Abstract
Background
Primary healthcare (PHC) integration has been promoted globally as a tool for health sector reform and universal health coverage (UHC), especially in low‐resource settings. However, for a range of reasons, implementation and impact remain variable. PHC integration, at its simplest, can be considered a way of delivering PHC services together that sometimes have been delivered as a series of separate or 'vertical' health programmes. Healthcare workers are known to shape the success of implementing reform interventions. Understanding healthcare worker perceptions and experiences of PHC integration can therefore provide insights into the role healthcare workers play in shaping implementation efforts and the impact of PHC integration. However, the heterogeneity of the evidence base complicates our understanding of their role in shaping the implementation, delivery, and impact of PHC integration, and the role of contextual factors influencing their responses.
Objectives
To map the qualitative literature on healthcare workers' perceptions and experiences of PHC integration to characterise the evidence base, with a view to better inform future syntheses on the topic.
Search methods
We used standard, extensive Cochrane search methods. The latest search date was 28 July 2020. We did not search for grey literature due to the many published records identified.
Selection criteria
We included studies with qualitative and mixed methods designs that reported on healthcare worker perceptions and experiences of PHC integration from any country. We excluded settings other than PHC and community‐based health care, participants other than healthcare workers, and interventions broader than healthcare services. We used translation support from colleagues and Google Translate software to screen non‐English records. Where translation was not feasible we categorised these records as studies awaiting classification.
Data collection and analysis
For data extraction, we used a customised data extraction form containing items developed using inductive and deductive approaches. We performed independent extraction in duplicate for a sample on 10% of studies allowed for sufficient agreement to be reached between review authors. We analysed extracted data quantitatively by counting the number of studies per indicator and converting these into proportions with additional qualitative descriptive information. Indicators included descriptions of study methods, country setting, intervention type, scope and strategies, implementing healthcare workers, and client target population.
Main results
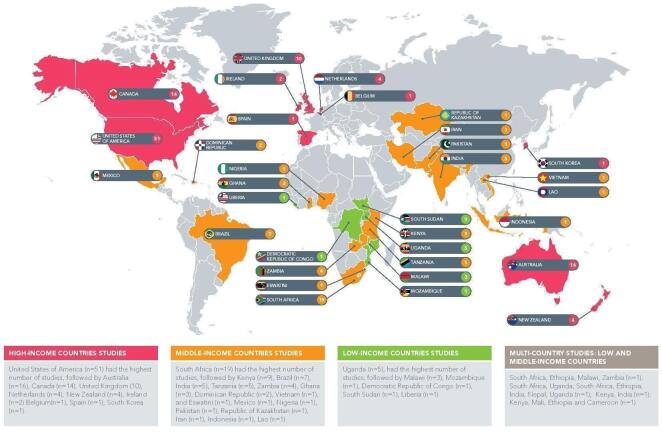
The review included 184 studies for analysis based on 191 included papers. Most studies were published in the last 12 years, with a sharp increase in the last five years. Studies mostly employed methods with cross‐sectional qualitative design (mainly interviews and focus group discussions), and few used longitudinal or ethnographic (or both) designs. Studies covered 37 countries, with close to an even split in the proportions of high‐income countries (HICs) and low‐ and middle‐income countries (LMICs). There were gaps in the geographical spread for both HICs and LMICs and some countries were more dominant, such as the USA for HICs, South Africa for middle‐income countries, and Uganda for low‐income countries. Methods were mainly cross‐sectional observational studies with few longitudinal studies. A minority of studies used an analytical conceptual model to guide the design, implementation, and evaluation of the integration study.
