Abstract
Introduction
The COVID-19 pandemic presented extraordinary challenges to the UK healthcare system. This study aimed to assess the impact of the COVID-19 lockdown on the epidemiology, treatment pathways and 30-day mortality rates of hip fractures. Outcomes of COVID-19 positive patients were compared against those who tested negative.
Methods
An observational, retrospective, multicentre study was conducted across six hospitals in the South East of England. Data were retrieved from the National Hip Fracture Database and electronic medical records. Data was collected for the strictest UK lockdown period (period B=23 March 2020–11 May 2020), and the corresponding period in 2019 (period A).
Results
A total of 386 patients were admitted during period A, whereas 381 were admitted during period B. Despite the suspension of the ‘Best Practice Tariff’ during period B, time to surgery, time to orthogeriatric assessment, and 30-day mortality were similar between period A and B. The length of inpatient stay was significantly shorter during period B (11.5 days vs 17.0 days, p<0.001). Comparison of COVID-19 positive and negative patients during period B demonstrated that a positive test was associated with a significantly higher rate of 30-day mortality (53.6% vs 6.7%), surgical delay >36h (46.4% vs 30.8%, p=0.049), and increased length of inpatient stay (15.8 vs 11.7 days, p=0.015).
Conclusions
The COVID-19 lockdown did not alter the epidemiology of hip fractures. A substantially higher mortality rate was observed among patients with a COVID-19 positive test. These findings should be taken into consideration by the healthcare policymakers while formulating contingency plans for a potential ‘second wave’.
Keywords: COVID-19, SARS-CoV-2, Coronavirus, Proximal femur fractures, Trauma
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic, caused by the Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has resulted in unprecedented global health and socioeconomic crisis. The UK has been one of the worst affected nations, registering 47,340 deaths and 1,057,045 confirmed cases to date.1 To contain the spread of the virus, the UK government instructed a national lockdown on 23 March 2020, enforcing the closure of schools, nonessential businesses, and restrictions to freedom of movement.2 To prevent the NHS from becoming overwhelmed by the anticipated surge of patients infected with COVID-19, healthcare resources were redirected towards acute medical and critical care services.3 Elective operating lists were suspended from 17 March 2020 to allow repurposing of operating theatres as critical care areas, and to facilitate deployment of anaesthetists and operating department practitioners to the intensive care units.4 These adaptations posed significant challenges to Trauma and Orthopaedic (T&O) departments nationally, resulting in reduced operative capacity.3
The annual incidence of hip fractures in the UK is approximately 76,000.5 These patients commonly have multiple comorbidities including cardiovascular, respiratory, renal and endocrine (diabetes) disease.6,7 A significant proportion of these patients also have pre-existing cognitive impairment and frequently present from residential or nursing care.5 These risk factors have been shown to be associated with a significantly higher risk of mortality from COVID-19 infection.8 Optimal management of these complex injuries during the pandemic was complicated by the evolving national guidance on testing, lack of operating theatre availability, transient shortages of personal protective equipment and unfamiliarity with the COVID-19 protocols.3 Despite these barriers, the widely recognised benefits of early surgery and swift postoperative mobilisation provided the impetus to continue providing prompt surgical care for patients with fragility hip fractures.9,10
Analysis of epidemiological patterns of commonly occurring public health problems during the pandemic provides vital information to guide future contingency plans. This multicentre study aimed to evaluate the impact of the COVID-19 pandemic on the epidemiology of fragility hip fractures during the strictest UK lockdown period, at the time of study, in the South East of England. Secondly, the treatment pathway and 30-day mortality rate in patients admitted during the lockdown versus those admitted during the same period in 2019 were also assessed. As a final objective, patient characteristics, treatment and early postoperative outcomes were also compared between patients who tested positive for COVID-19 on admission and those who tested negative during the lockdown period.
Methods
Study design
This was an observational, multicentre, retrospective cohort study conducted at six NHS hospitals across the South East of England. The participating units consisted of one major trauma centre and five district general hospitals. These hospitals provide acute orthopaedic trauma services to a combined population of 2.25 million.11 Two different study periods were investigated; period B represented the period of strictest lockdown between 23 March 2020 and 11 May 2020 (50 days), whereas period A corresponded to the same dates as period B in the past year, ie 23 March 2019 to 11 May 2019. This study was approved by the institutional review board at each participating hospital.
