Abstract
Introduction
Laparoscopic adhesiolysis is increasingly being used to treat adhesional small bowel obstruction (ASBO) as it has been associated with reduced postoperative length of stay (LOS) and faster recovery. However, concerns regarding limited working space, iatrogenic bowel injury and failure to relieve the obstruction have limited its uptake. This study reports our centre’s experience of adopting laparoscopy as the standard operative approach.
Methods
A single-centre prospective cohort study was performed incorporating local data from the National Emergency Laparotomy Audit Database; January 2015 to December 2019. All patients undergoing surgery for ASBO were included. Patient demographic, operative and inhospital outcomes data were compared between different surgical approaches. Linear regression analysis was performed for LOS.
Results
A total of 299 cases were identified. Overall, 76.3% of cases were started laparoscopically and 52.2% were completed successfully. Patients treated laparoscopically had lower Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity (P-POSSUM) predicted mortality (median 2.1 (interquartile range (IQR) 1.3–5.0) vs 5.7 (IQR 2.0–12.4), p=<0.001) and shorter postoperative LOS compared with open (median 4.2 days (IQR 2.5–8.2) vs 11.3 days (IQR 7.3–16.6), p=0.000). Inhospital mortality was lower in the laparoscopic group (2 vs 7 deaths, p=<0.001). In regression analysis, laparoscopic surgery was found to have the strongest association with postoperative LOS (β −8.51 (−13.87 to −3.16) p=0.002) compared with open surgery.
Conclusions
Laparoscopy is a safe and feasible approach for adhesiolysis in the majority of patients with ASBO. It is associated with reduced LOS with no impact on complications or mortality.
Keywords: Laparoscopy, Adhesiolysis, Intestinal obstruction
Introduction
Adhesional small bowel obstruction (ASBO) is one of the most common general surgical emergencies and places a substantial burden on health services, accounting for approximately 4,000 emergency laparotomies annually in England and Wales alone.1,2 While adhesiolysis has been performed traditionally using an open approach, laparoscopic adhesiolysis has been gradually adopted for selected cases in some centres.3,4
Recent meta-analyses have suggested that a laparoscopic approach may be associated with a reduction in postoperative pain, length of hospital stay and faster recovery from surgery.5,6 The recent laparoscopic versus open adhesiolysis for adhesive small bowel obstruction (LASSO) randomised trial reported that laparoscopic adhesiolysis reduced length of stay (LOS) and postoperative pain, with quicker return to normal bowel function, without increasing complications.7 The latest iteration of the World Society of Emergency Surgery guidelines for ASBO recognises the laparoscopic approach to ASBO, while highlighting the need for careful patient selection and sufficient surgical experience. Specifically, these recommendations identify patients with two or fewer previous laparotomies, or in whom a single adhesional band is expected, as those most likely to benefit from laparoscopy.8
Portsmouth Hospitals NHS Trust is a high-volume tertiary referral centre for gastrointestinal (GI) surgery and has been an early adopter of laparoscopy in both elective and emergency surgery. The emergency surgery service is staffed by a specialist upper and lower GI consultant surgeon each day. This allows provision of subspecialist care for all abdominal surgical emergencies, by surgeons with expertise in laparoscopy.9
This paper describes our centre’s experience of adopting laparoscopy as the standard operative approach to ASBO. Its primary objective is to describe and compare the characteristics and outcomes of patients having either open or laparoscopic adhesiolysis during the study period. Its secondary objectives include analysis of temporal trends; comparison of intention to treat vs treatment received; impact of time to surgery (TTS) on outcomes; and linear regression analysis with a uni- and multivariable model.
Methods
This was a single-centre prospective cohort study performed using data from the National Emergency Laparotomy Audit (NELA) database, for Portsmouth Hospital NHS Trust. NELA is a prospectively maintained database of all patients in England and Wales requiring major emergency abdominal surgery. Inclusion criteria and data collection for NELA have been described previously.2 The study used data extracted from January 2015 to December 2019.
