Abstract
Introduction
The epidemiology of acute paediatric orthopaedic trauma managed surgically across the NHS is poorly described. Compliance against national standards for the management of supracondylar humeral fractures is also unknown at a national level.
Methods
Collaborators in 129 NHS hospitals prospectively collected data on surgically managed acute paediatric orthopaedic trauma cases. Data were collected over a seven-day period and included demographics, injury characteristics, operative details and timing of surgery. A national audit was also undertaken to evaluate compliance with the British Orthopaedic Association Standards for Trauma Guideline 11: Supracondylar Fractures of the Humerus in Children.
Results
Data were captured on 770 surgically treated cases. The three most common injuries were forearm fractures of both bones (n = 235), distal radius fractures (n = 194) and supracondylar elbow fractures (n = 89). The mode day of injury was Friday (n = 136) and the mode day of surgery was Saturday (n = 138). 88% of supracondylar fractures received surgery on the day of presentation or the following day. Only 14% of supracondylar fractures were treated surgically after 8pm; 33/89 used 2.0mm Kirschner wires, 38/89 used 1.6mm wires and 2/89 used 1.2mm wires.
Conclusion
Forearm fractures of both bones, distal radius fractures and supracondylar humeral fractures were the three most common injuries treated surgically. There is wide variation in compliance against national standards in the management of supracondylar humeral fractures with 88% undertaking surgery on the day of or the day following presentation but only 37% using the recommended 2.0mm Kirschner wires.
Keywords: Supracondylar, Elbow, Paediatric, Orthopaedic, Fractures
Introduction
Paediatric orthopaedic trauma in the UK is managed in a variety of clinical situations including emergency departments, fracture clinics and operating theatres. Acute management has been organised into paediatric major trauma centres, trauma and non-trauma units. National level activity data for all healthcare episodes are recorded by Hospital Episode Statistics.1 However, data on paediatric acute orthopaedic trauma inpatient care are not easily identified using this database. Data on severely injured children, treated mainly in major trauma centres and specialist children’s hospitals, are captured and analysed by the Trauma Audit and Research Network.2 However, this only applied to major trauma patients with a significant injury severity score. Most commonly encountered paediatric orthopaedic trauma is relatively low energy and managed by the trauma units around the UK. A small fraction of all acute paediatric orthopaedic trauma is managed surgically. To date, the surgical level of activity in any given week across the healthcare system is not clearly described. The nature and surgical management of injuries is not known. Understanding the types of cases managed surgically across the healthcare system is important for allocating provision of services both locally and regionally.
Recommendations for the management of displaced supracondylar humeral fractures in children are outlined by the British Orthopaedic Association Standards for Trauma (BOAST Guideline 11). Sixteen standards for optimal care are summarised in the guideline.
The primary aim of this study was to report the incidence of acute paediatric fractures treated surgically in the UK in a seven-day period in summer. The secondary aim was to evaluate the surgical management supracondylar elbow fractures against national guidelines. The research questions were:
-
1.
What is the epidemiology of acute paediatric fractures treated surgically (ie having a procedure in the operating theatre) across a healthcare system?
-
2.
How does the management of supracondylar humeral fractures compare to recommendations published in national guidelines?
Patients and methods
This study was conducted as a trainee-led multicentre audit using a trainee-developed collaborative platform (British Orthopaedic Network Environment, BONE, developed by the British Orthopaedic Trainees Association, BOTA). Collaborators were recruited via email, newsletters and at conference events such as the British Orthopaedic Association Annual Congress. All collaborators were sent a study pack via email, which included information on the study aims, standards and protocol. In the study pack, a data collection tool (Microsoft Excel) was included that permitted prospective data collection. The study cohort included all acute paediatric orthopaedic trauma cases requiring surgical intervention during the study period. The study period was seven days from 8am Wednesday 6 July to 7.59am Wednesday 13 July 2016. This was set to allow reporting of cases requiring a procedure in an operating theatre across the NHS in the UK over a seven-day period.
