Abstract
Objective
Surgical training programmes are evolving from time-based to competency-based schedules, which define expected learning outcomes in surgical knowledge, clinical and technical skills according to training levels. This article aims to review current models in surgical skills acquisition and to propose an integrative process-driven, outcomes-based model for surgical skills acquisition and mastery.
Design
A literature review was conducted on the theories of motor skills acquisition using PubMed, Web of Science and Google Scholar from 2010 to February 2020. The review was limited to theories and models on surgical skills acquisition and mastery. Four models of surgical skills acquisition were included: Fitts and Posner’s three-stage model of motor skills acquisition, Bandura’s social learning theory, Ericsson’s deliberate practice model and Jeannerod’s motor simulation theory. These models are deficient in that there is no universally accessible opportunity to practise the surgical procedure outside of the operating theatre and without access to physical simulators.
Results
We propose an innovative model that allows deliberate practice of the procedure without the need for expensive physical simulators, and provides an on-demand, self-directed practice by the trainees to achieve the level of mastery. This new model, which incorporates motor imagery and mental practice, augmented by deliberate practice, will provide an alternative training path for expert performance in surgical procedures.
Conclusions
The innovative model provides a solution to the reduced opportunity for practice by surgical trainees to achieve mastery in surgical motor skills.
Keywords: Surgical education, Instructional design, Deliberate practice, Mental practice, Mastery
Highlights
Mental skills training for mental simulation should be incorporated into the surgical education programme. Faculty members must be trained in the design and development of instructional videos and mental scripts. Every index procedure in surgical skills training should have the following:
-
•
Expert instructional video of the procedure.
-
•
A mental script incorporating kinaesthetic cues.
-
•
Narration of the mental script incorporated into the video.
-
•
Inexpensive and easily accessible practice models for deliberate practice.
Introduction
Surgical training programmes are evolving from traditional time-based schedules to competency-based ones, which define expected learning outcomes in surgical knowledge, clinical and technical skills according to training levels. This has the potential to shorten the training time for some to become competent surgeons.1
Traditional surgical training employed the apprenticeship model, which is opportunity-based learning. It is characterised by trainees practising surgical procedures under the guidance of mentors for several years, incorporating long hours of practice, and frequent and intensive contacts between the trainer and the trainee. The adage, ‘See One, Do One, Teach One’ was often used in traditional surgical education but is no longer practised because of concerns for patient safety. ‘Learning on the job’ is still important, but other options such as simulation training are available, with clearly defined learning objectives and more stringent but reliable assessment processes.2
Changes in the surgical training curriculum and teaching approaches were brought about by multiple factors in healthcare, eg the restriction on residency duty hours, increasing safety standards, demands for service efficiency and zero tolerance for malpractice. These have brought significant challenges to surgical training, especially in the domain of motor skill acquisition.1
Advancement in surgical education research has shed light on the understanding of competency and assessment. Competence cannot be assumed when trainees can perform parts of a task or individual surgical skills, because surgery requires the integration of many skills. Literature has shown that surgical trainees at both undergraduate3 and postgraduate levels4 do not feel competent or ready to operate independently at the end of their training. Neither is competency equal to excellence, and unfortunately, due to lack of time and opportunities to practise, the learning process focuses on competence rather than excellence.5
To explore how to best prepare surgical trainees for independent practice, we propose to apply the instructional design (ID) model with multimedia design principles in surgical education. ID is the science of instruction, and provides a systematic and an evidence-based methodology for the creation of instructional materials for effective teaching. A commonly used ID model for developing learning programmes is the Analysis, Design, Development, Implementation and Evaluation (ADDIE) model.6 The ADDIE model includes assessing learners’ needs, defining the end goals of instruction, task and content analysis, planning assessment and developing activities to ensure the quality of instruction. Multimedia principles share the best practices in designing multimedia teaching materials such as video, animation or multimedia presentations.7 In this case, expert videos are suggested as a supplementary teaching resource for surgical trainees.
