Abstract
Introduction
The COVID-19 pandemic has increased the risks of surgery and management of common surgical conditions has changed, with greater reliance on imaging and conservative management. The negative appendectomy rate (NAR) in the UK has previously remained high. The aim of this study was to quantify pandemic-related changes in the management of patients with suspected appendicitis, including the NAR.
Methods
A retrospective study was performed at a single high volume centre of consecutive patients aged over five years presenting to general surgery with right iliac fossa pain in two study periods: for two months before lockdown and for four months after lockdown. Pregnant patients and those with previous appendectomy, including right colonic resection, were excluded. Demographic, clinical, imaging and histological data were captured, and risk scores were calculated, stratifying patients into higher and lower risk groups. Data were analysed by age, sex and risk subgroups.
Results
The mean number of daily referrals with right iliac fossa pain or suspected appendicitis reduced significantly between the study periods, from 2.92 before lockdown to 2.07 after lockdown (p<0.001). Preoperative computed tomography (CT) rates increased significantly from 22.9% to 37.2% (p=0.002). The NAR did not change significantly between study periods (25.5% prior to lockdown, 11.1% following lockdown, p=0.159). Twelve (75%) out of sixteen negative appendectomies were observed in higher risk patients aged 16–45 years who did not undergo preoperative CT. The NAR in patients undergoing CT was 0%.
Conclusions
Greater use of preoperative CT should be considered in risk stratified patients in order to reduce the NAR.
Keywords: Appendicitis, Appendectomy, Clinical Decision-Making, Diagnosis, Tomography, X-Ray
Acute appendicitis is a common surgical condition that is the most frequent indication for emergency abdominal surgery worldwide.1 Cases vary in severity from mild localised inflammation seen only on histology to gangrene or perforation with severe peritonitis.2 Overall mortality is observed in approximately 3 in 1,000 patients.3
Laparoscopic appendectomy is often recommended and has become the gold standard treatment.4 However, clinical diagnosis of appendicitis remains challenging, reflected in the persistently high negative appendectomy rate (NAR), the proportion of appendectomy specimens which are histologically normal, in the UK.5,6 Appendectomy of a histologically normal appendix carries similar risks to removing an inflamed appendix if local complications are absent7,8 but for limited benefit. Performing many such procedures has implications towards healthcare resource. In the UK, the cost of investigating and treating appendicitis was recently estimated to be greater than £2,000 per patient, with operative time being the most significant factor in costs.9 COVID-19 is an acute multisystem disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).10 The COVID-19 pandemic has caused problems for surgeons both by perioperative infection being associated with increased mortality and respiratory complications,11 and by extensive disruption to surgical services.12 These factors have made the adverse consequences of removal of histologically normal appendices only more significant.
In March 2020, the UK surgical royal colleges and specialty organisations issued guidance applying to emergency surgery during the pandemic,13 advising that patients with appendicitis should be managed conservatively where possible. It was recommended that patients requiring surgery should have preoperative SARS-CoV-2 testing and an open procedure (owing to perceived risks of aerosol generation with a laparoscopic approach). Extending planned abdominopelvic computed tomography (CT) up to the tracheal carina superiorly was also recommended to identify patients with interstitial pneumonitis suggestive of COVID-19.
In practice, our centre adopted a lower threshold for performing CT, intended to aid in the diagnosis of both surgical pathology and COVID-19. The COVID-19 pandemic has also changed patients’ threshold to accessing healthcare, with patients avoiding going to hospital or other healthcare settings from March to late June 2020.14 We hypothesised that these changes in patient behaviour and clinical management had an impact on the number of patients being referred with right iliac fossa pain, their management and outcomes, including the NAR.
Methods
A retrospective cohort study was carried out of consecutive patients presenting to general surgery from any source with right iliac fossa pain or suspected appendicitis in a single high volume surgical admissions unit. Patients aged over five years old were identified from electronically stored general surgery take lists between 26 January and 25 July 2020. Patients who had previously had a right hemicolectomy, ileocolic resection or appendectomy were excluded, as were patients who were pregnant at the time of presentation.
