Abstract
Introduction
Suspending elective surgery during the first wave of coronavirus (COVID-19) led to record-breaking numbers of patients on waiting lists. Patients in Black, Asian and minority ethnic (BAME) groups are disproportionately affected by COVID-19. This study compares the perspectives of patients from different ethnic backgrounds on the return to elective surgery.
Methods
Some 151 patients were sampled from cancelled operating lists at two hospitals. Semi-structured interviews focused on the impact of COVID-19, and views about resuming elective surgery. The Generalized Anxiety Disorder 7-iten Scale (GAD-7) measured anxiety. A visual analogue scale (VAS) measured pain. Data were analysed using exploratory thematic analysis.
Results
Fewer BAME patients were pleased about restarting surgery, compared with white patients (47.3% vs 82.6%, p<0.001), and a greater proportion wanted to postpone their operation until after the pandemic (21.8% vs 9.3%, p=0.048). White/white British patients had higher GAD-7 scores (2 (0–21) vs 0 (0–16), p=0.009). Black/Black British patients had significantly higher VAS scores compared with white/white British and Asian/Asian British patients (85 vs 75 vs 70 respectively, p<0.05).
Conclusion
The delay in surgery due to the pandemic has had a devastating impact on patients awaiting operations. The variation in pain and anxiety levels between ethnic groups must be addressed when redesigning services to avoid discrepancies in postoperative clinical outcomes. Patients in BAME groups are more likely to postpone their operation, which may lead to further health deterioration, psychosocial and socio-economic consequences, and poorer clinical outcomes following surgery. The thoughts, feelings and concerns of all must be considered when redesigning services to prevent health inequalities between patients from different backgrounds.
Keywords: COVID-19, Elective surgery, Waiting lists, Orthopaedic surgery
Introduction
Coronavirus (COVID-19) led to the unprecedented cancellation of elective surgery to reduce the patient exposure to the virus and release essential resources to help combat the pandemic. This led to a 100-fold increase in patients waiting over a year for NHS treatments, and the number on waiting lists is at an all-time high.1 It has been estimated that approximately 400,000 procedures are accumulating per month and that there will be an additional surge of referrals post-pandemic due to the reduced attendance at GP practices during the pandemic.2
Within the orthopaedic discipline in the UK, it has been modelled that surgeons would need to operate at 170% of pre-COVID levels for a year to clear the additional backlog.3 As the pandemic progresses, the prospect of operating at this level in the foreseeable future is unfeasible. It has been predicted that the extent of the backlog, along with the reduced capacity to carry out elective surgery, will lead to a public health crisis.2
The Royal College of Surgeons of England have advised that resuming elective services should take place following a sustained reduction in the rate of new COVID-19 cases to ensure adequate facilities and staff are available, and that this will not adversely impact the provision of emergency surgery.4 In October 2020, as part of redesigning services for a return to operating, NHS England introduced changes to waiting lists including the requirement for NHS trusts to establish the patient’s treatment wishes and introducing the option for patients to postpone surgery but remain on the waiting list, which was not previously possible. It has been found that although the majority of patients support the return of elective operating and are willing to go ahead with surgery, those unwilling to proceed were concerned about the risk of contracting COVID-19.5
Public Health England’s review on disparities in the risk and outcomes in COVID-19 found that patients from Black, Asian and minority ethnic (BAME) backgrounds are disproportionately affected by COVID-19 and are at greater risk of death.6 The disparity in the way that COVID-19 affects those in BAME groups raises questions about the ideas, concerns and expectations patients from different backgrounds might have about returning to elective surgery during the pandemic. Additionally, BAME individuals are underrepresented in clinical research, and information about patient ethnicities has not been collected in many COVID-19 themed studies.7
Understanding patient concerns and expectations is important because they are associated with clinical outcomes following surgery.8 This study aims to compare and contrast the thoughts, feelings and concerns of patients from different ethnic backgrounds on the re-introduction of elective surgery following the cancellation of operating during the pandemic.
