Abstract
Introduction
COVID-19 vaccine acceptance research has mostly originated from high-income countries and reasons why youth may not get vaccinated may differ in low-income settings. Understanding vaccination coverage across different population groups and the sociocultural influences in healthcare delivery is important to inform targeted vaccination campaigns.
Methods
A population-based survey was conducted in 24 communities across three provinces (Harare, Bulawayo and Mashonaland East) in Zimbabwe between October 2021 and June 2022. Youth aged 18–24 years were randomly selected using multistage sampling. Sociodemographic characteristics, COVID-19 vaccination uptake and reasons for non-uptake were collected, and odds of vaccination was investigated using logistic regression.
Results
17 682 youth were recruited in the survey (n=10 742, 60.8% female). The median age of participants was 20 (IQR: 19–22) years. Almost two thirds (n=10 652, 60.2%) reported receiving at least one dose of COVID-19 vaccine. A higher proportion of men than women had been vaccinated (68.9% vs 54.7%), and vaccination prevalence increased with age (<19 years: 57.5%, 20–22: 61.5%, >23: 62.2%). Lack of time to get vaccinated, belief that the vaccine was unsafe and anxiety about side effects (particularly infertility) were the main reasons for not getting vaccinated. Factors associated with vaccination were male sex (OR=1.69, 95% CI 1.58 to 1.80), increasing age (>22 years: OR=1.12, 95% CI 1.04 to 1.21), education level (postsecondary: OR=4.34, 95% CI 3.27 to 5.76) and socioeconomic status (least poor: OR=1.32, 95% CI 1.20 to 1.47).
Conclusion
This study found vaccine inequity across age, sex, educational attainment and socioeconomic status among youth. Strategies should address these inequities by understanding concerns and tailoring vaccine campaigns to specific groups.
Keywords: COVID-19, vaccines, epidemiology, health services research, public health
WHAT IS ALREADY KNOWN ON THIS TOPIC
Many countries have faced challenges when rolling out COVID-19 vaccines. Infrastructure, logistics, misinformation and vaccine hesitancy have been barriers to vaccine access and uptake globally. Vaccine nationalism by high-income countries has particularly affected countries in Africa and Asia, resulting in inequity between countries and regions.
WHAT THIS STUDY ADDS
Vaccine uptake among youth in Zimbabwe was more than 50% across all age-groups. Men, those with more education and those living under less socially deprived socioeconomic conditions were more likely to be vaccinated. Fear of side effects and myths circulating on social media were identified as barriers. Religion was less of a barrier than other studies reported, likely due to religious institutions’ collaborations in COVID-19 vaccination efforts.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Vaccination campaigns should actively address specific concerns of communities, especially concerns around fertility and early death, and provide vaccines in easy-access and convenient locations. Involving community leaders in both education and vaccination efforts is pivotal given their trust and influence.
Introduction
By February 2023, more than 750 million SARS-CoV2 infections and 6.8 million COVID-19 associated deaths had been reported globally.1 The development of vaccines against SARS-CoV2, which primarily protect against severe disease, has however greatly reduced both COVID-19-related mortality and morbidity.2 3 Global vaccination programmes were fast-tracked under the COVID-19 Vaccines Global Access (COVAX) initiative at the beginning of 2021.4 Vaccination rates have, however, failed to meet the targets of vaccinating 70% of the world’s population against COVID-19 by mid-2022 set by the WHO, especially in the African continent.5
By 3 February 2023, Africa has reported a vaccination coverage (receiving at least 1 dose of a COVID-19 vaccine) of eligible population of 46% and of total population of 27%, with coverage varying greatly from<6% in Madagascar, Cameroon and the Democratic Republic of Congo to more than two-thirds of the eligible population in Rwanda and Liberia.6 7 Differences are partly explained by availability of vaccines, infrastructural constraints and COVID-19 vaccine nationalism in high-income countries (HIC) leading to insufficient donations of vaccines to low-income and middle-income countries (LMICs).8 In addition, vaccine hesitancy has been reported to be one of the main barriers towards meeting global vaccine coverage targets.9–11 Studies conducted both in HICs and LMICs have reported widespread hesitancy towards receiving the COVID-19 vaccine, despite most of the population having previously received vaccines for other viruses.12 13
Zimbabwe recorded its first case of COVID-19 in March 2020 and was subsequently among the first African countries to implement vaccination, with the first vaccine administered on 18 February 2021.14 In contrast to other countries in the region, Zimbabwe procured COVID-19 vaccines (SinoPharm and SinoVac) through a bilateral agreement with China.15 16 While non-availability of vaccines was a major barrier for vaccine uptake in other African countries, this was not the case in Zimbabwe.16 Initially, healthcare workers and people working at borders were targeted for COVID-19 vaccination, followed by those with chronic conditions and essential workers such as teachers.17 With the availability of more vaccine doses, eligibility was rapidly extended to the rest of the adult population (people aged 18 and over). In November 2021, vaccines were also made available to adolescents aged 16–18 years and in March 2022 to children aged 12 years and older.16–18 The initial vaccine schedule was two doses of either SinoPharm or SinoVac taken 3 weeks apart. A third booster dose was introduced in January 2022.19–21
The Zimbabwe vaccination campaign was administered through vaccination centres established in hospitals, clinics and outreach services. In addition, the vaccination campaign included educational programmes in schools, national mobilisation of frontline workers to assist in getting to hard-to-reach populations and nationwide health education broadcasting.18 22 23 Once vaccination eligibility was extended to adolescents, the government partnered with organisations such as United Nations Children’s Fund (UNICEF) to generate vaccination messaging targeting children and adolescents.18 24–26 As of 3 February 2023, the Zimbabwean Government estimates that 44% of the total population have received at least one COVID-19 vaccine dose. With approximately 60% of the population being eligible (12+years), coverage among those eligible was 77%.1 2
Despite the tremendous efforts put into the vaccination campaign, a considerable proportion of the general population remains unvaccinated and more recently vaccination coverage has stagnated.14 While a Partnership for Evidence-Based Response to COVID-19 survey in September 2021 demonstrated that 82% of respondents in Zimbabwe were satisfied with the government’s response, there was still some vaccine hesistancy.27 Furthermore, there is a lack of evidence in the literature regarding uptake of COVID-19 vaccination among young people and potential causes of vaccine hesitancy in Zimbabwe.
