Abstract
Introduction
Caring for a child with cerebral palsy may be more emotionally and physically exhausting than caring for a typical growing child. The family caregivers’ perspective of this phenomenon needs exploring to facilitate the development of services. Our study explored the challenges family caregivers face with children with cerebral palsy in a resource-limited context in northern Ghana.
Methods
We conducted a qualitative study underpinned by phenomenological principles where it is believed that the reality of a phenomenon is tied to caregivers’ perspectives of their own experiences. In this study, we unearthed caregivers’ experiences/challenges from their own perspectives. The method of data analysis used was to allow the issues to emerge from the data (inductive process) using the content analysis approach. We recruited 13 caregivers of children with cerebral palsy from the physiotherapy unit at Tamale Teaching Hospital, and conducted individual in-depth interviews supported by an open-ended topic guide. Interviews were audio recorded, transcribed, and translated and coded inductively before conducting a content analysis of the data when grouped into themes.
Results
We have identified barriers to managing a child with cerebral palsy, including sociocultural barriers (values, attitudes and belief systems within society), economic challenges and immediate physical care burdens. Specific barriers included discrimination and isolation, lack of family and societal support, with poor access to health information and formal education. Others were lack of information on the cause and course of cerebral palsy, caregivers’ loss of jobs, increased healthcare expenditure and struggles in lifting and moving children, which resonate with evidence-based multidimensional model of caregiving process and caregiver burden.
Conclusion
Caregivers have the arduous task of caring for a child with cerebral palsy. Social support interventions and policy initiatives that seek to ameliorate caregivers’ finances and make formal education accessible to this marginalised child population may be beneficial in this context.
Keywords: Qualitative research, Rehabilitation
WHAT IS ALREADY KNOWN ON THIS TOPIC
Caring for a child with cerebral palsy may impact caregivers’ physical and psychological health.
Children with cerebral palsy may have functional limitations and depend on others for assistance with daily living activities.
How caregivers cope or adapt to caregiving responsibility varies and may depend on contextual factors.
WHAT THIS STUDY ADDS
Parents of children with cerebral palsy in Ghana describe experiences of social isolation and stigma within their communities.
Caregivers of children with cerebral palsy in Tamale Hospital in Ghana perceive that they have limited information on the cause and course of the condition.
Caregivers describe high levels of spending on healthcare as well as the loss of businesses and jobs.
There is a need to tackle how to prevent stigma and social isolation for caregivers of children with cerebral palsy.
Provision of better information for caregivers on the health-related issues, cause and prognosis for children with cerebral palsy may enable parents to feel more empowered to help their children in the future.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Pragmatic steps and policy initiatives that offset the cost of accessing healthcare services for children with cerebral palsy could be beneficial in this context.
The relevant authorities should operationalise the already existing ‘all-inclusive educational policy’ to make formal education accessible to children with cerebral palsy.
The findings of this study should serve as foundational research for empirical studies that seek to develop interventions for caregivers of children with cerebral palsy.
Introduction
Cerebral palsy (CP) is a lifetime physical disability due to non-progressive injuries to the immature or developing brain.1–3 The risk factors associated with developing CP occur before, during or after pregnancy and include but not limited to intrauterine hypoxia, premature rupture of membranes, placenta abnormalities, preterm or post-term birth, asphyxia, prolonged labour, infections, hypoglycaemia, intracranial haemorrhage and respiratory distress syndrome.4 5 CP is estimated to occur in approximately 2.11 per 1000 live births globally,6 affecting males more than females,7 with more living in resource-limited settings.5 8 9
In the Ghanaian context, official statistics on the number of children with CP are lacking. However, Cerebral Palsy Africa estimated that 1 child per 300 births has CP in Ghana.10 CP causes permanent brain damage, limiting the child’s ability to have full postural control, mobility and complete activities of daily living. The motor disorders of CP are frequently accompanied by impaired cognition, communication, sensation, perception, behavioural abnormalities, seizure disorders, musculoskeletal problems or a combination of these features.11 12 The condition adversely affects children’s daily living experiences and limits their self-care functions such as feeding, dressing, bathing and mobility.13 14 Because of the functional limitations experienced, some children with CP depend on caregivers for assistance with daily activities, leading to long-term caregiving that far exceeds the usual needs of typically developing children.12 15 16 For some caregivers, providing care can be burdensome, daunting task impacting their physical and psychological well-being.12 17 This is often worse in resource-limited settings where infrastructural amenities, social support and healthcare systems are not adequately developed to ameliorate the plight of caregivers.12 18 This study was designed to evaluate the challenges family caregivers of children with CP face in a resource-limited context in northern Ghana. This will serve as a basis for developing context-relevant services and policy initiatives to better the lives of caregivers and their children with CP.
