Abstract
Spontaneous urinary bladder rupture is a rare condition. Radiotherapy treatment for malignancy of a pelvic organ such as cervix or prostate is one cause of this condition. We report a case of a 71-year-old woman who presented with this illness 30 years after radiotherapy treatment.
Keywords: Deceiving, Encounter, Spontaneously, Ruptured, Urinary bladder
Introduction
Spontaneous urinary bladder rupture is a rare condition. Radiotherapy treatment for malignancy of a pelvic organ such as cervix or prostate is one cause of this condition. We report a case of a 71-year-old woman who presented with this illness 30 years after radiotherapy treatment.
Case history
A 71-year-old woman with a history of cervical cancer who underwent radiotherapy 30 years previously, presented with generalised abdominal pain of 1 day’s duration, associated with nausea. She denied fever, haematuria or dysuria. On examination, her vital signs were stable and her temperature was normal. Her abdomen was soft, but tender over the right iliac fossa and suprapubic region with a vague mass palpable over the suprapubic region. White blood cell count was 19 × 109/L. Her renal profile was normal. We proceeded with a computed tomography (CT) scan which showed a collection at the paracolic gutter (Figure 1). At this time it was thought to be a simple case of perforated appendix and we therefore proceeded with laparotomy. Intraoperatively, upon entering the peritoneum, 1L of clear yellowish fluid resembling urine was drained. No bowel perforation seen and the appendix was normal. However, there was perforation of the dome of the urinary bladder, with unhealthy edges and fibrotic wall. Bladder mucosa was very pale. No bladder tumour was palpable. The unhealthy edges were debrided. A Foley’s catheter was inserted under direct vision and primary repair of bladder perforation was done with Vicryl 3/0 sutures. The patient had a speedy recovery and a cystogram was performed at follow-up 1 month after surgery. No contrast leakage was seen. The Foley’s catheter was removed and the patient continued her follow-up. She denied dysuria and incontinence during further appointment. Histo-pathological examination of the edges of the bladder perforation showed inflamed granulation tissue and no malignant cells (Figures 2 and 3).
Figure 1 .
Edge of the perforation site showing an area of haemorrhage and granulation tissue (magnification ×20)
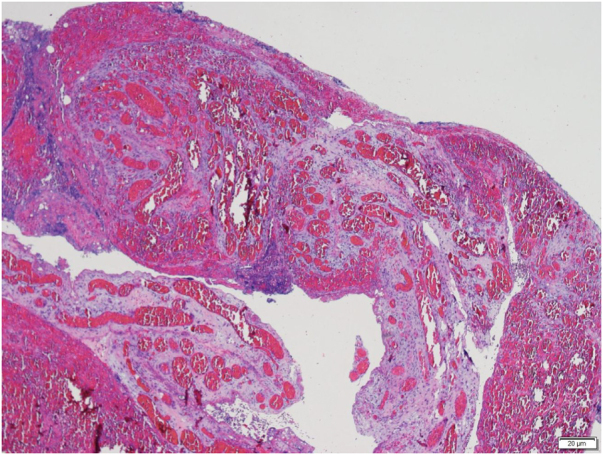
Figure 2 .

Edge of perforation showing reactive fibroblasts, lymphocytes, plasma cells and neutrophils (magnification ×40)
Figure 3 .

Contrasted CT of abdomen and pelvis showed collection of fluid at right paracolic gutter and subhepatic region. No obvious urinary bladder defect can be seen.
Discussion
Spontaneous bladder rupture was first reported in 1966 by Altman and Horsburgh as a case report.1 Since then, similar events have been reported very rarely, and even more rarely are caused by radiotherapy. To date, spontaneous bladder rupture remains elusive and mysterious in both its presentation and exact cause.
Several aetiologies had been reported to cause spontaneous perforation: tuberculosis, schistosomiasis, bladder diverticulum, intravesical obstruction and bladder carcinoma.2 Spontaneous bladder perforation post radiotherapy is an extremely rare complication and to the best of our knowledge, no study has addressed its incidence.2 The rate of side effects following curative radiotherapy for primary carcinoma is reported to be about 10% and 3% of side effects are urologic complications (haematuria, fistula formation, cystitis, fibrosis). The rate of side effects is related to dose and fractionation delivered and the volume of tissue irradiated.3
Spontaneous bladder rupture has been reported even 30 years after radiotherapy treatment.2 Radiation injury affecting division delay, reproductive failure and interphase arrest, which lead to cellular death and further bladder damage, are thought be the cause.4 Delay in diagnosis can lead to a mortality rate as high as 25% if more than 24 hours.2
Laboratory findings of changes in urea and creatinine are due to reabsorption of both through the peritoneum. However, it is hard to distinguish this from other causes such as acute renal failure.3 Cystography had been shown to be more sensitive and accurate than CT and ultrasonography as a diagnostic method.3 From our literature review, the majority of reported cases were managed surgically.
