Abstract
Introduction
Multiple traumatic rib fractures are associated with significant morbidity and mortality. The last decade has seen a significant increase in rates of surgical fixation for both flail and non-flail rib fractures; the evidence for this has come from largely retrospective studies. The aim of this meta-analysis was to compare the efficacy of this approach with that of non-operative management.
Methods
A systematic search of the literature was performed to identify randomised controlled trials (RCTs) comparing surgical stabilisation to non-operative management. Both flail and non-flail injuries were included.
Results
Five RCTs reported the results of 286 patients. Only one study assessed non-flail fractures. The studies were heterogenic in nature and of mixed quality. Surgical stabilisation was associated with a reduction in pneumonia (RR 0.46, 95% confidence intervals (CI) 0.29 to 0.73, I2=42%, p=0.001). The duration of mechanical ventilation (mean difference (MD) −6.3, 95% CI −12.16 to −0.43, I2=95%, p=0.05) and critical care length of stay was also shorter after surgery (mean difference −6.46 days, 95% CI 9.73 to −3.19, p<0.001); however, the overall length of stay in hospital was not (MD −7.18, 95% CI −15.63 to −1.28, I2=94%, p=0.1). No study demonstrated a significant reduction in mortality (RR 0.54, 95% CI 0.18 to 1.8, I2=0%, p=0.28).
Conclusions
Surgical stabilisation of rib fractures is associated with some improved clinical outcomes. Further large RCTs are still needed to confirm if there is also a survival benefit.
Keywords: Rib, Fractures, Surgical, Non-flailing, flail
Introduction
Approximately 10% of worldwide mortality is as a result of injury or trauma1 and blunt force trauma is the leading cause of death in people under the age of 40 years.2 Trauma to the chest causes or contributes to up to 25% of this annual trauma mortality.3 Rib fracture constitutes 55% of blunt chest trauma,4 and 10% of blunt force trauma patients admitted to a major trauma centre will have sustained one or more fractured ribs.5 Rib fractures are often painful and may cause instability to the chest wall. The mainstay of treatment has historically been supportive, with internal pneumatic splintage via mechanical ventilation on the intensive care unit (ITU) when needed to maintain respiratory function. The previous decade has seen a great increase in the rates of surgical fixation for both flail and non-flail rib fractures, with rates increasing from less than 1% to over 10%.6 The evidence to support this increase has come from largely retrospective studies, which may be at a higher risk of selection bias compared with a randomised study.
The aim of this systematic review was to compare outcomes after surgical rib fracture fixation for both flail and non-flail injuries using data from prospective randomised controlled trials (RCTs). The primary outcome measure was all cause mortality. Secondary outcomes extracted were length of stay (LOS) in ITU and hospital, the duration of mechanical ventilation, pneumonia, need for tracheostomy, patient-reported outcomes, including quality of life, pain and the results of spirometry (forced vital capacity (FVC), forced expiratory volume (FEV1), total lung capacity (TLC) and peak expiratory flow rate (PEFR).
Methods
The review was prospectively registered on Prospero (CRD42019157741). PubMed/MEDLINE, Embase and the Cochrane Library were searched from inception. The last search was performed on 9 July 2020. The search strategy was based on the search terms used in the previous Cochrane review and was tailored to each database. The search strategy is provided as Appendix 1.
Selection of articles and data extraction
After screening for duplication, two reviewers (SC and DO) performed initial screening and exclusion of studies based on the study title and abstract. Studies were included if they were RCTs comparing any form of surgical stabilisation with any form of non-operative management in patients with traumatic rib fractures. The full text of potential studies was then obtained and screened for eligibility by the two reviewers. Any studies in which the suitability was unclear were discussed with the senior author (BO). Duel independent data extraction was performed by two reviewers (SC and DO). When data on the primary or secondary outcomes were not available in the paper, further data were requested from the corresponding author of the study by using the email listed on the manuscript. Risk of bias was assessed by SC and BM.
