Abstract
Objectives
High-intensity interval training (HIT) improves peak oxygen consumption (VO2peak) in de novo heart transplant (HTx) recipients. It remains unclear whether this improvement early after HTx is solely dependent on peripheral adaptations, or due to a linked chain of central and peripheral adaptations. The objective of this study was to determine whether HIT results in structural and functional adaptations in the cardiovascular system.
Methods
Eighty-one de novo HTx recipients were randomly assigned to participate in either 9 months of supervised HIT or standard care exercise-based rehabilitation. Cardiac function was assessed by echocardiogram and the coronary microcirculation with the index of microcirculatory resistance (IMR) at baseline and 12 months after HTx.
Results
Cardiac function as assessed by global longitudinal strain was significantly better in the HIT group than in the standard care group (16.3±1.2% vs 15.6±2.2%, respectively, treatment effect = –1.1% (95% CI –2.0% to –0.2%), p=0.02), as was the end-diastolic volume (128.5±20.8 mL vs 123.4±15.5 mL, respectively, treatment effect=4.9 mL (95% CI 0.5 to 9.2 mL), p=0.03). There was a non-significant tendency for IMR to indicate improved microcirculatory function (13.8±8.0 vs 16.8±12.0, respectively, treatment effect = –4.3 (95% CI –9.1 to 0.6), p=0.08).
Conclusion
When initiated early after HTx, HIT leads to both structural and functional cardiovascular adaptations.
Trial registration number
Keywords: Exercise rehabilitation, Cardiology prevention, Exercise testing, Prevention
WHAT IS ALREADY KNOWN ON THIS TOPIC
High-intensity interval training compared with standard of care exercise-based rehabilitation early after heart transplantation improves peak oxygen consumption.
High-intensity interval training attenuates epicardial cardiac allograft vasculopathy progression in heart transplant recipients.
WHAT THIS STUDY ADDS
First reported evidence of cardiovascular adaptations in de novo heart transplant recipients related to exercise rehabilitation.
High-intensity interval training compared with standard of care exercise-based rehabilitation early after heart transplantation leads to cardiovascular adaptations and improved cardiac function.
High-intensity interval training may result in improved coronary microcirculatory function.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Exercise with higher intensity than recommended by the European Society of Cardiology may be considered safe in clinically stable de novo heart transplant recipients.
The exercise-based rehabilitation programme in de novo heart transplant recipients should be tailored individually for each patient.
The relationship between exercise intensity and cardiovascular adaptations needs further investigation.
Introduction
Previous studies have shown that peak oxygen consumption (VO2peak) is reduced in heart transplant (HTx) recipients. More than half of HTx recipients function in New York Heart Association class II, III or IV at 1 year after HTx.1 High-intensity interval training (HIT) in non-HTx populations has been demonstrated to be more effective than moderate-intensity continuous training (MICT) in improving VO2peak, preventing the onset and development of coronary artery disease and improving outcomes for patients with established cardiovascular disease.2–5 These beneficial effects of HIT are of particular interest in HTx recipients, many of whom develop hypertension, diabetes, cardiac allograft vasculopathy (CAV), left ventricular (LV) dysfunction and reduced exercise capacity.6–8
While exercise in HTx recipients has been recommended with caution for several decades, the High-Intensity Interval Training in De Novo Heart Transplant Recipients in Scandinavia (HITTS) trial demonstrated that early initiation of HIT in de novo HTx recipients is both safe and superior to standard care exercise-based rehabilitation in improving VO2peak.9 Based on measurements of increased muscle strength, the authors concluded that the improvement in VO2peak was mainly due to peripheral factors. However, the exercise-induced improvement in VO2peak is usually related to structural and functional adaptations occurring within a linked chain of central and peripheral systems, including pulmonary ventilation, cardiovascular function and the ability of muscle cells to utilise oxygen.10 Although the precise mechanisms have proved elusive, exercise-induced adaptations are believed to include favourable ventricular remodelling, angiogenesis and increased blood flow capacity, all of which may lead to increased cardiac output.11 12 In addition, there is increasing evidence that epicardial and microvascular allograft vasculopathy can develop and progress independently and serve as independent predictors of adverse outcomes.13 14 HIT has been shown to attenuate epicardial CAV progression in HTx recipients, but the effect of HIT on coronary microcirculation has not been reported.15 16
The global longitudinal strain (GLS) has increasingly been used to quantify LV function in clinical practice and graft monitoring due to its accuracy in detecting subclinical LV changes compared with LV ejection fraction (LVEF) and Doppler parameters.17 18 Coronary physiology investigations related to coronary angiography include calculations of the index of microcirculatory resistance (IMR), which is a specific and reproducible measure of microvascular function.19 20 Since VO2 peak increased in the main HITTS trial, this HITTS substudy aimed to determine the HIT outcomes in structural and functional cardiovascular adaptations.
Material and methods
This study was approved by the South-East Regional Committee for Medical and Health Research Ethics in Norway (ref no: 2012/2305) and registered at ClinicalTrials.gov. The study was conducted according to the Declaration of Helsinki, with written informed consent obtained from all participants.
Study population
This was a substudy of the multicentre HITTS trial in which stable de novo HTx recipients of either sex aged ≥18 years were eligible for inclusion between February 2013 and February 2017. Bicaval anastomosis was used as the surgical technique for all of the HTx patients. The design and results of the HITTS trial have been reported in detail previously.9 21 Within 13 weeks after HTx, 81 recipients were randomly assigned to receive 9 months of either supervised HIT or MICT. MICT is equivalent to standard care exercise-based cardiac rehabilitation as recommended by the European Society of Cardiology.22 Similar lifestyle advice was given to recipients in the HIT and standard care groups. HIT consisted of four 4 min intervals at 85%–95% of the peak effort separated by 3 min of active recovery at 60%–70% of the peak effort. Standard care consisted of 25 min of continuous training at 60%–80% of the peak effort. Supplementary strength training was applied equally in the two groups. Each patient completed approximately 60 exercise sessions during the intervention period.
