Abstract
Introduction
Postoperative pulmonary complications and mortality rates during the COVID-19 pandemic have been higher than expected, leading to mass cancellation of elective operating in the UK. To minimise this, the Guy’s and St Thomas’ Hospital NHS Foundation Trust elective surgery hub and the executive team at London Bridge Hospital (LBH) created an elective operating framework at LBH, a COVID-19 minimal site, in which patients self-isolated for two weeks and proceeded with surgery only following a negative preoperative SARS-CoV-2 polymerase chain reaction swab. The aim was to determine the rates of rates of postoperative COVID-19 infection.
Methods
The collaboration involved three large hospital trusts, covering the geographic area of south-east London. All patients were referred to LBH for elective surgery. Patients were followed up by telephone interview at four weeks postoperatively.
Results
Three hundred and ninety-eight patients from 13 surgical specialties were included in the analysis. The median age was 60 (IQR 29–71) years. Sixty-three per cent (252/398) were female. In total, 78.4% of patients had an American Society of Anesthesiologists grade of 1–2 and the average BMI was 27.2 (IQR 23.7–31.8) kg/m2. Some 83.6% (336/402) were ‘major’ operations. The rate of COVID-19-related death in our cohort was 0.25% (1/398). Overall, there was a 1.26% (5/398) 30-day postoperative all-cause mortality rate. Seven patients (1.76%) reported COVID-19 symptoms, but none attended the emergency department or were readmitted to hospital as a result.
Conclusion
The risk of contracting COVID-19 in our elective operating framework was very low. We demonstrate that high-volume major surgery is safe, even at the peak of the pandemic, if patients are screened appropriately preoperatively.
Keywords: COVID-19 minimal site, Surgical outcomes, Network, COVID-19 screening
Background
On 11 March 2020, the World Health Organization (WHO) declared COVID-19 a global pandemic, after the emergence of a severe acute respiratory disease that originated in Wuhan City, China in December 2019. At the time of writing, there have been over 44,236 deaths and 285,768 laboratory-confirmed cases in the UK.1 The pandemic has had significant impact on the delivery of safe surgical services worldwide, with an estimate of at least 28 million elective operations cancelled across 190 countries.2 Surgical departments have had to balance the risk of nosocomial transmission of infection, preserving hospital resources with the redistribution of staff, equipment and space, while maintaining essential operations during the pandemic. Advice on postoperative complications secondary to COVID-19 is limited in the context of a novel virus and the current published guidelines are based solely on expert opinion.3–5
An article from Wuhan, early in the pandemic, reviewed the outcomes of patients who unintentionally had elective surgery during the incubation period of the virus. Their data suggested that surgery may accelerate COVID-19 progression leading to an increased rate of intensive care unit admissions and a 20.5% mortality rate.6 A recent international cohort study reviewed the outcome of over 1,000 adult patients in 12 countries between 1 January and 31 March 2020, where approximately 26% of patients had confirmed preoperative COVID-19. Their study demonstrated a 30-day postoperative mortality of 23.8% and pulmonary complications in 51% of patients: associated risk factors were age over 70 years, male sex, poor preoperative physical health, American Society of Anesthesiologists (ASA) grades 3–5, emergency surgery, major surgery and malignant rather than benign disease.7 A scoping search and key informant interviews were conducted among surgeons and anaesthetists internationally in a plan for surgical services in the face of this pandemic.4 With an inevitable backlog of procedures after the end of the pandemic, context-specific pandemic preparedness plans were required to manage this, including ensuring that patients having elective treatments have the best possible outcomes.8 In a bid to manage this, the NHS surgical specialties led by Guy’s and St Thomas’ Hospital NHS Foundation Trust (GSTT) together with South East London Cancer Network (comprising University Hospital Lewisham NHS Trust and King’s College Hospital NHS Trust) set up a multicentre surgical network (the South East London (SEL) COVID-19 Hub) based at London Bridge Hospital (LBH) as a COVID-19 minimal site, aiming to perform essential elective surgery. In March 2020, 13 surgical specialties commenced elective surgery at LBH based on this principle under a mixed model of care.
