Abstract
Background
Perioperative anxiety and emergence delirium (ED) in young children may cause a series of adverse events, which are worth investigating. Pharmacological treatments of anxiety and delirium remain uncertain, while non-pharmacological treatments lack personalization and pertinence.
Aims
The aim of study was to determine whether an individual cartoon video can alleviate perioperative anxiety and reduce ED in young children undergoing adenoidectomy and tonsillectomy.
Methods
Children between 3 and 7 years old undergoing adenoidectomy and tonsillectomy were randomly assigned to an individual cartoon video group (group V) or a control group (group C). In group V, an individual cartoon video of the child’ s own choice was played throughout the whole waiting, anaesthesia induction and recovery periods. The children in group C were contacted through verbal conversation. The primary outcomes were anxiety measured by the Modified Yale Preoperative Anxiety Scale and ED assessed by the Paediatric Anaesthesia Emergence Delirium (PAED) scale. The secondary outcomes included cooperation during induction, postoperative pain and adverse events.
Results
The incidence of anxiety were comparable in group V and group C at the holding area (T0) (26% vs 22%, p=0.323), but the incidence of anxiety of group V were significantly lower than those of group C at the time of entering the operating room (T1), during the induction of anaesthesia (T2) and leaving the post anaesthesia care unit (T6) (p<0.001, p<0.001, p<0.001) after intervention. The peak PAED score in group V was significantly lower than that in group C (12.00 (9.00–13.00) vs 13.50 (10.00–15.00), p=0.016). We found no significant differences in cooperation during induction, postoperative pain or the incidence of adverse events between the groups (2.00 (0.00–4.00) vs 3.00 (1.25–4.00), p=0.110; F=0.059, Pgroup=0.808; 3 (7.5%) vs 4 (10), p=0.692).
Conclusions
The individual cartoon video is an effective method of reducing perioperative anxiety and alleviating ED in children.
Trial registration number
ChiCTR2200062300 (https://www.chictr.org.cn/index.aspx).
Keywords: anesthesia, adolescent health
What is already known on this topic?
Anxiety and emergence delirium are commonly observed in young children and cause many adverse effects.
The effectiveness of pharmacological treatments of anxiety and emergence delirium remains uncertain, while the effectiveness of non-pharmacological treatments lacks personalisation and pertinence.
What this study adds?
Using a child’ s favourite cartoon video can reduce the incidence of perioperative anxiety.
Using a child’ s favourite cartoon video may alleviate emergence delirium.
How this study might affect research, practice or policy?
The patients’ favourite cartoon video can be played as the intervention for anxiety and emergence delirium, which will be targeted, easy-accessed and the effect will be maximised.
Introduction
Emergence delirium (ED) is described as a complex of perceptual disturbances and psychomotor agitation that is most commonly observed in young children in the early postanaesthetic period following a sevoflurane-based anaesthetic.1 Anxiety is common in children before anaesthesia and surgery. It has been reported that up to 65% of children in the holding area and during the induction of anaesthesia experience intense anxiety about anaesthesia and surgery.2 Severe anxiety easily causes uncooperative behaviour, severe pain, ED and higher doses of sedation or preoperative analgesia.3–5 Therefore, alleviating anxiety and reducing the incidence of ED in children are of great significance for ensuring perioperative safety and improving surgical prognosis.
Tailored treatment for perioperative anxiety of a paediatric patient can use either pharmacological or non-pharmacological methods, often in tandem. The use of anxiolytic premedication in particular is valuable for certain groups,6 but the efficacy of these drugs is not clear, and the optimal dosage is unknown. In addition, due to the immaturity of children’s physical and psychological development, pharmacological treatment has side effects and potential risks, and the compliance of young children in taking medication is low. Compared with pharmacological therapy, non-pharmacological interventions are more comfortable, safer and free of drug side effects.7
As a whole non-pharmacological modalities comprise education approaches, behavioural techniques, parental presence at induction of anaesthesia and complementary medicine techniques, with each category including a range of effective strategies for reducing anxiety.7 Research has increasingly focused on exploring the effects of technology devices, especially based on audiovisual interventions.8 These technology devices (eg, smartphones,9 10 video glasses,11 streaming videoplayers,12 portable computers,13 14 iPads15 and video games16) have been widely used as a vehicle for streaming media content (eg, video games, streaming video clips, apps,17 virtual reality (VR) and cartoons) to reduce perioperative anxiety in children through distraction.
