Abstract
Hip disarticulation is the removal of the entire lower limb through the hip joint by detaching the femur from the acetabulum. This major ablative procedure is rarely performed for infection but may be required in severe necrotising fasciitis. We present a single centre retrospective review of all cases of emergency hip disarticulations in patients with necrotising fasciitis between 2010 and 2020. All five patients included in the review presented with acute lower limb pain and sepsis. Three patients had comorbidities predisposing them to necrotising fasciitis. Three were deemed to be high risk and two were at intermediate risk of developing necrotising fasciitis. There were two deaths in the postoperative period. Of the three survivors, two required revision surgery for a completion hindquarter amputation and one for flap closure. All three survivors had good functional outcomes after discharge from hospital. Despite its associated morbidity, emergency amputation of the entire lower limb is a life-saving treatment in cases of rapidly progressing necrotising fasciitis and should be considered as a first-line option in managing this condition.
Keywords: Necrotising Fasciitis, Disarticulation, Hemipelvectomy, Debridement
Background
Necrotising fasciitis is a progressive, rapidly spreading infection of the deep fascia with secondary involvement of the subcutaneous tissues. It affects men and women equally with an incidence of 0.4–1 per 100,000.1,2 Although seen rarely, the quickly spreading nature of the infection contributes to a staggering mortality rate of 24–80%.3,4 A high level of clinical suspicion together with swift surgical intervention is of paramount importance in attempting to achieve a favourable outcome in these patients.
The anatomical distribution of soft-tissue involvement in necrotising fasciitis can vary, with the most common sites affected being the extremities, perineum and external genitalia.1 Of the extremities, the lower limbs seem to be more susceptible, with an amputation rate of up to 26%.5,6 The level of limb loss depends on the distribution of tissue involvement and can vary from below the knee to a full disarticulation of the hip joint and hindquarter amputation.
A hip disarticulation is the removal of the entire lower limb through the hip joint by detaching the femur from the acetabulum. When this operation extends to include a portion of the ipsilateral pelvis, it is then classified as a hindquarter amputation or external hemipelvectomy. In the United States, hip disarticulations contribute to just 0.5% of all lower limb amputations performed and are rarely carried out for infectious disease.7 Case series and reports published describe hip disarticulations and hindquarter amputations for postoperative infections from orthopaedic surgery, vascular graft infections, decubitus ulcers and necrotising fasciitis.8–11 More common indications include malignant tumours of bone and soft tissue, trauma and limb ischaemia.
By virtue of the destructive nature of the disease, patients with necrotising fasciitis experience a huge degree of physiological setback. A major ablative procedure such a hip disarticulation can have long-lasting consequences for a patient and in itself carries significant mortality. We present our experience of five patients with necrotising fasciitis who underwent emergency hip disarticulations as an immediate procedure to control sepsis with completion hindquarter amputations in two of them and discuss our outcomes.
Case history
A 10-year review was performed of all patients who underwent a hindquarter amputation for necrotising fasciitis between 2010 and 2020. Clinical information, laboratory results, imaging and operative findings were obtained from electronic patient records and case notes.
The diagnosis of necrotising fasciitis was made on clinical grounds and in cases where there was diagnostic uncertainty, computed tomography (CT) was used to aid decision making. Patients were scored for severity of their infection as per the Laboratory Risk Indicator for Necrotising Fasciitis (LRINEC) score and classified into three risk categories suggesting the likelihood of them developing necrotising fasciitis. A score of less than six was considered low risk, six to seven was intermediate risk and eight or more was high risk.
All patients were given intravenous antibiotics as per hospital protocol within an hour of diagnosis of sepsis. The indication for surgical exploration was septic shock associated with a high index of clinical suspicion and/or radiological evidence of necrotising fasciitis. All patients underwent a hip disarticulation amputation in the initial setting together with debridement of involved tissue till healthy bleeding edges were reached. The operation was frequently performed as a combined procedure between specialties and involved at least two consultant surgeons from the general surgical, orthopaedic or vascular teams. The patients were nursed postoperatively in the intensive care unit and repeat surgery planned if required. Completion hindquarter amputations were then performed on patients if deemed necessary to assist wound closure and the regional plastic surgery service was consulted with to assist with this.