Analysis
Data from the studies we included were entered into RevMan 5.3. Continuous variables were reported as a mean difference (MD) with 95% confidence intervals (CIs), using a fixed or random effects inverse-variance model depending on the assessment of heterogeneity of the included studies. Dichotomous variables were analysed using the Mantel–Haenszel model and are reported as a risk ratio (RR), with the fixed or random effects model being selected after review of study heterogeneity.
Heterogeneity between studies was assessed both by a visual inspection of the forest plots and statistically by using the I2 statistic. An I2 statistic of less than 25% was defined as demonstrating low heterogeneity, 25% to 50% showing moderate heterogeneity and over 50% as demonstrating high heterogeneity. Funnel plots were constructed to assess for potential publication bias in the current literature.
Results
Identified studies
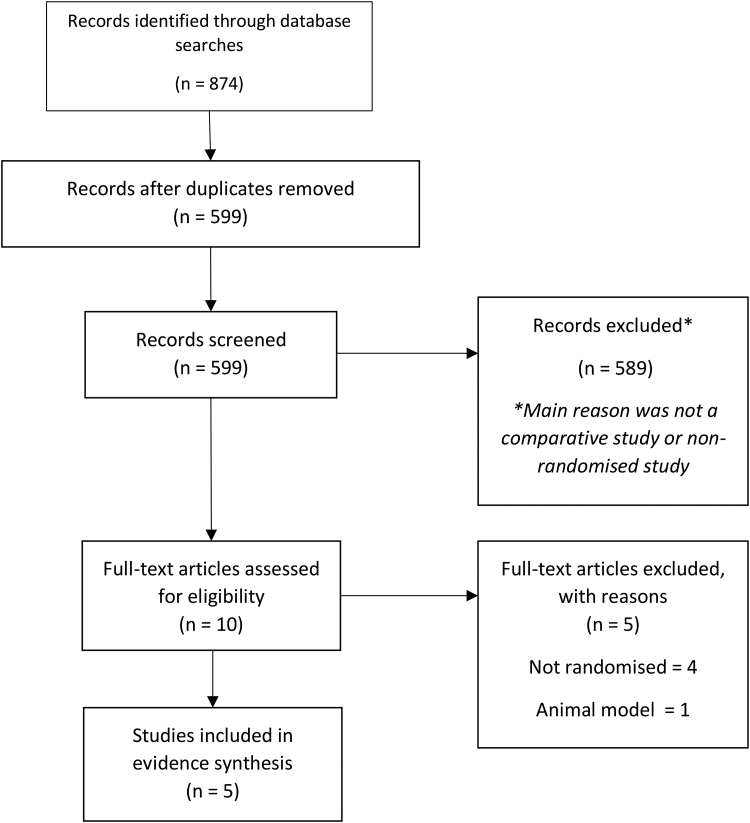
In total, 874 studies were returned by the search strategy, as shown in Figure 1. After removal of duplication, 599 studies were reviewed and assessed for eligibility. Of these, five RCTs were identified and included in the review.7–11 These studies reported outcomes for 286 patients, of which 139 underwent surgical rib fracture fixation and 147 were managed non-operatively. Four studies involved patients with a flail segment (number of patients 176); only one study assessed surgical fixation for patients with simple rib fractures and contained 110 patients. The authors of this study combined both randomised and non-randomised patients in their analysis; only 23 patients agreed to randomisation. Raw data were received from two authors (Granetzny and Marasco) where the original data was either missing or presented as a median. The included studies are summarised in Table 1.
Figure 1 .
PRISMA flow chart of screened studies
Table 1 .
