Abstract
Introduction
Autologous stem cell progenitor implantation into necrotic lesions of the femoral head has previously been described as a potential treatment for avascular necrosis (AVN), on the basis that there is a reduced number of functioning stem cells in the marrow within the necrotic segment. We present a case series of patients with AVN that underwent core decompression with autologous stem cell implantation using a new device.
Methods
The records and imaging of patients with AVN of the femoral head treated by a single surgeon were retrospectively reviewed. All patients were treated with core decompression and stem cell progenitor implantation, using the PerFuse system. Preoperatively, demographic information, AVN staging (as per Ficat and Arlet classification) and visual analogue pain scores (VAS) of the hips were recorded. These results were compared with postoperative VAS and imaging, with further review on the progression of AVN.
Results
We treated 14 hips in 13 patients with an average follow up of 12 months. Patients with Ficat I–II were selected for the procedure. The average preoperative VAS was 3.9. Postoperatively, this dropped to 2.6, with over half of patients reporting at least a two-point decrease in pain. Eight of the 14 treated hips showed no radiological progression of the disease, while six showed femoral head collapse requiring total hip arthroplasty (THA) at an average of ten months after treatment.
Conclusion
Our early findings indicate that hip decompression with stem cell progenitor implantation for AVN of the femoral head provides symptomatic relief and may be beneficial in arresting progression of disease using this simple new device.
Keywords: Avascular necrosis, Autologous bone marrow implantation, Stem cell progenitor, Femoral head, PerFuse
Introduction
Avascular necrosis (AVN) (or osteonecrosis) of the femoral head is an unrelenting, progressive disease that may affect 2 per 100,000 people in the UK.1 This results from a number of aetiologies including steroid use, alcohol abuse and sickle cell disease, although most remain idiopathic in the UK.2–6 AVN can lead to a painful and early collapse of the femoral head if left untreated. The pathogenesis of this disease stems from diminished blood supply to the femoral head from the circumflex arteries, leading to necrosis of the bone. In fact, several studies have suggested that thrombosis and osteonecrosis may be related and share similarities in pathophysiology.7,8
In the pre-collapse stage of AVN (Ficat I–II), surgical options exist in order to salvage the femoral head and decrease the likelihood of hip replacement.9–11 Previously this has been limited to simple core decompression of the femoral head, with some success.12 However, over the last two decades there have been a number of studies showing that core decompression augmented with autologous concentrated bone marrow from the iliac crest is successful in improving outcomes in early stage AVN.13–17 The largest study, from Hernigou et al in 2002, showed radiographic arrest of disease and the need for total hip arthroplasty (THA) was prevented in the vast majority of patients.12 More recent studies have shown similar results.13–16 Centres with large numbers, however, may not reflect the UK population, owing to these areas either having a primarily Asian population or high sickle cell prevalence. Patients with osteonecrosis of the femoral head typically have fatty infiltration of the bone marrow and a reduced number of stem cell progenitors.18 Therefore, it follows that concentrating stem cell progenitors, typically from the iliac crest, combined with core decompression would promote repopulation of stem cell progenitors and improve vascularity in the femoral head. In this paper, we describe our technique for core decompression augmented with bone marrow aspirate for Ficat stage I or II AVN of the femoral head and review the outcomes of this procedure in 14 hips using a new surgical instrument, PerFuse (Zimmer Biomet; see Figure 1).
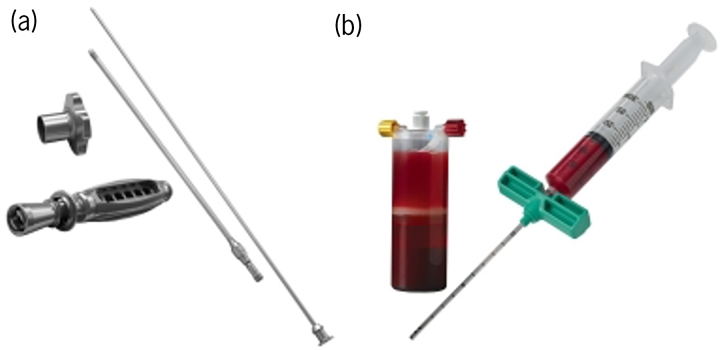
Figure 1 .