Collaborators were asked to prospectively collect data on surgically managed acute paediatric orthopaedic trauma at their hospital during these seven days. Once data collection was completed, the spreadsheet was emailed to the central data steering committee which analysed the data. Data were collected on demographics, injury type, surgical management and timing. Additional fields pertaining to supracondylar humeral fractures were included to allow audit against national standards (BOAST Guideline 11 Supracondylar Fractures of the Humerus in Children). Table 1 summarises the data collected by fields.
Table 1 .
Data fields collected in the study including examples for each field.
| Data recorded | Examples |
|---|---|
| Sex | Male, female |
| Injury side | Left, right, bilateral |
| Origin of referral | Emergency department, general practice, walk-in centre, other hospital |
| Age (years) | |
| Diagnosis | Distal radius fracture, both bone forearm fractures, supracondylar elbow fracture, lateral condyle elbow, medial epicondyle elbow, proximal humerus fracture, humeral shaft fracture, slipped upper femoral epiphysis, femoral neck fracture, femoral shaft fracture, distal femur fracture, tibial spine/tibial tubercle fracture, patellar fracture, both bone tibia/fibula shaft fracture, isolated tibial shaft fracture, distal fibula fracture, bimalleollar/trimalleolar ankle fracture, distal tibial physeal fracture (triplane, tillaux etc.) |
| Date of diagnosis (dd:mm:yyyy) | |
| Time of diagnosis (hh:mm) | |
| Operation type | Manipulation under anaesthesia + Kirschner wires, open reduction internal fixation, intramedullary nailing |
| Reduction | Closed, open |
| Grade of primary surgeon | Consultant, registrar, senior house office |
| Operation date (dd:mm:yyyy) | |
| Operation time (hh:mm) | |
| Additional data fields recorded for supracondylar humeral fractures | |
| Number of wires used | 2, 3, or 4 |
| Configuration of wires | Crossed, lateral only |
| Width of wires | 1.6mm, 2mm |
Audit standards
BOAST Guideline 11 contains 16 standards for clinical practice (Appendix 2, online only).3 Of these, three standards were identified that were amenable to a large-scale multicentre prospective clinical audit on surgically treated supracondylar fractures in children. These were standards 2, 4, and 6:
-
•
Standard 2: ‘These injuries require early surgical treatment, ideally on the day of admission. However, night-time operating is not necessary unless there are indications for urgent surgery.’
-
•
Standard 4: ‘Surgical stabilisation should be with bicortical wire fixation. Crossed wires are associated with a lower risk of loss of fracture reduction, whereas divergent lateral wires reduce the risk of injury to the ulnar nerve.’
-
•
Standard 6: ‘2mm diameter wires should be used, where possible, to achieve stability.’