This study investigates self-reported COVID-19 vaccine uptake among 17 862 young people aged 18–24 years across three provinces (Harare, Bulawayo and Mashonaland East) in Zimbabwe and explores sociodemographic and -economic factors associated with uptake and reasons for possible vaccine hesitancy.
Methods
Enrolment
This study used data from a population-based survey which was conducted to ascertain the outcome of the CHIEDZA trial. CHIEDZA is a cluster randomised controlled trial conducted in three provinces (Harare, Bulawayo and Mashonaland East) in Zimbabwe investigating the impact of providing community-based integrated HIV and sexual and reproductive health services to young people aged 16–24 years on population-level HIV outcomes (NCT03719521).28 Taking advantage of a large population-based survey being undertaken as the COVID-19 vaccination campaign was being rolled out, we sought to understand COVID-19 vaccination coverage among youth to inform future vaccination strategies. Youth were randomly selected from both the CHIEDZA intervention and control clusters (eight clusters per province, four being the intervention and four being the standard of care) using geographic information system methods. Each cluster was mapped and divided into street sections of approximately equal length. A random sample of street sections was selected, and all residents of those sections were enumerated. All residents aged 18–24 were assessed for eligibility to participate in the survey. The survey was conducted in Harare (October–December 2021), Bulawayo (January–March 2022) and Mashonaland East (April–June 2022) aiming to recruit 16 800 18–24 year-olds (5600 per province). The sample size was based on having sufficient power to ascertain the primary outcome of the trial, which was prevalence of viral suppression among young people living with HIV. A sample size of 700 per cluster was sufficient to detect a difference in the primary outcome of 21% at 80% power, assuming an HIV prevalence of 3%.28 COVID-19 vaccines became eligible for youth (aged 18 and above) in March/April 2021 and for 16–18 year olds in November 2021.17 Sociodemographic data, self-reported COVID-19 vaccination and reasons for not being vaccinated were collected using interviewer-administered questionnaires. Participants could select multiple reasons for non-vaccination from a predefined list or give additional reasons which were recorded as free text.
Data collection and management
Participants viewed an information video about the study on a tablet screen prior to providing electronic consent. Survey data were collected onto electronic tablets using SurveyCTO (Cambridge, USA) and uploaded to the Biomedical Research and Training Institute (BRTI) server at the end of each day. Data were managed using Microsoft Access and stored in a password-controlled database, with access limited to define study personnel. Participants were identified only by ID number and no identifying data were maintained on the database. This study was performed in accordance with the study protocol, the Declaration of Helsinki as well as national and other regulatory guidelines.
Outcome
The outcome of this analysis was self-report of having received at least one dose of a COVID-19 vaccine. This was ascertained in the population-based survey with questions about COVID-19 vaccination: ‘Have you had any dose of the COVID-19 vaccine?’ with answer options being ‘Yes—one dose’, ‘Yes—two doses’, ‘I have not had any doses’. At the time of the survey, everybody eligible for the survey (18–24 year olds) was also eligible for COVID-19 vaccination.
A binary ‘yes/no’ response to vaccination was used for the analyses investigating associations.
Risk factors
The sociodemographic characteristics included in this analysis to understand factors associated with self-report of having received at least one dose of a COVID-19 vaccine were: age, sex, educational attainment, socioeconomic status defined through a principal component analysis, marital status and employment. Age was categorised, sex was binary (male/female) and education attainment was split into (1) none/primary, (2) form 4, (3) form 6 and (4) postsecondary. Marital status was grouped into (1) single, (2) married/living as if married and (3) divorced widows. Finally, employment was grouped into (1) none, (2) student, (3) employed (formal) and (4) employed (informal).