This article reviews the current theoretical models in surgical skills acquisition and, by utilising ID models, proposes an integrative process-driven, outcome-based model for surgical skills acquisition and mastery.
Methods
The literature review was conducted using PubMed, Web of Science and Google Scholar from 2010 up to February 2020. The initial keywords used in the search included: ‘motor skill training’ OR ‘skill acquisition’ OR ‘surgical skill training’. Then additional search terms such as ‘motor imagery’, ‘mental practice’, ‘deliberate practice’ and ‘simulation’ were employed within the biography of these articles. The review was limited to theories and models on surgical skills acquisition and mastery and excluded studies on skills acquisition in non-surgical domains.
Review of surgical training theories
Four theories of surgical motor skill acquisition are commonly used: Fitts and Posner’s three-stage model of motor skills acquisition, Bandura’s theory of social learning, Ericsson’s deliberate practice model and Jeannerod’s motor simulation theory. The models focus on visuospatial awareness and fine motor dexterity, the two essential skills in surgical training (Table 1).8–11
Table 1 .
Summary of surgical training theories
| Theory | Summary |
|---|---|
| Fitts and Posner’s three-stage theory of motor skill acquisition8 | Motor skill acquisition goes through three stages, ie cognitive or learning stage, associative or motor behaviour stage and autonomous (expert) stage |
| Bandura’s theory of social learning9 | Based on observational learning and modelling: attention, internalisation (retention), reproduction and motivation |
| Ericsson’s deliberate practice model8,12 | Deliberate practice with regular reinforcement and feedback to support learning |
| Jeannerod’s motor simulation theory11 | Cognitive rehearsal of a task in the absence of overt physical movement using script-based mental rehearsal |
Fitts and Posner’s three-stage model of motor skills acquisition8
Fitts and Posner described a three-stage model of motor skills acquisition, including the trainee’s performance at each stage, but did not provide strategies to enable skill acquisition. In the cognitive stage, the learner intellectualises and understands the task by explanation and demonstration, but performs the task erratically in distinct and individual steps. With repeated practice and feedback the learner reaches the associative stage, in which knowledge is translated into appropriate motor behaviour.8,12 The task is executed smoothly and with fewer interruptions, but the learner still thinks actively about the various motor movements required for the task. In the final autonomous stage, the learner performs the task smoothly with minimal mental effort and almost automatically, to the level of an expert.6,13
For example, when beginners learn to suture, they need to learn how to hold the needle holder, how to place the hand, how to puncture the right side of the skin and how to tie a knot. These individual steps make up the cognitive stage. The ID strategy of ‘task and content analysis’ corresponds to the procedural guide, which is here presented in audio-visual format.6 Students reach the associative stage with practice and feedback, eg where they can suture the wound without thinking too much about how to hold the needle holder, but they still lack fluidity of movements. The ID strategy here is practising the task with feedback, which is delivered through the design and development of the practice task and materials, as well as implementation through practice sessions.6 Providing feedback through formative assessment and direct observation of performance and outcomes in the operating room ensures retention and transfer of the skill. In the autonomous stage, students are skilful in suturing, and can concentrate on other aspects of the procedure without thinking too much about how to suture.
Bandura’s social learning theory
Bandura discovered that learning, apart from being a cognitive process, occurs in a social context through observation of experts and interaction with instructors and peers.9 This is called role modelling14 (p199). It can happen by observing model behaviour and by noting the consequences of that behaviour (vicarious reinforcement).14,15 An expert surgeon’s demonstration can be recorded in videos, so trainees can watch the expert demonstration as needed. Live recording is not always an effective way to record demonstrations by experts, and it is good to apply ID principles such as ‘task and content analysis’ to decide on what to record,6 and to use multimedia learning principles16 to best design the videos.
Learning is affected by personal factors and the social environment.14 Personal factors refer to learners believing they can complete the task (self-efficacy).14 Social environment refers to trainees learning from modelled practice by a mentor, then practising and demonstrating the skills and receiving feedback from mentors.9,17 The environmental factors refer to the support from mentors, the training structure and the resources available.9
For observational learning to occur, Bandura17 posited that the following must occur:
-
•
Attention – observers must be attentive to the modelled behaviour, which in turn is impacted by observer and behaviour characteristics.