Methods
Design
Phenomenological research methods have been employed in underpinning this study as it aims to describe the lived experience of individuals caring for children with CP. The qualitative research design literature shows that phenomenological principles acknowledge people’s ties with their physical, social and emotional world,19–24 suggesting that truth about the reality of a phenomenon is embodied in people’s lived experiences.20 24 Thus, while a descriptive qualitative approach could equally be used to unearth the data required in this study to explain the experiences of carers of children with CP, the phenomenological approach fitted in better.19 22 Caregivers vary in how they adapt to caregiving demands, and the process is unique with a special meaning for the individual involved.25 The study design adapted enabled us to account for the variability in caregivers’ interpretations of their experience of care.26
Participants and setting
Thirteen family caregivers of children with CP participated in the study. We included individuals who resided with and provided care daily for a child under 18 years of age, diagnosed by a qualified medical doctor and confirmed in their medical records to have CP. The recruitment of participants took place at the physiotherapy unit of the Tamale Teaching Hospital, the only tertiary hospital in the northern region of Ghana. The hospital provides specialist care and physiotherapy services for children with diverse needs, including CP. Most of the inhabitants in this setting are Muslims, but they also practise and revere the traditional African religion. Thus, they believe in their ancestors and supernatural powers which could sometimes influence their perceptions about disease causation and management. Wholesale, retail and agricultural activities are the main occupation in the area.27 The first author, a female paediatric nurse specialist, has extensive knowledge of the study area through her residency programme. Anecdotal observations she made at this setting motivated the conduct of the study. However, she had no prior relationship with study participants.
Sampling and recruitment
We used a purposive (non-probability) sampling technique to identify and recruit participants. Once we met data saturation, we did not recruit further participants.28 29 All participants were recruited during their routine physiotherapy clinic appointment days. We observed COVID-19 protocols (maintaining social distancing, wearing personal protective equipment such as a nose mask or face shield and using hand sanitisers) during participant recruitment and data collection. We confirmed participants’ inclusion by checking diagnoses from children’s hospital records with the help of a physiotherapist to ensure that a medical professional had duly diagnosed children. We introduced the study aims and informed potential participants that involvement in the study was voluntary. Participants interested in joining the study were then provided further information using the information sheet by the researcher. Participants who consented then signed or printed their thumbprint on the consent form prior to data collection.
Data collection
We gathered participants’ demographic information such as caregiver relationship with the child, educational level, child age, marital status and caregiver occupation from all consenting participants. These characteristics were collected to add more context to the study findings as they could diversely influence caregivers’ experience. For pragmatic reasons and the challenges involved in bringing participants with different medical review dates together for focus group discussion, we conducted individual face-to-face interviews using an in-depth interview topic guide (online supplemental file 1) developed by the researchers based on the study’s objectives. Our topic guide provided open-ended questions which were then probed based on the participant’s responses.30 31 These interviews were either conducted in English language or the native language (Dagbani) at the hospital clinic based on the preferences of participants. All interviews were audio recorded and lasted 35–50 min. We wrote additional field notes to cover the observations made on each interviewee, and these were considered during the analysis for contextual issues. We conducted most interviews in the local Dagbani language. We manually transcribed recorded audio of interviews with participants verbatim into electronic text on a computer, taking cognisance of non-verbal cues captured in the field notes. We translated audio records in the local language (Dagbani) into English back to back to ensure we did not lose the meaning and were cross-checked between researchers for validation. Translated verbatim transcripts were also verified by a bilingual expert not part of the research team to ensure accuracy.32
bmjpo-2022-001807supp001.pdf (43.2KB, pdf)
Data analysis
Inductive content analysis, as described by Elo and Kyngäs,33 was used to analyse the data of this study. Content analysis is a systematic, replicable technique for compressing many words of text into fewer content categories based on explicit coding rules. Participants’ transcripts were anonymised with letters and numbers such as ‘P1’ and ‘P2’. All authors then read the transcripts repeatedly and compared samples with the interview audio files. We generated the codes inductively by highlighting critical ideas from the data. We then copied these codes and grouped them into subcategories based on their relationship. We further grouped subcategories with similar meanings to form categories. We reviewed and compared categories and subcategories with the code and the entire dataset to ensure that we captured the meaning of the entire dataset as presented by participants in the interviews.
Findings
All caregivers interviewed were women, 12 being biological parents to the child with CP. The majority were middle-aged women aged 30–68 years, with a mean age of 39 years. Most of the children (n=10) were between 2 and 4 years old. Table 1 presents the detailed demographic information of participants.
Table 1.
Demographic characteristics of participants
| Demographics | Frequency, n (%) |
| Caregiver relationship | N=13 |
| Mother | 12 (92) |
| Grandmother | 1 (8) |
| Age of caregiver | N=13 |
| 30–39 | 10 (76) |
| ≥40–49 | 3 (24) |
| Mean age | 39 |
| Educational level of caregiver | N=13 |
| Senior high school and below | 4 (31) |
| Tertiary | 6 (46) |
| No formal education | 3 (23) |
| Occupation of caregiver | N=13 |
| Trading | 5 (38) |
| Nurse | 2 (15) |
| Teacher | 1 (8) |
| Environmental health officer | 1 (8) |
| Unemployed | 4 (31) |
| Marital status of the caregiver | N=13 |
| Married | 11 (84) |
| Single | 1 (8) |
| Widow | 1 (8) |
| Age of child with CP | N=13 |
| <2 years | 2 (15) |
| 2–4 | 10 (77) |
| 5–7 | 1 (8) |
| Type of CP | N=13 |
| Spastic | 5 (38) |
| Not stated | 8 (62) |
CP, cerebral palsy.
