Abstract
Objectives
It is estimated that NHS staff consist of over 200 different nationalities, with a reported 30.7% of doctors holding a nationality other than British. Despite this, international medical students represent 7.5% of all medical students studying in the UK and pay on average, 4–6 times more in tuition fees when compared with the £9250 per annum (Great British Pounds (£) in 2021) paid by home students. This study’s aim and objective are to evaluate the perception of the financial cost and value of the UK medical degree for international students and their motivations for pursuing such a degree.
Methods
This is a cross-sectional observational study enquiring about international premedical, medical and medical school graduates’ perception of the value of the UK medical degree and factors influencing their decision to study in the UK.
A questionnaire was developed and distributed to 24 medical schools and 64 secondary schools both internationally and across the UK.
Results
A total of 352 responses from 56 nationalities were recorded. 96% of international students identified clinical and academic opportunities as the most important factors to study medicine in the UK, closely followed by quality of life (88%). The least important factor was family reasons, with 39% of individuals identifying this factor. Only 4.82% of graduates in our study considered leaving the UK after training. Overall, 54% of students felt the UK degree was value for money. This belief was significantly higher in premedical students compared with existing students and graduates (71% vs 52% and 20%, p<0.001 for all comparisons).
Conclusion
The quality of medical education and international prestige are attractive factors for international students to study medicine in the UK. However, further work is needed to ascertain reasons for the differing perceptions of the value by international students at different stages in their clinical training.
Keywords: medical education, international students, postgraduate training
STRENGTHS AND LIMITATIONS OF THIS STUDY.
First study that systematically evaluate the perceptions of premedical, medical and postgraduate international doctors on the value of a UK medical degree.
Selection bias as study survey targeted 24 medical schools and 64 secondary schools that were known to the study team.
Small sample size in postgraduate students further biases the subgroup comparison.
Introduction
The undergraduate medical degree is a highly popular and competitive degree in the UK with over 23 710 applicants (inclusive of British citizens, residents with settled status or overseas students) competing for less than 8000 places in 2021.1
International students traditionally account for a small percentage of medical students, as the annual intake is capped at 7.5% for the full cohort.2–6 In the UK, international students pay higher tuition fees compared with ‘home’ students (British citizens or residents with settled status) studying the same degree. Home students’ fees are currently capped at £9250 (Great British Pounds (£) in 2021) per annum2–4 while international fees are 4–6 higher, with the latter having the additional burden of their fees being subject to annual inflation as per the Retail Price Index.2 4 Furthermore, the ‘additional cost of training’ (ACT) levy was introduced in Scottish medical schools in 2016,4 and to Northern Irish medical schools in 2021.7 ACT levy is the additional medical training costs introduced for overseas students studying in the UK to finance clinical skills training on clinical placements delivered by the NHS. Its implementation is now under consultation to be introduced in England and Wales. This may result in a further substantial increase in medical tuition fees of up to an additional £10 000 annually for international medical students.2–7 A single cohort of all disciplines of international students was found to contribute £3.2 billion to the UK economy over a 10-year period through taxation and National Insurance payments, further highlighting the significant economic contribution from this population.8
Following the BREXIT transition in January 2021, the definition of international students’ fee status applies to a wider population, including students from European Union (EU) countries; this policy may potentially impact the recruitment of international medical students in the future.4 9 10 Ultimately, this may create a selection bias towards students who have the financial means to pursue a UK medical degree, excluding those who may be capable of undertaking a UK medical degree but are unable to afford the tuition fees.2 3
These circumstances place the UK medical degree in a unique position in the global medical education landscape for aspiring international students. Despite being a costly investment, with the current UK medical degree ranking as the most expensive undergraduate degree in the UK,1 4 7 it remains highly popular among international students with courses annually oversubscribed.1 There is currently no data to demonstrate the motivation of international students to come to the UK to pursue medicine, taking into account not only the monetary value but also the value gained from the quality of life, societal and educational opportunities afforded by these institutions in the UK.
Identifying the motivation of this important subset (or potential subset) of the National Health Service(NHS) medical workforce could allow policy-makers to consider the current junior doctor retention crisis within the NHS in a nation with the second lowest doctor to population ratio in the EU.11 One study found that one in ten junior doctors are considering leaving the NHS12 while 16% of those who completed foundation training do not enter further training within 3 years.13 These factors have significant implications on workforce planning and ultimately patient safety.
This study aimed to evaluate the perception of the financial cost and value of the UK medical degree for international students and their motivations for pursuing such a degree. The study analysed how these perceptions and motivations differ between premedical students, medical students and medical school graduates and analysed their perception of the ‘value’ of obtaining a UK medical degree.
Methods
Study design
This online, multicentred, cross-sectional study focused on the perceptions of a UK medical degree among premedical students, current medical students and recent medical graduates. A qualitative and quantitative-based questionnaire was disseminated through collaborating university medical schools and established student networks across the UK and internationally, from 1 April 2021 to 31 July 2021. The questionnaire was circulated to 24 medical schools and 64 secondary schools (from 6 countries—UK, Malaysia, Singapore, Mozambique, Brazil, Vietnam). The survey was accessible as a secure online questionnaire on Microsoft Teams. The 40-item, self-administered questionnaire was developed by medical students from the Cardiff Healthcare International Perspective Society, which is a student-led society at Cardiff University. A review of the existing literature was performed to identify the gaps in knowledge and to look at similar questionnaires and qualitative studies on the perception of prospective, current and recently graduated international students of a UK medical degree. This allowed an understanding of domains and items relevant to determining the aim of the project. The questionnaire included a seven-point Likert scale, checkboxes, multiple-choice and free-text questions to improve the granularity of the data. A pilot survey was distributed to a group of randomly selected 13 undergraduate international students (6 different nationalities represented), who were not involved in study conception or design, to seek feedback, improve clarity and ensure objectivity. A copy of the final questionnaire can be found in online supplemental table 1.
bmjopen-2022-065062supp002.pdf (21.3KB, pdf)
Data processing
Throughout the period of data collection, the information received was kept in a password-protected Excel file. Prior to data analysis, all data were deidentified and stored securely. All relevant information remained non-identifiable throughout this study.
