Abstract
Introduction
Aesthetic rhinoplasty remains a challenging procedure with high expectations and narrow tolerance for errors. Considerable training is required to achieve controlled and reliable results. Use of the Piezotome is gaining popularity for performing the nasal osteotomies, a key step in rhinoplasty, where it is reported to improve precision and predictability and to keep tissue damage to a minimum. We compare the outcomes of conventional osteotomy techniques to piezosurgery in human cadavers as undertaken by surgical trainees.
Materials and methods
Seven human cadavers were used and a total of 14 osteotomies were performed. Conventional osteotomies and piezosurgery were carried out each on one side of the cadaver. A number of fragments and a blinded assessment of the accuracy of the osteotomy compared with the preprocedure skin markings were carried out by two experienced rhinoplasty surgeons. The Mann–Whitney test for statistical analysis was used.
Results
The mean number of fragments was 1.57 in the piezosurgery osteotomy and 2.14 using conventional osteotomies. Four of seven piezosurgery osteotomies achieved an accuracy within 1mm. The conventional osteotomies as performed by the trainees showed a significant mismatch of more than 3mm in three of seven of cases. Accuracy within 1mm was achieved in one of seven cases.
Discussion
Piezosurgery offers a safe, reliable and precise method of performing lateral nasal osteotomies. This human cadaver study shows a high accuracy of osteotomy and fewer comminuted fractures using this technique compared with conventional osteotomy techniques.
Keywords: Lateral nasal osteotomy, Piezo surgery, Rhinoplasty, Human cadaver study
Introduction
Aesthetic rhinoplasty is one of the most challenging procedures in facial surgery. Expectations are high and the margin for error is narrow. Exposure and practical hands-on training is difficult to access. Yeolekar et al surveyed experienced rhinoplasty surgeons, who stated that at least 100 cases were required to achieve proficiency because of the complexity of the procedure. Adjuncts to an inevitable learning curve can include watching live operations by experts, specialist fellowships; cadaveric dissections or simulators.1 Several training models have been suggested, including animal and human cadaver training.2,3
Accurate osteotomies are often a key step for a successful operation. Different techniques and instruments have been developed to perform osteotomies in a predictable manner while minimising trauma and tissue damage.4,5 Piezoelectric technology was first described by Horton et al in 1975, when comparing bone healing using piezoelectric drilling or a chisel.6 They then went on to describe the first clinical applications in 1981.7 The technique has become more popular and the indications have been broadened to include oral surgery,8–10 and other surgical fields such as hands,11 spinal decompression,12 otology, skull base, and head and neck surgery.13
The first description of piezoelectric surgery (piezosurgery) for nasal osteotomies was in in 2007.14 Some authors have reported that piezosurgery provides more favourable clinical outcomes, including reduced morbidity within the first week of surgery; less periorbital oedema and pain and fewer mucosal injuries.15,16 One meta-analysis of six studies involving 327 patients found significant reduction in mucosal injuries and oedema and significantly lower pain scores in the first three postoperative days but a longer operating time.17 Histological studies suggest a better microcirculation with a positive effect on bone metabolism.18
Conventional perforated osteotomy was developed to preserve the periosteum and minimise haemorrhage and oedema,4 but this procedure does still cause more damage to the periosteum. Power-driven instruments have the advantage of being quicker, but they may cause coagulative necrosis compared with piezosurgery, keeping the osteocyte microscopically intact.19 Nasal osteotomies are difficult to teach, as they are generally accomplished through tactile feedback.20 Learning tools specifically for osteotomies include simulation or cadaver training programmes on humans, animals or silicone.3,21–24
Yazar et al compared piezosurgery percutaneous and endonasal techniques in a caprine animal model. Their main findings included no comminuted fractures or mucosal defects and a smaller osteotomy gap using piezosurgery.2 Ghassemi et al carried out a cadaver study on 10 human heads comparing osteotomy and a diamond surgical burr, which found precise osteotomies with no mucosal injuries.25
To date, there has been no study comparing conventional osteotomes and piezoelectric osteotomy directly in humans. This human cadaveric study was conducted to directly compare lateral and transverse nasal osteotomies using conventional internal osteotomy techniques and piezosurgery as performed by trainee surgeons.
