanji S.. 2021. Clinical and pharmacokinetic/dynamic outcomes of prolonged infusions of beta-lactam antimicrobials: an overview of systematic reviews. PLOS One. 16(1):e0244966. doi: 10.1371/journal.pone.0244966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourjman SV, Buck G, Jutras-Aswad D, Khullar A, McInerney S, Saraf G, Pinto JV, Potvin S, Poulin MJ, Frey BN, et al. 2023. Canadian Network for Mood and Anxiety Treatments (CANMAT) task force report: a systematic review and recommendations of cannabis use in bipolar disorder and major depressive disorder. Can J Psychiatry. 68(5):299–311. doi: 10.1177/07067437221099769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turna J, MacKillop J.. 2021. Cannabis use among military veterans: a great deal to gain or lose?. Clin Psychol Rev. 84:101958. doi: 10.1016/j.cpr.2021.101958. [DOI] [PubMed] [Google Scholar]
- Weeks M, Colman I.. 2017. Predictors of suicidal behaviors in Canadian adolescents with no recent history of depression. Arch Suicide Res. 21(2):354–364. doi: 10.1080/13811118.2016.1193076. [DOI] [PubMed] [Google Scholar]
- Welty L, Harrison A, Abram K, Olson N, Aaby D, McCoy K.. 2019. Substance Abuse and Mental Health Services Administration . Key substance use and mental health indicators in the United States: results from the 2016 national survey on drug use and health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality. (Substance Abuse and Mental Health Services Administration Retrieved College of Health Sciences. 106(5):128). [Google Scholar]
- Whitlow CT, Liguori A, Livengood LB, Hart SL, Mussat-Whitlow BJ, Lamborn CM, Laurienti PJ, Porrino LJ.. 2004. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend. 76(1):107–111. doi: 10.1016/j.drugalcdep.2004.04.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data were created or analysed except as fully presented in the full text and appendices.