Study population
An international student eligible to be included in this study was defined using the definition from the UK Council for International Student Affairs as ‘non-British students (full-time or part-time in education); or students whose normal residency is not in the UK and are regarded as students with overseas/international fee status’.14
The sampled population was divided into three subgroups: premedical students, medical students and medical school graduates. A premedical school student was defined as a student not currently studying a medical degree and who was planning to submit their application to medicine within 2 years of survey completion. This included high-school students, students currently taking a gap year and students who were planning to apply for graduate-entry medicine.
A medical student is defined as any student currently studying medicine or a preclinical component, where a medical degree is the outcome. A medical school graduate was defined as any individual who had completed a UK medical degree within 2 years of survey completion. This was to reduce the effect of recall bias and it is likely that some may have been affected by the ACT levy. Participants were excluded if they did not provide consent to use of the data in publication and if they were a home student.
Outcome and statistical analysis
The study aimed to classify students’ perceptions and concerns regarding a UK medical degree and determine the difference between these perceptions among prospective, existing and postgraduates of UK medical schools. Outcomes measured were predefined and categorised into four domains: (1) factors influencing international students to study medicine in the UK, (2) perception of the UK tuition fees (how much they believed or knew the total tuition fees paid by international students) and training cost for a medical degree (how much they felt or believed it cost to train a medical student to become a doctor in the UK) and Act levy, (3) concerns about current support for international medical students in the UK and (4) working in the NHS on graduation.
A thematic analysis was performed by two independent reviewers (SM and RB) who systematically analysed the free-text responses and categorised them into different themes. Any discrepancies in the results were discussed among the two reviewers. If a consensus could not be reached, this was resolved by a third reviewer (SML).
Quantitative data were analysed independently by two authors (CHL and SG). A Likert scale was used to quantify and rank the order of importance of the factors. The seven points on the Likert scale ranging from ‘strongly agree, agree, somewhat agree, neutral, somewhat disagree, disagree, strongly disagree’ were linked to a numerical value of 1–7, respectively. The Kruskal-Wallis rank sum test was used for inferential analysis to compare non-parametric data among the three groups: medical student, premedical, postgraduate. Dunn test with Bonferroni adjustment was used as post hoc adjustment. A Spearman rank correlation coefficient test was used to determine the association between the value of a UK medical degree and participants’ perception of total tuition fees paid and the cost to train a medical student to a doctor. A p<0.05 was set to be statistically significant in this study. All statistical analyses were performed in R program V.3.6 (Boston, Massachusetts, USA).
Patient and public involvement
No patients were involved in this study.
Participation in the survey was voluntary and confidential. On submitting the forms, participants confirmed their consent to participate in the study and to the handling of data according to Article 6 (1)(a) of the General Data Protection Regulation. Individuals were allowed the right to withdraw consent and request removal of their data from the Google Form platform at any time. Access to the data was only granted to the steering committee of the study.
Results
The study is reported based on the Strengthening the Reporting of Observational Studies in Epidemiology statement: guidelines for reporting cross-sectional studies.
Baseline characteristics
A total of 468 responses were recorded. There were 116 responses which were excluded (85 home students; 31 did not consent). A total of 352 responses were submitted by international students with 251 medical school students (median age 21, IQR: 20–23 years old), 76 premedical school students (median age 18, IQR: 17–19 years old) and 25 medical school graduates (median age 25, IQR: 24–26 years old). Of the 352 responses, 221 were female (62.8%), 122 were male (34.7%), 6 preferred not to say (1.7%), 1 was a transgender male (0.3%) and 2 mentioned that their gender was not listed (0.6%). Among those who provided a response (non-compulsory field), 104 reported having studied in the UK prior to applying for the medical degree, with a median time of 2 years (IQR 2–4).
Out of 276 international students who reported their current or previous medical schools, 43 (15.6%) were from Scotland, 4 (1.5%) form NI, 36 (13%) were from Wales and 193 (69.9%) were from England.
A total of 56 nationalities were represented in this study, with respondents from Asian countries accounting for 68.2% of total participants, followed by the continents of Europe—10% and North America—9.4% (table 1). The detailed breakdown in nationalities can be found in online supplemental table 2.
Table 1.
The nationality of the respondents to the survey
| Nationality | No of respondents |
| Asia | 239 |
| North America | 33 |
| South America | 1 |
| Europe | 35 |
| Middle East | 11 |
| Oceania and Australia | 7 |
| UK (British passport) | 12 |
| Africa | 11 |
| Russia | 1 |
bmjopen-2022-065062supp001.pdf (176.1KB, pdf)
29.5% (104/352) of international students studied in the UK prior to applying to medical school; of which 27 were premedical students (35.5%, 27/76), 67 were current international medical students (26.7%, 67/251) and 10 were medical postgraduates (40%, 10/25). The median duration of studying in the UK for international students prior to applying for medicine was 2 years (IQR 2–4).