-
•
Retention – observers must remember individual features of the behaviour.
-
•
Reproduction – observers must organise responses and actions by following a model.
-
•
Motivation – observers must be interested in performing or imitating the behaviour they have observed to reproduce that behaviour.
Bandura’s theory highlights the importance of observation of the mentor surgeon but is limited by the opportunity for direct observation in the operating room. However, with the use of instructional videos capturing the expert performance, it accedes to the production of standardised material that is universally accessible, thus maximising learning opportunities through asynchronous learning.18
Ericsson’s deliberate practice model
Deliberate practice allows acquisition and retention of motor skill for expert performances.19 Expert surgeons are experienced surgeons with consistently better outcomes. Ericsson discovered that expert performance requires deliberate practice (defined as repeated practice in motivated individuals receiving regular reinforcement and feedback) and that it is necessary to continue doing it to maintain mastery.10 The master level of performance is not merely associated with time spent in surgery, but with the number of hours spent in deliberate practice, including a highly structured set of activities with the explicit goal of improving performance.20,21 Studies have shown its effectiveness in surgical skills training.22–24 Trainees can improve their surgical knowledge through continuing learning and improvement.10 Deliberate practice with feedback is the cornerstone of the attainment and maintenance of expertise in surgery,25 and has become the gold standard in skills training.10,26 For example, in tendon repair surgery, the opportunity to practise is limited by the number of cases seen, but can be simulated using chicken tendon practice models, which can provide the trainees with on-demand self-paced deliberate practice.27,28
Jeannerod’s motor simulation theory
Jeannerod’s motor simulation theory is based on the finding that performing a motor action and thinking of doing that action activate similar motor systems in the brain.11 The motor simulation theory forms the basis of motor imagery,29 which is the mental execution of a motor task by incorporating the kinaesthetic cues without overtly performing the task. Motor imagery and mental practice are functionally equivalent,29 and have been used for surgical skills training,30 with persistent improvement in surgical performance.31–34 This has been corroborated further by research using trans-cranial magnetic stimulation with brain imaging, which shows the link between cortical reorganisation (ie structural changes in the brain) and behavioural changes with mental practice.35 Mental practice can activate stored information to such an extent that physiological and behavioural responses are triggered.34
Mirror neurons are activated when an action is executed or observed, anticipated or imagined,36 which explains our ability to observe and accurately imitate the actions of others. The activity of these neurons is higher if the learner has a strong sense of the goal being achieved.37 This explains the effectiveness of both mental practice and observation, which, when combined with physical practice, may enhance learning and shorten training times.38–40
A review of 28 studies showed mental practice underpinned successful surgical learning and performance through mental imagery, attention and thought management, goal setting and performance routines. This practice has been shown to improve the surgery performance and confidence of learners, as well as allowing the learners to anticipate complications and develop prevention strategies when preparing for surgery. This mental imagery also primed the learner’s motor system, as it used the same neural pathways as the surgery.41 Structured mental imagery instructions, which are a step-by-step breakdown of the motor actions, and a mental script specific to the procedure31 are needed for it to work effectively and can reduce surgical errors.42 Script-based mental rehearsal has been defined as ‘the cognitive rehearsal of a task in the absence of overt physical movement’.23,43
Mental imagery and practice are a low-cost and useful educational supplement for surgical simulation training in neurosurgery,23 basic surgical skills training, deliberate practice focused on specific weaknesses in performance44 and improving a surgeon’s confidence, knowledge and performance.45
Summary of the theories
The current body of knowledge on psychomotor skill acquisition to an expert level32,46 requires:
-
•
observation of the skill demonstrated by an expert;
-
•
internalisation with motor imagery;
-
•
mental practice and repetition;
-
•
physical deliberate practice.