Methods
Telephone interviews were conducted with patients on cancelled orthopaedic operating lists at two centres in West Yorkshire and the West Midlands. Purposive sampling of patients from different ethnic backgrounds was used to capture the perspectives of diverse patient populations. Ethnicity was considered with respect to the five aggregated ethnic groups: Asian/Asian British, Black/Black British, mixed/multiple ethnic groups, other ethnic groups and white/white British. The first four are occasionally referred to as a Black, Asian and minority ethnic (BAME) group.
Two researchers (HH and RG) conducted semi-structured interviews composed of 15 predetermined open-and-closed questions exploring patients’ perspectives on a return to elective surgery following cancellation of their procedure during the first wave of the pandemic. Questions enquired about the health impact the delay was having, and explored the thoughts, feelings and concerns patients had about restarting operating and the new protocols in place aimed at reducing transmission.
A visual analogue scale (VAS) was used to measure pain.9 The Generalized Anxiety Disorder 7-item Scale (GAD-7), a validated and universally used measure for anxiety, was used with the cut-off of 10 as a marker of generalised anxiety disorder.10 VAS and GAD-7 were assessed over the telephone. Interviews lasted up to 20 minutes and were not repeated. There was no previously established relationship between interviewers and participants.
Exploratory thematic analysis was used to analyse patterns within the data.11 Verbal data were transcribed, and two researchers (HH and AH) independently familiarised themselves with the data through active reading. Data-driven codes were generated and collated manually, and sorted into over-arching themes. Themes were named and analysed to identify the meanings and implications of each. Interviews ended when replication of data occurred, indicating that data saturation was reached. Similarities and differences in themes and sub-themes were compared between those from different backgrounds.
SPSS (v. 26) was used for statistical analysis. Mann–Whitney U test was used to assess significance between BAME and white groups for non-parametric data, and chi-squared test to assess differences between ordinal and nominal data. Analysis of variance (ANOVA) was used to assess differences in VAS score between ethnicities. Significance was set at p<0.05. The reasons for the research were explained and patients gave informed consent at the time of interview. Ethical approval was acquired from University of Leeds (MREC19-080).
Results
Some 151 of 233 eligible patients agreed to participate (101 from West Yorkshire, 50 from the West Midlands), of whom 59.6% (90) were female (Table 1). Median (interquartile range (IQR)) age was 64 (25) years. Patients were awaiting the following procedures: arthroplasty, 63.6% (96); arthroscopy, 13.9% (21); long bone non-union surgery, 16.6% (25); and other type of elective surgery, 6.0% (9). The number of participants in each ethnic group was as follows: Asian/Asian British, 31.1% (47); Black/Black British, 4.0% (6); mixed/multiple ethnic groups, 0% (0); other ethnic groups, 1.3% (2); white/white British, 57.0% (86); and not specified, 6.6% (10). For analysis, we considered ethnicity by the groups BAME 36.4% (55) and white 57.0% (86).
Table 1 .