Cohen et al used cartoons as an effective distraction tool during surgical procedures in children and in another study demonstrated that playing age-appropriate videos before medical procedures was a more effective distractor than was an interactive toy.18 19 Compared with premedication or parental presence only, a handheld video game with parental presence was found to be more effective for reducing anxiety in children aged 4–12 years.16 A study also demonstrates that paediatric patients who used VR were found to have significantly lower anxiety at the time of induction of anaesthesia compared with patients who did not use VR.20 However, we found that the choices of the videos,21 handheld video games16 or VR20 in previous studies seemed to be impersonalised and limited. Most studies used the same media content as interventions, regardless of the gender and age of patients.20 22 Even if the selection is based on age and gender, it is possible that the children cannot find his/her favourite cartoon video in the options of his/her age due to individual differences. Meanwhile, it has been proved that one of the causes of ED was preoperative anxiety and that reducing preoperative anxiety can reduce the incidence of postoperative delirium.1 23 Therefore, some studies have focused only on how to reduce preoperative anxiety, while few have continued to pay attention to the anxiety of children who are awakening in the post anaesthesia care unit (PACU).1
Therefore, this study was performed to emphatically determine whether individual cartoon videos are capable of alleviating perioperative anxiety and reducing ED in young children undergoing adenoidectomy and tonsillectomy. Simultaneously, the study also investigated the impact of individual cartoon videos on induction compliance, postoperative pain and adverse events.
Methods
Ethics
This clinical trial was approved by the Ethics Committee of the Second Hospital of Anhui Medical University (Reference number: YX2022-084 (F1)) and was registered at the Chinese Clinical Trial Registry (Reference number: ChiCTR2200062300). Written consent was obtained from parents (or guardians). This single-centre, randomised clinical trial was conducted from August to September 2022 in accordance with the principles of the Helsinki Declaration.
Participants
After the introduction and invitation of the clinical trial leader, 95 patients aged between 3 and 7 years with an American Society of Anesthesiologists physical status I–II and who were scheduled for their first elective adenoidectomy or tonsillectomy under general anaesthesia were enrolled. Children having emergency surgery and those with previous anaesthetic experience, developmental delays, intellectual disability, sedative medication or chronic illnesses were excluded from the study.
Patient and public involvement
Parents or the public were not directly involved in the design, conduct or plans for the dissemination of our research.
Procedures
The day before surgery, the eligible patients were visited by a trained anaesthesiologist, and their general information was recorded. Most importantly, through conversations with children, their favourite cartoon videos even specific to favourite clips were all recorded. There were no limits to the scope of cartoons, which were freely chosen according to children’s preferences. On the day of surgery, all of the patients were brought to the holding area 30 min before surgery and treated according to the group assignment. The enrolled children were randomised into two groups using a computer-generated randomisation programme: group V (distraction by watching an individual cartoon video) and group C (control). The patients in group V began to watch a favourite cartoon video on iPad throughout the whole waiting and anaesthesia induction process. Patients in group C were contacted by the medical staff through verbal conversation to relieve their anxiety.
The surgical interventions and the administration of anaesthesia were always performed by the same professionals (two surgeons and an anaesthesiologist), and standard anaesthetic regimens and techniques were used for all patients. After the application of standard monitoring, including blood pressure, electrocardiography, blood oxygen saturation and the bispectral index, inhalation anaesthesia induction was performed at tidal volume, with incrementing sevoflurane up to 8% with a 50% mixture of air and oxygen (6 L/min). At the same time, the induction compliance checklist (ICC) score was recorded by a trained nurse. Peripheral IV access was obtained, and an appropriately sized laryngeal tube was inserted after a suitable anaesthetic depth was obtained by the injection of propofol (2 mg/kg), sufentanil (0.2 µg/kg) and cisatracurium (0.1 mg/kg). Then, atropine (0.02 mg/kg) and dexamethasone (0.1 mg/kg) were administered, and anaesthesia was maintained with remifentanil 0.2–0.3 µg/kg/min and sevoflurane 3%–5% with a Bispectral index (BIS) target range of 40–60. At the end of surgery, the children were extubated after awakening with adequate spontaneous ventilation and were transferred to the PACU for observation. In group V, the individual cartoon video was continuously played in the early recovery stage until the children left the PACU and were reunited with their parents.
Measures
Every assessment was completed by the same trained anaesthesiologist who is blinded to the group allocation. The primary outcomes were perioperative paediatric anxiety measured by the Modified Yale Preoperative Anxiety Scale (mYPAS) and ED assessed by the Paediatric Anaesthesia Emergence Delirium (PAED) scale. The mYPAS is a validated perioperative paediatric anxiety instrument with 22 items in five categories (activity, emotional expressivity, state of arousal, vocalisation and use of parents).24 In terms of activity, this domain measures the child’s level of activity or restlessness, for example, whether the child is fidgeting in their seat or moving around the room. The domain of emotional expressivity estimates the child’s emotional state and expression, for example, the child is crying, worried or happy. In terms of state of arousal, this domain measures the child’s physiological arousal, such as vigilance, sucking on thumb or panicked whimpering. The domain of vocalisation investigates whether the child is reading, moaning, screaming, and so on. And in terms of use of parents, it measures the child’s reliance on their parents for comfort and support. Scores range from 23.33 to 100, with higher scores indicating higher levels of anxiety.25 The mYPAS was administered at four time points: in the preoperative holding area (baseline, or T0), on entering the operating room (T1), during the induction of anaesthesia (T2) and on leaving the PACU (T6). Behaviour on emergence was measured using the PAED scale.26 A specially trained anaesthesiologist assessed the PAED scale at four time points: immediately after extubation (T3), on arriving in the PACU (T4), 30 min after arriving in the PACU (T5) and on leaving the PACU (T6). ED was defined as PAED scores ≥10, and PAED scores ≥15 is considered as the occurrence of severe ED.26–30 The PAED scale was also used to measure the intensity of ED, where 0 represents no ED and 20 is the maximum intensity of ED. The ICC was used to assess the cooperation of the children during the induction of anaesthesia (T2). A validated simplified 3-point scoring system for ICC (perfect (ICC=0), moderate (ICC=1–3) and poor (ICC≥4)) was used in our trial.31 The Face, Legs, Activity, Consolability, Cry (FLACC) assessment tool was also administered to measure postoperative pain at the same time as PAED. The FLACC scale scores the pain intensity by rating five behaviours (face, legs, activity, consolability and cry) to derive a score out of 10.32 For the patients suffering from ED, the first measure was to comfort the patients with words. When this failed, the patients were treated with propofol (10–20 mg intravenous). If a child exhibited signs of pain with a FLACC scale >4, sufentanil (0.05 µg/kg intravenous) was administered as rescue medication.