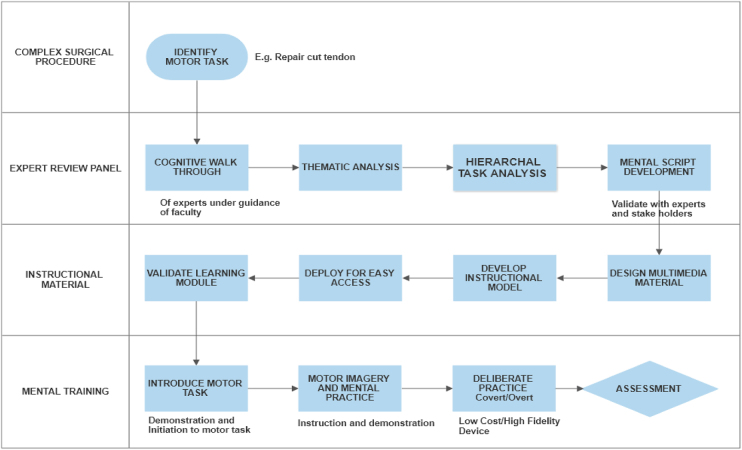
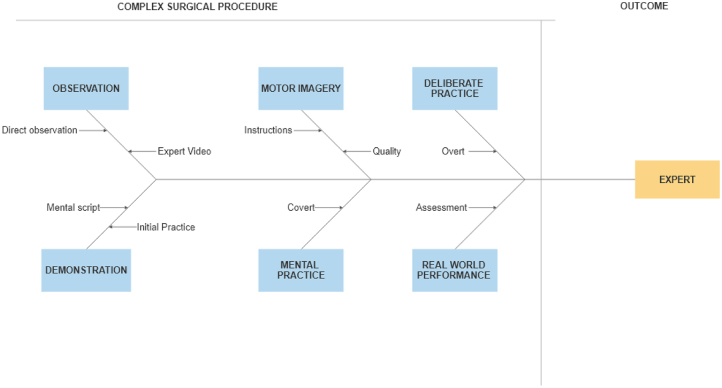
Figure 1 integrates the steps described in the four theories of skills acquisition and mastery.8–11 ID principles have been incorporated to design and develop learning material. The process is based on the design and development framework in instruction47 for the creation of product (training module – the outcome in Figure 1 and instructional materials in Figure 3), tool (process to create products – expert review panel and instructional materials in Figure 3) or a model development (Figure 1).48
Figure 1 .
Theoretical basis for the new integrated model for surgical skills training
Figure 3 .
Execution of the model to create a training programme for a surgical skill
To provide trainees with more opportunity to learn and practise, simulators including low-fidelity bench models, basic surgical skills, surgical laboratory practice and higher-fidelity human cadaver models have been used.49 Technology, from simulation to gaming and robotics, has become the enabler in surgical training.50,51 However these strategies require resources – both physical and trainee time – because they are synchronous learning platforms,52 which prevents universally accessible opportunities to practise the surgical procedure outside of the operating theatre. In addition, these expensive technologies are not commonly used in low-source training contexts.
An integrated model of expert skills acquisition: applying ID principles in developing surgical training programmes to promote mental deliberate practice
We propose to apply ID principles to develop the surgical training programmes that allow deliberate practice of the procedure without the need for expensive physical simulators and provide an on-demand, self-directed practice by the trainees to achieve the level of mastery. Figure 1 provides the theoretical basis for this integrated model and Figure 2 shows the process of surgical training based on the model. The execution of the model to create training programmes in specific surgical procedures is shown in Figure 3. To facilitate the understanding of the model and to demonstrate how to implement this model, we use an example of ‘how to repair a cut tendon’ to illustrate the steps described in Figure 3.
Figure 2 .