Summary of included studies
| Author | Year | Fracture type | Implant | Primary outcome | Number of patients | Age (SD) | Number male (%) | Mean number of rib fractures (SD) | Mean ISS (SD) | Mean time to SRF (hours) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SM | NSM | Total | SM | NSM | SM | NSM | SM | NSM | SM | NSM | ||||||
| Granetzny et al (8) | 2005 | Flail | K or stainless steel wire | Pulmonary function | 20 | 20 | 40 | 40.5 (8.2) | 36 (14.9) | 17 (85) | 14 (70) | 4.4 | 4.6 | 16.8 (3.5) | 18 (3.5) | 24 to 36 |
| Liu et al (9) | 2019 | Flail | U plate or locking plate | Ventilator time | 27 | 26 | 53* | 42† (25–58) | 39† (24-56) | 21 (84) | 20 (80) | 6† (4–9) | 5† (3–7) | 29† (22–36) | 27† (20–36) | 37† (21–25) |
| Marasco et al (11) | 2013 | Flail | Bio absorbable plates | Ventilator time / time on ITU | 23 | 23 | 46 | 57.8 (17.1) | 59.3 (10.4) | 20 (87) | 20 (87) | 11 (3.1) | 11.3 (4.7) | 35 (11.4) | 30 (6.3) | Not stated |
| Pieracci et al (7) | 2020 | Simple | Not specified | Pain | 51 | 59 | 110‡ | 54.6 | 55.3 | 39 (76.5) | 43 (74.1) | 7† | 7† | 13 | 14 | Not stated |
| Tanaka et al (10) | 2002 | Flail | Judet struts | Ventilator time | 18 | 19 | 37 | 43 (12) | 46 (9) | 43 (12) | 46 (9) | 8.2 (3.3) | 8.2 (2.6) | 33 (11) | 30 (8) | 196.8 (98.4) |
ISS = injury severity score; ITU = intensive care unit; NSM: non-surgical management; SM = surgical management; SRF = surgical rib fixation.
*While 53 patients were randomised, only patients who attended follow up and received their allocation were analysed.
†Median value (with IQR where available).
‡110 patients recruited to the study, but only 23 underwent randomisation. The remainder were included in an observational arm; the two arms were combined for all of the study analysis.
Assessment of bias
The identified studies were heterogeneic in their inclusion criteria, surgical instrumentation, time to theatre, definition of flail chest, assessed outcomes and length of follow up. Random effects models were therefore used throughout the analysis. The overall risk of bias for the studies was moderate, as shown in Figure 2. The sole study assessing non-flail rib fractures was rated as being at a high risk of bias owing to the inclusion of patients who had declined randomisation. No publication bias was apparent after inspection of the plots.
Figure 2 .
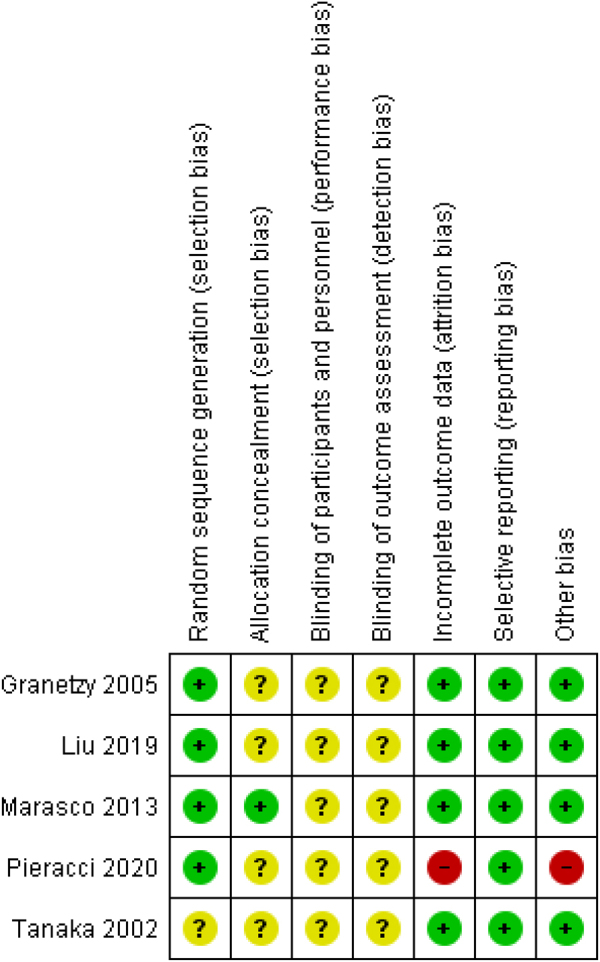
Risk of bias for included studies. ‘+’ represents a low risk of bias, ‘?’ an indeterminate risk and ‘−’ a high risk.
