ABSTRACT
Background:
Dance therapy is thought to improve mental and physical health by activating psychological and physiological processes such as motor coordination, and expression of emotions. Some currently used mind–body interventions for posttraumatic symptoms address both mental and physical health. Although some studies have evaluated the efficacy of dance therapy for posttraumatic symptoms, a systematic review of extant research has not been conducted.
Objectives:
To identify the effects of dance therapy in adults with psychological trauma as well as the barriers and facilitators associated with its therapeutic use.
Method:
Articles published between 2000 and March 2023 have been selected with the help of six relevant keyword combinations applied on seven databases. Two reviewers independently screened 119 titles and abstracts against inclusion and exclusion criteria. Bias evaluation has been conducted with the help of the NIH study quality assessment tools and JBI’s critical appraisal tools. A report of the results has been organized with the help of a thematic analysis.
Results:
Of the 15 articles included, only one case study directly reports a diminution of pathognomonic symptoms of trauma. Other studies present improvements in the key aspects of trauma therapy: bodily sensations and perceptions, psychological processes, and interpersonal skills. These improvements depend on the stability of the intervention, the applied method (dance as therapy or dance/movement therapy), and likely, the skill set of the therapists. However, the reviewed studies lacked uniformity in assessments of adherence and its effect on therapeutic outcomes.
Conclusion:
Dance therapy may be a useful technique for improving both psychological and physiological symptoms associated with trauma exposure, such as avoidance and dissociative phenomena. To complement the results of this qualitative systematic review, further quantitative and qualitative research on the impact of dance therapy interventions as a trauma treatment should be conducted.
KEYWORDS: Dance therapy, psychological trauma, violence, post-traumatic stress disorder, adults, psychotherapy
HIGHLIGHTS
Dance therapy may be a promising approach for the therapeutic management of psychological trauma as it can address both psychological and physical symptoms.
Therapist skills and training may be important factors to consider in evaluating the impact of dance therapy on posttraumatic symptoms.
Dance/movement therapy, a specific type of dance therapy, appears to be associated with improvements in sensory-motor perceptions and motor skills.
To date, examination of dance therapy as a trauma treatment in an adult population has been limited primarily to women and people facing migration.
Abstract
Antecedentes: Se cree que la terapia de baile mejora la salud mental y física al activar procesos psicológicos y fisiológicos como la coordinación motora y la expresión de emociones. Algunas intervenciones de mente y cuerpo utilizadas actualmente para los síntomas postraumáticos abordan tanto la salud mental como la física. Aunque algunos estudios han evaluado la eficacia de la terapia de baile para los síntomas postraumáticos, no se ha realizado una revisión sistemática de la investigación existente.
Objetivo: Identificar los efectos de la danzaterapia en adultos con trauma psicológico así como las barreras y facilitadores asociados a su uso terapéutico.
Método: Se seleccionaron artículos publicados entre el 2000 y marzo de 2023 con la ayuda de seis combinaciones de palabras clave relevantes usadas en siete bases de datos. Dos revisores examinaron de forma independiente 119 títulos y resúmenes según los criterios de inclusión y exclusión. La evaluación del sesgo se llevó a cabo con la ayuda de las herramientas de evaluación de la calidad del estudio del NIH y las herramientas de evaluación crítica del JBI. Se ha organizado un informe de los resultados con la ayuda de un análisis temático.
Resultados: De los 15 artículos incluidos, solo un estudio de caso reporta directamente una disminución de los síntomas patognomónicos del trauma. Otros estudios presentan mejoras en los aspectos clave de la terapia del trauma: sensaciones y percepciones corporales, procesos psicológicos y habilidades interpersonales. Estas mejoras dependen de la estabilidad de la intervención, el método aplicado (baile como terapia o terapia de baile/movimiento) y, probablemente, el conjunto de habilidades de los terapeutas. Sin embargo, los estudios revisados carecían de uniformidad en las evaluaciones de la adherencia y su efecto sobre los resultados terapéuticos.
Conclusión: La danzaterapia puede ser una técnica útil para mejorar los síntomas tanto psicológicos como fisiológicos asociados a la exposición al trauma, como los fenómenos de evitación y disociativos. Para complementar los resultados de esta revisión sistemática cualitativa, se deben realizar investigaciones cuantitativas y cualitativas adicionales sobre el impacto de las intervenciones de danzaterapia como tratamiento del trauma.
PALABRAS CLAVE: Terapia de baile, Trauma psicológico, Violencia, Trastorno de estrés postraumático, Adultos, Psicoterapia
Abstract
背景:舞蹈疗法被认为可以通过激活运动协调和情绪表达等心理和生理过程来改善身心健康。目前使用的一些针对创伤后症状的身心干预措施可同时解决心理和身体健康问题。尽管一些研究评估了舞蹈治疗对创伤后症状的疗效,尚未对现有研究进行系统综述。
目的:确定舞蹈治疗对心理创伤成人的影响,以及与其治疗使用相关的障碍和促进因素。
方法:2000 年至 2023 年 3 月之间发表的文章已在应用于七个数据库的六个相关关键词组合的帮助下进行了选择。两名综述者根据纳入和排除标准独立筛选了 119个标题和摘要。偏差评估在 NIH 研究质量评估工具和 JBI 关键评估工具的帮助下进行。在主题分析的帮助下组织了一份结果报告。
结果:在纳入的 15 篇文章中,只有一篇案例研究直接报告了创伤的特征性症状的减少。其他研究提出了创伤治疗关键方面的改进:身体感觉和知觉、心理过程和人际交往能力。这些改进取决于干预的稳定性、应用的方法(舞蹈疗法或舞蹈/运动疗法),可能还取决于治疗师的技能组合。然而,所综述的研究在评估依从性及其对治疗结果的影响方面缺乏一致性。
结论:舞蹈疗法可能是改善创伤暴露相关心理和生理症状的有用技术,例如回避和解离现象。为了补充这项定性系统综述的结果,应该对舞蹈治疗干预作为一种创伤治疗的影响进行进一步的定量和定性研究。
关键词: 舞蹈治疗, 心理创伤, 暴力, 创伤后应激障碍, 成年人, 心理治疗。
1. Background and purpose
Dancing activities have been used to improve the health and quality of life of individuals since the dawn of civilization (Dunphy et al., 2022). During the 1940s, Western societies started to operationalize dancing activities as a psychotherapeutic tool in order to promote a professional and standardized therapeutic use of dance (Dunphy et al., 2022). There is today no acknowledged definition of dance therapy (DT) and this appellation encompasses all practices that involve dance activities used as therapy (Dunphy et al., 2022). Dance/Movement Therapy (DMT) is however defined as ‘the psychotherapeutic use of movement to promote the emotional, social, cognitive, and physical integration of the individual’ (American Dance Therapy Association, 2023). Worldwide, DMT must be conducted by licensed or credentialed individuals with specific training (American Dance Therapy Association, 2023). Dance as Therapy (DaT) is generally carried out by professionals that commonly work in artistic and therapeutic fields where dance is considered as ‘a global healing practice’ (American Dance Therapy Association, 2023). Today, DT interventions (DaT and DMT) are frequently implemented in health (psychiatric hospitals), social (rehabilitation centres, drop-in centres), and educational (schools) settings (Dunphy et al., 2022).
On the psychological level, DT mobilizes the individual's cognitive sphere (learning ability, attention, memory, rhythmic motor coordination, and visual-spatial ability), as well as the creative and emotional sphere (movement improvization through music, imagination, emotion, and social interaction) (Pessoa et al., 2019). To date, meta-analyses and randomized clinical trials have evaluated the use of DT and demonstrated its positive impact on inpatients’ physical and mental health as well as in diverse outpatients’ mental health services (Koch et al., 2019; Ritter & Low, 1996; Wang et al., 2022). The positive effects of DT on physical and mental health thus make it a relevant psychotherapeutic tool for the management of psychological distress. Because of its emphasis on the body, DT is well-suited to specific clinical settings in which individuals have difficulty using conventional language-based psychotherapeutic approaches (Taylor et al., 2020; Van de Kamp et al., 2019). Consequently, health and social service institutions are increasingly looking to DT to address their patients’ needs. Today, several institutions that implement and explore the effects of DT protocols consider that DT may be beneficial for individuals with psychological trauma (Levine & Land, 2016; Pierce, 2014).
Nowadays, psychological trauma is defined as a significant psychological shock caused by one or more critical events that can alter an individual's psyche and physiological functioning (Perrotta, 2020). Psychological trauma may lead to post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (CPTSD) (American Psychiatric Association, 2013; World Health Organization, 2019). In the general population, PTSD affects women twice as much as men with an estimated prevalence of 5.6% of the general population (Koenen et al., 2017). Recent estimates suggest that up to 47% of people facing migration are at risk of developing PTSD (Bustamante et al., 2018; Lindert et al., 2009; Mesa-Vieira et al., 2022). This risk can be influenced by the duration of their journey, origin country, destination country, and their status (refugees or labour migrants) (Bustamante et al., 2018; Lindert et al., 2009; Mesa-Vieira et al., 2022). In order to diagnose PTSD, the symptoms (intrusion, avoidance, disturbances in cognition and mood, and changes in arousal and reactivity) must impair the daily life and cause significant distress (American Psychiatric Association, 2013). PTSD symptoms can extend to traumatic revivification mechanisms (restoring the traumatic memories and affects to consciousness) and dissociation phenomena (American Psychiatric Association, 2013). Psychological trauma can also significantly impact the mental, and somatic (cardiovascular system, immune status, metabolic systems, and inflammatory responses) aspects of the subject (American Psychiatric Association, 2013; Hillis et al., 2016; O’Donnell et al., 2021). Because of these multiple consequences, psychological trauma can alter the therapeutic and medical work, given that it hinders communication between the caregiver and the patient while contributing to the patient's disengagement (Bassuk et al., 2001; Green et al., 2016).
