The enormity of climate change can leave us feeling paralysed and uncertain where to direct our efforts, including how to reduce the environmental harms of healthcare. Many have enthusiastically asked me how they can start carbon footprinting aspects of care: I both encourage and discourage them. We can and should make approximations of environmental harm in what we do, but to accurately and comprehensively conduct a full life-cycle analysis of a product or process is a complex science, and in fact we already have enough evidence to know some of the principles we should follow.

Professor Mahmood F Bhutta is Chair in ENT at Brighton & Sussex Medical School and Honorary ENT Consultant & Clinical Green Lead at University Hospitals Sussex.
It is a fair approximation (and perhaps self-evident) that carbon footprint is proportional to the activity associated with a process or product. We can reduce activity in care pathways: for example through engaging with public health to prevent patients getting surgical disease,1 using remote consultation to eliminate patient travel,2 or minimising blood tests in the perioperative period.3,4 But of course, we will still be performing surgery, and in the operating theatre too we can have a big impact: in particular through reducing our reliance on single-use equipment.
The carbon footprint of equipment in the operating theatre
A typical operation in the UK has a carbon footprint of 173kgCO2e,5 equivalent to driving from London to Edinburgh in a petrol car. Major contributors to that carbon footprint include energy use and anaesthetic gases,6 but most UK hospitals are now transitioning to renewable energy sources and most of our anaesthetic colleagues have minimised or eliminated agents with potent greenhouse gas potential, such as desflurane and nitrous oxide.7 The other major carbon hotspot of an operation is single-use equipment, but to date our surgical community has afforded this little attention.
The amount of single use equipment in the operating theatre can be phenomenal, with theatres typically accounting for a quarter of all hospital waste.6 Even a simple tonsillectomy can generate over 100 pieces of disposable plastic.8 The manufacture and transport of a piece of equipment often generates a lot of carbon, so using it only once is understandably bad for our planet. And as we have adopted increasingly complex surgical systems, our use of single use equipment has also proliferated. A typical cataract operation in the UK generates 182 kgCO2e,9 but in India the same operation generates only 6 kgCO2e,10 with that 30-fold reduction largely accounted for by efficient systems and re-use of equipment. In the USA, a vaginal or abdominal hysterectomy generates around 280-290 kgCO2e, whereas a laparoscopic approach generates around 560 kgCO2e and a robotic hysterectomy over 800 kgCO2e, with that variation again almost entirely due to single-use equipment.11
There may be good clinical reasons to prefer one surgical approach over another, but it does not follow that we need to use huge volumes of single-use equipment. And just to be up front, recycling alone is not the answer to this problem: it should be promoted, but even with perfect use it would reduce the carbon footprint of a hysterectomy by less than 5%.12
Why do we use so many single-use items?
It may seem easy for surgeons to excuse ourselves on this agenda on notions of “quality” or “safety”, but there is really no evidence to support this.
The move to single use products gained traction following discovery in 1996 of variant Creutzfeld-Jakob Disease (vCJD), an incurable disease caused by transmissable misfolded proteins (prions) that in genetically susceptible individuals fatally accumulate in and damage the brain. At that time, UK practice around cleaning and sterilisation of surgical instruments was inconsistent and often inadequate,13 and a policy supporting single-use rather than re-use of instruments seemed an appropriate precaution against an uncertain risk. However, the world has moved on: under current UK regulations, all instruments are sterilised to robust and audited standards.14 Where transmission of infection has historically been documented, it had been using processes inconsistent with such standards,15 and there have been no definite recorded cases of surgically transmitted vCJD disease since exposures that occurred in the 1970s.16 In fact, many single-use items are sterilised outside of the UK, where standards may be less verifiable: recently the Italian company Steril Milano (no longer trading) was reported to have falsified data on sterilisation of products for at least 97 brands,17 including many used in the UK.