Data analysis
Data analysis was conducted using Stata V.16.1 (Stata, USA). A descriptive analysis was performed using proportions for categorical data, medians and means for continuous data, followed by a univariable logistic regression analysis to investigate the association between sociodemographic characteristics (sex, age, educational attainment, employment, marital status, socioeconomic status) and self-reported COVID-19 vaccine uptake. The outcome was self-report as having received at least one dose of a COVID-19 vaccine. Factors associated with the outcome in the univariable model were built into a multivariable logistic regression model, using only respondents with no missing data as only 22/17 682 (0.12%) were missing observations in the key covariates. To control for time, month of data collection was included in the model a priori. A likelihood ratio test was conducted for each variable to assess strength of evidence of association and reported as a p value. A sensitivity analysis was conducted including only participants from the control clusters of the CHIEDZA trial to understand whether the results of the analysis differed when including control clusters only as compared with using all data from intervention and control clusters. For the sensitivity analysis, a second multivariable logistic regression model was run using only participants from the control clusters. The socioeconomic status variable was created using a principal component analysis of ownership of assets (refrigerator, bicycle, car, TV, radio, microwave, cell phone and computer) and was then reported in quintiles (online supplemental table 4).29 Analysis was performed for all provinces and then performed separately for each province as enrolment was conducted sequentially. Reasons for not taking up the vaccine were categorised according to the ‘5C’s’ as described by Razai et al: (1) confidence (safety and efficacy of the vaccine), (2) complacency (perception of low risk and disease severity), (3) convenience (barriers and access), (4) communication (sources of information) and (5) context (sociodemographic characteristics).30
bmjgh-2023-012268supp001.pdf (118.8KB, pdf)
Patient and public involvement
The information video about the study was codesigned with and piloted among youth. The study questionnaire was also piloted with youth. The study had a Youth Advisory Board that provided guidance on study design and conduct. An extensive public engagement programme was undertaken alongside the study that included a national crowdsourcing competition to (a) elicit young people’s perceptions about health issues in their communities and (b) train youth as researchers through a mentored programme termed Youth Researchers Academy.31
Results
Of the 18 682 randomly sampled eligible youth in the study communities, 17 682 (94.6%) provided consent to participate. Of these, 5849 (33.1%) were recruited in Harare, 5969 (33.8%) in Bulawayo and 5864 (33.2%) in Mashonaland East. The median age of survey participants was 20 years (IQR: 19–22), and 10 742 (60.8%) were women. This higher proportion of women reflected the community composition.
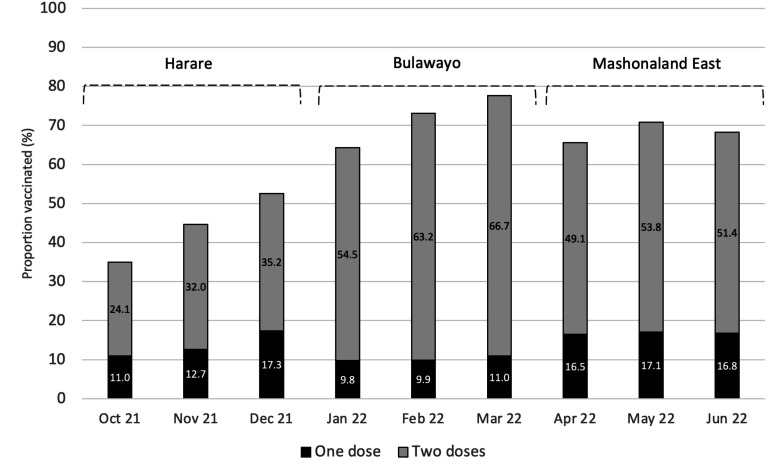
Overall, 10 652 (60.3%) participants self-reported having received at least one dose of a COVID-19 vaccine, with 8316 (78.1%) having received two doses (figure 1). The proportion vaccinated was higher among males (n=4779, 68.9%) compared with females (n=5872, 54.7%) and increased with age (<20: 57.5%, 20–22: 61.5%, >22: 62.2%) (table 1). Overall, Harare province, where data collection preceded the other provinces by 3 (Bulawayo) and 6 (Mashonaland East) months, had the lowest proportion vaccinated (42.6%) compared with Bulawayo (69.6%) and Mashonaland East (68.3%) (figure 1). The proportion vaccinated and double-vaccinated increased with each subsequent month during the survey in Harare and Bulawayo, but not in Mashonaland East.
Figure 1.
Proportion of young people aged 18-24 who reported being vaccinated by month of the CHIEDZA prevalence survey stratified by province.
Table 1.