Results
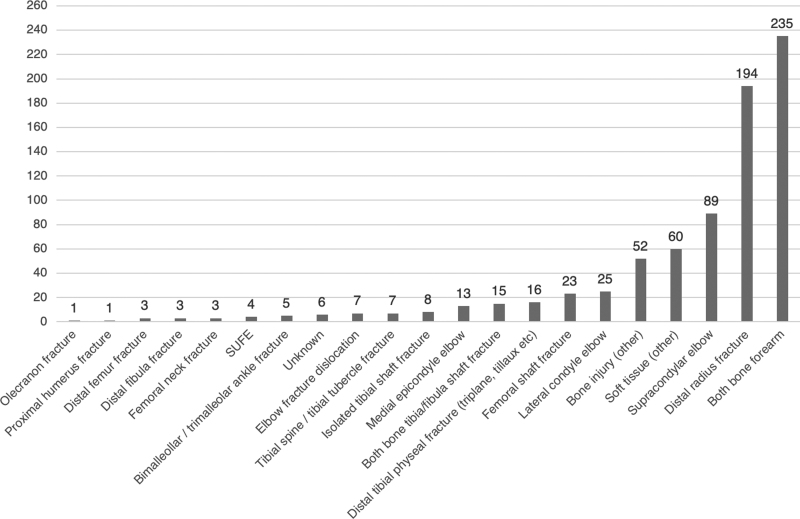
One hundred and twenty-nine hospitals participated in the study across the UK (including one hospital in the Republic of Ireland; Figure 1). A total of 770 acute paediatric fractures were managed surgically at these participating hospitals. Overall data completeness was 98.1% across all fields. Table 2 outlines the patient demographics and referral origin. Mean age was eight years (SD 3.75). The three most common injuries treated surgically were both bone forearm fractures (n = 235), distal radius fractures (n = 194) and supracondylar elbow fractures (n = 89). Figure 2 outlines the spread of injuries requiring surgical management by frequency. Both bone forearm fractures were treated with a closed reduction in 85% of cases. The majority were treated with manipulation under anaesthesia and application of plaster of Paris (63%), flexible intramedullary nailing in 19% and open reduction internal fixation in 8%. For distal radius fractures, 92% were reduced closed, 63% were managed with manipulation under anaesthesia and application of plaster of Paris, and 37% required Kirschner wire (K-wire) stabilisation after reduction. The mode day of injury was Friday (n = 136) and the mode day of surgery was Saturday (n = 138).
Figure 1 .
Geographic spread of the 129 participating hospital sites
Table 2 .
Demographic and referral origin data for common injuries
| Diagnosis | Mean age (years) | Male : female | Left : right | Origin of referral | ||||
|---|---|---|---|---|---|---|---|---|
| ED | GP | Walk-in centre | Other hospital | NR | ||||
| Distal radius fractures (n = 194) | 9.6 | 128 : 66 | 110 : 82 (1 bilateral) | 169 | 0 | 5 | 19 | 1 |
| Both bone forearm fractures (n = 235) | 7.8 | 151 : 84 | 135 : 98 | 217 | 0 | 4 | 12 | 2 |
| Supracondylar humeral fractures (n = 89) | 6.5 | 43 : 46 | 49 : 39 | 74 | 0 | 5 | 10 | 0 |
| All paediatric fractures (n = 770) | 8.6 | 484 : 285 | 417 : 343 (4 bilateral; 1 NR) | 669 | 3 | 15 | 78 | 0 |
ED, emergency department; GP, general practitioner; NR, not recorded
Figure 2 .
Chart representing frequency and range of paediatric orthopaedic injuries treated surgically
For supracondylar humeral fractures (n = 89), 70/89 (79%) were reduced closed. A total of 74/89 (83%) required manipulation under anaesthesia plus K-wires. When K-wires were required, 2 were used in 59 cases and 3 in 15 cases. Unlike distal radius and both bone forearm fractures, supracondylar fractures were most commonly treated surgically by consultants as primary surgeon (consultant as primary surgeon in 20% for distal radius fractures, 26% in both bone forearm fractures, and 48% in supracondylar fractures).
Compliance with national standards
Standard 2: 29% of supracondylar humeral fractures had surgery on the same day of injury, with 88% having surgery on the same day or the following day. 14% of supracondylar humeral fractures were treated surgically after 8pm. As data were not collected on the surgical decision-making process, it is not possible to report whether these cases required emergency out of hours surgical management. Those treated surgically on the same day of injury presented to the emergency department earlier in the day than those treated the following day (mean 13:39 vs 17:49).
Standard 4: 55/89 supracondylar fractures were stabilised with crossed wire configuration, 20/89 with lateral-only wires and 6/89 did not require K-wires. Data on K-wire configuration were not recorded for 9/89 cases.