Biomet PerFuse instruments used during the procedures. (a) Equipment used for percutaneous core decompression; (b) instrument used to acquire bone marrow aspirate for the autologous stem cell implantation.
Methods
Study design
We retrospectively reviewed the electronic medical records and imaging of a consecutive series of patients who were treated by the supervising consultant for AVN of the femoral head over a three-year period at our institution (ethical approval as part of multicenter PREOB trial).19 Patients included had AVN of one or both hips that was graded to be stage I or II by the Ficat classification. All patients were treated with the combination of core decompression with autologous stem cell progenitor implantation from the iliac crest as per the technique described by Hernigou et al.12 Overall, 14 hips in 13 patients were included in the study. Demographic information on age, gender, body mass index and the aetiology of AVN was collected and is shown in Table 1. Staging of AVN as per the Ficat classification was determined by preoperative radiographs and magnetic resonance imaging (MRI). Patient’s visual analogue pain scores (VAS) were recorded pre- and postoperatively on a scale of 0–10, with 10 being the worst pain. From the operative record, any concurrent procedure, including contralateral THA, subchondroplasty procedure, and hip arthroscopy, was noted. Statistical analysis of the data was performed using the Student’s t-test.
Table 1 .
Demographic information on age, gender, body mass index and the aetiology of AVN
| Demographics | ||
| Age (years) | 21–30 | 1 (8%) |
| 31–40 | 7 (54%) | |
| 41–50 | 2 (15%) | |
| 51–60 | 2 (15%) | |
| 61–70 | 1 (8%) | |
| Gender | Male | 7 (54%) |
| Female | 6 (46%) | |
| BMI | 22–26 | 6 (46%) |
| 27–30 | 5 (38%) | |
| 31–35 | 2 (15%) | |
| Aetiology | ||
| Steroid use | 14% | |
| Alcohol | 28% | |
| Idiopathic | 36% | |
| Post-traumatic | 22% | |
| Symptom progression | ||
| <30 days | 22% | |
| >30 days | 78% | |
| Comorbidities | ||
| Hypertension | 22% | |
| Diabetes mellitus | 14% | |
| Metastatic CA | 7% | |
| Atrial fibrillation | 14% | |
Data expressed as n (%) unless otherwise indicated.
Surgical technique
Aspiration of stem cell progenitors was performed in the anaesthetic room after induction of anaesthesia. With the patient in the lateral position, cells were harvested from the posterior superior iliac crest, after which the patient was positioned on the operating table in the supine position. In the anaesthetic room the patient was draped in such a manner that allows palpation of both anterior and posterior iliac spines. A small (2–3mm) incision was made over one (or both) of the posterior superior iliac crests (Venus’s dimple surface landmark). The trochar (Biomet MarrowStim system) was pushed through the outer pelvic cortex and inserted 1–2cm in a direction aiming for the anterior-superior iliac spine. The trochar and syringe were preloaded with an anticoagulant, and multiple repositioning of the trochar was performed to ensure good cellular pick-up. A minimum of 60ml of bone marrow aspirate was withdrawn from the ipsilateral hip, and 120ml was withdrawn for bilateral hip cases. A small dressing was applied, and the patient was brought into the operating theatre. The specimen was placed in the centrifuge (15 mins at 3,200rpm). This yields 6ml or 12ml of concentrated skeletal stem cell progenitors, for unilateral or bilateral hip procedures, respectively.