Themes and sub-themes, demographic information, VAS scores and GAD-7 scores for BAME and white groups
| Themes | Sub-theme | BAME (%)* | White (%)* | P-value | Statistical test |
|---|---|---|---|---|---|
| Demographics | Median age (IQR) | 55 (29) | 68 (24) | 0.028 | Mann–Whitney U |
| Female | 49.1 | 66.3 | 0.043 | Chi squared | |
| Impact of cancellation of elective surgery | Increase in pain | 50.9 | 62.8 | 0.163 | Chi squared |
| Reduction in mobility | 34.5 | 30.2 | 0.592 | Chi squared | |
| Mental health deterioration | 16.4 | 7 | 0.078 | Chi squared | |
| Median GAD-7 score (IQR) | 0 (4) | 2 (7) | 0.009 | Mann–Whitney U | |
| Meet criteria for generalised anxiety disorder | 7.3 | 15.1 | 0.163 | Chi squared | |
| Median VAS score (IQR) | 80 (50) | 75 (28) | 0.635 | Mann–Whitney U | |
| Feelings about cancellation | Understand and/or expected | 23.6 | 55.8 | <0.001 | Chi squared |
| Disappointed and/or upset | 43.6 | 50 | 0.460 | Chi squared | |
| Feelings about restarting | Pleased about restart | 47.3 | 82.6 | <0.001 | Chi squared |
| Nervous and/or apprehensive | 23.6 | 20.9 | 0.705 | Chi squared | |
| Concerned about COVID-19 | 54.5 | 66.3 | 0.162 | Chi squared | |
| No longer want surgery | 21.8 | 14 | 0.225 | Chi squared | |
| Want operation as soon as possible | 74.5 | 74.4 | 0.987 | Chi squared | |
| Want operation when pandemic is over | 21.8 | 9.3 | 0.048 | Chi squared | |
| Feeling about new preoperative and postoperative protocols | Preoperative assessment/swab acceptable | 80 | 90.7 | 0.070 | Chi squared |
| Self-isolation acceptable (2-week preoperative and 2-week postoperative) | 89.1 | 83.7 | 0.373 | Chi squared | |
| Telephone follow-up acceptable | 80 | 87.2 | 0.250 | Chi squared | |
| Written physiotherapy information acceptable | 83.6 | 87.2 | 0.553 | Chi squared |
*Unless specified otherwise.
Impact of the cancellation of surgery
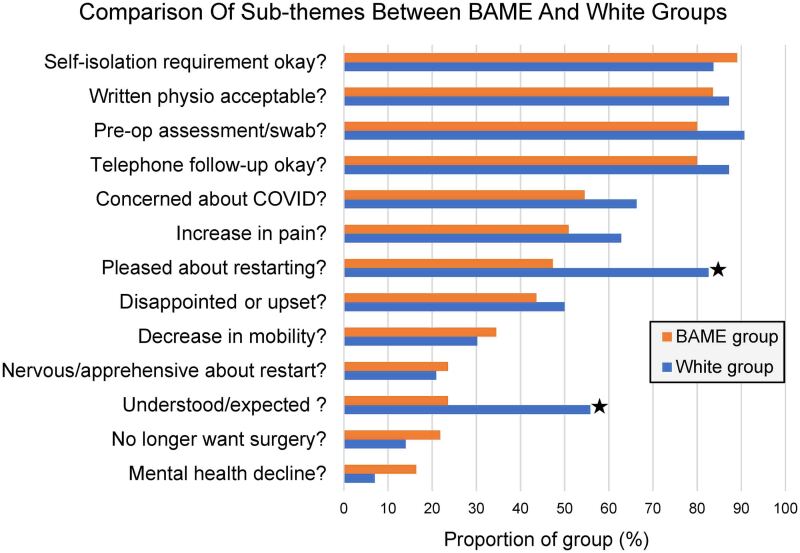
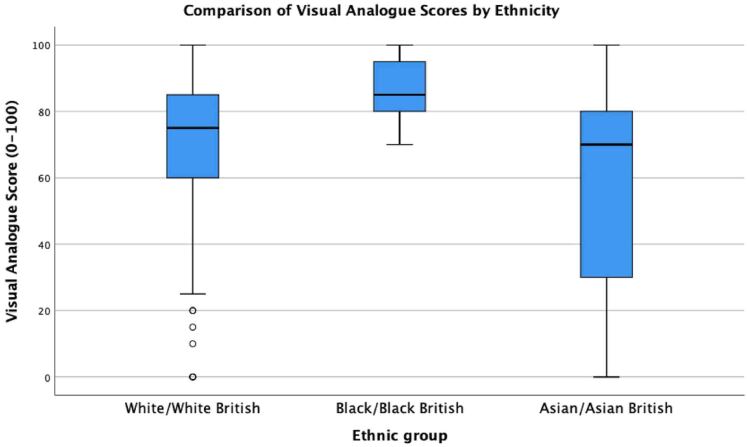
There was no difference between the proportion of patients in BAME groups reporting that their pain had worsened during the pandemic compared with white/white British patients (BAME 50.9% vs 62.8%, p=0.163), or in median (IQR) VAS scores (BAME 80 (50) vs 75 (28), p=0.635) (Figure 1). Black/Black British patients had significantly higher median VAS scores than patients in the white/white British and Asian/Asian British groups (85 (19) vs 75 (28) vs 70 (50) respectively, p<0.05) (Figure 2).