Standard 6: 33/89 used 2.0mm K-wires, 38/89 used 1.6mm and 2/89 used 1.2mm. One confounder that may influence the decision to use 2.0mm compared with 1.6mm K-wires was the weight and hence, by proxy, the age of the child. In this study, the mean age of children with supracondylar humeral fractures requiring manipulation under anaesthesia plus K-wire fixation with 2.0mm wires was 6.5 years compared with 6.7 years in those stabilised with 1.6mm wires, suggesting that age may not be a factor influencing choice of wire diameter in these cases.
Discussion
This study is the largest trainee collaborative of its kind; 381 collaborators captured data on 770 acute paediatric orthopaedic trauma treated surgically in 129 participating hospitals in the UK and Ireland. According to the NHS website, there are 146 acute hospital trusts that treat paediatric orthopaedic injuries. This study therefore accounts for data from approximately 88% of the NHS. The majority of patients were admitted through the emergency department (669/770). Both bone forearm fractures, distal radius fractures and supracondylar elbow fractures represented the most common types of fracture treated surgically during the seven-day study period. The most common day of admission was Friday, and Saturday was the most popular day for surgery in this cohort.
In the UK, specialist trainees in trauma and orthopaedic surgery follow a surgical curriculum.4 Clinical competence in the management of the breadth of paediatric orthopaedic trauma is outlined in the curriculum. Recently, assessments for manipulation under anaesthesia plus K-wiring of supracondylar humerus fractures was added to the list procedures required to complete surgical training. Trainees are now required to perform five or more of these procedures prior to completion of surgical training, and to demonstrate evidence of competence after procedural-based assessment by two consultant raters. In this snapshot study, surgical trainees performed 28/89 (31%) operations for supracondylar fractures as primary surgeon across the UK. A mean of 0.7 supracondylar fractures per hospital were treated operatively during the study period. As such, these findings suggest that it may challenging for surgical trainees to fulfil the requirements. Several studies have reported on the learning curve for surgeons treating paediatric humeral supracondylar fractures surgically. Higher rates of inadequate reduction, malunion and increased need for open reduction were observed in surgeons with fewer than 15 cases of experiences with these injuries.5,6 Manipulation under anaesthesia plus plaster of Paris application for both bone forearm fracture and distal radius fractures was commonly performed in this study. The assessment of competence in this skill may be more suitable and should also be considered in the next iteration of the surgical curriculum.
14% of supracondylar humeral fractures were treated surgically after 8pm. It is not clear whether these patients required emergency surgical management as the reasons for surgery or the presence of neurovascular compromise were not collected. Nearly 9 of 10 supracondylar fractures were operated on the same day of presentation or the next day, demonstrating good compliance with BOAST 11 guideline.2 Supracondylar fractures presenting earlier in the day were more likely to undergo surgical management on the same day than those presenting later in the day. The BOAST 11 guideline suggests that crossed K-wire configuration is more biomechanically stable, while lateral-only wires are associated with less nerve injury. The guideline does not indicate which configuration is recommended.
Of the total, 55/89 supracondylar fractures were stabilised with cross wires, while 20/89 used a lateral-only wire configuration. Data were not collected on intraoperative decision making. The guideline reflects the best knowledge available, which comes from observational studies and biomechanical laboratory studies.7–18 There are no level 1 studies investigating the clinical effectiveness of crossed compared with lateral-only wires for displaced supracondylar fractures to inform this standard. The use of either technique may also be confounded by familiarity and training. Fracture patterns included in the audit were not characterised; in particular, degree of comminution, which may influence wire configuration used.
Surgeons used 2.0mm K-wires in 33/89 of supracondylar cases. Despite this standard explicitly recommending 2.0mm in the BOAST 11 guideline, this study demonstrated poor compliance. Reasons for this are not identifiable from the data collected. The mean ages of patients receiving 2.0mm wires compared with those with 1.6mm wires showed no difference.