Process of surgical skills acquisition based on the new model
Complex surgical procedure
We start by identifying the key motor tasks for the complex procedure. This can be achieved through reviewing surgical curricula and guidelines, as well as surgical education textbooks or educational videos. It is important to know what the expected learning outcomes are for different levels of trainees, so the expected key tasks and competency levels can correspond to the trainee’s level. For example, to teach ‘how to repair a cut tendon’, the expected learning outcomes for a final-year medical student are different from an orthopaedic surgery resident. It also varies for a junior resident compared to a senior resident.
Expert review panel
Expert consensus plays an important role in finalising the key tasks and subsequent tasks. Using expert consensus to identify the key tasks of complex surgical procedures constructs a think-aloud walk-through of the motor skill, followed by a content and task analysis,19 then creates a detailed mental script which will be incorporated into the instructional materials.16 Trainees observe expert performance, followed by mental practice with motor imagery, then do deliberate practice to reach the mastery level.
Instructional material development
This model highlights the importance of applying ID strategies to develop surgical training materials. As discussed earlier, expert demonstration serves as role modelling for surgical trainees through observing model behaviour and by noting the consequences of that behaviour. The ADDIE model is used to perform a content, task and subtask analysis of the procedure with expert surgeons, which will aid the development of the instructional video. Instructional videos of the expert surgeon’s live demonstration will be developed based on the framework of multimedia learning of the surgical procedures.16 The video will include the narration of the mental script produced by expert review panel, as described in the previous step. This will help trainees for mental practice and is then augmented with deliberate practice using low-cost practice models. In tendon repair, for example, a cognitive walk-through is conducted with an expert surgeon and his or her instructions and reflections (inclusive of kinaesthetic cues) are recorded and analysed verbatim, to create a mental script validated by master surgeons. This will be used as the narration for an instructional video showing the master surgeon performing the tendon repair. After a test run by surgical trainees, the video will then again be modified and validated by master surgeons.
Mental training
Once the surgical training materials are developed, trainees will use this information to practice. The combination of the video and mental practice using the mental script allow the trainees to learn from expert surgeons anytime, anywhere, and can improve with deliberate practice using the chicken/sheep practice model. A low-cost practice model is needed for deliberate practice for tendon repair training. Once they are ready, they are then assessed in the operating room for real-world performance to verify retention and transfer of skills in tendon repair surgery.
This innovative model incorporates motor imagery and mental practice, augmented by deliberate practice. It will provide an alternative training path for expert performance in surgical procedures. The tools to design and develop the instructional materials (expert instructional videos and mental scripts; Figure 3) with task and content analysis is founded on sound ID model and multimedia design principles. It will, however, require further validation.
Conclusions
The innovative model described in this review provides a potential solution to the reduced opportunity for practice by surgical trainees to achieve mastery in surgical motor skills. That being said, this model is based on review of theories, and we do not yet have data from experimental studies to validate the model. We plan to study the effectiveness of the model in teaching surgical trainee motor skills in the future, and to explore how the model can be implemented as part of a surgical training programme. In addition, motor skills, although an important component of surgical training, are not the only skills required for mastery as a surgeon. This model addresses the technical expertise but not the adaptive, decision-making expertise and the other non-technical skills that are needed in a master surgeon in practice. Future studies are required to investigate how this model might be used for non-technical skills training.
Practice implications
Mental skills training through simulation should be incorporated into the surgical training programme. Faculty members must be trained in the design and development of instructional videos and mental scripts. Every index procedure in surgical skill training should have the following:
-
1.
Expert instructional video of the procedure.
-
2.
A mental script incorporating kinaesthetic cues.
-
3.
Narration of the mental script incorporated into the video.
-
4.
Inexpensive and easily accessible practice models for deliberate practice.
References
- 1.Royal College of Surgeons. Improving Surgical Training (IST). https://www.rcseng.ac.uk/careers-in-surgery/trainees/ist/ (cited March 2021).