While the concentrate was being prepared in the centrifuge, the core decompression of the hip was started. A 1cm incision was made laterally over the femur, just below the vastus ridge. The entry point of the trochar (PerFuse percutaneous decompression system – Zimmer Biomet) was kept above the level of the lesser trochanter. The trochar was directed towards the AVN lesion in the femoral head if possible, although a central position was acceptable. Perforation of the hard, necrotic bone was not attempted as this has been shown by Hernigou et al to be unnecessary. Use of fluoroscopy during the trochar insertion will help guide the instrument towards the necrotic lesion, which was driven in using a mallet, rather than drilling. The device is extremely stiff, which actually aids insertion compared to a more flexible drill. Once in place, the cannulated central trochar was removed and the bone marrow concentrate (via a ‘Luer Lock’ syringe attachment) was injected into the lesion, for which considerable force may be required. On removal of the trochar, the channel was disrupted to prevent the cells leaking back down the channel, by moving the trochar from side to side when halfway out.
Postoperatively, patients were allowed to bear weight as tolerated, with anticoagulation as per local guidelines for two weeks. Follow-up appointments were at 6 weeks, 3 months, 6 months, 1 year and 2 years. Radiographs were obtained at 6 weeks, 3 months, 6 months and 1 year postoperatively.
Results
Hip decompression with autologous concentrated bone marrow aspiration was performed on 13 patients in 14 affected hips. Our study included seven males and six females. Common aetiologies of AVN in the patient sample were corticosteroid use, alcohol and idiopathic, with idiopathic being the most prevalent of these affecting 36% of patients.
Patients were followed for an average of 18 months. Postoperatively, five patients experienced femoral head collapse after the decompression procedure, with one patient experiencing bilateral collapse. This led to a conversion to THA at a mean time of 12 months after the decompression. The remainder of patients showed no overt progression of AVN on postoperative imaging. No patient experienced a deep vein thrombosis. There were no postoperative infections or wound healing complications.
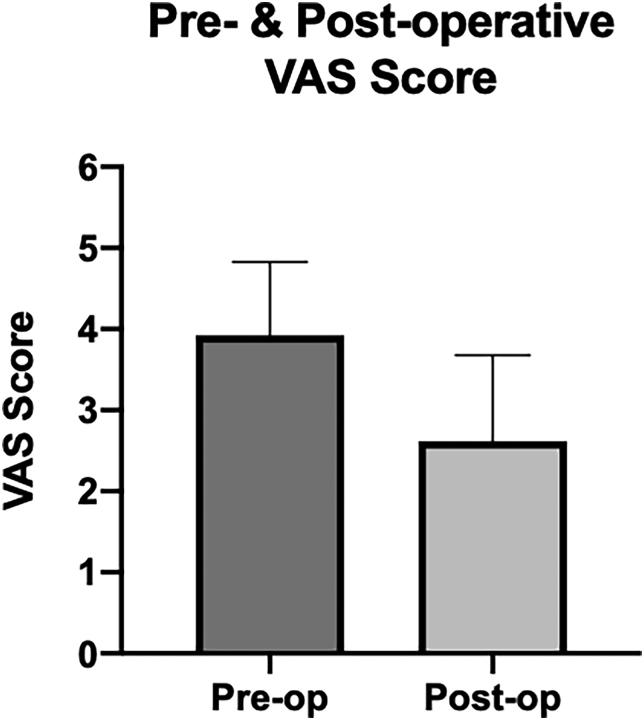
A comparison was made between preoperative and postoperative VAS pain scores. The mean preoperative score was 3.9, and the postoperative mean score was 2.6, as shown in Figure 2.
Figure 2 .
Graph comparing the visual analogue scores (VAS) of patients before and after decompression surgery with stem cell injection, where 0 is no pain and 10 is the worst imaginable. The mean preoperative VAS score is 3.92, and the mean postoperative score drops to 2.62. Also shown is the 95% confidence interval for each bar.