The overall value of the UK medical degree
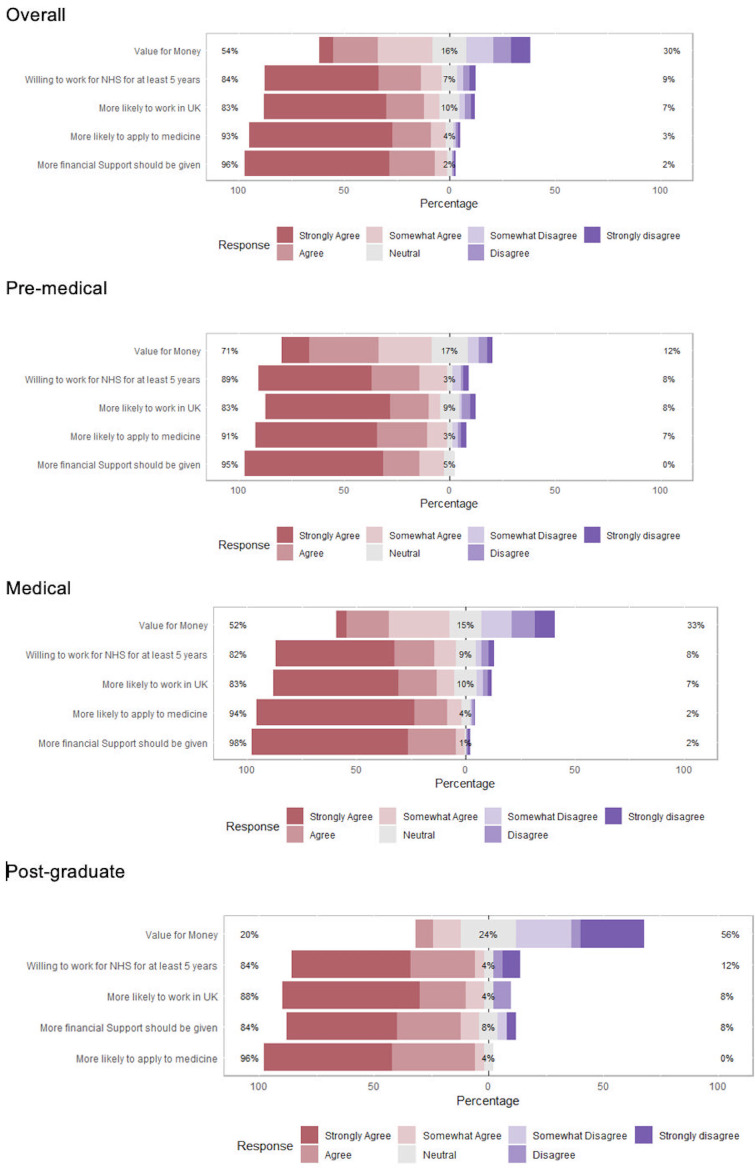
Overall, 96% of international students felt that more financial support should be given to them with 93% saying they would be more likely to apply for a UK medical degree if financial support was provided. Eighty-three per cent expressed that they would be more likely to work in the UK if more financial support was given, with 84% responding that they would consider entering into a contract to work for the NHS for at least 5 years, if there was more financial support for them to study medicine (figure 1).
Figure 1.
Shows five domains which premedical, medical and postgraduate students were asked to consider in relation to value of a UK medical degree. NHS stands for National Health Service. Percentages in the middle of the figure denote those who are neutral whilst the percentage on the left of the bar is a total of those who somewhat agree, agree and strongly agree and the percentage on the right of the bar is the total of those who somewhat disagree, disagree and strongly disagree.
In general, 54% of students felt the UK degree was value for money. There was a statistically significantly different opinion (p<0.05) among the subgroups; In the premedical school group, 71% felt that the UK degree is good value for money (17% were unsure, 12% disagreed with the statement), which was significantly (p<0.0001) higher than the 52% strongly agreeing and 20% of medical school students agreeing (15% were neutral, 23% disagreed) and postgraduate (24% remained neutral, 56% disagreed) groups, respectively. The postgraduate student’s perception of the value for money of the UK medical degree was also significantly different (p=0.0054) when compared with the other groups.
