Abstract
Secondary primary malignancies within the head and neck region are well documented. Within this group, synchronous tumours with an index oral cancer are usually found in the oropharyngeal or laryngeal sites. We present a rare case of an index squamous cell carcinoma in the tongue with a synchronous primary intraosseous squamous cell carcinoma. We discuss the challenges associated with investigation, diagnosis and subsequent management. Treatment aims remain the same; namely, eradicating the disease using surgery, radiotherapy, chemotherapy or a combination of these modalities. It is important to acknowledge the unpredictable pattern of tumour presentation and the need to maintain a high index of suspicion.
Keywords: Synchronous, Neoplasms, Multiple primary malignancy
Introduction
Second primary malignancies (SPMs) within the head and neck region have been reported previously.1 Specific criteria must be met to classify these tumours as SPMs, which can be further categorised as synchronous or metachronous, dependent on chronology of diagnoses (synchronous tumours present within 6 months of first diagnosis, whereas metachronous tumours present after 6 months). Within the head and neck, when the index (first) tumour is in the oral cavity, the typical sites of mucosal SPMs are the oropharynx or larynx.2 We present a rare case of an index squamous cell carcinoma (SCC) in the tongue with a synchronous primary intraosseous SCC with a completely intact overlying mucosa in the contralateral mandible and discuss the associated challenges in managing this presentation.
Case history
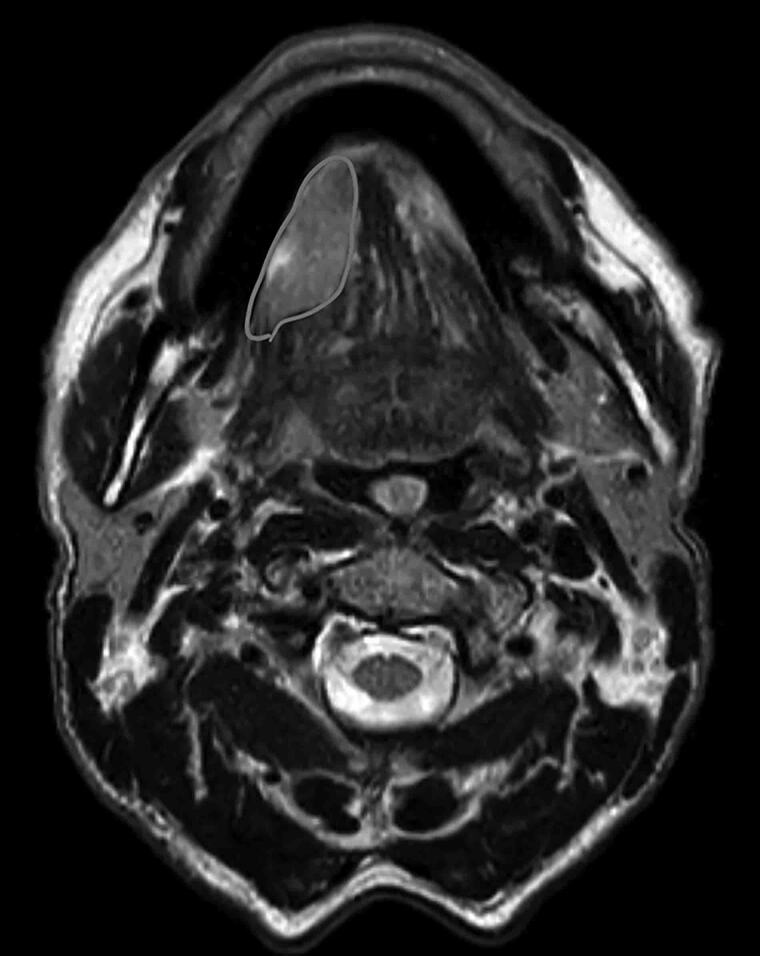
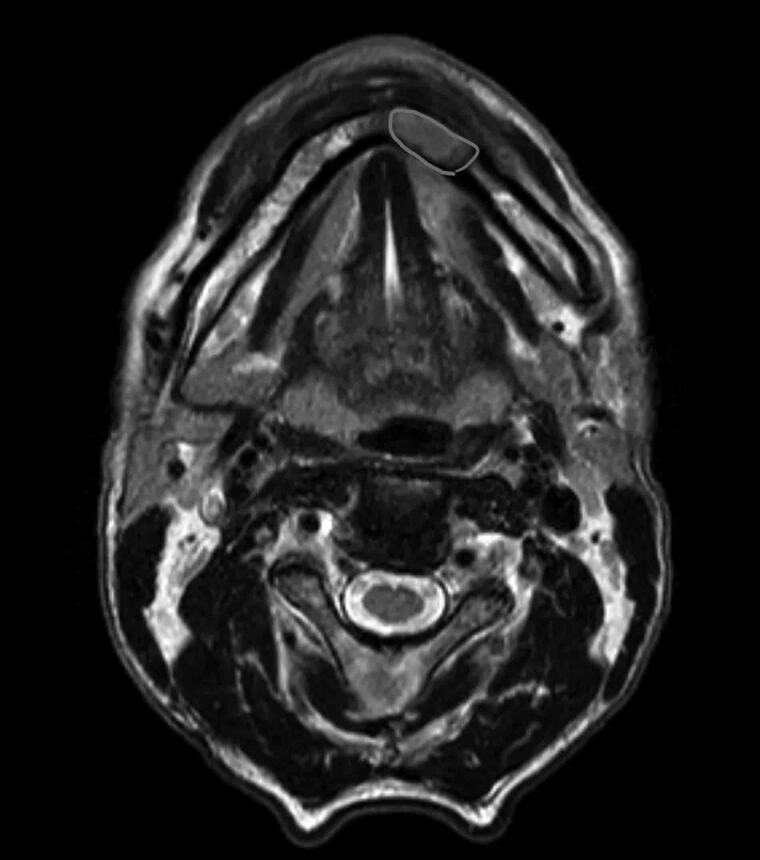