Sociodemographic characteristics and reported COVID-19 vaccination
| n | Vaccinated | |
| Sex | ||
| Male | 6940 | 4779 (68.9%) |
| Female | 10 742 | 5872 (54.7%) |
| Age | ||
| <20 | 6809 | 3916 (57.5%) |
| 20–22 | 4702 | 2894 (61.5%) |
| >22 | 6171 | 3841 (62.2%) |
| Province | ||
| Harare | 5849 | 2492 (42.6%) |
| Bulawayo | 5969 | 4155 (69.6%) |
| Mashonaland East | 5864 | 4004 (68.3%) |
| Education | ||
| Primary/None | 3254 | 1452 (44.6%) |
| Form 4 | 10 784 | 6352 (58.9%) |
| Form 6 | 2233 | 1702 (76.2%) |
| Postsecondary | 1411 | 1145 (81.2%) |
| Employment | ||
| Student | 4963 | 3479 (70.1%) |
| Employed (formal) | 835 | 585 (70.1%) |
| Employed (informal) | 3158 | 1821 (57.7%) |
| None | 8726 | 4766 (54.6%) |
| Marital status | ||
| Married | 3559 | 1511 (42.5%) |
| Single | 13 324 | 8732 (65.5%) |
| Divorced or widowed | 799 | 408 (51.1%) |
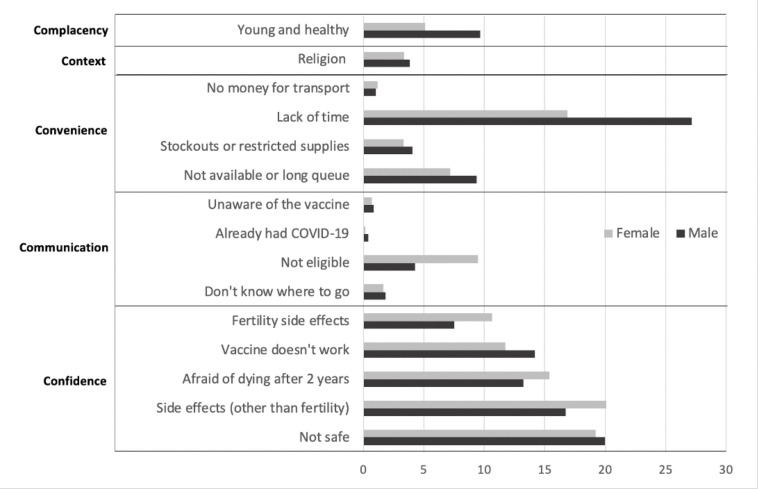
The major reasons given for not being vaccinated were lack of time, belief that the vaccine was unsafe and anxiety about side effects (figure 2). Men reported a lack of time as the main reason for not getting vaccinated. Women reported concerns related to side effects and safety as reasons for not getting vaccinated more frequently compared with men, especially infertility (10.7%). A total of 755 (4.3%) women in the survey were pregnant at the time of recruitment. Of these women, 297 (39.3%) reported having received at least one dose of a COVID-19 vaccine. Of note, participants frequently reported that they were ‘afraid to die within 2 years of receiving the vaccine’, 17.7%, 15.6% and 8.2% in Harare, Mashonaland East and Bulawayo, respectively. On the other hand, religious belief was a less commonly (<5.0%) mentioned reason for getting vaccinated. While those living under more deprived socioeconomic circumstances had lower vaccine uptake, reasons for not getting vaccinated were similar across all socioeconomic quintiles (online supplemental table 1).
Figure 2.
Reasons for not receiving the COVID-19 vaccine stratified by sex and grouped based on the 5C’s of vaccine hesitancy delineated by Razai et al. shown as proportions (%).31
Univariable analysis (online supplemental table 2) showed an association between vaccine uptake and age, sex, educational attainment and socioeconomic status. The association between vaccine uptake and predictors remained in the multivariable analysis (table 2). Men (OR 1.69, 95% CI 1.59 to 1.80), older youth (20–22: OR 1.06, 95% CI 0.98 to 1.15, >22: OR 1.12, 95% CI 1.04 to 1.21), those with higher educational attainment (form 4: OR 1.79, 95% CI 1.39 to 2.30, form 6: OR 3.56, 95% CI 2.72 to 4.66, postsecondary: OR 4.34, 95% CI 3.27 to 5.76) and higher socioeconomic status (second quintile: OR 1.06, 95% CI 0.96 to 1.17, third quintile: OR 1.12, 95% CI 1.01 to 1.23, fourth quintile: OR 1.17, 95% CI 1.06 to 1.29, least poor 20%: OR 1.32, 95% CI 1.20 to 1.47) were more likely to be vaccinated. Overall results and results stratified by province were comparable. The sensitivity analysis conducted with the same exposure variables using only the control clusters of the CHIEDZA intervention yielded similar results (online supplemental table 3).
Table 2.
