Abstract
Purpose
We investigated the effects of a warm compress immediately before surgery on the ocular surface and intraoperative visibility during surgery.
Methods
A randomised controlled quasi-experiment at Saitama Medical University Hospital. From November 2020 to September 2021, 200 patients scheduled for endophthalmic surgery were randomly assigned to a group that received a hot compress with a spontaneously heating eye mask (HM group) or a group that received only an eye mask (control group). The eye masks were applied for 20 min from 2 hours before surgery, and before and after mask application in the non-invasive tear break-up time (NIBUT), tear meniscus height (TMH) and obstruction score of the meibomian gland (meiboscore) were evaluated. The time from wetting to dry blurring of the corneal surface (corneal blurring time, CBT) was also compared before and after the warm compress.
Results
We enrolled 100 patients in the HM group (mean age 69.0±13.3 years) and 99 patients in the control group (mean age 69.5±16.2 years). In the control group, there were no significant changes in the NIBUT, meiboscore or TMH before and after eye mask use, whereas in the HM group, the NIBUT increased from 6.7±5.1 to 9.5±5.6 s (p<0.001), the meiboscore improved from 0.71±0.93 to 0.63±0.96 (p=0.03) and the TMH significantly improved from 0.22±0.08 to 0.24±0.08 mm (p<0.001). The CBT was longer the HM group than control group (33.5±13.4 s, 25.7±14.9 s, respectively, p=0.01).
Conclusions
The condition of the ocular surface and intraoperative visibility improved after a single warm compress.
Trial registration number
UMIN R000047286.
Keywords: Clinical Trial, Infection, Ocular surface, Tears, Lacrimal gland
WHAT IS ALREADY KNOWN ON THIS TOPIC
Intraoperative optical clarity is an important factor in all endophthalmic surgical procedures and is mainly inhibited by blurring due to corneal dryness. It was reported that the intraoperative visibility is improved by the application of diquafosol, the ophthalmic solution of choice for the treatment of aqueous-deficient dry eye type. However, there are no reports of the treatment of warm compress, for the treatment of the evaporative dry eye type.
WHAT THIS STUDY ADDS
This study found that a single warm compress for 20 min prior to surgery improves the condition of the ocular surface and improves visibility during endophthalmic surgery. A 20 min warm compress does not increase the detection rate of bacterial cultures in the conjunctival sac.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The results of this study indicate the potential to reduce the stress of corneal dryness during endophthalmic surgery. Prolonged the time from wetting to dry blurring of the corneal surface may also reduce the burden on the surgeon as well as surgical assistants.
Introduction
Intraoperative optical clarity is an important factor in all endophthalmic surgical procedures and is mainly inhibited by blurring due to corneal dryness. The factors reported to cause eye dryness in the perioperative period include forced opening of the eyelids,1 ageing,2 3 light and heat from surgical microscopes,4 5 preservatives in eye-drops,6 7 topical anaesthetics,8 9 and washing of conjunctival sacs and eyelids with povidone-iodine.10 The mechanism by which these risk factors induce dry eye (DE), its incidence and its prevention and treatment have not been established. Particularly in cataract surgery, DE not only results in complications of DE itself, such as increased risks of symptoms and infection, but also decreases the accuracy of preoperative evaluation.11 12
DE is a multifactorial disease of the ocular surface characterised by a loss of tear film homeostasis, accompanied by ocular symptoms.11 It is classified into evaporative and aqueous-deficient subtypes.13 An intact lipid layer may be necessary to prevent tear film evaporation,14 and meibomian gland dysfunction (MGD) is the most common cause of evaporative DE.15 It is important to assess and preoperatively manage any MGD prior to ophthalmic surgery.11 Treatment regimens for MGD include the regular use of warm compresses, eyelid hygiene, treatment of Demodex, administration of systemic tetracycline antibiotics and topical azithromycin.
In endophthalmic surgery on patients with senile cataract, the intraoperative visibility is reportedly improved by the application of diquafosol,16 the ophthalmic solution of choice for the treatment of aqueous-deficient DE type, but, to the best of our knowledge, there are no reports of the treatment of the evaporative DE type. Therefore, we conducted a prospective randomised controlled trial of the preoperative and intraoperative benefits of applying a single warm compress to the eye area prior to endophthalmic surgery.