Data collected included demographic variables, medical comorbidities, LRINEC scores, intraoperative findings, postoperative complications, nature of bacterial flora grown from specimens and mortality data.
Discussion
Five patients underwent emergency hip disarticulations for necrotising fasciitis of the lower limb during the study period. The ages of patients ranged from 32 years to 84 years (three men and two women). All patients presented to the emergency department with acute severe and progressive lower limb or groin pain, clinical signs of sepsis and progression to septic shock. One patient reported a week’s history of a flu-like illness before presentation, another had a history of trauma to the lower limb and three patients had no preceding symptoms. Patient demographics, LRINEC scores and other significant findings are shown in Table 1.
Table 1 .
Patient demographics and case details
| Case | Age | Gender | Comorbidities | LRINEC Score | Imaging | Causative Organism | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 40 | M | IVDU, Hepatitis C Cirrhosis | 11 | None | Mixed anaerobes | Died |
| 2 | 43 | F | Diabetes Mellitus | 10 | None | Peptostreptococcus, Group B Streprococcus | Survived |
| 3 | 84 | M | None | 9 | XR | Group A Hemolytic Streptococcus | Survived |
| 4 | 32 | F | None | 6 | CT | Group A Hemolytic Streptococcus | Died |
| 5 | 43 | M | Undiagnosed Hairy Cell Leukemia | 6 | CT | Group C Hemolytic Streptococcus | Survived |
IVDU: Intravenous drug use, XR: X-ray, M: Male, F: Female
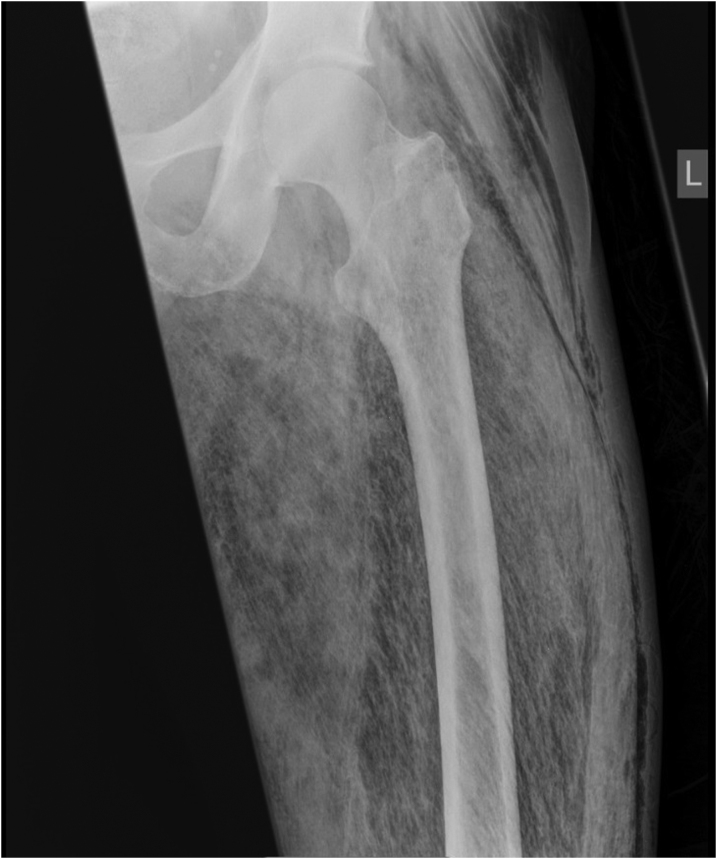
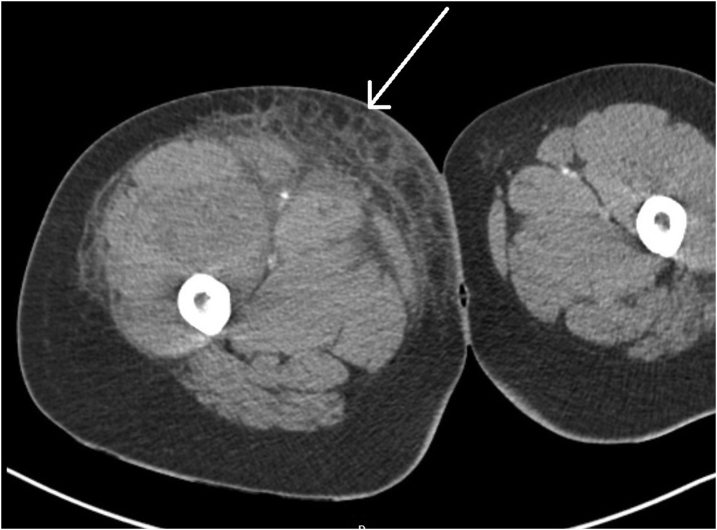
Three patients had underlying medical comorbidities including malignancies, diabetes and high-risk behaviour that predisposed them to developing necrotising fasciitis. The decision to operate in patients deemed to be at high risk of developing necrotising fasciitis with a LRINEC score of 9 and above was made immediately and not delayed by the need for cross-sectional imaging. One of those patients had an x-ray of the femur in the emergency department as there was a clinical suspicion of a closed fracture. This revealed a large amount of subcutaneous gas within the soft tissue of the limb which strongly pointed further towards a diagnosis of necrotising fasciitis (Figure 1). Both patients with an intermediate risk of necrotising fasciitis had CT of the pelvis and lower extremities before operative intervention to aid diagnosis. Findings noted on cross-sectional imaging were consistent with necrotising fasciitis and included extensive soft-tissue inflammation, subcutaneous oedema and thickening of the involved muscle groups (Figures 2 and 3).
Figure 1 .
X-ray of left femur (patient 3) demonstrating extensive abnormal distribution of air in the subcutaneous tissue plane