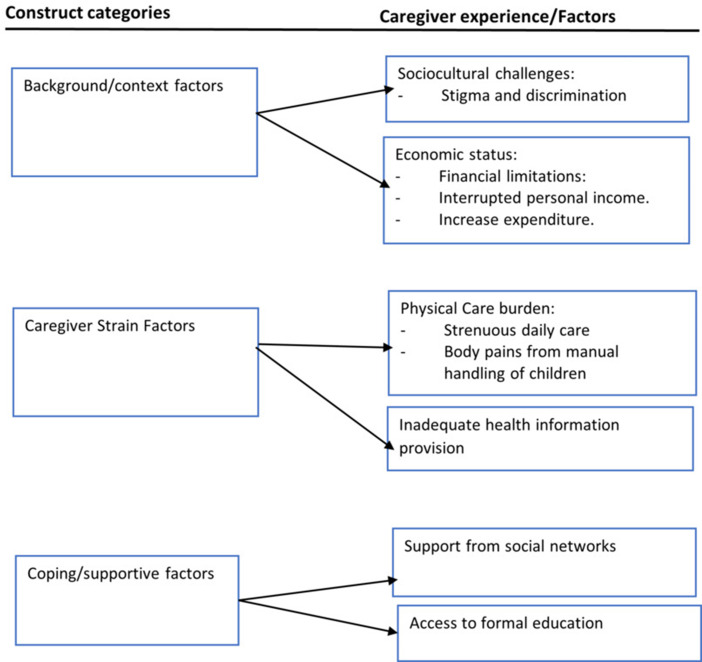
The interview data generated findings that embodied caregivers’ sociocultural issues, accessibility to health information and formal education, physical care burden and economic factors. These themes mirrored three constructs of the multidimensional model of caregiving process and caregiver burden proposed by Raina and colleagues.25 Thus, the model’s constructs of ‘background/context’, ‘caregiver strain’ and ‘coping/supportive factors’ were represented in the interview data. Generally, the model comprises of constructs and factors that facilitate the understanding of caregiving and processes affecting caregivers’ health.25 Guided by this framework, our study findings are presented in figure 1.
Figure 1.
Multidimensional experiences and challenges of caregivers.
Background/context factors
The first domain, background/context, relates more to the social and economic characteristics of the setting where caregiving takes place. Our findings depicted contextual sociocultural issues and economic status of caregivers impacting their caregiving experience as described in subsequent sections.
Sociocultural challenges
The sociocultural issues pertain to society’s cultural and intuitive beliefs about CP and its impact on caregivers. Caregivers reported how they perceived that individuals within society were often hostile to them, challenging their ability to live with their children with CP. In particular, caregivers mentioned how other members within their community often stigmatised them and had misconceptions about CP, including how it might have been caused. For example, one caregiver of a 2-year-old child with CP explained how attending social gatherings was a challenge due to the negative language used to describe her child as not human but animal:
Whenever there is an ‘occasion’ (marriage, naming ceremonies and funerals), I do not go because of how they treat the child; I do not like it. People will just be calling her all sorts of names, saying she is not human, so I should not waste my time on her. (P11, caregiver of a 2-year-old girl)
One mother enunciated how she felt the subject of ridicule—describing how she believed that some members of the community intentionally questioned her on things they knew her child could not do. Furthermore, this same mother recounted how she and her child were even seen as having something that might be ‘caught’ or infectious with others purposely not sitting near her on public transport:
We are now laughing stock to most people, some people know what the child is going through, and they will see you and intentionally ask you, so your child is still not walking ‘Penh’? Sometimes in a car like this, they do not even want you to sit closer to them, or the child should touch them… (P6, caregiver of a 2-year-old boy)
Similarly, some caregivers mentioned how they felt discriminated against even by their relatives who would not allow their own children to interact with a child with a disability in case it might be infectious. Thus, the child and caregiver could not freely relate with others due to emotional trauma and stigmatisation from others. Such constraints encountered by caregivers observed in their sample narrations are as follows:
As for discrimination, it exists. Some relatives do not allow their children closer to my child because they feel he is not normal. (P5, caregiver of a 7-year-old boy)
It was shocking to hear that one caregiver even described how much community members stigmatised children with CP—believing that CP results as a punishment from ‘the gods’ and furthermore, that children with CP are ‘spirits and not human’. This emerged in caregiver’s verbatim as emotionally very painful, leading some caregivers to seek cures through traditional healers to better understand whether their children were ‘spirits’ or ‘possessed’.
Others make insulting remarks like this your child is not a human being. We have even visited a shrine on several occasions because of that… They will give herbal preparation to bathing the child; if he is not human, he will die after bathing those herbs. But after bathing him, it is clear that he is not what they were thinking of. (P3, caregiver of a boy 4 years and 9 months)
Economic status
The caregivers in this study described through their interviews that their sources of income were interrupted, and they had financial limitations in meeting the child’s care needs. Having a child with CP means having an expenditure line inconsistent with routine household expenses, thus raising the cost of the family’s budget. Most caregivers, employed and unemployed, described their experience of having increased expenditures due to buying medications and assistive devices, transportation costs, laboratory investigations and food buying. The latter placed an extra financial burden on caregivers who may not also receive financial support as there is no clear, steady formal support for the vulnerable in Ghana. An example of experiences that were enunciated by caregivers include:
…I am supposed to be coming for review once every week, but because of the cost of transportation, I have made it once every two weeks. (P6, caregiver of a 2-year-old boy)
In this place (referring to the physio unit), I was told that health insurance would cover some part and you would also pay the rest after … sometimes. ‘Hmmm’…. It is not easy… I have even stopped the neurological consult because you have to pay for the consultation and still buy the drugs. After all, the hospital does not always have them. (P10, caregiver of a 4-year-old boy)
Besides the increased expenditure, caregivers’ economic situation was reportedly worsened when they could no longer engage in income-earning activities. Participants’ reports show that the caregiving demands of their children led to abandoning their employment as they could not combine the care of the child, which is a full-time job, with their income-generating activities, as shown in the quotes from participants:
I am no longer employed and cannot do any work again. I worked in a private hospital before I gave birth, but now this child is like this. I have stopped my employment because he has this problem (cerebral palsy). (P10, caregiver of a 4-year-old boy)
I am no longer in business because I can’t be holding him while preparing my local drinks, and there is no one to help. Where will I be getting money for his care? (P3, caregiver of a boy 4 years and 9 months)
Many of the caregivers who were initially engaged in personal businesses for income had their businesses collapse because they did not have time to continue trading. Other caregivers stopped because of the stress of juggling childcare and business. Caregivers were then left to deal with the effects of these income cuts and rising expenditures.
