Abstract
Purpose
Electric scooters (e-Scooters) are being increasingly used in urban areas as a new means of transport. E-scooter sharing schemes have recently been piloted in the United Kingdom; however, there are no published data on orthopaedic injuries and user behaviour patterns in the UK. We aim to identify the patterns and severity of orthopaedic injuries related to e-scooter use.
Methods
We performed a retrospective review of all orthopaedic referrals relating to e-scooter use from 1 March to 30 November 2020 at three hospitals, including one major trauma centre in central London. Data including patient demographics, mechanism of injury, diagnosis and treatment were collected.
Results
One hundred and five orthopaedic injuries were identified in 83 patients. The median age was 32 years and 83% were male. Seventy-nine (95.2%) patients were riders, four were pedestrians. All e-scooters were privately owned. There were 93 fractures (88.6% of total injuries noted) including 12 (12.9%) open. Fifty-two (56.0%) were upper limb fractures, 39 (41.9%) lower limb and 2 (2.1%) spinal and rib fractures. Twenty-five patients (30.1%) required an operation and 29 (34.9%) required hospital admission. Helmet use was present in 34.1%. The most common place of injury was the road (65.1%) followed by pavement (32.9%).
Conclusion
E-scooters can cause serious injury, most commonly in males. There was an equal distribution of upper and lower limb injuries, with many associated with high-energy trauma requiring operative intervention. Helmet use was seen in one third of riders. As e-scooter use continues to increase across the UK, additional steps should be taken to ensure the safety of the riders and public.
Keywords: Injury, Electric scooter, Fractures, Orthopaedic, Trauma, Scooter, United Kingdom
Introduction
There has been a world-wide increase in the use of electric scooters as micro-mobility devices. Since their introduction in 2017, large metropolitan cities in the US, Europe, New Zealand and Singapore have started using the electronic scooter to offer solutions to a wide range of transport policy goals.1–4 As the UK push for a ‘green’ restart to local travel in the time of COVID-19, e-scooters offer the potential for fast, clean and inexpensive travel that can also help ease the burden on transport networks and allow for social distancing.5
In the UK, privately owned e-scooters are currently illegal on public roads and pavements, with riders risking a £300 (US$400) fixed penalty notice if stopped by police. They can only be used legally on private land, and to purchase a privately owned e-scooter a driving licence is currently not required.6 On 4 July 2020, the Department of Transport announced the legalisation of e-scooters in England, Scotland and Wales if obtained through a government share scheme where independent firms are contracted to provide e-scooter models to be rented out. Similar scooter share schemes operate in over 100 cities in the world including Paris, Copenhagen and Brisbane.1–4 Under the government shared scheme, a rider must be 16 and above with a valid driver’s licence, mainly riding in the road or bicycle lane with a maximum speed limit set at 15.5mph.6 The use of a cycle helmet is recommended but not mandatory, and automatic vehicle lights should be used when possible. As the government share scheme is due to expand throughout London in the first quarter of 2021, it is possible that the legalisation of privately owned e-scooters may follow.7
With the increasing popularity of e-scooters, unfortunately, injuries are going to follow closely behind. World-wide data on musculoskeletal injury related to e-scooter use are relatively limited, owing to the short duration since their first introduction to the public. However recent studies carried out in the US, Singapore, Austria, Germany and New Zealand describe the growing problem.1–4,8,9 In the US, the population-adjusted incidence of electronic scooter-related injuries increased from 1.53 per 100,000 capita in 2014 to 9.22 per 100,000 capita in 2019 with head as the most common site of injury (27.1% of all injuries).3 Similarly, in New Zealand, they observed a significant increase of e-scooter-associated injuries, from two up to 35 injuries per week after the introduction of an urban e-scooter sharing system. They noted a significant increase in serious injuries, particularly to the extremities and to the axial skeleton.4 The current literature demonstrates that e-scooters can cause serious musculoskeletal injury and can be typically associated with high-energy trauma.9
At the time of writing, despite frequent reports in the British media of e-scooter-related incidents and tragically two fatalities, there are no valid figures on injury patterns available. With the advent of increasing the availability of e-scooters to the British public, there remains a paucity of published data on orthopaedic injury patterns from e-scooters in the UK. These data are essential to help estimate the injury burden associated with e-scooters and aid in identifying areas that could be targeted to improve user safety. We hypothesise that orthopaedic injuries associated with e-scooter use will mostly follow a high-energy injury pattern with low adherence to helmet or protective gear use. The aim of our study is to identify the patterns and severity of orthopaedic injuries related to the use of e-scooters in three urban hospitals in central London, the epicentre of the UK e-scooter phenomenon.7
Methods
We performed a retrospective review of all the operative cases that had been performed in the Department of Trauma and Orthopaedic Surgery and all the acute referrals from the Emergency Department, from 1 March 2020 to 30 November 2020 at two level two trauma centres (Chelsea and Westminster Hospital, Charing Cross Hospital) and one level one major trauma centre (St. Mary’s Hospital) in central London.