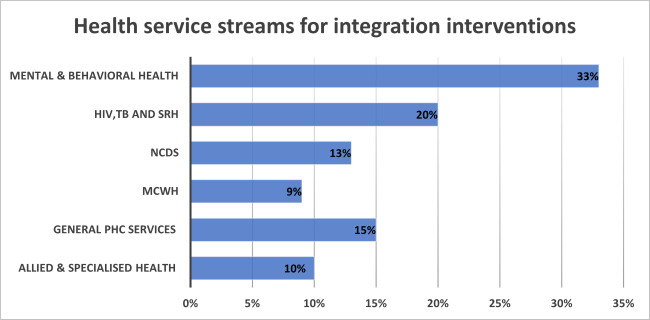
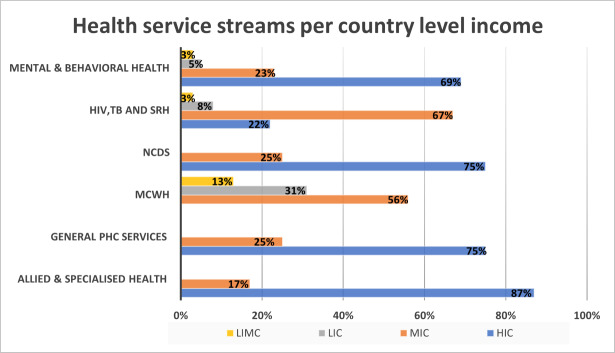
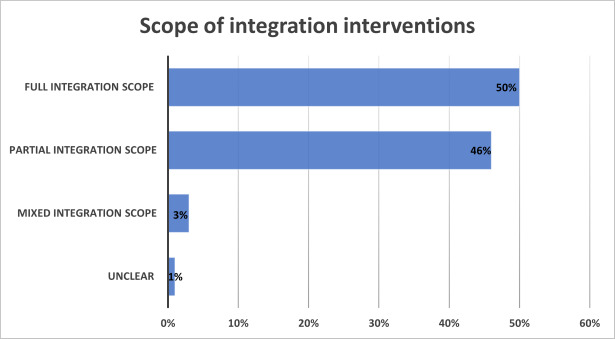
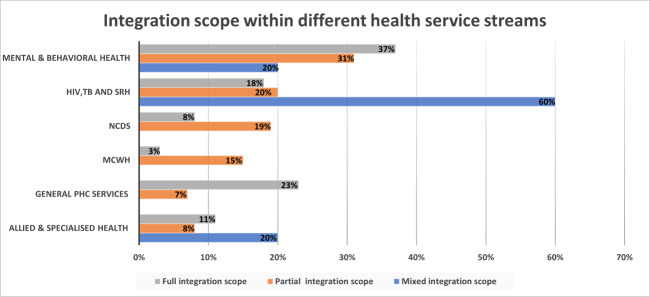
The main finding was the various levels of diversity found in the evidence base on PHC integration studies that examined healthcare workers' perceptions and experiences. The review identified six different configurations of health service streams that were being integrated and these were categorised as: mental and behavioural health; HIV, tuberculosis (TB) and sexual reproductive health; maternal, women, and child health; non‐communicable diseases; and two broader categories, namely general PHC services, and allied and specialised services. Within the health streams, the review mapped the scope of the interventions as full or partial integration. The review mapped the use of three different integration strategies and categorised these as horizontal integration, service expansion, and service linkage strategies. The wide range of healthcare workers who participated in the implementation of integration interventions was mapped and these included policymakers, senior managers, middle and frontline managers, clinicians, allied healthcare professionals, lay healthcare workers, and health system support staff. We mapped the range of client target populations.
Authors' conclusions
This scoping review provides a systematic, descriptive overview of the heterogeneity in qualitative literature on healthcare workers' perceptions and experience of PHC integration, pointing to diversity with regard to country settings; study types; client populations; healthcare worker populations; and intervention focus, scope, and strategies. It would be important for researchers and decision‐makers to understand how the diversity in PHC integration intervention design, implementation, and context may influence how healthcare workers shape PHC integration impact. The classification of studies on the various dimensions (e.g. integration focus, scope, strategy, and type of healthcare workers and client populations) can help researchers to navigate the way the literature varies and for specifying potential questions for future qualitative evidence syntheses.
Plain language summary
Healthcare workers' perceptions and experiences of primary healthcare integration: a scoping review of qualitative evidence
What is primary healthcare integration?
Primary healthcare integration is a way of combining different primary healthcare services that have previously been delivered separately. The aim of this integration is usually to give people better access to healthcare and to make more efficient use of limited health resources.