Data capture
Data on patient demographics, dates and times of admission, imaging, operation and discharge were captured. Sufficient clinical and biochemical data were recorded to allow calculation of the risk scores recommended by the RIFT (Right Iliac Fossa Treatment) study.5 Diagnoses from imaging, direct visualisation at operation and clinical factors were recorded, as was histology from all excised appendices. Data on polymerase chain reaction (PCR) based nasopharyngeal swab test results for SARS-CoV-2 were also captured. Patients were followed up for 30 days to identify any readmissions or complications using routinely collected data available on hospital systems.
Study registration
This study was registered as an audit (audit number 5329) and was subject to local approvals.
Analysis
Data were analysed in two study periods, intended to capture the changes in patient behaviour and clinical practice during the initial wave of the COVID-19 pandemic. The first period was from 26 January 2020 to 25 March 2020 while the second period was from 26 March 2020 (coinciding with the introduction of UK lockdown regulations)15 to 25 July 2020. Data analysis was also pre-planned to stratify patients by age (5–16 years, 16–45 years and >45 years) and sex.
Lower risk and higher risk groups were identified by calculating risk scores from the available data. For the purposes of analysis, missing data points were considered to represent the absence of a symptom or sign, or a laboratory value not meeting the threshold required to score. The scores and cut-off values were in accordance with those recommended by the RIFT study:5,16 children aged 5–16 years underwent Shera scoring17 while patients aged 16–45 years underwent appendicitis inflammatory response scoring18 or adult appendicitis scoring19 for men and women respectively. The RIFT study did not examine risk scoring in patients aged >45 years.
Statistical analysis was performed with R statistical software version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org). The Poisson test was employed to compare rates of referral between the study periods. Two-tailed Fisher’s exact tests were used to compare demographic variables, imaging rates and NARs between groups. The level of significance was set at 0.05.
Results
Table 1 summarises the demographics of the patients referred with right iliac fossa pain or suspected appendicitis in each study period. A total of 428 patients were included overall: 175 patients over the 60 days before lockdown and 253 patients over the 122 days after lockdown. The ratio of male to female patients was approximately 1:2 in each period. There were no significant differences in the proportion of referrals from risk stratified age and sex subgroups between study periods. The mean daily rate of referrals reduced significantly from 2.92 before lockdown to 2.07 after lockdown (p<0.001).
Table 1 .
Demographics and risk categories of patients
| Referrals | Risk category | Before lockdown | After lockdown | p-value | ||
|---|---|---|---|---|---|---|
| n | Daily mean | n | Daily mean | |||
| Total | 175 | 2.92 | 253 | 2.07 | <0.001 | |
| Male | 67 (38.3%) | 1.12 | 90 (35.6%) | 0.74 | 0.610 | |
| 5–16 years | Low risk | 3 (1.7%) | 0.05 | 6 (2.4%) | 0.05 | 0.743 |
| High risk | 15 (8.6%) | 0.25 | 14 (5.5%) | 0.11 | 0.244 | |
| 16–45 years | Low risk | 2 (1.1%) | 0.03 | 9 (3.6%) | 0.07 | 0.212 |
| High risk | 33 (18.9%) | 0.55 | 41 (16.2%) | 0.34 | 0.517 | |
| >45 years | N/A | 14 (8.0%) | 0.23 | 20 (7.9%) | 0.16 | 1.000 |
| Female | 108 (61.7%) | 1.80 | 163 (64.4%) | 1.34 | 0.610 | |
| 5–16 years | Low risk | 11 (6.3%) | 0.18 | 9 (3.6%) | 0.07 | 0.244 |
| High risk | 15 (8.6%) | 0.25 | 26 (10.3%) | 0.21 | 0.619 | |
| 16–45 years | Low risk | 33 (18.9%) | 0.55 | 51 (20.2%) | 0.42 | 0.805 |
| High risk | 33 (18.9%) | 0.55 | 48 (19.0%) | 0.39 | 1.000 | |
| >45 years | N/A | 16 (9.1%) | 0.27 | 29 (11.5%) | 0.24 | 0.522 |
Imaging
Data on CT rates are shown in Table 2. A total of 134 (31.3%) out of 428 patients overall underwent CT. This included 40 (22.9%) out of 175 prior to lockdown and 94 (37.2%) out of 253 following lockdown, a significant increase (p=0.002). Furthermore, this increase was significant in both male (p=0.021) and female patients (p=0.003), and was driven by increased CT imaging of high risk adults aged 16–45 years (p=0.009 and p=0.018 for male and female patients respectively), with other subgroups showing no significant change. The use of CT was positively correlated with increasing age, with greater proportions of patients undergoing imaging in older age categories both before and after lockdown.