Only patients who underwent surgery for ASBO were included in the study. Patients with other recorded causes of small bowel obstruction, such as malignancy or hernia, were excluded. The following variables were extracted from the NELA database: patient age and gender, pre-operative American Society of Anaesthesiology (ASA) physical status classification and Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity (P-POSSUM) scores, operative approach, findings and procedure performed, TTS, LOS, return to theatre and inhospital mortality. The primary outcomes measured were postoperative LOS, death and return to theatre. For cases where there was a death or return to theatre, electronic medical records were also interrogated to provide further information (see Tables 3 and 4). The NELA dataset does not record individual complications beyond return to theatre or death, and thus more generalised complications have not been included in the study.
Table 3 .
Case summary for each return to theatre
| Age | Sex | First surgery | Second surgery | Total postoperative LOS |
|---|---|---|---|---|
| 87 | Female | Laparoscopic adhesiolysis | Laparotomy day 10 for ongoing ASBO | 62 days |
| 83 | Female | Laparoscopic adhesiolysis, repair port site hernia & small bowel resection | Anastomotic leak - laparotomy day 7 & small bowel resection & stoma | 87 days |
| 45 | Male | Laparoscopic adhesiolysis | Laparotomy day 10 for ongoing ASBO | 52 days |
| 63 | Female | Laparoscopic adhesiolysis; tear noted & repaired | Laparotomy day 2 for resection & anastomosis | 16 days |
| 52 | Female | Laparotomy, adhesiolysis & small bowel resection | Unwell day 1, re-laparotomy & further resection & anastomosis | 9 days |
| 70 | Male | Laparotomy, adhesiolysis & small bowel resection for small bowel adenocarcinoma | Leak from join; relaparotomy day 6 for further small bowel resection & anastomosis. | 35 days |
ASBO = adhesional small bowel obstruction; LOS = length of stay
Table 4 .
Case summary for each mortality
| Age | Sex | P-POSSUM | Approach | Pathology | Operation | Survival | Cause of death |
|---|---|---|---|---|---|---|---|
| 48 | Male | 2.3 | Laparoscopic | ASBO | Adhesiolysis | 3 days | Massive systemic inflammatory response with multiorgan failure |
| 95 | Male | 23.7 | Lap-to-open | Adhesions with small bowel volvulus | Untwisting of volvulus | 2 days | Frailty – multiorgan failure |
| 65 | Female | 9.6 | Open | ASBO and pancreatic cancer | Adhesiolysis & resection | 49 days | Disseminated pancreatic cancer |
| 87 | Female | 12.5 | Open | ASBO after right hemicolectomy | Adhesiolysis & resection | 6 days | Massive systemic inflammatory response with multiorgan failure |
| 80 | Male | 61.1 | Open | ASBO with small bowel twisted around ileostomy | Adhesiolysis & reduction of small bowel | 1 day | Massive systemic inflammatory response with multiorgan failure |
| 86 | Female | 7.1 | Open | ASBO | Adhesiolysis & resection | 6 days | Stroke |
| 60 | Female | 16.5 | Open | ASBO | Adhesiolysis | 5 days | Upper gastrointestinal bleed |
| 62 | Male | 5.9 | Open | ASBO and metastatic rectal cancer | Adhesiolysis & bypass | 9 days | Metastatic rectal cancer |
| 75 | Male | 23.7 | Open | ASBO with internal hernia after cystprostatectomy | Adhesiolysis & resection | 50 days | Internal hernia after cystprostatectomy |
ASBO = adhesional small bowel obstruction; P-POSSUM = Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity
Surgical approach is classified in the database as laparoscopic, open, laparoscopically (lap) assisted and laparoscopic converted to open. Surgical approach was analysed both by intention-to-treat and by treatment received. For the purposes of analysis on the basis of treatment received, both lap-assisted and converted cases were considered to have been completed open. To assess the effect of a delay in surgery on outcomes, data was divided into three groups based on TTS: TTS <24h, TTS <48h and TTS <72h. The effect timing of surgery had on laparoscopy rates was compared by dividing the dataset into timeslots: day (8am–5pm), evening (5pm–12 midnight) and night (12 midnight–8am). Temporal trends were assessed in annualised increments.