Caregiver strain factors
The second domain of factors, caregiver strain, denotes caregiving demands and perception of family centredness of formal healthcare services. Some participants’ narratives generally reflected the sheer physical care burden and inadequate formal health information, as detailed below.
Physical care burden
Caregivers recounted the challenges with providing activities of daily living such as bathing, dressing and moving their child while maintaining their routine responsibilities to themselves and other family members. They lamented about the exhausting nature of caring for a child with CP. Due to the physical and neurological incapacity of the child, they depend exclusively on their caregivers to meet all their needs. Most participants of this study experienced struggles in meeting the demands of children’s daily care. Caregivers’ reports indicate that lifting and moving their children were particularly challenging as it affected their well-being, as stated in their narratives below:
I usually feel tired due to carrying him always. It is a problem lifting him. I sometimes get some body pain due to carrying him because he will not sit, so I do all the time I am carrying him. I pray he can walk someday. If not, he will be a burden while growing up because I cannot carry him. (P3, caregiver of a boy 4 years and 9 months)
I feel so tired of caring for him because he has a younger sibling I have to cater. At his age (7 years), he should have been able to bathe and move about, but I still have to do it. (P5, caregiver of a 7-year-old boy)
Caregivers expressed how they often experienced body pains—depending on medications to relieve the pain from the strenuous nature of the care they provide for their child with CP. Caregivers also commented that care became more challenging as their children grew older and particularly mentioned how body pains were related to having to lift and move the children manually.
…she doesn’t want anyone to carry her, only me…so every day I have to be taking pain medications, now she has reduced in weight… at first, she was heavy so when you carry her hmmm my waist. Sometimes when I am in the room I cry because of the pains. (P11, caregiver of a 2-year-old girl)
Inadequate health information
The data show that caregivers felt that healthcare professionals did not give them enough information to enable them to understand, cope and care for their children. The lack of health information made some caregivers believe in the community’s claims of such children being spirits or animals. For instance, some participants suggested that even though health workers took the history of their child’s condition, they failed to give them information about the condition. Caregivers with English literacy who could surf the internet resorted to finding information about their child’s condition, as demonstrated below.
They asked me questions some time ago about the child’s condition, which they wrote down, but I have not been given any information regarding his condition since then… they only said we should come to this place (referring to the physio unit) and do the exercise. (P5, caregiver of a 7-year-old boy)
Even though participants reported that the internet helped them to understand their child’s condition, finding information from the internet that is not censored could be misleading as there are sources that may not be credible. Thus, a lack of adequate information from health workers could compel caregivers to sources of information that are not helpful.
At first, I did not know what was wrong with him because the doctors would not give me more information about this condition…Now I am beginning to understand because I browse the internet and read about it…(P6, caregiver of a 2-year-old boy)
Coping/supportive factors
The factors included in this third and final construct consist of social support, family function and accessibility to formal education. Social support comprises of the informal support from immediate family members, friends, neighbours and the community, while function describes the extent to which the family functions as a unit in supporting caregivers. The findings related to these are described further below.
Inadequate support from social networks
Some caregivers indicated that they received minimal or no support from family members and others in providing care for their children. Most caregivers expressed concerns that their children may be abandoned in the event of their absence:
It is not easy to get someone to care for him, especially when I am not feeling well. I still have to manage and care for him because, the way he is, who will have time to take care of him? (P3, caregiver of a boy 4 years and 9 months)
As shown in the demographics, most caregivers were females and mothers to the children. Although caregiving in Ghana is traditionally a female role, considering the additional care needs of a child with CP, many mothers might benefit from support from spouses. It was clear however in the statements of most of the caregivers that we interviewed that spouses were unsupportive and unhelpful most of the time—almost in rejecting the child with CP and their caregiver.