We identified all the operative cases and referrals in which the mechanism of injury was an incident involving an ‘electric’ or ‘motorised’ scooter, either as a rider or pedestrian. Electronic notes were reviewed by two authors (N.D.C and C.M.) to confirm that the injury was related to an e-scooter. Injuries from a non-motorised ‘pushbike’, ‘bicycles’ or ‘mopeds’ were excluded. Cases in which there was any discrepancy in mechanism of injury or the use of an e-scooter was unclear from the documentation were excluded.
Data that included injury pattern, time of presentation, mechanism, treatment, length of hospital stay and follow-up were collected. Demographic data included age, gender and American Society of Anaesthesiologists (ASA) score. The use of illicit substances, either drugs or alcohol (established through clinical assessment, blood alcohol level or positive urine toxicology), while sustaining the injury was also noted, alongside whether the rider was wearing a helmet or had lights on the e-scooter. Where applicable, operation notes and radiological imaging of the injury were reviewed.
Ethical approval was sought but not required by our institution owing to the retrospective nature of the study in accordance with our hospitals’ policies. Descriptive analyses were performed. Absolute numbers and percentages for variables were reported. Age and ASA were reported as medians with median absolute deviations.
Results
Over a 9-month period (March to November 2020), across the three hospitals, 83 patients were referred to Orthopaedics for e-scooter-related injuries, of which 25 (30.1%) required operative intervention. E-scooter referrals comprised 1.6% (83/5177) of all referrals to orthopaedics. Of the 83 patients, 79 (95.2%) were riders and 4 (4.8%) were all male non-rider pedestrians (three hit by an e-scooter and one tripped over a parked e-scooter). Patients were predominantly male (83.1%) with a median age of 32 years (age range 12–63). Fourteen patients were younger than 16 years of age (16.9%). Table 1 demonstrates the full patient demographics and injury characteristics.
Table 1 .
Patient and incident characteristics for orthopaedic referrals associated with e-scooters during a 9-month period
| Characteristic | No. (%) riders (n=79) |
No. (%) non-riders (n=4) |
Total (n=83) |
|---|---|---|---|
| Age* | 31 (10–57) | 40 (15–63) | 32 (12–63) |
| Male | 65 (82.3) | 4 (100) | 69 (83.1) |
| ASA | |||
| 1 | 71 | 3 | 74 |
| 2 | 8 | 1 | 9 |
| Mechanism of injury | |||
| Fall | 58 (73.4) | – | 58 (69.9) |
| Collision with a stationary object | 10 (12.6) | – | 10 (12.0) |
| Collision with vehicle or moving object | 11 (13.9) | – | 11 (13.3) |
| Hit by scooter | NA | 3 (75.0) | 3 (3.6) |
| Tripped over scooter | NA | 1 (25.0) | 1 (1.2) |
| Helmet use† | |||
| Helmet | 27 (34.1) | – | – |
| Drug or alcohol intoxication‡ | 6 (7.6) | 0 | 6 (7.2) |
| Use of lights or reflective clothing† | 13(16.5) | – | – |
| Estimated speed of e-scooter at time of injury (mph) | |||
| <15.5 | 44 (55.7) | 4 (100.0) | 48 (57.8) |
| >15.5 | 35 (44.3) | 0 | 35 (42.2) |
| Place of injury | |||
| Pavement | 26 (32.9) | 2 (50.0) | 28 (35.4) |
| Road | 53 (67.1) | 1 (25.0) | 54 (65.1) |
| Private residence | 0 | 1 (25.0) | 1 (1.2) |
| Destination from ED | |||
| Home | 51 (64.6) | 3 (75.0) | 54 (65.1) |
| Admitted to ward | 28 (35.4) | 1 (25.0) | 29 (34.9) |
| Intensive care unit | 0 | 0 | 0 |
| Mean length of stay (SD) | 4.9 days (6.27) | 4.9 days (6.27) | |
| Management | |||
| Operative | 25 (31.6) | 0 | 25 (30.1) |
| Non-operative | 54 (68.3) | 4 (100.0) | 58 (69.9) |
ASA, American Society of Anaesthesiologists.