Outcomes
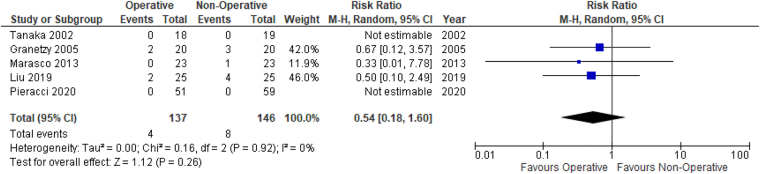
Mortality
All five studies reported mortality. Out of the 283 patients included in these five studies, 12 deaths were reported. The causes of death listed included pneumonia, pulmonary embolism, mediastinitis and sepsis. One of the deaths occurred on day 92 in Marasco et al; Granetzy et al did not give a time point of when the deaths occurred in their study. All deaths in Liu et al occurred during the initial admission episode. There were no significant differences in the rate of mortality between the groups (RR 0.54, 95% CI 0.18 to 1.6, p=0.26) (Figure 3).
Figure 3 .
Forrest plot of mortality for surgery vs non-operative management
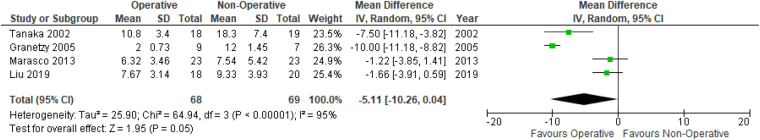
Mechanical ventilation
Four studies reported the duration of mechanical ventilation. Need for mechanical ventilation was an exclusion criteria for Pieracci. There was a statistically significant difference favouring the operative group (MD −6.3, 95% CI −12.16 to −0.43, I2=95%, p=0.05) (Figure 4).
Figure 4 .
Forrest plot of duration of mechanical ventilation for surgery vs non-operative management
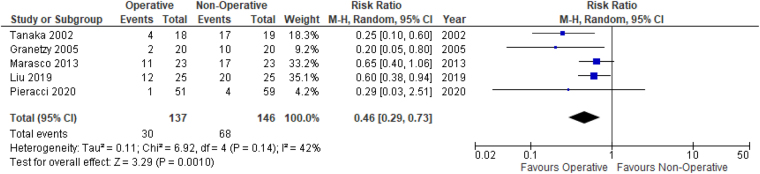
Pneumonia
All five studies reported rates of pneumonia. Only Pieracci and Liu provided a formal definition. Pieracci used the Centres for Disease Control and Prevention criteria, whereas Liu defined pneumonia as the presence of ‘new infiltrates on chest X-ray, positive sputum culture, and signs of systemic infection such as leucocytosis or fever’. There was a statistically significant difference favouring the operative group (RR 0.46, 95% CI 0.29 to 0.73, I2=42%, p=0.001) (Figure 5).
Figure 5 .