Materials and methods
Participants
Patient data were used only for this study and patient confidentiality was preserved. The datasets generated and/or analysed during the current study are provided in this article. Patients and the public were not involved in this study.
We prospectively enrolled 200 patients (88 men, 112 women) who underwent endophthalmic surgery at the Saitama Medical University Hospital between January 2020 and September 2021. Patients with any of the following criteria were excluded: redness or swelling of the eyelid skin, atopic dermatitis, DE diagnosis and prescription of eye-drops and lack of informed consent.
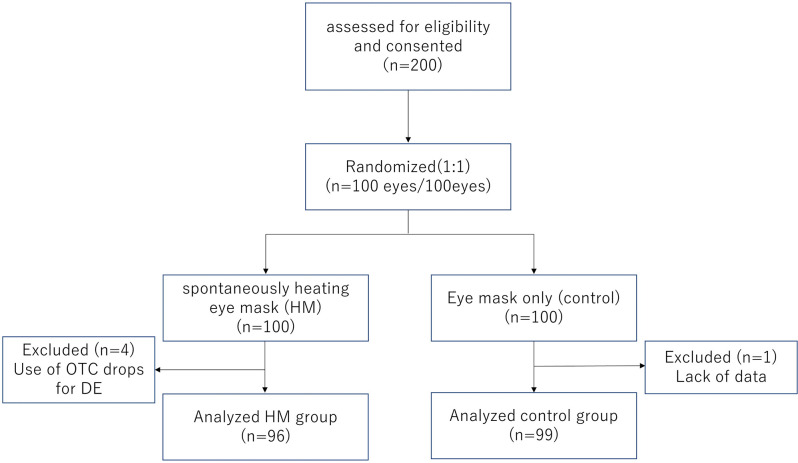
The detailed procedure was as follows. After confirming the provision of consent and eligibility, patients were randomly assigned to either a spontaneously heating eye mask (HM) group or an eye mask-only (control) group. Two hours before endophthalmic surgery, the Keratograph 5M (Oculus, Wetzlar, Germany) was used to determine the non-invasive tear break-up time (NIBUT), tear meniscus height (TMH), obstruction score of the meibomian gland (meiboscore) and conjunctival hyperaemia score (hyperaemia score) of all patients. The patients then wore the appropriate eye masks for either group for 20 min, and the NIBUT, TMH, meiboscore and hyperaemia score were remeasured. Conjunctival sac cultures were performed before and after the eye mask application, whereby seed swab no. 3 (Cygni Medical, Tokyo, Japan) was wiped on the conjunctival sac to collect specimens. At the time of surgery, we determined the corneal blurring time (CBT) as the time from when the corneal surface was wetted to the time it dried and blurred (figure 1).
Figure 1.
Study flow diagram. DE, dry eye; OTC, over the counter.
Randomisation and blinding
The RAND command in Excel was applied to assign each patient a number ranging from 0 to 1; patients numbered from 0 to <0.5 were assigned to the HM group, while those numbered 0.5–1 were assigned to the control group. The group assignments were placed in envelopes and given to patients in the order shown in the corresponding table (by SI). All examinations were performed by other examiners (SY and MH) who were blinded to the group allocations.
Eye masks
The HM was a disposable eyelid warming device (Hot Eye Mask; Kao, Tokyo, Japan). The outer part of the eye mask is made of polypropylene and polyethylene, and the part that contacts the eye has a sheet inside that contains a heating element containing iron powder and moisture. This warming device is individually sealed to prevent exposure to oxygen. When the mask is opened and contacts the air, the iron powder in the heating element oxidises and generates heat, turning the moisture contained in the heating element into steam. The HM maintains the ocular surface at approximately 40°C for 20 min. In the eye masks used in the control group, a small hole was made in the presealed bag to completely terminate the oxidation reaction so that it did not generate heat; thus, there was no visible difference between the eye masks used in the HM and control groups.