Materials and methods
Signed informed consent was obtained from donors in their lifetime for the use of their bodies for scientific research. The guidelines of the Helsinki Declaration were followed. Seven human heads were used for a total of 14 lateral nasal osteotomies. One conventional osteotomy and one using piezoelectric osteotomy were performed on each cadaver. All the surgical trainees were senior and had completed or were near the end of their training in plastic surgery. All trainees had previously seen rhinoplasty surgery, but none had previously performed any kind of nasal osteotomy.
Prior to the surgical procedures, participants were given a short lecture on nasal osteotomies. A coin toss was used to randomise the side of the osteotomy on each cadaver head. Trainees then marked on to the overlying skin their planned lateral and transverse osteotomies in order to mobilise the bony pyramid. Medical images were taken to document the preoperative markings (Figure 1).
Figure 1 .
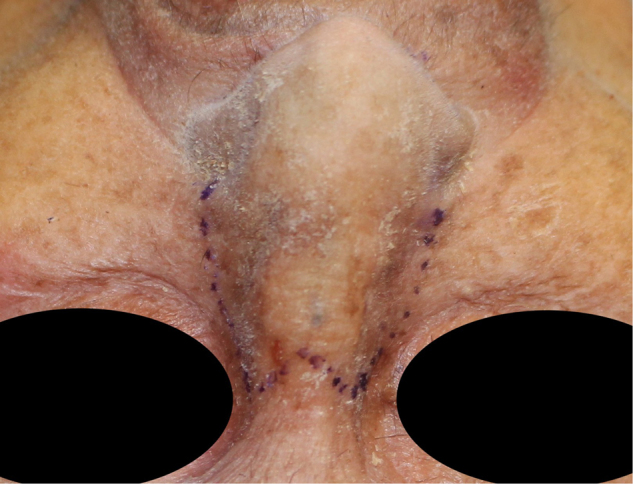
Skin markings for planned osteotomy site. The planned osteotomy course was marked on the skin. One side on each cadaver was used for conventional osteotomy and one for piezosurgery. The number of fragments and accuracy of the final position of the osteotomy were assessed afterwards.
For the conventional osteotomy side, having completed a standard open rhinoplasty exposure, a curved internal osteotome was passed through a separate stab incision at the pyriform aperture and join to the transverse osteotomy superiorly, usually using a greenstick fracture achieved by digital pressure to complete the osteotomy.
For the piezosurgery side, having completed a wider subperiosteal dissection to facilitate insertion of the piezo tip, again transverse and low to low lateral osteotomies were performed. A specific handheld device was used (Mectron Medical Technology, Carasco, Italy, Figures 2 and 3). At completion of their simulated procedure the overlying skin was removed to fully visualise the osteotomies. The procedures were photographed to allow comparison (Figures 4 and 5).
Figure 2 .

Piezotome handpiece (Mectron Medical Technology, Carasco, Italy)
Figure 3 .
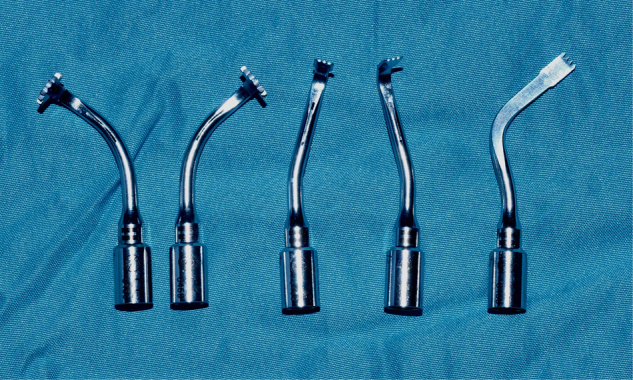
Different designs of cutting tips angled for left- and right-side nasal osteotomy (Mectron Medical Technology, Carasco, Italy)
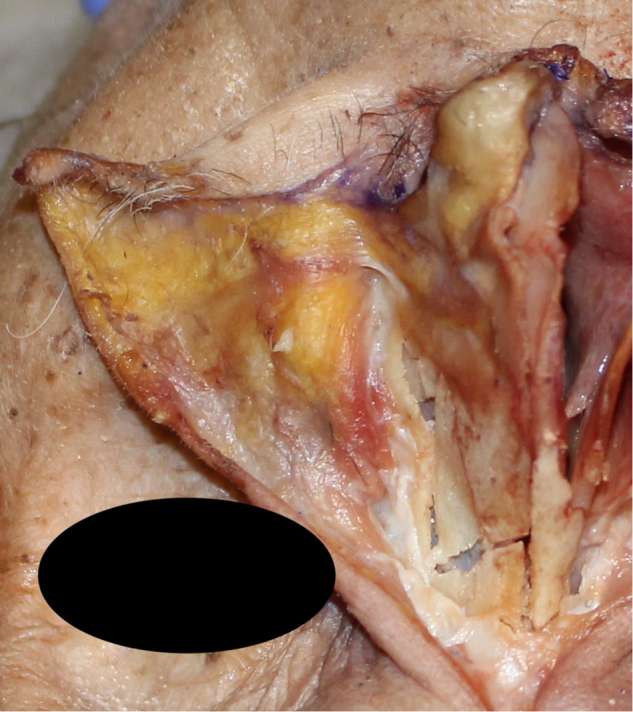
Figure 4 .