Factors influencing students to study medicine in the UK
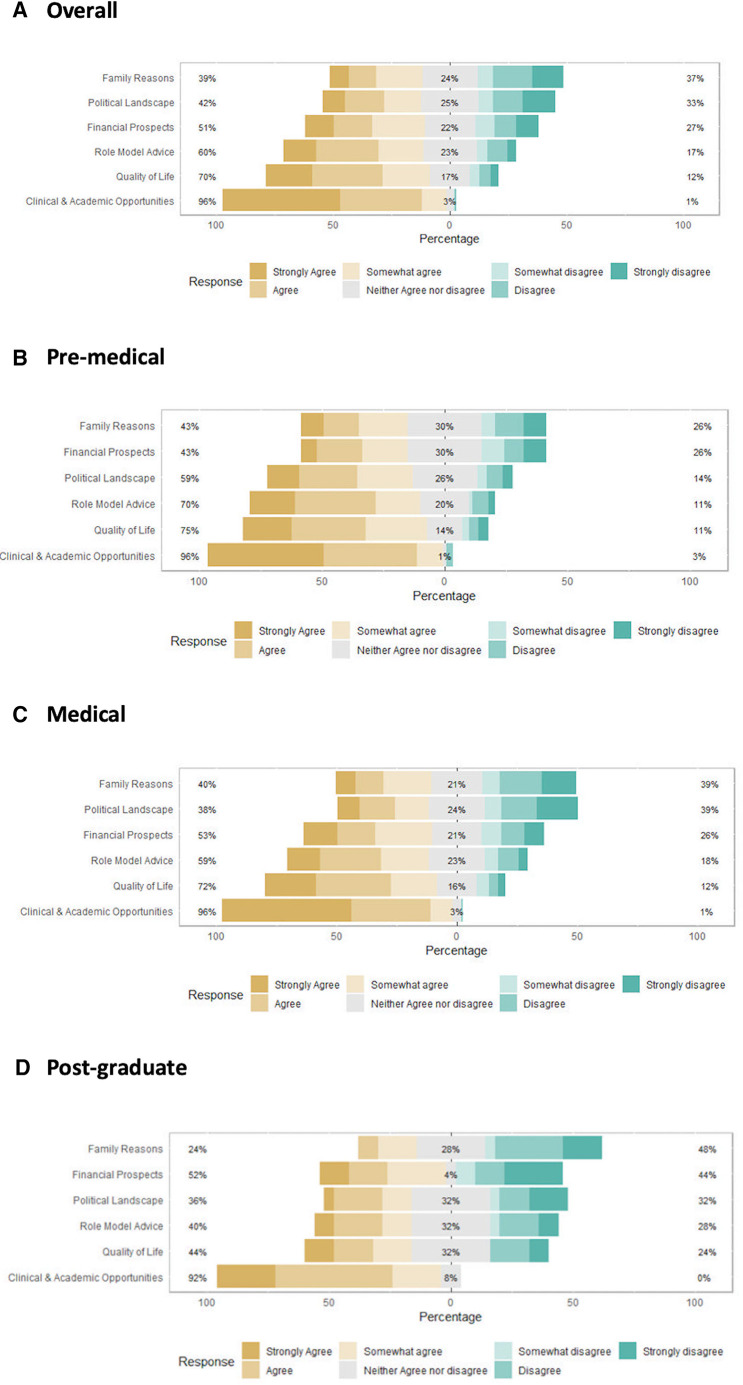
Out of six given reasons that influenced the decision to study medicine in the UK, clinical and academic opportunities were the most important factors (96%) among all the international students (figure 2A). This was consistently seen in all three subgroups (figure 2B–D).
Figure 2.
Shows the proportion of responses of factors influencing students to study medicine in the UK, (A) overall responses, (B) premedical responses, (C) medical responses (D) postgraduate responses. Percentages in the middle of the figure denote those who neither agree nor disagree whilst the percentage on the left of the bar is a total of those who somewhat agree, agree and strongly agree and the percentage on the right of the bar is the total of those who somewhat disagree, disagree and strongly disagree.
Among all respondents, this was followed by the quality of life (70%), role model advice (60%), financial prospects (51%), political landscape (42%) (figure 2A). The least important factor was for family reasons (39%) (figure 2A), which was seen consistently across all three groups: 43% in the premedical group, 40% in the medical group and 24% in the postgraduate group (figure 2B–D).
Fifty-nine per cent of students in the premedical student group ranked the political landscape in both the student’s home country and the UK as more important factors to be considered when compared with the medical student and postgraduate group. This was statistically higher (p=0.0002) compared with the medical student group (38%) and borderline significant (p=0.0503) compared with the postgraduate group (36%) (figure 2C–D).
Overall quality of life was the second most influential factor to motivate students to study medicine in the UK, this was demonstrated to be significantly lower in the postgraduate group, compared with the premedical (p=0.01) and medical group (p=0.02) (figure 2C–D).
Role model advice was also among the more important factors prompting premedical school students to study in the UK, with 70% of this cohort agreeing to this, compared with 59% in the medical student group (p=0.0697) and 40% in the postgraduate group (p=0.0114) (figure 2C–D).
42.3% (149/352) gave additional factors (assessed qualitatively below in online supplemental table 2) that influenced their decision to train in the UK. Some of the respondents stated the motivation to move abroad stems from the culture of practising medicine in the UK, while others came to experience living abroad. From the medical students’ and postgraduates’ perspectives, they cited that the UK medical degree is internationally recognised with clear training pathways, without the requirement of a previous degree. Many came for the high quality of education offered, with better career prospects following graduation. Eleven respondents cited that they did not get into the medical school in their home country (online supplemental table 3).
Perception about UK tuition fees and training costs for a medical degree
32.9% of international premedical students thought the average international student would have paid £200 000–£300 000 on completion of a medical degree in the UK, as shown in the table 2. This perceived amount is significantly higher compared with the medical student (p=0.00001) and postgraduate (p=0.0067) groups (table 2).
Table 2.
Perceived/known tuition fees paid by international students on completion of a medical degree by premedical student, medical student and medical school graduates
| On average, total tuition fees on completion of UK medical degree paid by international student | Premedical % (response) |
Medical students % (response) |
Medical school graduates % (response) |
| Less than £50 000 | 5.3 (4) | 0.8 (2) | – |
| £50 000–£100 000 | 5.3 (4) | 2.7 (7) | 12 (3) |
| £100 000–£200 000 | 13.2 (10) | 41.4 (104) | 44 (11) |
| £200 000–£300 000 | 32.9 (25) | 38.2 (96) | 20 (5) |
| £300 000–£400 000 | 6.6 (5) | 7.6 (19) | 12 (3) |
| £400 000–£500 000 | 15.8 (12) | 3.58 (9) | – |
| £500 000–£600 000 | 7.9 (6) | 2.4 (6) | – |
| More than £600 000 | 13.2 (10) | 3.2 (8) | 12 (3) |
Median perceived/known tuition fees are highlighted in bold.