Measurements of the NIBUT, TMH, meiboscore and conjunctival hyperaemia score
All patients underwent imaging with the Keratograph 5M, an advanced corneal topographer with a built-in keratometer and a colour camera optimised for external imaging equipped with a modified tear film scanning function. The Oculus K5M software was used to automatically obtain the TMH, first non-invasive keratograph tear breakup time (NIBUT first), average non-invasive keratograph tear breakup time (NIBUT average) and ocular redness. The NIBUT, TMH and ocular redness were measured three times and the mean values were used in the analysis. A blinded examiner (MH) used the Keratograph 5M to assess the meibomian gland and determine the meiboscore as grade 0 (no loss of the meibomian gland), grade 1 (loss of <33% of the entire gland area), grade 2 (loss of 33%–66% of the entire gland area) and grade 3 (loss of >66% of the entire gland area).17 R-scan software was used to automatically calculate the ocular redness scores, including the nasal limbal, temporal limbal, nasal bulbar and temporal bulbar redness, with the average of these scores as the conjunctival hyperaemia score.
Determination of the CBT
A blinded examiner (SY) determined the CBT using a previously reported method.16 The temperature in the operating room was maintained at 23°C and the humidity at 50%–60%. The CBT was determined at a relatively early stage of surgery without an ophthalmic viscosurgical device placed on the cornea or conjunctival sac. The microscope light power was 20%, and three light-source images of the cornea were confirmed to have 12×magnification. The evaluation was initiated after a balanced salt solution was instilled on the corneal surface; the endpoint was the time at which the three light-source images began to blur.
Perioperative drug use
All patients used topical moxifloxacin eye-drops four times a day for 3 days before surgery. They also applied eye-drops containing moxifloxacin, mydriatic and nonsteroidal anti-inflammatory drugs every 30 min for 2 hours before surgery. Before endophthalmic surgery, the skin was disinfected using a 10% povidone-iodine solution. The conjunctival sac was disinfected by soaking an eightfold dilution of 2% polyvinyl alcohol iodine solution into the conjunctival sac immediately before surgery. The eyelid was not flipped, scrubbed or pressed to extrude the meibomian gland.
Statistical analyses
All statistical analyses were performed using JMP V.16 software (SAS Institute). All data are expressed as means±SD. The meiboscore, conjunctival hyperaemia score and CBT were compared between the HM and control groups using the Mann-Whitney U test. Welch’s t-test was used to compare the NIBUT and TMH values before versus after eye mask application. Wilcoxon signed rank test was applied to compare the meiboscore and conjunctival hyperaemia score before versus after eye mask application. The ages of the two groups were compared using the unpaired t-test, while the sex distribution between groups and the bacterial detection rate before vs after eye mask application were compared using the χ2 test. Statistical significance was set at p<0.05. P values smaller than 0.001 are presented as p<0.001.
Results
A total of 200 patients (200 eyes) were enrolled and 100 patients (43 women, 57 men) were randomly assigned to the HM group and 100 patients (55 women, 45 men) to the control group. The types of surgery included cataract surgery in 176 eyes, trabeculectomy in 5 eyes and pars plana vitrectomy in 19 eyes, with 16 eyes involving the epiretinal membrane and 3 eyes involving the macular hole. One patient in the control group was excluded because of a lack of data. Four patients in the MH group were excluded after surgery because they were found to be using over-the-counter (OTC) drops for DE. Therefore, the final study cohort comprised 96 patients (39 women, 57 men) in the HM group and 99 patients (55 women, 44 men) in the control group. The HM and control groups did not significantly differ regarding the mean age (69.0±13.3 years vs 69.5±16.2 years; p=0.09), sex distribution (p=0.83), NIBUT first (6.72±5.05 s vs 6.49±4.89 s), NIBUT average (9.57±5.52 s vs 9.50±5.18 s), TMH (0.22±0.08 mm vs 0.22±0.07 mm), meiboscore (0.71±0.93 vs 0.59±0.94) or conjunctival hyperaemia score (1.23±0.59 vs 1.39±0.73) (table 1).
Table 1.
Profile of pretreatment
| HM group (n=96) | Control group (n=99) | P value | |
| Age (years) | 69.0±13.3 | 69.5±16.2 | 0.09* |
| Sex (female/male) | 39/57 | 44/55 | 0.58† |
| NIBUT first (sec) | 6.72±5.05 | 6.49±4.89 | 0.75* |
| NIBUT average (sec) | 9.57±5.52 | 9.50±5.18 | 0.93* |
| Meiboscore | 0.71±0.93 | 0.59±0.94 | 0.37‡ |
| Tear meniscus height (mm) | 0.22±0.08 | 0.22±0.07 | 0.19* |
| Conjunctive hyperemia score | 1.23±0.59 | 1.39±0.73 | 0.09‡ |
*unpaired-t test
†chi-square test
‡Mann-Whitney U test
HM, heating eye mask; Meiboscore, obstruction score of the meibomian gland; NIBUT, non-invasive tear break-up time.