Statistical analysis
For the sample size calculation, we used a proportion of ED and anxiety of 50%, as reported in previously published studies.2 33 Therefore, 40 subjects per group would have a significance level of 5% and a power of 80% in detecting a 30% reduction in ED incidence between the groups. While anticipating a 15% dropout rate, we estimated that 46 patients were needed in each group.
SPSS V.26.0 statistical software was used to statistically process and analyse the data. The measurement data conforming to the normal distribution were expressed as the mean±SD, and the comparison between the groups was performed by two independent samples t test. Enumeration data were expressed by the number of patients (percentage) (n(%)), and the comparison was made by χ2 test. The comparison of measurement data that did not conform to a normal distribution was expressed by a non-parametric test and is shown as the median (25th percentile, 75th percentile).
The changes of anxiety and ED over time between two groups were evaluated by generalised linear mixed models (GLMM) with logistic link followed by pairwise comparisons with Bonferroni correction. Linear mixed model (LMM) was used to evaluate the change of pain for comparison of FLACC. Both GLMM with logistic link and LMM were adjusted for age, gender, surgery type and length of surgery and anaesthesia. Taking α=0.05 as the test level, p<0.05 indicates a statistically significant difference.
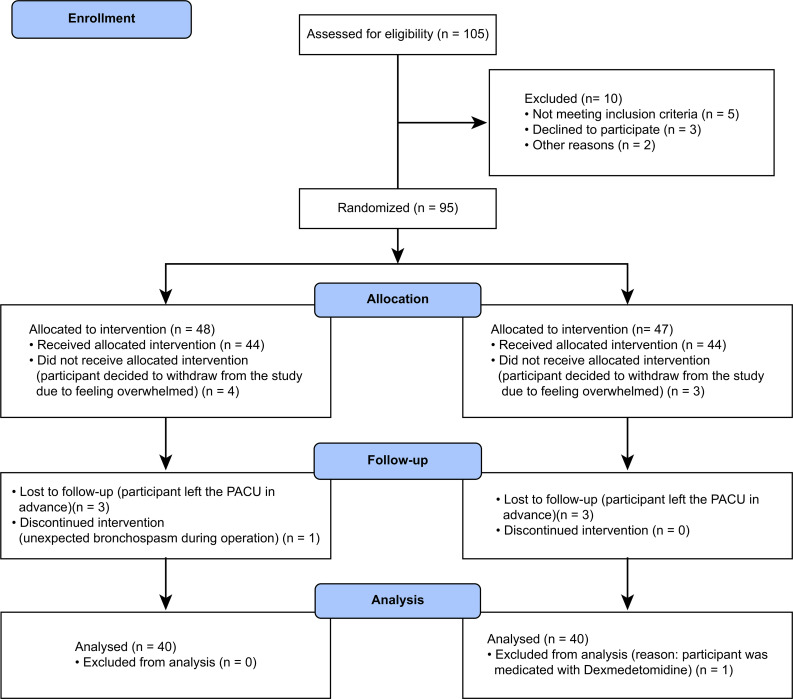
Results
As shown in the Consolidated Standards of Reporting Trials flow chart (figure 1), 95 children were enrolled in our study, and 15 children were excluded because of withdrawal of consent, loss of follow-up, discontinued intervention or extra medication. Thus, 80 participants completed the study and were included in the final data analysis. There were no statistically significant differences between the groups in terms of age, gender, height, weight, duration of surgery and anaesthesia or the type of surgery (table 1).
Figure 1.
Consolidated Standards of Reporting Trials flow diagram of the study. PACU, post anaesthesia care unit.
Table 1.