A variety of approaches have been utilized to address psychological trauma (e.g. mind–body strategies, art therapy, cognitive behavioural therapy) (VA/DOD, 2017; Watkins et al., 2018). When mind–body interventions are used, the activation of the body at a somatic level addresses profound physiological responses associated with risk, promotes relaxation, reduces stress, and facilitates interpersonal therapy (Grabbe & Miller-Karas, 2018; Watkins et al., 2018). From a psychotherapeutic point of view, DT mobilizes the cognitive, creative, and sensorial spheres of the subject, known to be particularly targeted by psychotherapeutic intervention devoted to psychological trauma (Koch et al., 2019; Levine & Land, 2016; Pessoa et al., 2019). For instance, on a cognitive and sensorial level, DT favours embodiment cognition (mental representation of the body) and interoception (awareness of the body and internal state), two cognitive functions impaired by the dissociation phenomena in psychological trauma and the ‘disturbances in cognition and mood’ symptoms in PTSD (Millman et al., 2021). On a creative and emotional level, DT supports the growth of relational skills (avoidance symptoms of PTSD), new interpretation and understanding of the traumatic event (mechanism of traumatic revivification, intrusion symptoms of PTSD), and new ways to express the emotions stored in the body and traumatic memory (intrusion symptoms of PTSD, changes in mood, arousal, and reactivity, and dissociation phenomena) (Levine & Land, 2016; Pierce, 2014).
To promote better therapeutic practice adjusted to the clinical particularities of patients, scientific research then needs to better understand and isolate the effects of DT on specific populations as well as their most associated mental health difficulties. The primary objective of this article is therefore to identify the effects of DT on adults with psychological trauma. Its second objective is to identify the barriers and facilitators associated with the impact of DT on adults suffering from psychological trauma. This systematic review aims to guide future studies on the effectiveness of DT in the management of psychological trauma, refine the quality of clinical referrals, and provide theoretical support for clinical DT practices.
2. Method
2.1. Search strategy
The present qualitative systematic review protocol, registered in PROSPERO under the reference CRD42022306326, is a part of the research project VaDDanC (Validation of a Dance-therapy Device in Co-therapy), funded by LOBA association. The aim of the present systematic review is to evaluate the impact of DT on adults suffering from psychological trauma.
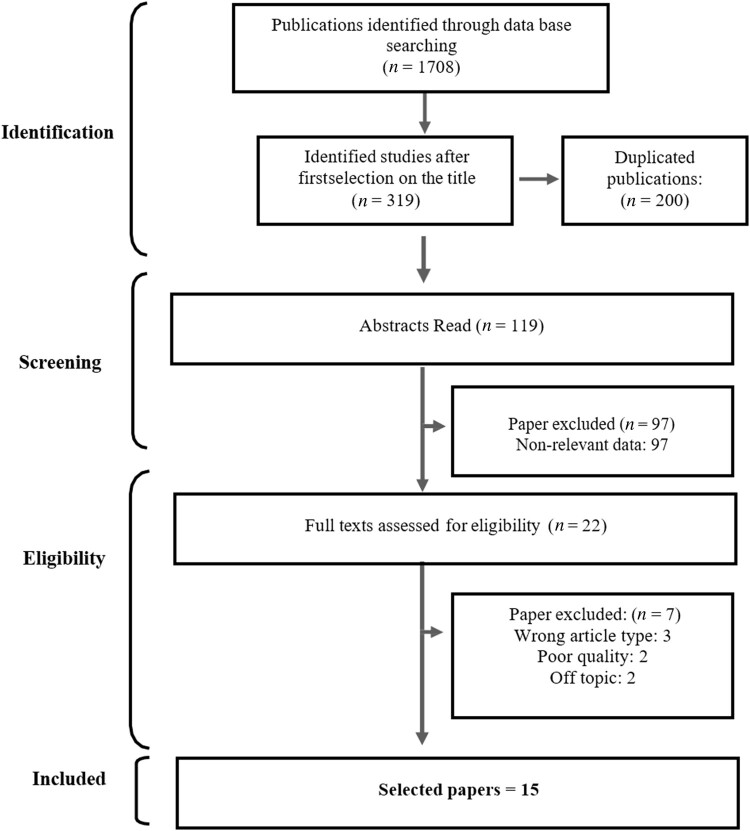
Two authors conducted the search strategy in a double-blind manner (CT and CC) (Figure 1). They initially screened the articles published between 2000 and February 2022 with the help of a list of French and English keywords: ‘dance/danse’, ‘therapy/therapies’, ‘trauma/trauma’, ‘intervention/intervention’, ‘group/groupe’, ‘violence/violence’, ‘dance/movement therapy’, ‘PTSD’. The articles search was updated in March 2023. The keywords were organized into 6 different keyword combinations applied on 7 databases: Cochrane, Embase, PubMed, Web of Science, PsycINFO, PsycArticles, and ScienceDirect (supp data 1). The authors also completed a complementary research on the 20 first result pages of Google Scholar with those keyword combinations as well as exploring the reference list of the selected articles, to ensure that no additional paper were missed.
Figure 1.
Flow diagram of the selection process.
2.2. Inclusion criteria and bias assessment
The inclusion criteria of the systematic review were: the scope of the study (over 18 years old adult-focused studies, individuals with psychological trauma, dance therapy, and dance movement therapy) and articles published between 2000 and June 2022. The exclusion criteria were: studies focusing on children and adolescents under 18, out-of-scope articles, literature reviews, book chapters, books, published theses, dissertations, conference abstracts, guides, and expert reports. Two researchers (CT and CC) carried out the bias assessment (Table 1) with the help of two types of assessment tools: the NIH study quality assessment tools (National Institutes of Health, 2014) and the Joanna Briggs Institute’s (JBI) critical appraisal tools (Aromataris & Munn, 2020). They used both tools when permitted by the article design, and cross-tabulated the results. They evaluated and assessed the case studies with the JBI’s critical appraisal tools only, the NIH study quality assessment tool being not designed for this purpose.
Table 1.
Bias analysis.
| Article | NIH analysis results | JBI analysis | Quality |
|---|---|---|---|
| Laird et al. (2021) | - Exposure was only assessed once - Modalities of outcome assessors (blinded) are not presented |
No bias | Fair |
| Koch et al. (2019) | - Eligibility criteria are not clearly described - The sample is not large enough to provide confidence in the findings - People assessing the outcomes were not blinded to the participants’ exposure - No multiple measurements before and after the intervention |
- No multiple measurements of the outcome both pre and post-intervention/exposure |
Average |
| Ho (2015) | - Information about the enrollment of all eligible participants meeting prespecified entry criteria is not presented - The sample size is too small to provide confidence in the findings - People assessing the outcomes are not blinded to the participants’ interventions |
Not adequate | Fair |
| Levine & Land (2016) | - Authors do not mention how many reviewers conducted the study - In the method, there is no mention of a way to minimize errors in data extraction - No bias assessment is mentioned - No mention of heterogeneity assessment |
- Authors do not mention how many reviewers conducted the study - In the method, there is no mention of a way to minimize errors in data extraction - No bias assessment is mentioned - No mention of heterogeneity assessment |
Average |
| Ko (2017) | - No follow-up (the last result is the last session) | - No description of post-intervention clinical condition - No adverse or unanticipated events are mentioned |
Fair |
| Verreault (2017) | - The exposures of interest are not measured before the measurement of the outcome | - Influence of the researcher on the research, and vice-versa, are unclear | Good |
| Dieterich-Hartwell et al. (2021) | - Outcome measures of interest were not taken multiple times before the intervention and multiple times after the intervention - People assessing the outcomes are not blinded to the participants’ exposure - The sample is not sufficiently large to provide enough confidence in the findings - Information about the enrollment of all eligible participants meeting prespecified entry criteria is not presented |
No bias | Average |
| Ley et al. (2017) | No bias | No bias | Good |
| Moe (2014) | Not adequate | - The congruity between the research methodology and the research question is unclear. - The influence of the researcher on the research and vice-versa is not addressed. - The conclusions do not report any flow. |
Average |
| Manford (2014) | Not adequate | - Patient's demographic characteristics are not described. - Patient's history is very brief. - The intervention procedure is not described at all. - The post-intervention clinical conditions remain unclear. |
Average |
| Fargnoli (2017) | Not adequate | - The influence of the researcher on the research, and vice-versa, is not addressed. | Good |
| Koch & Weidinger-von der Recke (2009) | Not adequate | - Diagnostic tests and assessments are not clearly described in the method and results. - The post-intervention clinical condition is not clearly described |
Fair |
| Lee et al. (2022) | No bias | No bias | Good |
| Özümerzifon et al. (2022) | - It is unclear if all participants that met inclusion criteria are enrolled - The sample size is too small to provide confidence in the findings - People assessing the outcomes are not blinded to the participants’ exposure - It is unclear if the loss to follow-up is accounted for in the analysis - No multiple measurements before and after the intervention |
No bias | Average |
| Schaeffer & Cornelius-White (2021) | - No bias assessment was conducted before including the publications | Good | |
| Colace (2017) | - Study question and objective are not clearly stated - The intervention is not clearly described - The outcome measures are not clearly defined - No length of follow-up was mentioned - The results are not well-described |
- The current clinical condition of the patient is not clearly described - No diagnostic tests or assessment methods, no clear description of the results - Interventions or treatment procedures are not clearly described |
Poor |
| Dunphy, Elton, & Jordan (2014) | - The population is not specified and defined - Eclectic population (not similar), no inclusion nor exclusion criteria - No mention of the exact sample size - No justification for the sample size - No data analysis - The timeframe is non-sufficient to establish an association between exposure and outcome. - No variation in exposure - The exposure measures are not defined - Exposure was assessed once, at the end of the session - Outcome assessors were not blinded to the exposure status of participants - Potential confounding variables are not measured |
- The congruity between the research methodology and the research question is unclear. - No congruity between the research methodology and the methods used to collect data. - No congruity between the research methodology and the representation and analysis of data. - Participants and their voices are not adequately presented - Ethics approval is not mentioned. - Conclusion does not report flow from the analysis or interpretation of the data |
Poor |
At the end of the selection process, authors extracted the following available data (Tables 2 and 3): authors, date of publication, the title of the publication, country undertaking the study, objectives, hypotheses, type of article, population, study parameters, type of analysis, main results (Table 2), secondary results, and authors’ main interpretations. At last, a thematic analysis (Braun & Clarke, 2021) based on the extracted data isolated relevant sub-themes and themes exploring the impact, associated factors, and barriers associated with DT and psychological trauma.