Table 2 shows the variables before and after eye mask treatment in the HM and control groups. The HM group showed significant improvements in the NIBUT first, NIBUT average and TMH after the treatment (9.46±5.75 s, 12.1±5.31 s and 0.24±0.08 mm, respectively) compared with the pretreatment values (6.72±5.05 s, 9.57±5.52 s and 0.22±0.08 mm, respectively). The meiboscore in the HM group improved from 0.71±0.93 before treatment to 0.63±0.96 after treatment; however, the conjunctival hyperaemia score worsened from 1.23±0.59 before treatment to 1.41±0.60 after treatment. The HM group had a longer CBT (33.5±13.4 s) than the control group (25.7±14.9 s)(p<0.001). In contrast with the HM group, the control group showed no significant improvements in the NIBUT first, NIBUT average, TMH or meiboscore after the treatment (6.17±4.69 s, 9.10±8.73 s, 0.22±0.07 mm and 0.59±0.94, respectively) compared with the pretreatment values (6.49±4.89 s, 9.49±5.18 s, 0.23±0.08 mm and 0.58±0.94, respectively). Furthermore, the conjunctival hyperaemia score in the control group was significantly improved after the eye mask treatment (1.36±0.70) compared with the pretreatment value (1.39±0.73). There were 10 patients in the HM group and 11 in the control group who were receiving eye-drops for glaucoma. Because glaucoma eye-drops cause conjunctival hyperaemia, these patients were excluded and the analyses were performed in a cohort comprising 86 patients in the HM group and 88 in the control group. The results did not differ from those of the analyses including patients with glaucoma (online supplemental table).
Table 2.
Results of post treatment
| HM group (n=96) | Control group (n=99) | |||||
| Pre | Post | Pre vs post | Pre | Post | Pre vs post | |
| NIBUT (first) | 6.72±5.05 | 9.46±5.75 | <0.001* | 6.49±4.89 | 6.17±4.69 | 0.41* |
| NIBUT (average) | 9.57±5.52 | 12.1±5.31 | <0.001* | 9.49±5.18 | 9.10±8.73 | 0.63* |
| Meiboscore | 0.71±0.93 | 0.63±0.96 | 0.03† | 0.58±0.94 | 0.59±0.94 | 0.15† |
| Tear meniscus height | 0.22±0.08 | 0.24±0.08 | <0.001* | 0.23±0.08 | 0.22±0.07 | 0.16* |
| Hyperemia score | 1.23±0.59 | 1.41±0.60 | <0.001† | 1.39±0.73 | 1.36±0.70 | 0.002† |
*unpaired-t test
†Mann-Whitney U test
HM, heating eye mask; Meiboscore, obstruction score of the meibomian gland; NIBUT, non-invasive tear break-up time.
bmjophth-2023-001307supp001.pdf (41.2KB, pdf)
The rate of positive conjunctival bacterial culture was 4% in both groups. Following eye mask treatment, these rates were 9% and 10% in the HM and control groups, respectively, but were not significantly different to the pretreatment values (p=0.15 and p=0.09, respectively). Coagulase-negative Staphylococcus was the most common organism detected after treatment, with eight cases in the HM group and six in the control group (table 3). No patient developed skin burns, skin redness or ocular surface abnormalities due to the eye mask treatment. No patient developed endophthalmitis after endophthalmic surgery.
Table 3.
Results of culture
| Result of culture | Pre | Post | |
| HM group | coagulase negative Staphylococcus | 2 | 8 |
| Methicillin-sensitive Staphylococcus aureus | 2 | 1 | |
| Not detected | 92 | 87 | |
| Control group | coagulase negative Staphylococcus | 4 | 6 |
| Methicillin-sensitive Staphylococcus aureus | 0 | 4 | |
| Not detected | 95 | 89 |
HM, heating eye mask.