Demographic and surgical characteristics of the paediatric patients between individual cartoon video group and control group
| Individual cartoon video (n=40) |
Control (n=40) |
P value | |
| Age (years)* | 5.75±1.21 | 5.68±1.58 | 0.812 |
| Gender (male) (n (%))* | 17 (42.5) | 23 (57.5) | 0.18 |
| Height (cm)* | 114.43±9.24 | 108.10±11.92 | 0.319 |
| Weight (kg)* | 21.47±6.18 | 21.63±5.26 | 0.271 |
| Surgery length (min)* | 34.45±12.07 | 34.63±12.20 | 0.596 |
| Anaesthesia length (min)* | 47.35±15.16 | 46.23±14.09 | 0.691 |
| Surgery (n (%))† | 0.875 | ||
| Adenoidectomy | 15 (37.5) | 17 (42.5) | |
| Tonsillectomy | 10 (25) | 10 (25) | |
| Adenoidectomy+tonsillectomy | 15 (37.5) | 13 (32.5) |
Data are presented as frequency (percentage) or mean±SD (SD).
*Two independent samples t test.
†χ2 test.
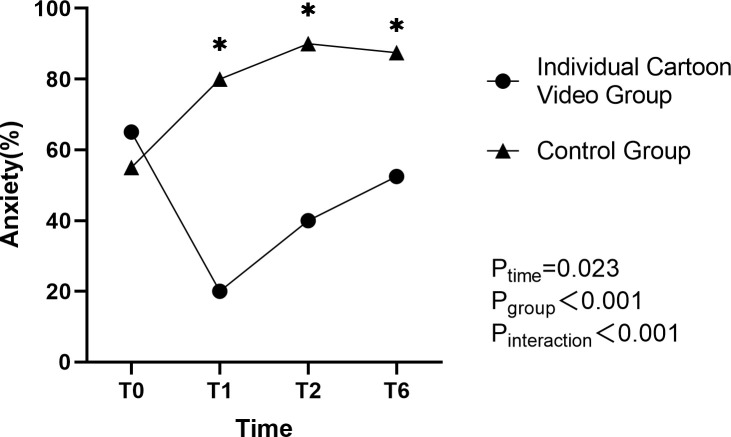
The incidence of anxiety was significantly different over time among children (F=3.212, p=0.023). There is also a significant difference in the incidence of anxiety between group V and group C (F=34.943, p<0.001) (figure 2, table 2). Moreover, the interaction effect between time and group was statistically significant (F=8.126, p<0.001) (table 2). The incidence of anxiety at T0 exhibiting baseline anxiety was not statistically different between the groups (p=0.323). After the intervention, the incidence of anxiety of group V is significantly lower than that of group C at T1 (p<0.001), T2 (p<0.001) and T6 (P<0.001) (figure 2). Meanwhile, the peak mYPAS scores showed significant difference between the two groups (p<0.001) (table 2).
Figure 2.
Anxiety occurrence in paediatric patients in the perioperative period. P<0.001 versus the control group; T0, preoperative holding area; T1, entry to the operating room; T2, induction of anaesthesia; T6, leaving the PACU; mYPAS>40 is considered as the occurrence of anxiety. mYPAS, Modified Yale Preoperative Anxiety Scale; PACU, post anaesthesia care unit.
Table 2.
Anxiety occurrence and levels in paediatric patients between individual cartoon video group and control group
| Individual cartoon video (n=40) | Control (n=40) | P value | |
| Anxiety* | <0.001† | ||
| T0 (n (%)) | 26 (65) | 22 (55) | |
| T1 (n (%)) | 8 (20) | 32 (80) | |
| T2 (n (%)) | 16 (40) | 36 (90) | |
| T6 (n (%)) | 21 (52.5) | 35 (87.5) | |
| Peak_mYPAS‡ | 51.00 (41.67–60.89) | 64.14 (53.57–85.47) | <0.001§ |
Data are presented as frequency (percentage) or median (25th percentile to 75th percentile) as appropriate.
T0, preoperative holding area.
T1, entry to the operating room.
T2, induction of anaesthesia.
T6, leaving the PACU.
mYPAS>40 is considered as the occurrence of anxiety.
Peak_mYPAS refers to the highest score of mYPAS in the four time points of T0, T1, T2 and T6.
Ptime=0.023; Pgroup<0.001; Pinteraction<0.001.
*GLMM with logistic link was adjusted for age, gender, surgery type and length of surgery and anaesthesia.
†P<0.05 is significant in GLMM with logistic link.
‡Mann-Whitney U test.
§P<0.05 versus the control group.
GLMM, generalised linear mixed model; mYPAS, Modified Yale Preoperative Anxiety Scale; PACU, post anaesthesia care unit.
The incidence of ED was significantly different over time among children (F=15.688, P<0.001). However, the incidence of ED between the groups and the interaction effect between time and group were not statistically different (F=2.169, p=0.142; F=1.220, p=0.302). Additionally, the peak of PAED in group V was significantly lower than that in group C (p=0.016) (table 3).
Table 3.
