Abstract
Kikuchi–Fujimoto is a rare but self-limiting disease usually affecting young ethnic females. The main clinical presentation is fever and cervical lymphadenopathy. Here we describe the cases of two patients with cervical lymphadenopathy, fever and fatigue. In addition, patients can present with neutropenia; hence, early diagnosis is crucial to exclude a malignant cause.
Keywords: Cervical lymphadenopathy, Kikuchi–Fujimoto disease, Necrotising lymphadenitis
Background
Cervical lymphadenopathy is a common clinical presentation. It has multiple differential diagnoses including malignancy, bacterial and viral infection, and autoimmune disorders such as systemic lupus erythematosus (SLE).1 In rare cases, patients may have Kikuchi–Fujimoto disease.
Kikuchi–Fujimoto disease was first described in 1972 by Kikuchi and Fujimoto in Japan.2,3 It has since been reported worldwide, although it is more common in Asian women.1 Kikuchi–Fujimoto disease is a benign, self-limiting condition causing histiocytic necrotising lymphadenopathy.1 The aetiology remains largely unknown; however, in patients presenting with cervical lymphadenopathy, it is an important differential to ensure early diagnosis and effective management. Here, we present two cases of Kikuchi–Fujimoto disease in young women.
Case reports
Case 1
A 24-year-old woman of East Asian descent was referred to the Oral and Maxillofacial Surgery (OMFS) unit presenting with a non-tender 4cm left neck lump and fatigue. Bilateral cervical lymphadenopathy was also noted. Blood and microbiology screening was unremarkable. An ultrasound scan excluded tuberculosis, sialadenitis and a suspected lymphoproliferative disorder. A core biopsy was performed, which excluded infection and malignancy. Additional node involvement and a lack of diagnosis resulted in the need for open excisional biopsy. The slides were reviewed by a tertiary unit and revealed a large number of histiocytes and necrosis (Figure 1). Immunohistochemistry highlighted CD68-positive histiocytes. This suggests a reactive process, in keeping with a diagnosis of Kikuchi–Fujimoto disease. At 3 months, the cervical lymphadenopathy resolved, although the patient reported continuing episodes of fatigue.
Figure 1 .
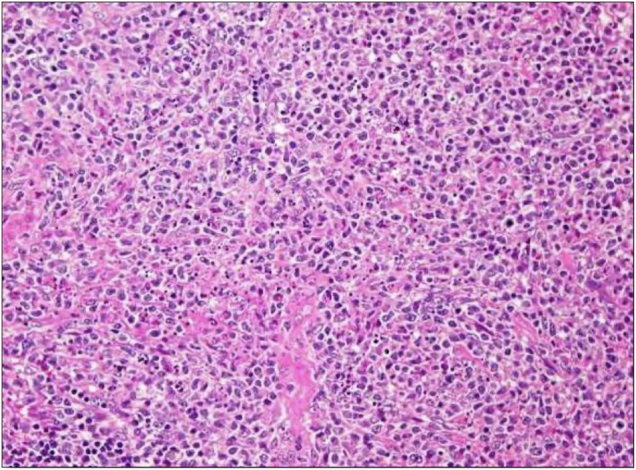
Histology showing abundant histiocytes and necrosis
Case 2
A 31-year-old woman of South Asian descent presented with acute onset tender right neck lump, fatigue and fever. She was treated with multiple courses of antibiotics in primary care for a suspected dental abscess prior to referral to the OMFS unit.
Initial clinical examination and radiographs excluded a dental cause. A magnetic resonance imaging (MRI) scan showed bilateral cervical lymphadenopathy, likely to be reactive, with no evidence of malignancy. Bloods showed neutropenia and elevated C-reactive protein; microbiology was unremarkable. An ultrasound-guided core biopsy showed histiocytes and necrosis with karyorrhectic, apoptotic debris. Immunohistochemistry identified CD3- and CD5-positive T cells, and histiocytes stained for CD68. Ki-67 antigen showed increased proliferation, suggestive of Kikuchi–Fujimoto disease. The patient was managed conservatively with anti-inflammatory medication. At 9 months follow up, the patient was asymptomatic.