Multivariable logistic regression analysis of the association between COVID-19 vaccination and sociodemographic variables
| Overall OR (95% CI) |
Harare OR (95% CI) |
Bulawayo OR (95% CI) |
Mashonaland East OR (95% CI) |
|
| Sex | ||||
| Female | 1 (p<0.0001) | 1 (p<0.0001) | 1 (p<0.0001) | 1 (p<0.0001) |
| Male | 1.69 (1.59 to 1.80) | 1.45 (1.29 to 1.64) | 1.43 (1.27 to 1.61) | 1.84 (1.63 to 2.08) |
| Age | ||||
| <20 | 1 (p=0.0123) | 1 (p<0.0001) | 1 (p=0.0002) | 1 (p=0.6537) |
| 20–22 | 1.06 (0.98 to 1.15) | 1.23 (1.06 to 1.42) | 1.24 (1.08 to 1.43) | 0.94 (0.81 to 1.08) |
| >22 | 1.12 (1.04 to 1.21) | 1.43 (1.25 to 1.63) | 1.31 (1.14 to 1.50) | 0.99 (0.86 to 1.14) |
| Education | ||||
| Primary | 1 (p<0.0001) | 1 (p<0.0001) | 1 (p<0.0001) | 1 (p<0.0001) |
| Form 4 | 1.79 (1.39 to 2.30) | 1.81 (1.15 to 2.86) | 1.83 (1.15 to 2.93) | 1.39 (0.88 to 2.20) |
| Form 6 | 3.56 (2.72 to 4.66) | 4.09 (2.55 to 6.57) | 3.50 (2.13 to 5.75) | 2.84 (1.73 to 4.66) |
| Secondary and above | 4.34 (3.27 to 5.76) | 5.20 (3.19 to 8.47) | 4.44 (2.60 to 7.58) | 3.51 (2.08 to 5.92) |
| Socioeconomic status | ||||
| Poorest 20% | 1 (p<0.0001) | 1 (p<0.0001) | 1 (p=0.3776) | 1 (p=0.0010) |
| 2nd poorest 20% | 1.06 (0.96 to 1.17) | 1.26 (1.05 to 1.50) | 1.04 (0.89 to 1.22) | 0.95 (0.81 to 1.13) |
| 3rd poorest 20% | 1.12 (1.01 to 1.23) | 1.38 (1.16 to 1.64) | 0.99 (0.78 to 1.25) | 0.99 (0.83 to 1.18) |
| 4th poorest 20% | 1.17 (1.06 to 1.29) | 1.70 (1.43 to 2.03) | 1.10 (0.92 to 1.32) | 1.01 (0.83 to 1.23) |
| Least poor | 1.32 (1.20 to 1.47) | 1.93 (1.61 to 2.31) | 1.09 (0.90 to 1.31) | 1.32 (1.09 to 1.61) |
Analysis was adjusted for month of recruitment.
P values are the result of a likelihood ratio test.
Discussion
This study found a COVID-19 vaccine coverage among young people aged 18–24 years of 69.6% in Bulawayo, 68.3% in Mashonaland East and 42.6% in Harare. Despite not being a high-risk group, the national vaccination campaign reached them effectively. Vaccine uptake was however inequitable. Those who were male, older, more educated and of higher socioeconomic status were more likely to report COVID-19 vaccination, which is in line with studies conducted in HICs, though the specific reasons may be different. Education attainment and male sex were the strongest predictors.
The difference in COVID-19 vaccine coverage among youth across the provinces is partly explained by the staggered timing of the survey. The national vaccination campaign started in February 2021 prioritising front-line workers. Vaccination eligibility was extended to all adults in March/April 2021 and 16–18 year-olds became eligible in November 2021 (1 month after study recruitment started in Harare). At the time the survey was completed in each province, the provincial vaccine coverage in Zimbabwe was 25.3% (Harare), 31.7% (Bulawayo) and 38.6% (Mashonaland East).32 Importantly, in the context of COVID-19 vaccination, coverage has been defined as the percentage of the total population that is vaccinated and includes children even though they may not be eligible.33 At the end of the survey, vaccine coverage using the total eligible population (16+ years) as denominator was 73.8% nationally and thus comparable to coverage among youth in Mashonaland East.2
In the full adjusted model, men had 1.69 times the odds of having received the vaccine compared with women. Other studies have found higher proportions of men compared with women reporting intention to getting the COVID-19 vaccine.34–36 These studies have also highlighted that the difference in intention to getting vaccinated against COVID-19 between men and women is less about increased health-seeking behaviour in men and more about decreased health-seeking behaviour among women, which is consistent with existing literature on general vaccine hesitancy.37 38 This difference is likely due to specific gender differences in risk aversion and potential side effects. Reasons for not getting vaccinated in our study were mainly related to confidence, that is, regarding safety and efficacy of the vaccine, especially among women. In this survey, 20.1% of women who were not vaccinated said they were afraid of side effects in general and 10.7% said they were afraid of infertility specifically. Furthermore, 66/458 (14.4%) of unvaccinated pregnant women reported fertility-related fears as a barrier, despite the WHO having recommended the use of SinoPharm in pregnant women.34–36 39 This disparity may be due to confusing communication regarding pregnancy and breast feeding at the start of the vaccination campaign, including information by official sources and on social media.40 41 The infodemic about vaccines spread through social media has undoubtably played an important role in Zimbabwe given the high proportion of individuals (both men and women) who reported being afraid of dying within 2 years of vaccination. This myth relates to a widely and globally circulated text message meme claiming that French virologist Luc Montagnier had said all vaccinated people will ‘die within 2 years’.42
Fear of side effects was less frequent among unvaccinated men compared with women, and a higher proportion of men did not feel at risk (felt ‘young and healthy’) or said they were too busy for vaccination. This is despite a vaccination campaign that tried to bring vaccines to the population by offering transport incentives such as transport money, decentralising vaccination to polyclinics and providing vaccine outreach services.16