Why is it important to know about healthcare workers' views and experiences?
Primary healthcare integration has been implemented in many different countries with varying success. Healthcare workers can influence the extent to which such changes in health services are implemented successfully. Learning about healthcare workers' views and experiences of primary healthcare integration can help us understand how healthcare workers might influence its implementation and its success or failure.
What was the purpose of this scoping review?
This scoping review searched for and mapped qualitative studies (studies with no numerical data) about healthcare workers' views and experiences of primary healthcare integration. We wanted to describe the available research to help inform future systematic reviews and research studies in this area.
How did we identify and map the evidence?
We searched for all published qualitative studies that reported on healthcare workers' views and experiences of primary healthcare integration up to 28 July 2020. We described the different study methods, countries, the scope and type of primary healthcare integration approaches, and the different types of healthcare workers and client groups involved. We then grouped the studies into categories.
What did we find?
We included 184 studies. The studies were from 37 countries. About half the studies took place in high‐income countries and half in low‐ and middle‐income countries.
The studies we found in our review covered a variety of settings, participants, and types of primary healthcare integration. There were different configurations for which healthcare service programmes were being combined for integrated service delivery. These were categorised into the following six configurations: mental health; HIV, tuberculosis, and sexual reproductive health; maternal, woman, and child health; non‐communicable diseases (for example, heart disease, diabetes); general primary health integration, and allied and specialised services. We also explored whether integrated service delivery was fully or partially integrated, and the different integration strategies used to link and co‐ordinate services.
The people participating in the implementation of integration interventions included policymakers, senior managers, middle and frontline managers, clinicians, allied healthcare professionals, lay health workers, and health system support staff. A wide range of clients were recipients of the integrated services.
Author's conclusions
This scoping review shows the variety of primary healthcare integration approaches that have been studied. Researchers and decision‐makers need to understand the relationship between different integration approaches and contexts, and the ways in which healthcare workers influence the impacts of this integration. The study categories we have developed can help researchers to understand these different types of integration approaches and to identify more focused questions for future systematic reviews.
Background
Efforts to promote delivery of integrated health services and systems at the primary healthcare (PHC) level have existed since the late 1970s. PHC was centrally embedded within the Alma Ata Declaration of 1978 as a mechanism for achieving health for all by 2000 (WHO 1987). Integration of PHC services (or PHC integration), at its simplest, can be considered "a way of delivering a series of targeted technologies and interventions together that sometimes have been delivered as a series of 'vertical' programmes" (Dudley 2011). PHC integration is considered one way to provide efficient and high‐quality services that are potentially cost‐effective, and that can lead to accessible and equitable healthcare for people most in need (Foreit 2002; Oleribe 2015).
PHC integration has been promoted globally as a tool for health sector reform that can promote universal health coverage (UHC), especially in low‐resource settings (Walley 2008). There is a renewed focus on PHC integration; first, the Millennium Development Goals (MDGs) and now the Sustainable Development Goals (SDGs) recognise that PHC integration is a vehicle for the delivery of comprehensive PHC services and UHC more broadly (Oleribe 2015). In its support to countries, the World Health Organization (WHO) has kept integration as a core mechanism for achieving UHC, through its approach of integrated People‐Centred Care (WHO 2013). More recently, this has been expressed in the Astana Declaration of 2018, emanating from the Global Conference on Primary Health Care (WHO 2018). However, despite the persistence of the concept of PHC integration as a mechanism, implementation has been slow and uneven, and the anticipated substantial, demonstrable, positive impact on universal access to quality healthcare has not been realised (Chuah 2017; Dudley 2011; Haldane 2017; Haldane 2018). Instead, research has shown variable and inconclusive impacts on service utilisation and disease outcomes (Baxter 2018a; Chuah 2017; Haldane 2017; Haldane 2018). Contributing factors have been shown to include political commitment, logistics, the burden of disease, health systems fragmentation, and financing arrangements (Hall 2003; Mounier‐Jack 2017; Schierhout 1999; Walley 2008).