ED occurrence and levels in paediatric patients between individual cartoon video group and control group
| Individual cartoon video (n=40) | Control (n=40) |
P value | |
| ED* | 0.302 | ||
| T3 (n (%)) | 22(55) | 31 (77.5) | |
| T4 (n (%)) | 13 (32.5) | 22 (55) | |
| T5 (n (%)) | 9 (22.5) | 10 (25) | |
| T6 (n (%)) | 6 (15) | 5 (12.5) | |
| Peak_PAED† | 12.00 (9.00–13.00) | 13.50 (10.00–15.00) | 0.016‡ |
Data are presented as frequency (percentage) or median (25th percentile to 75th percentile) as appropriate.
T3, immediately after extubation.
T4, arriving in the PACU.
T5, 30 min after arriving in the PACU.
T6, leaving the PACU.
Peak_PAED refers to the highest score of PAED in the four time points of T3, T4, T5 and T6.
PAED ≥10 is considered as the occurrence of ED.
Ptime<0.001, Pgroup=0.142, Pinteraction=0.302.
*GLMM with logistic link was adjusted for age, gender, surgery type and length of surgery and anaesthesia.
†Mann-Whitney U test.
‡P<0.05 versus the control group.
§P<0.05 is significant in GLMM with logistic link.
ED, emergence delirium; GLMM, generalised linear mixed model; PACU, post anaesthesia care unit; PAED, Paediatric Anaesthesia Emergence Delirium.
The FLACC score was significantly decreased over time among children (F=3.870, p=0.010). However, the FLACC scores between the groups and the interaction effect between time and group were not statistically different (F=0.059, p=0.808; F=1.381, p=0.249). Similarly, the ICC and the incidence of adverse events were not found to be significantly different (p=0.110, p=0.692) (table 4).
Table 4.
Secondary outcomes of the paediatric patients between individual cartoon video group and control group
| Individual cartoon video (n=40) |
Control (n=40) |
P value | |
| FLACC* | 0.249 | ||
| T3 | 3.00 (1.25–4.75) | 3.50 (2.00–5.00) | |
| T4 | 3.00 (1.00–5.00) | 3.50 (2.00–5.75) | |
| T5 | 2.50 (1.00–4.00) | 3.00 (2.00–5.00) | |
| T6 | 2.00 (1.00–3.75) | 3.00 (1.00–4.00) | |
| ICC† | 2.00 (0.00–4.00) | 3.00 (1.25–4.00) | 0.11 |
| Adverse events‡ (n (%)) | 3 (7.5) | 4 (10) | 0.692 |
Data are presented as frequency (percentage) or median (25th percentile to 75th percentile) as appropriate.
T3, immediately after extubation.
T4, arriving in the PACU.
T5, 30 min after arriving in the PACU.
T6, leaving the PACU.
Adverse events refer to severe hypoxaemia, bronchospasm, postoperative bleeding and so on.
Ptime=0.010; Pgroup=0.808; Pinteraction=0.249.
*LMM was adjusted for age, gender, surgery type and length of surgery and anaesthesia.
†Mann-Whitney U test.
‡Chi-Squared Test
§P<0.05 is significant in LMM.
FLACC, Face, Legs, Activity, Consolability, Cry; ICC, induction compliance checklist; LMM, linear mixed model; PACU, post anaesthesia care unit.
Discussion
In the present study, we found that individual cartoon videos can significantly reduce the incidence of perioperative anxiety and alleviate ED in paediatric patients undergoing adenoidectomy and adenotonsillectomy.
As demonstrated in figure 2, the incidence of anxiety at T0 was not significantly different between the two groups. The individual cartoon video helped the children in group V reduce anxiety at T1. While the incidence of anxiety at T1 in group C was higher than that at T0. This indicates that simply watching the individual cartoon video at holding area may have been sufficient to reduce anxiety during entry into the operation room. Without the impact of intervention measure, the children in group C showed the increasing levels of anxiety. While children who watched the individual cartoon video had lower levels of anxiety at T1, T2 and T6 compared with that at T0. These findings are sufficient to demonstrate a strong benefit of individual cartoon video by reducing the anxiety of paediatric patients during the whole perioperative period.
Katherine12 showed that the children in the group with video distraction displayed significantly less anxiety at anaesthetic induction and had a smaller increase in anxiety from the holding area to induction than those in the standard care group. This finding is consistent with our findings. We noticed that many studies focused only on preoperative anxiety and ignored the postoperative status of the patient’s anxiety. In daily work, we observed that some paediatric patients often cry and scream after surgery. So we speculate that they may long for the company of their parents, which could also be a form of anxiety. In our study, we found that the paediatric patients in the control group displayed more anxiety when they departed from the PACU than the patients who watched the individual cartoon videos. As a result, the individual cartoon videos play a key role in alleviating anxiety in the whole perioperative period.
Kain et al 4 pointed out an important correlation between ED and preoperative anxiety in children: for every 10-point increase in the mYPAS, the risk of delirium increases by 10%. A previous study34 suggested that preoperative anxiety was one of the risk factors for ED. Thus, interventions aimed at alleviating preoperative anxiety are of great significance for preventing ED. However, few studies evaluated the effect of non-pharmacological approaches especially the technology devices in reducing the ED.