Table 2 .
Use of computed tomography (CT) in each study period, stratified by demographic and risk category
| CT scans performed | Risk category | Before lockdown | After lockdown | p-value |
|---|---|---|---|---|
| Total | 40 (22.9%) | 94 (37.2%) | 0.002 | |
| Male | 20 (29.9%) | 44 (48.9%) | 0.021 | |
| 5–16 years | Low risk | 0 (0%) | 0 (0%) | 1.000 |
| High risk | 2 (13.3%) | 0 (0%) | 0.483 | |
| 16–45 years | Low risk | 0 (0%) | 4 (44.4%) | 0.491 |
| High risk | 8 (24.2%) | 23 (56.1%) | 0.009 | |
| >45 years | N/A | 10 (71.4%) | 17 (85.0%) | 0.410 |
| Female | 20 (18.5%) | 50 (30.7%) | 0.033 | |
| 5–16 years | Low risk | 0 (0%) | 0 (0%) | 1.000 |
| High risk | 1 (6.7%) | 2 (7.7%) | 1.000 | |
| 16–45 years | Low risk | 5 (15.2%) | 8 (15.7%) | 1.000 |
| High risk | 6 (18.2%) | 21 (43.8%) | 0.018 | |
| >45 years | N/A | 8 (50.0%) | 19 (65.5%) | 0.354 |
Appendectomy and NAR
Fifty-nine patients underwent an operation for suspected appendicitis prior to lockdown. Of these, 47 (79.7%) had an appendectomy, with the remaining 12 patients (20.3%) having diagnostic laparoscopy without appendectomy. The median length of stay (LOS) was 47 hours and 57 hours for the former and latter groups respectively. Five patients were managed conservatively with a median LOS of 23 hours.
After lockdown, 36 patients underwent an operation for suspected appendicitis. All of these had an appendectomy. The median LOS was 53 hours. Forty-eight patients were managed conservatively with a median LOS of 13 hours.
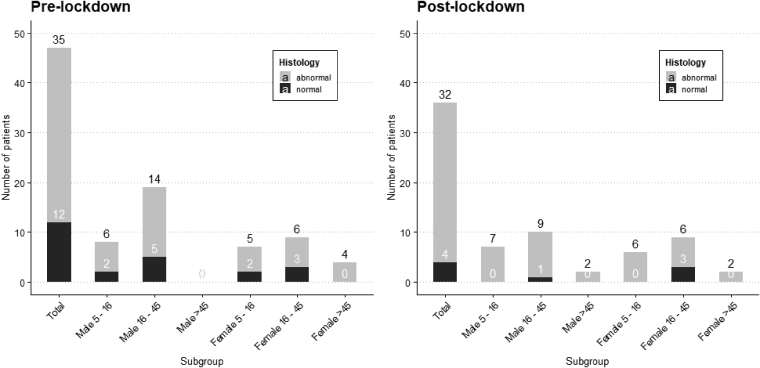
Figure 1 shows the number of appendectomies and histology for each study period. Of the 47 appendectomies performed prior to lockdown, 12 (25.5%) were histologically normal. Of the 36 appendectomies following lockdown, 4 (11.1%) were histologically normal. This difference in NAR did not reach significance (p=0.159).