The lack of a single, standard agreed‐upon definition and different approaches on how to achieve integration at a primary level may also be contributing to the variable impact of PHC integration implementation (Armitage 2009). Despite the tenaciousness of the thinking that integration is needed, there remains little coherence around what PHC integration is. This is evidenced in the plethora of definitions found across research studies and programme reports (Armitage 2009; Valentijn 2015). In practice, many governments, bilateral agencies, and non‐governmental organisations have attempted some form of PHC integration, but all using their own understanding, and even then, without necessarily having a shared understanding within their approaches. Yet, within this definitional morass, it is healthcare workers who are charged with the task of implementing integration and ensuring successful PHC coverage and UHC for all. Street‐level bureaucracy theory helps to show that healthcare workers determine interventions, arguing that what clients (or patients) and communities receive is based on healthcare workers' understanding of their task and shaped by their discretionary power in delivering the task (Erasmus 2011). To achieve the visions of the Alma Ata and Astana declarations, it would therefore be useful to better understand how integration is being operationalised by healthcare workers in PHC. To do so, it is essential that we first understand how healthcare workers perceive the meaning of PHC integration and how they experience the practice of integration in PHC.
We attempted to perform a qualitative evidence synthesis (QES) of healthcare workers' perceptions and experiences of PHC integration (Moloi 2020). However, as with the plethora of definitions found, the available evidence was plentiful and widely heterogeneous. An adequate synthesis would have required a reduction of the material through sampling. Still, such sampling seemed too soon, as we had not fully been able to get a clear understanding of the diversity of the available evidence. Therefore, we changed our approach, beginning with a scoping of what studies have been conducted on healthcare workers' perceptions and experiences of PHC integration, in the hope that this, at a further date, may inform comprehensive and meaningful QES.
Description of the topic
Typically, within health systems, senior members of the system, such as policymakers and senior managers, will decide on what interventions to implement and will decide on the form of these interventions (Buse 2012; Hudson 2009). Yet, it is healthcare workers who are tasked with implementing these interventions, including primary care reform and integration. Healthcare workers are the face of health delivery throughout the world. As such, healthcare workers can and do shape how policy options are delivered, especially when working in challenging contexts in the public sector (e.g. chronic shortages, multiple demands, poor performance management) (Erasmus 2011). Healthcare workers may exercise their discretionary power as 'street‐level bureaucrats', to act in support of the policy or not, to decide which services are offered, how services are offered, and the benefits and sanctions allocated to citizens who are seeking the services (Erasmus 2008; Gilson 2015; Walker 2004). Therefore, a premise of this scoping review is that healthcare workers may shape how integration is delivered or implemented in PHC.
For the purpose of this review, we considered PHC integration as a set of interventions aimed at strengthening co‐ordination and linkages in the organisation, management and delivery of health services and systems, for improved access to comprehensive, effective, and efficient healthcare. Integration can allow clients access to comprehensive multidisciplinary services attuned to their needs; clients may receive multiple services during a single visit, either from a single healthcare worker or different healthcare workers and health services (Msuya 2004; Walley 2008).
In some settings, PHC services are sometimes delivered as separate, stand‐alone, or specialised services, often referred to as vertical health programmes. Vertical programmes are commonly implemented to ensure good access to priority health programmes, good coverage of these priority health services, and efficient monitoring and quality improvement systems (Atun 2008). Potential problems of vertical programmes include fragmentation and duplication of service delivery, inconvenience and inefficiencies for both clients and staff, and potentially a lack of effective coverage of comprehensive PHC needs of the population (Sundaram 2017). PHC integration attempts to address the access and efficiency problems associated with vertical services by reducing service fragmentation and promoting access to comprehensive care delivery options. This is sometimes referred to as horizontal integration to show the contrast with the siloed approach of vertical integration (Kumar 2016; Msuya 2004; Oleribe 2015; Walley 2008).