This study has several limitations and the findings must be taken in the context of these limitations. Data were collected prospectively over a seven-day period in July. This is a short period that was chosen to reduce the data collection burden on collaborators. It only included one weekend and therefore weekly variation may exist, which potentially confounds the results. The study period was chosen to represent a typical summer week in the UK. The effect of school holidays on acute paediatric orthopaedic trauma is described.19,20 During the study period, schools in Scotland were on summer holiday while those in England and Wales were not. Weather is known to influence the incidence of paediatric orthopaedic trauma cases.20,21 Data were not collected on local weather during the study period. With 129 hospitals participating in the study from all areas of the UK (including one hospital from the Republic of Ireland), the variation in local weather may be somewhat mitigated.
The large number of participating trusts was a particular strength of this study, which permitted confidence that the findings were truly representative of acute paediatric orthopaedic trauma cases managed surgically across the NHS. Data were collected prospectively, usually by several collaborators per hospital. The accuracy of data collection was not investigated, but the study collaborators completed data on 770 cases with 98% completeness across all fields.
The study design was carefully considered to find a balance between meaningful data collection and reducing the administrative burden on collaborators. As such, it was decided to forego classification of fractures and limit the granularity of the data collected. Intraoperative decision making, neurovascular compromise and open compared with closed nature of fractures were some of the clinical features chosen not to collect data on. While collecting information in these areas would have allowed more colourful insights, the accuracy of the data collected would have been in question as these areas are often poorly documented in the case notes.22
Conclusions
Prospectively collected data from 770 acute paediatric orthopaedic cases treated in 129 hospitals over a seven-day period is presented. Variation in compliance against national standards in the management of supracondylar humeral fractures was noted. This study provides useful data that may help hospitals with allocating resources for acute paediatric orthopaedic trauma care. This information may be particularly useful to inform the feasibility of high-quality definitive randomised controlled trials in paediatric trauma surgery in the UK.
References
- 1.NHS Digital. Hospital Episode Statistics for Admitted Patient Care, Outpatient and Accident and Emergency Data. https://digital.nhs.uk/data-and-information/publications/ statistical/hospital-episode-statistics-for-admitted-patient-care-outpatient-and-accident-and-emergency-data (cited September 2020).
- 2.TARN. The Trauma Audit and Research Network (TARN). https://www.tarn.ac.uk (cited September 2020).
- 3.British Orthopaedic Association. Supracondylar Fractures of the Humerus in Children. British Orthopaedic Association Standards for Trauma. London: BOAST; 2014. [Google Scholar]
- 4.Intercollegiate Surgical Curriculum Programme (Version 10). https://www.iscp.ac.uk (cited September 2020).
- 5.Liu R, Roocroft J, Bastrom T, Yaszay B. Surgeon learning curve for pediatric supracondylar humerus fractures. J Pediatr Orthop 2011; 31: 818–824. 10.1097/BPO.0b013e3182306884 [DOI] [PubMed] [Google Scholar]
- 6.Pesenti S, Ecalle A, Peltier Eet al. Experience and volume are determinative factors for operative management of supracondylar humeral fractures in children. J Shoulder Elbow Surg 2018; 27: 404–410. 10.1016/j.jse.2017.10.014 [DOI] [PubMed] [Google Scholar]