Figure 2 .
Computed tomography axial slices (patient 4) showing subcutaneous inflammation and muscular oedema of the right lower limb
Figure 3 .
Computed tomography coronal slices (patient 5) showing subcutaneous inflammation and oedema of the soft tissue and muscles of the left lower limb
All patients underwent emergency surgery within four hours of the diagnosis of necrotising fasciitis and required extensive ionotropic support prior to commencement of surgery, intra- and postoperatively. Such was the haemodynamic instability encountered that one patient suffered four cardiac arrests during surgery.
Microbiological analysis of the debrided tissue specimens revealed a variety of causative organisms with the most common one being group B haemolytic Streptococcus. Other pathogens noted were group A and group C Streptococcus, Peptostreptococcus and mixed anaerobic organisms.
Unfortunately, two patients ultimately succumbed to their infection and died in the postoperative period (a mortality rate of 0.4). They had initially responded encouragingly after surviving the first operation but continued to deteriorate secondary to overwhelming sepsis. At the time, it was deemed clinically that further debridement would not have made a difference to their outcome and a decision to palliate was made. Two of three patients that survived the initial insult had re-look debridement and completion hindquarter amputations to facilitate better closure of the wound. This was following an extensive trial of vacuum-assisted closure therapy, which failed to provide adequate wound healing. The failure of vacuum-assisted closure therapy was largely due to the difficult postoperative anatomy and vast area of the debrided site, which posed a real challenge to achieving an adequate seal around the wound edge. Therefore, a further removal of bony tissue was required to close the wound appropriately. The third patient needed transfer to the regional plastic surgery unit for a flap closure.
Looking at long-term results postoperatively in the three patients who were successfully discharged from hospital, one was fitted with a prosthesis with a good functional outcome, one has good use of an electric wheelchair and one died following a new diagnosis of a lymphoma the year after the amputation but was able to mobilise on one leg with crutches up to that point. Routinely performing bowel and bladder diversion in the form of a colostomy or urostomy was not required in these patients. However, one of the three surviving patients required the creation of a laparoscopic defunctioning loop colostomy after surviving the sepsis to allow for better faecal management and continued to manage it well at the time of final follow up.