*Age is reported as median and median absolute deviation.
†Numbers for non-riders are not calculated, as they would not be wearing helmets.
‡Patients were considered not intoxicated unless there was physician documentation of intoxication.
Among e-scooter riders, the most common mechanism of injury was a fall (58 riders [73.4%]). This was followed by a collision with a moving vehicle or object (11 riders [13.9%]) and collision with a stationary object (10 riders [12.6%]). Twenty-seven riders (34.2%) were documented as wearing a helmet, and 13 riders (16.5%) had lights or reflective clothing while riding their e-scooters. Six patients (7.6%) had physician-documented intoxication, either alcohol or drug induced. Thirty-five (42.2%) riders reported to be travelling above the legal speed limit of 15.5mph. Fifty-four (65.1%) e-scooter incidents happened on the road, 28 incidents (12.0%) on the pavement and one within the patient’s private property.
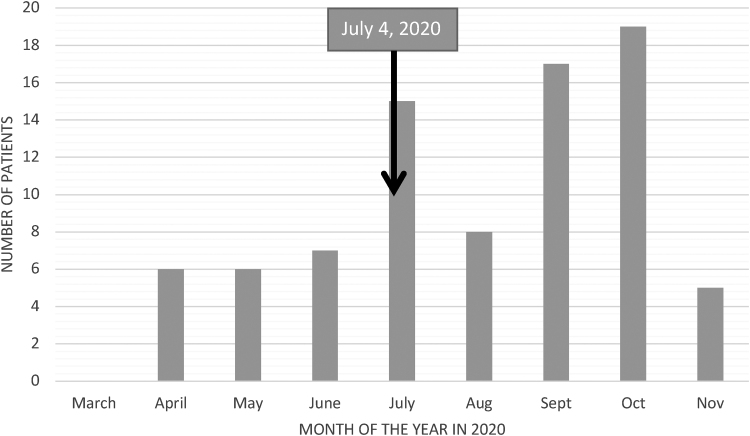
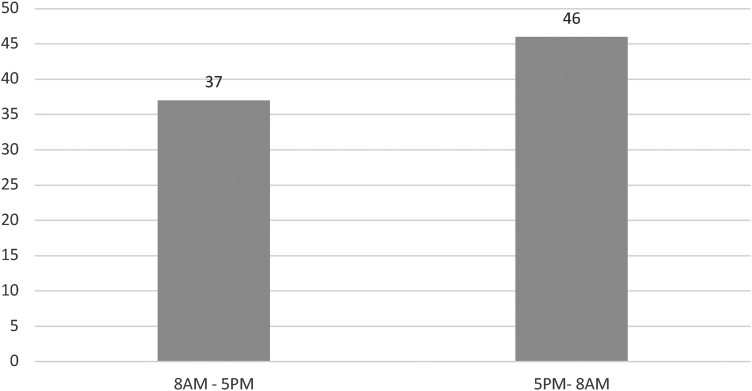
Figure 1 demonstrates a steady increase in number of incidents involving e-scooters from March to November 2020. The months with the highest number of injuries were July (15), September (17) and October (19). A large proportion of emergency department attendances (55.4%) occurred out of regular working hospital hours between 5 pm to 8 am (Figure 2). E-scooter injuries seemed to be evenly distributed across the week, with the lowest number of presentations seen on a Friday and Sunday (Figure 3).
Figure 1 .
Bar chart demonstrating the number of e-scooter-related injuries by month
Figure 2 .
Bar chart demonstrating the time of presentation to the emergency department with an e-scooter-related injury based on work shifts in the orthopaedic department
Figure 3 .