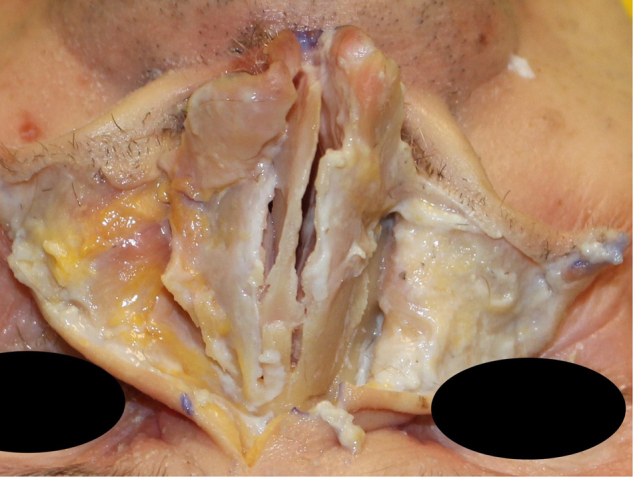
Direct comparison of conventional osteotomy and piezosurgery. The conventional osteotomy on the left side shows an unrounded osteotomy with a bony spike, compared with piezo osteotomy on the right.
Figure 5 .
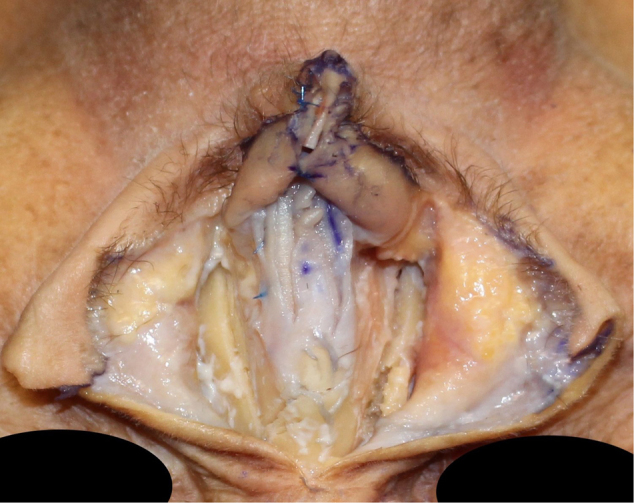
Osteotomy sites exposed after removal of skin. On the left side, the piezo osteotomy shows a precise cut with one fragment. The right side shows a multifragmentation of the osteotomy site.
For assessment of the osteotomy, the number of bony fragments of the conventional and the piezosurgery site were counted. Their accuracy was quantified by blinded assessment using a grading scheme comparing the outcome to the preprocedure skin markings indicating the planned osteotomy site and the final position (Table 1). The blinded assessment was carried out by two consultants experienced in rhinoplasty. Results were statistically analysed using Mann–Whitney test. Significance was defined for p < 0.05 (Graph Pad Prism 8 for Mac).
Table 1 .