Discussion
In the present study, we showed that a single treatment with a warm compress on the eye area significantly improved the NIBUT, TMH and meiboscore. The HM group also had a longer CBT than the control group. The bacterial detection rate was similar between the groups and was not increased after eye mask treatment in either group. However, the conjunctival hyperaemia score was worse after treatment with the warm compress compared with the pretreatment value.
DE is a major cause of corneal moisture loss and is classified into evaporative and aqueous-deficient subtypes.11 Diquafosol is a P2Y2 receptor agonist that stimulates water and mucin secretion onto the ocular surface18 19 and enhances ocular surface wetting.16 However, there are no reports of diquafosol improving intraoperative visibility in patients with the evaporative DE type. A randomised controlled trial reported that preoperative treatment of MGD comprising eyelid hygiene, application of warm compresses and routine postoperative anti-inflammatory treatment achieved the best MGD scores at both 1 and 3 months compared with routine postoperative anti-inflammatory treatment (tobramycin/dexamethasone drops four times daily for 1 week, then tapered over the following 4 weeks) or a more intense and extended postoperative anti-inflammatory regimen (tobramycin/dexamethasone drops six times daily for 1 week, then tapered over the following 4 weeks).20
We speculated that there were two reasons for the improvement in ocular surface conditions (such as the NIBUT and TMH) after HM treatment in the present study. One is the effect of DE treatment by improving MGD, and the other is the effect of parasympathetic nerve activation.
The DEWS II guidelines state that there are no clear standards regarding the optimal time or temperature for warm compress treatment, but that it takes a minimum of 8 min at ≥40°C to melt the oil in the meibomian glands.21 A variety of therapeutic warm compress devices have been reported to be effective in preventing obstruction of the meibomian glands immediately after treatment, including a conventional hot towel, disposable eyelid warming device (Hot Eye Mask; Kao), electrical warming and massaging device (Memoto Este; Panasonic, Osaka, Japan), warming eye pillow (Azuki no Chikara; Kiribai Chemical, Osaka, Japan), and infrared eyelid warming goggles (Eye Hot R; Cept, Tokyo, Japan).22 The effect of the disposable eyelid warming device used in the present study on DE has been previously reported, whereby a single 10 min warm compress treatment significantly improved the meiboscore.23 In our study, the application of a warm compress also improved the NIBUT and TMH, possibly because of the longer treatment time of 20 min. In patients undergoing corneal refractive surgery, the 20 min application of a spontaneous HM (Zhenshiming Pharmaceutical, Fuzhou, Jiangxi, CHN) reportedly improved the NIBUT, tear fluid lipid layer thickness and meibomian secretory function score measured 5 min after eye mask application.24 Our study confirmed these short-term increases in the tear film thickness and stability.
Parasympathetic preganglionic fibres from the pterygopalatine ganglion connect with the lacrimal nerve and reach the lacrimal gland; therefore, the parasympathetic nerves influence lacrimal gland function. Treatments to activate the parasympathetic nervous system (eg, nasal neurostimulation25 and abdominal breathing26) reportedly increase tear fluid volume. Therefore, we considered the possibility that the eye mask itself may affect the parasympathetic nervous system and ocular surface condition. However, our results showed that the NIBUT, TMH and meiboscore did not change after eye mask treatment in the control group.