Discussion
The primary insult in most cases of necrotising fasciitis is thought to be skin trauma against a background of immunosuppression. In some patients, the trauma may be extremely trivial and is unlikely to be elicited from history unless specific leading questions are asked. The most common causes of penetrating injury include recent surgery, minor invasive procedures, intravenous drug use and insect or animal bites.12 There is also a reported association between non-penetrating trauma, seemingly insignificant muscular strains and the development of necrotising fasciitis.13 Chronic illnesses such as liver cirrhosis, cardiac failure, uncontrolled diabetes mellitus and underlying malignancies are risk factors and poor prognostic indicators.14–16 This is further evidenced in these cases, with three of five patients having a predisposing medical condition. Nevertheless, the possibility of necrotising fasciitis in a previously fit and well patient should be strongly considered and must not be overlooked if there is a high level of clinical suspicion.
There is no doubt that the immediate source control of sepsis is extremely vital to achieving the best possible outcome in this cohort of patients. Therefore, rapid decision making facilitating urgent surgical debridement and amputation must be of paramount importance. CT is a useful adjunct when there is uncertainty of diagnosis but should not be relied on to guide management, especially if there is a delay in obtaining access to it. Clinical judgement, together with the LRINEC score, remains the most efficient diagnostic tool and a decision to operate must be taken early by an appropriately experienced clinician. As noted in our review, patients with a high risk of developing necrotising fasciitis were immediately transferred to the operating theatre without the wait for cross-sectional imaging. Surgical start time was achieved within four hours of diagnosis in all our cases, but despite early intervention, the survival rate was only three of five. This is likely because most patients have already suffered a devastating physiological setback on presentation, which is soon recognised to be irreversible in nature. We reviewed the number of severe soft-tissue infections of the lower limb that presented as an emergency at our centre across the same period that needed debridement alone and discovered that the 30-day mortality in this cohort of 50 patients was zero.
Such is the physiological strain of the infection and the insult of extensive surgery that all patients required aggressive perioperative inotropic support including combinations of metaraminol, noradrenaline, adrenaline and vasopressin. One patient required quadruple strength noradrenaline to maintain their blood pressure during the procedure and another patient suffered four intraoperative cardiac arrests. Coupled with the overwhelming burden of severe sepsis is further insult through hypovolaemia. All our patients required aggressive transfusion through surgery with units of red blood cells, fresh frozen plasma, cryoprecipitate and platelets given in combination in large numbers (range of 14–22 units of combined products). This suggests that while these patients require extensive resuscitation, aggressive treatment in the form of cardiovascular support, correction of fluid losses and rapid surgery can result in survival.
With the help of early decision making, a multidisciplinary surgical approach and perioperative treatment on the intensive care unit we were able to achieve a modest survival rate after emergency hip disarticulation. There is a lack of good quality data for us to compare our results against due to the infrequent occurrence of such cases. Unruh et al reported a 22% mortality in patients who underwent emergency hip disarticulation for femoral head osteomyelitis but most of the other patients in their experience had surgery for sequelae related to peripheral vascular disease with no reported cases of necrotising fasciitis.17 Another series by Endean et al demonstrated a postoperative mortality of 14% after hip disarticulation for infectious causes. However, only three of their patients were diagnosed with gas gangrene of the lower limb and the majority of patients had surgery for decubitus ulcers and osteomyelitis.18 In addition to mortality, there is a serious morbidity associated with this surgery as patients will be left severely disabled with a proportion of them being wheelchair bound for life.
Severe necrotising fasciitis requiring emergency amputation of the entire lower limb remains a rare occurrence in emergency surgery worldwide and consequently there is a paucity of literature. The cornerstone of the management of these patients is rapid emergency surgery in the form of a hip disarticulation but despite timely intervention, mortality and morbidity is high. In the absence of an alternative effective treatment, such life-saving ablative surgery is the only reliable way to effectively control the progression of necrotising fasciitis and should be the first-line treatment in this group of patients.