Grading scheme for preprocedure skin marking and outcome
| Grade | Description |
|---|---|
| 1 | Complete match of skin markings and osteotomy (within 1mm) |
| 2 | Close match; all osteotomies within 1–2mm |
| 3 | Fair match; all osteotomies within 2–3mm |
| 4 | Poor match; any osteotomies > 3mm |
Results
The average number of bony fragments using piezosurgery was 1.57, while the mean number of fragments on the conventional osteotomy site was 2.14 (Table 2, Figures 6 and 7). No piezosurgery-conducted osteotomy exceeded more than two fragments (Table 2, Figures 6 and 8). This did not, however, reach statistical significance (p = 0.108). The mean graded accuracy of the piezosurgery score was 1.43 and the conventional osteotomy mean score was 2.86, which was statistically significant (p = 0.046); Figure 9).
Table 2 .
Number of bony fragments and accuracy of osteotomy associated with piezosurgery and conventional nasal osteotomy
| Participants (n) | Bony fragments (n) | Blinded assessments of accuracy of osteotomy (n) | ||
|---|---|---|---|---|
| 1 | 1 | 2 | 1 | 2 |
| 2 | 2 | 3 | 2 | 4 |
| 3 | 1 | 2 | 1 | 2 |
| 4 | 2 | 2 | 2 | 4 |
| 5 | 2 | 2 | 2 | 4 |
| 6 | 2 | 3 | 1 | 3 |
| 7 | 1 | 1 | 1 | 1 |
| Mean | 1.57 | 2.14 | 1.43 | 2.86 |
| p-value | 0.1089 | 0.0466 | ||
Figure 6 .
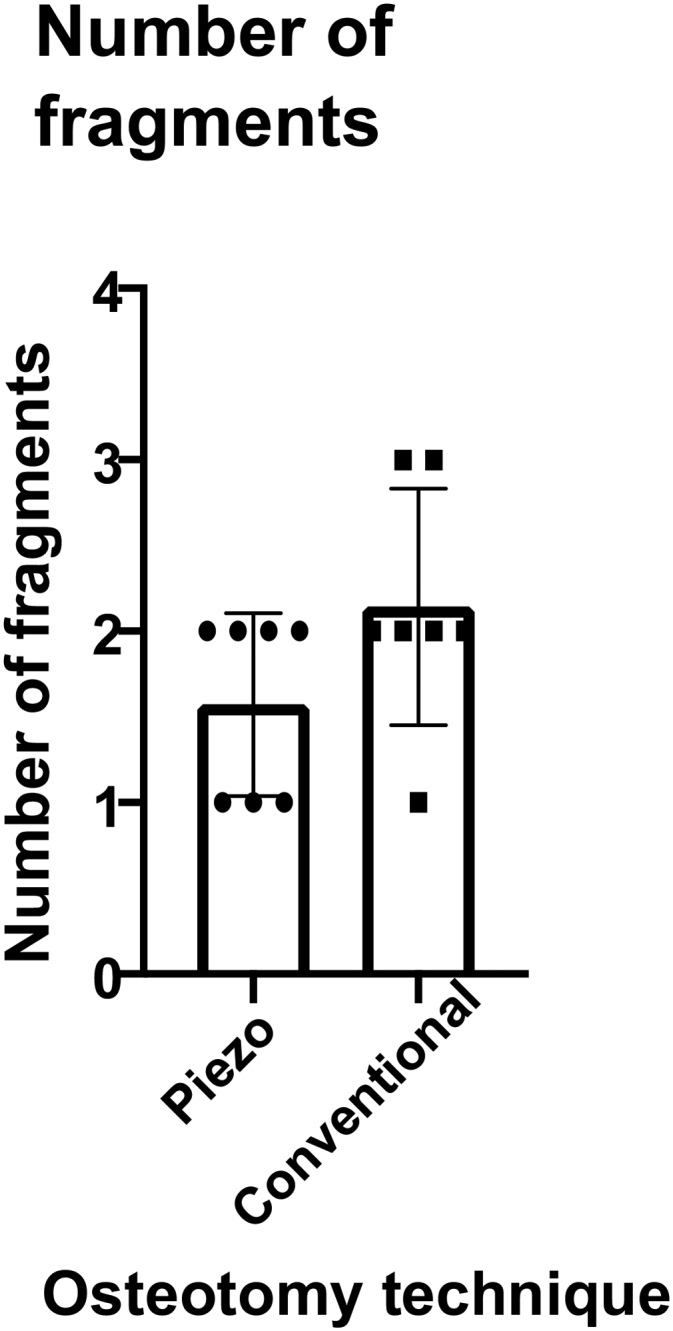
Comparison of the number of fracture fragments of piezosurgery and conventional osteotomy. The average number of fragments was 1.57 in the piezosurgery group and 2.14 in the conventional group.
