Abstract
Introduction
The first wave of the COVID-19 pandemic led to an unprecedented time for the management of colorectal cancer, with uncertainty as to cancer-specific risks and the circumventing of gold standard oncological strategies. Our study aimed to acquire a snapshot of the practice of multidisciplinary team (MDT) management and variability in response to rapidly emerging guidelines.
Methods
The survey was disseminated to 150 colorectal cancer MDTs across England and Wales taken from the National Bowel Cancer Audit data set between 15 April and 30 June 2020 for completion by colorectal surgeons.
Results
Sixty-seven MDTs responded to the survey. Fifty-seven centres reported that they continued to perform colorectal cancer resections during the initial lockdown period. Fifty centres (74.6%) introduced routine preoperative COVID-19 testing and 50 (74.6%) employed full personal protective equipment for elective cases. Laparoscopic resections were continued by 25 centres (42.1%), whereas 28 (48.3%) changed to an open approach. Forty-nine (79.0%) centres reported experiencing patient-led surgical cancellations in 0–25% of their listings. If surgery was delayed significantly then 24 centres (38.7%) employed alternative neoadjuvant therapy, with short-course radiotherapy being their preferred adjunct of choice for rectal cancer. Just over 50% of the MDTs stated that they were uncomfortable or very uncomfortable with their management strategies.
Conclusions
Our study demonstrates variability in the MDT management of colorectal cancer during the initial COVID-19 lockdown, incorporating adaptive patient behaviour and initially limited data on oncological safety profiles leading to challenging decision-making.
Keywords: Colorectal, Cancer, COVID-19
Introduction
There are 41,000 new cases of colorectal cancer in the United Kingdom (UK) each year, with approximately one-third being rectal in origin. The management of colorectal cancer varies significantly depending upon tumour location and staging, but often includes neoadjuvant chemoradiotherapy and surgical resection. Colorectal cancer treatment has improved significantly over the past 10 years, with improvements in magnetic resonance imaging (MRI) staging, neoadjuvant therapy and a multidisciplinary team (MDT) approach.
The first wave of the COVID-19 pandemic led to an unprecedented period in the National Health Service (NHS), with staff redeployment, reduced theatre and critical care capacity and a lack of underlying knowledge regarding the specific risks to patients with cancer. Patient behaviour in accessing healthcare changed, general practitioner referral rates fell and diagnostic services, including endoscopy for tissue biopsies, were limited.1 The development of COVID-19 with respiratory complications in the perioperative setting led to unacceptably high rates of morbidity and mortality.2
More novel neoadjuvant strategies evolved, especially for rectal cancer, to prevent disease progression during delays to resection, with increased use of short-course radiotherapy and avoidance of the morbidity of chemotherapy, often based on growing trial evidence alone rather than routine practice. Rapid intercollegiate and Association of Coloproctology of Great Britain and Ireland guidance based on best available evidence was released on 26–27 March 2020,3,4 advising among others, risk-reducing strategies such as reduced use of chemotherapy and stoma formation to avoid the morbidity of an anastomosis, and the more carefully considered use of laparoscopic surgery.
The impact of COVID-19 has been widespread to all aspects of colorectal cancer care with a sustained reduction in the number of people referred, diagnosed and treated for colorectal cancer.5 The repercussions of these delays are apparent in the increased incidence of high-risk emergency presentations and surgery at a more advanced stage.6
Our study aimed to acquire a snapshot of current MDT practice during the first national lockdown and the reactive response to that guidance.
The primary objective of this study was to determine the variation in adaptive practice for the management of colorectal cancer across England and Wales following the release of initial guidance during the first wave of the COVID-19 pandemic.