Risk adjustment to compare different treatment groups was performed using ASA grade and pre-operative P-POSSUM predicted mortality.10,11 ASA grade is a classification system used routinely to provide an overall assessment of physical health and fitness prior to surgery.10 P-POSSUM is an established and well-validated risk prediction tool for providing postoperative risk adjustment for abdominal surgery.11,12 Both tools have been demonstrated to be reasonably effective and well-validated tools in systematic review of validation studies.12
Data were compared using Pearson χ2 test, Fisher’s Exact and Mann–Whitney U tests. Univariable associations between variables and postoperative LOS were assessed using linear regression analysis; variables with a p-value <0.1 were included in a subsequent multivariable linear regression model. Mortality was not used as an outcome in regression analysis due to an insufficient number of events.13 Data analysis was performed in Microsoft Excel (Microsoft Corp, Redmond, WA) and statistical analysis in R software (R Foundation, Vienna, Austria).
Results
Data extracted from the local NELA database contained 1,240 operative episodes between January 2015 and December 2019. Of these, 494 patients were operated for small bowel obstruction, of which 299 cases with a recorded aetiology of adhesions were included in the final analysis.
Outcomes
Demographic, operative and outcomes data according to intention-to-treat are shown in Table 1. Patients in whom laparoscopic surgery was attempted (intention-to-treat comparison) were of similar age to open surgery but had a significantly lower mortality risk and ASA grade, and experienced a lower mortality rate and LOS.
Table 1 .
Demographic and operative characteristics for cases started laparoscopy or open (intended treatment)
| Started LAP n=228 |
Started Open n=71 |
p-value | |
|---|---|---|---|
| Males | 95 (41.7%) | 25 (35.2%) | 0.406 |
| Age (years) | 70 (53–78) | 69 (52.5–80.5) | 0.894 |
| TTS (days) | 1.7 (0.9–3.4) | 1.9 (1.1–4.4) | 0.220 |
| Surgery < 24h (%) | 70 (30.7%) | 17 (23.9%) | 0.275 |
| Surgery < 48h (%) | 126 (55.3%) | 37 (52.1%) | 0.643 |
| Surgery < 72h (%) | 159 (69.7%) | 46 (64.8%) | 0.434 |
| Pre-operative P-POSSUM (%) | 2.1 (1.3–5) | 5.7 (2–12.4) | <0.001 |
| Mean ASA grade (SD) | 2.2 (0.8) | 2.6 (0.8) | <0.001 |
| LOS (days) | 8.3 (5.2–15.7) | 14.4 (11.2–24.9) | <0.001 |
| Postoperative LOS (days) | 5.6 (3.2–12.5) | 11.3 (8.1–17.2) | <0.001 |
| Inhospital mortality | 2 (1%) | 7 (10%) | <0.001 |
| Bowel resection (%) | 29 (12.7%) | 21 (29.6%) | 0.002 |
Data are median (IQR) unless otherwise stated. p-values calculated with Pearson χ2 for gender, deaths and resection and Mann–Whitney U test for all other variables
ASA = American Society of Anaesthesiology; IQR = interquartile range; LAP = laparoscopically; LOS = length of stay; P-POSSUM = Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity; SD = standard deviation; TTS = time to surgery
Comparing patients for whom surgery was successfully completed laparoscopically versus open surgery (comparison of treatment received) revealed similar trends, with lower pre-operative mortality risk, and less mortality and lower LOS (see Table 2).
Table 2 .