Outcomes
The primary outcome measures were the changes in LV GLS, LV dimensions (interventricular septal thickness at end-diastole; IVSd, left ventricular posterior wall at end-diastole; LVPWd, left ventricular internal diameter at end-diastole; LVIDd) and end-diastole volume (EDV) assessed by echocardiography. The secondary outcome was the changes in the IMR and coronary flow reserve (CFR).
2D—transthoracic echocardiography
Transthoracic echocardiography was performed using a commercially available ultrasound system (GE Vivid E9 and GE Vivid E95, General Electric, Chicago, Illinois) with a 1.3–4.2 MHz phased array transducer. All postprocessing analyses were performed offline by the same researcher while blinded to the interventional status using EchoPAC plug-in V.2.04 to third-party PACS, General Electric, Chicago, Illinois. LV dimensions were quantified in the parasternal view by placing callipers perpendicular to the ventricular long axis. LV mass was calculated as LV mass=0.8 (1.04(LVD+IVS+PW)3—LVD3+0.6 g. Peak E-wave and peak A-wave velocities were obtained with pulsed wave (PW) Doppler between mitral leaflet tips in a four-chamber view. The mitral valve (MV) E/A ratio was calculated by dividing the E-wave velocity by the A-wave velocity. The MV deceleration time was obtained from PW Doppler between mitral leaflet tips. Stroke volume (SV) was estimated by multiplying the velocity–time integral at the LV outflow tract by the LV outflow tract area. The LV volumes were acquired tracing the LV endocardial border in apical four-chamber and two-chamber views. The change in LV volumes between end-systole and end-diastole allowed estimation of LVEF. Strains were obtained by tracing 2D speckle in images from three apical views. GLS was calculated as the mean strain of 18 segments.
Coronary physiology
Cardiac catheterisation was performed following the standard procedure at our laboratory at Oslo University Hospital, Oslo, Norway, with radial access being preferred. A pressure-temperature sensor guidewire (Certus Pressure Wire or Pressure Wire X, Abbot, Lake County, Illinois) was used for physiology measurements. A pressure measurement made using the wire was first equalised with the guiding catheter and then positioned in the distal third of the left anterior descending artery. Intracoronary glyceryl trinitrate (200 µg) was administered at the beginning of the procedure and repeated if necessary. Maximum hyperemia was induced by infusing 140 µg/kg/min adenosine through a large antecubital vein. Saline (3–4 mL) at ambient temperature was injected three times or until stable measurements were acquired in the resting state and also during maximum hyperemia. The transit time of saline from the thermistor in the guidewire shaft to the distal thermistor was recorded in the resting state (Tmnr) and during maximum hyperemia (Tmnh), as were the aortic pressure (Pa) and distal coronary pressure (Pd). The coronary physiology indices were calculated as follows:
FFR=Pd/Pa at maximum hyperemia (averaged over three heart beats for which its value was the lowest).
IMR=Pd×Tmnh
CFR=Tmnr/Tmnh
The continuous equalisation of pressures was confirmed at the end of the procedure by repositioning the pressure wire in the ostium of the vessel. The coronary physiology measurements were made in approximately the same position in the vessel during the second heart catheterisation procedure.
Biochemical and blood pressure assessment
The blood samples were collected prior to the testing regardless of group adherence. Blood samples collected at baseline and 12 months were analysed for the complete blood cell count and by performing serum biochemical tests, including high-sensitivity C reactive protein (CRP), creatine kinase, troponin T, N-terminal pro B-type natriuretic peptide, haemoglobin, cholesterol, triglycerides and electrolytes. Serum concentrations were measured using standard laboratory techniques. A 24-hour blood pressure measurement was carried out during the hospital stay. The equipment was removed in connection with the testing and right catheterisation.
Rejection score
The presence of cellular rejection was based on the revised version of the 1990 working formulation for the standardisation of nomenclature in the diagnosis of heart rejection as follows: grade 1 R, mild rejection; grade 2 R, moderate rejection; and grade 3 R, severe rejection.23 The rejection score was calculated as (number of grade−1−R rejections)×1 + (number of grade−2−R rejections)×2 + (number of grade−3−R rejections)×3.
Statistical analyses
All data were analysed using standard statistical software (Stata/SE V.16, Stata Corporation, College Station, Texas). Histograms and Q-Q plots were used to check whether continuous variables conformed to a normal distribution; those that did are reported as mean±SD or median with IQR values. Baseline variables were compared using the t-test or Mann-Whitney U test as appropriate. Categorical data are presented as absolute values with percentages. Baseline variables were compared using the χ2 test or Fisher’s exact test as appropriate. Mixed-effects multilevel regression was used to detect treatment effects in repeated measurements. All reported p values were two-sided, and the threshold for statistical significance was set at p<0.05.