Study population
The inclusion criteria consisted of the following:
-
(a)
Patients admitted with hip fractures over the age of 60 years.
-
(b)
Intracapsular neck of femur fractures, trochanteric fractures, and subtrochanteric fractures (proximal third of the femur).
The exclusion criteria were as follows:
-
(a)
Patients under the age of 60 years.
-
(b)
Open proximal femur fractures.
-
(c)
Fractures due to polytrauma.
-
(d)
Periprosthetic femur fractures and fractures that are distal to the proximal third of the femur.
Data collection
Data were collected retrospectively from the National Hip Fracture Database (NHFD) at each participating hospital. NHFD is a national hip fracture registry that audits hip fracture care in 175 trauma units in England, Wales and Northern Ireland against six evidence-based standards set out by British Geriatrics Society (BGS) and the British Orthopaedic Association (BOA).5 The collected data were assessed for accuracy and, where necessary, it was checked against electronic medical records. Incomplete entries were excluded from the analysis. For data analysis, all patient identifiable data were anonymised.
Data relating to patient demographics, treatment and postoperative outcomes were collected. Demographic variables included age, gender, American Society of Anaesthesiologists (ASA) grade, preoperative Abbreviated Mental Test Score (AMTS), pre-admission residence and fracture type. Data pertaining to treatment included date and time of admission, time to surgery, time to orthogeriatric assessment, and type of treatment (surgical and nonsurgical). Postoperative outcomes comprise of length of inpatient stay, return to theatre and 30-day mortality. The results of the COVID-19 tests (oropharyngeal and nasopharyngeal swabs for SARS-CoV-2 RNA reverse transcriptase polymerase chain reaction (RT-PCR)) performed at the time of admission for patients presenting during period B were collected from local electronic records at each institution.
Statistical methods
Statistical analysis was performed using JASP version 0.12.2.0 (https://jasp-stats.org/). Patient demographics, treatment, and outcomes were compared between period A and period B. Additionally, similar analysis was undertaken to compare patients with COVID-19 positive and negative test results admitted during period B. Continuous variables were presented as mean and standard deviation (SD). Independent samples t-test was used to compare continuous variables with normal distribution, whereas the Mann–Whitney U test was used to compare non-normally distributed data. Categorical variables were reported as absolute numbers and percentages. Pearson chi-square test was used to compare categorical variables. A p-value<0.05 was considered statistically significant.
Results
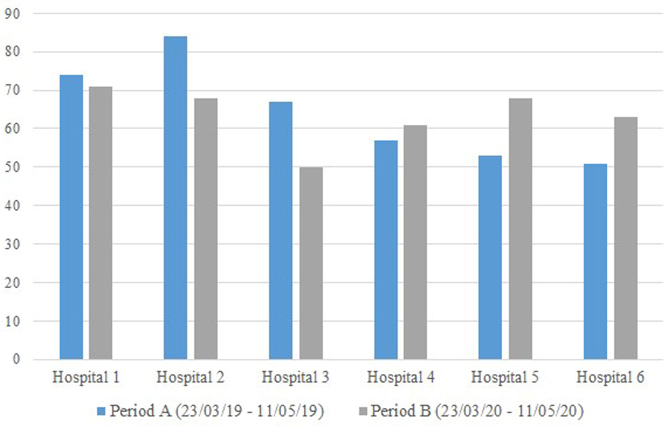
Overall, 767 records were identified; 386 patients were admitted with a hip fracture during period A, whereas 381 were admitted during period B. The difference in the number of admissions between period A and period B at each participating hospital is summarised in Figure 1.
Figure 1 .
Comparison of number of hip fractures admitted at each participating unit during period A and period B.
Period A versus period B
After excluding 32 incomplete entries, 735 records were available for data analyses (period A=380, period B=355). In terms of patient demographics, there were no significant differences in mean age, gender, ASA grade, preoperative AMTS score and pre-admission residence between patients admitted during period A and B. There was a significant difference in the type of fracture sustained among patients during period A and period B, ie there was a higher proportion of intracapsular neck of femur fractures and lower proportion of trochanteric and subtrochanteric fractures in period B, p=0.039. With regards to treatment, no significant differences were found between both groups in the time to surgery, time to orthogeriatric assessment and type of treatment provided (Table 1).
Table 1 .
