Abstract
Retroperitoneal liposarcomas are very infrequent retroperitoneal malignant tumours. Most patients complain of palpable abdominal mass and only half present with abdominal pain. With haematogenous spread they can reach, mainly, lungs and liver, but only in 10% of cases. Here we report the presentation and surgical treatment of a giant massive retroperitoneal liposarcoma in a 53-year-old man.
Keywords: Liposarcoma, Giant liposarcoma, Retroperitoneal liposarcoma, Retroperitoneum
Background
Liposarcomas are the most frequent retroperitoneal tumours.1 Because of their anatomical location and low metastatic potential, well-differentiated retroperitoneal liposarcomas (RLSs) can grow significantly before being detected clinically. These tumours have an average size at diagnosis of over 5cm1,2 and 20% of tumours are larger than 10cm at the time of diagnosis.2,3 Giant RLSs, defined as tumours weighing more than 20kg are a significant challenge for surgical oncologists because of the complexity of managing such bulky tumours and the multivisceral involvement often encountered. Neither systemic chemotherapy nor radiation therapy have shown significant improvement in outcomes for well-differentiated RLSs,4,5 and surgical therapy is the mainstay of treatment for these rare tumours. Therefore, these patients are considered at great risk of perioperative complications. We present the case of a giant RLS successfully managed surgically.
Case history
A 53-year-old man presented to the surgical oncology clinic with increasing abdominal girth despite having undergone a bariatric sleeve gastrectomy 2 years prior and losing 15kg in weight. He reported regular physical activity and had no prior relevant medical history. Physical examination revealed a non-tender, distended abdomen with a palpable mass extending from the epigastrium to the pelvic region and an abdominal girth of 127cm (Figure 1).
Figure 1 .
Giant abdominal mass
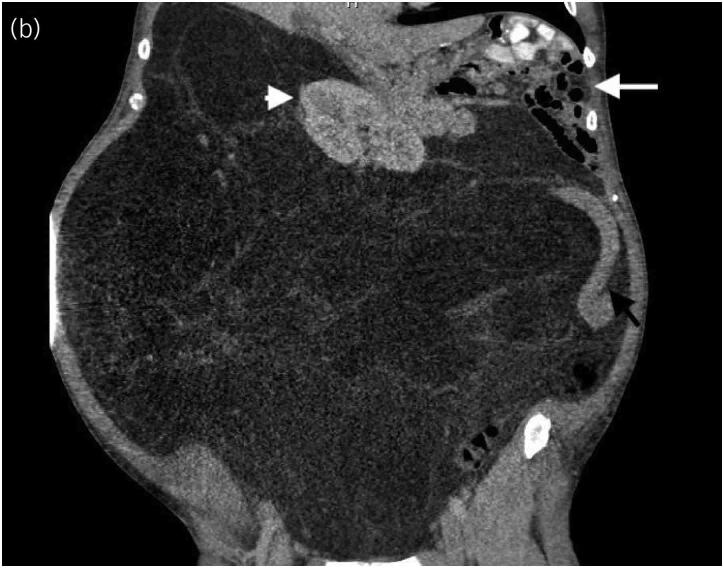
Computed tomography (CT) scan of the abdomen showed a giant heterogeneous mass, measuring 60cm × 75cm × 80cm, leading to displacement of the right kidney, descending colon, small bowel and mesentery to the left upper quadrant (Figure 2).
Figure 2 .
Computed tomography scan of the abdomen showed a giant heterogeneous mass, measuring 60cm × 75cm× 80cm
The mass was homogeneous, and no areas suggesting a dedifferentiated component were noted. Metastatic workup was negative. Both endoscopy and colonoscopy were negative. After physiological evaluation and a multidisciplinary meeting the patient was deemed a candidate for surgery.
A midline laparotomy was performed and an enormous, well-defined, retroperitoneal mass was encountered. Intraperitoneal and retroperitoneal organs were all displaced to the left upper quadrant. The tumour was in close contact with duodenum, liver and vena cava as well as the right kidney. The tumour was resected en bloc (Figure 3) and no additional organ resection was required. Retroperitoneal and peritoneal organs returned to their normal anatomical location after resection.
Figure 3 .
En bloc resected giant liposarcoma
On macroscopic examination, the tumour dimensions were 70cm × 90cm × 100cm and it weighed 26kg (Figure 3). Histopathological examination revealed a low-grade, well-differentiated liposarcoma with typical MDM2 gene amplification.
Two drains were placed to manage the large empty space. The patient had a postoperative ileus that resolved and was discharged on postoperative day 10. Drains were removed on postoperative day 14. The patient had a complete recovery and postoperative follow-up shows no recurrence.