With this one, my husband is not helping me care for him. Do you think I will try to give birth again? He does not mind us any longer. At least once in a while, he should also pick him, and I will also rest, but he doesn’t. (P3, caregiver of a boy 4 years and 9 months)
Inadequate access to formal education
Another challenge caregivers encountered was that they could not find a suitable school that would render quality education for their children. Some mothers felt their children would not be accepted into the mainstream schools due to their condition, and special schools were unavailable. Thus, all schools within reach of caregivers were not resourced to admit children with special needs like CP. Some community members who seem not to know the depth of the child schooling problem kept recommending that the child be taken to school. See the following expression of a participant:
They said I should take her to school, but in our place, they will not admit her. They said she could not sit, and she could not walk… When you send her to these regular schools, they will not take her. Moreover, no school in our area trains such children. (P11, caregiver of a 3-year-old girl)
Discussion
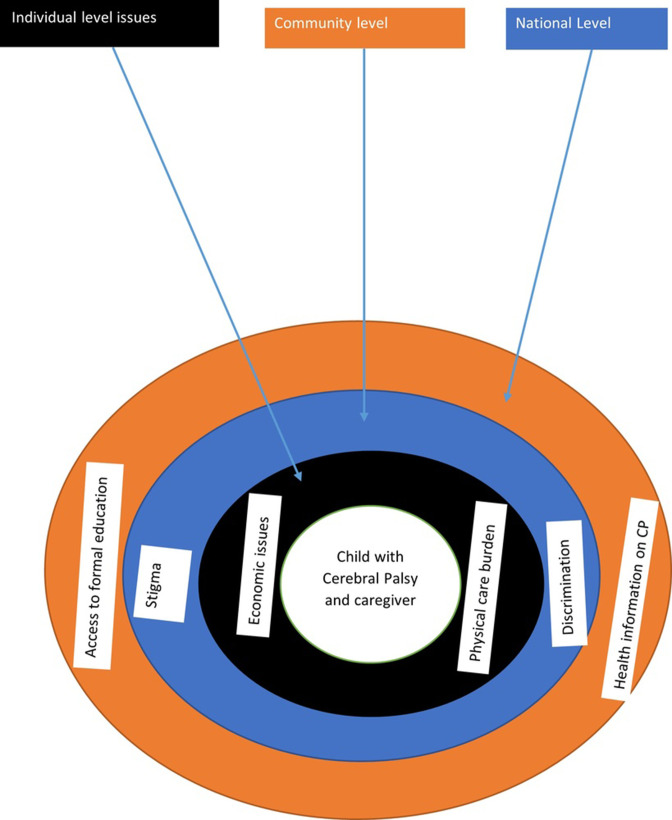
Our findings show that caregivers in this context encounter sociocultural, physical and economic challenges in caring for their children with CP. The study’s findings resonate with existing evidence and signpost critical contextual and global issues that need consideration to develop support systems and relevant interventions. To support policymakers, practitioners and researchers in the design of interventions, key findings of this study are discussed in three domains: (1) individual-level issues, (2) community level and (3) national level (see figure 2). The study findings in these domains, according to existing literature, impact caregivers’ physical health, psychological health and general well-being.25 34–36
Figure 2.
Contextual framing of caregivers’ experiences and challenges. CP, cerebral palsy.
Individual-level issues
Our finding indicates that caregivers of children with CP face physical care burdens and economic pressures. Due to muscle spasticity, weakness and uncoordinated motor control, children with CP rely mainly on their caregivers for physical care, irrespective of age.37 Although there are assistive devices for aiding in the care of sick individuals with neuromuscular inadequacies and self-care deficit,38 the caregivers in this study had to lift and move their children manually, without such devices, resulting in caregivers’ altered well-being such as aches and pains sometimes requiring medical attention. Meanwhile, the well-being of caregivers is critical, considering that most children with CP depend solely on them for their care.39 40 Therefore, though it might be useful to solicit the support of social networks to assist primary caregivers, it might even be more beneficial for health professionals to assist caregivers in learning manual handling and body mechanics to empower them to safely lift and move children.41 42
Also, at the individual level were the income cuts and increased expenditures of caregivers and their families. The loss of jobs, businesses and increased healthcare expenditures for a child with CP necessitate employers and policymakers to create a more flexible work culture that allows caregivers to engage in income-generating activities to lessen their financial burden.15 43 44 Even though the economic challenges for caregivers in this study are unavoidable, considering that the setting is generally a deprived area, the absence or limited financial support could limit caregivers’ ability to access healthcare such as rehabilitation services for the care of their child as reported in other studies.15 Specific to this study’s setting and similar populations, it might be beneficial if the current cost-sharing system of the National Health Insurance Scheme45 is re-evaluated to meet the health financing needs of these marginalised populations with CP.
Community level
The relations of children with CP, the general public and caregivers misunderstand CP especially in settings with limited general literacy,46 leading to the attribution of the condition to supernatural causes, such as punishment from the gods and witchcraft, as reported in this study and others.46 47 In our study context, children with CP were perceived as spirit children and punished by the gods. These perceptions were translated into the level of community engagement with the caregivers and the children. Existing evidence shows that beliefs in witchcraft and punishment by the gods lead to labelling, stigmatisation and discrimination against families and children with CP.47 Lack of support for caregivers resulting from stigma has been reported in the existing literature.11 17 This limited support could compound the inherent challenges of having a child with special needs. Thus, society’s understanding of CP is critical in reducing stigmatisation and discrimination against families with children with CP and the associated cyclical effect on the child and caregiver. It is therefore critical that health information on CP is intensified to ensure that communities understand the causes and course of CP, promoting empathy and involvement of support systems in providing care for the child to improve their quality of life.
National level
The study’s findings suggest that primary caregivers received limited or no health information about their child’s condition. Limited information on health issues and services is a global challenge.48–50 However, challenging settings such as Ghana, with limited economic independence, are worst in this regard.43 51–55 Anecdotal evidence from the study setting suggests that health professionals provide ad hoc health education to caregivers of children with CP and other disabilities, using medical terms that caregivers and their support systems may not understand. Yet, there is evidence that adequate caregiver knowledge may promote better care for children with CP.55 56 Indeed, the trend of breaching the gap in service users’ understanding of health issues and contributing effectively to service provision is through deliberate efforts to ensure public participation.57 Therefore, to forestall the challenges communities encounter with their health management, conscious efforts must be made to use evidence such as that identified in this study and introduce appropriate interventions that ensure optimal public participation in healthcare at every health service level.