Discussion
We present a consecutive series of patients with pre-collapse (Ficat stage I and II) femoral head AVN lesions treated with core decompression and biological augmentation using a single surgical technique. Our results for treating pre-collapse AVN of the femoral head with decompression augmented by autologous concentrated bone marrow injection reinforce the results of other case series and randomised control trials.5,11,13–17 Moreover, the results presented above further the case against non-operative treatment, which has been shown to lead to 80% of patients requiring a salvage operation, which is double the rate presented here.20
Physiologically, the goal of this procedure is to stimulate new bone formation and replace the bone marrow of the femoral head with viable, new stem cell progenitors, as patients with AVN have been shown to have a decreased stem cell population in their area of necrosis.3,18 Compared to only hip decompression, the addition of concentrated bone marrow has been shown to improve clinical outcomes such as pain and function and may retard the radiographic progression of disease.13 This was reflected in our patients as well, as over 50% experienced at least a two-point decrease in pain VAS scores after the operation. However, there are many factors that need to be considered in this study, namely the aetiology, the pre- and postoperative pain score, the patient age and failure rates before drawing a conclusion to say that our improved scores were solely due to the procedure.
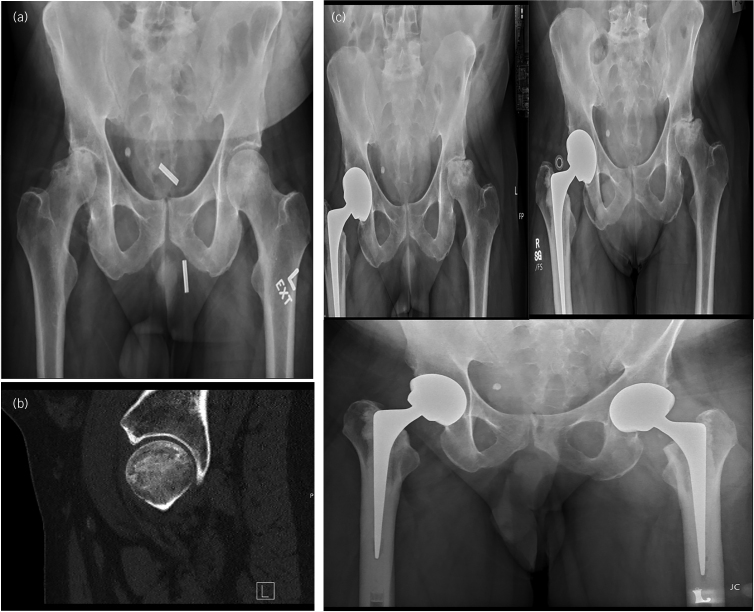
However, 38% of cases showed progression in symptoms and thus resulted in end-stage osteoarthritis requiring THA. One such example was of a young man with a one-year history of progressively worsening pain in his left hip and difficulty mobilising for long distances after suffering a tackling injury during a football match. He was treated with hip decompression and autologous stem cell progenitor implantation, which later had to be converted to THA because of worsening symptoms and disease progression. Figure 3a–c shows x-ray images of initial treatment, disease progression and post THA, respectively. Taking into consideration both personal and environmental factors, one could attribute the cause of failure in this patient to the large volume of head involved (a Mitchell ‘C’ classification), a rather dysmorphic original hip morphology and possible ligamentous laxity combined with inadequate rehabilitation. Additional factors to consider apart from the size of the lesion and underlying anatomical abnormalities may even include the playing surface and mechanism of injury.21
Figure 3 .
(a) Bilateral anteroposterior (AP) and left-sided lateral x-rays of the patient’s hip prior to hip decompression and stem cell injection showing the level of deterioration of the joint. (b) Bilateral MRI scan of the patient’s hips showing the progressive deterioration of the left hip. (c) Bilateral AP x-ray post left-sided total hip arthroplasty (THA).
Egger and Ballock have reiterated the detrimental effect of inhalational steroids on femoral head leading to osteonecrosis.22 This was a contributing factor in a further patient failure in this study. The patient presented with worsening pain in his right hip and trouble mobilising. He had significant comorbidities including bacterial endocarditis with valve replacement and regular anticoagulation, artificial pacing, hypertension, obesity, longstanding cigarette smoking and asthma requiring steroid treatment. Preoperative imaging is shown in Figure 4a. He underwent a right total hip replacement and decompression of the left hip at the same time. The postoperative MRI scan of the left hip can be seen in Figure 4b. Recurrent presentations revealed worsening pain in the left hip with collapse of the femoral head on imaging, warranting an eventual left-sided THA as shown in Figure 4c. One might argue that the resultant failure in this case was multifactorial and not limited to the use of steroids alone. Our study size has obvious limitations in examining these variables.