Forrest plot of cases of pneumonia for surgery vs non-operative management
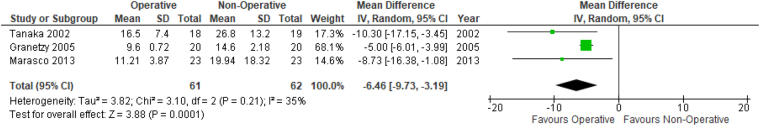
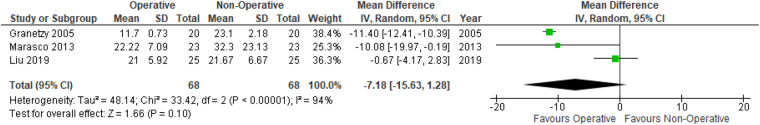
Length of stay
All five studies reported LOS in ITU. Pieracci reported no significant difference between the two groups (2 days in each group); however as no p value was provided, and the values given were reported as a median without a range, appropriate mean values could not be imputed. The four other studies demonstrated a statistically significant difference favouring the surgical group (MD −6.46, 95% CI −9.73 to −3.19, I2=35%, p<0.001).
Four studies reported overall hospital LOS, with outcomes data from 86 patients (43 operative, 43 non-operative). Again, while Pieracci reported no difference between groups (6 days in each group), insufficient data were provided in the manuscript to allow the study to be included in the meta-analysis. The remaining three studies did not demonstrate a statistically significant difference between the groups (MD –7.18, 95% CI –15.63 to −1.28, I2=94%, p=0.1) (Figures 6 and 7).
Figure 6 .
Forrest plot of length of stay in ITU for surgery vs non-operative management
Figure 7 .
Forrest plot of overall length of stay for surgery vs non-operative management
Respiratory function
FEV1 was reported by three studies containing outcomes for 145 patients. In Pieracci, only the mean values at the two-week follow-up were given so the SD was imputed. There was no significant difference between the two groups (MD −0.27, 95% CI −1.96 to 1.42, I2=0%, p=0.76). FCV was reported in three studies containing the outcomes for 111 patients (55 operative, 56 non-operative).8,10,11 No significant difference was found at 3 months post-injury (MD 8.08, 95% CI −4 to 20.16, I2=92%, p=0.19). Marasco and Granetzy both reported PEFR and TLC. There were no significant differences in any of these spirometry outcomes (PEFR MD 0.38, 95% CI −0.76 to 1.53, p=0.51, TLC MD of 3.69, 95% CI −3.08 to 10.46, p=0.29).
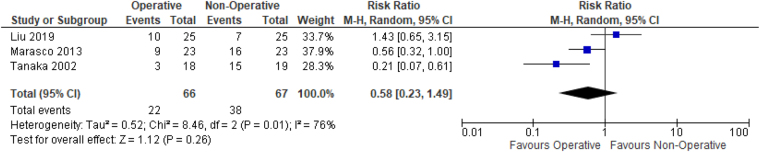
Need for tracheostomy
Three studies reported rates of tracheostomy. They reported a combined 60 events out of 133 patients. There was no significant difference between the groups (RR 0.58, 95% CI 0.23 to 1.49, I2=76%, p value=0.26) (Figure 8).
Figure 8 .
Forrest plot of need for tracheostomy for surgery vs non-operative management
Pain
Four studies reported pain using different instruments administered at different time points, precluding meta-analysis. Pieracci et al reported improved pain scores at 8 weeks post-injury using a Numeric Pain Scale (NPS) (1.5 vs 3.3 at 8 weeks, p=0.02). Liu reported (NPS) at 1 week post-treatment. No difference in pain at rest was found (5 vs 5, p=0.99); however, pain on deep inspiration (5 vs 7, p=0.038) and when coughing (6 vs 8, p=0.029) was lower following surgery. Marasco reported bodily pain assessed using the SF-36 at 6 months and found no difference in mean scores (42.2±9.4 for operative participants vs 37.9±11.0 for non-operative patients, p=0.22). Tanaka reported less subjective chest pain and tightness at 12 months post-injury following surgery (chest pain 39% vs 89%; chest tightness: 33% vs 84%).