Furthermore, existing evidence suggests that children with CP without cognitive impairment could benefit from formal education.58 Nevertheless, caregivers reported that one of their challenges was finding school placement for their children with CP. Although Ghana has an all-inclusive education policy,59 it thus appears that most schools in this setting do not have the capacity in terms of human resources and space to admit children with CP. This situation resonates with other study findings in India and Kenya reporting lack of formal education opportunities.43 60 61 This suggests the need to operationalise educational policies that make formal education more accessible to all including children with CP.
Conclusively, though the study findings might not be generalisable, it raises issues related to child physical care, cultural perceptions, health information and educational needs that must be translated into appropriate individual, community and national-level response.
Supplementary Material
Footnotes
Contributors: MMM, YNA and MWK conceptualised the study, methodology and literature review. MMM and JNS undertook the data collection, transcription and analysis. YNA reviewed transcripts and compared them with audio files. JNS and MWK drafted the manuscript. MWK and MMM reviewed the manuscript for intellectual content. All authors read and approved the final manuscript for publication. MMM is responsible for the overall content and act as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Parental/guardian consent obtained.
Ethics approval
We observed all relative ethical issues, including maintaining privacy and confidentiality, upholding the autonomy of caregivers, occasioning voluntary involvement and obtaining informed consent. We also involved a third party to assess our ethical conduct and provide ethical clearance. We therefore obtained ethical approval from the Committee on Human Research, Publication and Ethics (CHRPE) of Kwame Nkrumah University of Science and Technology (KNUST), Ghana, with reference number CHRPE/AP/231/21 and the Department of Research and Development of the Tamale Teaching Hospital with reference number TTH/R&D/SR/039, which also provided administrative permission for the study setting.
References
- 1. Cans C. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol 2000;42:816. 10.1017/S0012162200001511 Available: https://pubmed.ncbi.nlm.nih.gov/11132255/ [DOI] [PubMed] [Google Scholar]
- 2. KINSNER-OVASKAINEN A, LANZONI M. Surveillance of cerebral palsy in Europe: development of the JRC-SCPE central database and public health indicators. 2017. Available: https://publications.jrc.ec.europa.eu/repository/handle/JRC109418 [Accessed 1 2023].
- 3. Rosenbaum P, Paneth N, Leviton A. A report: the definition and classification of cerebral palsy April 2006 - PubMed. Dev Med Child Neurol 2007;49:8–14. Available: https://pubmed.ncbi.nlm.nih.gov/17370477/ [PubMed] [Google Scholar]
- 4. McIntyre S, Taitz D, Keogh J, et al. A systematic review of risk factors for cerebral palsy in children born at term in developed countries. Dev Med Child Neurol 2013;55:499–508. 10.1111/dmcn.12017 [DOI] [PubMed] [Google Scholar]
- 5. Sellier E, Platt MJ, Andersen GL, et al. Decreasing prevalence in cerebral palsy: a multi-site European population-based study, 1980 to 2003. Dev Med Child Neurol 2016;58:85–92. 10.1111/dmcn.12865 [DOI] [PubMed] [Google Scholar]
- 6. Oskoui M, Coutinho F, Dykeman J, et al. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 2013;55:509–19. 10.1111/dmcn.12080 [DOI] [PubMed] [Google Scholar]
- 7. Chounti A, Hägglund G, Wagner P, et al. Sex differences in cerebral palsy incidence and functional ability: a total population study. Acta Paediatr 2013;102:712–7. 10.1111/apa.12240 [DOI] [PubMed] [Google Scholar]
- 8. Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and National cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 2017;3:524–48. 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van Naarden Braun K, Doernberg N, Schieve L, et al. Birth prevalence of cerebral palsy: a population-based study. Pediatrics 2016;137. 10.1542/peds.2015-2872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kyeremateng JDA, Edusei A, Dogbe JA, et al. Experiences of primary Caregivers of children with cerebral palsy across the trajectory of diagnoses in Ghana. Afr J Disabil 2019;8. 10.4102/ajod.v8i0.577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Majnemer A, Shevell M, Law M, et al. Indicators of distress in families of children with cerebral palsy. Disabil Rehabil 2012;34:1202–7. 10.3109/09638288.2011.638035 Available: https://pubmed.ncbi.nlm.nih.gov/22235883/ [DOI] [PubMed] [Google Scholar]
- 12. Raina P, O’Donnell M, Rosenbaum P, et al. The health and well-being of Caregivers of children with cerebral palsy. Pediatrics 2005;115:e626–36. 10.1542/peds.2004-1689 Available: https://pubmed.ncbi.nlm.nih.gov/15930188/ [DOI] [PubMed] [Google Scholar]
- 13. Galpin J, Barratt P, Ashcroft E, et al. 'The dots just don't join up': understanding the support needs of families of children on the autism spectrum. Autism 2018;22:571–84. 10.1177/1362361316687989 [DOI] [PubMed] [Google Scholar]
- 14. Rajan AM, John R. Resilience and impact of children's intellectual disability on Indian parents. J Intellect Disabil 2017;21:315–24. 10.1177/1744629516654588 [DOI] [PubMed] [Google Scholar]