- 7.Chen TL, He CQ, Zheng TQet al. Stiffness of various pin configurations for pediatric supracondylar humeral fracture: a systematic review on biomechanical studies. J Pediatr Orthop 2015; 24: 389–399. 10.1097/BPB.0000000000000196 [DOI] [PubMed] [Google Scholar]
- 8.Gottschalk H, Sagoo D, Glaser Det al. Biomechanical analysis of pin placement for pediatric supracondylar humerus fractures: does starting point, pin size, and number matter? J Pediatr Orthop 2012; 32: 445–451. 10.1097/BPO.0b013e318257d1cd [DOI] [PubMed] [Google Scholar]
- 9.Hamdi A, Poitras P, Louati Het al. Biomechanical analysis of lateral pin placements for pediatric supracondylar humerus fractures. J Pediatr Orthop 2010; 30: 135–139. 10.1097/BPO.0b013e3181cfcd14 [DOI] [PubMed] [Google Scholar]
- 10.Jaeblon T, Anthony S, Alan Ogden A, Andary J. Pediatric Supracondylar Fractures: Variation in Fracture Patterns and the Biomechanical Effects of Pin Configuration. J Pediatr Orthop 2016; 36: 787–92. 10.1097/BPO.0000000000000554 [DOI] [PubMed] [Google Scholar]
- 11.Srikumaran U, Tan E, Belkoff Set al. Enhanced biomechanical stiffness with large pins in the operative treatment of pediatric supracondylar humerus fractures. J Pediatr Orthop 2012; 32: 201–205. 10.1097/BPO.0b013e31824536c8 [DOI] [PubMed] [Google Scholar]
- 12.Weinberg AM, Castellani C, Arzdorf Met al. Osteosynthesis of supracondylar humerus fractures in children: a biomechanical comparison of four techniques. Clin Biomech 2007; 22: 502–509. 10.1016/j.clinbiomech.2006.12.004 [DOI] [PubMed] [Google Scholar]
- 13.Aydogmus S, Duymus TM, Kececi Tet al. Comparison of daytime and after-hours surgical treatment of supracondylar humeral fractures in children. J Pediatr Orthop B 2017; 26: 400–404. 10.1097/BPB.0000000000000403 [DOI] [PubMed] [Google Scholar]
- 14.Gupta N, Kay R, Leitch Ket al. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop 2004; 24: 245–248. 10.1097/01241398-200405000-00001 [DOI] [PubMed] [Google Scholar]
- 15.Kocher MS, Kasser JR, Waters PMet al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children: a randomized clinical trial. J Bone Joint Surg Am 2007; 89: 706–712. 10.2106/00004623-200704000-00002 [DOI] [PubMed] [Google Scholar]
- 16.Mayne AI, Perry DC, Bruce CE. Delayed surgery in displaced paediatric supracondylar fractures: a safe approach? Results from a large UK tertiary paediatric trauma centre. Eur J Orthop Surg Traumatol 2014; 24: 1107–1110. 10.1007/s00590-013-1292-0 [DOI] [PubMed] [Google Scholar]
- 17.Srikumaran U, Tan E, Erkula Get al. Pin size influences sagittal alignment in percutaneously pinned pediatric supracondylar humerus fractures. J Pediatr Orthop 2010; 30: 792–798. 10.1097/BPO.0b013e3181f6d3af [DOI] [PubMed] [Google Scholar]
- 18.Yousri T, Tarassoli P, Whitehouse Met al. Systematic review of randomized controlled trials comparing efficacy of crossed versus lateral K-wire fixation in extension type Gartland type III supracondylar fractures of the humerus in children. Ortop Traumatol Rehabil 2012; 14: 397–405. 10.5604/15093492.1005083 [DOI] [PubMed] [Google Scholar]
- 19.Barr LV. Paediatric supracondylar humeral fractures: epidemiology, mechanisms and incidence during school holidays. J Child Orthop 2014; 8: 167–170. 10.1007/s11832-014-0577-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segal D, Slevin O, Aliev Eet al. Trends in the seasonal variation of paediatric fractures. J Child Orthop 2018; 12: 614–621. 10.1302/1863-2548.12.180114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atherton WG, Harper WM, Abrams KR. A year’s trauma admissions and the effect of the weather. Injury 2005; 36: 40–46. 10.1016/j.injury.2003.10.027 [DOI] [PubMed] [Google Scholar]
- 22.Goodall R, Claireaux H, Hill Jet al. Comparison between a multicentre, collaborative, closed-loop audit assessing management of supracondylar fractures and the British Orthopaedic Association Standard for Trauma 11 (BOAST 11) guidelines. Bone Joint J 2018; 100-B: 346–351. 10.1302/0301-620X.100B3.BJJ-2017-0780.R2 [DOI] [PubMed] [Google Scholar]