In our study, the conjunctival hyperaemia score was increased after eye mask treatment in the HM group and decreased in the control group. We suggest that this effect may be due to mydriatics. The topical mydriatic agent used in our study was a combination of phenylephrine and tropicamide, which constricts the conjunctival vessels. Therefore, mydriatic drug application 2 hours before surgery may have significantly lowered the conjunctival hyperaemia score in the control group. Conversely, in the HM group, the parasympathetic nervous system was activated by the eye-warming effect, which caused the blood vessels to dilate and the conjunctival hyperaemia score to increase. Takamoto et al reported that the application of a heat-generating and steam-generating sheet to the eyelid area decreases sympathetic activity while increasing parasympathetic activity.27
According to previously reported intraclass correlation coefficient (ICC) values, the Keratograph 5M has moderate to excellent repeatability of the TMH and NIBUT scores measured in healthy individuals.28 29 However, some studies have reported poorer repeatability of NIBUT scores measured by the Keratograph 5M.30 31 Regarding ocular redness, Wu et al reported an ICC of 0.947 for the repeatability of bulbar redness measurements in 30 eyes.32 García-Montero et al suggested that performing three TMH, NIBUT first and ocular redness measurements achieved similar high ICC values; therefore, we measured the NIBUT, TMH and conjunctival hyperaemia three times.33
In the present study, we found no significant increase in the rate of bacterial detection from the conjunctival sacs before vs after warm compress treatment. Various bacteria, including commensal bacteria, are detected when meibum from healthy individuals is cultured.34 Because the rate of detection of bacteria from the meibomian glands is higher than that from the conjunctival sacs,35 we thought that the warm compress might drain the meibum and affect the results of the conjunctival sac culture, but found no significant difference in the rate of bacterial detection after warm compress treatment. Staphylococcus was the most common bacterium detected in the conjunctival sacs in our study, as previously reported.35 36 The percentage of conjunctiva with no bacteria detected (89%–91%) was higher in our study than previously reported (79.3%),35 which may be due to the use of moxifloxacin eye-drops for 3 days prior to surgery in our study. Inoue et al reported that the application of 0.5% levofloxacin ophthalmic solution for 3 days after surgery resulted in significantly higher disinfection rates than control.37 There were no cases of endophthalmitis in our study.
Conclusions
We demonstrated that treatment with a single warm compress for 20 min significantly improved the NIBUT, TMH and meiboscore. Furthermore, the warm compress lengthened the CBT, providing a longer period of good visibility during endophthalmic surgery.
Limitations
The present study has several limitations. First, we did not examine how long the intraoperative visibility remained improved after warm compress treatment. The effect of a single warm compress on the ocular surface reportedly disappears after approximately 30 min22; however, this previous report was based on a 10 min warm compress application, and it is unclear whether the effect would last longer after a 20 min application. Second, we did not assess sympathetic or parasympathetic activity. A previous report measured haemodynamic activity and performed electrocardiography.27 Because we did not measure these variables, we could not evaluate how the autonomic nervous system was affected preoperatively or intraoperatively. Third, we could not fully ascertain the effects of eye-drops on the ocular surface. Although we were aware that some patients used eye-drops for DE and glaucoma, we were not able to confirm whether other OTC medications were used, and we cannot completely exclude the possibility that this may have affected the results. OTC drugs were not used in patients with glaucoma in Japan. Statistical analysis was performed with and without the patients to exclude the effects of glaucoma and eye-drops used for glaucoma treatment (online supplemental table 1). The results of the statistical analyses did not differ between patients with and without glaucoma. However, because of the continuing relatively low cost of medical consultations in Japan and the benefits of the Japanese national health insurance system, OTC drugs are not as widely used in Japan as in other developed countries.38 Therefore, we believe that OTC medications did not have a large effect on our results. Fourth, although there was no visible difference between the eye masks used in the HM and control groups, the participants may have felt that they were receiving a hot compress treatment. To minimise bias, the study was designed to use objective parameters for assessment. Fifth, we only evaluated the short-term effects of warm compress treatment on the ocular surface. Further research on postoperative DE symptoms and changes is needed.
Acknowledgments
We thank Kelly Zammit, BVSc and Robert Blakytny, DPhil, from Edanz (https://jp.edanz.com/achttps://jp.edanz.com/ac) for editing a draft of this manuscript.
Footnotes
Contributors: SI contributed to data analysis and drafting and critically revising the paper. SY and MH conducted the experiment and collected data. KS supervised the study and revised the paper. SI is a guarantor of this paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Institutional review board/ethics committee approval was obtained from the Ethical Committee of Saitama Medical University Hospital (20090). The research adhered to the tenets of the Declaration of Helsinki. All participants provided written informed consent.