Results
Patient population
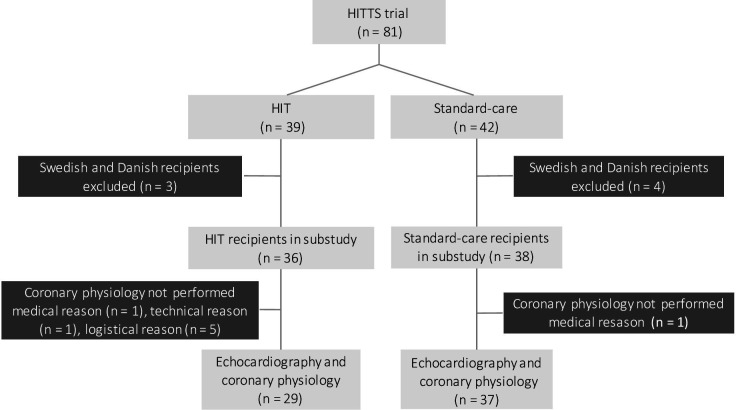
In the multicentre HITTS trial, coronary physiology measurements were planned only in HTx recipients from Oslo University Hospital, Rikshospitalet, Oslo, Norway, and they were eligible for enrolment in the current substudy. Patients who were included for the main HITTS trial at Sahlgrenska University Hospital, Gothenburg, Sweden and at Rikshospitalet, Copenhagen, Denmark were excluded from the current substudy. This criterion resulted in the inclusion of 74 recipients. Figure 1 displays a flowchart of the participants. There were more recipients with coronary physiology measurements in the standard care group (n=37) than in the HIT group (n=29). Examinations were missed at random in each group, and, hence, this did not result in selection bias. The adherence to training was 94% in the HIT group and 97% in the Standard care group. The mean exercise session bout in the HIT group increased from 2.3±0.7 min in the first period to 3.6±0.7 min in the last period. The mean length of the exercise session in the Standard care group was 56±13 min throughout the intervention period. Transthoracic echocardiogram images obtained at baseline and 12 months were available for all of the included HTx recipients. None of the recipients were lost to follow-up. There were no severe complications related to any of the procedures in the study, and all of the included patients were alive after 12 months of follow-up.
Figure 1.
HIT, high-intensity interval training; HITTS, High-Intensity Interval Training in De Novo Heart Transplant Recipients in Scandinavia.
Baseline characteristics
None of the clinical characteristics and medication differed significantly between the groups at baseline (table 1). Five (8%) of the recipients had undergone previous HTx. The leading cause of HTx was dilated cardiomyopathy (42%). The recipients were aged 52 (40–58) years and 47 (71%) of them were men, while the donors were aged 33 (23–48) years and 45 (68%) of them were men. The cold ischaemic time was 211 (94–240) min. Standard immunosuppressive medication was given according to local protocols. Forty-eight (73%) of the patients were treated with cyclosporine, 18 (27%) were treated with tacrolimus and 21 (32%) were treated with everolimus. All except one of the recipients were using statins. The body mass index (BMI) at the time of inclusion was 25±4 kg/m².
Table 1.
Patient characteristics and medications at baseline
| HIT (n=29) | Standard care (n=37) | P | |
| Characteristic | |||
| Age of donor, years | 29 (22 to 46) | 34 (29 to 48) | 0.25 |
| Sex of donor, male | 19 (66) | 26 (70) | 0.68 |
| Cold ischaemic time, min | 205 (92 to 235) | 214 (95 to 245) | 0.56 |
| Age of recipient, years | 52 (42 to 58) | 52 (40 to 57) | 0.90 |
| Sex of recipient, male | 20 (69) | 27 (73) | 0.72 |
| LVAD | 4 (14) | 6 (16) | 0.79 |
| Reason for transplantation | 0.22 | ||
| DCM | 14 (48) | 14 (38) | |
| ICM | 9 (31) | 8 (22) | |
| Other | 6 (21) | 15 (41) | |
| Immunosuppressant | |||
| Cyclosporine | 20 (69) | 28 (76) | 0.54 |
| Tacrolimus | 9 (31) | 9 (24) | 0.54 |
| Everolimus | 10 (34) | 11 (30) | 0.68 |
| Mycophenolate | 26 (90) | 33 (89) | 1.00 |
| Prednisolone | 29 (100) | 37 (100) | 1.00 |
| Medication at baseline | |||
| Antiplatelet agents | 4 (14) | 4 (11) | 0.72 |
| Anticoagulation | 4 (14) | 2 (5) | 0.39 |
| Beta-blockers | 8 (28) | 11 (30) | 0.85 |
| ACE inhibitors | 0 (0) | 1 (3) | 1.00 |
| Angiotensin-receptor blockers | 2 (7) | 1 (3) | 0.58 |
| Statins | 28 (97) | 37 (100) | 0.44 |
| Diuretics | 25 (86) | 31 (84) | 1.00 |
Data are n (%), median (IQR), or mean±SD values. p values are for between-groups comparisons at baseline.
ACE, angiotensin-converting enzyme; DCM, dilated cardiomyopathy; HIT, high-intensity interval training; ICM, ischaemic cardiomyopathy; LVAD, left ventricular assist device.
Transthoracic echocardiography
Analysis of GLS reproducibility showed good to excellent intraobserver and interobserver agreement levels. The intraclass correlation coefficient (ICC) for intrarater reliability was 0.99 (95% CI 0.95 to 0.99) and ICC for inter-rater reliability was 0.88 (95% CI 0.60 to 0.97). The failure rate for analysing GLS was 22%. The average framerate of images that was analysed for GLS was 59.8 frames/s. Manual contour adjustment was performed and optimised for all patients.
The treatment effect on LV morphology is presented in table 2. The GLS and LV end-diastolic volume (LVEDV) were significantly higher in the HIT group than in the standard care group. The treatment effect on GLS was –1.1% (95% CI −2.0% to –0.2%, p<0.05), and that on LVEDV was 4.9 mL (95% CI 0.5 to 9.2 mL, p<0.05). There were significant changes in LV end-diastolic dimensions in the standard care group, including in the IVSd, LVPWd, LVIDd, and LVPWd in the HIT group.
Table 2.
