Abstract
Objectives: Fire in the operating theater is a potential source of important morbidity for the patient. Laser surgery of the head and neck district presents a particularly high risk of fire due to the presence of all three elements of the ‘fire triad,’ necessary to cause combustive or explosive events: an oxidiser, a fuel, and a heat source. The aim of the present study is to emphasise the need of new prevention tools and greater adherence to the recommendations available in the literature.
Methods: The sudden occurrence of combustion within the airway of an infant undergoing laryngeal laser surgery was presented along with his management.
Results: An infant underwent CO2 laser surgery for the treatment of the laryngeal stenosis. Unfortunately, the endoscopic procedure was complicated by a fire of the tracheal tube. The tube was immediately removed, the saline was flushed down the trachea and the ventilation was maintained through a face mask. Subsequently, a fiberoscopy was performed and showed a vocal cord burn.
Conclusions: Since operating room fires are still an underreported occurrence, we believe that this present work might raise awareness about this potential complication and give useful suggestions for the management of airway fires in paediatric anaesthesia.
Keywords: Airway fire, perioperative complications, paediatric anaesthesia, laser surgery, airways management, safety
Introduction
Fire during laser airway surgery is rare but a serious complication with an estimated incidence between 0.4 and 0.57%.1 The fire occurs when the three components of the ‘fire triad’ (an oxidiser, an ignition source and a fuel) coexist.2 Even more, laser can act as an ignition source on its own, and it is extremely important to know due to its extensive use in ear, nose, and throat (ENT) surgery.3,4 In fact, the three elements of the fire triad are often in close proximity during an ENT surgery.5
Safety precautions to prevent fire in this setting are represented by the reduction of laser output (lowest clinically acceptable power intensity), the administration of the lowest possible fraction of inspired oxygen (FiO2), the usage of a laser resistant endotracheal tube (ET), or to opt for alterative techniques (jet ventilation JV) and intermittent apneic technique).6,7 However, it is not always possible to use laser resistant tubes or to choose for non-conventional ventilation, especially in paediatric patients. We reported the case of fire breakout in the airway during laser surgery.
Case Report
A 6-month-old infant (weighing 6 kg), born preterm at 31 weeks of gestation, developed laryngeal stenosis due to vocal cord granulomas after repeated and prolonged intubations during his paediatric intensive care unit (PICU) stay. He was scheduled for a carbon dioxide (CO2) laser surgery for the treatment of the laryngeal stenosis.
Anaesthesia was induced using increasing concentrations of sevoflurane. Baseline saturation of peripheral oxygen (SpO2), non-invasive blood pressure, and heart rate were 97%, 85/48 mmHg, and 128 beats min−1, respectively. A 24-G venous access was placed, and fentanyl (1 mcg kg−1) was administered, followed by dexamethasone at a dose of 0.3 mg kg−1 and propofol continuous infusion using a target plasma drug concentration (Cpt) 3-4 mcg mL−1. For the ventilation management, an uncuffed Portex® tube of 3.5 mm was positioned in the pharynx through the nasal cavity (Figure 1), and a pressure control ventilation was initiated (inspiratory pressure 15-20 cmH2O, positive-end expiratory pressure 5-6 cmH2O, and air-oxygen mixtures with FiO2 0.3-0.4 in order to keep SpO2 > 92%). The patient was placed for suspension microlaryngoscopy (Figure 2), but the ventilation proved to be ineffective (SpO2 < 85%), and the tracheal intubation was necessary; the patient underwent nasotracheal intubation with an uncuffed ET Portex® tube of 3.5 mm (outer diameter 5.1 mm). We could not use a laser-proof tube because of its excessive size (the outer diameter of a 3.5 mm tube is 5.7 mm), which did not allow positioning; a further try with a laser safe ET with an internal diameter of 3.0 mm (external diameter 5.2 mm) did not allow adequate ventilation. Anaesthesia was maintained with propofol target controlled infusion (Cpt 4 mcg mL−1) and remifentanil (0.25 mcg kg−1 min−1). Mechanical ventilation was started with unchanged ventilation parameters.
Figure 1.