References
- 1.Nakamori K, Odawara M, Nakajima T, et al. Blinking is controlled primarily by ocular surface conditions. Am J Ophthalmol 1997;124:24–30. 10.1016/s0002-9394(14)71639-3 [DOI] [PubMed] [Google Scholar]
- 2.Mathers WD, Lane JA, Zimmerman MB. Tear film changes associated with normal aging. Cornea 1996;15:229–34. 10.1097/00003226-199605000-00001 [DOI] [PubMed] [Google Scholar]
- 3.Patel S, Farrell JC. Age-related changes in precorneal tear film stability. Optom Vis Sci 1989;66:175–8. 10.1097/00006324-198903000-00008 [DOI] [PubMed] [Google Scholar]
- 4.Paschides CA, Stefaniotou M, Papageorgiou J, et al. Ocular surface and environmental changes. Acta Ophthalmol Scand 1998;76:74–7. 10.1034/j.1600-0420.1998.760113.x [DOI] [PubMed] [Google Scholar]
- 5.Cho YK, Kim MS. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J Ophthalmol 2009;23:65–73. 10.3341/kjo.2009.23.2.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol 2002;86:418–23. 10.1136/bjo.86.4.418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Congdon NG, Schein OD, von Kulajta P, et al. Corneal complications associated with topical ophthalmic use of nonsteroidal antiinflammatory drugs. J Cataract Refract Surg 2001;27:622–31. 10.1016/s0886-3350(01)00801-x [DOI] [PubMed] [Google Scholar]
- 8.Pharmakakis NM, Katsimpris JM, Melachrinou MP, et al. Corneal complications following abuse of topical anesthetics. Eur J Ophthalmol 2002;12:373–8. 10.1177/112067210201200505 [DOI] [PubMed] [Google Scholar]
- 9.Chen HT, Chen KH, Hsu WM. Toxic keratopathy associated with abuse of low-dose anesthetic: a case report. Cornea 2004;23:527–9. 10.1097/01.ico.0000114127.63670.06 [DOI] [PubMed] [Google Scholar]
- 10.Yanai R, Yamada N, Ueda K, et al. Evaluation of povidone-iodine as a disinfectant solution for contact lenses: antimicrobial activity and cytotoxicity for corneal epithelial cells. Cont Lens Anterior Eye 2006;29:85–91. 10.1016/j.clae.2006.02.006 [DOI] [PubMed] [Google Scholar]
- 11.Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf 2017;15:276–83. 10.1016/j.jtos.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 12.Ishrat S, Nema N, Chandravanshi SCL. Incidence and pattern of dry eye after cataract surgery. Saudi J Ophthalmol 2019;33:34–40. 10.1016/j.sjopt.2018.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf 2017;15:539–74. 10.1016/j.jtos.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 14.Willcox MDP, Argüeso P, Georgiev GA, et al. TFOS DEWS II tear film report. Ocul Surf 2017;15:366–403. 10.1016/j.jtos.2017.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albietz JM. Prevalence of dry eye subtypes in clinical Optometry practice. Optom Vis Sci 2000;77:357–63. 10.1097/00006324-200007000-00010 [DOI] [PubMed] [Google Scholar]
- 16.Miyake G, Ota I, Miyake K, et al. Effects of topical diquafosol pretreatment on intraoperative corneal wetting. J Cataract Refract Surg 2014;40:1682–8. 10.1016/j.jcrs.2014.02.035 [DOI] [PubMed] [Google Scholar]
- 17.Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology 2009;116:2058–63. 10.1016/j.ophtha.2009.04.037 [DOI] [PubMed] [Google Scholar]
- 18.Jumblatt JE, Jumblatt MM. Regulation of ocular mucin secretion by P2Y2 nucleotide receptors in rabbit and human conjunctiva. Exp Eye Res 1998;67:341–6. 10.1006/exer.1998.0520 [DOI] [PubMed] [Google Scholar]
- 19.Li Y, Kuang K, Yerxa B, et al. Rabbit conjunctival epithelium transports fluid, and P2Y2(2) receptor agonists stimulate Cl(-) and fluid secretion. Am J Physiol Cell Physiol 2001;281:C595–602. 10.1152/ajpcell.2001.281.2.C595 [DOI] [PubMed] [Google Scholar]