Quality of life
Two studies reported quality of life using a variety of patient-reported outcome measures (PROMs). The different constructs of interest measured and instruments used precluded a meaningful meta-analysis. Pieracci assessed quality of life and respiratory disability using a composite of the American Chronic Pain Association Quality of Life Scale and a modified Chronic Pulmonary Disease Assessment Test. No difference was seen in quality of life at 8 weeks (mean 10 operative group vs 7 non-operative group, p=0.28). Lower respiratory disability was reported at 2 weeks in the operative group (21 vs 25, p=0.03); by week 8 this difference was no longer statistically significant (10 vs 16, p=0.27).
Marasco reported quality of life using the 36-item Short-form Health Survey (SF-36) at 6 months. No difference was found in either the physical (33.6±9.8 in the operative group vs 35.2±10.7 non-operative group, p=0.65) or mental components (45.1±13.8 in the operative group vs 45.2±9.2 non-operative group, p=0.98).
Discussion
This review did not find convincing evidence of a significant survival benefit following chest wall fixation. The strongest evidence of clinical benefit appears to be for patients who have a flail chest and require mechanical ventilation. These patients appear to benefit from surgical rib fixation, as they are faster to wean from their ventilators and develop lower rates of pneumonia.
There was mixed evidence to support an analgesic effect after rib fracture fixation, while neither longer-term respiratory function nor quality of life appeared to improve significantly following surgery. There was a lack of consistency in the PROMs used to assess these outcomes, making direct comparisons difficult. The lack of an agreed ‘gold standard’ in measuring healthcare-related quality of life after rib fracture appears to be a significant limitation of the current rib fracture literature.12
Patients with multiple non-flail rib fractures are underrepresented in the current literature. We did not find convincing prospective evidence to support the significant increase in routine fixation of non-flail rib fractures seen in some national trauma registries.13 The sole RCT suggests a significant but short-term analgesic effect. The conclusions that can be drawn from this study are unfortunately limited by the inclusion of patients who declined randomisation, adding potential bias to the study. While the authors report no differences in the measured patient baseline characteristics, it is possible that other non-measured differences between the two groups exist. Further prospective research is needed in this group before the routine fixation of non-flail ribs can be recommended. The challenges of conducting a study in this group are apparent in the paper, as 80% of eligible patients declined randomisation.7
Our study was largely in line with the other reviews of RCTs only. Since the 2015 Cochrane review on surgical fixation of flail chest, only two further RCTs have been published.7,9,14 As only one of these trials focused on flail chest injuries, we were unable to show significant new findings and therefore our study is largely a replication of the previous Cochrane review.14 So far, no review has demonstrated a survival benefit following rib fixation, despite the observed reduction in rates of pneumonia.14–16
Despite the relatively few RCTs there are discrepancies in the published reviews. Coughlin et al found a significant reduction in duration of mechanical ventilation, critical care and overall hospital stay after rib fixation; the Cochrane review did not pool these data.14,15 While our review did demonstrate a reduced ITU LOS and a reduced time on mechanical ventilation with surgery, the inclusion of Liu et al in our review caused the difference in overall LOS to become insignificant. Both the Cochrane review and Coughlin et al reported a significant reduction in rates of tracheostomy after surgery. Again, the inclusion of Liu et al in our review made the difference non-significant. It is possible that the contribution to LOS and need for tracheostomy from the concomitant polytrauma and lung contusions sustained by the patients in this paper was greater than any benefit possible from rib fracture fixation.17 Apamba et al did include Liu et al in their systematic review but not Granetzny.16 Data from a trial which terminated early owing to poor recruitment were also included;18 this study does not appear to have undergone peer review and the full results and study methodology are currently not published.