The aim of our study was to determine the number of patients who developed COVID-19 (defined as a positive swab, COVID-19-like symptoms in the 30 days post discharge, hospital admission or mortality related to COVID-19).
Methods
Setting
LBH, an independent hospital that is part of Hospital Corporation of America, was chosen to be part of the SEL COVID-19 Hub owing to its pre-existing infrastructure and relationships with GSTT. LBH is well situated geographically and met capacity requirements, consisting of 155 single rooms, 26 intensive care unit beds, 8 high-dependency unit beds and 10 operating theatres. In addition, it was well suited in terms of a known working relationship between the key hospitals with prior experience in all of the specialties involved (Supplementary Appendix 1, online only).
Patients
All adult NHS patients (over 18 years old) from 13 surgical specialties from GSTT and the South East London Cancer Network, who had a planned elective procedure between 27 March 2020 and 22 May 2020, with final discharge from LBH on 29 May 2020, were included. Patients undergoing procedures for any indication were eligible (Supplementary Appendix 1, online only). For each specialty, a complexity code of ‘minor’ or ‘major’ was applied to the procedure performed, as defined in the COVIDSurg study7 and based on coding typically provided by insurance companies (www.ccsd.org.uk).
Admission pathway and inpatient management
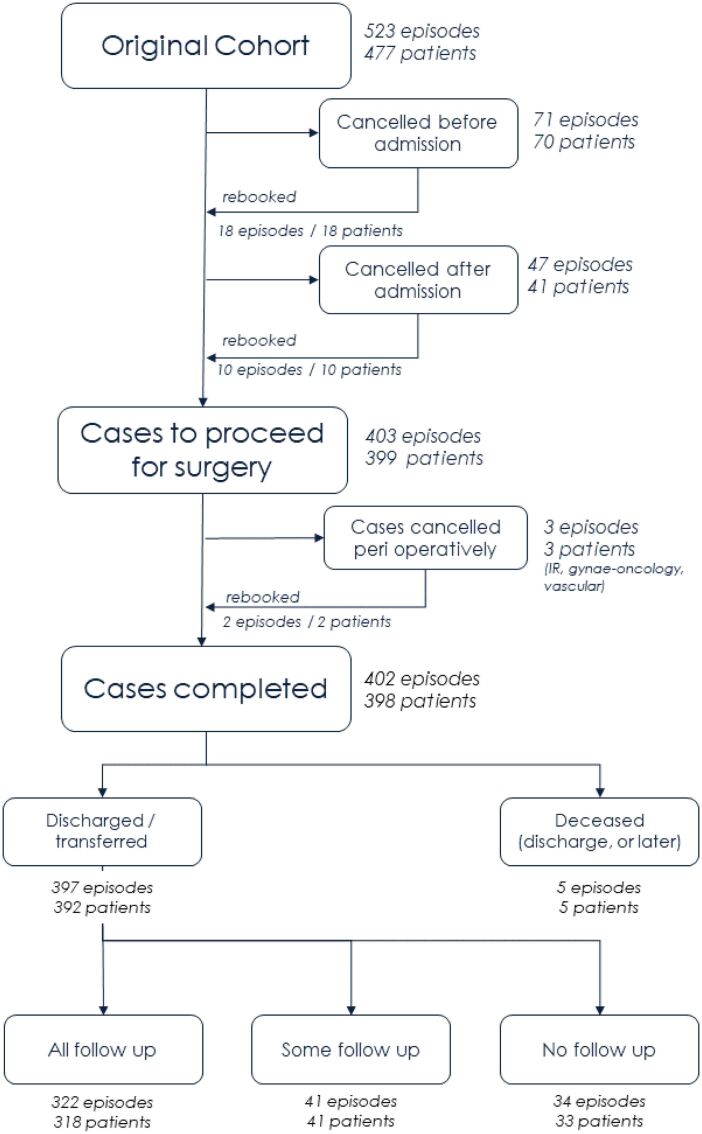
Rapid restructuring of the hospital and hospital processes was performed to minimise risk of viral transmission in admitted patients. This incorporated sets of principles around patient triage and screening, staff education and screening, pathways to minimise potential COVID-19 contacts, and processes for travel, clustering and isolation, as described in the ‘COVID-minimal cancer surgery pathway’.9 All patients and their entire household were advised to shield (Supplementary Appendix 2, online only) for two weeks prior to admission and screening was undertaken 24–48 hours pre-procedure for COVID-19 infection using a nasopharyngeal swab, which was sent for viral RNA detection via quantitative real-time polymerase chain reaction (RT-PCR). Prior to admission it was confirmed that the patient had complied with the period of self-isolation and was not exhibiting any signs or symptoms of COVID-19. Patients were then invited to be admitted, ensuring that they travelled using private transport. On admission, a further symptom check and temperature screening were performed and the patient was cleared to proceed with their planned procedure after confirming a negative SARS-CoV-2 PCR test result. Any patient who had a positive SARS-CoV-2 screening swab at admission did not proceed with surgery and was discharged home or transferred to GSTT or King’s College Hospital depending on clinical state. These patients were rebooked as appropriate following two negative swabs performed after two weeks. Patients cancelled for any other reason were excluded from our study (Figure 1). Theatres were cleaned between each case in line with infection control advice.