Figure 7 .
Detailed view of the conventional osteotomy of the same patient as shown in Figures 6. Multifragmentation at the osteotomy and unfavourable fracture at the cranial site.
Figure 8 .
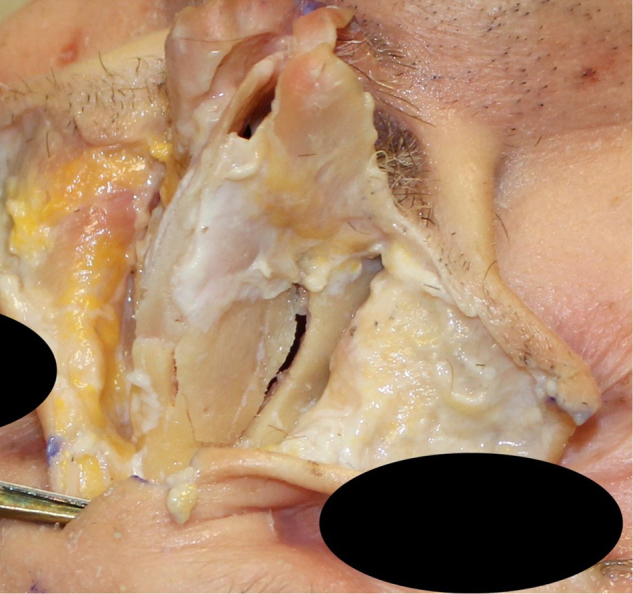
Detailed view of the piezo osteotomy, showing a clean single fragment
Figure 9 .
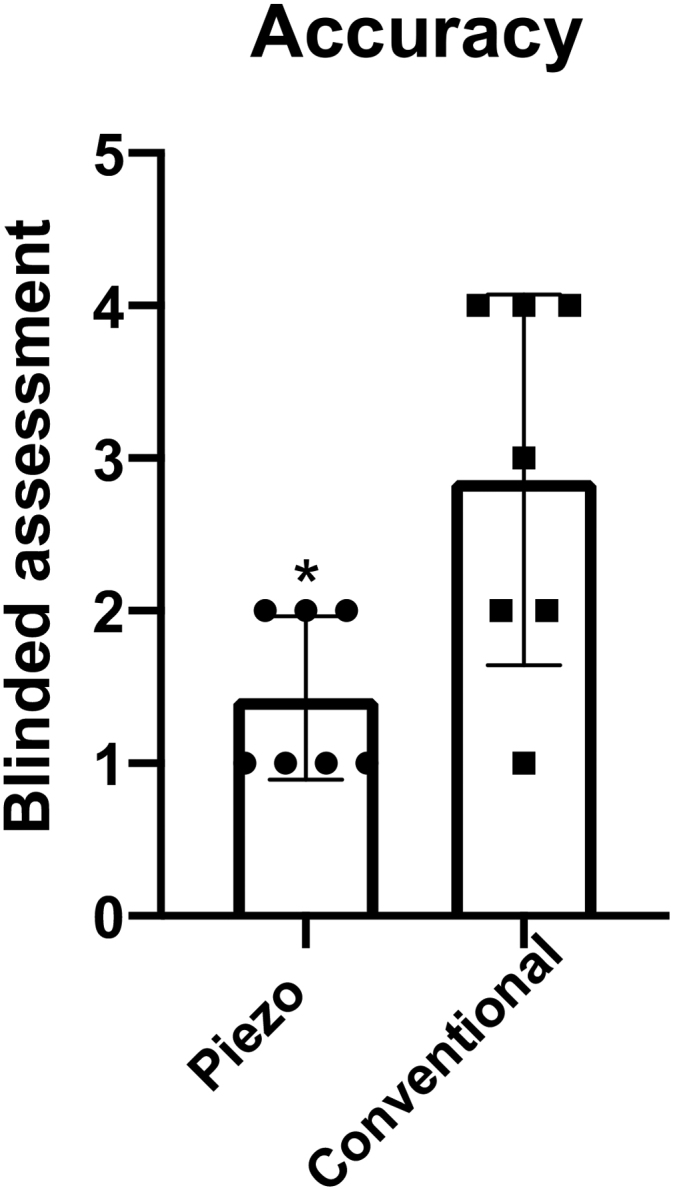
Comparison of the accuracy of planned osteotomy using skin markings and assessment of the final position using a grading scheme (Table 1). The average accuracy in the piezosurgery was 1.43 and 2.86 in the conventional group. The difference was significant.