Figure 1 .
Appendix histology in each study period broken down by sex and age
NAR by risk score and imaging status
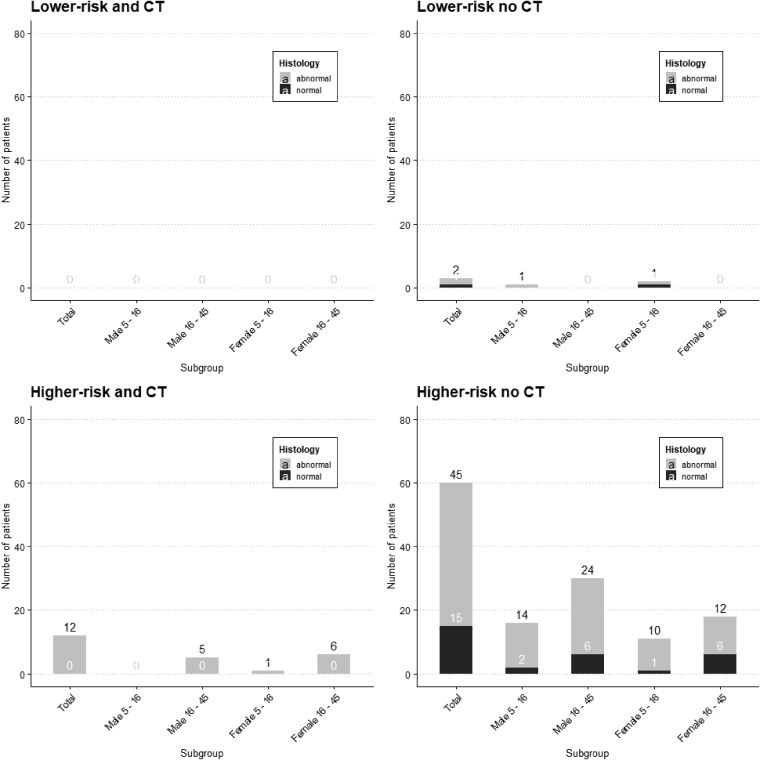
Figure 2 shows the number of appendectomies and histology across both study periods stratified by risk score and CT status. Data from patients aged >45 years are not displayed as the RIFT study did not recommend risk scoring this age group and the NAR in this group was 0% (Figure 1). There were no lower risk patients who underwent CT and were subsequently operated on. Three lower risk patients proceeded to an operation without preoperative CT, with one specimen showing normal histology. Twelve higher risk patients imaged by CT underwent appendectomy, all with abnormal histology. Sixty higher risk patients who were not imaged preoperatively by CT underwent appendectomy, with fifteen specimens showing normal histology (a NAR of 25%). Twelve (75%) out of sixteen negative appendectomies occurred in higher risk, young adult patients who did not have preoperative CT.
Figure 2 .
Appendix histology for risk score and computed tomography (CT) status across both study periods broken down by sex and age
SARS-CoV-2
Three patients (1.7%) underwent swab testing for SARS-CoV-2 before lockdown. All of these had a negative result. In the follow-up period, one patient (0.6%) was readmitted to the medical team with symptomatic COVID-19.
After lockdown, 199 patients (78.7%) underwent swab testing, with 2 found to be positive for SARS-CoV-2. Both patients had undergone CT confirming a diagnosis of acute appendicitis; one was managed conservatively and one was managed by an open operation. In the follow-up period, there were no readmissions for symptomatic COVID-19.
Discussion
Negative appendectomies
The negative appendectomies predominantly occurred in higher risk, young adult patients who did not undergo preoperative CT. No patient undergoing CT subsequently had a negative appendectomy. The NAR in our centre compares less favourably with the NAR found in similar studies5,16,20 and with reported outcomes during the COVID-19 pandemic.21 Targetting preoperative CT to higher risk, young adult patients may represent a promising method to reduce the risks of unnecessary operations in this group.