Figure 1 .
Study design (all rebooked cases are included in the original cohort)
All patients were admitted to an ‘amber’ area (denoting uncertain COVID-19 status) for assessment before proceeding for surgery, and to postoperative care in a ‘green’ zone (confirmed negative COVID-19 swab). All patients were admitted to individual rooms. All healthcare interaction involved the use of universal personal protective equipment including disposable aprons, gloves, surgical masks (or FFP3 mask if performing aerosol-generating procedures) and eye protection. Efforts were taken to maintain social distancing where possible, including telephone consultations for pharmacy and physiotherapy initial assessments.
On discharge, advice regarding shielding was variable depending on the clinical team.
Data collection
The following data were obtained by telephone interview between three and four weeks after discharge from LBH: presence of COVID-19 signs or symptoms, contact with healthcare professionals, attendance at emergency department (ED) or other hospital contact, self-isolating practices post discharge from LBH, and if any household contacts were diagnosed with or had symptoms of COVID-19. Verbal consent was obtained to confirm participation. Baseline patient demographic data were confirmed from the electronic database (Meditech Electronic Health Record, Westwood, MA, USA) and included age, sex, BMI, length of stay, operation length and ASA grade.
For patients who could not be contacted by telephone for follow-up, their clinical teams were contacted and the GSTT electronic patient record system was interrogated to determine whether ED attendance or admissions had occurred.
Governance
This audit was registered with GSTT as part of the SEL COVID-19 Hub NHS and independent sector clinical governance framework (project number 10905).
Outcomes
The primary outcome was COVID-19 infection in the four weeks post discharge. Secondary outcomes were hospital readmission rates and COVID-19-related deaths. COVID-19 infection was defined as clinical symptoms suggesting infection including cough, fever and myalgia, and/or viral RNA detection by RT-PCR.
Data processing and statistical analysis
The study was conducted based on the STROBE guidelines for observational studies.10 Data were received from the collection team as flat files, which were loaded into the R statistical computing environment for processing (www.R-project.org). A tidyverse processing pipeline was constructed to produce a final data set for analysis. This pipeline stripped all patient-identifiable data (except for NHS number), combined the flat files and linked to other data sources. Linkage to the LBH patient administration system was performed to confirm which of the patients had been admitted and undergone surgery, which episodes had been cancelled, and at what point in the pathway any cancellations had occurred. This data linkage was also used to determine each patient’s discharge status and retrieve supplementary data items such as ASA physical status classification and BMI. Analysis of free-text fields was performed by breaking the text corpus into n-grams (for n = 1, 2, 3) using the tidytext package. Term-frequency analysis and text pattern recognition were used to detect and extract key information from this free text.
Patient and public involvement
There was no patient and public involvement in this project.