Methods
Study design
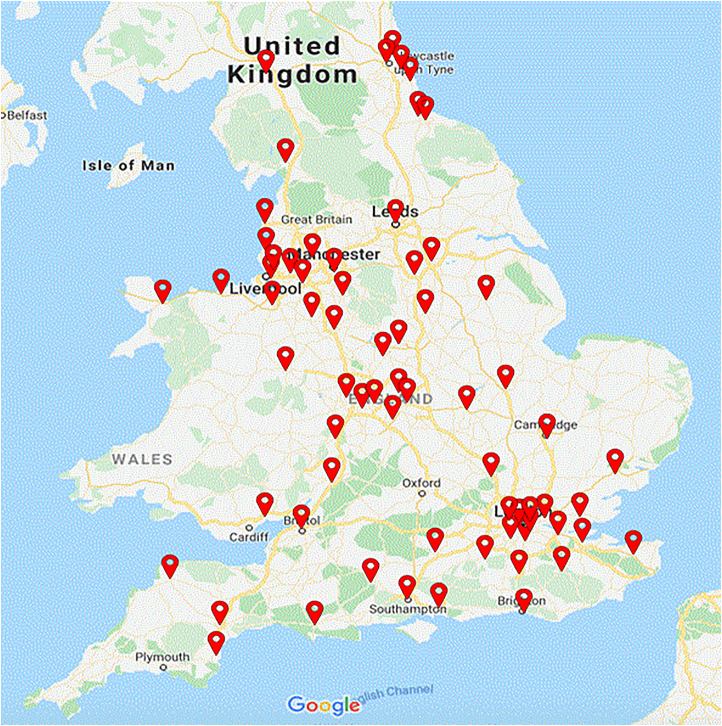
A 12-point electronic survey was designed to ascertain current surgical practice at each individual MDT across the UK. Google Forms was used to collect responses. This survey was disseminated via email to a list acquired from the National Bowel Cancer Audit (NBOCA) database7 of 150 colorectal cancer MDTs in England and Wales for completion by consultant colorectal surgeons. Figure 1 represents a geographical representation of the colorectal cancer MDT locations across England and Wales. Study duration was between 15 April and 30 June 2020. No formal ethical approval was required for the survey.
Figure 1 .
Colorectal cancer multidisciplinary team locations across England and Wales
Inclusion criteria
Each hospital trust with a colorectal cancer MDT across England and Wales was eligible for inclusion. One consultant surgeon response from each MDT was included in the analysis, and data fully anonymised prior to analysis.
Statistical analysis
Data were included from all survey responses, including the eight (11.9%) with incomplete forms, and presented as a percentage of the total responses.
Results
Of 150 colorectal cancer MDTs listed on the NBOCA database, 67 responded to the survey. Table 1 summarises the responses for each specific question.
Table 1 .
Individual multidisciplinary team survey responses between 15 April and 30 June 2020
| Cohort characteristics | n (%) |
|---|---|
| CCR during COVID-19 pandemic (N = 67) | |
| Yes | 57 (85.1) |
| No | 10 (14.9) |
| Preoperative COVID-19 screening (N = 59) | |
| Yes | 50 (84.7) |
| No | 9 (15.3) |
| Full PPE for elective cases (N = 59) | |
| Yes | 50 (84.7) |
| No | 8 (13.6) |
| Only suspected/confirmed cases | 1 (1.7) |
| Planned laparoscopic cases (N = 58) | |
| Performed as laparoscopic | 25 (42.1) |
| Performed as open instead | 28 (48.3) |
| Performed using other approach | 5 (8.6) |
| Complications from CCR (N = 59) | |
| Yes | 7 (11.9) |
| No | 52 (88.1) |
| If cancer resections cancelled, were additional neoadjuvant treatments used | |
| Yes | 24 (38.7) |
| Short-course radiotherapy | 16 (23.9) |
| Chemoradiotherapy | 1 (1.5) |
| Chemotherapy | 1 (1.5) |
| Biological therapy | 1 (1.5) |
| No response | 5 |
| No | 38 (61.3) |
| Cancers re-staged after neoadjuvant therapy (N = 60) | 60 (100) |
CCR = colorectal cancer resections; PPE = personal protective equipment.
Surgical resections
Of the 67 (44.7%) centres responding, 57 stated that they had continued colorectal cancer resections (CCR) to some degree since the date of the first national governmental lockdown (23 March 2020). By contrast, ten (14.9%) trusts ceased performing CCR during same period. For those patients achieving resection, 84.7% underwent preoperative COVID-19 polymerase chain reaction screening in an attempt to reduce respiratory morbidity as per national guidance. Fifty (84.7%) centres were routinely using full personal protective equipment (PPE) for all resections, including a filtering face piece (FFP3) grade mask and eye protection. Only one centre was limiting use to confirmed COVID-19 cases, with the rest (13.6%) having no full PPE requirements.