The effect sizes seen in our study and other previous reviews are smaller than those seen in retrospective and non-randomised studies.19 Data determining the cost effectiveness of rib fracture fixation have utilised these retrospective studies, which may overstate any potential functional benefits.20
There are limitations to this review. Although all study authors were approached regarding missing data, only two returned raw data. The studies appeared heterogeneic in inclusion criteria and design, limiting the conclusions that can be drawn from a meta-analysis of the pooled results. A period of 18 years separates the first RCT identified from this study from the most recent. During these years there have been changes in practice and the advancement of rib fracture care, including an increase in regional analgesic regimens, more modern surgical technique and fixation method, and reduced time from injury to surgery. Different implants were used in all four studies; no study solely examined non-absorbable locking plates, which represents the current standard of practice in the UK. No RCT has been performed in a UK population, with the current studies coming from China, Egypt, Australia, Japan and the USA.
The main limitation to this review is the continuing lack of prospective evidence in the form of well-designed RCTs to support surgical fixation of fractured ribs. There are several potential barriers to conducting an adequately powered RCT in rib fracture that have been proposed.21 These barriers may have limited the number of trials completed so far. The previous Cochrane review identified three ongoing RCTs assessing the surgical management of flail chest; as of now none of these studies have reported their full results.18,22,23 One newly registered trial was found during this review with a recruitment target of 300 patients. The primary outcome is LOS on ITU after a flail chest injury. Recruitment began in January 2020; reporting of the results is not anticipated until December 2022.24 It is hoped that these trials may eventually provide further evidence to the role of rib fracture fixation.
Conclusions
Surgical rib fracture fixation is associated with some improved clinical outcomes for patients requiring mechanical ventilation. However, there is no strong evidence of improved survival to support the increased rates of surgical fixation seen over the previous decade. Further well-designed RCTs are urgently needed to confirm a survival benefit from surgery.
Author contributions
Simon Craxford (Registrar): performed the searches, performed the data extraction, undertook the analysis, prepared the first draft of manuscript, designed the study.
Dean Owyang (Foundation Doctor): performed the data extraction, prepared the manuscript.
Ben Marson (NIHR Doctoral Fellow): performed the data extraction, undertook the analysis, prepared the manuscript.
Katie Rollins (Research Fellow): designed the study and search strategy, prepared the manuscript.
Tim Coughlin (Consultant in Trauma and Orthopaedics): designed the study, prepared the manuscript.
Daren Forward (Consultant in Trauma and Orthopaedics): designed the study, prepared the manuscript.
B. J. Ollivere (Professor): designed the study, resolved issues with data extraction, prepared the manuscript.
Conflict of interest
Ben Marson is funded by a National Institute for Health Research (NIHR) Doctoral Fellowship NIHR300240 for research outside this project.
References
- 1.Haagsma JA, Graetz N, Bolliger Iet al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev 2016; 22: 3–18. 10.1136/injuryprev-2015-041616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health 2000; 90: 523–526. 10.2105/AJPH.90.4.523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lafferty PM, Anavian J, Will RE, Cole PA. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am 2011; 93: 97–110. 10.2106/JBJS.I.00696 [DOI] [PubMed] [Google Scholar]
- 4.Haines KL, Zens T, Warner-Hillard Cet al. Rib fracture location should be evaluated when predicting morbidity and mortality in trauma patients. Am Surg 2018; 84: 1462–1465. 10.1177/000313481808400950 [DOI] [PubMed] [Google Scholar]