The reputation of reusable hospital linens as a potential infection risk is also historical, with older studies analysing textiles not manufactured or quality assured to modern requirements.18 In a recent report of medical gowns, single-use versions were found to have lower barrier protection than reusable equivalents.19 This fact, coupled with UK standards and assurances for decontamination of linens,20 makes for a compelling argument that we should be using reusable rather than single-use drapes and gowns if we want to reduce risk of infection.
Myths, deceptive marketing and unhealthy supply chains
The events of the 1990s kick-started the market for single-use medical products, but it has grown, perpetuated by misguided cultures of practice.
The myth that disposable items reduce infection risk seem to still be present. Yet in a study of over 2 million cataract operations performed in India predominantly using reuseable equipment, rates of infective endophthalmitis were significantly lower than those reported in the UK (where single-use products are routinely used).21
There is also a myth that single-use items cost less to the environment or our purse than reusable. In many circumstances, and on first principles, this is plain nonsense. If I place a metal gallipot within a surgical tray it will be sterilised with that tray, with negligible additional environmental or financial cost, yet many of us routinely use plastic gallipots. But even outside that context, reuse is almost always preferable: a recent systematic review found reusable medical products associated with less environmental harm than single-use equivalents in just about every reported instance,22 with one notable exception being an industry sponsored study where methodology was unclear.
And that brings us to the industry. Let us not forget that the linear (single-use) model of consumption is the backbone of capitalism and profitable for companies. Deception, even if subtle, is a well-rehearsed strategy for marketing.23 The market for medical products is unique in that the end-user (patient) is separate to the consumer (the surgeon) who in turn is separate to the payer (the health facility).24 It would be naïve to think that companies do not know how to exploit that space of differing drivers and priorities, where the winner is the one who dupes an unsuspecting and uninformed surgeon into thinking a single-use product is better. My colleague was recently asked by a company rep “aren’t you worried about infection when you use a reuseable endoscope?”. I suggested in return he ask the rep for the data that informed his scientific critique of the issue: that was not forthcoming.
And we should also remember that where we are being sold single-use products in quantity, price becomes key and can perpetuate other harms. To reduce costs, the production of many medical goods exploits the sorts of global value chains described for other manufactured products such as clothing: many of our surgical instruments are produced in sweatshops in Pakistan,25 most gloves are manufactured using forced immigrant labour in Malaysia,26 and some of our gowns and masks are made using state-sponsored modern slavery in China.27
The way forward
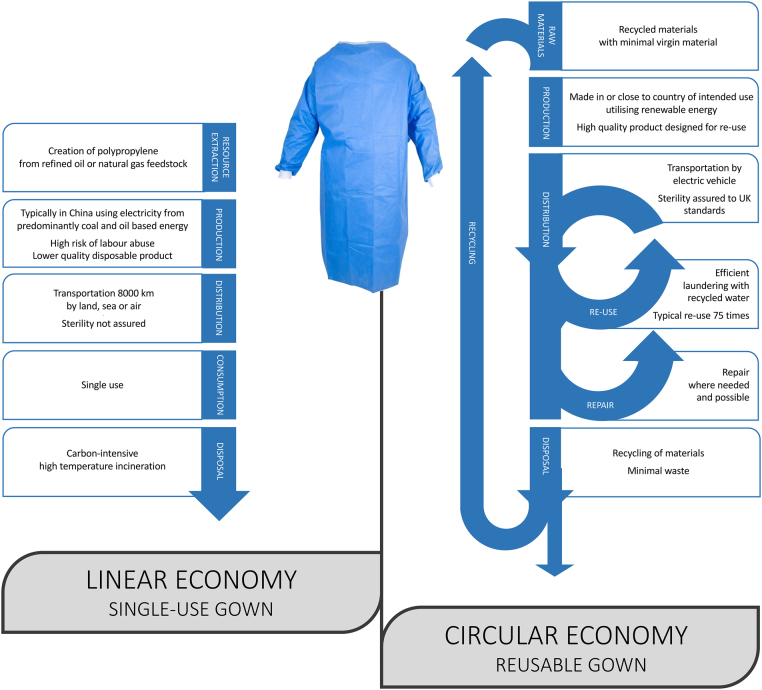
Our over-reliance on single use equipment in the operating theatre is an archetypal example of the linear model of consumption and shows contempt for our planet. Except where there really is no alternative, everything we use in the operating theatre should align with the principles of a circular economy (figure 1).