Transthoracic echocardiography
| HIT | Standard care | Treatment effect | P | |||
| n=29 | n=37 | |||||
| Baseline | 12 months | Baseline | 12 months | Change (95% CI) | ||
| Dimensions | ||||||
| IVSd (mm) | 10.2±1.5 | 9.9±1.3 | 10.6±1.6 | 10.3±1.5* | 0.03 (–0.28 to 0.33) | 0.86 |
| LVPWd (mm) | 9.1±1.3 | 8.9±1.2* | 9.2±1.0 | 8.9±1.0* | 0.03 (–0.26 to 0.32) | 0.83 |
| LVIDd (mm) | 48.4±4.8 | 48.3±5.0 | 48.6±4.1 | 47.6±4.4* | 0.6 (–0.1 to 1.3) | 0.09 |
| IVSs (mm) | 13.8±1.3 | 13.7±1.2 | 14.1±1.3 | 14.3±2.3 | –0.3 (–0.9 to 0.4) | 0.43 |
| LVPWs (mm) | 14.7±1.4 | 14.6±1.2 | 14.8±1.2 | 14.7±1.1 | 0.1 (–0.1 to 0.4) | 0.32 |
| LVIDs (mm) | 31.9±2.7 | 32.1±3.2 | 31.5±3.4 | 31.1±3.4 | 0.5 (–0.1 to 1.2) | 0.12 |
| LVM ACE (gr) | 157.3±28.9 | 158.5±30.5 | 157.6±25.4 | 153.7±26.7 | 4.6 (–1.6 to 10.8) | 0.14 |
| LVMI ACE (gr) | 81.8±12.9 | 80.7±13.5 | 82.0±10.6 | 79.3±12.1 | 1.8 (–2.0 to 5.6) | 0.35 |
| Diastolic function | ||||||
| EA-ratio | 1.88±0.37 | 1.86±0.39 | 1.92±0.63 | 1.86±0.38 | 0.02 (–0.22 to 0.26) | 0.88 |
| IVRT (ms) | 85±14 | 83±12 | 87±13 | 89±15 | –3.0 (–9.6 to 3.5) | 0.37 |
| EdecT (ms) | 162±28 | 158±27 | 165±27 | 160±29 | 3.1 (–14.1 to 18.4) | 0.79 |
| Systolic function | ||||||
| HR (beats/min) | 88±11 | 89±12 | 82±11 | 87±11 | –3.5 (–8.7 to 1.7) | 0.19 |
| SV (mL) | 66.5±13.8 | 66.4±14.8 | 72.5±14.3 | 69.6±14.4 | 2.6 (–1.3 to 8.9) | 0.15 |
| CO, L/min | 5.8±1.2 | 5.8±1.1 | 5.9±1.1 | 5.9±1.0 | 0.09 (–0.27 to 0.46) | 0.62 |
| CI, L/min/m2 | 3.1±0.5 | 3.0±0.6 | 3.1±0.5 | 3.0±0.5 | –0.003 (–0.208 to 0.201) | 0.97 |
| EF Biplan (%) | 54±3 | 54±3 | 55±3 | 54±2* | 1.1 (–0.2 to 2.3) | 0.09 |
| GLS (%) | 15.8±1.7 | 16.3±1.2 | 16.1±2.2 | 15.6±2.2 | –1.1 (–2.0 to –0.2) | 0.02 |
| EDV (mL) | 128.2±19.0 | 128.5±20.8 | 128.0±16.3 | 123.4±15.5* | 4.9 (0.5 to 9.2) | 0.03 |
| ESV (mL) | 60.0±10.0 | 59.3±10.9 | 57.6±7.8 | 56.7±7.5 | –0.2 (–2.8 to 2.5) | 0.91 |
Data are mean±SD values or mean (95% CI). p values are from mixed-effects multilevel regression and are for between-groups comparisons.
*P<0.05 within group.
CI, cardiac index; CO, cardiac output; EdecT, e deceleration time; EDV, end diastolic volume; EF, ejection fraction; ESV, end systolic volume; GLS, global longitudinal strain; HIT, high-intensity interval training; IVRT, isovolumic relaxation time; IVSd, interventricular septal end diastole; IVSs, interventricular septal end systole; LVIDd, left ventricular internal diameter end diastole; LVIDs, left ventricular internal diameter end systole; LVM, left ventricular mass; LVMI, left ventricular mass index; LVPWd, left ventricular posterior wall end diastole; LVPWs, left ventricular posterior wall end systole; SV, stroke volume.
The LV end-diastolic dimensions decreased significantly in the overall study population: IVSd from 10.4±1.6 mm to 10.2±1.4 mm (change=0.3 mm, (95% CI 0.1 mm to 0.4 mm, p<0.05), LVPWd from 9.1±1.1 mm to 8.9±1.1 mm (change=0.3 mm), (95% CI 0.1 mm to 0.4 mm, p<0.05) and LVIDd from 48.5±4.4 mm to 47.9±4.7 mm (change=0.6 mm) (95% CI 0.3 mm to 1.0 mm, p<0.05). The heart rate (HR), SV, cardiac mass, cardiac index and diastolic function parameters did not change significantly. There was no significant correlation between VO2peak and GLS at 12 months (r=–0.13, p=0.42).
Quantitative coronary physiology assessment
The results of the coronary physiology assessment are presented in table 3. IMR improved in the HIT group and worsened in the standard care group. The difference in the IMR change between the two treatment arms was –4.3 mm Hg∙s (95% CI −9.1 to 0.6 mm Hg∙sec, p=0.08). CFR increased in the HIT group but remained virtually unchanged in the standard care group (change=0.8, 95% CI −0.8 to 2.3, p=0.32). The difference in fractional flow reserve between the groups was negligible. There was no significant correlation between VO2peak and IMR after 12 months (r=0.24, p=0.08), or between IMR and GLS (r=0.26, p=0.12). However, in a linear regression model, IMR was significantly related to LVEF (r=−0.37, p<0.05).
Table 3.
Coronary physiology measurements
| HIT | Standard care | Treatment effect | P | |||
| n=29 | n=37 | |||||
| Baseline | 12 months | Baseline | 12 months | Change (95% CI) | ||
| Clinical features | ||||||
| IMR | 14.8±9.5 | 13.8±8.0 | 13.8±5.8 | 16.8±12.0 | –4.3 (–9.1 to 0.6) | 0.08 |
| FFR | 0.92±0.04 | 0.93±0.05 | 0.92±0.05 | 0.93±0.05 | 0.007(–0.02 to 0.04) | 0.61 |
| CFR | 4.0±2.5 | 4.8±2.9 | 4.2±2.1 | 4.1±1.9 | 0.8 (–0.8 to 2.3) | 0.32 |
Data are mean±SD values or mean (95% CI). P values are from mixed-effects multilevel regression and are for between-groups comparisons.