As for the total cost of training, 19.7% of international premedical students thought it cost £300 000—£400 000 to train a medical student to be a doctor; 14.5% thought it cost more than £600 000 to train a doctor. 30.7% (77/251) international medical students thought it cost £50 000—£100 000. In the international medical school graduates’ group, 32% (8/25) thought it cost £50 000—£100 000. This perceived amount by the premedical student group is significantly higher compared with the medical student group (p<0.0001) and postgraduate group (p<0.0001) (table 3) (online supplemental table 4).
Table 3.
Perceived estimated total cost of medical training required to produce a doctor by premedical students, medical students and medical school graduates
| Total cost to train a medical student to become a doctor in the UK (average) | No of responses (premedical international students) |
No of responses (international medical students) |
No of responses (international medical school graduates) |
| Less than £50 000 | 2.6% (2) | 17.1% (43) | 20% (5) |
| £50 000–£100 000 | 7.9% (6) | 30.7% (77) | 32% (8) |
| £100 000–£200 000 | 15.8% (12) | 20.3% (51) | 32% (8) |
| £200 000–£300 000 | 18.4% (14) | 13.5% (34) | 12% (3) |
| £300 000–£400 000 | 19.7% (15) | 9.2% (23) | 4% (1) |
| £400 000–£500 000 | 10.5% (8) | 4.8% (12) | – |
| £500 000–£600 000 | 10.5% (8) | 1.6% (4) | – |
| More than £600 000 | 14.5% (11) | 2.8% (7) | – |
Median estimated cost is highlighted in bold.
Both the medical student and premedical students thought the tuition fees paid by international students on completion of a medical degree were statistically different to the total cost of medical training for a student to become a doctor (p=0.0007) and (p<0.0001), respectively. In the postgraduate group, there is no statistically significant difference (p=0.1965) in the perception of total tuition fees paid and the total cost of medical training.
There was a significant association between the students’ perception of the value of a UK medical degree and their perception of the cost to train a medical student to a doctor where those that tended to disagree that the UK medical degree was value for money suggested lower cost to train a medical student to a doctor (p=0.00013, online supplemental figure 1). There was no association between their perception of value of a UK medical degree and their perception of total tuition fees paid (p=0.1613, online supplemental figure 2).
ACT levy
Eighty-four per cent (296/352) of international students were not aware of ACT levy. Overall, 85% of international students stated that Act levy would probably influence their decision to study medicine in the UK (44% very likely, 24.1% likely, 16.2% somewhat likely). The premedical student group was significantly influenced by ACT levy compared with the (p<0.001) medical and (p=0.0026) postgraduate group. Seventy-four per cent of the premedical student group rated Act levy would affect their decision to study medicine in the UK (23.7% very likely, 23.7% likely, 25% somewhat likely) with neutral and unlikely being 13% and 14% of the cohort, respectively.
International students’ concerns
Free-text responses were provided by 26.1% (92/352) of respondents, and qualitative analysis demonstrated the students’ general concerns. The majority of the premedical student group had no concerns (49.9%), 16.5% felt that the cost of the degree was the major concern, followed by 11.0% who feared unconscious bias and racism (online supplemental table 5). Other concerns include challenging application process for medical school admissions, learning style and potential terrorism.
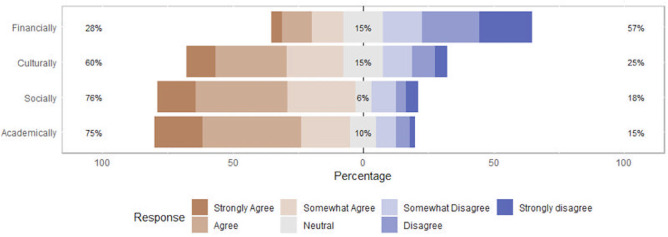
Postgraduate and existing medical students (276/352) were asked if they had adapted well to the UK and been well supported by their medical school, university students’ societies and other methods of support, according to four specific domains (figure 3). Most students felt they had adapted well academically (75%) and socially (76%). 60% felt they had adapted well culturally while 25% disagreed. Only 28% of the international medical students felt well supported financially, 15% were neutral and 57% disagreed.
Figure 3.
Shows four domains in which postgraduate and existing medical students (276/352) were asked if they had adapted well to the UK and were well supported through the medical school, university students’ societies and other methods of support. Percentages in the middle of the figure denote those who are neutral while the percentage on the left of the bar is a total of those who somewhat agree, agree and strongly agree and the percentage on the right of the bar is the total of those who somewhat disagree, disagree and strongly disagree.
Working in NHS on graduation
28.4% (100/352) of the respondents were unsure about working in the NHS on graduation with 58% (204/352) saying they would like to work in NHS and 8% (28/352) saying they did not want to work in the NHS, respectively. Of the total respondents, 5.6% (20/352) are currently working in the UK, thereby accounting for 80% (20/25) of the postgraduate cohort.
All respondents were asked whether they would consider working in the NHS; 27.8% (98/352) were unsure, 29.3% (103/352) would like to work for 2 years until the completion of Foundation Year 2, 28.7% (101/352) would like to work for up to 10 years or until the completion of specialty training. A further 9.4% (33/352) would like to work as a consultant indefinitely, meanwhile 4.8% (17/352) would like to leave immediately on medical school graduation. Their wishes regarding work in the NHS did not significantly differ among the subgroups (p=0.3).
Discussion
This study evaluates the perceptions of previous, current and prospective international students regarding UK medical education.
The results showed that clinical and academic opportunities were the most significant factors that attracted respondents to pursue medicine in the UK. However, among the three groups, there are significant differences in perspectives regarding the financial value of a medical degree in the UK, establishing that premedical students are the most optimistic, closely followed by the existing medical students and then postgraduates. The study’s results highlight two important aspects for consideration regarding the future of medical education in the international arena: the cost of a medical degree and quality of medical training.