Figure 4 .
(a) Preoperative bilateral anteroposterior (AP) x-ray of the patient showing degeneration of both hips. (b) Postoperative lateral view computed tomography scan of left hip following decompression and autologous stem cell implantation. (c) Bilateral AP x-rays showing progressive worsening of left hip after surgical decompression and stem cell implantation, which eventually led to total hip arthroplasty (THA) of the left hip as well as the right.
Overall, the results of our study have been variable with a multitude of factors being responsible for failure of the procedure as listed in the Tables 1–4. Our results can be comparable to standard core decompression, but caution should be used in comparison with different populations owing to social, ethnic and disease-specific differences in AVN aetiology. In 1998, Iorio et al reported a study on 33 hips in 23 patients (followed for 5.3 years) who were treated with core decompression for early osteonecrosis of the femoral head (Ficat and Arlet I, IIA, IIB).23 The authors found no radiological progression of 61% at 2 years, with 70% overall patient satisfaction rate in those not undergoing THA.
Owing to the low incidence of the disease in our local population, we did not have a control to compare our results with. We therefore are unable to prove whether the success rates in our patients was solely due to core decompression or due to the additional injection of stem cell progenitors. We did find, however, that it added little additional morbidity or complexity to the procedure, with theoretical advantages that could be controlled for in larger studies.
Conclusion
Our study adds to the growing body of literature that femoral head core decompression combined with autologous bone marrow transplantation is a safe and effective way to treat early stage AVN of the hip. The surgical technique seems to be easier to guide radiologically than traditional drilling and allows simple introduction of concentrated bone marrow aspirate into the relatively acellular necrotic head. Our patients experienced no serious complications, and 65% had significant pain relief. It is of note that five patients who failed this treatment had significant comorbidities. For patients with Ficat stage I or II of the femoral head, early results suggest that hip core decompression combined with autologous bone marrow transplant appears to be a viable treatment option to provide symptomatic relief, particularly in patients with no comorbidities or smaller zones of head involvement; however, our sample size was small, so this trend should be investigated fully in future studies.
References
- 1.Lau RL, Perruccio AV, Evans HMKet al. Stem cell therapy for the treatment of early stage avascular necrosis of the femoral head: A systematic review. BMC Musculoskelet Disord 2014; 15: 10. 10.1186/1471-2474-15-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjorkman A, Svensson PJ, Hillarp Aet al. Factor V Leiden and prothrombin gene mutation. Clinical Orth Relat Res 2004; 425: 168–172. 10.1097/00003086-200408000-00023 [DOI] [PubMed] [Google Scholar]
- 3.Marcacci M, Andriolo L, Kon Eet al. Aetiology and pathogenesis of bone marrow lesions and osteonecrosis of the knee. Efort Open Rev 2016; 1: 219–224. 10.1302/2058-5241.1.000044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg 1999; 7: 250–261. 10.5435/00124635-199907000-00005 [DOI] [PubMed] [Google Scholar]
- 5.Hernigou P, Trousselier M, Roubineau Fet al. Stem cell therapy for the treatment of hip osteonecrosis: A 30-year review of progress. Clin Orthop Surg 2016; 8: 1–8. 10.4055/cios.2016.8.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mont A, Jones CL, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: Ten years later (vol 88, pg 1117, 2006). J Bone Joint Surg Am 2006; 88A: 1117–1132. [DOI] [PubMed] [Google Scholar]