CFR, coronary flow reserve; FFR, fractional flow reserve; HIT, high-intensity interval training; IMR, index of microvascular resistance.
Exploratory variables
The exploratory variables are compared between groups in table 4. BMI, 24-hour blood pressure measurements, and CRPs were significantly higher in the HIT group than in the standard care group.
Table 4.
Exploratory variables
| HIT | Standard care | Treatment effect | P | |||
| n=29 | n=37 | |||||
| Baseline | 12 months | Baseline | 12 months | Change (95% CI) | ||
| Clinical features | ||||||
| Weight, kg | 75±13 | 81±16* | 78±15 | 81±17* | 2.9 (0.02 to 5.86) | 0.05 |
| Body mass index, kg/m2 | 24.4±3.3 | 26.4±4.0* | 25.3±3.9 | 26.3±4.3* | 1.0 (0.1 to 2.0) | 0.04 |
| Systolic BP, mm Hg | 131±10 | 139±11* | 133±13 | 135±15 | 6.7 (0.5 to 12.9) | 0.03 |
| Diastolic BP, mm Hg | 79±5 | 86±6* | 81±8 | 83±11 | 5.1 (1.0 to 9.1) | 0.01 |
| Biochemistry | ||||||
| CRP, mg/L | 2.7 (1.0 to 4.2) | 2.0 (0.6 to 5.5) | 2.3 (0.9 to 6.7) | 2.0 (0.6 to 3.8) | 8.2 (0.6 to 15.8) | 0.03 |
| HbA1c, % | 5.5 (5.1 to 6.4) | 5.8 (5.2 to 6.8) | 5.4 (5.0 to 6.0) | 5.5 (5.2 to 5.8) | 0.3 (–0.1 to 0.6) | 0.12 |
| Total cholesterol, mmol/L | 5.0 (4.6 to 5.8) | 5.1 (4.5 to 5.5) | 4.8 (4.3 to 5.7) | 4.5 (3.7 to 6.1) | –0.1 (–0.8 to 0.6) | 0.78 |
| LDL cholesterol, mmol/L | 2.8 (2.3 to 3.5) | 2.9 (2.4 to 3.2) | 2.7 (2.1 to 3.1) | 2.4 (2.0 to 3.3) | –0.2 (–0.6 to 0.3) | 0.43 |
| HS-troponin T, ng/L | 27 (19 to 66) | 11 (7 to 20)* | 33 (20 to 56) | 13 (8 to 27)* | –1.0 (–17.4 to 15.5) | 0.91 |
| NT-proBNP, pmol/L | 100 (64 to 217) | 42 (14 to 61)* | 108 (74 to 173) | 28 (19 to 58)* | –43 (–102 to 15) | 0.15 |
| Creatinine, µmol/L | 117±35 | 99±21* | 119±29 | 104±28* | –2.7 (–14.5 to 9.1) | 0.65 |
| Rejection score | 0.38 | |||||
| 0 | 19 (66) | 18 (62) | 22 (59) | 17 (46) | ||
| 1 | 6 (21) | 5 (17) | 7 (19) | 9 (24) | ||
| 2 | 1 (3) | 2 (7) | 4 (11) | 6 (16) | ||
| 3 | 2 (7) | 2 (7) | 1 (3) | 0 | ||
| 4 | 0 | 1 (3) | 1 (3) | 1 (3) | ||
| 5 | 0 | 0 | 2 (5) | 2 (5) | ||
| 6 | 1 (3) | 0 | 0 | 2 (5) | ||
| 7 | 0 | 0 | 0 | 0 | ||
| 8 | 0 | 1 (3) | 0 | 0 | ||
| Peak oxygens consumption, L/min | 1.5±0.4 | 2.0±0.6* | 1.6±0.4 | 2.0±0.6* | 0.2 (–0.01 to 0.33) | 0.06 |
| Right heart catheterisation | ||||||
| RAP, mm Hg | 5±3 | 4±3 | 5±3 | 4±3* | 0.7 (–1.2 to 2.6) | 0.46 |
| PCWP, mm Hg | 13±6 | 10±5* | 11±5 | 10±5 | –1.5 (–4.0 to 1.1) | 0.27 |
| CO, L/min | 7.0±1.7 | 7.0±1.9 | 6.6±1.7 | 6.9±1.5 | –0.2 (–1.0 to 0.6) | 0.59 |
| CI, L/min/m2 | 3.9±1.1 | 3.7±0.8 | 3.4±0.8 | 4.1±3.5 | –1.0 (–2.3 to 0.5) | 0.20 |
Data are n (%), median (IQR), or mean±SD values. P values are from mixed-effects multilevel regression and are for between-groups comparisons.
*P<0.05 within group.
CAV, cardiac allograft vasculopathy; CRP, C reactive protein; HbA1c, glycated haemoglobin; HIT, high-intensity interval training; HS, high sensitivity; LDL, low-density lipoprotein; NT-proBNP, N-terminal pro-brain natriuretic peptide.
Discussion
This substudy of the randomised controlled HITTS trial has demonstrated that initiating HIT early after HTx results in improved LV function as assessed by GLS and a change in IMR that indicates improved microcirculatory function.