In our study, analysing the ED in the GLMM with logistic link, we did not find the significant difference in the groups and the interaction effect between time and group. When comparing the peak PAED scores between the groups, we found that the degree of ED in group V is significantly lower than that in group C. These results show that the individual cartoon video can only alleviate the severity of ED and fails to reduce the incidence of ED. Our study may not have been powered to fully demonstrate the association of other factors with anxiety and ED, such as age, gender, surgery type and length of surgery and anaesthesia. In this study, these factors did not differ between the two groups, had no impact in the multivariable analysis and thus did not impact our conclusions. There were no significant differences in the incidence of adverse events between the two groups. However, previous studies35 have found that ED increases the risk of these adverse events. The possible reason is that our study may be limited by the sample size. We calculated the sample size with the incidence of ED and anxiety, and a larger sample size is required for determining differences in adverse events.
Most young children are very fond of watching cartoon videos. A favourite cartoon can immerse children in videos and distract their attention from the unfamiliar environment and the absence of their parents so that children will not cry because of fear and anxiety. Meanwhile, many popular cartoons are freely available with public access. Therefore, the intervention of watching individual cartoons to reduce anxiety can be used without increasing healthcare costs. Inan36 demonstrated three different distraction techniques on the pain and anxiety levels of children during venipuncture, in which there are only several popular fixed options, whether in cartoon movies or video games. In our study, we did not limit the number and types of cartoon videos. We determined the patients’ favourite cartoon video 1 day before the operation and downloaded it in advance. In this way, the intervention for anxiety will be targeted, and the effect will be maximised.
Video display for paediatric patients has been an emerging audiovisual distraction modality to reduce anxiety. Initial studies in audiovisual distraction during induction of anaesthesia in paediatric patients used video games, apps and streaming video clips to demonstrate reductions in mYPAS scores.12 16 17 We innovatively chose the individual cartoon video as the intervention throughout the whole perioperative period to evaluate the anxiety and ED. Thus, the purpose and findings of this study complement existing literature examining perioperative psychological and mental state of children and offer a fresh approach to relieve perioperative anxiety and ED in paediatric patients.
In terms of the strengths of this study, first of all, the individual cartoon video is an easy and effective modality which can capture children’s attention to the maximum extent and is freely available with public access. Second, the established outcome scales we used are validated and behaviour based to reduce observer bias. Third, we included a time point after surgery to evaluate the anxiety in children and ultimately confirmed that the individual cartoon video can reduce anxiety throughout the whole perioperative period.
Several limitations related to this study should also be discussed. One limitation is that the outcomes were limited to the immediate period. Though it has been proved that the negative psychological impact of perioperative anxiety can stretch beyond the perioperative period and includes maladaptive postoperative behaviours, such as separation anxiety, nightmares and eating disorders,37–40 it remains unclear whether interventions aimed at reducing preoperative anxiety would lead to a decrease in such behaviours. Besides, the sample size of study is relatively limited. We found no significant difference of adverse events between the two groups. The most likely reason is that we calculated the sample size based on the incidence of ED and anxiety. Thus, the number of children recruited may have been insufficient to detect the effects of the individual cartoon videos on postoperative adverse events. Third, though the trained investigator was blinded to the group allocation before assessment, the blinding was impossible at some time points because cartoon video watching was visible to the investigator. As a result, observer bias may have influenced assessments of anxiety, ED, pain and compliance at induction of anaesthesia.
On the basis of our findings, future directions for further studies include longer postoperative follow-up, larger sample size and more application fields, including paediatric cardiovascular and cerebrovascular intervention therapies, radiological examinations and endoscopic examinations and treatments outside the operation room.
Conclusion
We concluded that the individual cartoon video was demonstrated to be an easy, effective and non-invasive modality for perioperative anxiety and ED in paediatric patients.
Supplementary Material
Acknowledgments
The authors thank all nurses and anaesthetists for their participation in the study.
Footnotes
XT and MZ contributed equally.
Contributors: XT and MZ contributed equally to this paper. XH is responsible for the overall content as the guarantor. All authors contributed to the study conception and design. Material preparation and data collection were performed by XT, YL, YW and XW. Data analysis was conducted by XT and MZ. The first draft of the manuscript was written by XT and MZ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding: This work is supported by the Second Affiliated Hospital of Anhui Medical University and Hefei Research Institute of Chinese Academy of Sciences (202004), Anhui Provincial Health Commission (AHWJ2021a017), Education Department of Anhui Province (KJ2021ZD0030).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Ethics Committee of the Second Hospital of Anhui Medical University (Reference number: YX2022-084 (F1)). Participants gave informed consent to participate in the study before taking part.