- 7.Jones JP. Intravascular coagulation and osteonecrosis. Clinical Orth Relat Res 1992; 277: 41–53. [PubMed] [Google Scholar]
- 8.Glueck CJ, Freiberg RA, Wang P. Heritable thrombophilia-hypofibrinolysis and osteonecrosis of the femoral head. Clinical Orth Relat Res 2008; 466: 1034–1040. 10.1007/s11999-008-0148-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cornell CN, Salvati EA, Pellicci PM. Long-term follow-up of total hip-replacement in patients with osteonecrosis. Orthop Clin North Am 1985; 16: 757–769. 10.1016/S0030-5898(20)30442-9 [DOI] [PubMed] [Google Scholar]
- 10.Issa K, Pivec R, Kapadia BHet al. Osteonecrosis of the femoral head the total hip replacement solution. Bone Joint J 2013; 95B: 46–50. 10.1302/0301-620X.95B11.32644 [DOI] [PubMed] [Google Scholar]
- 11.Makihara T, Yoshioka T, Sugaya Het al. Autologous concentrated bone marrow grafting for the treatment of osteonecrosis of the humeral head: A report of five shoulders in four cases. Case Rep Orthop 2017; 2017: 4898057. 10.1155/2017/4898057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang GJ, Dughman SS, Reger SI, Stamp WG. The effect of core decompression on femoral-head blood-flow in steroid-induced avascular necrosis of the femoral-head. J Bone Joint Surg Am 1985; 67A: 121–124. 10.2106/00004623-198567010-00015 [DOI] [PubMed] [Google Scholar]
- 13.Tabatabaee RM, Saberi S, Parvizi Jet al. Combining concentrated autologous bone marrow stem cells injection with core decompression improves outcome for patients with early-stage osteonecrosis of the femoral head: A comparative study. J Arthroplasty 2015; 30: 11–15. 10.1016/j.arth.2015.06.022 [DOI] [PubMed] [Google Scholar]
- 14.Daltro GC, Fortuna V, de Souza ESet al. Efficacy of autologous stem cell-based therapy for osteonecrosis of the femoral head in sickle cell disease: A five-year follow-up study. Stem Cell Res Ther 2015; 6: 18. 10.1186/s13287-015-0105-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sen RK, Tripathy SK, Aggarwal Set al. Early results of core decompression and autologous bone marrow mononuclear cells instillation in femoral head osteonecrosis A randomized control study. J Arthroplasty 2012; 27: 679–686. 10.1016/j.arth.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 16.Zhao DW, Cui DP, Wang BJet al. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone 2012; 50: 325–330. 10.1016/j.bone.2011.11.002 [DOI] [PubMed] [Google Scholar]
- 17.Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clinical Orth Relat Res 2002; 405: 14–23. 10.1097/00003086-200212000-00003 [DOI] [PubMed] [Google Scholar]
- 18.Gangji V, Hauzeur JP, Schoutens Aet al. Abnormalities in the replicative capacity of osteoblastic cells in the proximal femur of patients with osteonecrosis of the femoral head. J Rheumatol 2003; 30: 348–351. [PubMed] [Google Scholar]
- 19.Lamb JN, Holton C, O'Connor P, Giannoudis PV. Avascular necrosis of the hip. Br Med J 2019; 365: 4. [DOI] [PubMed] [Google Scholar]
- 20.Mont MA, Carbone JJ, Fairbank AC. Core decompression versus nonoperative management for osteonecrosis of the hip. Clinical Orth Relat Res 1996; 324: 169–178. 10.1097/00003086-199603000-00020 [DOI] [PubMed] [Google Scholar]
- 21.Schuh A, Doleschal S, Schmickal T. Anterior hip dislocation in a football player: A case report. Case Rep Med 2009; 2009: 363461. 10.1155/2009/363461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egger AC, Ballock RT. Osteonecrosis of the femoral head in an adolescent on long-term inhalational corticosteroids. Case Rep Pediatr 2017; 2017; 6969787. 10.1155/2017/6969787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iorio R, Healy WL, Abramowitz AJ, Pfeifer BA. Clinical outcome and survivorship analysis of core decompression for early osteonecrosis of the femoral head. J Arthroplasty 1998; 13: 34–41. 10.1016/S0883-5403(98)90073-0 [DOI] [PubMed] [Google Scholar]