HIT was more effective than standard care in improving VO2peak in the main HITTS trial.9 There was no difference between the exercise groups in the measured echocardiography and right catheterisation variables. As a result of improved muscle strength, the authors concluded that peripheral factors played a central role in improving VO2peak. Using the oxygen pulse as a surrogate marker for SV, the authors suggested that central factors were also involved in improving VO2peak. However, the results of the HITTS trial were based on non-dedicated routine echocardiography, and GLS was not analysed despite this parameter being independently correlated with VO2peak and superior to LVEF for identifying patients with reduced aerobic capacity.24 GLS is less operator dependent, more reproducible and more sensitive than LVEF for evaluating LV function.25 26
The temporal changes in LV morphology early after HTx are characterised by increases in LV wall thickness and mass due to inflammatory cell infiltration and graft oedema, which decrease successively during the first year. Although there is no description in the literature of cardiovascular adaptation arising from HIT in de novo HTx recipients, previous studies in athletes have suggested two different types of cardiac remodelling: (1) eccentric remodelling that results from volume load in endurance training with thickening of the LV wall and LV dilatation and (2) concentric remodelling resulting from pressure load in resistance training with increased myocardial mass and wall thickness without LV dilatation.27 28 Given that the wall thickness, including IVSd and LVPWd in the standard care group, reduced as expected, whereas IVSd remained unchanged in the HIT group, our findings in the latter group indicate the presence of cardiac remodelling without a single specific mechanism. However, given the significant intergroup difference in LVEDV, our findings suggest that HIT in de novo HTx recipients is closer to eccentric remodelling than concentric remodelling.
The increases in maximum HR in the HITTS trial were similar in the HIT and standard care groups.9 Thus, an increased cardiac output induced by HIT would be explained by an increased SV due to a larger ventricular volume or improved contractile function. A study evaluating the LV volume in endurance athletes using contrast echocardiography found that a large increase in SV in endurance athletes could be explained by an almost linear increase in LVEDV.29 Although the difference in SV between groups did not reach statistical significance, the GLS and LVEDV were both significantly higher in the HIT group than in the standard care group. Increased BP is associated with reduced GLS.30 Both the systolic and diastolic BP increased significantly in the HIT group, while it remained unchanged in the standard care group. In addition, the BP was significantly higher in the HIT group than in the standard care group at follow-up. These results suggest that HIT in de novo HTx recipients leads to remodelling of the left ventricle and (most likely) increased cardiac output as one of the mechanisms for the increased VO2peak observed in the HITTS trial.
Microvascular dysfunction is associated with the development of heart failure with a reduced LVEF in patients with diabetes, HT and hypertrophic cardiomyopathy.31 Vasodilatory capacity decreases and microvascular resistance increases as the heart ages, but the effects of exercise training on microvascular function in humans have not been studied extensively, especially for HTx recipients.32–37 In a rat model, exercise training was shown to reduce the age-related decline in microvascular function.38 In the current study, microvascular function as assessed with IMR and CFR improved in the HIT group but not in the standard care group during the first year after HTx. Although the difference between groups did not reach statistical significance, this tendency suggests that HIT improves coronary microcirculation compared with standard care.
In HTx recipients, the mean capillary density is only about half of that in non-HTx controls, which may significantly impact total microcirculatory resistance.39 Microvascular CAV is a concentric medial disease that affects more than 40% of HTx recipients, and it may also substantially impact microcirculatory resistance.39 However, exercise leads to adaptations in the myocardium that increases the maximum cardiac output and the maximum total body oxygen consumption.40 According to Duncker and Bache, exercise training is associated with adaptations in the coronary microvasculature, including increased arteriolar densities and diameters, and functional adaptations such as changes in neurohumoral control mechanism or in local vascular control mechanism, which all may contribute to increased oxygen supply to the myocardium.41 Our results indicate that HIT is an effective intervention to stimulate some or all of these mechanisms.42
Leung et al showed that LV contractile reserves as measured with low-dose dobutamine, echocardiography can be used to estimate IMR non-invasively, and that an impaired contractile reserve indicates microvascular dysfunction.43 In contrast, Kobayashi et al found that IMR does not correlate with GLS at 1 year after HTx, and that IMR and GLS may be used as independent predictors of late death or repeated HTx.44 In accordance with this, we also found that there was no correlation between IMR and GLS, and it seems like that the beneficial effects of HIT on LV function and the coronary microcirculation are mediated via different and independent mechanisms.
Our study had several limitations. The required sample size was primarily calculated for VO2peak in the main HITTS trial.21 This resulted in a small sample that restricted the statistical power of our results and may have resulted in type II errors, in particular, for the primary outcome of coronary physiology measurements. Also, the study protocol was prespecified and designed to only determine the effects of HIT on cardiac function and the coronary microcirculation. A better understanding of the mechanism underlying the improved IMR could have been obtained by reinvestigating myocardial biopsies. An improvement in VO2peak is usually expected after HTx, and it is unclear whether all of the observed improvements in our trial were caused by the exercise intervention rather than representing the natural course after HTx, since there was no control group.
Conclusion
This study found that early initiation of HIT in de novo HTx recipients results in beneficial adaptations of the cardiovascular system characterised by higher GLS, higher LVEDV and probably also improved microvascular function.
Footnotes
Contributors: MR, OGS, LG, BB, KN, KM and KL conceived the study and designed the analysis method. MR, OGS, KR and KL collected the data. MR, OGS and KL performed the analyses. MR, OGS and KL drafted the paper. LG, BB, KR and KM reviewed and edited the paper. KL was responsible for funding acquisition. MR and KL are responsible for the overall content.
Funding: This study was supported by Stiftelsen DAM (grant number 2018/FO189552). We thank the Department of Cardiology, Oslo University Hospital, Rikshospitalet for assistance during coronary physiology measurements, study nurse Elisabeth Bjørklund for coordinating the procedures, and Dr. Øyvind Lie for valuable discussions on performing statistical analyses and interpreting the results.
Competing interests: MR received institutional research grants from Stiftelsen DAM; LG received personal fees from Astra Zeneca, Boehringer Ingelheim, Novartis, and Amgen during the conduct of the study; None of the other authors have a conflict of interest to disclose.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. The data are not publicly available due to strict national guidelines on privacy policies and data sharing.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by South-East Regional Committee for Medical and Health Research Ethics in Norway (ref number: 2012/2305). Participants gave informed consent to participate in the study before taking part.