References
- 1.Hakkarainen TW, Kopari NM, Pham TN, Evans HL. Necrotizing soft tissue infections: review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg 2014; 51: 344–362. 10.1067/j.cpsurg.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maya SP, Beltrán DD, Lemercier P, Leiva-Salinas C. Necrotizing fasciitis: an urgent diagnosis. Skeletal Radiol 2014; 43: 577–589. 10.1007/s00256-013-1813-2 [DOI] [PubMed] [Google Scholar]
- 3.Yaghoubian A, de Virgilio C, Dauphine Cet al. . Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Arch Surg 2007; 142: 840–846. 10.1001/archsurg.142.9.840 [DOI] [PubMed] [Google Scholar]
- 4.Magala J, Makobore P, Makumbi Tet al. . The clinical presentation and early outcomes of necrotizing fasciitis in a Ugandan tertiary hospital: a prospective study. BMC Res Notes 2014; 7: 476. 10.1186/1756-0500-7-476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anaya DA, McMahon K, Nathens ABet al. . Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch Surg 2005; 140: 151–157. 10.1001/archsurg.140.2.151 [DOI] [PubMed] [Google Scholar]
- 6.Angoules A, Kontakis G, Drakoulakis Eet al. . Necrotising fasciitis of upper and lower limb: a systematic review. Injury. 2007; 38: S19–S26. [DOI] [PubMed] [Google Scholar]
- 7.Dillingham TR, Pezzin LE, Mackenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 2002; 95: 875–883. 10.1097/00007611-200208000-00018 [DOI] [PubMed] [Google Scholar]
- 8.Fenelon G, Foerster GV, Engelbrecht E. Disarticulation of the hip as a result of failed arthroplasty: a series of 11 cases. J Bone Joint Surg Br 1980; 62-B:441–446. 10.1302/0301-620X.62B4.7430220 [DOI] [PubMed] [Google Scholar]
- 9.Virgilio CD, Cherry KJ, Gloviczki Pet al. . Infected lower extremity extra-anatomic bypass grafts: management of a serious complication in high-risk patients. Ann Vasc Surg 1995; 9: 459–466. 10.1007/BF02143860 [DOI] [PubMed] [Google Scholar]
- 10.Lawton RL, De Pinto V. Bilateral hip disarticulation in paraplegics with decubitus ulcers. Arch Surg 1987; 122: 1040–1043. 10.1001/archsurg.1987.01400210078011 [DOI] [PubMed] [Google Scholar]
- 11.Jacobs PP, van der Sluis RF, Tack CJ, Wobbes T. Necrotising fasciitis of the lower limb caused by undiagnosed perforated appendicitis, which necessitated disarticulation of the hip. Eur J Surg 1993; 159: 307–308. [PubMed] [Google Scholar]
- 12.Puvanendran R, Huey JCM, Pasupathy S. Necrotizing fasciitis. Can Fam Physician 2009; 55: 981–987. [PMC free article] [PubMed] [Google Scholar]
- 13.Nuwayhid ZB, Aronoff DM, Mulla ZD. Blunt trauma as a risk factor for group a streptococcal necrotizing fasciitis. Ann Epidemiol 2007; 17: 878–881. 10.1016/j.annepidem.2007.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khamnuan P, Chongruksut W, Jearwattanakanok Ket al. . Necrotizing fasciitis: risk factors of mortality. Risk Manag Healthc Policy 2015; 8: 1–7. 10.2147/RMHP.S77691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang JM, Lim HK. Necrotizing fasciitis: eight-year experience and literature review. Braz J Infect Dis 2014; 18: 137–143. 10.1016/j.bjid.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hung T, Tsai C, Tsai Cet al. . Liver cirrhosis as a real risk factor for necrotising fasciitis: a three-year population-based follow-up study. Singapore Med J 2014; 55: 378–582. 10.11622/smedj.2014090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unruh T, Fisher DH, Unruh TAet al. . Hip disarticulation. Arch Surg 1990; 125: 791–793. 10.1001/archsurg.1990.01410180117019 [DOI] [PubMed] [Google Scholar]
- 18.Endean E, Schwarcz T, Barker Det al. . Hip disarticulation: factors affecting outcome. J Vasc Surg 1991; 14: 398–404. 10.1016/0741-5214(91)90094-B [DOI] [PubMed] [Google Scholar]