Results
Between 27 March 2020 and 22 May 2020, 523 cases from 13 specialities were referred from GSTT, King’s College Hospital and University Hospital Lewisham to the SEL COVID-19 Hub for elective surgery at LBH. Each referred case was an individual surgical booking (episode) and a rebooking or booking of a second-stage procedure was considered a second episode. One hundred and twenty-one cases were excluded. Of these, 71 (13.6%) episodes were cancelled before admission for unspecified reasons, 47 (9.0%) episodes cancelled after admission (17 [3.25%] were cancelled due to a positive SARS-CoV-2 PCR test, two were cancelled on clinical grounds, and the cause for cancellation was unknown for the remaining 28 episodes). A further three cases were cancelled on clinical reasons peri-procedure; these included an interventional radiology case, a gynaecological oncology case and a vascular procedure. In total, 403 cases (from 398 patients) were completed from admission to discharge and included in the final analysis (Figure 1). However, of the 403 completed cases, one patient was cancelled perioperatively and not rebooked but completed the process from admission to discharge and was included in the analysis. Some 99.3% (400/403) of cases had a negative preoperative SARS-CoV-2 PCR test. Three patients had a positive SARS-CoV-2 PCR test at the NHS site prior to admission and a negative result on admission to LBH. These patients proceeded for surgery and were considered as ‘positive’ in the reporting. All three patients had an uncomplicated inpatient stay, with no reported deaths, ED attendance or readmission, although one patient in this group reported COVID-19 symptoms during the follow-up period.
The median age of patients was 60 (IQR 29–71) years. Some 63.3% (252/398) of patients were female, 78.4% (312/398) had an ASA grade of 1–2 and the average BMI was 27.2 (IQR 23.7–31.8; Table 1). The ethnic distribution is unknown as ethnicity was recorded for only ten patients. Median length of stay was 3 (range: 1–26) days, with a median operation time of 132.5 (15–1,526) minutes. The operations performed were predominantly for confirmed or suspected cancer in breast surgery, gastrointestinal, gynaecology, hepatobiliary, neurosurgery, head and neck, urology, plastic surgery and thoracic specialities, and for urgent non-cancer cases in interventional cardiology, interventional radiology, cardiac and vascular surgery. Of the operations, 16.4% (66/402) were classed as ‘minor’ and 83.6% (336/402) as ‘major’ (Figure 1).
Table 1 .
Demographics of cohort by specialty
| Cardiac surgery | Cardiology (interventional) | Thoracic | Breast | Gastrointestinal | Gynae oncology | Head and neck | Hepatobiliary | Interventional radiology | Neurosurgery | Plastics | Urology | Vascular | Overall | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | F | 0 | 0 | 48 | 69 | 29 | 43 | 10 | 6 | 3 | 7 | 5 | 31 | 1 | 252 |
| M | 2 | 4 | 15 | 1 | 19 | 0 | 17 | 14 | 5 | 12 | 10 | 39 | 12 | 150 | |
| Age group (years) | 18–29 | 0 | 0 | 1 | 2 | 3 | 3 | 3 | 0 | 1 | 1 | 0 | 2 | 1 | 17 |
| 30–49 | 1 | 0 | 4 | 28 | 12 | 13 | 4 | 2 | 1 | 7 | 1 | 19 | 1 | 93 | |