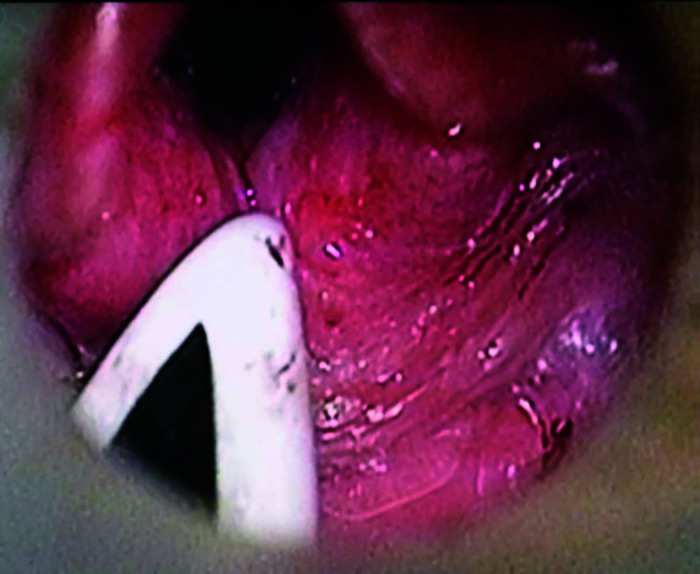
Positioning of the nasopharyngeal tube.
Figure 2.
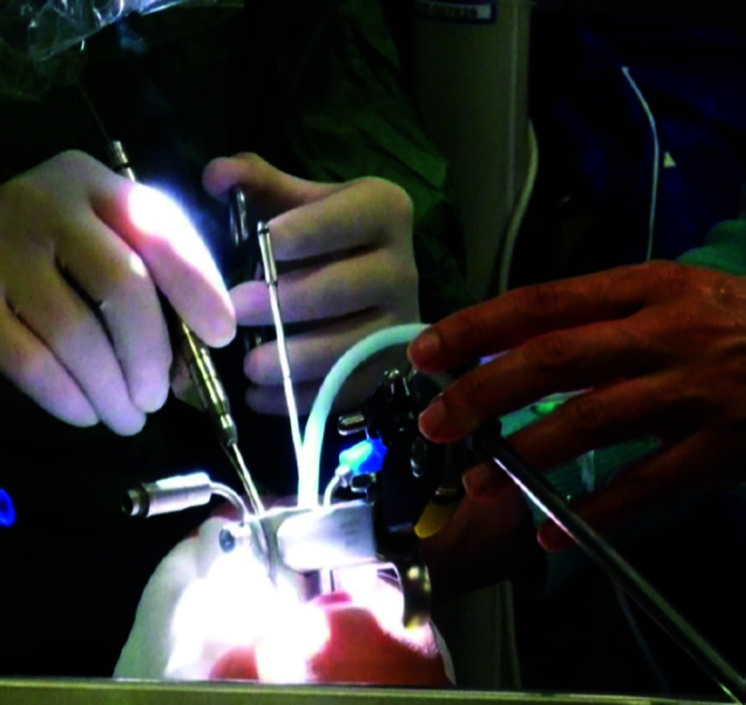
Positioning of the patient in laryngoscopy and beginning of the laser procedure.
During cauterisation of vocal cords granulomas, the ET was ignited by the laser beam (Figure 3). The operation was immediately suspended, the tube was removed, and a bolus of 5 mL saline was flushed through the airpipe, followed after by another saline bolus. Oxygen administration was discontinued, and the ventilation was maintained with room air through face mask. SpO2 and respiratory exchanges are always kept to the limits of the norm with modest oxygen saturation values (SpO2 90-92%). Once stabilised, the airway was examined with fiberoscopy and showed a left vocal cord burn. During the subsequent PICU stay, the patient did not present respiratory distress and did not need any further treatment. Serial fiberoscopy examinations showed a gradual and complete healing of the cord injury in 7 days. The last fiberoptic checkup was performed 30 days after the event, and no complications were observed with complete healing.
Figure 3.