Comparison between hip fractures admitted during period A and period B
| Period A | Period B | p-value | |
|---|---|---|---|
| Total number of hip fractures (n) | 380 | 355 | |
| Mean age (SD) | 83.7 (8.8) | 83.5 (8.1) | 0.743 |
| Gender | |||
| Female | 276 (72.6%) | 242 (68.2%) | 0.185 |
| Male | 104 (27.4%) | 113 (31.8%) | |
| ASA Grade | |||
| 1 | 3 (0.8%) | 2 (0.6%) | 0.158 |
| 2 | 103 (27.1%) | 74 (20.8%) | |
| 3 | 219 (57.6%) | 213 (60.0%) | |
| 4 | 55 (14.5%) | 66 (18.6%) | |
| Preoperative AMTS | |||
| 0–6 | 100 (26.3%) | 113 (31.8%) | 0.1 |
| 7–10 | 280 (73.7%) | 242 (68.2%) | |
| Pre-admission residence | |||
| Nursing care | 36 (9.5%) | 32 (9.0%) | 0.967 |
| Own home/sheltered housing | 310 (81.6%) | 290 (81.7%) | |
| Residential care | 34 (8.9%) | 33 (9.3%) | |
| Fracture type | |||
| Intracapsular – displaced | 172 (45.3%) | 198 (55.8%) | 0.039 |
| Intracapsular – undisplaced | 37 (9.7%) | 28 (7.9%) | |
| Subtrochanteric | 19 (5.0%) | 12 (3.4%) | |
| Trochanteric - grade A1/A2 | 128 (33.7%) | 105 (29.6%) | |
| Trochanteric - grade A3 | 24 (6.3%) | 12 (3.4%) | |
| Mean time to surgery - hours (SD) | 31.7 (35.4) | 31.3 (24.7) | 0.865 |
| Delay in surgery >36h? | |||
| No | 273 (71.8%) | 241 (67.9%) | 0.235 |
| Yes | 102 (26.8%) | 112 (31.5%) | |
| N/A – surgery not performed | 5 (1.3%) | 2 (0.6%) | |
| Mean time to orthogeriatric assessment – hours (SD) | 31.1 (31.5) | 28.2 (26.2) | 0.187 |
| Treatment | |||
| Hemiarthroplasty (cemented) | 137 (36.1%) | 166 (46.8%) | 0.103 |
| Hemiarthroplasty (uncemented) | 10 (2.6%) | 16 (4.5%) | |
| Cannulated hip screws | 18 (4.7%) | 13 (3.7%) | |
| Dynamic hip screw | 105 (27.6%) | 84 (23.7%) | |
| Long intramedullary nail | 40 (10.5%) | 33 (9.3%) | |
| Short intramedullary nail | 33 (8.7%) | 23 (6.5%) | |
| Total hip replacement (cemented) | 12 (3.2%) | 5 (1.4%) | |
| Total hip replacement (hybrid) | 15 (3.9%) | 10 (2.8%) | |
| Total hip replacement (uncemented) | 5 (1.3%) | 3 (0.8%) | |
| Nonsurgical treatment | 5 (1.3%) | 2 (0.6%) | |
| Mean length of inpatient stay – days (SD) | 17.0 (11.0) | 11.5 (8.1) | <0.001 |
| Return to operating theatre (%) | 5 (1.3%) | 2 (0.6%) | 0.329 |
| 30-day mortality (%) | 45 (11.8%) | 37 (10.4%) | 0.541 |
| Discharge destination | |||
| Death during inpatient admission | 28 (7.4%) | 36 (10.1%) | 0.046 |
| Nursing care | 51 (13.4%) | 27 (7.6%) | |
| Own home/sheltered housing | 190 (50.0%) | 159 (44.8%) | |
| Rehabilitation unit | 82 (21.6%) | 103 (29.0%) | |
| Residential care | 23 (6.1%) | 23 (6.5%) | |
| Transfer to another acute hospital | 3 (0.8%) | 3 (0.8%) | |
| Other | 3 (0.8%) | 4 (1.1%) | |
| Discharge to pre-admission residence? | |||
| No | 151 (39.7%) | 156 (43.9%) | 0.248 |
| Yes | 229 (60.3%) | 199 (56.1%) | |
ASA = American Society of Anaesthesiologists; AMTS = abbreviated mental test score; SD = standard deviation
Postoperatively, there were no significant differences in the 30-day mortality and unplanned return to the operating theatre. The mean length of inpatient stay was significantly shorter during period B, ie 11.5 days compared with 17.0 days in period A, p<0.001. Additionally, there was a significant difference in the discharge destination between the two groups; during period B, a higher proportion of patients were discharged to rehabilitation units and a lower proportion were discharged to their own homes or nursing care compared with period A, p=0.046 (Table 1).