Table 2.
Selected articles.
| Study | Design | Intervention/Settings | Population | Type of therapist | Main results |
|---|---|---|---|---|---|
| Levine & Land (2016) | Qualitative meta-synthesis | 5 keywords, 6 databases ‘5 inclusion criteria: written in English, published during or after 1992, focused on trauma, primary research, qualitative methods only’ (p. 3) 9 studies included | Women and men from 5 to 38 years old, with trauma. Samples from 1 to 294 participants | Dance/movement therapist | Dance therapy creates awareness and increases the range of movement. It also creates a new and healthy relationship with the self/therapist/group through the moving process, and a new and healthy relationship with movement. |
| Verreault (2017) | Qualitative study | ‘Four weekly DMT sessions of 75 min each, for a period of one month.’ (p. 123) Observations and exit interviews of the participants | ‘8 female asylum seekers and refugees, from 19 to 50 years [with] traumatic complaints, mostly accompanied by depressive and somatic symptoms’ (p. 123) | Dance/movement therapist and drama therapist (co-facilitator) | Dance therapy ameliorates body awareness and increases the feeling of safety and religious, spiritual, psychological, and cultural resources. It provides group support as well. |
| Moe (2014) | Qualitative study | Semi-structured interviews of 45 min, with 11 general questions, in 2009 and 2010. ‘Focused on experience with belly dance’ (p. 328). 18 face-to-face, 49 by phone | 20 belly dancer women, from 22 to 68, who ‘disclosed victimization’ (p. 330) | Facilitators of belly dance | Dance therapy helps participants feel their bodies, and reconnect with and reclaim their objectified bodies. Acceptance of emotions, especially fear, is facilitated by dance, as it is a way of expressing themselves. Finding their interest allows them to retake power, and release themselves of judgment and rigid control. Dance helps them feel beautiful again, whole, and worthwhile. Participants feel alive, sensual, feminine, and strong, and find confidence and a sense of self. Communal support, social support, and communal benefits are very important. |
| Fargnoli (2017) | Qualitative study | Semi-structured interviews of 45 min to 1 h, audio recorded, with a Bengali interpreter. Starts with meditation, then questions, and finishes with movement ‘to reflect on the interview and their experience of self-care’ (p. 235) | 6 women survivors of human trafficking, between 22 and 30, and practicing as DMT trainers for at least 5 years. | Dance/movement therapist | Dance therapy creates connection through movement, emotional awareness, and release, and enhances kinesthetic empathy. It allows participants to have a self-reflection, and to initiate a creative, sharing and empowering process. It generates pride and balances life roles through dignity and autonomy. |
| Schaeffer & Cornelius-White (2021) | Qualitative meta-synthesis | 9 keywords, 7 databases Inclusion criteria: peer-reviewed articles published between 2010 and 2020, written in English, on qualitative studies on body-focused therapeutic interventions for refugees, forced migrants, and/or torture survivors. 11 articles included |
Immigrants, refugees et asylum seekers, from 18 to 57 years old | Art-therapist | Dance therapy improves physical health, and emotional experience and increases bodily awareness. Considerations for clinicians and treatment revolve around cultural competencies, linguistic barriers, attending to re-traumatization, engagement and attunement, and obstacles to treatment. The creation of safety, ritual, symbolism, and metaphorical dancing is important. Dance therapy enhances embodiment, freedom of expression, and a process of empowerment. Participants can feel their ‘here and now presence’ and improve their interpersonal skills. |
| Koch et al. (2019) | Quantitative experimental study | Two groups: control (N = 16), and experimental (N = 16). Pre-test, post-test form, demographic data, ‘sessions twice a week. The control group received treatment as usual.’ (p. 7) Four different Flamenco sessions (2015, 2016). |
32 traumatized inpatients, men (N = 6) and women (N = 27) in psychiatric hospital wards, from 18 to 59 years old | Music-therapist | They measured positive (F = 0.60, p = .445, eta² = 0.02) and negative dimensions of well-being, and the perception of general health, physical pain, fitness (F = 0.37, p = .549, eta²=0.01), and body-related self-efficacy (F = 0.71, p = .405, eta²=0.02). Exploration and expression of thoughts, behaviours, and emotions are favoured by dance therapy. Dance therapy also grants access to the perception of boundaries, and embodied intersubjectivity. |
| Manford (2014) | Case study | Individual sessions, in a psychology and psychotherapy team | 1 woman, diagnosed with borderline personality, hospitalized in a secure hospital | Dance/movement psychotherapist | Through dance therapy, participants experience their bodies, feelings, and behaviours. Movement creates a connection. Anxiety and aggression are expressed. It improves their capacity to think and check their emotional state. Dance therapy creates distance from emotional distress, with movement defense mechanisms |
| Ko (2017) | Case study | 10 weekly 60 min therapy sessions with movement and verbal processing. Dance with a scarf. ‘Individual DMT and social services were continued after the 10 sessions.’ (p. 66) Written notes of the sessions and open-ended questions | 1 woman 40 years old, with ‘haan’ (similar to trauma in Korea) | Dance/movement therapist | The participant’s body is in pain, and she feels shame. She gets wisdom from both her moving and silent body. She feels like a boiling hot emotional container that fluctuates emotions, and she adds feelings with dance therapy. She desires to move forward as she feels stuck in the past. Dancing through emotional burden allows expressing emotions, physical expression facilitated, airing of her suppressed emotions. She dances to feel strong and explore resilience, heavy emotions (linked to trauma) that are lightened by movement (symbolic in space and form). Need for space. |
| Dieterich-Hartwell et al. (2021) | Qualitative study | 3 locations, individual (N = 5) or group intervention (N = 7). First meeting with a survey (general resources and relationship to body and movement). Then 3–5 meetings (60 min) to explore and develop expressive movement phrases. Final meeting with another survey (movement experience). |
N = 13, over 18 years old ‘with a refugee or asylum-seeker status, a trauma history and had lived in the USA for five years or less’ (p. 77). Mostly women: 10/13 ‘Exclusion criteria: cognitive impairment, current substance abuse, active psychosis, an indication of current suicide or homicide risk.’ (p. 77) |
Dance/movement therapist | Dance therapy allows one to experience expressive movements, and bear active movement factors. It extends resources (cultural, environmental, family). |
| Ley et al. (2017) | Qualitative study | Observations of group interventions (one male only and one female only per year since 2013). Group twice a week for three months. | 4 participants, war, and torture survivors, over 18 years old, with ‘post-traumatic stress disorders, depression, anxiety disorders and various other physical psychosomatic and psychosocial impairments’ (p. 86) | Two trainers and a trauma expert | Achieving flow is very important for dance therapy to be effective. It improves an affective state and creates a new sense of safety and confidence. |
| Koch & Weidinger-von der Recke (2009) | Case study | Group therapy with verbal trauma therapy methods and elements of dance/movement therapy (DMT). | 9 Albanian women, from Kosovo, with post-traumatic stress disorder, depression, and anxiety disorders | Art-therapist | Dance therapy emotionally engages the participants, reducing feelings of shame and guilt. Cultural verbal and non-verbal support is important. Dance therapy grants inner stability. The reintegration of the fragmented and negatively cathected body image is facilitated by dance therapy. Processing trauma starts at a sensorimotor level to activate bodily resources and turns in advance the emotional and cognitive processing of the trauma. Group prevents dissociative phenomena and re-traumatization. |
| Ho (2015) | Uncontrolled clinical trial | 5 weekly DMT (dance/movement therapy) sessions of 2 h. 4 questionnaires + open-ended questions at T0 before, T1 immediately after, and T2 5 weeks after intervention. | 21 Chinese women 25–52 years old, who suffered childhood sexual abuse | Dance/movement therapist | Dance therapy tends to improve self-esteem (t = 1.85, d = 0.3 p = .08) and the over-attachment dimension of stagnation (t = −1.63, d = −0.2, p = .12). It grants awareness of body, personal space, rhythm, and pace, and improves feelings and emotions, sensations, and awareness of inner space. It helps develop new perspectives and positive meaning. Mental distress (t = −1.46, p = .16, d = −0.4), perception of boundaries (F = 3.19, p = .084, eta²=0.10), personified intersubjectivity (F = 3.37, p = .076, eta²=0.10) are improved. |
| Laird, Vergeer, Hennelly, & Siddarth (2021) | Cross-sectional study | An online survey from July to December 2019, on duration, frequency, and form of conscious dance, mental and physical health conditions, psychological well-being, and experiences during and after a conscious dance. | Self-identifying adult conscious dancers (N = 1003), mean age 47 years old. Health Conditions (N responded): Chronic Pain (N = 867) 255 (29.4%) Depression (N = 864) 298 (34.5%) History of Trauma (N = 864) 511 (59.1%) Anxiety (N = 872) 451 (51.7%) |
Facilitators of conscious dance | Flow state during dance helps with the management of chronic pain (t(237) = 4.08, d = 0.91, p < .0001), depression (t(276) = 5.06, d = 1.94, p < .0001), anxiety (t(434) = 5. 58, d = 1.52, p < .0001), and history of trauma (t(482) = 5.84, d = 1.30, p < .0001). Dance therapy improves perceived health (F = 18.71, p < .001, eta² = 0.38). The duration and frequency of the dance therapy interventions are very important, as they improve flow state (frequency: t(806) = 3.25, d = 0.23, p = .001, duration: t(840) = 3.11, d = 0.22, p = .002), life satisfaction (duration: t(932) = 2. 94, d = 0.19, p = .003) and mindfulness (frequency: t(850) = 2.72, d = 0.19, p = .007, duration: t(932) = 7.86, d = 0.52, p < .0001). The interaction term of duration and frequency is not correlated with the intensity of mindfulness (F(1,803) = 0.8, p = .4), life satisfaction (F(1,803) = 0.6, p = .4), and flow state (F(1,803) = 0.02, p = .9). |
| Lee et al. (2022) | Systematic Review | 12 keywords, 5 databases, 4 inclusion criteria: ‘peer-reviewed, English, reported on an interventional outcome, reported on therapeutic dance for sexual trauma’ (p. 4) 11 studies included | Mostly female, from 11 to 48 years old, with sexual trauma. Samples from 1 to 152 participants. | Dance/movement therapist Dance therapist Facilitators of dance as therapy |
Therapeutic Dance positively affects participants’: - emotional states, as it improves self-awareness of emotion, expression of emotions, and regulation of emotions - relational lives, as it improves boundary formation, and experience of interpersonal relationships - perception of self, as it improves the sense of safety and freedom, body awareness and body image, gives a positive future orientation, and favours self-empowerment. |
| Özümerzifon et al. (2022) | Randomized control trial & Qualitative investigation | 12 virtual sessions of creative dance/movement program (90 min, twice a week for 6 weeks), and usual care for group control. Pre- and post-intervention surveys, self-administratered electronically. 16 women in the intervention group participated in a 45–60 min focus group. | 45 women, 23–48 years old, survivors of Intimate Partner Violence (IPV). 25 in the intervention group, and 20 in the control group minus 2 lost for the second measure. | Two Gibney facilitators Move to Move Beyond: collaboration between dancers, survivors and social workers | Intervention and control group experienced a similar decrease in PCL-5 scores (F(1) = 1.093, p = .302, η² = 0.026). Before and after the intervention, ‘the affective valence, the quality of an event or experience to be perceived as being pleasant or unpleasant improved (t(22) = −2.187, p = .04, d = 2.426).’ (p. 7). Six themes emerged from the focus group: ‘Connection to self and body, Expressing oneself through movement, Community building, Relaxation/stress relief, Elicitation of positive emotions, and Transfer of self-care habits learned during the workshop to everyday life.’ (p. 8) |
Table 3.