Discussion
Nasal osteotomy remains a challenging task and a key procedure in rhinoplasty. The technique used should cause minimal tissue damage and should be precise and reliable to achieve controlled changes of the nasal framework.26 Several osteotomy techniques and instruments have been described and have been compared.4,6,27 Gaining experience in this key step of the procedure without compromising real-life surgical outcomes can be difficult. Recent studies have shown that piezosurgery is a safe and reliable method for nasal osteotomy, which causes little tissue damage and heals well.18 A comparison of the outcomes on a training/cadaver model have not been previously described.
The aim of this human cadaver study was to perform a direct comparison of a conventional internal osteotomy technique and piezosurgical osteotomy as performed by surgical trainees on a cadaveric rhinoplasty course. The rationale for involving trainees was twofold. First, the study model should rule out the bias towards conventional osteotomies carried out by experienced surgeons. Second, it allows assessment of how safely and precisely lateral osteotomies using the Piezotome may be performed by trainees, even with limited experience. The results show significantly higher accuracy of osteotomy as performed by surgical trainees using piezosurgery. The mean accuracy grading was 1.43, with more than half of all osteotomies completed within 1mm of the planned position. The remaining osteotomies were within 2mm. The conventional osteotomies were far less accurate, with an average blinded accuracy grading of 2.86. The numbers of fragments were not statistically significant. Piezosurgery showed a single fragment in about three of seven osteotomies, compared with only one conventional osteotomy.
Conventional perforated lateral osteotomies have been demonstrated to preserve the periosteum, which supports the lateral nasal wall from collapse and reduces haemorrhage and oedema.28 Rohrich et al identified 74% mucosal injuries in the continuous technique and 11% when using the perforated technique.29
Ghassemi et al performed lateral osteotomies using piezosurgery with an endonasal approach. They showed no mucosal injuries using piezosurgery and reported high accuracy with no comminuted fractures in 20 osteotomies, but the authors did not report specific numbers of fragments.25 They achieved a single fragment using a diamond burr compared with an osteotome.27 Another comparative study using caprine skulls demonstrated no comminuted fractures or mucosal defects using piezosurgery compared with endonasal or percutaneous conventional osteotomy techniques.2 Soft tissue injury, haemorrhage and ecchymosis were observed less frequently by Robiony et al, using piezosurgery in rhinoplasty compared with other techniques.14 Tirelli conducted postoperative evaluation on 22 patients after performing lateral wall osteotomies on 12 patients with conventional method and 10 using piezosurgery. There was significantly less pain, oedema and ecchymosis, as well as fewer mucosal injuries, in the piezosurgery group.16 A meta-analysis also showed significantly lower oedema and ecchymosis score.15 It is also well suited to cutting selectively mineralised tissue. Good healing potential was observed.6 Piezosurgery has a steep learning curve; Ghassemi et al reported an operative time of ten minutes for the first nose, seven minutes for the second, while the following eight noses required five minutes.27
The limitations of this study clearly include the small numbers but, despite this, we have shown a statistically significant greater degree of accuracy of the osteotomy for novice rhinoplasty surgeons and, while not statistically significant in this small study, there were also fewer bone fragments. Additionally, these osteotomies were performed on cadavers and it could be argued that different results may be seen in live patients. It remains to be seen whether this translates to greater accuracy in patients but use of the Piezotome is increasing among rhinoplasty surgeons and training models are increasingly important for newer surgeons to gain experience. As mentioned, rhinoplasty needs a large number of cases to gain proficiency. The logical next step could be a study model involving a greater number of trainees doing osteotomies on several cadavers sequentially to investigate the comparative learning curves, both in speed and precision, between the conventional technique and the Piezotome.
