Abstract
Adverse reactions to metal debris in relation to metal-on-metal hip arthroplasty has been heavily discussed in the literature. In contrast, few cases have been reported in the context of total knee arthroplasty. A 77-year-old woman presented with a painful total knee arthroplasty. At the time of revision surgery, intra-articular cream-coloured fluid and material was found in association with a well-fixed prosthesis. Synovial and capsular samples were obtained for histological assessment and a diagnosis of aseptic lymphocytic vasculitis associated lesion was confirmed. The patient went on to have an uncomplicated recovery following a two-stage revision to a constrained knee prosthesis.
Keywords: Arthroplasty, Replacement, Knee, ALVAL
Background
Aseptic lymphocytic vasculitis-associated lesion (ALVAL) is a histological diagnosis describing cellular changes that occur in response to metal debris within surrounding soft tissue structures. It is grouped with similar soft tissue reactions, such as metallosis and pseudotumours under the broader term ‘adverse reactions to metal debris’. It is a well-recognised response seen in total hip arthroplasty, predominantly associated with metal-on-metal bearing surfaces and trunnionosis.1 However, the presence of adverse reactions to metal debris in relation to total knee arthroplasty has only been highlighted more recently, predominantly in relation to aseptic loosening or polyethylene bearing wear. We report a case of ALVAL in a 77-year-old woman, four years after a routine cemented total knee arthroplasty, which was found to be well-fixed with minimal bearing wear at the time of revision surgery.
Case history
A 77-year-old woman was referred to our tertiary knee unit with right knee pain, having had an uncomplicated standard cruciate-retaining total knee arthroplasty four years earlier. Despite initially making an uneventful recovery, within 18 months joint pain had started to develop. The symptoms progressed further, and a symptomatic valgus deformity also developed. The patient’s medical history included hypertension, hypothyroidism, coeliac disease and osteoporosis.
At initial examination, a well-healed scar with no concerning features or effusion was noted. There was an active range of motion from 0 to 90 degrees, with stability in the sagittal plane. A partially correctable valgus deformity of 20 degrees was present, with a clinically deficient medial collateral ligament, but this was considered to have a firm end point.
Standard departmental preoperative investigations were conducted, which included a normal white cell count and inflammatory markers (C-reactive protein, erythrocyte sedimentation rate), plain radiographs and single-photon emission computed tomography, which showed no radiological signs of loosening or infection (Figure 1).
Figure 1 .
Long-leg radiograph with the right knee demonstrating the primary total knee arthroplasty and significant valgus deformity
Following discussion in the multidisciplinary team meeting, the patient agreed to undergo a single-stage revision to a constrained knee prosthesis, with the option of a hinge design if necessary. On the day of surgery, general anaesthesia was administered but no antibiotics were given until collection of tissue samples. The previous midline incision was used and the wound aspirated prior to the capsular incision. Surprisingly, 20ml of cream-coloured liquid was aspirated (Figure 2).
Figure 2 .
Cream-coloured fluid in sample pot aspirated at the time of revision surgery
The arthrotomy was completed, revealing further intra-articular white fluid, as well as pale, cheese-like material. There were no obvious soft tissue masses and both tibial and femoral components were found to be well-fixed with no osteolysis and minimal wear to the polyethylene bearing. Multiple biopsies for histopathology and microbiology were taken, followed by thorough debridement. The decision was then made to abandon a single-stage procedure, insert a cement spacer and manage initially with intravenous antibiotics for a possible periprosthetic joint infection while awaiting biopsy results.
Histology samples from the synovium and capsule demonstrated areas of necrosis with scattered metal particles, with some focal areas of macrophage sheets and mild chronic inflammation present (Figure 3). Inflammatory infiltrate-containing lymphocytes were found centred on small vessels, diagnostic of ALVAL (Figure 4).
Figure 3 .
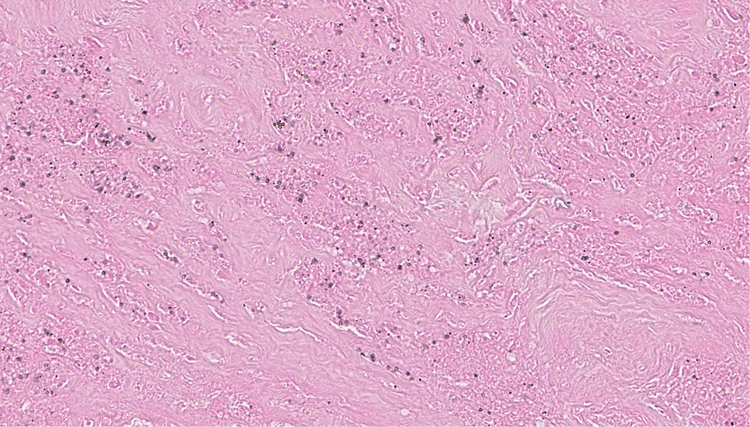
Histology of synovial tissue demonstrated metallic debris
Figure 4 .