Results of the thematic analysis.
| Themes | Sub-themes | Frequency |
|---|---|---|
| Body in Motion | Bodily sensations and perceptions | 11 |
| Movement | 6 | |
| Individual psychological factors | Emotions | 9 |
| Mental health afflictions symptoms | 4 | |
| Identity and mental health | 8 | |
| Relationship | Relationship with others | 9 |
| Self-expression | 4 | |
| Group intervention | Security | 5 |
| Culture | 4 | |
| Group characteristics | 4 | |
| General Health | Well-being | 6 |
| Physical pain | 3 | |
| Psychological process | Linking affects and representations | 2 |
| Mental movement | 2 |
2.3. Study selection
The authors screened 1708 articles during the database search (supp data 1). Among the 119 selected titles, a dual evaluation of the abstracts was undergone using the Rayyan QCRI software (Ouzzani et al., 2016). Then, the application of inclusion and exclusion criteria led to an exclusion of 102 articles. Finally, an analysis of bias on the 17 remaining articles has been performed and it consequently excluded 2 articles that presented too much methodological bias (the description of the intervention was too vague, the variables were not established, the data collection and analysis did not correspond to the protocol presented, the sample was not described). As a result, the authors included 15 articles in this qualitative systematic review.
2.4. Data analysis
As data extraction did not isolate enough quantitative data per studied variables (two or more quantitative results per the same variable (Deeks et al., 2022)), a meta-analysis could not be performed. Two researchers conducted a thematic analysis and identified 14 common subthemes grouped into 6 main themes. They presented and discussed the results of this qualitative systematic review according to the Synthesis Without Meta-analysis (SWiM) protocol (Campbell et al., 2020). The SWiM protocol recommends synthesizing the findings and their certainty, mentioning and numbering the exact studies contributing to the synthesis, reporting the key characteristics of the included studies, and reporting the limitations of the synthesis in the discussion (Campbell et al., 2020). A list of recommendations for research and clinical practice is also formulated to shed light on future theoretical, psychotherapeutic, and psychopathological directions applied to DT.
3. Results
This qualitative systematic review includes a total of 15 articles. The authors extracted the main characteristics and results of the papers (Table 2). These studies have been conducted in Europe (Germany/3, The Netherlands/2, Austria/2, The United Kingdom/2), the United States of America (6), and China (1). Selected studies encompass two meta-syntheses (two articles already included by our selection process (Ley et al., 2017; Verreault, 2017)), 1 systematic review (one article already included by our selection process (Lee et al., 2022)), 4 quantitative studies (2 monocentric and 2 multicentric), 5 qualitative studies (3 monocentric and 2 multicentric), and 3 monocentric case studies.
Sample sizes of studies range from 1 to 1003 including individuals with psychological trauma (self-reported trauma history and/or traumatic event/7, characterized as traumatized and/or with a PTSD diagnosis/5, traumatic complaints/3). Psychological trauma (PTSD and psychological trauma) was associated with migration (4 studies), childhood maltreatment (3 studies), gendered interpersonal victimization (3 studies), human trafficking (1 study), and war survival (2 studies). The samples are predominantly female (7 papers with exclusively female populations and 8 papers with predominantly female populations), allegedly because of patient self-selection bias and referral bias, and female populations have been a selection criterion for 2 studies. Data were collected through semi-structured interviews (6 studies), questionnaires (6 studies), and observations (5 studies). The DT interventions took place in health (7 papers), social (4 papers), and educational settings (1 paper). The thematic analysis (Braun & Clarke, 2006) isolated 6 major themes: Body and Space, Individual Psychological Factors, Relationship, Group intervention, General Health, and Psychological Processes (Table 3).
3.1. Body in motion
3.1.1. Bodily sensations and perceptions
Selected studies suggested that DT improves the sensory-motor perceptions of individuals suffering from psychological trauma. Qualitative studies pointed to an improved body awareness and the emergence of a mind–body connection through the sensory experience of movement, rhythm, and relaxation (Fargnoli, 2017; Levine & Land, 2016; Moe, 2014; Özümerzifon et al., 2022; Schaeffer & Cornelius-White, 2021; Verreault, 2017). Also, as demonstrated by an experimental quantitative study using one Flamenco session, the intervention needs to be long enough to produce a change in physical skills, body self-efficacy, or perceived level of fitness (Koch et al., 2019). As a consequence, the differences between the control group, receiving treatment as usual in a psychiatric hospital ward, and the Flamenco group were not significant (fitness: F = 0.37, p = .549, eta² = 0.01, and body-related self-efficacy: F = 0.71, p = .405, eta² = 0.02). Two major limitations of this study should then be reported: the small sample size and the fact that only one Flamenco dance session was implemented. On another level, a different case study article focusing on a patient suffering from a borderline personality disorder described the presence of mechanisms associated with bodily experience and the mind–body connection (Manford, 2014). The study highlighted that improvement of the sensory-motor perception associated with DMT are more related to individual caracteristics than the psychiatric diagnosis.
3.1.2. Movement
Included studies demonstrated that DMT may improve the motor skills of individuals with psychological trauma. The qualitative studies pointed to an increase in the range of motion, an expansion of movement repertoire, and the creation of a mind–body connection through movement (Dieterich-Hartwell et al., 2021; Fargnoli, 2017; Levine & Land, 2016). Repetition of the sessions seemed essential for participants to become aware of these improvements (Dieterich-Hartwell et al., 2021). A case study of a migration-affected woman similarly reported the experience of the moving and silent body (Ko, 2017). However, expression through movement can only occur with a dance/movement therapist trained to observe, decipher, and therefore perceive the expressivity of the patient’s movement (Fargnoli, 2017; Levine & Land, 2016).
3.2. Individual psychological factors
3.2.1. Emotions
When applied to individuals suffering from psychological trauma, DT is associated with an improvement in the identification, expression, and externalization of emotions. A systematic review (Lee et al., 2022) and several qualitative studies particularly identified an improvement in an emotional state, a better recognition of emotions, a better focus on emotions, an improvement in emotional release, and the development of kinesthetic empathy (to feel in one’s own body the movement of the other) (Fargnoli, 2017; Ley et al., 2017; Moe, 2014; Schaeffer & Cornelius-White, 2021). A longitudinal cohort study (associated with a RCT studying other dimensions) supported these results, through measurement of the affective valence of 25 women before and after participating in 12 virtual sessions of a creative dance/movement programme (t(22) = −2.187, p = .04, d = 2.426) (Özümerzifon et al., 2022).
On a qualitative level, two case studies noticed that the first emotional expressions after DMT and DaT involve the expression of fear, shame, and guilt (Ko, 2017; Koch & Weidinger-von der Recke, 2009). DMT and DaT also promoted the emergence of psyche processes such as awareness and verbalization of affects, as well as an alleviation of suffering (Ho, 2015; Koch & Weidinger-von der Recke, 2009). The emotional expression promoted by DMT then facilitated the processing of the trauma (Ko, 2017). On the other hand, DaT facilitated the improvement of the emotional experience (Schaeffer & Cornelius-White, 2021). It is important to mention that the authors observed these improvements during the treatment or just after the last session. The lack of longitudinal observations in the selected studies prevents any conclusion about the persistence of these improvements.
3.2.2. Identity and mental health
Our analysis shows that when employed with individuals suffering from psychological trauma, DT should mobilize identity factors and improve their mental health. Qualitative studies indicated that DMT and DaT mobilize psychological resources and improve reflexivity and creativity (Fargnoli, 2017; Moe, 2014; Özümerzifon et al., 2022; Schaeffer & Cornelius-White, 2021; Verreault, 2017). DMT and DaT also generated a renewed feeling of being alive, a better enjoyment in ‘the here and now’ as well as a facilitated initiation of the process of empowerment. Additionally, DT facilitated the rediscovery of self-encouraged individual and social dimensions (femininity, sensuality, and spirituality) (Moe, 2014; Verreault, 2017). These movements contributed to the reconstruction of the self and increase self-confidence and pride in being oneself. On this point, case studies also show the emergence of a will to move towards the future, an improvement in the ability to think and to be attentive to one’s emotional state (Dieterich-Hartwell et al., 2021; Ko, 2017; Manford, 2014). One case study assessed those improvements as a way to better construct a new internal and psychological stability while helping to construct a new internal and psychological stability (Koch & Weidinger-von der Recke, 2009). In sum, these results converged sufficiently to suggest a positive impact of DT on the mental health of individuals with psychological trauma.