Figure 1 .
Principles of a linear versus circular economy, illustrated for a single-use versus reuseable gown. Data sources: 27,31,32,33,34.
To make change will require many things. Maturity in our approach to using equipment: could I really do without that thing for my operation (those who have operated in low resource settings know that often the answer is yes) and could I do this procedure under local anaesthetic (reducing the environmental costs of anaesthetic equipment)? Industry will need to design and manufacture long-lasting products designed for reuse (especially because current UK regulations prohibit reuse of single-use items,28) or where that is difficult, hybrids of reusable and disposable products (eg for laparoscopic instruments.29) We need expansion of UK infrastructure to sterilise, maintain and repair equipment. And we need maturity in health economics that recognises investment above meeting short-term financial targets.
The UK government has recently announced changes to public procurement which will hopefully financially incentivise the healthcare industry to decarbonise their products.30 Let’s match that with leadership and behaviour change in the operating theatre, to reduce what we use, and to reuse wherever we can.
References
- 1.Rizan C, Bhutta MF. Strategy for net-zero carbon surgery. Br J Surg 2021; 108: 737–9. [DOI] [PubMed] [Google Scholar]
- 2.Purohit A, Smith J, Hibble A. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Futur Heal J 2020; 8: e85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhatariya KK, Wiles MD. Pre-operative testing guidelines: a NICE try but not enough. Anaesthesia 2016; 71: 1403–7. [DOI] [PubMed] [Google Scholar]
- 4.Barrett-Lee J, Vatish J, Vazirian-Zadeh M, P W. Routine blood group and antibody screening prior to emergency laparoscopy. Ann R Coll Surg Engl 2018; 100: 322–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Heal 2017; 1: e381–8. [DOI] [PubMed] [Google Scholar]
- 6.Rizan C, Steinbach I, Nicholson Ret al. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann Surg 2020; 272: 986–95. [DOI] [PubMed] [Google Scholar]
- 7.McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. BJA Br J Anaesth 2020; 125: 680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rizan C, Mortimer F, Stancliffe R, Bhutta MF. Plastics in healthcare: time for a re-evaluation: J R Soc Med 2020; 113: 49-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morris DS, Wright T, Somner JEA, Connor A. The carbon footprint of cataract surgery. Eye 2013; 27: 495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thiel CL, Schehlein E, Ravilla Tet al. Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg 2017; 43: 1391–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thiel CL, Eckelman M, Guido Ret al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol 2015; 49: 1779–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thiel CL, Woods NC, Bilec NM. Strategies to Reduce Greenhouse Gas Emissions from Laparoscopic Surgery. Am J Public Health 2018; 108: S158–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coulter WA, Chew-Graham CA, Cheung SW, Burke FJT. Autoclave performance and operator knowledge of autoclave use in primary care: A survey of UK practices. J Hosp Infect 2001; 48: 180–5. [DOI] [PubMed] [Google Scholar]
- 14.NHS England. (HTM 01-01) Decontamination of surgical instruments. https://www.england.nhs.uk/publication/decontamination-of-surgical-instruments-htm-01-01/ (cited October 2021). [Google Scholar]
- 15.Southworth PM. Infections and exposures: reported incidents associated with unsuccessful decontamination of reusable surgical instruments. J Hosp Infect 2014; 88: 127–31. [DOI] [PubMed] [Google Scholar]
- 16.Stevenson M, Uttley L, Oakley JEet al. Interventions to reduce the risk of surgically transmitted Creutzfeldt-Jakob disease: a cost-effective modelling review. Health Technol Assess 2020; 24: 1–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.FDA. Sterility Issues with Medical Devices Processed at Steril Milano Facilities - Letter to Industry. www.fda.gov/medical-devices/industry-medical-devices/sterility-issues-medical-devices-processed-steril-milano-facilities-letter-industry (cited October 2021).