References
- 1. Banchs RJ, Lerman J. Preoperative anxiety management, emergence delirium, and postoperative behavior. Anesthesiol Clin 2014;32:1–23. 10.1016/j.anclin.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 2. Kain ZN. Preoperative anxiety in children. Arch Pediatr Adolesc Med 1996;150:1238. 10.1001/archpedi.1996.02170370016002 [DOI] [PubMed] [Google Scholar]
- 3. Chieng YJS, Chan WCS, Liam JLW, et al. Exploring influencing factors of postoperative pain in school-age children undergoing elective surgery. J Spec Pediatr Nurs 2013;18:243–52. 10.1111/jspn.12030 [DOI] [PubMed] [Google Scholar]
- 4. Kain ZN, Caldwell-Andrews AA, Maranets I, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg 2004;99:1648–54. 10.1213/01.ANE.0000136471.36680.97 [DOI] [PubMed] [Google Scholar]
- 5. Kim JE, Jo BY, Oh HM, et al. High anxiety, young age and long waits increase the need for preoperative Sedatives in children. J Int Med Res 2012;40:1381–9. 10.1177/147323001204000416 [DOI] [PubMed] [Google Scholar]
- 6. Heikal S, Stuart G. Anxiolytic premedication for children. BJA Educ 2020;20:220–5. 10.1016/j.bjae.2020.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agbayani C-J, Fortier MA, Kain ZN. Non-pharmacological methods of reducing perioperative anxiety in children. BJA Educ 2020;20:424–30. 10.1016/j.bjae.2020.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chow CHT, Van Lieshout RJ, Schmidt LA, et al. Systematic review: audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. J Pediatr Psychol 2016;41:182–203. 10.1093/jpepsy/jsv094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Low DK, Pittaway AP. The 'iPhone' induction - a novel use for the apple iPhone. Paediatr Anaesth 2008;18:573–4. 10.1111/j.1460-9592.2008.02498.x [DOI] [PubMed] [Google Scholar]
- 10. Kennedy N, McDonnell JG. Cartoons and the art of Paediatric inhalational induction. Anaesthesia 2010;65:1233. 10.1111/j.1365-2044.2010.06554.x [DOI] [PubMed] [Google Scholar]
- 11. Kerimoglu B, Neuman A, Paul J, et al. Anesthesia induction using Video glasses as a distraction tool for the management of preoperative anxiety in children. Anesth Analg 2013;117:1373–9. 10.1213/ANE.0b013e3182a8c18f [DOI] [PubMed] [Google Scholar]
- 12. Mifflin KA, Hackmann T, Chorney JM. Streamed Video clips to reduce anxiety in children during inhaled induction of anesthesia. Anesth Analg 2012;115:1162–7. 10.1213/ANE.0b013e31824d5224 [DOI] [PubMed] [Google Scholar]
- 13. Fortier MA, Bunzli E, Walthall J, et al. Web-based tailored intervention for preparation of parents and children for outpatient surgery (Webtips): formative evaluation and randomized controlled trial. Anesth Analg 2015;120:915–22. 10.1213/ANE.0000000000000632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tourigny J, Chartrand J. Evaluation of a preoperative virtual tour for parents and children. Rech Soins Infirm 2009:52–7. [PubMed] [Google Scholar]
- 15. Lacquiere DA, Courtman S. Use of the iPad in Paediatric anaesthesia. Anaesthesia 2011;66:629–30. 10.1111/j.1365-2044.2011.06735.x [DOI] [PubMed] [Google Scholar]
- 16. Patel A, Schieble T, Davidson M, et al. Distraction with a hand-held Video game reduces pediatric preoperative anxiety. Paediatr Anaesth 2006;16:1019–27. 10.1111/j.1460-9592.2006.01914.x [DOI] [PubMed] [Google Scholar]
- 17. Liguori S, Stacchini M, Ciofi D, et al. Effectiveness of an App for reducing preoperative anxiety in children: A randomized clinical trial. JAMA Pediatr 2016;170:e160533. 10.1001/jamapediatrics.2016.0533 [DOI] [PubMed] [Google Scholar]
- 18. Cohen LL, Blount RL, Panopoulos G. Nurse coaching and cartoon distraction: an effective and practical intervention to reduce child, parent, and nurse distress during immunizations. J Pediatr Psychol 1997;22:355–70. 10.1093/jpepsy/22.3.355 [DOI] [PubMed] [Google Scholar]
- 19. MacLaren JE, Cohen LL. A comparison of distraction strategies for Venipuncture distress in children. J Pediatr Psychol 2005;30:387–96. 10.1093/jpepsy/jsi062 [DOI] [PubMed] [Google Scholar]
- 20. Jung MJ, Libaw JS, Ma K, et al. Pediatric distraction on induction of anesthesia with virtual reality and perioperative Anxiolysis: A randomized controlled trial. Anesth Analg 2021;132:798–806. 10.1213/ANE.0000000000005004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Härter V, Barkmann C, Wiessner C, et al. Effects of educational Video on pre-operative anxiety in children - A randomized controlled trial. Front Pediatr 2021;9:640236. 10.3389/fped.2021.640236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee J, Lee J, Lim H, et al. Cartoon distraction Alleviates anxiety in children during induction of anesthesia. Anesth Analg 2012;115:1168–73. 10.1213/ANE.0b013e31824fb469 [DOI] [PubMed] [Google Scholar]