3.2.3. Mental health afflictions symptoms
Several articles provided an evaluation of specific symptoms of mental health afflictions associated with psychological trauma. A non-randomized clinical trial involving 21 women participating in a DT programme demonstrated a non-significant decrease in mental distress before and after participation in a DMT programme (t = −1.46, p = 0.16, d = −0.4) (Ho, 2015). The case study focusing on a woman diagnosed with borderline personality disorder notified similar mental health improvements (Manford, 2014). In parallel, a cross-sectional study with self-identifying conscious dancers (N = 1,003) associated the improvement in the psychological state with the flow state of participants, defined as a ‘state in which people are so involved in an activity that nothing else seems to matter; the experience itself is so enjoyable that people will do it even at great cost, for the sheer sake of doing it’ (Csikszentmihalyi, 1990) (Laird et al., 2021). Within the total sample of this study (N = 1003), N = 899 people reported one or more mental health afflictions: traumatic experience (N = 511), anxiety (N = 451), depression (N = 298), chronic pain (N = 255), and drug addiction (N = 205). Most of the 899 people in this subsample reported that conscious dance helped them to manage their mental health affliction (depression 96.3%, anxiety 96.2%, trauma 94.9%, chronic pain 89.4%, and substance abuse, 87.8%). Flow state appears as a significant facilitator for mental health improvements. The correlation between each mental health affliction variable and flow state was significant for 276 individuals in the management of depression (t(276) = 5.06, d = 1.94, p < .0001), for 434 in the management of anxiety (t(434) = 5.58, d = 1.52, p < .0001), for 482 in managing traumatic experience (t(482) = 5.84, d = 1.30, p < .0001), and for 237 in managing chronic pain (t(237) = 4.08, d = 0.91, p < .0001). This study is based on a self-report method that could induce bias in the identification of symptoms (Laird et al., 2021). However, DMT and DaT may improve the management of the symptoms of depression, anxiety, traumatic experience, and chronic pain, as the participants can enter a flow state.
3.3. Relationship
3.3.1. Relationship with others
One of the leading themes of the selected articles is the evaluation of the impact of DT on interpersonal dimensions and relationships. First, the systematic review identified the positive effect of therapeutic dance on boundary formation and interpersonal relationships (Lee et al., 2022). This has been similarly observed from the very first session of Flamenco with significant improvement in boundary perception (F = 3.19, p = .084, eta² = 0.10) and personified intersubjectivity (F = 3.37, p = .076, eta² = 0.10) (Koch et al., 2019). Four qualitative studies confirm this aspect by showing that DaT and DMT improved the construction of spatial and bodily limits, and the ability to create links with others (Fargnoli, 2017; Moe, 2014; Özümerzifon et al., 2022; Schaeffer & Cornelius-White, 2021; Verreault, 2017). These effects are facilitated by the quality of group support with DMT (Verreault, 2017) as well as the development of a sense of safety & the attention to the cultural and social characteristics of the participants with DMT and DaT (Fargnoli, 2017; Moe, 2014; Schaeffer & Cornelius-White, 2021). As demonstrated by a group case study, the presence of peers during the trauma narrative is essential (Koch & Weidinger-von der Recke, 2009). It favored sustained attention and the mirroring of the individual’s emotional state (Koch & Weidinger-von der Recke, 2009). In addition, the group setting offered a verbal and non-verbal holding function to the individual (Koch & Weidinger-von der Recke, 2009). This helps to prevent too much internal rigidity and reduces the phenomenon of dissociation while encouraging the expression of the patient’s need for space (Ko, 2017).
3.3.2. Self-expression
Investigation of self-expression through DMT and DaT was essential. In two qualitative studies and a case study, participants with psychological trauma experienced a long-lasting improvement in verbal expression, self-expression, and freedom of speech (Manford, 2014; Moe, 2014; Schaeffer & Cornelius-White, 2021). A feeling of confidence and safety facilitated these improvements (Manford, 2014; Moe, 2014; Schaeffer & Cornelius-White, 2021).
3.4. Group intervention
3.4.1. Security
When combined with the development of the ritual and symbolic aspects of DaT, the sense of security experienced in the group contributed to the development of a generalized individual sense of safety (Lee et al., 2022; Ley et al., 2017; Schaeffer & Cornelius-White, 2021; Verreault, 2017). With DMT, this sense of safety then allowed individual resources to emerge in participants (Verreault, 2017) while DaT facilitated the transition through a flow state (Schaeffer & Cornelius-White, 2021). The emergence of these associated factors should be facilitated by the permanence and the framework of the interventions (quality of the premises, geographical location, and regularity) (Schaeffer & Cornelius-White, 2021).
3.4.2. Culture
As reported by the included studies, cultural, religious, and spiritual support may facilitate the management of psychological trauma. Two qualitative studies supported this statement, showing how the subject's cultural, family, and environmental resources expanded as the subjects were involved in a DMT programme (Dieterich-Hartwell et al., 2021; Verreault, 2017). DMT and DaT could be especially useful for trauma management in a multicultural setting, as it mobilize non-verbal skills while complementing psychosocial interventions through cultural and family support (Dieterich-Hartwell et al., 2021; Koch & Weidinger-von der Recke, 2009; Özümerzifon et al., 2022; Verreault, 2017).
3.4.3. Group characteristics
Scientific literature reviewed the specific settings of group intervention. For DaT activities, duration (dance practice for more than 5 weeks vs. less than 5 weeks) and frequency (dance practice at least once a week vs. twice a month or less) were positively correlated with flow state (frequency: t(806) = 3.25, d = 0.23, p = .001, duration: t(840) = 3.11, d = 0.22, p = .002), life satisfaction (duration: t(932) = 2.94, d = 0.19, p = .003) and mindfulness (frequency: t(850) = 2.72, d = 0.19, p = .007, duration: t(932) = 7.86, d = 0.52, p < .0001) (Laird et al., 2021). The combination of long duration and high frequency of dance sessions however did not intensify their individual positive effect on the intensity of mindfulness (F (1,803) = 0.8, p = .4), life satisfaction (F(1,803) = 0.6, p = .4), and flow state (F (1,803) = 0.02, p = .9). Settings of the interventions appeared crucial to create a new healthy relationship with oneself, the group, the therapist, and the movements, for DMT and DaT (Levine & Land, 2016; Schaeffer & Cornelius-White, 2021).
Especially in DaT, the quality of these relationships depended on the ability of the therapist to consider cultural dimensions, difficulties in verbal expression, and the risk of repetition of the trauma (Schaeffer & Cornelius-White, 2021). Moreover, the quality of the relationships engaged by the subject was conditioned by the therapist's ability to identify obstacles, engage with the group, and adapt to the patients (Schaeffer & Cornelius-White, 2021). In DT, patients needed and valued the therapist’s ability to set a proper therapeutic framework through movements, mainly containing and holding functions (Schaeffer & Cornelius-White, 2021). Dance/movement therapists could particularly play a critical role in the care and must be aware of their countertransference, their use of space, and the theoretical paradigms associated with their movements (Levine & Land, 2016). From the participants and dance/movement therapists, instigation, and copying mechanisms of the movements (e.g. mirroring games, teaching, limit testing) created and nurtured the therapeutic relationship (Levine & Land, 2016). These results are supported by two case studies (Koch & Weidinger-von der Recke, 2009; Manford, 2014). However, the studies lack uniformity in assessments of adherence, its effect on therapeutic outcomes, and the therapists’ skill set.
3.5. General health
3.5.1. Well-being
Several different variables assessed well-being in quantitative studies (Ho, 2015; Koch et al., 2019; Laird et al., 2021). Among them, self-identified conscious dancers practicing for more than 5 weeks presented higher mindfulness scores (t(932) = 7.86, d = 0.52, p < .0001), higher levels of life satisfaction (t(932) = 2.94, d = 0.19, p = .003) and better flow states (t(840) = 3.11, d = 0.22, p = .002) (Laird et al., 2021). In a different sample assessed by this same study (Laird et al., 2021), self-identified conscious dancers practicing at least once a week had also higher mindfulness scores (t(850) = 2.72, d = 0.19, p = .007) and a better flow (t(806) = 3.25, d = 0.23, p = .001). However, this study does not provide information on the level of severity of the subjects’ mental health afflictions (Laird et al., 2021). Two other qualitative studies (Ley et al., 2017; Schaeffer & Cornelius-White, 2021) corroborate these results for DaT. The well-being component assessed through perceived health seemed also ameliorated by DaT, after a single session of Flamenco therapy (F = 18.71, p < .001, eta² = 0.38) (Koch et al., 2019).
Similarly, a non-randomized clinical trial reported a slight improvement in well-being through five sessions of DMT with childhood sexual abuse survivors (Ho, 2015). They focused on self-esteem and stagnation, a concept in Eastern medicine that resembles to depression in western medicine (Ho, 2015). The increase in self-esteem presented a tendency to statistical significance (t = 1.85, d = 0.3 p = .08) that did not persist 5 weeks after the end of the programme (t = 1.11, d = 0.2, p = .28). Stagnation Scale’s (Ng et al., 2006) overattachment dimension did not report a decrease in stagnation (t = −1.63, d = −0.2, p = .12) whereas a non-statistically significant tendency seemed to emerge 5 weeks after the programme (t = −1.81, d = −0.3, p = .08). A quantitative experimental study reports a similar trend, by showing that positive well-being dimensions were not significantly higher after a single session of DaT Flamenco (F = 0.60, p = .445, eta² = 0.02) (Koch et al., 2019). To ensure persistency in perceived health amelioration and observe a change in well-being, the Flamenco therapy intervention should be repeated and of longer duration. Finally, a focus group with 16 participants in 12 virtual sessions of a creative dance/movement programme identified a more relaxed state of mind and stress relief after the programme (Özümerzifon et al., 2022).
3.5.2. Physical pain
A few studies investigated the evolution of physical pain through self-report. In a large sample study (N = 1003), the majority of participants with chronic pain (n = 255), 89.4% reported being helped in the management of their pain by DaT sessions (Laird et al., 2021). Participants who reported improvement in pain management had a better flow state compared to those who reported not being helped (t (237) = 4.08, d = 0.91, p < .0001) (Laird et al., 2021). This result is complemented by the study focusing on a Flamenco session showing that when performing a dance session, participants present less physical pain (F = 4.25, p = .048, eta² = 0.12) (Koch et al., 2019). Cases study’s results also consider that not only DaT but also DMT sessions could improve emotional pain and consequently could reduce physical pain (Ko, 2017).