- 5.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994; 37: 975–979. 10.1097/00005373-199412000-00018 [DOI] [PubMed] [Google Scholar]
- 6.Dehghan N, de Mestral C, McKee MDet al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014; 76: 462–468. 10.1097/TA.0000000000000086 [DOI] [PubMed] [Google Scholar]
- 7.Pieracci FM, Leasia K, Bauman Zet al. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J Trauma Acute Care Surg 2020; 88: 249–257. 10.1097/TA.0000000000002559 [DOI] [PubMed] [Google Scholar]
- 8.Granetzny A, Abd El-Aal M, Emam Eet al. Surgical versus conservative treatment of flail chest. evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005; 4: 583–587. 10.1510/icvts.2005.111807 [DOI] [PubMed] [Google Scholar]
- 9.Liu T, Liu P, Chen Jet al. A randomized controlled trial of surgical rib fixation in polytrauma patients with flail chest. J Surg Res 2019; 242: 223–230. 10.1016/j.jss.2019.04.005 [DOI] [PubMed] [Google Scholar]
- 10.Tanaka H, Yukioka T, Yamaguti Yet al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002; 52: 727–732; discussion 32. 10.1097/00005373-200204000-00020 [DOI] [PubMed] [Google Scholar]
- 11.Marasco SF, Davies AR, Cooper Jet al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013; 216: 924–932. 10.1016/j.jamcollsurg.2012.12.024 [DOI] [PubMed] [Google Scholar]
- 12.Craxford S, Deacon C, Myint Y. et al. Assessing outcome measures used after rib fracture: A COSMIN systematic review. Injury 2019; 50: 1816–1825. 10.1016/j.injury.2019.07.002 [DOI] [PubMed] [Google Scholar]
- 13.Kane ED, Jeremitsky E, Pieracci FMet al. Quantifying and exploring the recent national increase in surgical stabilization of rib fractures. J Trauma Acute Care Surg 2017; 83: 1047–1052. 10.1097/TA.0000000000001648 [DOI] [PubMed] [Google Scholar]
- 14.Cataneo AJ, Cataneo DC, de Oliveira FHet al. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev 2015; 7: Cd009919. 10.1002/14651858.CD009919.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coughlin TA, Ng JW, Rollins KEet al. Management of rib fractures in traumatic flail chest: a meta-analysis of randomised controlled trials. Bone Joint J 2016; 98-b: 1119–1125. 10.1302/0301-620X.98B8.37282 [DOI] [PubMed] [Google Scholar]
- 16.Apampa AA, Ali A, Kadir B. et al. Safety and effectiveness of surgical fixation versus non-surgical methods for the treatment of flail chest in adult populations: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 2021; Feb 6: 1–10. 10.1007/s00068-021-01606-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Althausen PL, Shannon S, Watts Cet al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma 2011; 25: 641–647. 10.1097/BOT.0b013e318234d479 [DOI] [PubMed] [Google Scholar]
- 18.NCT01147471. Flail chest: early operative fixation versus non-operative management - a prospective randomized study. http://clinicaltrialsgov/ct2/show/NCT01147471 (cited August 2020).
- 19.Ingoe HMA, Coleman E, Eardley Wet al. Systematic review of systematic reviews for effectiveness of internal fixation for flail chest and rib fractures in adults. BMJ Open 2019; 9: e023444. 10.1136/bmjopen-2018-023444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swart E, Laratta J, Slobogean G, Mehta S. Operative treatment of rib fractures in flail chest injuries: A meta-analysis and cost-effectiveness analysis. J Orthop Trauma 2017; 31: 64–70. 10.1097/BOT.0000000000000750 [DOI] [PubMed] [Google Scholar]
- 21.Pieracci FM, Leasia K, Whitbeck S. Barriers to conducting a multi-center randomized controlled trial of surgical stabilization of rib fractures (and how to overcome them). J Thorac Dis 2019; 11: S1049–s60. 10.21037/jtd.2018.12.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NCT01308697. Operative versus non operative management of flail chest: a randomized controlled feasibility study. http://clinicaltrialsgov/ct2/show/NCT01308697 (cited August 2020).
- 23.NCT01367951. A multi centered randomized controlled trial of operative versus non-operative treatment of acute, unstable chest wall injuries. http://clinicaltrialsgov/ct2/show/NCT01367951 (cited August 2020).
- 24.NCT02595593. Rib Fixation for Clinically Severe Rib Fractures From Trauma. http://clinicaltrialsgov/ct2/show/NCT02595593 (cited August 2020).