Bar chart demonstrating the number of presentations of e-scooter-related injuries by day of the week
There was a total of 105 injuries sustained in the 83 patients. Twenty-five of the 83 patients had multiple injuries (30.1%). A total of 93 (88.6%) of injuries were fractures, of which 12 (12.9%) were open. An open fracture was defined as a wound or break in the skin that communicated directly with the broken bone (for full results, see Table 2). Eleven patients had dislocations (10.5%), most commonly of the shoulder (81.8%). Twenty-nine patients (34.9%) required admission to the ward, and the mean length of stay was 4.9 days. No patients required ITU admission, and there were no mortalities.
Table 2 .
Injury and management characteristics
| Characteristic | No. (%) riders |
No. (%) non-riders |
Total (%) |
|---|---|---|---|
| Total number of injuries | 101 | 4 | 105 |
| Fracture | 89 (88.1) | 4 (100) | 93 (88.5) |
| Open fractures | 12 (13.5) | 0 | 12 (12.9) |
| Closed fractures | 73 (82.0) | 4 (100) | 77 (82.8) |
| Closed fracture | 4 (4.5) | 0 | 4 (4.3) |
| dislocations | |||
| Dislocations (no fracture) | 7 (6.9) | 0 | 7 (6.7) |
| Shoulder | 5 (6.3) | 0 | 5 (4.7) |
| Elbow | 1 (1.0) | 0 | 1 (0.9) |
| Finger | 1 (1.0) | 0 | 1 (0.9) |
| Isolated soft tissue injuries | 5 (5.0) | 0 | 5 (4.8) |
| Ankle | 2 (2.0) | 0 | 2 (1.9) |
| Knee | 2 (2.0) | 0 | 2 (1.9) |
| Forearm | 1 (1.0) | 0 | 1 (0.9) |
| Operations* | 30 (29.7) | 30 (29.7) | |
| Open reduction/internal fixation | 14 | 14 | |
| External fixation + delayed ORIF | 4 | 4 | |
| Manipulation under anaesthesia/closed reduction | 6 | 6 | |
| Dynamic hip screw | 1 | 1 | |
| Intramedullary device | 3 | 3 | |
| Circular frame | 1 | 1 | |
| Isolated soft tissue repair | 5 | 5 | |
ORIF, open reduction internal fixation.
*Categories are not mutually exclusive, some patients underwent multiple procedures.
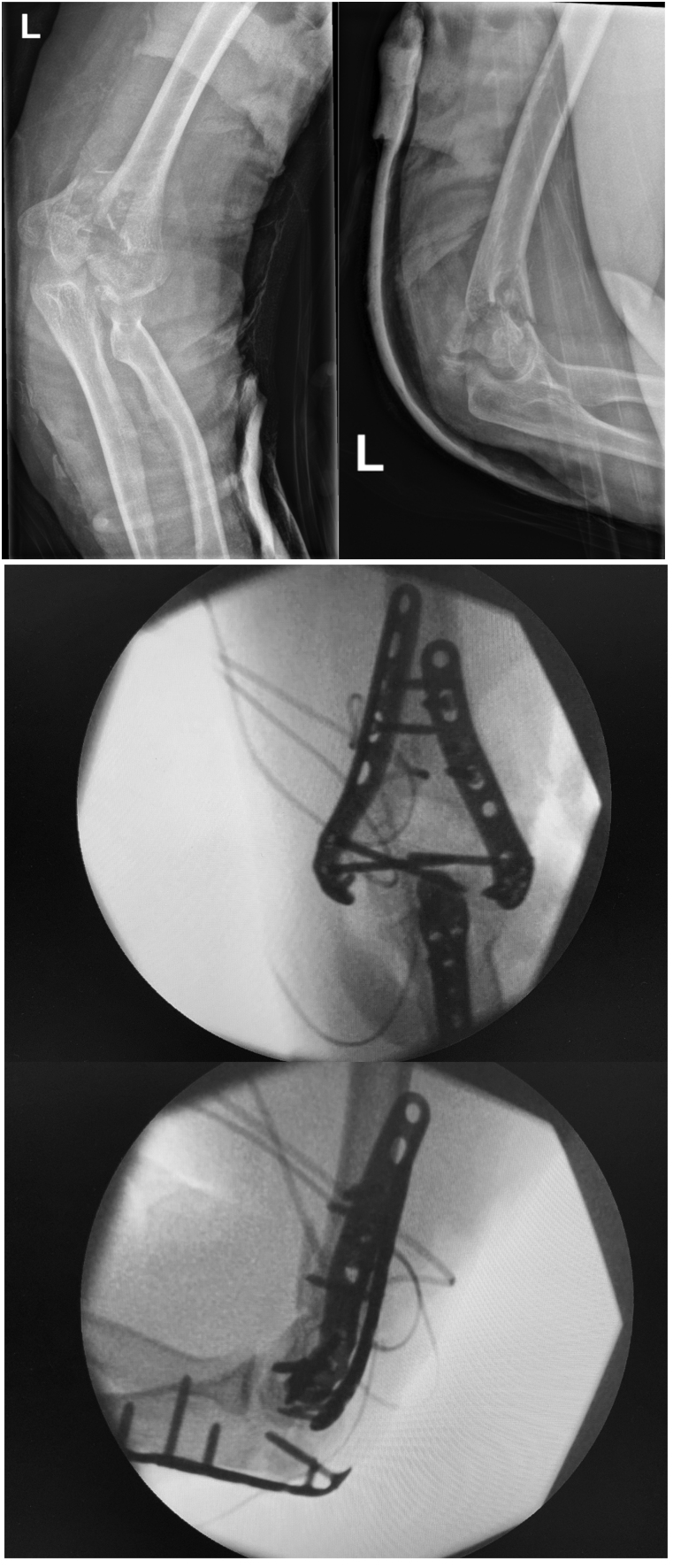
There were 52 upper limb fractures (56.0%), 39 lower limb fractures (41.9%), 1 spinal fracture and 1 rib fracture (for full results, see Table 3). The most common fracture was to the radius, with 14 radial head fractures, 9 distal radial fractures and 3 mid shaft fractures. Two patients sustained bilateral radial head fractures. Metatarsal fractures were the next most common, with four patients sustaining multiple fractures to three metatarsals in the same foot. Two male patients aged 34 and 37, sustained neck of femur fractures (Figure 4) requiring a dynamic hip screw and an intramedullary nail, respectively. Of note, other high-energy injuries included an open tibial plateau facture, open distal humerus fracture (Figure 5) and open tibia and fibula fracture with an associated degloving injury.
Table 3 .
Anatomical distribution of fractures
| Anatomical location | Total (n=93) |
|---|---|
| Upper extremity fracture | |
| Total | 52 (56.0%) |
| Clavicle | 6 |
| Humerus Radius | 8 (4 of which were fracture dislocations) 26 |
| Ulna | 8 |
| Hand | 4 |
| Lower extremity fracture | |
| Total | 39 (41.9%) |