Demographic and operative characteristics for treatment received, comparing laparoscopic group to open group (including both laparoscopically assisted and converted to open in the ‘open’ group); and just the converted group (containing both laparoscopically assisted and converted to open)
| LAP (n=156) | Open (n=143) | p-value | Converted (n=72) | p-value vs LAP | |
|---|---|---|---|---|---|
| Males | 69 (44.2%) | 51 (35.7%) | 0.164 | 26 (36.1%) | 0.312 |
| Age (years) | 68.5 (52.8–79) | 70 (53–79) | 0.581 | 70 (57–77) | 0.561 |
| TTS (days) | 1.8 (0.9–3.7) | 1.8 (0.9–3.4) | 0.735 | 1.7 (0.9–2.9) | 0.627 |
| Surgery < 24h, N (%) | 49 (31.4%) | 38 (26.6%) | 0.359 | 21 (29.2%) | 0.734 |
| Surgery < 48h, N (%) | 84 (53.8%) | 79 (55.2%) | 0.809 | 42 (58.3%) | 0.528 |
| Surgery < 72h, N (%) | 105 (67.3%) | 100 (69.9%) | 0.627 | 54 (75%) | 0.241 |
| Pre-operative P-POSSUM (%) | 2.1 (1.2–5) | 3 (1.8–10.5) | 0.001 | 2.5 (1.5–5) | 0.215 |
| Mean ASA grade (SD) | 2.2 (0.8) | 2.4 (0.8) | 0.008 | 2.2 (0.7) | 0.419 |
| LOS (days) | 6.5 (4.4–12.4) | 13.7 (9.2–20.7) | 0.000 | 12.9 (8.4–19) | <0.001 |
| Postoperative LOS (days) | 4.2 (2.5–8.2) | 11.3 (7.3–16.6) | 0.000 | 10.4 (6.6–16.1) | <0.001 |
| Inhospital mortality | 1 (1%) | 8 (6%) | 0.014 | 1 (1%) | 0.286 |
| Bowel resection (%) | 6 (3.8%) | 44 (30.8%) | 0.000 | 23 (31.9%) | <0.001 |
Data are median (IQR) unless otherwise stated. p-values calculated with Pearson χ2 for gender, deaths and resection and Mann–Witney U test for all other variables
ASA = American Society of Anaesthesiology; IQR = interquartile range; LAP = laparoscopically; LOS = length of stay; P-POSSUM = Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity; SD = standard deviation; TTS = time to surgery
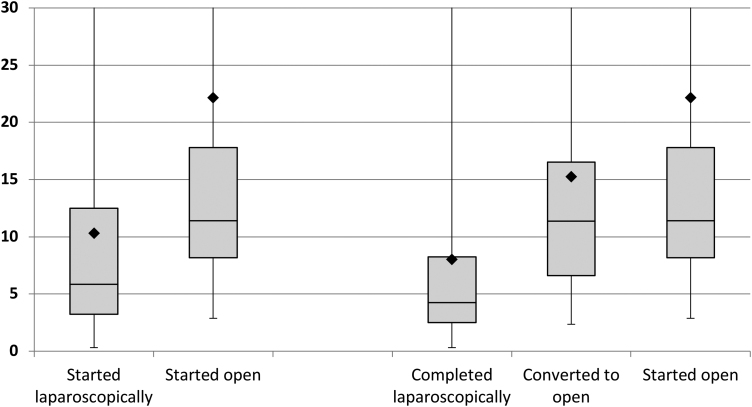
Patients for whom surgery was started laparoscopically but required conversion to laparoscopically assisted or laparotomy did not exhibit significantly different pre-operative mortality risk or ASA grade from the laparoscopically successful group (see Table 2) but experienced a longer LOS (see Figure 1). A further subgroup comparison between the converted group and patients who went straight to open surgery demonstrated lower pre-operative P-POSSUM scores (p=0.005) and ASA grade (p=0.014), but no differences in lengths of stay (p=0.333) or mortality (p=0.088).
Figure 1 .
Median postoperative LOS (days) by procedure displayed as boxplots with mean denoted by ♦. LOS = length of stay.
No differences were observed in TTS between operative approaches (see Table 1). Additional subanalysis on timing of surgery found that approximately two-thirds of cases for each operative approach were done during the day, with no significant increase in rates of open surgery at night (p=0.3628; Fisher’s Exact test). The majority of procedures were performed by a consultant surgeon. Of the 11 cases performed by a specialty trainee, 10 were completed laparoscopically and 1 open. There were no deaths or returns to theatre for this group.