3.6. Psychological processes
3.6.1. Links between affects and representations
Selected case studies also report that DMT investigates the link between affects and representations through emotional expression (Ko, 2017). As physical activity allows for the expression of repressed emotions and leads to a feeling of liberation and relief, DMT could create a safe distance from emotional distress, often described as an overwhelming feeling (Manford, 2014). Both selected case studies consider these mechanisms to occur through the link made by the subject between her affects and his somatic expression (Ko, 2017; Manford, 2014). They identified the outlet function of movement (Ko, 2017) and established a correlation between physical movements and psyche movements (Manford, 2014).
3.6.2. Mental movement
Practicing DaT in a group also allowed one to explore sensorimotor perceptions, which initiated the processing of the trauma (Koch & Weidinger-von der Recke, 2009). Identifying and activating the processes at the base of the body's resources enabled the process of emotional and cognitive integration of the trauma to begin. Activation of the sensory-motor pole allowed for the reintegration of the fragmented and negatively invested body image (Koch & Weidinger-von der Recke, 2009). In addition, DMT enabled the patient to gain a sense of strength and to express intense emotions linked to past trauma (Ko, 2017). The reduction of symptoms could be associated with the reintegration of fragmented body image and the reinforcement of psyche resources. Movement could have a symbolic function when facilitating the emergence of a diversity of affects that would be subjected to interpretation (Ko, 2017).
3.7. Psychological trauma
Of the 15 selected articles, only one case study (Koch & Weidinger-von der Recke, 2009) directly reported a diminution of traumatic revivification and dissociation after a patient got enrolled in a DT programme. This diminution was due to addressing psychological trauma on a bodily level through movement and dance, which helped the patients to regain a positive relationship with their body (Koch & Weidinger-von der Recke, 2009). The authors consider that combining verbal and nonverbal processes of psychotherapy was essential for the symptom’s diminution, as well as the reconstruction of the fragmented image of the body and the reinforcement of the individual’s resources. One randomized control trial (N = 45) measured the evolution of PTSD symptoms before and after 12 virtual sessions of a creative dance/movement programme (Özümerzifon et al., 2022). The PCL-5 total scores significantly decreased over time (F(1) = 15.52, p < .001, η² = 0.275), but they found no significant difference between the intervention group (N = 25) and the control group (N = 18), receiving the usual care (F(1) = 1.093, p = .302, η² = 0.026).
No included study measured other typical symptoms such as intrusion, avoidance, disturbances in cognition and mood, and disabling changes in arousal and reactivity. Despite a lack of evidence directly focusing on symptoms of PTSD and CPTSD, selected studies provided an evaluation of the physical, psychological, and social processes affected by psychological trauma. Those key processes (relaxation, diminution of stress, interpersonal therapy, mobilization of the body) are targeted by mind–body intervention aiming at facilitating the remission of psychological trauma while being an asset in the recovery process of the subject.
4. Discussion
The 15 included studies suggest that despite not providing typical quantitative measures about symptoms of trauma, DT (DMT and DaT) appears to be a useful trauma treatment. On one hand, DT can improve the reappropriation of the body, and expression of emotions, and ameliorates the management of psychopathological symptoms in people with psychological trauma. Also, group DT seems to favor self-expression and the creation of a new relationship with others. On the other hand, the feeling of safety and the ability of participants to be in a flow state appears to facilitate the emergence of these improvements. Finally, improvements are likely associated with the skill set and training of the therapists and consistent delivery of the interventions.
As only one case study directly reported a diminution of traumatic revivifications and dissociations (Koch & Weidinger-von der Recke, 2009), it is impossible to draw general conclusions about the evolution of these trauma phenomena when treated by DT. These emerging results still need to be extensively investigated by qualitative and quantitative research that targets a reduction of PTSD and CPTSD cases, as well as a reduction in psychological trauma symptoms. Among the key traumatic aspects targeted by psychotherapeutic trauma treatments, our analysis shows that DT can improve bodily sensations, perceptions & movements, psychological processes, and interpersonal skills (Dieterich-Hartwell et al., 2021; Fargnoli, 2017; Levine & Land, 2016; Schaeffer & Cornelius-White, 2021; Verreault, 2017). These improvements led to consider that DT may be efficient in the resolution of psychological trauma and should be considered as a trauma treatment. In that context, future recommendations and guidelines devoted to psychological trauma support could also include DT as a relevant intervention particularly adjusted to diverse ethnic and cultural populations such as people affected by migration.
Among the key aspects positively improved by DT, only DMT seems to improve sensory-motor perceptions and motor skills. These results have been highlighted by other studies on DMT, especially in the case of mental health afflictions prevention policies and when applied to children with disabilities (Koch et al., 2019; May et al., 2021). It is indeed established that repeated physical activity is strongly correlated with the development of motor skills (Hirano et al., 2015). By being a potent reminder of the initial sensory-motor skills acquisition, DMT could also strengthen sensory-motor perceptions (Todd & Lee, 2015). All of those ameliorations may improve the body schema, which in turn promotes the development of motor skills (Maravita & Iriki, 2004). Positive results on this key aspect are considered a great help for psychological trauma management (Grabbe & Miller-Karas, 2018). Engaging this process could help the subject to redevelop a deep connection with its body, and sensations, known to be distanced by dissociation and amnesia (Van der Kolk, 2006). Potential emphasizes by group feedback after DMT sessions, working with mirroring, weight, rhythm, body perception exercises, and spatial reference can be applied to reinforce these effects (Koch, 2020).
DT seems to improve the identification, expression, and externalization of emotions. This is consistent with the literature on the effectiveness of DT in the general population (Koch et al., 2019; May et al., 2021; Schwender et al., 2018). As dance is a non-verbal medium, it instigates the expression of emotions through the body while initiating the process of emotional identification (San-Juan-Ferrer & Hípola, 2020). Emotional improvements fostered by DT can be particularly relevant in the case of traumatic dissociation as this pathognomonic symptom is characterized by a disruption in the integration of emotions (American Psychiatric Association, 2013). DT can then strengthen the psycho-affective state of the subject (Schaeffer & Cornelius-White, 2021). It may therefore improve the subject’s mentalization abilities frozen by sideration and, enable a reduction of the feelings of shame and guilt often expressed by individuals suffering from psychological trauma (Pugh et al., 2015; Wilson et al., 2006). To adequately address the crisis that may arise from this expression, a trauma-informed approach and credentialed practitioners are essential (Koch, 2020). Moreover, authentic movement exercises with closed eyes, group touching, and without music should be avoided in the early stages of treatment to avoid a risk of retraumatization (Koch, 2020).
A special focus is needed on the potential ameliorations brought by DT in terms of personal safety, cultural support, and the creation of new interpersonal relationships. These improvements might allow for the intrusive re-emergence of the traumatic image, linked to the traumatic memory, to be contained and processed in the group (Kruse et al., 2009). Aside from the implications of these key factors in the management and the resolution of psychological trauma (Watkins et al., 2018), it is possible that holding and containment mechanisms are key facilitators of their apparition, as theorized by Winnicott, and Bion (Bion, 1961; Karampoula & Panhofer, 2018; Winnicott, 1960). Through these mechanisms, the presence of the group (Koch et al., 2019), synchronization of the music, and creation of a specific group identity can facilitate these improvements. Unity of time, place, and space of the group may also contributes to the development of participants’ sense of security (Sloan et al., 2013). Finally, combined with holding mechanisms, improvement in cultural support can be associated with individual development and cultural belonging intertwined with music and dance (Clarke et al., 2015). Cultural support and a sense of safety can be even more important for people facing migration (Kira & Tummala-Narra, 2015). These mechanisms should be highly regarded by clinicians and dance therapists, considering that the quality of the group is important in the resolution of psychological trauma (Koch et al., 2019).
Finally, to improve the effectiveness of DT in the management of psychological trauma, clinicians, dance/movement therapists, and dance facilitators should pay attention to specific settings inherent to the intervention. For example, the effects of physical activity through DT depend on the context (White et al., 2017), the regularity, and the intensity of the activity (Chastin et al., 2021). Therefore, planning the DT interventions should provide a better therapeutic setting. Reaching a flow state also facilitates the management of psychological trauma as it may reduce excessive self-consciousness (Riva et al., 2016). Within the group, professionals should be aware of their own skill set, and deploy interventions that encompass a better entrance in the flow state for their participants. However, the severity of the trauma varies (the form of trauma e.g. PTSD, CPTSD, type of traumatic event, age, symptoms, and their duration), and entering a deep flow state at an early stage of treatment might be threatening to some patients. Consequently, compared to non-trained facilitators’ specialized trauma training makes a significant difference in trauma treatment.
4.1. Recommendations
Based on the results of this systematic review, some recommendations for research and practice can be considered. First, to complement the results of this qualitative systematic review, further quantitative, and qualitative research on the impact of DT interventions as a trauma treatment should be conducted. This research could incorporate more standardized measures (especially regarding PTSD and pathognomonic symptoms of psychological trauma), long-term follow-up (six months and more), standardized protocols (randomized control trials, semi-structured interviews), diversified populations (men, non-binary adults, broader type of traumatic events), and larger samples. When DT is applied as a trauma treatment, quantitative and qualitative research could further explore the emotional register, characteristics of the movement, and evolution of mental health afflictions associated with psychological trauma. Regarding DT practice for the management of psychological trauma, mental health professionals should particularly ensure the stability of their intervention (unity of time, space, and place), the quality of the group, and their patients’ flow state. A trauma-informed approach and specialized training are strongly recommended for the practitioners.
4.2. Strengths and limitations
The systematic article search was conducted on seven databases, in English and French. Quantitative, qualitative, and case studies were included, allowing for a fine-grained and complex analysis of the results. Bias analysis, performed by two researchers using two tools (NIH quality study assessment tools (National Institutes of Health, 2014) and JBI critical appraisal checklists (Aromataris & Munn, 2020)), allowed the exclusion of studies with too much bias. Transparency in the reporting of the synthesized estimated effects is ensured through the presentation and discussion of the results according to the SWiM protocol (Campbell et al., 2020). The small number of available studies, the diversity in variables, and the need for further quantitative research are the main limitations of our study.