Vaccination rates varied by socioeconomic status and particularly educational attainment, pointing towards health inequity. Other studies have reported that poorer and less educated people experience more barriers to vaccination.43 44 Those with lower educational attainment are less likely to have access to accurate information and the vaccine information itself might be inaccessible in terms of language, content and format, especially if this is provided in a written format.45 Public health information may also include jargon which discriminates against those of lower education level. Those of lower socioeconomic status were also more likely to experience adverse events such as a cut in household income, inability to access food, higher disease risk or loss of work than those in higher quintiles, which affects people’s ability to receive a vaccine.46
In this study, only a small proportion of individuals said they were not vaccinated because of their religious beliefs. This is in contrast to the results from studies conducted in other countries in Africa where religious beliefs were among the most frequent reasons given for vaccine hesitancy.10–12 In Zimbabwe, the Apostolic church, a Pentecostal Christian denomination, has an estimated 3.5 million followers mainly among poorer and rural households. Children of members of the Apostolic church have been found to have low childhood vaccination coverage.47 Religious affiliation was not collected in the survey, but membership of the Apostolic church is less common in urban and periurban settings, which may explain some of our findings. Also, the Ministry of Health and Child Care, supported by UNICEF, actively reached out to churches including the Apostolic Church to support vaccine education and public engagement.48 The Apostolic Women’s Empowerment Trust started a COVID-19 awareness programmes in 2021 with the aim to address vaccine hesitancy among those of Apostolic faith.49
Strengths of this study include a large representative sample of young people from three provinces at the time of the COVID-19 vaccine rollout. Participation in the survey was high and results were comparable across all three provinces. The main limitation of this study is that COVID-19 vaccination status was self-reported and social desirability bias may have resulted in overestimation of vaccination coverage. However, the survey included a range of potentially sensitive questions, on topics including sexual and reproductive health, and substantial efforts were invested in training the survey team. The survey was conducted in urban and periurban settings only and vaccination coverage may be very different among young people living in rural areas. There were no questions specifying the type of vaccine received or the date of vaccination. Another limitation was that the timing of the survey relative to the COVID-19 vaccination campaign differed between the three provinces. Furthermore, the multivariable logistic regression used univariable analysis screening methods to select the covariates for the model. This method may have erroneously excluded covariates in the full model and have led to biased estimates. Finally, while we asked young people to provide reasons for not being vaccinated, more detailed questions on beliefs, myths and sources of information might have provided better understanding. Further qualitative research investigating the barriers towards vaccination, especially among women, would strongly contribute to the findings reported in this study.
Conclusion
This study showed inequitable COVID-19 vaccine coverage among young people aged 18–24 years in three provinces in Zimbabwe (Harare, Bulawayo and Mashonaland East). Vaccination rates were lower among women, people with lower educational attainment and among those living in more deprived socioeconomic circumstances. Fear around death and infertility were among the main reasons for vaccine hesitancy. Therefore, we recommend that national vaccination campaigns should include a major focus on health education, especially for women and those with less education, and particularly around infertility and death. Information that is clear and consistent provided by trusted sources is crucial, and in this way, social media can be used in a positive manner to combat misinformation. Furthermore, campaigns should focus on community and religious leaders as they have a strong impact on their respective groups. No single programme is likely to address vaccine hesitancy in this population and thus strategies should address these inequities by understanding concerns and tailoring vaccine campaigns to specific groups which may be at a socioeconomic disadvantage instead of a one-size-fits-all approach.
Footnotes
Handling editor: Seema Biswas
Twitter: @LarssonLeyla, @chidodc, @rashida_abbferr
Contributors: RJH, RAF, CDC and KK conceptualised and designed the study. CDC, ED and MT were responsible for project management. LL, TB and VS were responsible for data curation. LL, VS and TB analysed the data. LL and KK wrote the first draft of the paper. All authors contributed to writing and/or review of the manuscript. KK approved the content as guarantor.
Funding: The CHIEDZA study is funded by the Wellcome Trust (Senior Fellowship to RAF: 206316/Z/17/Z).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The data will be made available on LSHTM Data Compass within 12 months of publication.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study received ethical approval from the Medical Research Council of Zimbabwe (MRCZ) (MRCZ/A/2387), the BRTI Institutional Review Board (IRB) (AP149/2018) and the London School of Hygiene and Tropical Medicine (LSHTM) ethics committee (16124).