Figure 1 .
Bar chart comparing sub-themes between BAME and white groups (*p<0.05)
Figure 2 .
Box-plot of VAS scores for Asian/Asian British, Black/Black British and White/White British groups. (Mixed ethnic groups and other ethnic groups were not included in this analysis due to limited data.)
A common theme across ethnic groups was the detrimental impact that pain was having on aspects of day-to-day life, such as sleep, fatigue and challenges in caring for loved ones. Many patients had developed new pain in different joints, had an increased analgesia requirement and reported an increased reliance on primary care. Similar proportions of each group reported worsening mobility (BAME 34.5% vs 30.2%, p=0.592), and explained that this had led to difficulties in performing activities of daily living. An emerging theme was the negative impact on jobs and being unable to work.
White/white British patients had higher GAD-7 scores than those in BAME groups (2 (0–21) vs 0 (0–16), p=0.009), and 15.1% met the criteria for generalised anxiety disorder (vs 7.3%, p=0.163). Individual components of the GAD-7 score are shown in Figure 3. There was no difference between groups in the proportion of patients reporting that their mental health had deteriorated since the start of the pandemic (BAME 16.4% vs 7.0%, p=0.078). A common theme was feeling more anxious and having low mood, often directly as a result of worsening physical health: ‘I’m now having to use a [walking] stick, and I’m worsening at day-to-day activities which has really affected my mood’ (Asian/Asian British (Indian) patient).
Figure 3 .
Bar chart of mean average components of GAD-7 score comparison between BAME and white groups. Error bars denote standard error of mean.
Feelings about the cancellation of surgery
More than double the proportion of white patients expected cancellation of their operation compared with patients in BAME groups (55.8% vs 23.6%, p<0.001). There was no difference in the proportions of patients who were disappointed or upset about the cancellation (BAME 43.6% vs 50%, p=0.460). Patients explained the disappointment was due to having mentally prepared for an operation, but were also upset about not having been kept up-to-date about the cancellation.
Perspectives on restarting surgery
Fewer of the BAME group were pleased about the resumption of elective surgery (47.3% vs 82.6%, p<0.001). Patients expressed worry: ‘I’m concerned that there will be a second wave’ (Asian/Asian British (Indian) patient). There was no difference in the levels of feeling nervous about restarting surgery (BAME 20.9% vs 23.6%, p=0.705), or in the level of concern about contracting COVID-19 in hospital (BAME 54.5% vs 66.3%, p=0.162).
A greater proportion of BAME patients wanted to delay their operation until after the pandemic (21.8% vs 9.3%, p=0.048). A perceived risk of a bad outcome following COVID-19 appeared to influence decisions, through statements like ‘I would prefer to have my surgery at a later date as I have lots of health problems’ (Asian/Asian British (any other Asian background) patient). Some patients expressed concerns about how their care would be different due to COVID-19: ‘I’m concerned about where it will be done [different hospital]’ (Asian/Asian British (Bangladeshi) patient).
Similar proportions of each group wanted to have their operation as soon as possible (BAME 74.5% vs 74.4%, p=0.987). Many rationalised their decision using comparisons of the return to normal within society, ‘I want to get it done quickly, especially as people are now going back to work’ (Asian/Asian British (Pakistani) patient).
There was no difference in the proportion of patients who wanted to cancel their operation entirely (BAME 21.8% vs 14%, p=0.225). For lots of patients, there was uncertainty in their decision: ‘at present I am concerned [about catching COVID-19] as although the numbers [of positive cases] has come down, there is still a risk’ (Asian/Asian British (Indian) patient). In others, we sensed the decision was evolving as the pandemic and the impact of the delay progressed: ‘[I]nitially I was quite worried [about COVID-19], but now I want it done because my quality of life is deteriorating’ (Asian/Asian British (Indian) patient).