Discussion
RLSs over 20kg are extremely rare and are classified as giant liposarcomas. Giant RLSs have a peak incidence between 40 and 60 years of age. The gender distribution of RLS is approximately equal, although some studies have reported female predominance.1,3,4 There are certain predisposing factors for RLS such as genetic aberrations, ionising radiation exposure, particularly in children undergoing repeated CT and those with diabetes mellitus; the co-existence of RLS and diabetes mellitus has been associated with adverse prognosis. CT or magnetic resonance imaging is the gold standard for diagnosis in all cases.1,5,6 This case is similar to other reported cases in terms of non-specific presentation. Usually these giant tumours are asymptomatic and reach a size of more than 15cm by the time of diagnosis. Clinical manifestations are discomfort or a palpable abdominal mass. There are four histological types, well-differentiated, myxoid/round cell, pleomorphic and dedifferentiated, and three grades (I, II and III) according to the grading system of French Federation Cancer Centres. The most common forms are well-differentiated (46%) followed by myxoid/round cell (28%), dedifferentiated (18%) and pleomorphic (8%).6–8
Surgery remains the mainstay of oncological treatment for well-differentiated RLS as these tumours have very poor response rates to chemotherapy or radiotherapy.2,9 In a review by Zeng et al,9 long-term 5- and 10-year survival rates without complete resection were given as 16.7% and 8.0%, respectively. Lewis et al2 reported their single institutional data for 500 RLS cases, with a median survival of 103 months for those who underwent complete resection with grossly negative margins compared with 18 months for those who underwent incomplete resection. Thus all efforts must be done to achieve complete surgical resection in the initial procedure. Many patients with giant liposarcomas present with hypoproteinaemia or anaemia as a result of tumour consumption. Therefore prehabilitation is required to improve nutritional status prior to this major procedure that often requires multivisceral resection.2,10
Negative microscopic margins can be achieved with combined resection of involved organs (kidney, large and small bowel). Incomplete resection is a negative prognosis factor with average 5- and 10-year survival rates of 16.7% and 8.0% respectively. Local recurrence and metastasis risk are related to the tumour size. If the size of the tumour is less than 2.5cm, the 5-year rate of metastasis is approximately 3%. In cases in which the tumours are larger than 20cm, the metastasis rate is 55–60%. In a cohort study of 72 patients, Neuhaus et al11 found only two variables associated with a decrease in the local recurrence: R0 excision and histological grade I. Finally, long-term follow-up CT scan is necessary within 2 years after initial surgery.2,10,12,13
Conclusion
Size alone does not contraindicate complete resection of giant RLS. Even if huge, they can be removed by a multidisciplinary team in a specialised centre, which is consistent with the consensus management of RLS in the adult. This type of tumour must be treated by a multidisciplinary teamwork involving surgeons, pathologists, imaging specialists, radiation therapists and medical oncologists as in our case.1,5,6,8
References
- 1.Hassan I, Park SZ, Donohue JHet al. Operative management of primary retroperitoneal sarcomas. A reappraisal of an institute experience. Ann Surg 2004; 239: 244–250. 10.1097/01.sla.0000108670.31446.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 1998; 228: 355–365. 10.1097/00000658-199809000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herzberg J, Niehaus K, Holl-Ulrich Ket al. Giant retroperitoneal liposarcoma: A case report and literature review. J Taibah Univ Med Sci 2019; 14: 466–471. 10.1016/j.jtumed.2019.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guraya SY, Al Naami M, Al Tuwaijri T, Arafah MMI. Malignant melanoma of the small bowel with unknown primary: a case report. J Ayub Med Coll Abbottabad 2007; 19: 63–65. [PubMed] [Google Scholar]
- 5.Guraya SY. Malignant duodeno-colic fistula: a rare complication of colorectal cancer. J Clin Diagn Res JCDR 2015; 9: L01. 10.7860/JCDR/2015/16429.6800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lehnert T, Cardona S, Hinz Uet al. Primary and locally recurrent retroperitoneal soft-tissue sarcoma: local control and survival. Eur J Surg Oncol 2009; 35: 986–993. 10.1016/j.ejso.2008.11.003 [DOI] [PubMed] [Google Scholar]
- 7.Nizri E, Fiore M, Barretta Fet al. Intraperitoneal invasion of retroperitoneal sarcomas: a risk factor for dismal prognosis. Ann Surg Oncol 2019; 26: 3535–3541. 10.1245/s10434-019-07615-1 [DOI] [PubMed] [Google Scholar]
- 8.van Houdt WJ, Raut CP, Bonvalot Set al. New research strategies in retroperitoneal sarcoma. The case of TARPSWG, STRASS and RESAR: making progress through collaboration. Curr Opin Oncol 2019; 31: 310–316. 10.1097/CCO.0000000000000535 [DOI] [PubMed] [Google Scholar]
- 9.Zeng X, Liu W, Wu Xet al. Clinicopathological characteristics and experience in the treatment of giant retroperitoneal liposarcoma: a case report and review of the literature. Cancer Biol Ther 2017; 18: 660–665. 10.1080/15384047.2017.1345388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee HS, Yu JI, Hoon D, Lim SJK. Retroperitoneal liposarcoma: the role of adjuvant radiation therapy and the prognostic factors. Radiat Oncol J 2016; 34: 216. 10.3857/roj.2016.01858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuhaus SJ, Barry P, Clark MAet al. Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 2005; 92: 246–252. 10.1002/bjs.10305 [DOI] [PubMed] [Google Scholar]
- 12.Ecker B, Peters M, McMillan Met al. Preoperative radiotherapy in the management of retroperitoneal liposarcoma. Br J Surg 2016; 103: 1839–1846. 10.1002/bjs.10305 [DOI] [PubMed] [Google Scholar]
- 13.Zenga X, Liua W, Wub Xet al. Clinicopathological characteristics and experience in the treatment of giant retroperitoneal liposarcoma: A case report and review of the literature. Cancer Biol Ther 2017; 18: 660–665. 10.1080/15384047.2017.1345388 [DOI] [PMC free article] [PubMed] [Google Scholar]