COVID-19 negative versus COVID-19 positive patients during period B
A total of 381 patients were admitted during period B, of which 355 complete records were available for analyses; 32% (113/355) of the patients were not tested for COVID-19 on admission, while 60% (214/355) tested negative and 8% (28/355) tested positive (Figure 2).
Figure 2 .
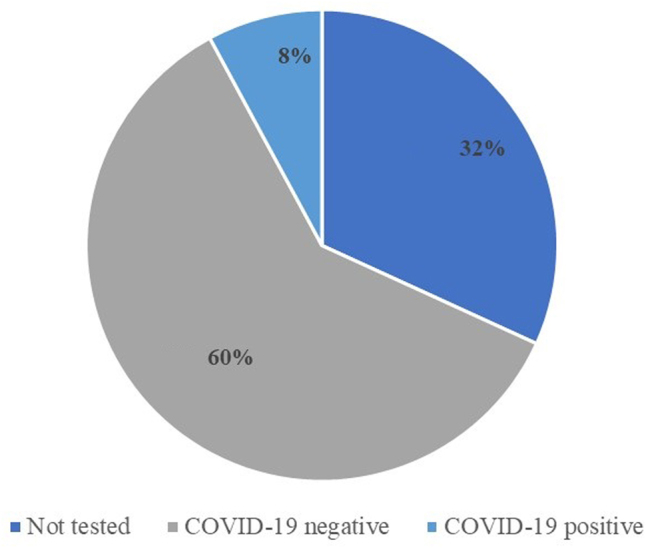
Pie chart demonstrating the COVID-19 test status on admission (period B).
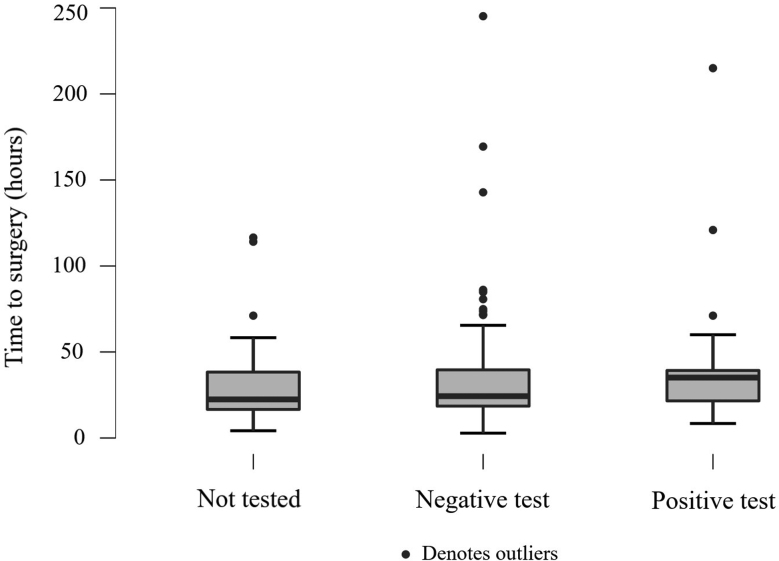
No significant differences were identified in gender, ASA grade, preoperative AMTS score and pre-admission residence between patients who tested positive and those who tested negative for COVID-19 on admission. Patients who tested positive were significantly older (87.2 vs 83.4 years, p=0.021) and sustained a higher proportion of trochanteric A1/A2 fractures and lower proportion of intracapsular neck of femur fractures, p=0.024. A significantly higher percentage of COVID-19 positive patients waited longer than 36h for surgery (46.4% vs 30.8%, p=0.049) (Table 2 and Figure 3). The length of inpatient stay was significantly longer in these patients (15.8 in COVID-19 positive versus 11.7 days in COVID-19 negative, p=0.015), with lower rates of discharge to their pre-admission residence (28.6% vs 58.4%, p=0.002). The 30-day mortality rate among the COVID-19 positive patients was 53.6%, which was significantly higher than those who tested negative (6.7%), p<0.001 (Table 2).