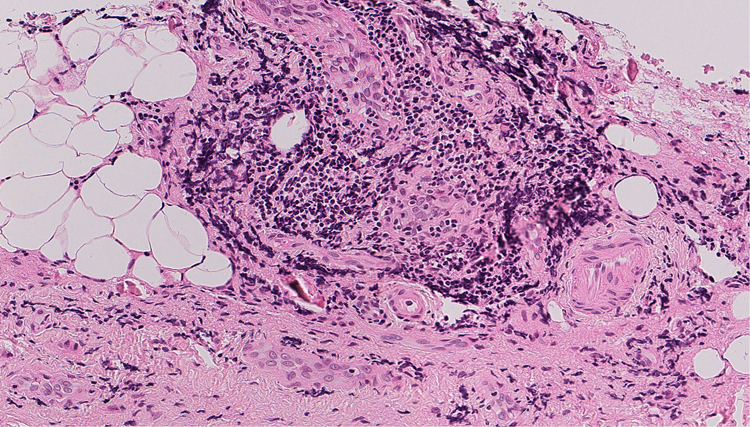
Histology demonstrating lymphocytic perivascular infiltration, diagnostic of an aseptic lymphocytic vasculitis-associated lesion
Blood tests for metal ion levels, post first-stage revision, demonstrated raised cobalt levels of 141.8nmol/l (reference range 0–10nmol/l) and normal chromium levels (31.1nmol/l; reference range 0–40nmol/l). Tissue cultures showed no growth at 48 hours and only one of five samples showed a scanty growth of Staphylococcus aureus on enrichment culture only. Following discussion in the multidisciplinary team, this was thought to be a contaminant. The diagnosis of ALVAL was confirmed and the patient proceeded to have an uneventful and uncomplicated second-stage revision to a constrained design, because of unexpected and significant medial collateral ligament laxity. Six months postoperatively, the patient was found to be pain free and was mobilising well.
Discussion
Recent reports have shown that ALVAL is more prevalent in revision total knee arthroplasty than previously thought. In a retrospective cohort study of 321 aseptic revision total knee arthroscopies, histological analysis found high-grade ALVAL in 7.2%.2 The majority of these cases were revised for loosening, bearing wear or instability. In contrast, our report describes a case of ALVAL in the context of a well-fixed primary total knee arthroplasty.
Adverse local tissue reactions have also been described in total knee arthroplasty in the context of modular designs and in relation to wear of polyethylene bearings, with histological examination demonstrating polyethylene particles, giant cells and macrophages.3,4 However, our patient had a standard monobloc design in place with minimal bearing wear, as well as histological findings of metal debris and lymphocytic infiltrate, diagnostic of ALVAL.
To our knowledge, this is the first report in the literature of a case of ALVAL in the context of a well-fixed nonmodular primary total knee arthroplasty. However, with the prosthesis found to be in good condition at revision surgery, the question of where the metal debris originated is raised. There was no obvious damage to either of the metallic components or the polyethylene liner. There was laxity in her medial collateral ligament, but this was found to be intact. We cannot exclude a partial injury to the medial collateral ligament at the time of the primary arthroplasty, which gradually led to excessive wear and loading in the medial tibiofemoral compartment causing the gradual valgus deformity. However, there was adequate separation of the two metallic components with the polyethylene liner. Klontz et al reported a case of acute metallosis in a total knee arthroplasty, despite noting a prosthesis in pristine condition at the time of revision surgery.5 Histological analysis in their case revealed iron debris. They hypothesised that this may have arisen from the saw at the time of the primary surgery, as iron was the main component of the saw blade. In contrast, our case showed raised level of cobalt ions, in association with consistent histological interpretation of ALVAL.
Conclusions
ALVAL can occur in the setting of seemingly uncomplicated total knee arthroplasty in the absence of direct loosening or direct metallic surface bearings. We recommend adherence to national and local revision pathways as regards to management of painful total knee arthroplasty, while considering this condition as a possible cause.
References
- 1.Drummond J, Tran P, Fary C. Metal-on-metal hip arthroplasty: a review of adverse reactions and patient management. J Funct Biomater 2015; 6: 486–499. 10.3390/jfb6030486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurmis AP, Herman A, McIntyre ARet al. Pseudotumors and high-grade aseptic lymphocyte-dominated vasculitis-associated lesions around total knee replacements identified at aseptic revision surgery: findings of a large-scale histologic review. J Arthroplasty 2019; 34: 2434–2438. 10.1016/j.arth.2019.05.025 [DOI] [PubMed] [Google Scholar]
- 3.Nadlacan LM, Freemont AJ, Paul AS. Wear debris-induced pseudotumour in a cemented total knee replacement. Knee 2000; 7: 183–185. 10.1016/S0968-0160(00)00049-1 [DOI] [PubMed] [Google Scholar]
- 4.McMaster WC, Patel J. Adverse local tissue response lesion of the knee associated with morse taper corrosion. J Arthroplasty 2013; 28: 375.e5–375.e8. 10.1016/j.arth.2012.04.005 [DOI] [PubMed] [Google Scholar]
- 5.Klontz KC, Smith WI, Jonathan CK. Acute metallosis following total knee replacement: a case report. J Orthop Case Rep 2014; 4: 21–23. 10.13107/jocr.2250-0685.142 [DOI] [PMC free article] [PubMed] [Google Scholar]