Discussion
Impact of the cancellation of surgery
The consequences of the delay in elective surgery have been devastating for patients. Most patients, irrespective of their ethnic group, reported that their pain had worsened, and that their mobility had reduced. Patients in Black/Black British groups had higher VAS scores, which is concerning as it is well known that preoperative pain is a predictor of poor postoperative clinical outcomes.12 Many patients required increased analgesia, which is worrying as long-term use of non-steroidal anti-inflammatory drugs predisposes patients to the risk of gastrointestinal bleeding, renal dysfunction and adverse cardiovascular events,13 while chronic use of opiate painkillers impacts on most organ systems, along with the risk of addiction.14 Additionally, use of preoperative analgesia is associated with poorer postoperative clinical outcomes.12
Patients reported how the pain had led to a deterioration in their sleep, particularly in Asian/Asian British Indian patients. Our study was underpowered to find significant differences between ethnicities, but this is consistent with the literature15 and is concerning because poor sleep is another predictor of poor clinical outcomes following surgery.12
Many patients had a significant deterioration of mobility, which may lead to disuse muscle atrophy. This is particularly concerning in older patients for whom recovery of muscle mass is delayed and may not recover back to baseline levels.16 In some patients reduced mobility had led to weight gain, predisposing them to obesity-related health complications.
There is variation in anxiety between ethnic groups, and in our study white/white British patients had higher GAD-7 scores, with over 15% meeting criteria for generalised anxiety disorder. Preoperative anxiety is known to confer poorer clinical and functional outcomes following elective orthopaedic surgery,12 therefore it is important that this is addressed appropriately in redesigned services. It is interesting that although a common theme was feeling more anxious, median GAD-7 scores are relatively low, suggesting that anxiety levels started at a low baseline.
Many patients reported the wider implications of their increased pain and reduced mobility on others and society. Patients expressed concern about being unable to care for others or were now unable to work and had either had to take sick leave or had been laid off completely.
Feelings about the cancellation of surgery
Patients in both groups were annoyed or upset about the cancellation. Although this was often due to having mentally prepared for surgery, some were frustrated about the lack of contact from the hospital to inform them of the cancellation. Patients must receive clear communication about their procedure and be updated regularly with changes, especially as the redesigned elective surgery services may be subject to cancellations and changes to planned care during subsequent COVID-19 waves.
Perspectives on restarting surgery
Fewer BAME patients were pleased about the NHS resuming elective surgery during the pandemic and were more than twice as likely to want to delay their operation until after the pandemic was over. Understanding the motive for this decision is not straightforward; there was no difference between BAME and white groups regarding concern over the risk of contracting COVID-19, and other researchers have found that the decision to proceed with surgery is not correlated with perceived COVID-19 risk.5 However, patients often rationalised their decision to delay surgery by explaining that they were ‘high-risk’ because they had one or more comorbidities, and therefore perceived risk from COVID-19 does appear to drive at least some of the decision-making in patients. As it is well known that BAME patients are disproportionately affected by COVID-19,6 this may explain some of the decision-making.
The enthusiasm for recommencing elective surgery is reassuring, but clearing the backlog relies on patients taking up operations when offered the opportunity, and for this to happen patients must have confidence in a healthcare system that is safe. Although it remains difficult to quantify the risk of contracting COVID-19 in hospital, it does appear as though elective procedures can be performed safely during the pandemic, on the provision that measures are in place to reduce virus transmission.17 It is important that patients are well informed of the risks and benefits of delaying surgery further, as well as the risks of having elective surgery during the pandemic. However, we have identified that the decision to delay surgery is more complicated than just concern about the risk of contracting COVID-19.