- 15. Nuri RP, Aldersey HM, Ghahari S. Needs of families of children with cerebral palsy in Bangladesh: A qualitative study. Child Care Health Dev 2019;45:36–44. 10.1111/cch.12624 [DOI] [PubMed] [Google Scholar]
- 16. Romley JA, Shah AK, Chung PJ, et al. Family-provided health care for children with special health care needs. Pediatrics 2017;139. 10.1542/peds.2016-1287 [DOI] [PubMed] [Google Scholar]
- 17. Dambi JM, Jelsma J, Mlambo T. Caring for a child with cerebral palsy: the experience of Zimbabwean mothers. Afr J Disabil 2015;4. 10.4102/ajod.v4i1.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hamzat TK, Mordi EL. Impact of caring for children with cerebral palsy on the general health of their Caregivers in an African community. Int J Rehabil Res 2007;30:191–4. 10.1097/MRR.0b013e3281e5af46 [DOI] [PubMed] [Google Scholar]
- 19. Alase A. The interpretative phenomenological analysis (Ipa): a guide to a good qualitative research approach. IJELS 2017;5:9–19. 10.7575/aiac.ijels.v.5n.2p.9 [DOI] [Google Scholar]
- 20. Creswell JW, Poth CN. Qualitative inquiry & research design + 30 essential skills for the qualitative researcher. Sage, 2017. Available: https://market.android.com/details?id=book-yMEKMQAACAAJ [Google Scholar]
- 21. Van Manen M. Researching Lived Experience: Human Science for an Action Sensitive Pedagogy: Second Edition. 2016: 1–202. Available: https://www.taylorfrancis.com/books/mono/10.4324/9781315421056/researching-lived-experience-max-van-manen [Google Scholar]
- 22. van Manen M. But is it Phenomenology? Qual Health Res 2017;27:775–9. 10.1177/1049732317699570 [DOI] [PubMed] [Google Scholar]
- 23. Neubauer BE, Witkop CT, Varpio L. How Phenomenology can help us learn from the experiences of others. Perspect Med Educ 2019;8:90–7. 10.1007/s40037-019-0509-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Herbert S. Doing Phenomenology: essays on and in Phenomenology. 2012. Available: https://books.google.com/books/about/Doing_Phenomenology.html?id=BmUyBwAAQBAJ [Google Scholar]
- 25. Raina P, O’Donnell M, Schwellnus H, et al. Caregiving process and Caregiver burden: conceptual models to guide research and practice. BMC Pediatr 2004;4. 10.1186/1471-2431-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lalvani P, Polvere L. Historical perspectives on studying families of children with disabilities: a case for critical research. DSQ 2013;33. 10.18061/dsq.v33i3.3209 [DOI] [Google Scholar]
- 27. Ghana Statistical Service . 2010 population & housing census: summary report of final results. Accra: Ghana Statistical Service, 2012. [Google Scholar]
- 28. Dworkin SL. Sample size policy for qualitative studies using in-depth interviews. Arch Sex Behav 2012;41:1319–20. 10.1007/s10508-012-0016-6 [DOI] [PubMed] [Google Scholar]
- 29. Mason M. Sample size and saturation in PHD studies using qualitative interviews. Forum Qualitative Sozialforschung 2010;11. Available: https://www.researchgate.net/publication/47408617_Sample_Size_and_Saturation_in_PhD_Studies_Using_Qualitative_Interviews [Google Scholar]
- 30. Britten N. Qualitative interviews in Healthcare. 2nd Edn. London: BMJ Books, 2006. Available: https://scholar.google.com/scholar_lookup?title=Qualitative%20interviews%20in%20healthcare&pages=11-19&publication_year=1999&author=Britten%2CN [Google Scholar]
- 31. Stuckey H. The first step in data analysis: transcribing and managing qualitative research data. Journal of Social Health and Diabetes 2014;02:006–8. 10.4103/2321-0656.120254 [DOI] [Google Scholar]
- 32. Fossey E, Harvey C, McDermott F, et al. Understanding and evaluating qualitative research. Aust N Z J Psychiatry 2002;36:717–32. 10.1046/j.1440-1614.2002.01100.x [DOI] [PubMed] [Google Scholar]
- 33. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 34. Eicher PS, Batshaw ML. Cerebral palsy. Pediatr Clin North Am 1993;40:537–51. 10.1016/s0031-3955(16)38549-2 [DOI] [PubMed] [Google Scholar]
- 35. King G. Family-centered Caregiving and well-being of parents of children with disabilities:linking process with outcome. J Pediatr Psychol 1999;24:41–53. 10.1093/jpepsy/24.1.41 [DOI] [Google Scholar]
- 36. Wallander JL, Varni JW, Babani L, et al. Disability parameters, chronic strain, and adaptation of physically handicapped children and their mothers. J Pediatr Psychol 1989;14:23–42. 10.1093/jpepsy/14.1.23 [DOI] [PubMed] [Google Scholar]
- 37. Elangkovan IT, Shorey S. Experiences and needs of parents caring for children with cerebral palsy: A systematic review. J Dev Behav Pediatr 2020;41:730–9. 10.1097/DBP.0000000000000880 [DOI] [PubMed] [Google Scholar]
- 38. Patel DR, Neelakantan M, Pandher K, et al. Cerebral palsy in children: a clinical overview. Transl Pediatr 2020;9(Suppl 1):S125–35. 10.21037/tp.2020.01.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gokcin Eminel A, Kahraman T, Genc A. Physical workload during Caregiving activities and related factors among the Caregivers of children with cerebral palsy. Ir J Med Sci 2021;190:701–9. 10.1007/s11845-020-02337-w [DOI] [PubMed] [Google Scholar]
- 40. Krigger KW. Cerebral palsy: an overview. Am Fam Physician 2006;73:91–100. Available: https://www.google.com/search?q=KRIGGER%2C+K.+W.+2006.+Cerebral+palsy%3A+an+overview.+American+family+physician%2C+73%2C+91-100.&oq=KRIGGER%2C+K.+W.+2006.+Cerebral+palsy%3A+an+overview.+American+family+physician%2C+73%2C+91-100.&aqs=chrome..69i57.1052j0j7&sourceid=chrome&ie=UTF-8 [PubMed] [Google Scholar]