- 18.Kieser DC, Wyatt MC, Beswick Aet al. Does the type of surgical drape (disposable versus non-disposable) affect the risk of subsequent surgical site infection? J Orthop 2018; 15: 566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McQuerry M, Easter E, Cao A. Disposable versus reusable medical gowns: A performance comparison. Am J Infect Control 2021; 49: 563–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NHS England. (HTM 01-04) Decontamination of linen for health and social care. https://www.england.nhs.uk/publication/decontamination-of-linen-for-health-and-social-care-htm-01-04/ (cited October 2021). [Google Scholar]
- 21.Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: Results from 2 million consecutive cataract surgeries. J Cataract Refract Surg 2019; 45: 1226–33. [DOI] [PubMed] [Google Scholar]
- 22.Drew J, Christie SD, Tyedmers Pet al. Operating in a Climate Crisis: A State-of-the-Science Review of Life Cycle Assessment within Surgical and Anesthetic Care. Environ Health Perspect 2021; 129: 76001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Serota KB. Deceptive Marketing Outcomes: A Model for Marketing Communications. In: Docan-Morgan T. The Palgrave Handbook of Deceptive Communication. London: Palgrave Macmillan; 2019. pp 813-837. [Google Scholar]
- 24.Smith BD. Brand Therapy. London: Practical Inspiration; 2018. [Google Scholar]
- 25.British Medical Association. Healthier Procurement: Improvements to working conditions for surgical instrument manufacture in Pakistan. https://www.bma.org.uk/what-we-do/working-internationally/our-international-work/healthier-procurement (cited October 2021).
- 26.NCL Blog Service. Forced Labour in the Malaysian Medical Gloves Supply Chain before and during the COVID-19 Pandemic: Evidence, Scale and Solutions. https://blogs.ncl.ac.uk/alexhughes/2021/06/30/forced-labour-in-the-malaysian-medical-gloves-supply-chain-during-the-covid-19-pandemic/ (cited October 2021).
- 27.British Medical Association. Labour rights abuse in global supply chains for PPE through COVID-19: Issues and solutions. https://www.bma.org.uk/media/4288/ppe-labour-rights-abuse-in-global-chains-for-ppe-through-covid-july-2021.pdf (cited October 2021).
- 28.Medicines and Healthcare Products Regulatory Agency. Single-use medical devices: implications and consequences of reuse v2.4. https://www.gov.uk/government/publications/single-use-medical-devices-implications-and-consequences-of-re-use (cited October 2021).
- 29.Rizan C, Bhutta MF. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc 2021; 1: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cabinet Office. Procurement Policy Note – Taking Account of Carbon Reduction Plans in the procurement of major government contracts. https://www.gov.uk/government/publications/procurement-policy-note-0621-taking-account-of-carbon-reduction-plans-in-the-procurement-of-major-government-contracts (cited October 2021).
- 31.Rizan C, Reed M, Bhutta MF. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J R Soc Med 2021; 114: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rizan C, Bhutta MF, Reed M, Lillywhite R. The carbon footprint of waste streams in a UK hospital. J Clean Prod 2021; 286: 125446. [Google Scholar]
- 33.The IEA. China. www.iea.org/countries/china (cited October 2021).
- 34.Eionet. Greenhouse gas emissions and natural capital implications of plastics (including biobased plastics). https://www.eionet.europa.eu/etcs/etc-wmge/products/greenhouse-gas-emissions-and-natural-capital-implications-of-plastics-including-biobased-plastics (cited October 2021).