Approaches to integration lie on a continuum in terms of scope, from delivering more comprehensive clinical services at the point of care during a single visit to the integration of and across health system functions such as leadership and management functions, financial systems, human resource management, information systems, and equipment and drug supply systems. Integrated services may be delivered to different levels of integration of clinical and support services (full or partially integrated functions and levels), to enable the delivery of integrated clinical care and integrated health service systems. For example, the integration of preventive health screening services, together with the delivery of disease treatment services, may require not only the joint delivery of screening tests and medical treatment in one consultation, but may also require changes to human resources (who does what), drug supply systems (to provide the screening tests), and information systems (to allow for documentation of the integrated service) (WHO 2016). One example is the shift from vertical, stand‐alone delivery of priority disease programmes (such as HIV and tuberculosis (TB) services) to a more unified, integrated (horizontal) delivery of two or more disease programmes (such as integrating various elements of HIV and TB services for joint delivery at the point of care) (Kumar 2016; Oleribe 2015; Walley 2008).
Why is it important to do this scoping synthesis?
The evidence base on implementation and evaluation of PHC integration is large and diverse, including studies on healthcare workers' perceptions and experiences of different types of PHC integration. Healthcare workers may be involved with the implementation of PHC integration along the full continuum (from policy formulation to service delivery), and in different roles, as senior‐level decision‐makers, managers, and frontline implementers. Frontline healthcare managers and staff are also recipients of integration interventions that are planned higher up in management. Integration may have different meanings in different settings based on geographic, social, political, cultural, and historical contexts (Armitage 2009; Baxter 2018b). The role of context may also shape the design, delivery and implementation perceptions and experiences of PHC integration (Armitage 2009; Ryman 2012a).
Diverse understandings of what PHC integration is, and the diverse forms it can take, may influence healthcare workers' perceptions, and shape their responses and implementation experiences. Examining the perceptions and experiences of healthcare workers can help understand how they shape the implementation and delivery of PHC integration, and how contextual factors influence their responses. However, the heterogeneity of the evidence base complicates our efforts at understanding. Premature synthesis across the heterogeneous literature may lead to premature conclusions and missed opportunities to understand contextual influences.
This scoping review maps the qualitative literature on healthcare workers' perceptions and experiences to characterise the evidence base, with a view to informing future evidence synthesis (Sutton 2019). The value of a scoping review prior to conducting further quantitative or QES is to identify and better understand heterogeneity in the evidence base. This can allow for more focussed research synthesis questions that take account of heterogeneity, as well as allow for more precise search terms or better sampling strategies.
Objectives
To map the qualitative literature on healthcare workers' perceptions and experiences of PHC integration to characterise the evidence base, with a view to better inform future syntheses on the topic.
To map the study characteristics in terms of the publication date and study design
To map the context of the studies in terms of geographical and service settings
-
To map the integration intervention characteristics in terms of the:
stakeholders (the client target population of the intervention and the healthcare workers who are the respondents in the study)
intervention components, including the health services that are being integrated, the scope of the integration intervention, and strategies used to deliver integrated services
To identify the conceptual models used in the studies
Review author reflexivity
Our review team have diverse backgrounds, which have likely shaped our contributions to the review. Our team consists of emerging and senior researchers in health policy and systems, public health, clinical research, and social sciences. As a team, we have skills in primary and secondary qualitative and quantitative research methods. Furthermore, four members of the review team have conducted and completed at least one full Cochrane QES study as lead or senior authors. All in our team have experience of research in low‐ and middle‐income countries (LMICs), and some team members have experience working for and with international health organisations, including the WHO. In the development of the QES protocol that preceded this scoping review (Moloi 2020), we included a public sector health policymaker and a mid‐level health service manager to help guide our thinking about information health authorities would find useful. This thinking also informed our approach to the scoping review.
This review team includes researchers based in South Africa and one review author from Kenya. The review question is of interest to the review team because both countries support different types of PHC integration. In South Africa, the National Department of Health has a record of health reforms that include PHC integration, especially for priority disease programmes such as HIV, TB, and mental health. In Kenya and South Africa, the delivery of PHC has often been characterised by successful priority health programmes that are delivered vertically (separately or in parallel to other PHC services), for example, immunisation, HIV prevention care and treatment, and most recently, the COVID‐19 response. However, to achieve UHC, Kenya and South Africa have embraced service integration within PHC to improve access to integrated PHC services.