References
- 1.Niset G, Hermans L, Depelchin P. Exercise and heart transplantation. A review. Sports Med 1991;12:359–79. 10.2165/00007256-199112060-00003 [DOI] [PubMed] [Google Scholar]
- 2.Helgerud J, Høydal K, Wang E, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 2007;39:665–71. 10.1249/mss.0b013e3180304570 [DOI] [PubMed] [Google Scholar]
- 3.Ramos JS, Dalleck LC, Tjonna AE, et al. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports Med 2015;45:679–92. 10.1007/s40279-015-0321-z [DOI] [PubMed] [Google Scholar]
- 4.Bacon AP, Carter RE, Ogle EA, et al. VO2max trainability and high intensity interval training in humans: a meta-analysis. PLoS One 2013;8:e73182. 10.1371/journal.pone.0073182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wisløff U, Støylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 2007;115:3086–94. 10.1161/CIRCULATIONAHA.106.675041 [DOI] [PubMed] [Google Scholar]
- 6.Valantine H. Cardiac allograft vasculopathy after heart transplantation: risk factors and management. J Heart Lung Transplant 2004;23:S187–93. 10.1016/j.healun.2004.03.009 [DOI] [PubMed] [Google Scholar]
- 7.Perrier-Melo RJ, Figueira FAMDS, Guimarães GV, et al. High-intensity interval training in heart transplant recipients: a systematic review with meta-analysis. Arq Bras Cardiol 2018;110:188–94. 10.5935/abc.20180017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobashigawa JA, Leaf DA, Lee N, et al. A controlled trial of exercise rehabilitation after heart transplantation. N Engl J Med 1999;340:272–7. 10.1056/NEJM199901283400404 [DOI] [PubMed] [Google Scholar]
- 9.Nytrøen K, Rolid K, Andreassen AK, et al. Effect of high-intensity interval training in de novo heart transplant recipients in scandinavia. Circulation 2019;139:2198–211. 10.1161/CIRCULATIONAHA.118.036747 [DOI] [PubMed] [Google Scholar]
- 10.Bassett DR, Howley ET. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc 2000;32:70–84. 10.1097/00005768-200001000-00012 [DOI] [PubMed] [Google Scholar]
- 11.Scharf M, Schmid A, Kemmler W, et al. Myocardial adaptation to high-intensity (interval) training in previously untrained men with a longitudinal cardiovascular magnetic resonance imaging study (running study and heart trial). Circ Cardiovasc Imaging 2015;8:e002566. 10.1161/CIRCIMAGING.114.002566 [DOI] [PubMed] [Google Scholar]
- 12.Lee PT, Dweck MR, Prasher S, et al. Left ventricular wall thickness and the presence of asymmetric hypertrophy in healthy young army recruits: data from the LARGE heart study. Circ Cardiovasc Imaging 2013;6:262–7. 10.1161/CIRCIMAGING.112.979294 [DOI] [PubMed] [Google Scholar]
- 13.Fearon WF, Hirohata A, Nakamura M, et al. Discordant changes in epicardial and microvascular coronary physiology after cardiac transplantation: physiologic investigation for transplant arteriopathy II (PITA II) study. J Heart Lung Transplant 2006;25:765–71. 10.1016/j.healun.2006.03.003 [DOI] [PubMed] [Google Scholar]
- 14.Ahn J-M, Zimmermann FM, Arora S, et al. Prognostic value of comprehensive intracoronary physiology assessment early after heart transplantation. Eur Heart J 2021;42:4918–29. 10.1093/eurheartj/ehab568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nytrøen K, Rustad LA, Erikstad I, et al. Effect of high-intensity interval training on progression of cardiac allograft vasculopathy. J Heart Lung Transplant 2013;32:1073–80. 10.1016/j.healun.2013.06.023 [DOI] [PubMed] [Google Scholar]
- 16.Rafique M, Solberg OG, Gullestad L, et al. A randomized clinical study using optical coherence tomography to evaluate the short-term effects of high-intensity interval training on cardiac allograft vasculopathy: a HITTS substudy. Clin Transplant 2022;36:e14488. 10.1111/ctr.14488 [DOI] [PubMed] [Google Scholar]
- 17.Kalam K, Otahal P, Marwick TH. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 2014;100:1673–80. 10.1136/heartjnl-2014-305538 [DOI] [PubMed] [Google Scholar]
- 18.Clemmensen TS, Løgstrup BB, Eiskjær H, et al. Changes in longitudinal myocardial deformation during acute cardiac rejection: the clinical role of two-dimensional speckle-tracking echocardiography. J Am Soc Echocardiogr 2015;28:330–9. 10.1016/j.echo.2014.10.015 [DOI] [PubMed] [Google Scholar]
- 19.Ng MKC, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation 2006;113:2054–61. 10.1161/CIRCULATIONAHA.105.603522 [DOI] [PubMed] [Google Scholar]
- 20.Solberg OG, Ragnarsson A, Kvarsnes A, et al. Reference interval for the index of coronary microvascular resistance. EuroIntervention 2014;9:1069–75. 10.4244/EIJV9I9A181 [DOI] [PubMed] [Google Scholar]
- 21.Nytrøen K, Yardley M, Rolid K, et al. Design and rationale of the HITTS randomized controlled trial: effect of high-intensity interval training in de novo heart transplant recipients in Scandinavia. Am Heart J 2016;172:96–105. 10.1016/j.ahj.2015.10.011 [DOI] [PubMed] [Google Scholar]
- 22.Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the secondary prevention and rehabilitation section of the European Association of preventive cardiology. Eur J Prev Cardiol 2021;28:460–95. 10.1177/2047487320913379 [DOI] [PubMed] [Google Scholar]
- 23.Stewart S, Winters GL, Fishbein MC, et al. Revision of the 1990 working formulation for the standardization of nomenclature in the diagnosis of heart rejection. J Heart Lung Transplant 2005;24:1710–20. 10.1016/j.healun.2005.03.019 [DOI] [PubMed] [Google Scholar]