Imaging in suspected appendicitis
The purpose of imaging patients with suspected appendicitis is to provide a timely, accurate diagnosis where it remains in doubt. In order to use imaging to reduce the NAR, it is especially important that the chosen modality is sufficiently sensitive to provide a low negative predictive value in patients with a high pre-test probability of appendicitis (ie in higher risk patients being considered for surgery).
Both CT22 and magnetic resonance imaging (MRI)23 meet these requirements, allowing many patients with a negative test to be safely observed or discharged. However, MRI is a costly and limited resource, and it is not readily accessible out of hours in our centre. Ultrasonography performs poorly in diagnosing appendicitis and has an unacceptably high negative predictive value in higher risk patients,24 preventing its use in avoiding unnecessary laparoscopy. It is also associated with a high proportion of indeterminate results,25 further limiting its utility.
The use of CT in the management of suspected appendicitis is associated with an increased risk of haematological malignancies, especially in paediatric patients.26 Low dose CT is as effective as standard CT in investigating suspected appendicitis and the use of low dose protocols would be likely to partially mitigate these risks.27 Furthermore, intravenous administration of contrast media carries risks of anaphylaxis, nephropathy and extravasation injury but these risks may be difficult to avoid as the use of contrast provides greater accuracy in CT assessment of suspected appendicitis.22
A blanket policy to perform CT in all patients presenting with right iliac fossa pain or suspected appendicitis (regardless of the likelihood of appendicitis) may expose many patients to these risks without sufficient justification. Where the radiology department is busy, as in our centre, it may also not be possible to perform the many additional CT scans required by a blanket policy. The use of risk scoring to stratify adult patients prior to CT may provide the correct balance of mitigating the risk of negative appendectomy while avoiding exposing patients unnecessarily to risks including radiation and using limited resources in an effective manner.
Study limitations
This study was retrospective in design and the reduction in NAR observed with the use of preoperative CT may therefore not have been because of the use of imaging. It is possible that the patients who did not undergo CT may have been less likely to have appendicitis than those imaged. Nevertheless, if this were the case, then the question of whether this group should undergo diagnostic laparoscopy or imaging remains. We believe that the pressures of the COVID-19 pandemic mean that this question should be settled in favour of the latter.
The cohort was taken from consecutive patients referred to surgery in a single district general hospital in the UK. Although the results may be generalisable to similar settings, they should be interpreted with caution in other settings where patient populations and investigation pathways for suspected appendicitis may differ.
The effect of an incomplete dataset on the calculation of risk scores means that for some patients, the risk score may have been underestimated. However, even with this limitation, the risk scores seemed to perform well, with only 2 out of over 100 low risk patients across both periods having histology proven appendicitis.
It is possible that grouping patients by risk category and imaging across both study periods may have obscured relevant differences in the patients referred with suspected appendicitis before and after lockdown. The fact that the proportions of patients in each risk category were unchanged between the study periods suggests that any effect on the data would likely be minor.
From our data, the precise times of performing swab testing for SARS-CoV-2 and receiving the result are unknown. It is therefore not possible to comment on when the patients who tested positive were likely to have acquired the infection (ie whether this was before presenting to hospital or during their admission). Many patients who acquired COVID-19 in the follow-up period will have been missed as it was only possible to capture those who re-presented to our hospital trust. Those patients who underwent testing in the community and subsequently self-isolated will have not been identified.
Conclusions
The negative appendectomies predominantly occurred in higher risk, young adult patients who had not undergone preoperative CT. Greater use of CT in this group should be considered given the increased risks of surgery during the COVID-19 pandemic in order to reduce the NAR.