Table 2 .
Comparison between COVID-19 positive vs. COVID-19 negative patients in period B
| COVID-19 negative | COVID-19 positive | p-value | |
|---|---|---|---|
| Number of hip fractures (n) | 214 | 28 | |
| Mean age (SD) | 83.4 (8.2) | 87.2 (7.5) | 0.021 |
| Gender | |||
| Female | 149 (69.6%) | 19 (67.9%) | 0.848 |
| Male | 65 (30.4%) | 9 (32.1%) | |
| ASA Grade | |||
| 1 | 1 (0.5%) | 0 (0.0%) | 0.629 |
| 2 | 42 (19.6%) | 6 (21.4%) | |
| 3 | 130 (60.7%) | 14 (50.0%) | |
| 4 | 41 (19.2%) | 8 (28.6%) | |
| Pre-operative AMTS | |||
| 0–6 | 70 (32.7%) | 12 (42.9%) | 0.286 |
| 7–10 | 144 (67.3%) | 16 (57.1%) | |
| Pre-admission residence | |||
| Nursing care | 22 (10.3%) | 4 (14.3%) | 0.126 |
| Own home/sheltered housing | 171 (79.9%) | 18 (64.3%) | |
| Residential care | 21 (9.8%) | 6 (21.4%) | |
| Fracture type | |||
| Intracapsular – displaced | 114 (53.3%) | 9 (32.1%) | 0.024 |
| Intracapsular – undisplaced | 20 (9.3%) | 1 (3.6%) | |
| Subtrochanteric | 8 (3.7%) | 1 (3.6%) | |
| Trochanteric – grade A1/A2 | 64 (29.9%) | 17 (60.7%) | |
| Trochanteric – grade A3 | 8 (3.7%) | 0 (0.0%) | |
| Mean time to surgery - hours (SD) | 31.6 (24.9) | 41.6 (41.1) | 0.074 |
| Delay in surgery >36h? | |||
| No | 147 (68.7%) | 14 (50.0%) | 0.049 |
| Yes | 66 (30.8%) | 13 (46.4%) | |
| N/A – surgery not performed | 1 (0.5%) | 1 (3.6%) | |
| Mean time to orthogeriatric assessment – hours (SD) | 30.0 (29.7) | 23.9 (13.6) | 0.297 |
| Treatment | |||
| Hemiarthroplasty (cemented) | 98 (45.8%) | 9 (32.1%) | 0.198 |
| Hemiarthroplasty (uncemented) | 8 (3.7%) | 0 (0.0%) | |
| Cannulated hip screws | 10 (4.7%) | 0 (0.0%) | |
| Dynamic hip screw | 54 (25.2%) | 13 (46.4%) | |
| Long intramedullary nail | 21 (9.8%) | 4 (14.3%) | |
| Short intramedullary nail | 12 (5.6%) | 1 (3.6%) | |
| Total hip replacement (cemented) | 2 (0.9%) | 0 (0.0%) | |
| Total hip replacement (hybrid) | 6 (2.8%) | 0 (0.0%) | |
| Total hip replacement (uncemented) | 2 (0.9%) | 0 (0.0%) | |
| Nonsurgical treatment | 1 (0.5%) | 1 (3.6%) | |
| Mean length of inpatient stay – days (SD) | 11.7 (8.2) | 15.8 (10.1) | 0.015 |
| Return to operating theatre (%) | 2 (0.6%) | 0 (0.0%) | – |
| 30-day mortality (%) | 22 (6.7%) | 15 (53.6%) | <0.001 |
| Discharge destination | |||
| Death during inpatient admission | 23 (7.0%) | 13 (46.4%) | <0.001 |
| Nursing care | 25 (7.6%) | 2 (7.1%) | |
| Own home/sheltered housing | 154 (47.1%) | 5 (17.9%) | |
| Rehabilitation unit | 96 (29.4%) | 7 (25.0%) | |
| Residential care | 22 (6.7%) | 1 (3.6%) | |
| Transfer to another acute hospital | 3 (0.9%) | 0 (0.0%) | |
| Other | 4 (1.2%) | 0 (0.0%) | |
| Discharge to pre-admission residence? | |||
| No | 136 (41.6%) | 20 (71.4%) | 0.002 |
| Yes | 191 (58.4%) | 8 (28.6%) | |
ASA = American Society of Anaesthesiologists; AMTS = abbreviated mental test score; SD = standard deviation
Figure 3 .