Fifty-eight (86.6%) centres detailed their surgical approach for cases that would routinely have been performed laparoscopically. Intercollegiate guidance advised caution and careful case selection for the use of aerosol-generating laparoscopic surgery due to the lack of data regarding potential peritoneal expression and risk. Twenty-five (42.1%) centres continued a laparoscopic approach as standard, whereas 28 (48.2%) performed laparotomy and 5 (8.6%) stated an alternative approach had been employed, although they gave no further specific details in the free-text box.
Perioperative risk
While performing CCR during the first wave of the COVID-19 pandemic, seven (11.9%) centres reported experiencing postoperative respiratory complications attributed to COVID-19 infection. Routine re-swabbing detected patients with asymptomatic COVID-19 reported in two (3.3%) centres, which led to no change in patient outcome. Although not specifically questioned, one (1.7%) centre reported those complications in the free-text box to be Clavien–Dindo Grade V.
Resource utilisation
Forty-nine (79%) centres reported experiencing patient-led surgical cancellations in 0–25% of their listings. Additionally, eight centres (13%) experienced 25–50% cancellations due to patient choice, one centre (2%) experienced 50–75% patient cancellations and four centres (6%) reported 75–100% patient cancellations. Figure 2 summarises cancellations for CCR led by patients.
Figure 2 .
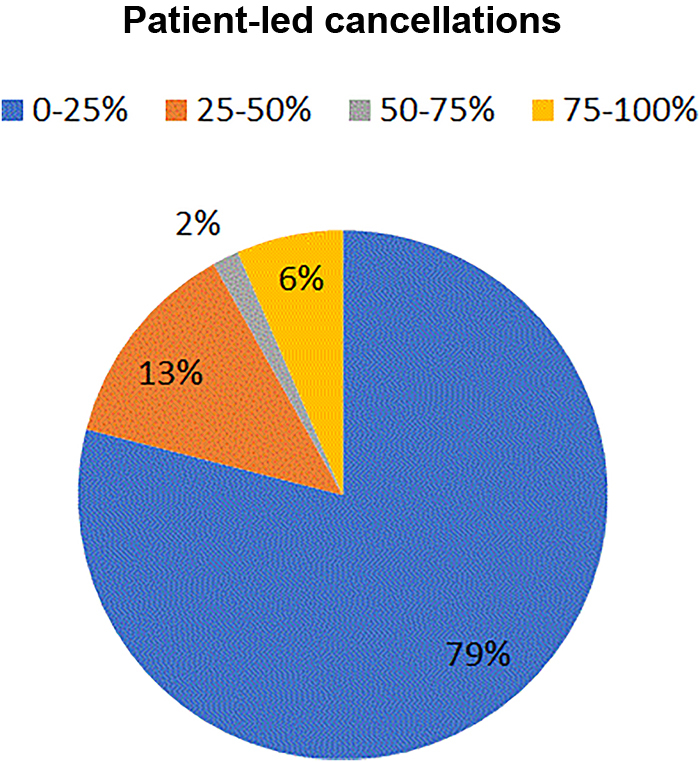
Proportion of colorectal cancer resections cancelled by patients between 15 April and 30 June 2020
If CCR were cancelled due to risk of incurring COVID-19, additional neoadjuvant treatment was started in 24 (38.7%) centres as a preventative measure to try to prevent disease progression. An increase in short-course radiotherapy, recommended by Association of Coloproctology of Great Britain and Ireland (ACPGBI) guidance, was reportedly used by 16 (23.9%) centres, neoadjuvant chemoradiotherapy alone by one (1.5%), chemotherapy by one (1.5%) and biological agents by one (1.5%) centre. All 60 (100%) centres reported continuation of restaging investigations and re-discussion at MDT following an adapted treatment pathway.
Where CCR were not performed, the decision was led by the clinical team in 29 (43.2%) centres (see Figure 3). Twenty (29.9%) centres reported patient choice influencing cancellations and 12 (17.9%) centres experienced managerial-led decision to halt colorectal cancer resections during the first 3 months of the COVID-19 pandemic.
Figure 3 .