- 23. Vinícius Caldeira Q, Ricardo Vieira C, Leslie Domenici K, et al. Association between adult and child behavioral interactions with preoperative anxiety and emergence delirium. Paediatr Anaesth 2022. 10.1111/pan.14622 [DOI] [PubMed] [Google Scholar]
- 24. Jenkins BN, Fortier MA, Kaplan SH, et al. Development of a short version of the modified Yale preoperative anxiety scale. Anesth Analg 2014;119:643–50. 10.1213/ANE.0000000000000350 [DOI] [PubMed] [Google Scholar]
- 25. N KZ, C ML, V CD, et al. The Yale preoperative anxiety scale: how does it compare with a "gold standard. Anesth Analg 1997;85:783–8. 10.1213/00000539-199710000-00012 [DOI] [PubMed] [Google Scholar]
- 26. Sikich N, Lerman J. Development and Psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology 2004;100:1138–45. 10.1097/00000542-200405000-00015 [DOI] [PubMed] [Google Scholar]
- 27. Ali MA, Abdellatif AA. Prevention of sevoflurane related emergence agitation in children undergoing Adenotonsillectomy: A comparison of dexmedetomidine and propofol. Saudi J Anaesth 2013;7:296–300. 10.4103/1658-354X.115363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shi M, Miao S, Gu T, et al. Dexmedetomidine for the prevention of emergence delirium and postoperative behavioral changes in pediatric patients with sevoflurane anesthesia: a double-blind, randomized trial. Drug Des Devel Ther 2019;13:897–905. 10.2147/DDDT.S196075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen J, Li W, Hu X, et al. Emergence agitation after cataract surgery in children: a comparison of midazolam, propofol and ketamine. Paediatr Anaesth 2010;20:873–9. 10.1111/j.1460-9592.2010.03375.x [DOI] [PubMed] [Google Scholar]
- 30. Ringblom J, Wåhlin I, Proczkowska M. A Psychometric evaluation of the pediatric anesthesia emergence delirium scale. Paediatr Anaesth 2018;28:332–7. 10.1111/pan.13348 [DOI] [PubMed] [Google Scholar]
- 31. Kain ZN, Mayes LC, Wang SM, et al. Parental presence during induction of anesthesia versus sedative premedication: which intervention is more effective. Anesthesiology 1998;89:1147–56. 10.1097/00000542-199811000-00015 [DOI] [PubMed] [Google Scholar]
- 32. Crellin DJ, Harrison D, Santamaria N, et al. The Psychometric properties of the FLACC scale used to assess procedural pain. J Pain 2018;19:862–72. 10.1016/j.jpain.2018.02.013 [DOI] [PubMed] [Google Scholar]
- 33. Chandler JR, Myers D, Mehta D, et al. Emergence delirium in children: a randomized trial to compare total intravenous anesthesia with propofol and remifentanil to inhalational sevoflurane anesthesia. Paediatr Anaesth 2013;23:309–15. 10.1111/pan.12090 [DOI] [PubMed] [Google Scholar]
- 34. Kim J, Kim SY, Lee JH, et al. Low-dose dexmedetomidine reduces emergence agitation after Desflurane anaesthesia in children undergoing Strabismus surgery. Yonsei Med J 2014;55:508–16. 10.3349/ymj.2014.55.2.508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Malarbi S, Stargatt R, Howard K, et al. Characterizing the behavior of children emerging with delirium from general anesthesia. Paediatr Anaesth 2011;21:942–50. 10.1111/j.1460-9592.2011.03646.x [DOI] [PubMed] [Google Scholar]
- 36. Inan G, Inal S. The impact of 3 different distraction techniques on the pain and anxiety levels of children during Venipuncture: A clinical trial. Clin J Pain 2019;35:140–7. 10.1097/AJP.0000000000000666 [DOI] [PubMed] [Google Scholar]
- 37. Fortier MA, Del Rosario AM, Rosenbaum A, et al. Beyond pain: predictors of postoperative maladaptive behavior change in children. Paediatr Anaesth 2010;20:445–53. 10.1111/j.1460-9592.2010.03281.x [DOI] [PubMed] [Google Scholar]
- 38. Fortier MA, Del Rosario AM, Martin SR, et al. Perioperative anxiety in children. Paediatr Anaesth 2010;20:318–22. 10.1111/j.1460-9592.2010.03263.x [DOI] [PubMed] [Google Scholar]
- 39. Kain ZN, Mayes LC, Caldwell-Andrews AA, et al. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics 2006;118:651–8. 10.1542/peds.2005-2920 [DOI] [PubMed] [Google Scholar]
- 40. Kain ZN, Wang SM, Mayes LC, et al. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg 1999;88:1042–7. 10.1097/00000539-199905000-00013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.