Acknowledgements
We would like to thank the team from the anatomy department at Guy’s and St Thomas’, Hospital for their help with the human cadavers. Further we thank Device Technologies for the loan of the Piezotome and for providing the surgical kit for the study.
References
- 1.Yeolekar A, Qadri H. The learning curve in surgical practice and its applicability to rhinoplasty. Indian J Otolaryngol Head Neck Surg 2018; 70: 38–42. 10.1007/s12070-017-1199-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yazar S Kurt, Serin M, Rakici IT. et al. Comparison of piezosurgery, percutaneous osteotomy, and endonasal continuous osteotomy techniques with a caprine skull model. J Plast Reconstr Aesthet Surg 2019; 72: 107–113. 10.1016/j.bjps.2018.08.025 [DOI] [PubMed] [Google Scholar]
- 3.Jacovella PF. Developing skills in rhinoplasty through cadaver training. Aesthet Surg J 2005; 25: 643–645. 10.1016/j.asj.2005.09.007 [DOI] [PubMed] [Google Scholar]
- 4.Gryskiewicz JM, Gryskiewicz KM. Nasal osteotomies: a clinical comparison of the perforating methods versus the continuous technique. Plast Reconstr Surg 2004; 113: 1445–1458. 10.1097/01.PRS.0000113031.67600.B9 [DOI] [PubMed] [Google Scholar]
- 5.Harshbarger RJ, Sullivan PK. The optimal medial osteotomy: a study of nasal bone thickness and fracture patterns. Plast Reconstr Surg 2001; 108: 2114–2121. 10.1097/00006534-200112000-00049 [DOI] [PubMed] [Google Scholar]
- 6.Horton JE, Jr Tarpley TM, Wood LD. The healing of surgical defects in alveolar bone produced with ultrasonic instrumentation, chisel, and rotary bur. Oral Surg Oral Med Oral Pathol 1975; 39: 536–546. 10.1016/0030-4220(75)90192-9 [DOI] [PubMed] [Google Scholar]
- 7.Horton JE, Jr Tarpley TM, Jacoway JR. Clinical applications of ultrasonic instrumentation in the surgical removal of bone. Oral Surg Oral Med Oral Pathol 1981; 51: 236–242. 10.1016/0030-4220(81)90051-7 [DOI] [PubMed] [Google Scholar]
- 8.Vercellotti T. Piezoelectric surgery in implantology: a case report – a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent 2000; 20: 358–365. [PubMed] [Google Scholar]
- 9.Vercellotti T, De Paoli S, Nevins M. The piezoelectric bony window osteotomy and sinus membrane elevation: introduction of a new technique for simplification of the sinus augmentation procedure. Int J Periodontics Restorative Dent 2001; 21: 561–567. [PubMed] [Google Scholar]
- 10.Rullo R, Addabbo F, Papaccio G. et al. Piezoelectric device vs. conventional rotative instruments in impacted third molar surgery: relationships between surgical difficulty and postoperative pain with histological evaluations. J Craniomaxillofac Surg 2013; 41: e33–e38. 10.1016/j.jcms.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 11.Hoigne DJ, Stubinger S, Von Kaenel O. et al. Piezoelectric osteotomy in hand surgery: first experiences with a new technique. BMC Musculoskelet Disord 2006; 7: 36. 10.1186/1471-2474-7-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bydon M, Xu R, Papademetriou K. et al. Safety of spinal decompression using an ultrasonic bone curette compared with a high-speed drill: outcomes in 337 patients. J Neurosurg Spine 2013; 18: 627–633. 10.3171/2013.2.SPINE12879 [DOI] [PubMed] [Google Scholar]
- 13.Meller C, Havas TE. Piezoelectric technology in otolaryngology, and head and neck surgery: a review. J Laryngol Otol 2017; 131(Suppl 2): S12–S18. 10.1017/S0022215117000767 [DOI] [PubMed] [Google Scholar]