For patients who choose to delay their operation until the end of the COVID-19 pandemic, it is unclear what the repercussions might be,18 or when this may be. Longer waiting times are associated with greater disability prior to surgery,19 and our study shows that the delay caused by the pandemic has had a devastating impact on the physical and mental health of patients on waiting lists. By further postponing surgery, it is likely that the impact will only get worse for these patients. Any further deterioration in quality of life is particularly concerning given that 12–19% of patients waiting for joint replacements had a score of ‘worse than death’20 (EuroQol five-dimension score) before the pandemic started. Delays in surgery have an adverse impact on other aspects of patients’ lives, including their ability to work or care for others, which may lead to financial concerns and family tension.
Longer waiting times are also associated with significantly poorer functional status and clinical outcomes even after an operation.19,21 Delaying surgery in certain patient groups can result in a requirement for more complex surgery, carrying greater risks of complications and greater costs.22 Because BAME patients are twice as likely to want to delay their operation, the potential health inequalities that may arise from this further delay are of tremendous concern.
Future research should explore the views of ethnicities that are underrepresented in this study and should address how patients on waiting lists feel as the pandemic phases out of the second wave. It will also be helpful to know how patients awaiting other types of elective procedure outside of the orthopaedic discipline feel about the return to elective procedures.
Strengths, weaknesses and bias
This study has many strengths. The mixed-methods design allowed triangulation of qualitative and quantitative data, giving a rich analysis of patients’ perspectives. There are numerous limitations. Although it includes an overrepresentation of patients in BAME groups compared with the general population, our study does not include anyone in mixed/multiple ethnic groups, and for Black/Black British and other ethnic groups the number of participants is small. The study is underpowered to find significant differences between individual ethnicities, but this does not mean that these differences do not exist. By using the categories of BAME and white, the findings may not capture the views of different groups within BAME. The population may not be generalisable to other countries.
Patients were awaiting a variety of types of elective procedure. Although the sample size is too small to allow subgroup analysis, the views of the day case patients may be different from those of patients requiring a postoperative inpatient stay. There are age and gender differences between groups which may have confounded the results. Other potential covariates, such as socio-economic status, may have influenced the results. The study was conducted by members of the orthopaedic team at both centres which may have led to researcher bias at all levels. Interviews took place between June and November 2020; the extended period may have introduced temporal bias. Purposive sampling may lead to selection bias. Responder bias may exist due to the patients the researchers were unable to contact.
Conclusion
The extended waiting time due to the COVID-19 pandemic has had a devastating impact on patients awaiting elective operations. There is variation in pain and anxiety levels between different ethnic groups, which must be sufficiently addressed when redesigning services to avoid discrepancies in clinical and functional outcomes following surgery. There are differences in the perspectives of patients from different ethnic backgrounds on the return to elective surgery, which may reflect disparities in outcomes, particularly with regards to ethnicity. Those in BAME groups are more likely to be upset about their operation being cancelled, but are more likely to postpone their postponed operation, which may lead to further deterioration in their mental and physical health, negative psychosocial and socioeconomic consequences, and poorer clinical outcomes following surgery.
As the NHS redesigns services to facilitate a return to elective operating and tackle the extraordinary backlog of operations, efforts should be made to reassure patients that it is safe to resume operating to prevent health inequalities between patients from different backgrounds, and to yield the best clinical outcomes for all. Additionally, there may be a need for screening patients on the waiting list to prioritise those on the basis of current clinical need rather than time on the list alone.
Conflicts of interest
Professor Pandit is a National Institute for Health Research (NIHR) Senior Investigator. The views expressed in this article are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Funding
This paper presents independent research funded/supported by the National Institute for Health Research (NIHR) and Leeds Biomedical Research Centre (BRC).
References
- 1.Royal College of Surgeons of England. CSR: £3bn ‘stop-gap’ falls short of what NHS needs to tackle mammoth waiting list. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/statement-in-advance-of-the-comprehensive-spending-review/ (cited January 2021).