- 24.Hasselberg NE, Haugaa KH, Sarvari SI, et al. Left ventricular global longitudinal strain is associated with exercise capacity in failing hearts with preserved and reduced ejection fraction. Eur Heart J Cardiovasc Imaging 2015;16:217–24. 10.1093/ehjci/jeu277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karlsen S, Dahlslett T, Grenne B, et al. Global longitudinal strain is a more reproducible measure of left ventricular function than ejection fraction regardless of Echocardiographic training. Cardiovasc Ultrasound 2019;17:18. 10.1186/s12947-019-0168-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badano LP, Miglioranza MH, Edvardsen T, et al. European Association of cardiovascular imaging/cardiovascular imaging department of the Brazilian society of cardiology recommendations for the use of cardiac imaging to assess and follow patients after heart transplantation. Eur Heart J Cardiovasc Imaging 2015;16:919–48. 10.1093/ehjci/jev139 [DOI] [PubMed] [Google Scholar]
- 27.Mihl C, Dassen WRM, Kuipers H. Cardiac remodelling: concentric versus eccentric hypertrophy in strength and endurance athletes. Neth Heart J 2008;16:129–33. 10.1007/BF03086131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bjerring AW, Landgraff HE, Stokke TM, et al. The developing athlete’s heart: a cohort study in young athletes transitioning through adolescence. Eur J Prev Cardiol 2019;26:2001–8. 10.1177/2047487319862061 [DOI] [PubMed] [Google Scholar]
- 29.Sundstedt M, Hedberg P, Jonason T, et al. Left ventricular volumes during exercise in endurance athletes assessed by contrast echocardiography. Acta Physiol Scand 2004;182:45–51. 10.1111/j.1365-201X.2004.01304.x [DOI] [PubMed] [Google Scholar]
- 30.Stylidis M, Leon DA, Rӧsner A, et al. Global myocardial longitudinal strain in a general population-associations with blood pressure and subclinical heart failure: the Tromso study. Int J Cardiovasc Imaging 2020;36:459–70. 10.1007/s10554-019-01741-3 [DOI] [PubMed] [Google Scholar]
- 31.Mohammed SF, Redfield MM. Response to letters regarding article, "coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction" Circulation 2015;132:e206. 10.1161/CIRCULATIONAHA.115.017050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kyriakidis M, Triposkiadis F, Dernellis J, et al. Effects of cardiac versus circulatory angiotensin-converting enzyme inhibition on left ventricular diastolic function and coronary blood flow in hypertrophic obstructive cardiomyopathy. Circulation 1998;97:1342–7. 10.1161/01.cir.97.14.1342 [DOI] [PubMed] [Google Scholar]
- 33.Franssen C, Chen S, Unger A, et al. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction. JACC Heart Fail 2016;4:312–24. 10.1016/j.jchf.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 34.Csiszar A, Ungvari Z, Edwards JG, et al. Aging-induced phenotypic changes and oxidative stress impair coronary arteriolar function. Circ Res 2002;90:1159–66. 10.1161/01.res.0000020401.61826.ea [DOI] [PubMed] [Google Scholar]
- 35.Shipley RD, Muller-Delp JM. Aging decreases vasoconstrictor responses of coronary resistance arterioles through endothelium-dependent mechanisms. Cardiovasc Res 2005;66:374–83. 10.1016/j.cardiores.2004.11.005 [DOI] [PubMed] [Google Scholar]
- 36.Kang LS, Reyes RA, Muller-Delp JM. Aging impairs flow-induced dilation in coronary arterioles: role of NO and H(2)O(2). Am J Physiol Heart Circ Physiol 2009;297:H1087–95. 10.1152/ajpheart.00356.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leblanc AJ, Chen B, Dougherty PJ, et al. Divergent effects of aging and sex on vasoconstriction to endothelin in coronary arterioles. Microcirculation 2013;20:365–76. 10.1111/micc.12028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hotta K, Chen B, Behnke BJ, et al. Exercise training reverses age-induced diastolic dysfunction and restores coronary microvascular function. J Physiol 2017;595:3703–19. 10.1113/JP274172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Escaned J, Flores A, García-Pavía P, et al. Assessment of microcirculatory remodeling with intracoronary flow velocity and pressure measurements: validation with endomyocardial sampling in cardiac Allografts. Circulation 2009;120:1561–8. 10.1161/CIRCULATIONAHA.108.834739 [DOI] [PubMed] [Google Scholar]
- 40.Evans DL. Cardiovascular adaptations to exercise and training. Vet Clin North Am Equine Pract 1985;1:513–31. 10.1016/s0749-0739(17)30748-4 [DOI] [PubMed] [Google Scholar]
- 41.Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev 2008;88:1009–86. 10.1152/physrev.00045.2006 [DOI] [PubMed] [Google Scholar]
- 42.Yardley M, Ueland T, Aukrust P, et al. Immediate response in markers of inflammation and angiogenesis during exercise: a randomised cross-over study in heart transplant recipients. Open Heart 2017;4:e000635. 10.1136/openhrt-2017-000635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leung M, Juergens CP, Lo ST, et al. Evaluation of coronary Microvascular function by left ventricular contractile Reserve with low-dose dobutamine echocardiography. EuroIntervention 2014;9:1202–9. 10.4244/EIJV9I10A202 [DOI] [PubMed] [Google Scholar]
- 44.Kobayashi Y, Kobayashi Y, Yang H-M, et al. Long-term prognostic value of invasive and non-invasive measures early after heart transplantation. Int J Cardiol 2018;260:31–5. 10.1016/j.ijcard.2018.01.070 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available. The data are not publicly available due to strict national guidelines on privacy policies and data sharing.