Discussion
Kikuchi–Fujimoto disease is a rare, self-limiting condition that should be considered as an important differential for patients presenting with cervical lymphadenopathy. A combination of history, background, clinical examination, imaging, histology and immunohistochemistry is essential for accurate diagnosis.
The most common clinical manifestation of Kikuchi–Fujimoto disease is acute onset cervical lymphadenopathy, as seen in both our cases. Other presentations include weight loss, nausea, vomiting, night sweats, generalised lymphadenopathy, hepatosplenomegaly, joint pain and cutaneous involvement: disseminated erythema and urticarial rashes.4 Thorough investigation is crucial to rule out differential diagnoses of these non-specific signs and symptoms.
Although not well described, there are two main hypotheses regarding the aetiology of the disease. First, there is a possible link to a bacterial, viral or parasitic infection.1 This is illustrated by the raised inflammatory markers and imaging findings in Case 2. Second, there may be an association with autoimmune disorders such as SLE and rheumatoid arthritis.1
A physical examination will indicate cervical lymphadenopathy.5 Imaging, including MRI and ultrasound scans, are then used to confirm lymph node enlargement.5 The cases described here highlight the importance of early core or excisional biopsy when imaging is inconclusive.5 Histological examination from solid tissue biopsy will reveal paracortical expansion with areas of necrosis containing karyorrhectic nuclear debris and histiocytes with three stages, proliferative, necrotising and xanthomatous, with the absence of granulocytes being an important feature.4 Immunohistochemistry can be performed to support morphological findings. The presence of lysosome, myeloperoxidase, CD3-positive CD8 T cells, or histiocytes expressing CD68, CD163 or CD4 indicate a positive result.4
Kikuchi–Fujimoto disease does not alter life span and, in most cases described in the literature, resolves spontaneously with supportive treatment.5 However, some patients may later go on to develop autoimmune diseases such as SLE. There are no universally accepted management guidelines and, because there is no cure, treatment focuses on symptom relief. Treatment options include non-steroidal anti-inflammatory drugs, steroids for severe cases and potentially immunoglobulin or hydroxychloroquine.5
In young female patients of Asian origin presenting with cervical lymphadenitis and fever, physicians should consider Kikuchi–Fujimoto disease as a differential. However, alternative differentials for the non-specific symptoms of Kikuchi–Fujimoto disease have variable, and in some cases invasive, management options. Misdiagnosis of malignancy or infection is detrimental to patient health and increases patient mortality due to administration of inappropriate treatments. Therefore, it is important to raise awareness of Kikuchi–Fujimoto disease to facilitate appropriate investigation and accurate diagnosis.
References
- 1.Lahma J, Arkoubi Z, Hejjouji Ret al. About a rare disease misdiagnosed as malignant lymphoma or tuberculosis: Kikuchi–Fujimoto’s disease. Pan Afr Med J 2018; 31: 77. 10.11604/pamj.2018.31.77.16569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fujimoto Y, Kojima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis: a new clinicopathological entity. Nippon Naika Gakkai Zasshi 1972; 20: 920–927. [Google Scholar]
- 3.Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytosis. Nippon Ketsueki Gakkai Zasshi 1972; 35: 379–380. [Google Scholar]
- 4.Perry AM, Choi SM. Kikuchi–Fujimoto disease: a review. Arch Pathol Lab Med 2018; 142: 1341–1346. 10.5858/arpa.2018-0219-RA [DOI] [PubMed] [Google Scholar]
- 5.Xu S, Sun W, Liu J. Kikuchi–Fujimoto disease: a case report and the evaluation of diagnostic procedures. BMC Oral Health 2019; 19: 223. 10.1186/s12903-019-0920-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