- 41. Gideon Asuquo E, Tighe SM, Bradshaw C. Interventions to reduce work-related musculoskeletal disorders among Healthcare staff in nursing homes; an integrative literature review. International Journal of Nursing Studies Advances 2021;3:100033. 10.1016/j.ijnsa.2021.100033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Prall J, Ross M. The management of work-related musculoskeletal injuries in an occupational health setting: the role of the physical therapist. J Exerc Rehabil 2019;15:193–9. 10.12965/jer.1836636.318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vadivelan K, Sekar P, Sruthi SS, et al. Burden of Caregivers of children with cerebral palsy: an Intersectional analysis of gender, poverty, stigma, and public policy. BMC Public Health 2020;20:1–8. 10.1186/s12889-020-08808-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chiluba BC, Moyo G. Caring for a cerebral palsy child: a Caregivers perspective at the University teaching hospital, Zambia. BMC Res Notes 2017;10:724. 10.1186/s13104-017-3011-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Akweongo P, Aikins M, Wyss K, et al. Insured clients out-of-pocket payments for health care under the national health insurance scheme in Ghana. BMC Health Serv Res 2021;21:1–14. 10.1186/s12913-021-06401-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stigma BM. Discrimination & Marginalization: gateways to oppression of persons with disabilities in Ghana, West Africa, Michael Baffoe – WATHI. Africa Journal of Educational and Social Research 2013;3:187. Available: https://www.wathi.org/stigma-discrimination-marginalization-gateways-to-oppression-of-persons-with-disabilities-in-ghana-west-africa-michael-baffoe/ [Google Scholar]
- 47. Opoku MP, Alupo BA, Gyamfi N, et al. The family and disability in Ghana: highlighting gaps in achieving social inclusion. DCID 2018;28:41. 10.5463/dcid.v28i4.666 [DOI] [Google Scholar]
- 48. Avery JC, Braunack-Mayer AJ. The information needs of women diagnosed with Polycystic ovarian syndrome – implications for treatment and health outcomes. BMC Womens Health 2007;7:9. 10.1186/1472-6874-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Budtz S, Witt K. Consulting the Internet before visit to general practice. patients' use of the Internet and other sources of health information. Scand J Prim Health Care 2002;20:174–6. 10.1080/028134302760234645 [DOI] [PubMed] [Google Scholar]
- 50. Clarke MA, Moore JL, Steege LM, et al. Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: A literature review. Health Informatics J 2016;22:992–1016. 10.1177/1460458215602939 [DOI] [PubMed] [Google Scholar]
- 51. Atakro CA, Atakro A, Aboagye JS, et al. Older people's challenges and expectations of Healthcare in Ghana: A qualitative study. PLoS One 2021;16. 10.1371/journal.pone.0245451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Priyadharishini J, Sadan V, Prashanth STC. Based intervention package on knowledge, attitude and selected skills of home care among primary care givers of children with cerebral palsy. Indian Journal of Continuing Nursing Education 2017;18:46. Available: https://www.ijcne.org/article.asp?issn=2230-7354;year=2017;volume=18;issue=2;spage=46;epage=50;aulast=Priyadharishini [Google Scholar]
- 53. Resch JA, Mireles G, Benz MR, et al. Giving parents a voice: a qualitative study of the challenges experienced by parents of children with disabilities. Rehabil Psychol 2010;55:139–50. 10.1037/a0019473 [DOI] [PubMed] [Google Scholar]
- 54. Singogo C, Mweshi M, Rhoda A. Challenges experienced by mothers caring for children with cerebral palsy in Zambia. S Afr J Physiother 2015;71:274. 10.4102/sajp.v71i1.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zuurmond M, Nyante G, Baltussen M, et al. A support programme for Caregivers of children with disabilities in Ghana: understanding the impact on the wellbeing of Caregivers. Child Care Health Dev 2019;45:45–53. 10.1111/cch.12618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Adams MS, Khan NZ, Begum SA, et al. Feeding difficulties in children with cerebral palsy: low-cost Caregiver training in Dhaka, Bangladesh. Child Care Health Dev 2012;38:878–88. 10.1111/j.1365-2214.2011.01327.x [DOI] [PubMed] [Google Scholar]
- 57. Florin D, Dixon J. Public involvement in health care. BMJ 2004;328:159–61. 10.1136/bmj.328.7432.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gillies MB, Bowen JR, Patterson JA, et al. Educational outcomes for children with cerebral palsy: a linked data cohort study. Dev Med Child Neurol 2018;60:397–401. 10.1111/dmcn.13651 [DOI] [PubMed] [Google Scholar]
- 59. Ministry of Education . Inclusive education policy | UNICEF Ghana. 2015. Available: https://www.unicef.org/ghana/reports/inclusive-education-policy
- 60. Geere JL, Gona J, Omondi FO, et al. Caring for children with physical disability in Kenya: potential links between Caregiving and Carers' physical health. Child Care Health Dev 2013;39:381–92. 10.1111/j.1365-2214.2012.01398.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Vanderpuye I. Piloting inclusive education in Ghana: parental perceptions, expectations and involvement [PhD thesis]. Leeds, University of Leeds, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2022-001807supp001.pdf (43.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.