| Pelvis | 1 |
| Neck of femur | 2 |
| Femoral shaft | 2 |
| Tibial plateau | 1 |
| Tibial shaft and fibula | 6 |
| Ankle | 8 |
| Calcaneal | 1 |
| Foot | 18 |
| Axial fracture | |
| Total | 2 (2.1%) |
| Spine | 1 |
| Rib | 1 |
Figure 4 .
Preoperative and postoperative antero-posterior (AP) radiographs of the pelvis and lateral of the left hip demonstrating a left neck of femur fracture
Figure 5 .
Preoperative and postoperative antero-posterior (AP) and lateral radiographs of the left elbow demonstrating a comminuted fracture of the distal humerus
Discussion
To the best of the authors' knowledge, this is the first study describing orthopaedic-related e-scooter injuries in the UK. People avoiding public transport during the COVID-19 pandemic is a likely contributing factor to the recent boom in e-scooter sales across the UK, especially in large urban areas. With the steep rise of e-scooter use and ownership follows an increase in e-scooter-related injuries. In the cohort reviewed, there was a noticeable increase in the number of patients referred for orthopaedic injuries through e-scooter use from 19 (22.8%) between March to June 2020 to 59 (71.1%) from July to October 2020. This corresponds to a three-fold increase in orthopaedic injuries from e-scooter incidents, which is most likely related to the announcements of the introduction of the government e-scooter trial schemes. It should be noted that on the 4 July 2020, the government introduced the legal use of e-scooters as part of a rental scheme. Owing to strict UK lockdown restrictions during the COVID- 19 pandemic, the number injured in March was the lowest seen (no injuries sustained) in keeping with the findings of a study conducted in Germany where similar restrictions were in place.9
In our data set, of the 93 fractures, 81 were closed and 12 were open. More than half of these fractures involved the upper limb (56.0%). This follows a very similar injury pattern to studies conducted in Germany where they attributed upper limb fractures to a short distance fall combined with a short reaction time.9 Similarly, another study carried out in the US also recorded radial fractures as the most common injury.10 All e-scooters involved in the injuries were privately owned, and therefore based on the Road Traffic Act of 1988, were being used illegally.5 Sixty-nine out of 83 riders (83.1%) were male with a median age of 32 years. Twenty-five patients (30.1%) required an operation and 29 patients (34.9%) required in-hospital admission with a mean length of stay of 4.9 days. A similar trend is reported by hospitals in Auckland and Southern California where one in five patients required surgical intervention.11,12 This study demonstrated that e-scooter use can be associated with high-energy trauma including neck of femur fractures in otherwise fit young adults, open upper and lower limb fractures and fracture dislocations. These are life-changing injuries that may be preventable with the introduction and enforcement of specific safety measures for e-scooters.