- 20.Song P, Sun Z, Ren S, et al. Preoperative management of MGD Alleviates the aggravation of MGD and dry eye induced by cataract surgery: a prospective. Biomed Res Int 2019;2019:2737968. 10.1155/2019/2737968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf 2017;15:575–628. 10.1016/j.jtos.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 22.Arita R, Morishige N, Shirakawa R, et al. Effects of eyelid warming devices on tear film parameters in normal subjects and patients with Meibomian gland dysfunction. Ocul Surf 2015;13:321–30. 10.1016/j.jtos.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 23.Arita R, Morishige N, Sakamoto I, et al. Effects of a warm compress containing Menthol on the tear film in healthy subjects and dry eye patients. Sci Rep 2017;7:45848. 10.1038/srep45848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou X, Shen Y, Shang J, et al. Effects of warm compress on tear film, blink pattern and Meibomian gland function in dry eyes after corneal refractive surgery. BMC Ophthalmol 2021;21:330. 10.1186/s12886-021-02091-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baroody FM. How nasal function influences the eyes, ears, sinuses, and lungs. Proc Am Thorac Soc 2011;8:53–61. 10.1513/pats.201007-049RN [DOI] [PubMed] [Google Scholar]
- 26.Sano K, Kawashima M, Ikeura K, et al. Abdominal breathing increases tear secretion in healthy women. Ocul Surf 2015;13:82–7. 10.1016/j.jtos.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 27.Takamoto K, Hori E, Urakawa S, et al. Thermotherapy to the facial region in and around the eyelids altered prefrontal hemodynamic responses and autonomic nervous activity during mental arithmetic. Psychophysiology 2013;50:35–47. 10.1111/j.1469-8986.2012.01488.x [DOI] [PubMed] [Google Scholar]
- 28.Alfaro-Juárez A, Caro-Magdaleno M, Montero-Iruzubieta J, et al. Keratograph 5m as A useful and objective tool for evaluating the ocular surface in Limbal stem cell deficiency. Clin Ophthalmol 2019;13:2025–33. 10.2147/OPTH.S218313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tian L, Qu J-H, Zhang X-Y, et al. Repeatability and reproducibility of noninvasive Keratograph 5m measurements in patients with dry eye disease. J Ophthalmol 2016;2016:8013621. 10.1155/2016/8013621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fernández J, Rodríguez-Vallejo M, Martínez J, et al. Agreement and repeatability of objective systems for assessment of the tear film. Graefes Arch Clin Exp Ophthalmol 2018;256:1535–41. 10.1007/s00417-018-3986-9 [DOI] [PubMed] [Google Scholar]
- 31.Markoulli M, Duong TB, Lin M, et al. Imaging the tear film: a comparison between the subjective Keeler Tearscope-plus and the objective Oculus(R) Keratograph 5m and Lipiview(R) interferometer. Curr Eye Res 2018;43:155–62. 10.1080/02713683.2017.1393092 [DOI] [PubMed] [Google Scholar]
- 32.Wu S, Hong J, Tian L, et al. Assessment of bulbar redness with a newly developed keratograph. Optom Vis Sci 2015;92:892–9. 10.1097/OPX.0000000000000643 [DOI] [PubMed] [Google Scholar]
- 33.García-Montero M, Rico-Del-Viejo L, Lorente-Velázquez A, et al. Repeatability of noninvasive keratograph 5m measurements associated with contact lens wear. Eye Contact Lens 2019;45:377–81. 10.1097/ICL.0000000000000596 [DOI] [PubMed] [Google Scholar]
- 34.Zhang SD, He JN, Niu TT, et al. Bacteriological profile of ocular surface flora in meibomian gland dysfunction. Ocul Surf 2017;15:242–7. 10.1016/j.jtos.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 35.Jiang X, Deng A, Yang J, et al. Pathogens in the meibomian gland and conjunctival SAC: microbiome of normal subjects and patients with meibomian gland dysfunction. Infect Drug Resist 2018;11:1729–40. 10.2147/IDR.S162135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hara J, Yasuda F, Higashitsutsumi M. Preoperative disinfection of the conjunctival SAC in cataract surgery. Ophthalmologica 1997;211 Suppl 1:62–7. 10.1159/000310888 [DOI] [PubMed] [Google Scholar]
- 37.Inoue Y, Usui M, Ohashi Y, et al. Preoperative disinfection of the conjunctival SAC with antibiotics and iodine compounds: a prospective randomized multicenter study. Jpn J Ophthalmol 2008;52:151–61. 10.1007/s10384-008-0517-y [DOI] [PubMed] [Google Scholar]
- 38.Shiina A, Niitsu T, Iyo M. Need for self-medication using over-the-counter psychoactive agents: a national survey in Japan. PLoS One 2021;16:e0245866. 10.1371/journal.pone.0245866 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjophth-2023-001307supp001.pdf (41.2KB, pdf)
Data Availability Statement
Data are available on reasonable request.