A 55-year-old white man, with a medical history of hypertension and alcoholic liver disease alongside a positive history of smoking and alcohol consumption, was referred regarding a non-healing ulcer in his right tongue of 4 weeks’ duration. Clinical examination revealed an isolated indurated ulcer on the right lateral border of the tongue extending onto the floor of mouth, which was confirmed histologically as a moderately differentiated SCC. Contrast-enhanced magnetic resonance imaging (MRI) and computed tomography (CT) scan of the neck revealed a lesion in the right tongue measuring 10×21×17mm3 with no genioglossus or mandibular cortical involvement (Figure 1). In addition, imaging revealed a second lesion in the left anterior mandible, measuring 15×8×14mm3, with no breach in the lingual cortex, and not in continuity with the tongue lesion (Figure 2). Clinical examination did not reveal any mucosal abnormality of the left anterior mandible or the adjacent vestibule. Positron emission tomography (PET) scanning was carried out and excluded a distant source of metastatic spread but demonstrated this intraosseous area to have high fluorodeoxyglucose avidity, and a subsequent incisional biopsy confirmed moderately-to-poorly differentiated SCC. The two lesions were staged as pT3N0M0 right tongue moderately-to-poorly differentiated SCC, and pT4aN0M0 left anterior mandible poorly differentiated SCC. This patient underwent tracheostomy, bilateral selective neck dissection (levels I–IV), anterior segmental mandibulectomy, subtotal glossectomy and reconstruction with a composite fibular free flap.
Figure 1 .
MRI scan showing right tongue tumour
Figure 2 .