Bowel resection or stoma formation was required in 17.7% of procedures and, in almost all cases, resulted in conversion to open or lap-assisted surgery. Complications, such as iatrogenic bowel injury, are not recorded in NELA. However, rates of unplanned return to theatre in patients having either laparoscopic or open surgery were low and not significantly different, 4/155 (2.6%) versus 2/142 (1.4%), respectively (p=0.189, see Table 3). Overall inhospital mortality was low (3%), with the majority of deaths occurring with open adhesiolysis (see Table 4).
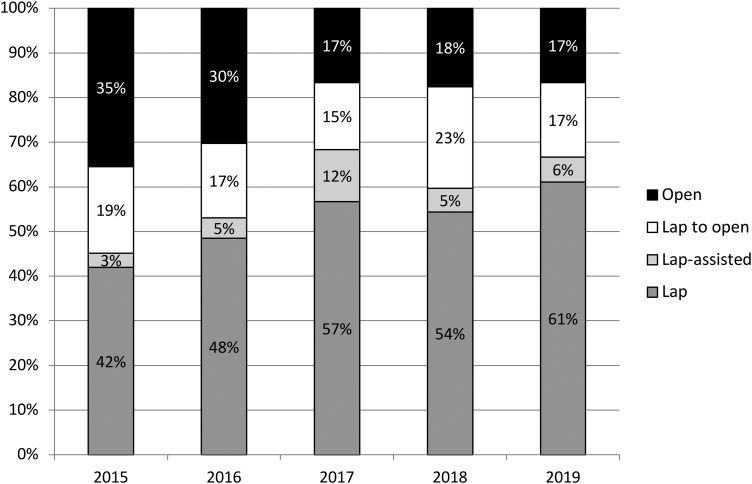
Temporal trends
The proportion of cases started laparoscopically increased incrementally between 2015 and 2019 (64.5% to 83.3%), with the number of cases completed successfully following the same trend (41.9% to 61.1%, Figure 2). The rate of conversion to open remained broadly similar at around 25%, and there was a concomitant reduction in the proportion of cases started with a laparotomy (35.5% to 16.7%). No significant difference was found (p=0.262, Fisher’s Exact test).
Figure 2 .
Number of cases (%) completed open, laparoscopy and lap-assisted/converted to open from 2015 to 2019. Lap = laparoscopically.
Regression analysis
Multivariable linear regression was applied to all demographic and operative factors (see Table 5). Laparoscopic surgery was found to have the strongest association with postoperative LOS (beta coefficient −8.51 (−13.87 to −3.16) p=0.002) compared with open surgery. No significant difference was seen between open and converted groups (beta coefficient −4.90 (−10.88–1.08) p=0.108). Bowel resection, ASA grade, and P-POSSUM scores were also found to have positive associations with LOS.
Table 5 .