Based on our collective and individual experiences and interests, both methodologically and in terms of content, we brought a richness of insights and a balance of views to conducting the review. The review authors are generally in agreement that PHC integration is potentially a useful tool for promoting UHC, while also being aware of the complexity of the intervention, and the importance of contextual influences. The team remained mindful of our presuppositions; we discussed these views, especially when faced with difficult judgements during the screening process. Through these discussions, we supported each other to minimise the risk of us skewing our analysis and interpretation of our findings. In the absence of standard definitions of PHC integration and related strategies, we often had to apply our judgement in categorising information for extraction. We consulted with each other and checked with a local policymaker (Tracey Naledi), to help us develop a common understanding of key areas.
Methods
Scoping reviews can be used to map a broad overview of the evidence on a topic, including identifying sources and types of evidence, clarifying key concepts and conceptual boundaries underpinning the topic area, and identifying gaps in evidence (Arksey 2005; Sutton 2019; Tricco 2016). The review objective is in line with that of scoping reviews, where the aim is 'to explore and define conceptual and logistic boundaries around a particular topic with a view to informing a future predetermined systematic review or primary research' (Sutton 2019). We used the 2020 JBI (formerly Joanna Briggs Institute) guide for scoping reviews (Peters 2015). Thus, for this scoping review, we include components such as the criteria for considering studies for this review, search methods for identification of studies, selection of studies, data extraction, management, and analysis. We describe these components in more detail below. There was no formal critical appraisal of the studies, as this is not required for scoping reviews (Tricco 2016). The review report is guided by the reporting format suggested in the PRISMA for Scoping Reviews extension (Page 2021; Tricco 2018).
Criteria for considering studies for this review
Criteria for inclusion
Studies
We included primary studies that used qualitative study designs such as observational, cross‐sectional, case, and process evaluations study.
We included mixed methods studies (quantitative and qualitative methods) where it was possible to extract the data that were collected and analysed using qualitative methods.
Participants
-
We included studies that reported healthcare workers' perceptions and experiences of PHC integration. We defined healthcare workers as:
clinical healthcare workers and lay healthcare workers (where the lay healthcare workers were classified as healthcare workers rather than volunteers), on both healthcare provision and management levels;
other individuals involved in supporting the provision and management of PHC integration interventions. These individuals could include administrative, managerial, supervisory staff, advisors, and policymakers.
Interventions
We included PHC integration interventions that had a focus on PHC‐level services, including community‐based services.
-
This could have included a range of integration‐type interventions such as:
horizontal integration of previously vertical programmes;
multidisciplinary teams working together to deliver more integrated care;
health systems functions combined (i.e. human resource and finance systems) to deliver more integrated management of disease programmes;
expansion of services towards more comprehensive care (e.g. adding a new service to an existing disease programme, such as screening for non‐communicable diseases (NCDs) in HIV/TB care). Or introducing a new PHC service that was previously delivered at a specialist level (e.g. such as PHC‐based follow‐up for cancer care clients that are now being delivered by general or specialised nurses in a PHC setting);
integration interventions that differ in scale and scope. These could be on a continuum from full to partial integration efforts. There are no standard definitions for full or partial integration. We made judgements based on the extent to which the intervention aimed to deliver integrated clinical services at the point of care, and the extent to which healthcare service support functions were integrated into support of that integrated clinical service. We also considered the extent to which the integrated service delivery was embedded in existing general PHC services, versus the need for additional, specialised staff to deliver integrated services at the PHC level. For full integration, for example, we considered the extent of integration of health service support functions, such as management, finances, human resources, information systems, and supply systems. Where a new service was devolved from the hospital for delivery at the PHC level, we considered the extent of efforts to embed the new service within existing generalised PHC staff skills and capacity, or whether a new or specialised cadre of healthcare workers was required to deliver the service at PHC level.