Cost of UK medical degree
Potential reasons for premedical students perceiving the cost of a UK medical degree higher than actual paid cost of the degree compared with the perception of medical students and medical graduates may be explained by the influence of the ‘perceived prestige and glamour’ by friends, family and social media.15 As evidenced by our findings, medical students and graduates think that the tuition fees paid for a UK medical degree are higher than the actual cost to train a medical student to become a doctor. This gradual skewing of perception from premedical to postgraduate could be due to the progressive disagreement that a UK medical degree is good value for money (online supplemental figures 3 and 4).
In 2017, the Department of Health quoted an average funding cost of £230 000 per medical student, of which 67% (£151 000) is a grant to the placement provider and medical school, while 33% (£64 300) constitutes repayable loans and bursary to students for living costs and tuition.5 9 This cost of £230 000 per student is closer to the estimates suggested by the premedical student group than that of the medical student and graduate groups. Despite this, there is no clear breakdown of how these costs are utilised. For example, the costs of insurance and indemnity, placement-based teaching sessions, and other clinical resources. Given the plans to further increase international medical tuition fees via the ACT levy, it is important that this breakdown should be transparent.
It should be noted that the future salary offered to graduates may not offset the total cost of the degree for international students.2 16 Given the current trend and the assumption that international medical graduates (IMGs) use 10% of their basic salary to repay student debts, it could take up to 28 years to complete repayment of the total debt accumulated during their degree.2 16 The implementation of ACT levy will further contribute to the financial burden on international medical students; it is therefore important that applicants are well aware of these long-term financial implications before applying to medical schools.
More work could be done to increase the transparency of the cost of medical training, especially for international medical students. This applies to the current cost of training and the added cost from the ACT levy.17 Universities are keen to enrol international students for financial reasons; maintaining an element of transparency is key to ensuring that the consumer rights of these students are preserved.18 For the international student, having the knowledge of the breakdown of these additional costs is a key factor in the decision-making process when applying to study medicine in the UK.
Quality of undergraduate training
The quality of medical education and international prestige are attractive factors for international students.19 Medical education in the UK is renowned for advanced technological facilities, research and intercalation opportunities.19–21 Furthermore, the General Medical Council (GMC) oversees undergraduate and postgraduate training experience and provides quality assurance, when stipulated professional outcomes need to be achieved.19 20 This instils confidence in international students as it reduces the variation in the abilities of graduates from different UK medical schools.
However, there has recently been a rapid increase in the number of GMC-approved medical schools in the UK and overseas,5 6 9 10 with up to 13 new medical schools currently being developed. Furthermore, as intercalated degrees no longer count for points in the UK foundation programme application,22 this policy might lower students’ motivation to intercalate and reduce the focus on research in the undergraduate curriculum.22 Current and new medical schools will need to ensure their curriculum provide research opportunities as part of their high quality teaching. International students’ expectations of the UK medical degree have to be maintained despite these changes in policies.5 6 9 10
The COVID-19 pandemic increased the virtual delivery of the medical curriculum.23 24 Distance learning inevitably reduces the use of university facilities, student-to-student interaction and social experience. In our study, 15% of students felt that they did not receive adequate support academically during the pandemic, while 18%–25% of international students reported that they did not feel supported socially or culturally during medical school. The study was unable to determine the actual contribution of the pandemic on this perception as only 2.2% described the COVID-19 impact on the curriculum (supplementary table 3 online supplemental file 1) as an additional factor causing concern for international students studying medicine in the UK. However, lack of cultural diversity and knowledge, potential discrimination and homesickness are long-standing issues for international students adapting to life away from home.25
Strengths and limitations
This is the first study to systematically evaluate the perceptions of premedical, medical and postgraduate international doctors on the value of a UK medical degree and factors influencing their decision to study in the UK. It is important to understand these concerns following the adverse impact of the pandemic on globalisation and dissatisfaction among UK junior doctors towards their working conditions and their pay postgraduation.
A key study limitation is the selection bias introduced through questionnaire distribution by contacts and networks known to the study team. However, 24 medical schools and 64 secondary schools (nationally and internationally—6 countries in total) were approached. Individuals did not enter their secondary school name/location due to small numbers of respondents so it was not possible to determine a response rate for each secondary school approached. Although not a limitation per se, the majority of respondents were female (62.8%) and from Asian nationalities (67.8%); motivations and perceptions of a UK medical degree within these demographics need to be considered when interpreting the results. With regards to postgraduate students, there is also likely recall bias towards their perceptions of the value of the degree and the influences for decisions to study in the UK and this was our smallest sample size (n=25).
The study period encompassed the COVID-19 pandemic (April–July 2021) and some students may have experienced additional stress and isolation which might have affected their motivation to pursue a medical degree during this time.
Future work
With the removal of the residential labour market stress test, IMGs from overseas can compete freely with graduates from the UK and in 2020, the GMC reported that more IMGs registered with the GMC than UK graduates.26 It is likely that IMGs pay less fees in their home countries than international students in the UK. Due to this change in policy, there is no longer an advantage for the UK medical graduate, as competition is equal among all medical graduates.23 Obtaining a medical degree prior to migrating to the UK to obtain postgraduate training could be perceived as a more economical way to progress in the medical career.
The high tuition fees will be a major obstacle for students who are unable to secure funding from their home country, with only 28% of students feeling financially supported. In this study, 84% of international students stated that they are willing to enter a contract to work for the NHS for at least 5 years if financial support is provided. This would be a favourable strategy so they can contribute to national taxation and help retain the doctors who have benefited from UK training. The development of medical apprenticeships and widening access schemes to medicine are also being discussed as methods of increasing the number of doctors and healthcare professionals to address the workforce shortage. This raises the question as to whether there is a need for widening access schemes for international medical students,5 6 especially if the government would like to attract the best candidates from the international community to work in the UK.