| 50–69 | 0 | 2 | 28 | 32 | 26 | 21 | 15 | 9 | 5 | 7 | 1 | 27 | 4 | 177 | |
| >69 | 1 | 13 | 30 | 8 | 7 | 6 | 5 | 9 | 1 | 4 | 2 | 22 | 7 | 115 | |
| BMI (kg/m2) | <18.5 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 4 |
| 18.5–24 | 0 | 1 | 19 | 26 | 11 | 11 | 7 | 4 | 3 | 7 | 1 | 13 | 4 | 107 | |
| 25–29 | 0 | 0 | 21 | 14 | 23 | 15 | 13 | 11 | 2 | 8 | 7 | 25 | 4 | 143 | |
| 30–35 | 1 | 2 | 14 | 15 | 12 | 8 | 5 | 4 | 3 | 2 | 2 | 17 | 4 | 89 | |
| >35 | 1 | 1 | 5 | 13 | 2 | 9 | 2 | 1 | 0 | 1 | 5 | 14 | 1 | 55 | |
| Unknown | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | |
| ASA classification | 1 | 0 | 0 | 1 | 8 | 12 | 12 | 6 | 4 | 0 | 1 | 0 | 10 | 0 | 54 |
| 2 | 0 | 3 | 37 | 56 | 30 | 27 | 20 | 13 | 4 | 15 | 1 | 47 | 5 | 258 | |
| 3 | 1 | 1 | 20 | 5 | 5 | 4 | 1 | 2 | 3 | 2 | 9 | 11 | 7 | 71 | |
| 4 | 1 | 0 | 5 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 4 | 2 | 1 | 17 | |
| Unknown | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 2 | |
| Length of stay (days) | Median (range) | 8 (7–9) | 2 (1–2) | 6 (1–23) | 2 (1–6) | 5 (1–11) | 4 (1–11) | 3 (1–19) | 9 (6–24) | 1.5 (1–3) | 5 (2–8) | 3 (1–8) | 2 (1–10) | 2 (2–6) | 3 (1–26) |
| Procedure duration (minutes) | Median (range) | 183.5 (176–191) | 82 (47–87) | 139 (64–240) | 104.5 (57–224) | 117 (20–296) | 126 (20–300) | 100 (38–538) | 258.5 (171–615) | 194 (15–388) | 196 (65–292) | 69 (45–1526) | 70 (18–498) | 132 (44–388) | 132.5 (15–1526) |
In the study group, there was one (0.25%) outpatient death due to COVID-19 and a total of five (1.26%) deaths. There were three in-hospital deaths: following lobectomy in one patient and following transcatheter aortic valve implantation (TAVI) procedures in two patients; one of these patients required transfer back to GSTT from LBH following an intracerebral event after a TAVI procedure. None of these patients had a positive SARS-CoV-2 PCR test. However, there was suspicion of a possible COVID-19-related syndrome for the lobectomy patient. Two deaths occurred following discharge; one patient was readmitted to hospital and another was found dead at home. The cause of death remains unknown in the latter, pending coroner’s review. The former, aged 83 years, died of COVID-19 pneumonitis. This patient was discharged to an inpatient rehabilitation facility following resection of a bladder tumour under general anaesthetic. It is unclear if he had been shielding prior to surgery. He was readmitted to his local hospital 16 days after discharge and died nine days later of COVID-19 pneumonitis.
No other patients attended ED or were readmitted with COVID-19 following discharge (Table 2); 7.5% (30 of 398) were readmitted for non-COVID-19-related issues. Seven patients (of 398; 1.76%) reported COVID-19 symptoms; none had a PCR-confirmed diagnosis. Of these patients, only one was above the age of 75, two patients had a BMI > 35 and five had undergone major surgery. Seventy-two patients reported symptoms not felt to be related to COVID-19 (Table 3). The three patients with a positive preadmission SARS-CoV-2 PCR test who underwent planned surgery had no ED attendance or readmission, although one reported COVID-19 symptoms during the follow-up period.
Table 2 .