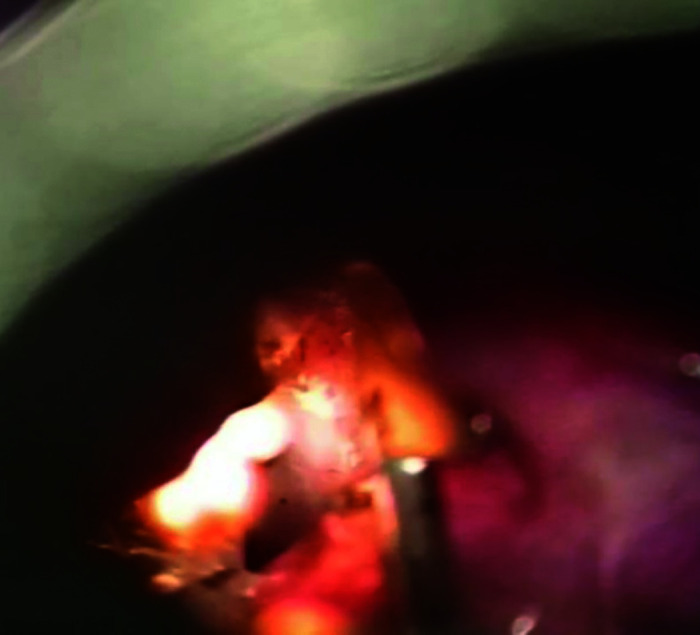
Fire of the tracheal tube of the airways.
Discussion
Operating room (OR) fires can be a cause of devastating complications for the patient. The American Society of Anaesthesiologists developed recommendations to promote safe practice and reduce burn injuries.2 These guidelines stressed the importance to follow an operating fire algorithm that consists in few but fundamental step, reducing the closeness between ignition sources and oxidiser-enriched atmosphere, recognising high-risk procedure, and early identification of warning signs of fire. In case of fire, the aforementioned algorithm identifies two different situations: airway fire and non-airway fire.
For laser surgery, laser safe ET has to be utilised.1 , 8 Wrapping of the ET with aluminum foil tape has been suggested and is a method to prevent ignition of the tube during laser procedures.9 However, this modified ET may be a cause of further complications itself.10 It is commonly believed that the choice of a stainless ET is the safest option during laser surgery.11 However, in paediatric patients, these tubes are often difficult to place, can be traumatic, oppose high resistance to the flow of ventilation, may be of inadequate size for younger children, and occupy the surgical field obstructing some types of procedure.12 The JV represents an alternative technique to conventional ventilation that allows an excellent surgical condition. However, JV does not provide definitive airway protection.13 The JV consists in delivering of oxygen trough high pressure ventilator; gas is intermittently administered by an injector with a high frequency and exhalation occurs passively. During JV, monitoring gas exchange and mechanics of ventilation could be difficult. Furthermore, severe tracheal stenosis, risk of bleeding during the procedure, risk for aspiration, and exacerbation of lung diseases are contraindications for JV. Intermittent apneic and insufflation techniques are other alternative options during laser surgery; however, all these methods require specific training and show particular challenge in communication between the medical personal in the OR.8 Unfortunately, in our case, we could not use a safe laser tube because its external diameter was not adequate for our patient, making its insertion impossible. Postponement of surgery to an older age of the patient was not an option, given the dimension of the granulomas, responsible of obstruction of the upper airway. For all these technical reasons and for the particular challenge related to the patient characteristics, we decided to perform conventional ventilation.
Conclusion
The purpose of this report is to raise awareness on the high risk posed by laser surgery in the ENT district and emphasise the need of new prevention tools and greater adherence to the recommendations. Unfortunately, it is not always possible to accurately comply with the recommendations due to the size or characteristics of the routinely available devices. Even more, it is not possible to completely remova the fire triad in an environment like the OR. It is also advisable for laser interventions in children to be performed only in centers with great experience with these procedures in paediatric age.