Currently, there is a problem with retention of junior doctors in UK due to dissatisfaction about pay and work–life balance.27 28 There has also recently been overwhelming support of junior doctors to carry out industrial action (98% voted for industrial action with a 77% turnout) for better pay.29 Policy-makers need to consider how to address some of these problems to retain this important workforce within the NHS. Our current study focused primarily on the financial cost of a UK medical degree. It is important to bear in mind other geographic are an option for international applicants, including the USA and other parts of Europe. It would, therefore, be of interest to compare and contrast the different regions, although this was beyond the scope of this study.
Conclusion
The quality of medical education and international prestige are still the most important factors that influence international students to study medicine in the UK. However, further work is needed to ascertain reasons for the differing perceptions of the value by international students at different stages in their clinical training.
The UK currently faces a shortage of doctors, and it is, therefore, important to retain junior doctors who have benefited from undergraduate training in the UK. Policy-makers could consider financially supporting international students who graduate and would like to continue to work for the NHS.
Supplementary Material
Acknowledgments
The authors would like to thank Cardiff University Healthcare International Perspectives Society (CHIPS), OSCEazy, In2MedSchool, The Hong Kong Medical University of United Kingdom (HKMUSK) for their collaboration on this study.
Footnotes
Twitter: @amandagodoimed, @ravanth97
CHL and SG contributed equally.
Collaborators: VISION Collaborators Sai Pill, Paarth Kishan Gupta, Renee Punia, Katie Cheung, Diva Jhaveri, Aaron Gnanabalan, Italia-Rosa Leech, Faith Lee, Elizabeth Wong, Kar Phoong, Memory Moyo, Isha Thakar, Viraj Shah, Rohan Gupta, Tushar Rakhecha, Movin Peramuna Gamage, Nishaanth Dalavye, Allen Mathew, Parvathy Sureshkumarnair, Sripradha Srinivasan, Becky Leveridge.
Contributors: CHL and SG contributed equally to the study, act as guarantors to the publication and should be considered joint first authors (conception, methodology, data curation, formal analysis, writing and reviewing). TP (methodology, project administration, writing, reviewing and editing), AG (methodology, project administration, data collection, writing, reviewing and editing, SML (methodology, project administration, data collection, data analysis, writing), RB and SM (creating data collection form, data collection, data analysis, writing), EFF (methodology, writing, organising webinar, project administration), SZYO (methodology, project administration, reviewing and editing), TW (conception, design, reviewing and editing), VY (writing, reviewing and editing). HS (conception, design, methodology, writing, reviewing and editing and supervising). All authors contributed to this article and approved the submitted version. VISION Collaborators have contributed to data collection and distribution of the study survey. SG is responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: VISION collaborators, Sai Ram Pillarisetti, Paarth Kishan Gupta, Renee Punia, Katie Cheung, Diva Jhaveri, Aaron Gnanabalan, Italia-Rosa Leech, Faith Lee, Elizabeth Wong, Kar Yen Phoong, Memory Moyo, Isha Thakar, Viraj Shah, Rohan Gupta, Tushar Rakhecha, Movin Peramuna Gamage, Nishaanth Dalavye, Allen Mathew, Parvathy Sureshkumarnair, Sripradha Srinivasan, and Becky Leveridge
Data availability statement
Data are available on reasonable request. Please contact the corresponding author to request any data. The request would be discussed among the VISION committees and deidentified participants’ data may be shared according to Cardiff University’s Data Protection Policy. The research protocol is available to the public online.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved by Cardiff Ethics committee (SMREC reference number 21/22). Participants gave informed consent to participate in the study before taking part.
References
- 1.UCAS . UCAS undergraduate data release Archive; 2022. Available: https://www.ucas.com/corporate/data-and-analysis/ucas-undergraduate-releases/ucas-undergraduate-analysis-reports/ucas-undergraduate-end-cycle-reports [Accessed 15 Feb 2022].
- 2.Royal College of Physician London . The bubble set to burst: is the UK’s medical recruitment unsustainable after BREXIT? In: RCP annual conference 5. 2021: 23. Available: https://70b706f2.flowpaper.com/NovemberCommentary/#page=23 [accessed 3 Oct 2021]. [Google Scholar]
- 3.Enoch TR, Ooi R, Ooi SZY. Impact of the implementation of the additional cost of teaching (ACT) levy on prospective International medical students applying to Northern Ireland and Scotland. Postgrad Med J 2022;98:e144–5. 10.1136/postgradmedj-2021-140194 [DOI] [PubMed] [Google Scholar]
- 4.Aberdeen U. Tuition fees the school of medicine, medical sciences and nutrition the University of Aberdeen; 2021. Available: https://www.abdn.ac.uk/smmsn/undergraduate/medicine/tuition-fees.php [Accessed Oct 2021].
- 5.GOV.UK Department of Health and Social Care . Expanding undergraduate medical education; 2021. Available: https://www.gov.uk/government/consultations/expanding-undergraduate-medical-education [Accessed 3 Oct 2021].
- 6.Expanding undergraduate medical education in the UK - but at whose cost?; 2021. Available: https://www.bmj.com/content/356/bmj.j1370/rr-0 [Accessed 3 Oct 2021]. [DOI] [PubMed]
- 7.Queen’s University Belfast . International tuition fees; 2022. Available: https://www.qub.ac.uk/International/International-students/International-tuition-fees/ [Accessed Feb 2022].