Box plot comparing the time to surgery for patients who were (a) not tested, (b) tested negative, (c) tested positive for COVID-19 on admission during period B.
Discussion
This study demonstrates that the implementation of a nationwide lockdown in the UK amid COVID-19 pandemic did not reduce the incidence of fragility hip fractures. Although the 30-day mortality rate was comparable between period B and period A, a positive COVID-19 test on admission was associated with a significantly higher 30-day mortality rate during period B.
The social distancing measures introduced by the UK government resulted in a significant reduction in the demand for emergency services across the NHS. Attendance to emergency departments in the UK fell by 57%.12 Scott et al reported a 58% reduction in all orthopaedic trauma referrals in Edinburgh.13 Similarly, Park et al showed that acute trauma referrals during the pandemic decreased by 53%.14
Reduced frequency of polytrauma and nonfragility fractures during the pandemic correlates with a lower number of motor vehicle accidents, sporting and alcohol-related injuries directly attributable to the lockdown restrictions. However, fragility fractures among the elderly predominantly occur due to low energy mechanisms in the domestic setting and, therefore, are least likely to be influenced by social interaction or travel.15 This has been proven in the present study, as the number of admissions due to hip fractures during the lockdown period was similar to the prepandemic era. Our findings are consistent with other studies conducted in the UK, Spain and Italy.13,16–18
The ‘best practice tariff’ (BPT) is a quality improvement framework that aims to financially incentivise and reimburse NHS hospitals for providing high-quality care measured against specific criteria. The BPT for fragility hip fractures is composed of seven timed interventions, including surgery within 36h and orthogeriatric assessment within 72h of admission.19 In response to the COVID-19 pandemic, BPT for all conditions including hip fractures was suspended until 31 July 2020.20
Given the undisputed evidence in favour of early surgery, prompt orthogeriatric care and early postoperative ambulation in hip fractures, the T&O departments at the participating hospitals, where feasible, aimed to continue providing timely multidisciplinary care to these patients.9,10,21 Therefore, despite the suspension of the BPT during period B, the mean time to surgery and orthogeriatric assessment was found to be similar between period B and period A. It is plausible that the disruption to the T&O services caused by redeployment of staff and limited operating theatre capacity was neutralised by a reduction in the number of admissions secondary to nonfragility fractures and cancellation of elective orthopaedic operations. Additionally, the length of inpatient stay in period B was significantly shorter than in period A. This was due to the improved availability of rehabilitation beds during the pandemic resulting from the suspension of elective orthopaedic services.22
During the lockdown period B, only 68% of patients underwent testing for COVID-19 on admission. This was due to the evolving public health guidelines on COVID-19 testing, and limited testing capacity at the beginning of the pandemic. During the initial phases of the pandemic, only patients that presented to hospitals with symptoms suggestive of a COVID-19 infection were tested, ie new cough, shortness of breath and associated fever.
The increasing testing capacity in NHS hospitals coincided with an improvement in the turnaround time for COVID-19 test results, decreasing from 48–96h to 3–4h during period B. The delay in receiving the COVID-19 test results for patients with suspected COVID-19 infection in the earlier period of lockdown, detailed anaesthetic assessments, and logistical challenges surrounding the COVID-19 protocols, could all potentially explain why a significantly lower proportion of COVID-19 positive patients underwent surgery within 36h of admission compared with the patients who tested negative (Table 2 and Figure 3). These variables may also account for the significantly longer inpatient stay among the COVID-19 positive patients.
In the present study, the 30-day mortality rate among hip fracture patients with a positive COVID-19 test on admission was 53.6%, which was significantly higher than those who tested negative (6.7%), p<0.001. Similar findings have been reported by the multicentre studies conducted in London (30.5% positive vs 10.3% negative), New York (35.3% vs 7.1% suspected vs 0.9% negative), Scotland (35.5% positive vs 8.3% negative) and Spain (30.4% positive vs 10.3% negative).23–26 Assessment of risk factors for increased mortality among COVID-19 positive patients was outside the remit of this study. Nevertheless, Kayani et al found that positive smoking history and more than three comorbidities were significantly associated with increased mortality in COVID-19 positive hip fracture patients.