Footnotes
Informed Consent: A written informed consent was obtained from the patient’s parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.S., R.A.; Design - A.S.,E.B., R.A.; Supervision - A.S., R.A.; Resource - A.S., E.B., O.M., I.P., G.M., G.C., R.A.; Materials - A.S., E.B., O.M., I.P., G.M., G.C., R.A.; Data Collection and/or Processing - A.S., E.B., O.M., I.P., G.M., G.C., R.A.; Analysis and/or Interpretation - A.S., E.B., O.M., I.P., G.M., G.C., R.A.; Literature Search - A.S., E.B., R.A.; Writing - A.S., E.B., O.M., I.P., G.M., G.C., R.A.; Critical Reviews - A.S., E.B., R.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1. Burgess GE, III,, LeJeune FE., Jr. Endotracheal tube ignition during laser surgery of the larynx. Arch Otolaryngol. 1979;105:(10):561‐562. 10.1001/archotol.1979.00790210059013 [DOI] [PubMed] [Google Scholar]
- 2. Apfelbaum JL, Caplan RA, Barker SJ.et al. Practice advisory for the prevention and management of operating room fires: An updated report by the American Society of Anesthesiologists task force on operating room fires. Anesthesiology. 2013;118:271‐290. 10.1097/ALN.0b013e31827773d2 [DOI] [PubMed] [Google Scholar]
- 3. Ossoff RH. Laser safety in otolaryngology–head and neck surgery: Anesthetic and educational considerations for laryngeal surgery. Laryngoscope. 1989;99:1‐26. [PubMed] [Google Scholar]
- 4. Arnold JE, Allphin AL. Effect of extraluminal oxygen on carbon dioxide laser ignition of endotracheal tubes. Arch Otolaryngol Head Neck Surg. 1992;118:(7):722‐724. 10.1001/archotol.1992.01880070052010 [DOI] [PubMed] [Google Scholar]
- 5. Roy S, Smith LP. Preventing and managing operating room fires in otolaryngology. Otolaryngol Clin North Am. 2019;52:(1):163‐171. 10.1016/j.otc.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 6. Haas CF, Eakin RM, Konkle MA, Blank R. Endotracheal tubes: Old and new. Respir Care. 2014;59:(6):933‐52; discussion 52-5. 10.4187/respcare.02868 [DOI] [PubMed] [Google Scholar]
- 7. Weisberger EC, Miner JD. Apneic anesthesia for improved endoscopic removal of laryngeal papillomata. Laryngoscope. 1988;98:(7):693‐697. [DOI] [PubMed] [Google Scholar]
- 8. Roy S, Smith LP. Prevention of airway fires: Testing the safety of endotracheal tubes and surgical devices in a mechanical model. Am J Otolaryngol. 2015;36:(1):63‐66. 10.1016/j.amjoto.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 9. Walker P, Temperley A, Thelfo S, Hazelgrove A. Avoidance of laser ignition of endotracheal tubes by wrapping in aluminium foil tape. Anesth Intensive Care. 2004;32:(1):108‐112. 10.1177/0310057X0403200118 [DOI] [PubMed] [Google Scholar]
- 10. Soong WJ, Lee YS, Soong YH.et al. Tracheal foreign body after laser supraglottoplasty: A hidden but risky complication of an aluminum foil tape-wrapped endotracheal tube. Int J Pediatr Otorhinolaryngol. 2010;74:(12):1432‐1434. 10.1016/j.ijporl.2010.08.019 [DOI] [PubMed] [Google Scholar]
- 11. Fried MP, Mallampati SR, Liu FC, Kaplan S, Caminear DS, Samonte BR. Laser resistant stainless steel endotracheal tube: Experimental and clinical evaluation. Lasers Surg Med. 1991;11:(3):301‐306. 10.1002/lsm.1900110315 [DOI] [PubMed] [Google Scholar]
- 12. Best C. Anesthesia for laser surgery of the airway in children. Paediatr Anesth. 2009;19:(Suppl. 1):155‐165. 10.1111/j.1460-9592.2009.03015.x [DOI] [PubMed] [Google Scholar]
- 13. Rosal Martins M, Van Boven M, Schmitz S, Hamoir M, Veyckemans F. Technical description of a modified jet ventilation injector for airway laser surgery in neonates and infants: Retrospective analysis of 20 cases. J Clin Anesth. 2016;32:142‐147. 10.1016/j.jclinane.2016.01.031 [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a