Uni- and multivariable linear regression analysis for postoperative LOS
| Univariable beta-coefficient (95% CI) | p-value | Multivariable beta-coefficient (95% CI) | p-value | |
|---|---|---|---|---|
| Gender (female) | 2.26 (−2.31–6.84) | 0.331 | ||
| Age | 0.16 (0.03–0.29) | 0.018 | ||
| P-POSSUM | 0.53 (0.38–0.68) | <0.001 | 0.43 (0.27–0.59) | <0.001 |
| ASA grade | 5.99 (3.16–8.82) | <0.001 | 2.54 (0.27–0.56) | <0.001 |
| Bowel resection | 10.63 (4.63–16.62) | <0.001 | 6.50 (0.62–12.38) | 0.030 |
| TTS | 0.18 (−0.44–0.80) | 0.572 | ||
| <24hr to surgery | −0.39 (−5.29–4.51) | 0.875 | ||
| Surgical approach | ||||
| Open | 1 | 1 | ||
| Laparoscopic | −13.22 (−18.70 to −7.75) | <0.001 | −8.51 (−13.87 to −3.16) | 0.002 |
| Converted | −7.54 (−13.91 to −1.17) | 0.020 | −4.90 (−10.88–1.08) | 0.108 |
ASA = American Society of Anaesthesiology; CI = confidence interval; LOS = length of stay; P-POSSUM = Portsmouth – Physiological and Operative Severity Score for the enuMeration of Mortality and morbidity; TTS = time to surgery
Discussion
Our centre has successfully adopted the laparoscopic approach as the preferred treatment for ASBO, with 76.3% of cases routinely attempted via this approach, with an acceptable safety profile and shorter postoperative LOS compared with open surgery. We recommend a ‘laparoscopy-first’ approach wherever possible. Careful pre-operative discussion with a subspecialist radiologist is useful for operative planning and can help determine optimal port placement for laparoscopy, likelihood of success or need for major resection. Where diagnostic uncertainty remains, initial laparoscopy is unlikely to add significant comorbidity or operative time and should be considered. Adequate surgical experience, anaesthetic and theatre support are necessary. However, many of the skills obtained from minimal access approaches to elective GI cancer and benign surgery are readily transferrable to emergency adhesiolysis and could be safely adopted in many centres. Furthermore, supervised trainees have been allowed to perform parts of these procedures, with 6.4% of laparoscopic cases successfully completed by a specialty trainee as lead surgeon. We believe these are skillsets and mindsets that should be encouraged in the next generation of surgeons.
The significant differences seen, between patients for whom a laparoscopic approach was attempted and those for whom it was not, for pre-operative patient ASA and predicted P-POSSUM mortality risk reflects the fact that some patient selection is still required. Patients who require major or complex resectional surgery, or have severe intraperitoneal contamination, may still need to be considered for traditional laparotomy. Patient age, or duration of symptoms, as reflected in the data presented here, need not influence decision-making in this context. Even in cardiovascularly compromised patients, low pressure pneumoperitoneum can often be tolerated.14 Particularly if an upper abdominal incision is required, studies in the context of elective surgery have demonstrated that respiratory complications may be reduced with laparoscopy, as the postoperative reduction in pain, resulting atelectasis, and infective risk outweigh any transient intraoperative insult to ventilation.6,15 Similar findings have been reported in obese populations, suggesting body mass index (BMI) need not be a factor in considering surgical approach; intraoperative exposure and visualisation may in fact be superior via a laparoscopic approach compared with laparotomy.16
When controlling for P-POSSUM – which includes physiological, demographic, and diagnostic variables – as well as ASA, age and the need for bowel resection, laparoscopic completion of surgery remained the variable most strongly associated with a reduced LOS. Patients who could not be completed laparoscopically and were converted to open surgery experienced similar outcomes (LOS and mortality) to those who underwent primary laparotomy, despite differences in pre-operative risk and comorbidity.
It has been suggested that one of the effects of laparoscopy is to minimise systemic surgical insult; studies have suggested this may reduce the physiological and inflammatory response to injury.14 This has potential implications not only for patient outcomes, but hospital systems. Patients in whom the systemic effect of surgery can be minimised may be less likely to require prolonged admission in high-intensity care settings (high dependency units (HDUs) or intensive care units (ICUs)), reduction in ICU stays and overall admission LOS can have significant impact on hospital resource usage.
While operative times were not recorded as part of this study, it has been our experience that, in many cases, a laparoscopic approach can be as quick, if not quicker, than open surgery. Particularly in cases of simple band or limited adhesiolysis, avoiding full laparotomy and abdominal closure can reduce operative times substantially. In addition, patients undergoing laparoscopy may also require less anaesthetic intervention such as central venous access or placement of epidural catheters.