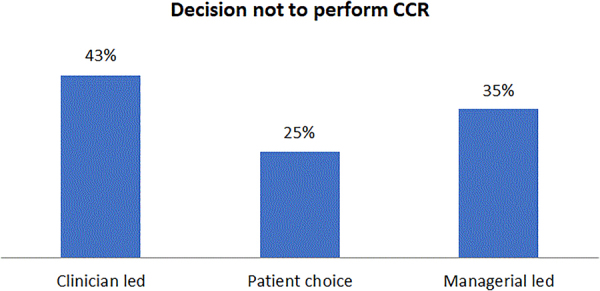
Decision made to cancel colorectal cancer resections (CCR) between 15 April and 30 June 2020
Clinician satisfaction
The final question in the survey assessed clinician-perceived comfort with change in MDT decision-making as a result of COVID-19 lockdown disruption (see Figure 4). Eleven (16.1%) centres reported feeling very uncomfortable, 28 (41.8%) uncomfortable and only 8 (12%) comfortable/very comfortable.
Figure 4 .
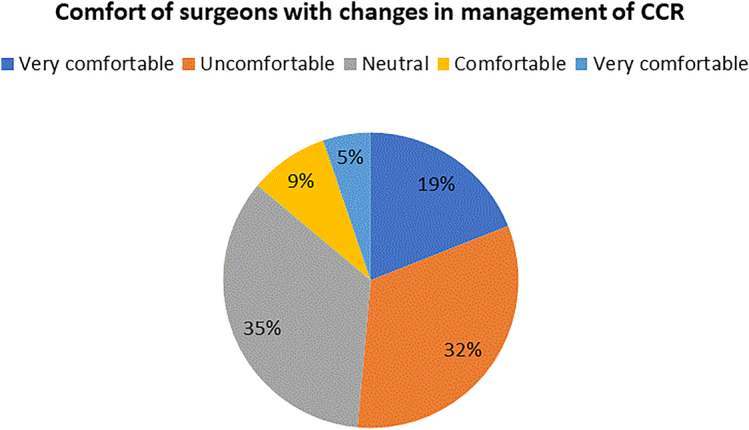
Surgeon comfort with changes in the management of colorectal cancer resections (CCR) from 15 April to 30 June 2020
Discussion
The COVID-19 pandemic has disrupted all facets of human existence. Healthcare systems all over the world continue to face unanticipated challenges leading to rapid responses and changes to standard practice.8 This study was undertaken live during the first lockdown to demonstrate a snapshot of practice across England and Wales, highlighting inter-MDT variation and interpretative responses to the release of national guidance.
Following implementation of the first national governmental lockdown, resource capacity in terms of surgical list availability and surgical staffing changed dramatically to prioritise safe emergency care and COVID-19 burden. This was combined with an increase in personal staff sickness and isolation periods, and significantly reduced critical care availability. There is established evidence of increased time to surgery, and adapted neoadjuvant strategies, alternative surgical approaches and increased stoma formation were employed routinely to reduce patient morbidity and mortality, and minimise resource demand.2,6 There was also, evidenced by this study, a hesitancy among MDTs on the best way to proceed given often limited data and the initial COVIDSurg data demonstrating unacceptable levels of postoperative mortality.8
There are discrepancies noted from our study in inter-MDT consensus on the management of colorectal cancers to suit available resources and expertise. The impact of not having national set guidelines for the management of colorectal cancers made many surgical departments very uncomfortable (as depicted in our survey). National guidelines are important to provide transparency and uniformity for the management of critical conditions in the NHS. However, during the peak of the pandemic, resources were scarce across the UK. This potentially resulted in patients receiving differing levels of care depending on the resources available and the burden of COVID-19 in particular regions. In addition, there were rapid ongoing updates to the national guidelines, which made it difficult for clinicians to keep up-to-date with the ever-changing recommendations.3
A majority (85.1%) of the trusts who responded to the survey reported continuing CCR at their trust during lockdown. Adhering to updated guidance from the ACPGBI,4 precautions were taken where necessary to limit the spread of COVID-19. Because rapid testing was yet to be routinely implemented, full PPE was advised for all cases, particularly for a laparoscopic approach owing to concerns over peritoneal expression and aerosol generation.3 Alternatively, centres chose to perform resections as an open approach, rather than laparoscopically as previously planned, to limit the risk of COVID-19 aerosolisation. It would be beneficial for further studies to review the correlation between local rates of COVID-19 and preferred approach for open resection against laparoscopic surgery.