5. Conclusion
DT seems to be a promising trauma treatment, as it mobilizes the key factors involved in the management of psychological trauma (body, relaxation, diminution of stress, and interpersonal therapy). Positive effect on these factors mainly depends on the group’s quality, the stability of the intervention, and the patient’s flow state. A distinct difference is to be made between DaT and DMT. DaT does not require a specialized trained and credentialed dance therapist. The efficacy of DT interventions is likely correlated with the therapist's skill set and training, yet the studies lacked uniformity in assessments of adherence and skill to present generalized information on this point. Improvement of the motor skills, mobilization of the individual resources, and link between affects and representations are only observed with DMT. Nevertheless, due to the paucity of research in this field, these observed effects can not be generalized yet. Further studies about the effect of DaT and DMT as a trauma treatment should be conducted with standardized measures and protocol, long-term follow-up, and a diversified and larger sample.
Acknowledgments
We thank the LOBA association for granting us the funds and time necessary for this project.
Supplementary Material
Funding Statement
The lead researcher, Crystal Tomaszewski, and Heloise Onumba-Bessonnet are funded by the LOBA association, which launched a dance-therapy protocol. C.T. and H.O-B. are funded by the LOBA Association [grant number: 126000].
Disclosure statement
The lead researcher, Crystal Tomaszewski, and Heloise Onumba-Bessonnet are funded by the LOBA association, which launched a dance-therapy protocol. The other author(s) declare no potential conflicts of interest concerning this article's research, authorship, and publication.
Authors’ contributions
C.T. and C.C. conceived and designed the analysis and collected the data. C.T., C.C., R-A.B., and A. E. performed the analysis. C.T. and C.C. wrote the paper with input from all authors. CC directed and supervised the work on this paper. All authors reviewed the results and approved the final version of the manuscript.
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
- American Dance Therapy Association . (2023). What is Dance/movement Therapy? ADTA. https://www.adta.org/.
- American Psychiatric Association . (2013). Diagnostic and Statistical Manual of Mental Disorders: Dsm-5 (5th edition. Washington, DC: Author. [Google Scholar]
- Aromataris, E., & Munn, Z. (Eds.). (2020). JBI Manual for Evidence Synthises. JBI. 10.46658/JBIMES-20-01 [DOI] [Google Scholar]
- Bassuk, E. L., Dawson, R., Perloff, J., & Weinreb, L. (2001). Post-traumatic stress disorder in extremely poor women: Implications for health care clinicians. Journal of the American Medical Women’s Association (1972), 56(2), 79–85. [PubMed] [Google Scholar]
- Bion, W.-R. (1961). Experiences in Groups and Other Papers. Tavistock. [Google Scholar]
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun, V., & Clarke, V. (2021). One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 18(3), 328–352. 10.1080/14780887.2020.1769238 [DOI] [Google Scholar]
- Bustamante, L. H. U., Cerqueira, R. O., Leclerc, E., & Brietzke, E. (2018). Stress, trauma, and posttraumatic stress disorder in migrants: A comprehensive review. Revista Brasileira de Psiquiatria, 40(2), 220–225. 10.1590/1516-4446-2017-2290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, M., McKenzie, J. E., Sowden, A., Katikireddi, S. V., Brennan, S. E., Ellis, S., Hartmann-Boyce, J., Ryan, R., Shepperd, S., Thomas, J., Welch, V., & Thomson, H. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ, 368, Article l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chastin, S. F. M., Abaraogu, U., Bourgois, J. G., Dall, P. M., Darnborough, J., Duncan, E., Dumortier, J., Pavón, D. J., McParland, J., Roberts, N. J., & Hamer, M. (2021). Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: Systematic review and meta-analysis. Sports Medicine, 51, 1673–1686. 10.1007/s40279-021-01466-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, E., DeNora, T., & Vuoskoski, J. (2015). Music, empathy and cultural understanding. Physics of Life Reviews, 15, 61–88. 10.1016/j.plrev.2015.09.001 [DOI] [PubMed] [Google Scholar]
- Colace, E. (2017). Dance movement therapy and developmental trauma: dissociation and enactment in a clinical case study. Body, Movement and Dance in Psychotherapy, 12(1), 36–49. 10.1080/17432979.2016.1247115 [DOI] [Google Scholar]
- Csikszentmihalyi, M. (1990). Flow: The Psychology of Optimal Experience. Harper Perennial. https://eduq.info/xmlui/handle/11515/34667. [Google Scholar]
- Deeks, J., Higgins, J., & Altman, D. (Eds.). (2022). Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions. https://training.cochrane.org/handbook/current/chapter-10 [Google Scholar]
- Dieterich-Hartwell, R., Haen, C., Kaimal, G., Koch, S., Villanueva, A., & Goodill, S. (2021). Developing movement experiences with refugees to the United States who have undergone trauma. International Journal of Migration, Health and Social Care, 17(1), 75–91. 10.1108/IJMHSC-04-2020-0036 [DOI] [Google Scholar]
- Dunphy, K., Elton, M., & Jordan, A. (2014). Exploring dance/movement therapy in post-conflict timor-leste. American Journal of Dance Therapy, 36, 189–208. 10.1007/s10465-014-91 [DOI] [Google Scholar]
- Dunphy, K., Federman, D., Fischman, D., Gray, A., Puxeddu, V., Zhou, T. Y., & Dumaresq, E. (2022). Dance therapy today: An overview of the profession and Its practice around the world. Creative Arts in Education and Therapy, 7(2), 158–186. 10.15212/CAET/2021/7/13 [DOI] [Google Scholar]
- Fargnoli, A. (2017). Maintaining stability in the face of adversity: Self-care practices of human trafficking survivor-trainers in India. American Journal of Dance Therapy, 39(2), 226–251. 10.1007/s10465-017-9262-4 [DOI] [Google Scholar]
- Grabbe, L., & Miller-Karas, E. (2018). The trauma resiliency model: A “bottom-Up” intervention for trauma psychotherapy. Journal of the American Psychiatric Nurses Association, 24(1), 76–84. 10.1177/1078390317745133 [DOI] [PubMed] [Google Scholar]
- Green, B. L., Saunders, P. A., Power, E., Dass-Brailsford, P., Schelbert, K. B., Giller, E., Wissow, L., Hurtado de Mendoza, A., & Mete, M. (2016). Trauma-Informed medical care: Patient response to a primary care provider communication training. Journal of Loss and Trauma, 21(2), 147–159. 10.1080/15325024.2015.1084854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillis, S., Mercy, J., Amobi, A., & Kress, H. (2016). Global prevalence of past-year violence against children: A systematic review and minimum estimates. Pediatrics, 137. 10.1542/peds.2015-4079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirano, M., Kubota, S., Tanabe, S., Koizume, Y., & Funase, K. (2015). Interactions Among learning stage, retention, and primary motor cortex excitability in motor skill learning. Brain Stimulation, 8(6), 1195–1204. 10.1016/j.brs.2015.07.025 [DOI] [PubMed] [Google Scholar]
- Ho, R. T. H. (2015). A place and space to survive: A dance/movement therapy program for childhood sexual abuse survivors. The Arts in Psychotherapy, 46, 9–16. 10.1016/j.aip.2015.09.004 [DOI] [Google Scholar]
- Karampoula, E., & Panhofer, H. (2018). The circle in dance movement therapy: A literature review. The Arts in Psychotherapy, 58, 27–32. 10.1016/j.aip.2018.02.004 [DOI] [Google Scholar]
- Kira, I. A., & Tummala-Narra, P. (2015). Psychotherapy with refugees: Emerging paradigm. Journal of Loss and Trauma, 20(5), 449–467. 10.1080/15325024.2014.949145 [DOI] [Google Scholar]
- Ko, K. S. (2017). A broken heart from a wounded land: The use of Korean scarf dance as a dance/movement therapy intervention for a Korean woman with haan. The Arts in Psychotherapy, 55, 64–72. 10.1016/j.aip.2017.04.002 [DOI] [Google Scholar]
- Koch, S. C. (2020). Indications and contraindications in dance movement therapy: Learning from practitioners’ experience. GMS Journal of Arts Therapies, 1. 10.3205/JAT000006 [DOI] [Google Scholar]
- Koch, S. C., Riege, R. F. F., Tisborn, K., Biondo, J., Martin, L., & Beelmann, A. (2019). Effects of dance movement therapy and dance on health-related psychological outcomes. A meta-analysis update. Frontiers in Psychology, 10. https://www.frontiersin.org/article/10.3389fpsyg.2019.01806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch, S. C., & Weidinger-von der Recke, B. (2009). Traumatised refugees: An integrated dance and verbal therapy approach. The Arts in Psychotherapy, 36(5), 289–296. . 10.1016/j.aip.2009.07.002 [DOI] [Google Scholar]
- Koch, S. C., Wirtz, G., Harter, C., Weisbrod, M., Winkler, F., Pröger, A., & Herpertz, S. C. (2019). Embodied self in trauma and self-harm: A pilot study of effects of flamenco therapy on traumatized inpatients. Journal of Loss and Trauma, 24(5-6), 441–459. 10.1080/15325024.2018.1507472. [DOI] [Google Scholar]
- Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., Karam, E. G., Meron Ruscio, A., Benjet, C., Scott, K., Atwoli, L., Petukhova, M., Lim, C. C. W., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Bunting, B., Ciutan, M., … Kessler, R. C. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. 10.1017/S0033291717000708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse, J., Joksimovic, L., Cavka, M., Wöller, W., & Schmitz, N. (2009). Effects of trauma-focused psychotherapy upon war refugees. Journal of Traumatic Stress, 22(6), 585–592. 10.1002/jts.20477 [DOI] [PubMed] [Google Scholar]