Where compromised bowel is identified, this can be addressed through a limited open incision, as demonstrated in our data. Unsurprisingly, the requirement for bowel resection leads to a significantly longer postoperative stay. However, our data demonstrates that it is still of benefit to start such cases laparoscopically. This may be because an initial laparoscopy allows freeing up of intra-abdominal adhesions, the selection of an appropriate region of the abdominal wall to make a small laparotomy, and the inspection of the closed laparotomy wound on completion of the anastomosis. It is clear that a smaller, appropriately sited laparotomy wound, using a wound retractor, and rectus sheath cannulas for postoperative analgesia, retains most of the benefits of the laparoscopic approach.
Concerns regarding limited working space, iatrogenic bowel injury, and failure to relieve the obstruction have limited the uptake of laparoscopic adhesiolysis in the past. In the 2018 national audit of ASBO in the UK, only 15% of cases were attempted laparoscopically, with only 7% of all cases completed successfully without conversion to laparotomy.17 This study demonstrates an increasing use of laparoscopy across the 5 year study period. However, the rate of conversion to open surgery has hardly altered and the requirement for bowel resection has not changed. This is the result of learning among the specialist upper and lower GI surgeons, with both laparoscopic enthusiasts and sceptics increasingly implementing laparoscopy in their emergency practice. Weekly governance meetings, incorporating the sharing of good practice in a no-blame culture, have helped to move the culture of the entire surgical team.
Evidence investigating the use of laparoscopy in ASBO remains limited. The most recent meta-analysis identified 18 studies containing 38,927 patients, with the mean number of cases completed laparoscopically (38.1%). Its findings very much support those demonstrated in this study, with laparoscopy conferring a lower mortality rate and shorter total LOS compared to laparotomy (1.6% vs 4.9% (p=0.001) and 6.7 vs 11.6 days (p=0.001), respectively) with a reduction in both complications and reoperation rate.6 The LASSO trial is the only randomised controlled trial comparing laparoscopy with laparotomy for a limited population of ASBO patients, where obstruction is deemed secondary to simple band adhesions only. Its major findings, with laparoscopy conferring a mean reduction in LOS of 1.3 days and no significant difference in complications or mortality (p=0.23), are in keeping with our findings reported here. In our broader cohort of ASBO patients, the rate of conversion to open surgery was also similar to that reported in the LASSO (23% vs 25%). However, LASSO’s strict inclusion/exclusion criteria meant only 1 in 5 patients screened were considered eligible, which contrasts with our centre’s more forthcoming approach.7 We believe the high rates of attempted laparoscopy, which increases throughout the study period (64.5% to 83.3%) demonstrates how our centre has adopted an ‘all comers’ approach to laparoscopy, with laparotomy reserved for cases where open surgery is clearly needed from the start.
A key strength of our study is that it uses longitudinal data collected prospectively from a national database. This has allowed us to observe reliably the impact of adopting laparoscopy in the treatment of ASBO in our centre. The limitations of the data included in this study, such as lack of information on prior surgery, comorbidity and severity of adhesions, means that we are unable to definitively identify those patients who should not be selected for laparoscopy, or that are most likely to require conversion (beyond those requiring bowel resection). The dataset also does not provide information on the size of the incisions used in lap-assisted and converted to open cases. Thus, we have grouped both types of conversion together, recognising that this may include patients who had small utility ports with those who had larger open incisions. While such a cohort study must be expected to reflect a degree of selection bias, we believe the high rates of attempted laparoscopy, demonstrates how laparoscopy has been adopted as the standard operative approach in our centre. Larger scale observational data in future should aim to identify appropriate algorithms to aid surgical decision-making in this context
Conclusion
This study demonstrates that laparoscopy should be the operative approach of choice for the surgical management of ASBO; it is safe, feasible, and widely applicable. It confers significantly reduced LOS and inhospital mortality compared with open surgery. These findings challenge the currently held view that laparoscopy should be reserved for selected, straightforward cases.
Funding and Sponsorship
This project did not receive any funding or sponsorship.
Conflicts of Interests
None declared.