Hall et al showed that a diagnosis of COVID-19 was an independent risk factor for increased 30-day mortality in patients with hip fractures.23 It is also worth noting that nonsurgical treatment for hip fractures during the COVID-19 pandemic is shown to be associated with poorer outcomes.18,26 Interestingly, Catellani et al reported that early surgical treatment in symptomatic COVID-19 positive patients with proximal femoral fractures resulted in improvement of their respiratory parameters.18 These studies demonstrate that even during public health emergencies, where possible, prompt surgery for fragility hip fractures should be prioritised.
The main limitations of this study are its retrospective design and reliance on the accuracy of the data submitted to the NHFD. Additionally, the sensitivity of the reverse transcriptase PCR test for COVID-19 ranges between 71% to 98% and varies depending on the timing of the test and the anatomical site.27 Since 32% of patients were not tested, it is possible that asymptomatic carriers were not detected, leading to an overestimation of the mortality rate in COVID-19 positive patients. Furthermore, as repeat testing during the inpatient stay was not universally implemented during study period B, we could not account for patients who might have been infected postoperatively. Finally, the long-term outcomes of our study population were not reported.
The strengths of this study include its multicentre design covering a sizeable region of the UK and the inclusion of a large sample size. The participating hospitals provide acute orthopaedic services to 3.4% of the UK population and treat 3.9% of all hip fractures in the UK, increasing the wider generalisability of our findings.5,11 The current study provides a valuable and timely insight into the epidemiology of fragility hip fractures during the COVID-19 pandemic. Following widespread implementation of routine testing and specific patient pathways to prevent cross-infection in UK hospitals, further studies assessing the accurate impact of the COVID-19 infections on postoperative outcomes in hip fractures are warranted.
Conclusion
In conclusion, the nationwide lockdown due to the COVID-19 pandemic did not result in a reduced incidence of hip fractures in the elderly. A positive COVID-19 test on admission was associated with a significantly higher mortality rate. Future contingency plans for a potential second wave of infections must take into account the commonly occurring public health issues, such as hip fractures among the elderly, which continue to pose a significant healthcare burden despite the pandemic. This study highlights the importance of timely delivery of multidisciplinary care to this cohort of patients. While the adaptive response may inevitably involve diverting healthcare resources towards maximising medical and intensive care capacity to accommodate for the critically unwell COVID-19 patients, the stakeholders must also ensure adequate provision of multidisciplinary care for this particularly vulnerable group of patients.
Acknowledgements
We thank our clinical data administrators Ben Goring (Conquest Hospital) and Stephen Rickman (Queen Elizabeth The Queen Mother Hospital) for helping with data extraction.
Ethical review statement
This study adhered to the ethical principles outlined by the UK Medical Research Council. Since this was a retrospective analysis of anonymised data from National Hip Fracture Database (NHFD), ethics review by the Research Ethics Committee (REC) was not required. This study was approved by the institutional review board at each participating hospital.
Conflict of interest
Professor Benedict Rogers is the Editor-in-Chief of the Annals of the Royal College of Surgeons. He was not involved in the review or editorial process for this paper, on which he is listed as an author. All other authors declare no conflict of interest.
References
- 1.COVID-19 Map. Johns Hopkins coronavirus resource center. https://coronavirus.jhu.edu/map.html (cited November 2020).
- 2.Cabinet Office. Staying at home and away from others (social distancing) - GOV.UK. https://www.gov.uk/government/publications/full-guidance-on-staying-at-home-and-away-from-others (cited June 2020).
- 3.Al-Jabir A, Kerwan A, Nicola Met al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 2 (surgical prioritisation). Int J Surg Lond Engl 2020; 79: 233–248. 10.1016/j.ijsu.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Nuffield Trust. Cancelled operations. https://www.nuffieldtrust.org.uk/resource/cancelled-operations (cited August 2020).
- 5.National Hip Fracture Database (NHFD) annual report 2019. https://www.rcplondon.ac.uk/projects/outputs/national-hip-fracture-database-nhfd-annual-report-2019 (cited June 2020).