- 2.Macdonald N, Clements C, Sobti Aet al. Tackling the elective case backlog generated by Covid-19: the scale of the problem and solutions. J Public Health (Oxf) 2020; 42: 712–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mishra B, BODS Collaborators, Roy B. BODS/BOA survey of impact of COVID-19 on UK orthopaedic practice and implications on restoration of elective services - part 2. Transient J 2020. https://www.boa.ac.uk/resources/bods-boa-survey-of-impact-of-covid-19-on-uk-orthopaedic-practice-and-implications-on-restoration-of-elective-services-part-2.html (cited January 2021). [Google Scholar]
- 4.Royal College of Surgeons. Recovery of surgical services during and after COVID-19. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/#s1 (cited January 2021).
- 5.Madanipour S, Al-Obaedi O, Ayub Aet al. Resuming elective hip and knee arthroplasty in the COVID-19 era: a unique insight into patient risk aversion and sentiment. Ann R Coll Surg Engl 2020. https://pubmed.ncbi.nlm.nih.gov/33185459/ (cited January 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Public Health England. Disparities in the risk and outcomes of COVID-19. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf (cited January 2021).
- 7.Treweek S, Forouhi NG, Narayan KMVet al. COVID-19 and ethnicity: who will research results apply to? Lancet 2020; 395: 1955–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swarup I, Henn CM, Gulotta LVet al. Patient expectations and satisfaction in orthopaedic surgery: A review of the literature. J Clin Orthop Trauma 2019; 10: 755–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delgado DA, Lambert BS, Boutris Net al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. JAAOS Glob Res Rev 2018; 2: e088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spitzer RL, Kroenke K, Williams JBWet al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 11.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 12.Yang MMH, Hartley RL, Leung AAet al. Preoperative predictors of poor acute postoperative pain control: A systematic review and meta-analysis. BMJ Open 2019; 9: e025091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcum ZA, Hanlon JT. Recognizing the risks of chronic nonsteroidal anti-inflammatory drug use in older adults. Ann LongTerm Care 2010; 18, 24–27. [PMC free article] [PubMed] [Google Scholar]
- 14.Baldini A, von Korff M, Lin EHB. A review of potential adverse effects of long-term opioid therapy: A practitioner’s guide [internet]. Prim Care Companion J Clin Psychiatry 2012; 14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3466038/ (cited January 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office for National Statistics. Coronavirus and the social impacts on different ethnic groups in the UK. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/coronavirusandthesocialimpactsondifferentethnicgroupsintheuk/2020 (cited January 2021).
- 16.Bodine SC. Disuse-induced muscle wasting. Int J Biochem Cell Biol 2013; 45: 2200–2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Royal College of Surgeons of England. Managing elective surgery during the surges and continuing pressures of COVID-19. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/tool-7/ (cited January 2021).
- 18.Williams P, Beard DJ, Verghese N. Yet another iceberg? The hidden potential harm of elective orthopaedic waiting lists. Transient J 2020. https://www.boa.ac.uk/resources/knowledge-hub/yet-another-iceberg-the-hidden-potential-harm-of-elective-orthopaedic-waiting-lists.html (cited January 2021). [Google Scholar]
- 19.Hajat S, Fitzpatrick R, Morris Ret al. Does waiting for total hip replacement matter? Prospective cohort study. J Heal Serv Res Policy 2002; 7: 19–25. [DOI] [PubMed] [Google Scholar]
- 20.Scott CEH, MacDonald DJ, Howie CR. ‘Worse than death’ and waiting for a joint arthroplasty. Bone Jt J 2019; 101B: 941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortin PR, Clarke AE, Joseph Let al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum 1999; 42: 1722–1728. [DOI] [PubMed] [Google Scholar]
- 22.Arthritis and Musculoskeletal Alliance. ‘Rationing’ Access to Joint Replacement Surgery and Impact on People with Arthritis and Musculoskeletal Conditions. http://arma.uk.net/wp-content/uploads/2017/08/Policy-Position-Paper-Surgery_v5_Interactive.pdf (cited January 2021).