- 2.Kotsis SV, Chung KC. Application of see one, do one, teach one concept in surgical training. Plast Reconstr Surg 2013; 131: 1194–1201. 10.1097/PRS.0b013e318287a0b3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayes P. Newly qualified doctors’ views of medical school training and its adequacy in making them ‘fit for purpose’ as first year doctors. Open Access Libr J 2016; 3: 1–20. 10.4236/oalib.1102799 [DOI] [Google Scholar]
- 4.Elfenbein DM. Have we created a crisis in confidence for general surgery residents? A systematic review and qualitative discourse analysis. JAMA Surg 2016; 151: 1166–1175. 10.1001/jamasurg.2016.2792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels AH, DiGiovanni CW. Is subspecialty fellowship training emerging as a necessary component of contemporary orthopaedic surgery education? J Grad Med Educ 2014; 6: 218–221. 10.4300/JGME-D-14-00120.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalil MK, Elkhider IA. Applying learning theories and instructional design models for effective instruction. Adv Physiol Educ 2016; 40: 147–156. 10.1152/advan.00138.2015 [DOI] [PubMed] [Google Scholar]
- 7.Mayer RE. Applying the science of learning to medical education. Med Educ 2010; 44: 543–549. 10.1111/j.1365-2923.2010.03624.x [DOI] [PubMed] [Google Scholar]
- 8.Fitts PM, Posner MI. Human Performance. Belmont, CA: Brooks/Cole Publishing Company; 1967. [Google Scholar]
- 9.Bandura A. Social Learning Theory. 2nd edn. Englewood Cliffs, NJ: : Prentice Hall, 1977. [Google Scholar]
- 10.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med J Assoc Am Med Coll 2004; 79: S70–81. 10.1097/00001888-200410001-00022 [DOI] [PubMed] [Google Scholar]
- 11.Jeannerod M. Mental imagery in the motor context. Neuropsychologia 1995; 33: 1419–1432. 10.1016/0028-3932(95)00073-C [DOI] [PubMed] [Google Scholar]
- 12.Sadideen H, Kneebone R. Practical skills teaching in contemporary surgical education: how can educational theory be applied to promote effective learning? Am J Surg 2012; 204: 396–401. 10.1016/j.amjsurg.2011.12.020 [DOI] [PubMed] [Google Scholar]
- 13.Sattelmayer M, Elsig S, Hilfiker R, Baer G. A systematic review and meta-analysis of selected motor learning principles in physiotherapy and medical education. BMC Med Educ 2016; 16: 15. 10.1186/s12909-016-0538-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandura A (ed). Self-Efficacy in Changing Societies. Cambridge: Cambridge University Press; 1995. pp 1–45. [Google Scholar]
- 15.Grusec JE. Social learning theory and developmental psychology: The legacies of Robert Sears and Albert Bandura. Dev Psychol 1992; 28: 776–786. 10.1037/0012-1649.28.5.776 [DOI] [Google Scholar]
- 16.Mayer RE. Multimedia Learning. 2nd edn. Cambridge: Cambridge University Press; 2009. [Google Scholar]
- 17.Bandura A. Influence of models’ reinforcement contingencies on the acquisition of imitative responses. J Pers Soc Psychol 1965; 1: 589–595. 10.1037/h0022070 [DOI] [PubMed] [Google Scholar]
- 18.Mota P, Carvalho N, Carvalho-Dias Eet al. Video-based surgical learning: improving trainee education and preparation for surgery. J Surg Educ 2018; 75: 828–835. 10.1016/j.jsurg.2017.09.027 [DOI] [PubMed] [Google Scholar]
- 19.Ericsson KA. Protocol Analysis and Expert Thought: Concurrent Verbalizations of Thinking during Experts’ Performance on Representative Tasks. In Ericsson KA, Charness N, Feltovich PJ, Hoffman RR. The Cambridge Handbook of Expertise and Expert Performance. Cambridge: Cambridge University Press. 2006: pp223–241. [Google Scholar]
- 20.Nestel D, Dalrymple K, Paige J, Aggarwal R (eds). Advancing Surgical Education: Theory, Evidence and Practice. Springer Singapore; 2019. 10.1007/978-981-13-3128-2 [DOI] [Google Scholar]