Outcomes
| Cardiac surgery | Cardiology (interventional) | Thoracic | Breast | Gastrointestinal | Gynae oncology | Head and neck | Hepatobiliary | Interventional radiology | Neurosurgery | Plastics | Urology | Vascular | Overall | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 symptoms | Yes | 0 | 0 | 0 | 1 | 1 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 1 | 7 |
| No | 2 | 3 | 56 | 61 | 46 | 39 | 22 | 17 | 8 | 15 | 11 | 55 | 11 | 346 | |
| Unknown | 0 | 1 | 7 | 8 | 1 | 4 | 2 | 3 | NA | 4 | 3 | 15 | 1 | 49 | |
| Nurse / GP / consultant follow-up | Yes – COVID | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Yes – non-COVID | 2 | 0 | 56 | 54 | 13 | 31 | 24 | 16 | 5 | 12 | 11 | 38 | 8 | 270 | |
| No | 0 | 3 | 1 | 8 | 30 | 8 | 0 | 1 | 3 | 3 | 0 | 16 | 3 | 76 | |
| Unknown | 0 | 1 | 6 | 8 | 5 | 4 | 2 | 3 | 0 | 4 | 4 | 16 | 2 | 55 | |
| A&E visit | Yes – COVID | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes – non-COVID | 1 | 0 | 10 | 1 | 1 | 4 | 6 | 1 | 2 | 0 | 0 | 4 | 1 | 31 | |
| No | 1 | 3 | 47 | 62 | 41 | 35 | 20 | 16 | 6 | 15 | 11 | 50 | 10 | 317 | |
| Unknown | 0 | 1 | 6 | 7 | 6 | 4 | 1 | 3 | 0 | 4 | 4 | 16 | 2 | 54 | |
| Readmission | Yes – COVID | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes – non-COVID | 1 | 0 | 3 | 2 | 0 | 3 | 10 | 1 | 1 | 0 | 0 | 7 | 2 | 30 | |
| No | 1 | 3 | 54 | 61 | 43 | 37 | 16 | 16 | 7 | 15 | 11 | 47 | 9 | 320 | |
| Unknown | 0 | 1 | 6 | 7 | 5 | 3 | 1 | 3 | 0 | 4 | 4 | 16 | 2 | 52 | |
| Postoperative COVID-19 swab | Yes | 2 | 0 | 7 | 28 | 0 | 11 | 9 | 4 | 2 | 4 | 1 | 6 | 3 | 77 |
| No | 0 | 3 | 49 | 35 | 43 | 29 | 17 | 13 | 6 | 11 | 10 | 47 | 8 | 271 | |
| Unknown | 0 | 1 | 7 | 7 | 5 | 3 | 1 | 3 | 0 | 4 | 4 | 17 | 2 | 54 | |
| Postoperative COVID-19 swab result | Positive | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (for patients re-swabbed) | Negative | 0 | 0 | 5 | 2 | 0 | 4 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 12 |
| Unknown | 2 | 0 | 2 | 26 | 0 | 7 | 9 | 4 | 1 | 4 | 1 | 6 | 3 | 65 |
Table 3 .
Symptoms, not thought to be COVID-19 related, reported by patients from each specialty
| Cardiac surgery | Cardiology (interventional) | Thoracic | Breast | Gastrointestinal | Gynae oncology | Head and neck | Hepatobiliary | Interventional radiology | Neurosurgery | Plastics | Urology | Vascular | Overall | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 1 | n = 1 | n = 34 | n = 2 | n = 1 | n = 5 | n = 7 | n = 8 | n = 0 | n = 3 | n = 0 | n = 9 | n = 1 | 72 | |
| Fever | 1 | 0 | 0 | 1 | 0 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 8 |
| Coryzal symptoms/ hay fever | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Fatigue | 0 | 0 | 0 | 0 | 0 | 2 | 5 | 1 | 0 | 0 | 0 | 7 | 0 | 15 |
| Chronic cough | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 4 |
| Loss of smell or taste | 0 | 0 | 4 | 0 | 0 | 0 | 3 | 0 | 0 | 2 | 0 | 2 | 0 | 11 |
| Non-persistent cough | 0 | 0 | 16 | 2 | 1 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 24 |
| Myalgia | 0 | 0 | 5 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 9 |
| Loss of appetite | 1 | 0 | 16 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 5 | 0 | 24 |
| Breathlessness | 0 | 1 | 14 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 4 | 0 | 22 |
| Dizziness | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Diarrhoea | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 6 |
| Headaches | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 4 |
In total, 270 episodes had follow-up from their clinical team during the study time frame. Of these, 49.6% were face-to-face visits; only one consultation was related to possible COVID-19. Seventy-nine patients had a repeat SARS-CoV-2 PCR test following discharge as part of routine follow-up outpatient clinic screening; all were negative (Table 2).
In total, 64.8% (258/398) of patients reported ‘shielding’ for two weeks following discharge and 22.4% (89/398) reporting isolating and social distancing in accordance with government advice. Two patients reported less stringent social contact following discharge.