Established evidence demonstrates that bicycle helmet use in cyclists is associated with a reduced incidence of serious head and facial injuries.13 Despite this, only 27 of the 83 (34.1%) e-scooter riders in our study used them. A similar finding was demonstrated by Trivedi et al in Southern California where among 193 e-scooter riders, 182 (94.3%) were not wearing a helmet.10 Siow et al reported 2.9% helmet use among the e-scooter riders they reviewed.14 In our series, only one patient had a concomitant head injury (subarachnoid and subdural haemorrhage), which is less than expected based on the published literature.3 Thirty-five of the e-scooter riders (42.2%) identified in our data reported to be travelling at a speed of more than 15.5mph, which is above the legal speed limit for these micro-mobility devices. Travelling at greater speeds has the potential to lead to more serious high-energy injuries.5 Some electronic scooter models have been reported to go up to speeds greater than 40mph.5,7 These data highlight the need for a strict enforcement of a maximum speed limit with the possible safe use of geo-fencing technology. This technology creates ‘zones’ to enforce specific speed rules based on the location of the e-scooter from designated parking areas to reduce the maximum speed limit in busy corridors using a global positioning system (GPS).15 However, the use of this technology is controversial, as there are reports of e-scooters suddenly stopping or slowing down without warning, causing riders to lose balance and crash.16 Therefore, further research is warranted to evaluate the safety of this technology in relation to e-scooters. There were 14 (16.9%) e-scooter riders who were aged less than 16 years old, with the youngest rider in our cohort 11 years of age. Injuries in this group may be preventable with enforcement of an e-scooter licence that specifies a minimum age for use. The introduction of a licence may also reduce the occurrence of riding under the influence of alcohol or recreational drugs, which has been reported to range from 17.8% to 36.6% of cases.10,14,17 In our data, six e-scooter riders (7.2%) were either intoxicated or perceived to be intoxicated.
Designated spaces for e-scooters are currently undefined. The most common place of injury among this cohort was on the road (65.1%). Twenty-six (32.9%) were riding on the pavement and only one was riding on private property. The government shared-scheme proposals require e-scooter users to use the road and cycle lanes, with use on pavements prohibited.5–7 On the pavement, e-scooters can be travelling at high speeds and pose a risk to pedestrians. In this study, four pedestrians were injured (three being directly hit by e-scooters and one tripped on a parked e-scooter), which is not insignificant.
Study limitations
There are limitations to our study including its retrospective nature and short study period, providing only a snapshot of the orthopaedic injury patterns. This study may not have captured less-significant injuries, which may have been managed purely by the emergency department, potentially introducing an exclusion bias, which could result in underestimation of the true injury incidence. Nevertheless, this is a multicentre study in a large urban centre and is the first study to report e-scooter-related orthopaedic injuries in the UK. Further studies are required to fully understand the long-term impact of e-scooter-related injuries on the patient and the economic burden on the NHS.
Conclusion
As electronic scooter use continues to grow in the UK and across the world, the number of both minor and major orthopaedic injuries is likely to increase. Despite the attractiveness of an affordable, socially distanced means of transportation, e-scooters can cause serious musculoskeletal injury, and the long-term implication of this is currently unknown. As the UK plans to significantly increase the availability of e-scooter rental schemes, serious consideration should be taken in the drafting of safety regulations to ensure appropriate injury prevention mechanisms are in place to protect both the riders and the public.