- Laird, K. T., Vergeer, I., Hennelly, S. E., & Siddarth, P. (2021). Conscious dance: Perceived benefits and psychological well-being of participants. Complementary Therapies in Clinical Practice, 44, 101440. 10.1016/j.ctcp.2021.101440 [DOI] [PubMed] [Google Scholar]
- Lee, J., Dhauna, J., Silvers, J. A., Houston, M. H., & Barnert, E. S. (2022). Therapeutic dance for the healing of sexual trauma: A systematic review. Trauma, Violence, & Abuse, 1–22. 10.1177/15248380221086898 [DOI] [PubMed] [Google Scholar]
- Levine, B., & Land, H. M. (2016). A meta-synthesis of qualitative findings about dance/movement therapy for individuals With trauma. Qualitative Health Research, 26(3), 330–344. Medline. 10.1177/1049732315589920. [DOI] [PubMed] [Google Scholar]
- Ley, C., Krammer, J., Lippert, D., & Rato Barrio, M. (2017). Exploring flow in sport and exercise therapy with war and torture survivors. Mental Health and Physical Activity, 12, 83–93. 10.1016/j.mhpa.2017.03.002 [DOI] [Google Scholar]
- Lindert, J., Ehrenstein, O. S., von, Priebe, S., Mielck, A., & Brähler, E. (2009). Depression and anxiety in labor migrants and refugees – A systematic review and meta-analysis. Social Science & Medicine, 69(2), 246–257. 10.1016/j.socscimed.2009.04.032 [DOI] [PubMed] [Google Scholar]
- Manford, B. (2014). Insecure attachment and borderline personality disorder: Working with dissociation and the ‘capacity to think’. Body, Movement and Dance in Psychotherapy, 9(2), 93–105. Embase. 10.1080/17432979.2014.891261 [DOI] [Google Scholar]
- Maravita, A., & Iriki, A. (2004). Tools for the body (schema). Trends in Cognitive Sciences, 8(2), 79–86. 10.1016/j.tics.2003.12.008 [DOI] [PubMed] [Google Scholar]
- May, T., Chan, E. S., Lindor, E., McGinley, J., Skouteris, H., Austin, D., McGillivray, J., & Rinehart, N. J. (2021). Physical, cognitive, psychological and social effects of dance in children with disabilities: Systematic review and meta-analysis. Disability and Rehabilitation, 43(1), 13–26. 10.1080/09638288.2019.1615139 [DOI] [PubMed] [Google Scholar]
- Mesa-Vieira, C., Haas, A. D., Buitrago-Garcia, D., Roa-Diaz, Z. M., Minder, B., Gamba, M., Salvador, D., Gomez, D., Lewis, M., Gonzalez-Jaramillo, W. C., Mortanges, A. P., de, Buttia, C., Muka, T., Trujillo, N., & Franco, O. H. (2022). Mental health of migrants with pre-migration exposure to armed conflict: A systematic review and meta-analysis. The Lancet Public Health, 7(5), e469–e481. 10.1016/S2468-2667(22)00061-5 [DOI] [PubMed] [Google Scholar]
- Millman, L. S. M., Terhune, D. B., Hunter, E. C. M., & Orgs, G. (2021). Towards a neurocognitive approach to dance movement therapy for mental health: A systematic review. Clinical Psychology & Psychotherapy, 28(1), 24–38. 10.1002/cpp.2490 [DOI] [PubMed] [Google Scholar]
- Moe, A. (2014). Healing through movement. Affilia, 29(3), 326–339. 10.1177/0886109913516454 [DOI] [Google Scholar]
- National Institutes of Health . (2014). Study Quality Assessment Tools NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- Ng, S., Chan, C., Ho, D., Wong, Y., & Ho, R. (2006). Stagnation as a distinct clinical syndrome: Comparing ‘Yu' (stagnation) in traditional Chinese medicine with depression. British Journal of Social Work, 36(3), 467–484. 10.1093/bjsw/bcl008 [DOI] [Google Scholar]
- O’Donnell, C. J., Schwartz Longacre, L., Cohen, B. E., Fayad, Z. A., Gillespie, C. F., Liberzon, I., Pathak, G. A., Polimanti, R., Risbrough, V., Ursano, R. J., Vander Heide, R. S., Yancy, C. W., Vaccarino, V., Sopko, G., & Stein, M. B. (2021). Posttraumatic stress disorder and cardiovascular disease. JAMA Cardiology, 6(10), 1207–1216. 10.1001/jamacardio.2021.2530 [DOI] [PubMed] [Google Scholar]
- Ouzzani, M., Hammady, H., Federowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. 5(210). 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed]
- Özümerzifon, Y., Ross, A., Brinza, T., Gibney, G., & Garber, C. E. (2022). Exploring a dance/movement program on mental health and well-being in survivors of intimate partner violence during a pandemic. Frontiers in Psychiatry, (13), 10.3389/fpsyt.2022.887827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrotta, G. (2020). Psychological trauma: Definition, clinical contexts, neural correlations and therapeutic approaches. Recent Discoveries. Curr Res Psychiatry Brain Disord, 2019(01). [Google Scholar]
- Pessoa, R., Neves, C., & Caputo Ferreira, M. (2019). Dance therapy in aging: A systematic review. Journal of Physical Education and Sport, 2019((02|2)), 1180–1187. 10.7752/jpes.2019.02171 [DOI] [Google Scholar]
- Pierce, L. (2014). The integrative power of dance/movement therapy: Implications for the treatment of dissociation and developmental trauma. The Arts in Psychotherapy, 41(1), 7–15. 10.1016/j.aip.2013.10.002 [DOI] [Google Scholar]
- Pugh, L. R., Taylor, P. J., & Berry, K. (2015). The role of guilt in the development of post-traumatic stress disorder: A systematic review. Journal of Affective Disorders, 182, 138–150. 10.1016/j.jad.2015.04.026 [DOI] [PubMed] [Google Scholar]
- Ritter, M., & Low, K. G. (1996). Effects of dance/movement therapy: A meta-analysis. The Arts in Psychotherapy, 23(3), 249–260. 10.1016/0197-4556(96)00027-5 [DOI] [Google Scholar]
- Riva, E., Freire, T., & Bassi, M. (2016). The flow experience in clinical settings: Applications in psychotherapy and mental health rehabilitation. In Harmat L., Ørsted Andersen F., Ullén F., Wright J., & Sadlo G. (Eds.), Flow Experience: Empirical Research and Applications (pp. 309–326). Springer International Publishing. 10.1007/978-3-319-28634-1_19 [DOI] [Google Scholar]
- San-Juan-Ferrer, B., & Hípola, P. (2020). Emotional intelligence and dance: A systematic review. Research in Dance Education, 21(1), 57–81. 10.1080/14647893.2019.1708890 [DOI] [Google Scholar]
- Schaeffer, A. J., & Cornelius-White, J. H. D. (2021). Qualitative studies on body-based interventions for refugees: A meta-synthesis. Body, Movement and Dance in Psychotherapy, 16(4), 267–285. Embase. 10.1080/17432979.2021.1893810 [DOI] [Google Scholar]
- Schwender, T. M., Spengler, S., Oedl, C., & Mess, F. (2018). Effects of dance interventions on aspects of the participants’ self: A systematic review. Frontiers in Psychology, 9(1130), 1–25. 10.3389/fpsyg.2018.01130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan, D. M., Feinstein, B. A., Gallagher, M. W., Beck, J. G., & Keane, T. M. (2013). Efficacy of group treatment for posttraumatic stress disorder symptoms: A meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 5(2), 176–183. 10.1037/a0026291 [DOI] [Google Scholar]
- Taylor, J., McLean, L., Korner, A., Stratton, E., & Glozier, N. (2020). Mindfulness and yoga for psychological trauma: Systematic review and meta-analysis. Journal of Trauma & Dissociation, 21(5), 536–573. 10.1080/15299732.2020.1760167 [DOI] [PubMed] [Google Scholar]
- Todd, N., & Lee, C. (2015). The sensory-motor theory of rhythm and beat induction 20 years on: A new synthesis and future perspectives. Frontiers in Human Neuroscience, 9, 1–25. https://www.frontiersin.org/articles/10.3389fnhum.2015.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VA/DOD . (2017). VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf. [DOI] [PMC free article] [PubMed]
- Van de Kamp, M. M., Scheffers, M., Hatzmann, J., Emck, C., Cuijpers, P., & Beek, P. J. (2019). Body- and movement-oriented interventions for posttraumatic stress disorder: A systematic review and meta-analysis. Journal of Traumatic Stress, 32(6), 967–976. 10.1002/jts.22465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Kolk, B. A. (2006). Clinical implications of neuroscience research in PTSD. Annals of the New York Academy of Sciences, 1071(1), 277–293. 10.1196/annals.1364.022 [DOI] [PubMed] [Google Scholar]
- Verreault, K. (2017). Dance/movement therapy and resilience building with female asylum seekers and refugees. Intervention, 15(2), 120–135. 10.1097/WTF.0000000000000150 [DOI] [Google Scholar]
- Wang, L., Sun, C., Wang, Y., Zhan, T., Yuan, J., Niu, C.-Y., Yang, J., Huang, S., & Cheng, L. (2022). Effects of dance therapy on non-motor symptoms in patients with Parkinson’s disease: A systematic review and meta-analysis. Aging Clinical and Experimental Research, 34(6), 1201–1208. 10.1007/s40520-021-02030-7 [DOI] [PubMed] [Google Scholar]
- Watkins, L. E., Sprang, K. R., & Rothbaum, B. O. (2018). Treating PTSD: A review of evidence-based psychotherapy interventions. Frontiers in Behavioral Neuroscience, 12, 1–9. 10.3389/fnbeh.2018.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, R. L., Babic, M. J., Parker, P. D., Lubans, D. R., Astell-Burt, T., & Lonsdale, C. (2017). Domain-Specific physical activity and mental health: A meta-analysis. American Journal of Preventive Medicine, 52(5), 653–666. 10.1016/j.amepre.2016.12.008 [DOI] [PubMed] [Google Scholar]
- Wilson, J. P., Droždek, B., & Turkovic, S. (2006). Posttraumatic shame and guilt. Trauma, Violence, & Abuse, 7(2), 122–141. 10.1177/1524838005285914 [DOI] [PubMed] [Google Scholar]
- Winnicott, D. W. (1960). The theory of parent-infant relationship. International Journal of Psycho-Analysis, 41, 585–595. [PubMed] [Google Scholar]
- World Health Organization . (2019). International classification of diseases, Eleventh Revision (ICD-11). https://icd.who.int/browse11.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.