We were unable to contact 32 patients for telephone consultation. For these patients, follow-up data were obtained from the relevant specialist nursing teams or by review from of the electronic patients records. The majority had been reviewed by their clinical teams with no reports of COVID-19 infection, death or readmission. Four patients remain uncontactable.
Discussion
This study demonstrated that at our COVID-19 minimal site, where patients are actively screened for COVID-19, there was one confirmed case of COVID-19 three weeks postoperatively and an all-cause 30-day postoperative mortality rate of 1.25%. Only 1.75% of patients reported symptoms of COVID-19, of whom none required COVID-19-related hospital admission or ED attendance. These data have implications for surgical specialties worldwide, especially as current recommendations suggest postponement of non-critical procedures and promotion of nonoperative treatments avoiding the need for surgery.11
Both the patient who died with confirmed COVID-19 pneumonitis and the patient with PCR-negative suspected COVID-19 syndrome were operated on in the first week of our pathway, before the requirement for two-week self-isolation had effectively taken place. Furthermore, the patient readmitted with COVID-19 pneumonitis was discharged to a community hospital for rehabilitation prior to hospital readmission. As the incubation period of SARS-CoV-2 is estimated to be up to 14 days,12 it is likely that this patient acquired SARS-CoV-2 following discharge, as 16 days elapsed prior to readmission.
Kasivisvanathan et al reported no COVID-related deaths at their COVID minimal site where only 14% of patients were swabbed preoperatively.13 They report a similar proportion of patients diagnosed with COVID-19 postoperatively (confirmed or probable, based on symptoms). Of these patients, 40% had confirmed positive swabs and 4% required a chest CT for further investigation. In comparison, none of our patients who reported COVID-19-like symptoms presented to hospital for further management of their symptoms. Because the UK guidelines for COVID-19 published during the study period did not recommend swabbing unless the patient required hospital admission, we were unable to confirm the status of COVID-19 infection in our symptomatic and asymptomatic patients postoperatively.
The reported postoperative mortality rate during this pandemic ranged between 19% and 21%6,11 compared with our mortality rate of 1.26%, which is in line with the risk of death in a non-COVID-19 era postoperative surgical population.14 It is possible that there is selection bias in our cohort; a majority of our patients were lower risk, with an ASA grade of 1–2 and younger age. It is also likely that patients referred to the Hub were preferentially selected by the referring clinicians as those who would benefit from immediate surgery after balancing the risk of complications from COVID-19 in the wake of current surgical recommendations during this pandemic. Despite this, the majority of surgery was cancer related and 84% were classified as major operations, both reported as risk factors for mortality during this pandemic. Furthermore, of the five patients who died, all had major surgery, which carries a mortality risk on its own of approximately 3%.15 It is possible that our pathway of screening for COVID-19 preoperatively and maintaining a COVID-19 minimal site throughout, contributed to mortality levels equivalent to those pre-pandemic.
The main COVID-19 symptom reported was a cough that is non-specific and can be due to irritation of the throat after intubation. The other reported symptom was fever, again a common postoperative complication with infective aetiology. Despite being unable to determine if all patients who reported symptoms had confirmed COVID-19, none required admission to hospital. This further supports the importance of performing surgeries in a COVID-19 minimal site.
Many hospitals in the UK are now resuming elective surgery work and the risks of COVID-19 complications postoperatively are currently still significant. Since the UK landmark Montgomery v Lanarkshire case of March 2015,16 full disclosure regarding the risks involved in any operation is required, supporting patient autonomy in a shared decision-making process. During this pandemic, doctors are required to take reasonable care to ensure that patients are informed of any perioperative risks related to COVID-19 during the consent process.17 Our data show that the risk of COVID-19 complications in our setting was low and comparable with pre-pandemic levels. Further studies are required to further confirm this, but it appears that the risk of COVID-19 can be mitigated if appropriate steps are taken.