- 6.Smith T, Pelpola K, Ball Met al. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing 2014; 43: 464–471. 10.1093/ageing/afu065 [DOI] [PubMed] [Google Scholar]
- 7.Sheikh HQ, Hossain FS, Aqil Aet al. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg 2017; 9: 10–18. 10.4055/cios.2017.9.1.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williamson EJ, Walker AJ, Bhaskaran Ket al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436. 10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klestil T, Röder C, Stotter Cet al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep 2018; 8: 13933. 10.1038/s41598-018-32098-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oldmeadow LB, Edwards ER, Kimmel LAet al. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 2006; 76: 607–611. 10.1111/j.1445-2197.2006.03786.x [DOI] [PubMed] [Google Scholar]
- 11.Office for National Statistics. Overview of the UK population. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/november2018 (cited November 2020).
- 12.NHS England. A&E Attendances and Emergency Admissions. https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/05/Statistical-commentary-April-2020-jf8hj.pdf (cited August 2020).
- 13.Scott CEH, Holland G, Powell-Bowns MFRet al. Population mobility and adult orthopaedic trauma services during the COVID-19 pandemic: fragility fracture provision remains a priority. Bone Jt Open 2020; 1: 182–189. 10.1302/2633-1462.16.BJO-2020-0043.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park C, Sugand K, Nathwani Det al. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the ‘golden month’. Acta Orthop 2020; 91: 556–561. 10.1080/17453674.2020.1783621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Norton R, Campbell AJ, Lee-Joe Tet al. Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc 1997; 45: 1108–1112. 10.1111/j.1532-5415.1997.tb05975.x [DOI] [PubMed] [Google Scholar]
- 16.Murphy RF, LaPorte DM, Wadey VMR, American Academy of Orthopaedic Surgeons Orthopaedic Education Study Group. Musculoskeletal education in medical school: deficits in knowledge and strategies for improvement. J Bone Joint Surg Am 2014; 96: 2009–2014. 10.2106/JBJS.N.00354 [DOI] [PubMed] [Google Scholar]
- 17.Nuñez JH, Sallent A, Lakhani Ket al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in spain. Injury 2020; 51: 1414–1418. 10.1016/j.injury.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Catellani F, Coscione A, D’Ambrosi Ret al. Treatment of Proximal Femoral Fragility Fractures in Patients with COVID-19 During the SARS-CoV-2 Outbreak in Northern Italy. J Bone Joint Surg Am 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7224593/ (cited 2020 June). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oakley B, Nightingale J, Moran CG, Moppett IK. Does achieving the best practice tariff improve outcomes in hip fracture patients? An observational cohort study. BMJ Open 2017; 7: e014190. 10.1136/bmjopen-2016-014190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norton T, Dunhill L. Payment by results suspended. Health Serv J. https://www.hsj.co.uk/finance-and-efficiency/payment-by-results-suspended/7027150.article (cited August 2020). [Google Scholar]
- 21.Neuburger J, Currie C, Wakeman Ret al. Increased orthogeriatrician involvement in hip fracture care and its impact on mortality in England. Age Ageing 2017; 46: 187–192. 10.1093/ageing/afw201 [DOI] [PubMed] [Google Scholar]
- 22.Independent. Nearly three-quarters of a million fewer hospital admissions during first two months of lockdown in England. https://www.independent.co.uk/news/health/coronavirus-hospital-admissions-reduced-lockdown-england-a9593021.html (cited August 2020). [Google Scholar]
- 23.Hall AJ, Clement ND, Farrow Let al. IMPACT-Scot report on COVID-19 and hip fractures. Bone Jt J 2020; 102-B: 1–10. 10.1302/0301-620X.102B9.BJJ-2020-1100.R1 [DOI] [PubMed] [Google Scholar]
- 24.Kayani B, Onochie E, Patil Vet al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt J 2020; 102-B: 1–10. 10.1302/0301-620X.102B9.BJJ-2020-1127.R1 [DOI] [PubMed] [Google Scholar]
- 25.Egol KA, Konda SR, Bird MLet al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a new york city perspective. J Orthop Trauma 2020; 34: 395–402. 10.1097/BOT.0000000000001845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muñoz Vives JM, Jornet-Gibert M, Cámara-Cabrera Jet al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. J Bone Joint Surg Am 2020; 102: e69. 10.2106/JBJS.20.00686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watson J, Whiting PF, Brush JE. Interpreting a covid-19 test result. BMJ 2020; 369: m1808. 10.1136/bmj.m1808 [DOI] [PubMed] [Google Scholar]