A case reported by Basiri and Radfar in which the patient did not have signs of peritonism was managed conservatively with Foley catheter insertion.5 Addar et al6 described six principles in the operative management of spontaneous bladder rupture: (1) identify and confirm the defect; (2) thoroughly lavage the peritoneal cavity to minimise any irritant or contamination; (3) excise the defect widely to remove any aetiologies such as infection, neoplasia or reduced vascular supply; (4) reconstitute intact bladder using tissue with an intact blood supply; (5) prolong bladder drainage and prophylaxis antibiotics to support tissue healing; and (6) exclude recurrence due to previous malignancy or primary tumour from the bladder.
Intraperitoneal rupture of urinary bladder classically presents with abdominal pain of sudden onset and impaired micturition. The patient can present with diaphragmatic irrtation.7 Physical examination would divulge signs of peritonitis or might still present with minimal findings.8 Finding urine upon insertion of a urinary catheter does not rule out the possibility of bladder rupture.9
The most common region for intraperitoneal rupture is the dome or the posterior wall of the bladder. This is because these are the weakest parts of the bladder and are where the bladder would lacerate with an increase in intravesical pressure. It is the intraperitoneal part of the bladder that becomes distended.10
A delay in diagnosis of more than 24 hours will result in a mortality rate as high as 25%. Nevertheless, the mortality rate can be lessened by appropriate diagnosis and prompt surgical management.9
Conclusion
Spontaneous urinary bladder rupture post radiotherapy is not an uncommon complication and should be one of the differential diagnosis in a patient who presents with acute abdomen. The crucial key to prompt an accurate diagnosis of bladder rupture is to suspect this disorder in patients with a previous history of pelvic radiation therapy who present with peritonism and features of acute renal derangement or failure.
References
- 1.Altman B, Horsburgh AG. Spontaneous rupture of the bladder. Br J Urol 1966; 38: 85–88. 10.1111/j.1464-410X.1966.tb09681.x [DOI] [PubMed] [Google Scholar]
- 2.Ketata S, Boulaire JL, Al-Ahdab Net al. Spontaneous intraperitoneal perforation of the bladder: a late complication of radiation therapy for prostate cancer. Clin Genitourin Cancer 2007; 5: 287–290. 10.3816/CGC.2007.n.006 [DOI] [PubMed] [Google Scholar]
- 3.Labanaris AP, Zugor V, Nützel R, Kühn R. Spontaneous rupture of the urinary bladder 10 years after curative radiotherapy. Scientific World Journal 2008; 8: 405–408. 10.1100/tsw.2008.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liberman D, Mehus B, Elliott SP. Urinary adverse effects of pelvic radiotherapy. Transl Androl Urol 2014; 3: 186. 10.3978/j.issn.2223-4683.2014.04.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basiri A, Radfar MH. Conservative management of early bladder rupture after postoperative radiotherapy for prostate cancer. Urol J 2008; 5: 269–271. [PubMed] [Google Scholar]
- 6.Addar MH, Stuart GC, Nation JG, Shumsky AG. Spontaneous rupture of the urinary bladder: a late complication of radiotherapy–case report and review of the literature. Gynecol Oncol 1996; 62: 314. 10.1006/gyno.1996.0234 [DOI] [PubMed] [Google Scholar]
- 7.Gregory AM, Christopher MD, McAninch JW. Substance abuse-related spontaneous bladder rupture: report of 2 cases and review of literature. J Urol 1991; 145: 135–137. 10.1016/S0022-5347(17)38269-1 [DOI] [PubMed] [Google Scholar]
- 8.Schraut WH, Huffman J, Bagley DH. Acute abdominal pain caused by spontaneous perforation of the urinary bladder. Surg Gynecol Obstet 1983; 156: 589–592. [PubMed] [Google Scholar]
- 9.Shaked A, Merrtyk S, Pode Det al. Non traumatic spontaneous rupture of the urinary bladder. Can J Surg 1986; 29: 107–109. [PubMed] [Google Scholar]
- 10.Wan YL, Yu TZ, Lee TY, Tsai CC. Spontaneous intraperitoneal rupture of bladder with spontaneous healing. Clin Imaging 1992; 16: 247–249. 10.1016/0899-7071(92)90006-U [DOI] [PubMed] [Google Scholar]