Although 84.7% of the centres surveyed were using full PPE, for those who were not it would be of interest to assess perioperative COVID-19 rates for both patients and staff and ascertain the variation in local guidance. It would also be interesting to investigate the impact of supply chain disruptions on timely delivery of PPE. This likely affected the use of appropriate PPE and potentially explains the eight centres not donning full PPE during CCR. There were also regional variations in the prevalence of COVID-19, which could have meant the footprint of these MDTs was not affected by higher numbers of COVID-positive patients compared with other trusts. Although local risk assessment for COVID-19 burden, availability of PPE and MDT experience was not analysed, each would certainly have played a role in decision-making for operative timing and approach.
In line with the guidance set out by the ACPGBI,4 centres implemented neoadjuvant therapy with an objective to halt disease progression where cancer resections were unsafe during the pandemic. As a result of these unprecedented times, disruptions in MDT pathways are clearly apparent, with centres using various forms of neoadjuvant therapies such as short-course radiotherapy, chemoradiotherapy, chemotherapy and biological therapy. All centres chose to restage the cancer after neoadjuvant therapy to re-evaluate while taking into consideration the available resources. Studies published by the COVIDSurg collaborative indicate the significantly increased risk of respiratory complications and mortality from incurring COVID-19 following a major operation such as a CCR.8
Interestingly, 49 (79%) of centres reported patient-led cancellations of 0–25%. By contrast, 43% of cancellations of CCR were led by the clinical team. On a risk versus benefit scale, most patients preferred undergoing their cancer resection against the probability of suffering from COVID-19-related complications. The consequences on colorectal services of these cancelled CCR are apparent in the post-lockdown season.6 A significantly higher number of emergency colorectal operations were performed, along with a higher incidence of T4 cancers being diagnosed. An additional contributory factor is the steep reduction in colonoscopies performed during lockdown.6
Perhaps the most interesting result warranting further exploration is the reported surgeon comfort with the forced rapid change in MDT management. Stark changes in terms of neoadjuvant radiotherapy strategies for locally advanced rectal cancer, avoidance of chemotherapy and delay to surgery have an emerging wealth of trial data but are yet to be employed routinely across the country. Further investigation to assess perceptions 12 months on from the start of the first wave, now with first-hand experience of surgical and oncological outcomes, may provide useful qualitative data on the role of trial implementation and anecdotal experience. The impact of formal guidance, an increased wealth of knowledge of the pathophysiology of COVID-19 and ‘cold’ operating sites has significantly evolved our standard practice during this pandemic.
There is lack of comparison data, from COVID-19 being a novel pandemic in the western world. This remains a current limitation of this study. Although survey responses were received from fewer than 50% of the MDTs approached, this number and geographical spread is sufficient to provide a snapshot of practice. The survey outlines the struggles and management strategies implied by individual trusts during the uncertainties of the pandemic. It was not possible for the authors who were actively involved in clinical activities to persevere to obtain all the responses. Equally, it was highly likely that the centres who did not respond had more pressing clinical priorities during the height of the pandemic.
Conclusions
To fully assess the outcomes following change and variation in MDT management strategies long-term, prospective data will need to be assessed to focus upon patient-specific surgical and oncological outcomes. The ReCaP study will aim to address this for patients with rectal cancer, and NBOCA data nationally for both.
References
- 1.Raj Kumar B, Pandey D, Rohila Jet al. An observational study of the demographic and treatment changes in a tertiary colorectal cancer centre. J Surg Oncol 2020; 122: 1271–1275. [DOI] [PubMed] [Google Scholar]
- 2.Glaseby JC, Nepogodiev D, Simoes JFFet al. Elective cancer surgery in COVID-19 free surgical pathways during the SARS-CoV2 pandemic: an international, multicentre, comparative cohort study. J Clin Oncol 2021; 39: 66–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Royal College of Surgeons of England. Updated Intercollegiate General Surgery Guidance on COVID-19. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/ (cited April 2021).
- 4.Nicola Fearnhead N. ACPGBI Guidance for Colorectal Surgeons and Trainees on Rising to the Challenges of COVID-19 as Citizens, Doctors and Surgeons. https://www.acpgbi.org.uk/content/uploads/2020/03/ACPGBI-statement-on-COVID-19.pdf (cited April 2021).
- 5.Morris EJA, Goldacre R, Spata Eet al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet 2021; 6: 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shinkwin M, Silva L, Vogel Iet al. COVID-19 and the emergency presentation of colorectal cancer. Colorectal Dis 2021; 23: 2014–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.https://www.nboca.org.uk/resources/nboca-dataset-2019-2020/ (cited May 2021).
- 8.Glaseby JC, Bhangu Aet al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]