- 21.Ericsson KA. The Road to Excellence: The Acquisition of Expert Performance in the Arts and Sciences, Sports, and Games. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp 1–50. [Google Scholar]
- 22.Kirkman MA. Deliberate practice, domain-specific expertise, and implications for surgical education in current climes. J Surg Educ 2013; 70: 309–317. 10.1016/j.jsurg.2012.11.011 [DOI] [PubMed] [Google Scholar]
- 23.Marcus H, Vakharia V, Kirkman MAet al. Practice makes perfect? The role of simulation-based deliberate practice and script-based mental rehearsal in the acquisition and maintenance of operative neurosurgical skills. Neurosurgery 2013; 72: A124–A130. 10.1227/NEU.0b013e318270d010 [DOI] [PubMed] [Google Scholar]
- 24.Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ 2010; 44: 75–84. 10.1111/j.1365-2923.2009.03421.x [DOI] [PubMed] [Google Scholar]
- 25.Siddaiah-Subramanya M, Smith S, Lonie J. Mastery learning: how is it helpful? An analytical review. Adv Med Educ Pract 2017; 8: 269–275. 10.2147/AMEP.S131638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oviedo-Peñata CA, Tapia-Araya AE, Lemos JDet al. Validation of training and acquisition of surgical skills in veterinary laparoscopic surgery: a review. Front Vet Sci 2020; 7. 10.3389/fvets.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khunger N, Kathuria S. Mastering surgical skills through simulation-based learning: practice makes one perfect. J Cutan Aesthetic Surg 2016; 9: 27. 10.4103/0974-2077.178540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pafitanis G, Serrar Y, Raveendran Met al. The chicken thigh adductor profundus free muscle flap: a novel validated non-living microsurgery simulation training model. Arch Plast Surg 2017; 44: 293–300. 10.5999/aps.2017.44.4.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Shea H, Moran A. Does motor simulation theory explain the cognitive mechanisms underlying motor imagery? A critical review. Front Hum Neurosci 2017 Feb 17; 11: 72. 10.3389/fnhum.2017.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slimani M, Tod D, Chaabene Het al. Effects of mental imagery on muscular strength in healthy and patient participants: a systematic review. J Sports Sci Med 2016; 15: 434–450. [PMC free article] [PubMed] [Google Scholar]
- 31.Arora S, Aggarwal R, Sevdalis Net al. Development and validation of mental practice as a training strategy for laparoscopic surgery. Surg Endosc 2010; 24: 179–187. 10.1007/s00464-009-0624-y [DOI] [PubMed] [Google Scholar]
- 32.Schuster C, Hilfiker R, Amft Oet al. Best practice for motor imagery: a systematic literature review on motor imagery training elements in five different disciplines. BMC Med 2011; 9: 75. 10.1186/1741-7015-9-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spruit EN, Band GP, Hamming JF, Ridderinkhof KR.. Optimal training design for procedural motor skills: a review and application to laparoscopic surgery. Psychol Res 2014 Nov; 78: 878–891. 10.1007/s00426-013-0525-5 [DOI] [PubMed] [Google Scholar]
- 34.Ji JL, Heyes SB, MacLeod C, Holmes EA. Emotional mental imagery as simulation of reality: fear and beyond—a tribute to Peter Lang. Behav Ther 2016; 47: 702–719. 10.1016/j.beth.2015.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruffino C, Papaxanthis C, Lebon F. Neural plasticity during motor learning with motor imagery practice: review and perspectives. Neuroscience 2017; 341: 61–78. 10.1016/j.neuroscience.2016.11.023 [DOI] [PubMed] [Google Scholar]
- 36.Cook R, Bird G, Catmur Cet al. Mirror neurons: from origin to function. Behav Brain Sci 2014; 37: 177–192. 10.1017/S0140525X13000903 [DOI] [PubMed] [Google Scholar]