References
- 1.World Health Organization (WHO) . WHO Coronavirus (COVID-19) dashboard 2023. 2023. Available: https://covid19.who.int/
- 2.Statista . Zimbabwe: age structure from 2011 to 2021. 2023. Available: https://www.statista.com/statistics/455307/age-structure-in-zimbabwe/
- 3.Ullrich F, Hanoun C, Turki AT, et al. Early report on the severity of COVID‐19 in hematologic patients infected with the SARS‐Cov2 Omicron variant. Eur J Haematol 2022;109:364–72. 10.1111/ejh.13818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahmani K, Shavaleh R, Forouhi M, et al. The effectiveness of COVID-19 vaccines in reducing the incidence, hospitalization, and mortality from COVID-19: A systematic review and meta-analysis. Front Public Health 2022;10:873596. 10.3389/fpubh.2022.873596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Strategy to achieve global COVID-19 vaccination by mid-2022. 2021. [Google Scholar]
- 6.CGTN Africa . Zimbabwean President, government officials receive COVID-19 booster shots. n.d. Available: https://africa.cgtn.com/2022/01/05/zimbabwean-president-government-officials-receive-covid-19-booster-shots/
- 7.Africa CDC COVID-19 vaccine dashboard 2023. n.d. Available: https://africacdc.org/covid-19-vaccination/
- 8.Our world in data. Coronavirus (COVID-19) vaccinations . Our world in data. 2022. Available: https://ourworldindata.org/covid-vaccinations
- 9.Njoga EO, Awoyomi OJ, Onwumere-Idolor OS, et al. Persisting vaccine hesitancy in Africa: the whys, global public health consequences and ways-out—COVID-19 vaccination acceptance rates as case-in-point. Vaccines (Basel) 2022;10:1934. 10.3390/vaccines10111934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ackah BBB, Woo M, Stallwood L, et al. COVID-19 vaccine hesitancy in Africa: a Scoping review. Glob Health Res Policy 2022;7:21.:21. 10.1186/s41256-022-00255-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahn K, Pettifor A, Mataboge P, et al. COVID-19 vaccine hesitancy in rural South Africa: deepening understanding to increase uptake and access. J Glob Health 2022;12:05013. 10.7189/jogh.12.05013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Larson HJ. The vaccine-hesitant moment. reply. N Engl J Med 2022;387:1050–1. 10.1056/NEJMc2210367 [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . Immunization Zimbabwe 2022 country profile. n.d. Available: https://www.who.int/publications/m/item/immunization-zwe-2022-country-profile
- 14.Chitungo I, Dzinamarira T, Tungwarara N, et al. COVID-19 response in Zimbabwe: the need for a paradigm shift COVID 2022;2:895–906. 10.3390/covid2070065 [DOI] [Google Scholar]
- 15.Sadeghalvad M, Mansourabadi AH, Noori M, et al. Recent developments in SARS‐Cov‐2 vaccines: A systematic review of the current studies. Rev Med Virol 2023;33:e2359. 10.1002/rmv.2359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murewanhema G, Musuka G, Denhere K, et al. The landscape of COVID-19 vaccination in Zimbabwe: A narrative review and analysis of the strengths, weaknesses, opportunities and threats of the programme. Vaccines (Basel) 2022;10:262. 10.3390/vaccines10020262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murewanhema G, Burukai TV, Chireka B, et al. Implementing national COVID-19 vaccination programmes in sub-Saharan Africa- early lessons from Zimbabwe: a descriptive cross-sectional study. Pan Afr Med J 2021;40:180. 10.11604/pamj.2021.40.180.30824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UNICEF . Children’s vaccination campaign gathers momentum in Zimbabwe. 2022. Available: https://www.unicef.org/zimbabwe/stories/childrens-vaccination-campaign-gathers-momentum-zimbabwe
- 19.Xinhua . Zimbabwe receives latest vaccine donation from China amid 4TH wave of COVID-19 pandemic. XINHUANET 2021. Available: http://www.news.cn/english/africa/2021-12/21/c_1310384569.htm [Google Scholar]
- 20.Ministry of Health and ChildCare . Zimbabwe COVID-19 Sitrep 15/10/2022 Harare. 2022. Available: https://twitter.com/MoHCCZim/status/1581528130157543425
- 21.allAfrica . Zimbabwe: experts advocate for Covid booster jab. 2022. Available: https://allafrica.com/stories/202201060203.html
- 22.Dzinamarira T, Nachipo B, Nyathi A, et al. The case to scale up Edutainment as an effective public health communication intervention to combat the COVID-19 pandemic in Zimbabwe. Health Promot Perspect 2022;12:34–6. 10.34172/hpp.2022.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Herald . Zimbabwe: GOVT launches COVID-19 vaccination blitz. 2022. Available: https://allafrica.com/stories/202203170495.html
- 24.UNICEF . Youth advocates make the difference in Zimbabwe’s COVID Hotspots. 2022. Available: https://www.unicef.org/zimbabwe/stories/youth-advocates-make-difference-zimbabwes-covid-hotspots
- 1.Murals a game Changer in Zimbabwe’s battle against COVID-19. 2022. Available: https://www.unicef.org/zimbabwe/stories/murals-game-changer-zimbabwes-battle-against-covid-19
- 26.UNICEF . UNICEF partners with youth advocates Zimbabwe in youth-led COVID-19 campaign. 2022. Available: https://www.unicef.org/zimbabwe/stories/unicef-partners-youth-advocates-zimbabwe-youth-led-covid-19-campaign