MRI scan showing left mandibular tumour
Discussion
SPMs were first described more than a century ago, which led to description of the following criteria to classify this disease, that is the tumours must: (1) individually represent a picture of malignancy, (2) be anatomically distinct and (3) have been excluded as being metastases of each other based on their small size and timeline of diagnosis.3 The risk of developing a SPM with an index head and neck cancer is as high as 36% over 20 years.1 For an index oral cavity cancer, the incidence of developing a synchronous oral cavity SPM has been reported as 3.3%.4
Synchronous and metachronous tumours can arise due to ‘field cancerisation’, as first proposed by Slaughter et al,5 who observed the presence of histologically abnormal cells surrounding established oral carcinomas and proposed that exposure to carcinogens (such as in tobacco products) induced an anaplastic tendency in cells in the field, which then led to independent malignancies arising at different rates within the oral cavity.6
Although synchronous oral cavity SCCs, where the lesions are mucosal in origin, have been reported previously,7 our case is interesting because the second primary lesion arose as a non-contiguous intraosseous lesion. This is particularly unusual, given that primary intraosseous SCC is itself a rare tumour, with a reported incidence of only 1.45%.8
In this case, the intraosseous primary lesion was not readily detectable on clinical examination because the overlying mucosa was completely unremarkable. The lesion was only demonstrated on staging CT and MRI scans, supplemented thereafter with an orthopantogram (Figure 3) alongside a raised suspicion due to uptake on the PET–CT which necessitated histological evaluation of the mandibular lesion. The lesions in this case were of different origins (mucosal and intraosseous), differed in their anatomic subsites and laterality. Critically, they were excluded as metastatic deposits of each other based on size, location, histology, timing of presentation and the onset of lesions being within 6 months of each other, which classifies them as synchronous primary oral cavity malignancies. To the best of the authors' knowledge, this combination of synchronous mucosal and intraosseous SCCs has not been reported previously in the literature. The occult nature of the mandibular tumour was a particular diagnostic challenge, highlighting the potential pitfalls in management of multiple primary malignancies.
Figure 3 .
Orthopantogram taken following staging scans showing indeterminate radiolucency in the left anterior mandible
Given this unpredictable pattern in presentation, clinicians must always be cautious and cognisant of the possibility of an otherwise unseen or occult lesion, and ensure appropriate work-up, staging and prognostication of head and neck carcinoma. In the absence of distant metastases, and in patients deemed fit for surgery, the preferred treatment aims remain the same for solitary or multiple primary lesions, namely ablation of the primary lesions and management of potential or confirmed cervical nodal disease, by primary surgery and adjuvant (chemo)radiotherapy according to disease stage.
Reconstruction in such cases of SPMs can prove challenging if the lesions are far apart (possibly necessitating two free flaps); however, in our case a single composite free flap was sufficient due to the proximity of the lesions. In our patient, postoperative radiotherapy was recommended due to aggressive histological features.
Conclusion
The diagnosis and management of synchronous primary tumours of the oral cavity can be a challenge, as demonstrated in this case, in which the second intraosseous lesion could not have been identified at initial examination due to the normal overlying mucosa. Indeed, the second primary lesion was only demonstrated on three-dimensional staging scans which necessitated further targeted investigations. Management of these lesions can prove challenging, particularly with respect to the reconstruction. To the best of the authors' knowledge, there are no other reported instances of a primary intraosseous SCC presenting as a synchronous tumour. This case highlights the diagnostic benefit of PET–CT imaging in selected instances of staging head and neck cancer.
References
- 1.Chuang S-C, Scelo G, Tonita JMet al. Risk of second primary cancer among patients with head and neck cancers: A pooled analysis of 13 cancer registries. Int J Cancer 2008; 123: 2390–2396. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz LH, Ozsahin M, Zhang GNet al. Synchronous and metachronous head and neck carcinomas. Cancer 1994; 74: 1933–1938. [DOI] [PubMed] [Google Scholar]
- 3.Warren S GO. Multiple primary malignant tumors: A survey of the literature and statistical study. Am J Cancer 1932; 16: 358–414. [Google Scholar]
- 4.Kao H-K, Abdelrahman M, Huang Yet al. Multiple concomitant oral cavity cancers: incidence, management, and outcomes. J Surg Oncol 2017; 115: 835–841. [DOI] [PubMed] [Google Scholar]
- 5.Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 1953; 6: 963–968. [DOI] [PubMed] [Google Scholar]
- 6.Mohan M, Jagannathan N. Oral field cancerization: an update on current concepts. Oncol Rev 2014; 8: 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mochizuki Y, Harada H, Ikuta Met al. Clinical characteristics of multiple primary carcinomas of the oral cavity. Oral Oncol 2015; 51: 182–189. [DOI] [PubMed] [Google Scholar]
- 8.Naruse T, Yanamoto S, Sakamoto Yet al. Clinicopathological study of primary intraosseous squamous cell carcinoma of the Jaw and a review of the literature. J Oral Maxillofac Surg 2016; 74: 2420–2427. [DOI] [PubMed] [Google Scholar]