- 37.Gazzola V, Rizzolatti G, Wicker B, Keysers C. The anthropomorphic brain: the mirror neuron system responds to human and robotic actions. Neuroimage 2007; 35: 1674–1684. 10.1016/j.neuroimage.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 38.Gentili RJ, Papaxanthis C. Laterality effects in motor learning by mental practice in right-handers. Neuroscience 2015; 297: 231–242. 10.1016/j.neuroscience.2015.02.055 [DOI] [PubMed] [Google Scholar]
- 39.Gentili R, Papaxanthis C, Pozzo T. Improvement and generalization of arm motor performance through motor imagery practice. Neuroscience 2006; 137: 761–772. 10.1016/j.neuroscience.2005.10.013 [DOI] [PubMed] [Google Scholar]
- 40.Gentili R, Han CE, Schweighofer N, Papaxanthis C. Motor learning without doing: trial-by-trial improvement in motor performance during mental training. J Neurophysiol 2010; 104: 774–783. 10.1152/jn.00257.2010 [DOI] [PubMed] [Google Scholar]
- 41.Anton NE, Bean EA, Hammonds SC, Stefanidis D. Application of mental skills training in surgery: a review of its effectiveness and proposed next steps. J Laparoendosc Adv Surg Tech 2017; 27: 459–469. 10.1089/lap.2016.0656 [DOI] [PubMed] [Google Scholar]
- 42.Patel SR, Gohel MS, Hamady Met al. Reducing errors in combined open/endovascular arterial procedures: influence of a structured mental rehearsal before the endovascular phase. J Endovasc Ther Off J Int Soc Endovasc Spec 2012; 19: 383–389. 10.1583/11-3785R.1 [DOI] [PubMed] [Google Scholar]
- 43.Sanders CW, Sadoski M, Bramson Ret al. Comparing the effects of physical practice and mental imagery rehearsal on learning basic surgical skills by medical students. Am J Obstet Gynecol 2004; 191: 1811–1814. 10.1016/j.ajog.2004.07.075 [DOI] [PubMed] [Google Scholar]
- 44.Pugh CM. Warm-ups, mental rehearsals and deliberate practice: adopting the strategies of elite professionals. J Surg Res 2012; 176: 404–405. 10.1016/j.jss.2011.05.063 [DOI] [PubMed] [Google Scholar]
- 45.Sevdalis N, Moran A, Arora S. Mental Imagery and Mental Practice Applications in Surgery: State of the Art and Future Directions. In: Lawson R. Multisensory Imagery. New York: Springer; 2013. pp 343–363. [Google Scholar]
- 46.Frank C, Land WM, Popp C, Schack T. Mental representation and mental practice: experimental investigation on the functional links between motor memory and motor imagery. PLoS ONE 2014; 9: e95175. 10.1371/journal.pone.0095175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richey R, Klein JD. Design and Development Research: Methods, Strategies, and Issues. New York: L. Erlbaum Associates; 2007. [Google Scholar]
- 48.Richey RC, Klein JD. Design and Development Research. In: Spector JM, Merrill MD, Elen J, Bishop MJ. Handbook of Research on Educational Communications and Technology. New York: Springer; 2014: pp 141–150. [Google Scholar]
- 49.Javid P, Aydın A, Mohanna P-Net al. Current status of simulation and training models in microsurgery: a systematic review. Microsurgery 2019; 39: 655–668. 10.1002/micr.30513 [DOI] [PubMed] [Google Scholar]
- 50.Evans CH, Schenarts KD. Evolving educational techniques in surgical training. Surg Clin 2016; 96: 71–88. 10.1016/j.suc.2015.09.005 [DOI] [PubMed] [Google Scholar]
- 51.Kerr RS. Surgery in the 2020s: implications of advancing technology for patients and the workforce. Future Heal J 2020; 7: 46–49. 10.7861/fhj.2020-0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh M, Ziolkowski N, Ramachandran Set al. Development of a five-day basic microsurgery simulation training course: a cost analysis. Arch Plast Surg 2014; 41: 213. 10.5999/aps.2014.41.3.213 [DOI] [PMC free article] [PubMed] [Google Scholar]