- 8.HEPI . The UK’s tax revenues from international students post-graduation; 2022. Available: https://www.hepi.ac.uk/2019/03/21/the-uks-tax-revenues-from-international-students-post-graduation/ [Accessed 15 Feb 2022].
- 9.Royal College of Physicians . Double or quits: a blueprint for expanding medical school places; 2021.
- 10.Office for Students . Health education funding, medical and dental target intakes; 2021. Available: https://www.officeforstudents.org.uk/advice-and-guidance/funding-for-providers/health-education-funding/medical-and-dental-target-intakes/ [Accessed 3 Oct 2021].
- 11.Team PSL. Medical staffing in England: A defining moment for doctors and patients (BMA, 11 July 2021), patient safety learning - the Hub; 2021. Available: https://www.pslhub.org/learn/improving-patient-safety/workforce-and-resources/safe-staffing-levels/medical-staffing-in-england-a-defining-moment-for-doctors-and-patients-bma-11-july-2021-r4856/ [Accessed 8 Apr 2023].
- 12.Working together to improve NHS staff experiences: NHS staff survey (no date) working together to improve NHS staff experiences | NHS staff survey; Available: https://www.nhsstaffsurveys.com/ [Accessed 8 Apr 2023].
- 13.Training pathways: Why do doctors take breaks - general medical Council; Available: https://www.gmc-uk.org/-/media/documents/dc11392-training-pathways-report_pdf-75268632.pdf [Accessed 0 Apr 2023].
- 14.UK Council for International Student Affairs . International student advice and guidance — England: fee status; 2021. Available: https://www.ukcisa.org.uk/information--advice/fees-and-money/england-fee-status [Accessed 3 Oct 2021].
- 15.McHarg J, Mattick K, Knight LV. Why people apply to medical school: implications for widening participation activities. Med Educ 2007;41:815–21. 10.1111/j.1365-2923.2007.02798.x [DOI] [PubMed] [Google Scholar]
- 16.Ooi SZY, Ooi R, Godoi A, et al. Motivations of medical students and doctors leaving the NHS explored in a Residency training application Webinar series. Postgrad Med J 2022;98:942–7. 10.1136/postgradmedj-2021-140795 [DOI] [PubMed] [Google Scholar]
- 17.GOV.UK Competition, Markets Authority . Higher education: guide to consumer rights for students; 2015. Available: https://www.gov.uk/government/publications/higher-education-guide-to-consumer-rights-for-students [Accessed 29 Mar 2022].
- 18.Levent F. The economic impacts of international student mobility in the globalization process. J Human Sci 2016;13:3853. 10.14687/jhs.v13i3.3877 [DOI] [Google Scholar]
- 19.General Medical Council . Standards of UK medical education; 2021. Available: https://www.gmc-uk.org/education/becoming-a-doctor-in-the-uk/standards-of-uk-medical-education [Accessed 3 Oct 2021].
- 20.Quraishi S, Wade W, Black D. Development of a GMC aligned curriculum for internal medicine including a qualitative study of the acceptability of ‘capabilities in practice’ as a curriculum model. Future Healthc J 2019;6:196–203. 10.7861/fhj.2018-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bustin S. Science in the UK - whereto now? Biomol Detect Quantif 2016;9:A1–4. 10.1016/j.bdq.2016.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tonkin T. Additional achievements ruled out of foundation programme applications. BMA; 2021. Available: https://www.bma.org.uk/news-and-opinion/additional-achievements-ruled-out-of-foundation-programme-applications [Accessed 04 Oct 2021].
- 23.Harries AJ, Lee C, Jones L, et al. Effects of the COVID-19 pandemic on medical students: a multicentre quantitative study. BMC Med Educ 2021;21:14. 10.1186/s12909-020-02462-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papapanou M, Routsi E, Tsamakis K, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J 2022;98:321–7. 10.1136/postgradmedj-2021-140032 [DOI] [PubMed] [Google Scholar]
- 25.Kristiana IF, Karyanta NA, Simanjuntak E, et al. Social support and Acculturative stress of international students. IJERPH 2022;19. 10.3390/ijerph19116568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The changing medical workforce - GMC-UK.org (no date); Available: https://www.gmc-uk.org/-/media/documents/somep-2020-chapter-3_pdf-84686032.pdf?la=en&hash=D2F3AD68AF8820D40A285BDC6A391A85A780C88B [Accessed 8 Apr 2023].
- 27.Lock FK, Carrieri D. Factors affecting the UK Junior doctor workforce retention crisis: an integrative review. BMJ Open 2022;12:e059397. 10.1136/bmjopen-2021-059397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.A;, W.H.C.P.A.S.S.B. (no date) Drexit: understanding why Junior doctors leave their training programs to train overseas: an observational study of UK physicians, health science reports. U.S. National Library of Medicine; Available: https://pubmed.ncbi.nlm.nih.gov/34646946/ [Accessed 8 Apr 2023]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patterson C. Junior doctors vote Yes to industrial action, the British Medical Association is the trade Union and professional body for doctors in the UK; 2023. British Medical Association Available: https://www.bma.org.uk/news-and-opinion/junior-doctors-vote-yes-to-industrial-action [Accessed 8 Apr 2023].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065062supp002.pdf (21.3KB, pdf)
bmjopen-2022-065062supp001.pdf (176.1KB, pdf)
Data Availability Statement
Data are available on reasonable request. Please contact the corresponding author to request any data. The request would be discussed among the VISION committees and deidentified participants’ data may be shared according to Cardiff University’s Data Protection Policy. The research protocol is available to the public online.