References
- 1.GlobalSurg Collaborative . Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg 2016; 103: 971–988. [DOI] [PubMed] [Google Scholar]
- 2.Bhangu A, Søreide K, Di Saverio Set al. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 2015; 386: 1278–1287. [DOI] [PubMed] [Google Scholar]
- 3.Gomes CA, Abu-Zidan FM, Sartelli Met al. Management of Appendicitis Globally based on Income of Countries (MAGIC) study. World J Surg 2018; 42: 3903–3910. [DOI] [PubMed] [Google Scholar]
- 4.Di Saverio S, Birindelli A, Kelly MDet al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 2016; 11: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhangu A. Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg 2020; 107: 73–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Surgical Research Collaborative. Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg 2013; 100: 1240–1252. [DOI] [PubMed] [Google Scholar]
- 7.Allaway MG, Eslick GD, Cox MR. The unacceptable morbidity of negative laparoscopic appendicectomy. World J Surg 2019; 43: 405–414. [DOI] [PubMed] [Google Scholar]
- 8.Lee M, Paavana T, Mazari F, Wilson TR. The morbidity of negative appendicectomy. Ann R Coll Surg Engl 2014; 96: 517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clement KD, Emslie K, Maniam P, Wilson MS. What is the operative cost of managing acute appendicitis in the NHS: the impact of stump technique and perioperative imaging. World J Surg 2020; 44: 749–754. [DOI] [PubMed] [Google Scholar]
- 10.Shi Y, Wang G, Cai XPet al. An overview of COVID-19. J Zhejiang Univ Sci B 2020; 21: 343–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Søreide K, Hallet J, Matthews JBet al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg 2020; 107: 1250–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Royal College of Surgeons of England. COVID-19. https://www.rcseng.ac.uk/coronavirus/ (cited June; 2021). [Google Scholar]
- 14.Imperial College Health Partners. Covid-19 behaviour tracker. http://www.coviddatahub.com (cited June 2021).
- 15.The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020. https://www.legislation.gov.uk/uksi/2020/350/contents/made (cited June 2021).
- 16.Nepogodiev D, Wilkin RJ, Bradshaw CJet al. Appendicitis risk prediction models in children presenting with right iliac fossa pain (RIFT study): a prospective, multicentre validation study. Lancet Child Adolesc Health 2020; 4: 271–280. [DOI] [PubMed] [Google Scholar]
- 17.Shera AH, Nizami FA, Malik AAet al. Clinical scoring system for diagnosis of acute appendicitis in children. Indian J Pediatr 2011; 78: 287–290. [DOI] [PubMed] [Google Scholar]
- 18.Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg 2008; 32: 1843–1849. [DOI] [PubMed] [Google Scholar]
- 19.Sammalkorpi HE, Mentula P, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis – a prospective study. BMC Gastroenterol 2014; 14: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sartelli M, Baiocchi GL, Di Saverio Set al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Surg 2018; 13: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Javanmard-Emamghissi H, Boyd-Carson H, Hollyman Met al. The management of adult appendicitis during the COVID-19 pandemic: an interim analysis of a UK cohort study. Tech Coloproctol 2021; 25: 401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rud B, Vejborg TS, Rappeport EDet al. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev 2019; 11: CD009977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duke E, Kalb B, Arif-Tiwari Het al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR Am J Roentgenol 2016; 206: 508–517. [DOI] [PubMed] [Google Scholar]
- 24.Giljaca V, Nadarevic T, Poropat Get al. Diagnostic accuracy of abdominal ultrasound for diagnosis of acute appendicitis: systematic review and meta-analysis. World J Surg 2017; 41: 693–700. [DOI] [PubMed] [Google Scholar]
- 25.Crocker C, Akl M, Abdolell Met al. Ultrasound and CT in the diagnosis of appendicitis: accuracy with consideration of indeterminate examinations according to STARD guidelines. AJR Am J Roentgenol 2020; 215: 639–644. [DOI] [PubMed] [Google Scholar]
- 26.Lee KH, Lee S, Park JHet al. Risk of hematologic malignant neoplasms from abdominopelvic computed tomographic radiation in patients who underwent appendectomy. JAMA Surg 2021; 156: 343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yun SJ, Ryu CW, Choi NYet al. Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol 2017; 208: W198–W207. [DOI] [PubMed] [Google Scholar]