- 27.PERC . Finding the balance: public health and social measures in Zimbabwe. 2021. Available: https://preventepidemics.org/wp-content/uploads/2021/10/zimbabwe_en_20211028_1236.pdf
- 28.Dziva Chikwari C, Dauya E, Bandason T, et al. The impact of community-based integrated HIV and sexual and reproductive health services for youth on population-level HIV viral load and sexually transmitted infections in Zimbabwe: protocol for the CHIEDZA cluster-randomised trial [version 1; peer review: awaiting peer review]. Wellcome Open Res 2022;7:54. 10.12688/wellcomeopenres.17530.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 2006;21:459–68. 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 30.Razai MS, Oakeshott P, Esmail A, et al. COVID-19 vaccine hesitancy: the five CS to tackle behavioural and Sociodemographic factors. J R Soc Med 2021;114:295–8. 10.1177/01410768211018951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tembo M, Mackworth-Young C, Kranzer K, et al. Youth researchers Academy: a report on an innovative research training programme for young people in Zimbabwe. BMJ Innov 2022;8:183–9. 10.1136/bmjinnov-2021-000885 [DOI] [Google Scholar]
- 32.Our world in data . Coronavirus (COVID-19) Vaccinations. 2022. Available: https://ourworldindata.org/covid-vaccinations
- 33.Cutts FT, Claquin P, Danovaro-Holliday MC, et al. Reply to comments on monitoring vaccination coverage: defining the role of surveys. Vaccine 2016;34:6112–3. 10.1016/j.vaccine.2016.09.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jensen A, Stromme M, Moyassari S, et al. COVID-19 vaccines: considering sex differences in efficacy and safety. Contemp Clin Trials 2022;115:S1551-7144(22)00026-X. 10.1016/j.cct.2022.106700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zintel S, Flock C, Arbogast AL, et al. Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis. Z Gesundh Wiss 2022:1–25. 10.1007/s10389-021-01677-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Afrifa-Anane GF, Larbi RT, Addo B, et al. Facilitators and barriers to COVID-19 vaccine uptake among women in two regions of Ghana: A qualitative study. PLoS One 2022;17:e0272876. 10.1371/journal.pone.0272876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borga LG, Clark AE, D’Ambrosio C, et al. Characteristics associated with COVID-19 vaccine hesitancy. Sci Rep 2022;12:12435. 10.1038/s41598-022-16572-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dabla-Norris E, Khan H, Lima F, et al. Who doesn’t want to be vaccinated? determinants of vaccine hesitancy during covid-19. SSRN Journal 2021. 10.2139/ssrn.4026306 [DOI] [Google Scholar]
- 39.World Health Organization . The Sinopharm COVID-19 vaccine: What you need to know. 2021. [Google Scholar]
- 40.Srivastava KC, Shrivastava D, Chhabra KG, et al. n.d. Facade of media and social media during COVID-19: A review. Ijrps;11:142–9. 10.26452/ijrps.v11iSPL1.2288 [DOI] [Google Scholar]
- 41.Rocha YM, de Moura GA, Desidério GA, et al. The impact of fake news on social media and its influence on health during the COVID-19 pandemic: a systematic review. Z Gesundh Wiss 2021:1–10. 10.1007/s10389-021-01658-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CRUX . Did French Virologist Luc Montagnier actually say vaccination will kill us & create more variants. 2021. Available: https://www.youtube.com/watch?v=wkZKRNDo5Ks
- 43.Humer E, Jesser A, Plener PL, et al. Education level and COVID-19 vaccination willingness in adolescents. Eur Child Adolesc Psychiatry 2023;32:537–9. 10.1007/s00787-021-01878-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shifa M, Gordon D, Leibbrandt M, et al. Socioeconomic-related inequalities in COVID-19 vulnerability in South Africa. Int J Environ Res Public Health 2022;19:10480. 10.3390/ijerph191710480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Razai MS, Chaudhry UAR, Doerholt K, et al. Covid-19 vaccination hesitancy. BMJ 2021;373:1138. 10.1136/bmj.n1138 [DOI] [PubMed] [Google Scholar]
- 46.Wright L, Steptoe A, Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of Lockdown in the UK. J Epidemiol Community Health 2020;74:683–8. 10.1136/jech-2020-214475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Machekanyanga Z, Ndiaye S, Gerede R, et al. Qualitative assessment of vaccination hesitancy among members of the apostolic church of Zimbabwe: A case study. J Relig Health 2017;56:1683–91. 10.1007/s10943-017-0428-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kholwani Nyathi (UNICEF) . Zimbabwe: experts advocate for Covid booster jab. 2021. Available: https://www.unicef.org/zimbabwe/stories/religious-groups-warm-covid-19-vaccines-zimbabwe
- 49.Maiden James (UNICEF) . Zimbabwe’s religious leaders increase efforts to tackle COVID-19 and support vaccines. 2021. Available: https://www.unicef.org/zimbabwe/press-releases/zimbabwes-religious-leaders-increase-efforts-tackle-covid-19-and-support-vaccines
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-012268supp001.pdf (118.8KB, pdf)
Data Availability Statement
Data are available on reasonable request. The data will be made available on LSHTM Data Compass within 12 months of publication.