Settings
We defined PHC services as including all therapeutic, preventive, promotive, and rehabilitation services delivered at the first contact point of healthcare (Awofeso 2004), including at the level of PHC and community‐based healthcare (Muldoon 2006).
We included studies of PHC integration in public and private healthcare settings and public–private partnerships.
We included studies of PHC integration in any country and both rural and urban settings.
Criteria for exclusion
Studies
Hypothetical studies (planned, modelled, but not implemented and evaluated), for example, where there was a situational analysis or healthcare workers were asked about the feasibility of providing integrated services (planned, anticipated) in the absence of actual implementation of such integrated services.
We excluded studies that collected data using qualitative methods but did not analyse these data using qualitative analysis methods (e.g. open‐ended survey questions where the response data were analysed using descriptive statistics only).
Participants
We excluded studies that did not report on healthcare workers' perceptions and experiences of being involved in PHC integration or if it was not possible to separate the data on the views and experiences of healthcare workers from the views and experiences of other stakeholders.
Interventions
Transitional care between PHC and levels above (hospital, secondary), for example, a referral from PHC to secondary care or discharge from secondary care to PHC. This includes services around emergency care services where linkages are required between PHC and hospital care. Improved referral services could be considered part of designing integrated services, but given the additional layer of complexity around interorganisational linkages, we consider this warrants a separate review.
Integration of non‐health programmes with PHC health programmes. We excluded all programmes addressing social determinants of health (e.g. social services, social protection, nutrition, safety, housing, and legal help). We recognised that certain conditions related to social dynamics and social determinants require a non‐medical intervention, such as housing and employment. This may warrant a separate review.
Digital tools being evaluated in PHC, where the digital tool intervention was not the key element of facilitating the PHC integration intervention.
Training of health workers for PHC integration. We excluded evaluation of training for PHC integration unless it was also linked to evaluating the health workers' experience of implementing PHC integration.
'Care co‐ordination' strategies, where the core intervention was one person co‐ordinating care for a group of clients for a specific area (e.g. elder care). We recognise that care co‐ordination is a specific and widespread intervention strategy with its own set of variations, and feel this may warrant a separate review.
We excluded alternative medicine interventions. Alternative medicine refers to a broad set of practices that a country may not consider mainstream biomedical/clinical medicine and this includes traditional, faith healing, and Chinese medicine. We excluded these as they are not central to the focus of our review and may warrant a separate review.
Settings
Inpatient community‐based services, for example, drug rehabilitation centres, step‐down physical rehabilitation, and hospice centre for inpatient palliative care.
Non‐health delivery site, that is, integration occurring in schools, jails, retirement complexes/nursing homes, workplace health services, and home‐based care.
Search methods for identification of studies
The Effective Practice and Organisation of Care (EPOC) Information Specialist developed the search strategies for different databases in consultation with our scoping review team. To develop the search strategy, we used the PI (Phenomenon of Interest) and the R (Research type) from the SPIDER framework to develop the MEDLINE search strategy (www.nccmt.ca/knowlege-repositories/search/191). We did not use the S (Sample), as the scoping review included health workers (professionals and non‐professionals).
We did not apply geographic location limits and language limits, and we searched all databases from 1948 to the date the search was conducted. This date range was used to include health workers' experiences and perceptions since the Alma Ata declaration on PHC (WHO 1987). The search was completed on 15 February 2020 and reran to update the results on 28 July 2020. Appendix 1 shows the MEDLINE search strategy, which we adapted for other databases.
Electronic searches
We searched PDQ‐Evidence, Epistemonikos Foundation, for related reviews to identify eligible studies for inclusion (www.PDQ-evidence.org/), and the following electronic databases on 28 July 2020.
MEDLINE and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions 1946 to 24 July 2020, Ovid
CINAHL from 1981, EBSCOhost
Scopus Elsevier
Global Index Medicus, WHO
Grey literature
We found an extensive peer‐reviewed dataset from our database search. Thus, we did not conduct a grey literature search to identify studies not indexed in the databases. Also given a large number of records included, we did not screen the reference list of included studies to identify more records.