References
- 1.Matsushima K, Sabour A, Park Cet al. Management of adhesive small bowel obstruction. J. Trauma Acute Care Surg 2019; 86: 383–391. 10.1097/TA.0000000000002150 [DOI] [PubMed] [Google Scholar]
- 2.The NELA Project Team. The Fifth Patient Report of the National Emergency Laparotomy Audit. The Royal College of Anaethetists; 2019: 1–61.
- 3.Catena F, Di Saverio S, Kelly MDet al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2010 evidence-based guidelines of the world society of emergency surgery. World J Emerg Surg 2011; 6: 5–24. 10.1186/1749-7922-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li MZ, Lian L, Xiao Let al. Laparoscopic versus open adhesiolysis in patients with adhesive small bowel obstruction: a systematic review and meta-analysis. AJS 2012; 204: 779–786. 10.1016/j.amjsurg.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 5.Sajid MS, Khawaja AH, Sains Pet al. A systematic review comparing laparoscopic vs open adhesiolysis in patients with adhesional small bowel obstruction. Am J Surg 2016; 212: 138–150. 10.1016/j.amjsurg.2016.01.030 [DOI] [PubMed] [Google Scholar]
- 6.Quah GS. Laparoscopic versus open surgery for adhesional small bowel obstruction: a systematic review and meta-analysis of case–control studies. Surg Endosc 2019; 33: 3209–3217. 10.1007/s00464-018-6604-3 [DOI] [PubMed] [Google Scholar]
- 7.Sallinen V, Di Saverio S, Haukijärvi Eet al. Laparoscopic versus open adhesiolysis for adhesive small bowel obstruction (LASSO): an international, multicentre, randomised, open-label trial. Lancet Gastroenterol Hepatol 2019; 4: 278–286. 10.1016/S2468-1253(19)30016-0 [DOI] [PubMed] [Google Scholar]
- 8.Broek ten RPG, Krielen P, Di Saverio Set al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg 2018; 13: 24. 10.1186/s13017-018-0185-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pucher PH, Carter NC, Knight BCet al. Impact of laparoscopic approach in emergency major abdominal surgery: single-centre analysis of 748 consecutive cases. Annals 2018; 100: 279–284. 10.1308/rcsann.2017.0229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Society of Anaesthesiologists. ASA Physical Status Classification System 2019. pp. 1–2. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (cited Jun 2020).
- 11.Prytherch DR, Whiteley MS, Higgins Bet al. POSSUM and Portsmouth POSSUM for predicting mortality. Br J Surg 1998; 85: 1217–1220. 10.1046/j.1365-2168.1998.00840.x [DOI] [PubMed] [Google Scholar]
- 12.Moonesinghe SR, Mythen MG, Das Pet al. Risk stratification tools for predicting morbidity and mortality in adult patients undergoing major surgery. Anesthesiology 2013; 119: 959–981. 10.1097/ALN.0b013e3182a4e94d [DOI] [PubMed] [Google Scholar]
- 13.van Smeden M. No rationale for 1 variable per 10 events criterion for binary logistic regression analysis. BMC Med Res Methodol 2016; 16: 1–12. 10.1186/s12874-016-0267-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grabowski JE, Talamini MA. Physiological effects of pneumoperitoneum. J Gastrointest Surg 2008; 13: 1009–1016. 10.1007/s11605-008-0662-0 [DOI] [PubMed] [Google Scholar]
- 15.Mariette C, Markar SR, Dabakuyo-Yonli TSet al. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med 2019; 380: 152–162. 10.1056/NEJMoa1805101 [DOI] [PubMed] [Google Scholar]
- 16.Reoch J, Mottillo S, Shimony Aet al. Safety of laparoscopic vs open bariatric surgery: a systematic review and meta-analysis. Arch Surg 2011; 146: 1314–1322. 10.1001/archsurg.2011.270 [DOI] [PubMed] [Google Scholar]
- 17.Lee MJ, Sayers AE, Wilson TRet al. Current management of small bowel obstruction in the UK: results from the National Audit of Small Bowel Obstruction clinical practice survey. Colorectal Dis 2018; 20: 623–630. 10.1111/codi.14016 [DOI] [PubMed] [Google Scholar]