The strengths of this study include being the first report about surgical outcomes in a COVID minimal site that tested all patients preoperatively, where only patients confirmed negative for COVID-19 were allowed to proceed. Patients who had a positive test were rebooked where possible following two consecutive negative SARS-CoV-2 tests and completion of self-isolation practices as per WHO COVID-19 guidelines. This study also included patients who required major surgery and cancer-related operations, suggesting that COVID-19 infection risk is low despite these factors. The limitations of this study include recall bias, as patients reported symptoms based on memory. However, as the time since their operation was relatively short, it is unlikely that there would be major distortion of symptoms recalled. More information on other factors including ethnicity and comorbidities such as hypertension and diabetes would be useful to compare against reported risk factors of COVID-19 infections.18,19 It is important to note that four patients were uncontactable. The team made every effort to trace them including contacting their original clinical team at the patient’s local hospital and checking admission records. These missing patients could represent unreported cases of COVID-19 in our cohort, producing bias in our results.
Conclusion
We have shown that the risk for acquiring COVID-19 in our setting is very low and that performing high-volume major surgery is safe, even at the peak of the pandemic, if patients are screened preoperatively. Appropriate measures to facilitate the effort to keep the hospital COVID-19 minimal are required, including staff training, stringent infection control practices and infrastructural capacity to manage the screening process.
References
- 1.Coronavirus (COVID-19) in the UK. https://coronavirus.data.gov.uk/ (cited June 2020).
- 2.COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020. 10.1002/bjs.11746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coccolini F, Perrone G, Chiarugi Met al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg 2020; 15: 25. 10.1186/s13017-020-00307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020. 10.1002/bjs.11646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tao K, Zhang B, Zhang Pet al. Recommendations for General Surgery Clinical Practice in Novel Coronavirus Pneumonia Situation. Zhonghua Wai Ke Za Zhi 2020; 58. 10.3760/CMA.J.ISSN.0529-5815.2020.0001 [DOI] [PubMed] [Google Scholar]
- 6.Lei S, Jiang F, Su Wet al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020; 21: 100331. 10.1016/j.eclinm.2020.100331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Archer JE, Odeh A, Ereidge Set al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. 10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang ZC, Chong MSY, Liu GKPet al. COVID-19 and elective surgery. Ann Surg 2020. 10.1097/SLA.0000000000004091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boffa DJ, Judson BL, Billingsley KGet al. Pandemic recovery using a covid-minimal cancer surgery pathway. Ann Thorac Surg 2020. 10.1016/J.ATHORACSUR.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger Met al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–1457. 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 11.COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/triage (cited July 2020).
- 12.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 2020; 25: 2000062. 10.2807/1560-7917.ES.2020.25.5.2000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kasivisvanathan V, Lindsay J, Rakhshani-moghadam Set al. Evaluation of 30-day mortality for 500 patients undergoing non-emergency surgery in a COVID-19 cold site within a multicentre regional surgical network during the COVID-19 pandemic. medRxiv 2020. 10.1101/2020.06.10.20115543 [DOI] [Google Scholar]
- 14.Alleway R, Butt A, Ellis Det al. Knowing the risk a review of the peri-operative care of surgical patients a report by the national confidential enquiry into patient outcome and death. https://www.ncepod.org.uk/2011report2/downloads/POC_summary.pdf (cited July 2020). [Google Scholar]
- 15.Myrdal G, Gustafsson G, Lambe Met al. Outcome after lung cancer surgery. Factors predicting early mortality and major morbidity. Eur J Cardio-Thoracic Surg 2001; 20: 694–699. 10.1016/S1010-7940(01)00875-2 [DOI] [PubMed] [Google Scholar]
- 16.Supreme Court T. Montgomery (Appellant) v Lanarkshire Health Board (Respondent). https://www.supremecourt.uk/cases/docs/uksc-2013-0136-judgment.pdf (cited July 2020).
- 17.Sokol D, Dattani R. How should surgeons obtain consent during the covid-19 pandemic? BMJ 2020; 369. 10.1136/BMJ.M2539 [DOI] [PubMed] [Google Scholar]
- 18.Pan D, Sze S, Minhas JSet al. The impact of ethnicity on clinical outcomes in COVID-19: A systematic review. EClinicalMedicine 2020; 23: 100404. 10.1016/j.eclinm.2020.100404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guan W, Liang W, Zhao Yet al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 2020: 55. 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]