References
- 1.Moftakhar T, Wanzel M, Vojcsik Aet al. Incidence and severity of electric scooter-related injuries after introduction of an urban rental programme in Vienna: a retrospective multicentre study. Arch Orthop Trauma Surg 2021; 141: 1207–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cha Sow King C, Liu M, Patel Set al. Injury patterns associated with personal mobility devices and electric bicycles: an analysis from an acute general hospital in Singapore. Singapore Med J 2020; 61: 96–101. 10.11622/smedj.2019084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aizpuru M, Farley KX, Rojas JCet al. Motorized scooter injuries in the era of scooter-shares: A review of the national electronic surveillance system. Am J Emerg Med 2019; 37: 1133–1138. 10.1016/j.ajem.2019.03.049 [DOI] [PubMed] [Google Scholar]
- 4.Brownson AB, Fagan PV, Dickson S, Civil ID. Electric scooter injuries at Auckland city hospital. N Z Med J 2019; 132: 62–72. [PubMed] [Google Scholar]
- 5.Hirst D. Regulating electric scooters. https://commonslibrary.parliament.uk/research-briefings/cbp-8958/ (cited December 2020).
- 6.Department for Transport. E-Scooter trials: Guidance for local areas and rental operators. https://www.gov.uk/government/publications/e-scooter-trials-guidance-for-local-areas-and-rental-operators/e-scooter-trials-guidance-for-local-areas-and-rental-operators (cited December 2020).
- 7.Transport for London. TfL And London Councils Look For E-Scooter Operators to Take Part in Year-Long Rental Trial.https://tfl.gov.uk/info-for/media/press-releases/2020/november/tfl-and-london-councils-look-for-e-scooter operators-to-take-part-in-year-long-rental-trial (cited December 2020).
- 8.Ishmael CR, Hsiue PP, Zoller SDet al. An early look at operative orthopaedic injuries associated with electric scooter accidents: bringing high-energy trauma to a wider audience. JBone Joint Surg Am 2020; 102: e18. 10.2106/JBJS.19.00390 [DOI] [PubMed] [Google Scholar]
- 9.Störmann P, Klug A, Nau Cet al. Characteristics and injury patterns in electric-scooter related accidents-A prospective two-center report from Germany. J Clin Med 2020; 9: 1569. 10.3390/jcm9051569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trivedi TK, Liu C, Antonio ALMet al. Injuries associated with standing electric scooter Use. JAMA Netw Open 2019; 2: e187381. 10.1001/jamanetworkopen.2018.7381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bekhit MNZ, Le Fevre J, Bergin CJ. Regional healthcare costs and burden of injury associated with electric scooters. Injury 2020; 51: 271–277. 10.1016/j.injury.2019.10.026 [DOI] [PubMed] [Google Scholar]
- 12.Dhillon NK, Juillard C, Barmparas Get al. Electric scooter injury in southern California trauma centers. J Am Coll Surg 2020; 231: 133–138. 10.1016/j.jamcollsurg.2020.02.047 [DOI] [PubMed] [Google Scholar]
- 13.Olivier J, Creighton P. Bicycle injuries and helmet use: a systematic review and meta-analysis. Int J Epidemiol 2017; 46: 278–292. 10.1093/ije/dyw153 [DOI] [PubMed] [Google Scholar]
- 14.Siow MY, Lavoie-Gagne O, Politzer CSet al. Electric scooter orthopaedic injury demographics at an urban level I trauma center. J Orthop Trauma 2020; 34: e424–e429. 10.1097/BOT.0000000000001803 [DOI] [PubMed] [Google Scholar]
- 15.Maheswaranathan G. Mobile device with configurable communication technology modes and geofences. https://patents.google.com/patent/US10064005B2/en (cited December 2020).
- 16.Kawamoto D. Is geofencing the answer to cities’ electric scooter challenges? Government Technology. https://www.govtech.com/fs/Is-Geofencing-the-Answer-to-Cities-Electric-Scooter-Challenges.html (cited March 2021). [Google Scholar]
- 17.Blomberg SNF, Rosenkrantz OCM, Lippert F, Collatz Christensen H. Injury from electric scooters in Copenhagen: a retrospective cohort study. BMJ Open. 2019; 9(12): e033988. 10.1136/bmjopen-2019-033988 [DOI] [PMC free article] [PubMed] [Google Scholar]