- 14.Robiony M, Toro C, Costa F. et al. Piezosurgery: a new method for osteotomies in rhinoplasty. J Craniofac Surg 2007; 18: 1098–1100. 10.1097/scs.0b013e3180de6489 [DOI] [PubMed] [Google Scholar]
- 15.Mirza AA, Alandejani TA, Al-Sayed AA. Piezosurgery versus conventional osteotomy in rhinoplasty: A systematic review and meta-analysis. Laryngoscope 2020; 130: 1158–1165. 10.1002/lary.28408 [DOI] [PubMed] [Google Scholar]
- 16.Tirelli G, Tofanelli M, Bullo F. et al. External osteotomy in rhinoplasty: piezosurgery vs osteotome. Am J Otolaryngol 2015; 36: 666–671. 10.1016/j.amjoto.2015.05.006 [DOI] [PubMed] [Google Scholar]
- 17.Kim DH, Kang H, Jin HJ, Hwang SH. Effect of piezoelectric osteotomy on postoperative oedema and ecchymosis after rhinoplasty. Clin Otolaryngol 2019; 44: 968–974. 10.1111/coa.13415 [DOI] [PubMed] [Google Scholar]
- 18.Stoetzer M, Felgentrager D, Kampmann A. et al. Effects of a new piezoelectric device on periosteal microcirculation after subperiosteal preparation. Microvasc Res 2014; 94: 114–118. 10.1016/j.mvr.2014.06.003 [DOI] [PubMed] [Google Scholar]
- 19.Salami A, Dellepiane M, Crippa B, Mora R. A new method for osteotomies in oncologic nasal surgery: Piezosurgery. Am J Otolaryngol 2010; 31: 150–153. 10.1016/j.amjoto.2008.12.001 [DOI] [PubMed] [Google Scholar]
- 20.Chen JX, Kozin ED, Dedmon MM, Lee LN. Teaching and practice patterns of lateral osteotomies for rhinoplasty. Am J Otolaryngol 2017; 38: 498–500. 10.1016/j.amjoto.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 21.Sheckter CC, Kane JT, Minneti M. et al. Incorporation of fresh tissue surgical simulation into plastic surgery education: maximizing extraclinical surgical experience. J Surg Educ 2013; 70: 466–474. 10.1016/j.jsurg.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 22.Dini GM, Gonella HA, Fregadolli L. et al. Training rhinoseptoplasty, sinusectomy, and turbinectomy in an animal model. Plast Reconstr Surg 2012; 130: 224e–e226e. 10.1097/PRS.0b013e318255021e [DOI] [PubMed] [Google Scholar]
- 23.Weinfeld AB. Chicken sternal cartilage for simulated septal cartilage graft carving: a rhinoplasty educational model. Aesthet Surg J 2010; 30: 810–813. 10.1177/1090820X10386945 [DOI] [PubMed] [Google Scholar]
- 24.Zabaneh G, Lederer R, Grosvenor A, Wilkes G. Rhinoplasty: a hands-on training module. Plast Reconstr Surg 2009; 124: 952–954. 10.1097/PRS.0b013e3181b17bf5 [DOI] [PubMed] [Google Scholar]
- 25.Ghassemi A, Prescher A, Talebzadeh M. et al. Osteotomy of the nasal wall using a newly designed piezo scalpel–a cadaver study. J Oral Maxillofac Surg 2013; 71: 2155.e1-6. 10.1016/j.joms.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 26.Thomas JR, Griner NR, Remmler DJ. Steps for a safer method of osteotomies in rhinoplasty. Laryngoscope 1987; 97: 746–747. 10.1288/00005537-198706000-00021 [DOI] [PubMed] [Google Scholar]
- 27.Ghassemi A, Ayoub A, Modabber A. et al. Lateral nasal osteotomy: a comparative study between the use of osteotome and a diamond surgical burr – a cadaver study. Head Face Med 2013; 9: 41. 10.1186/1746-160X-9-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldfarb M, Gallups JM, Gerwin JM. Perforating osteotomies in rhinoplasty. Arch Otolaryngol Head Neck Surg 1993; 119: 624–627. 10.1001/archotol.1993.01880180038006 [DOI] [PubMed] [Google Scholar]
- 29.Rohrich RJ, Minoli JJ, Adams WP, Hollier LH. The lateral nasal osteotomy in rhinoplasty: an anatomical endoscopic comparison of the external versus the internal approach. Plast Reconstr Surg 1997; 99: 1309–1313. 10.1097/00006534-199705000-00015 [DOI] [PubMed] [Google Scholar]