Selection of studies
Two review authors independently assessed the titles and abstracts of the identified records to evaluate eligibility, and a third review author resolved conflicts. We retrieved the full text of the titles and abstracts identified as potentially eligible. Two review authors independently assessed the full‐text articles, and a third review author resolved conflicts. All review authors participated in at least one online training and practice session (led by HM or NL, or both), prior to abstract and full‐text screening, to ensure a standard approach to screening.
Where multiple publications reported on the same intervention study, we collated these publications (and treated them as one data source), so that each unique intervention (rather than each publication/study) was the unit of interest for analysis.
We included a PRISMA flow diagram to show our search results and the process of screening and selecting studies for inclusion. Additionally, we included a table of excluded studies with reasons for exclusion.
Translation of languages other than English
We considered all studies regardless of the language of publication. We found 17 non‐English studies: three in French, two in German, one in Japanese, one in Italian, eight in Portuguese, and two in Spanish.
We performed an initial translation through open‐source software (Google Translate) for all the titles and abstracts of studies not published in English. If Google translation was not sufficient to decide on inclusion or exclusion, we asked members of Cochrane networks, Social Science Approaches for Research and Engagement in Health Policy and Systems (SHAPES) networks, or other networks that are proficient in that language to assist us. We received translation assistance from six SHAPES network members.
From the translated studies, if this translation indicated inclusion, or if the translation was too limited to inform a decision, we retrieved the full text of the paper. We followed the same process for translating and screening the full text. For all studies included after the full‐text screening, we used Google Translate and also asked members of the SHAPES network proficient in that language to translate key information items needed for data extraction. If we could not do this for a study in a particular language, we listed the study as 'studies awaiting classification' to ensure transparency in the review process.
Data extraction
Two review authors (HM and NL) extracted data. We used a customised data extraction form with items for data extraction and sorting. We expanded the form with further subcategories based on emerging data. Table 1 shows items extracted and their subcategories. We used a combination of an inductive and deductive approach to data extraction and synthesis. We drew lightly on two frameworks to identify useful categories for data extraction. The SURE framework on implementation factors, guided us to identify data on key stakeholders, such as the providers and recipients of care, and the care setting (Sure Collaboration 2011). The Health Systems framework guided us to identify different health systems functions that were being integrated, such as human resources, information systems, and supply systems (van Olmen 2010). We also drew on various sources of taxonomies for integrated care to guide the categorisation of intervention type, scope, breadth, and strategies (Atun 2004; Kodner 2002; Valentijn 2015). Given the plethora of definitional sources, we adapted these a priori concepts on type, scope, and strategies as part of our deductive approach to data extraction. In places where there were no predefined definitional categories, we used an inductive approach based on emerging data, as in the case of identifying the health stream configurations.
1. Items extracted and their subcategories.
| 1. Study ID: author – publication, date, title, aim 2. Study methods: study design, data source 3. Setting: income level, country, urban/rural, healthcare level 4. Target client population to receive the intervention 5. Research participants 6. The intervention description: 6.1. Health service streams that were being integrated 6.2. The scope of the integration intervention (e.g. full or partial) 6.3. Intervention strategies used 7. Conceptual models used in the study |
For consistency between the review authors, HM and NL initially performed duplicate extraction on a sample of 10 studies (5%) and compared their data. The duplicate extraction process continued for another 10 studies (in total 10%) until there was sufficient agreement for single review author extraction. As an additional quality check, the senior author (NL) reviewed the data extraction of 40 studies (22% of the total sample) completed by HM.
Management and analysis
We imported and managed all the retrieved studies in Covidence (www.covidence.org). We screened and assessed the eligibility of all retrieved studies in Covidence.
After data extraction into our Excel template, we refined the extraction by providing drop‐down lists for subcategories for some of the indicators. For example, categorising country‐income levels, health stream interventions, and intervention scope and strategies. We then used the sorting function in Excel to present the information quantitatively by counting the number of studies per indicator and converting these into proportions. Where relevant, we provided additional qualitative descriptive information. Where appropriate, we disaggregated indicators per country income level. Below we provide details on how we analysed and categorised information for the indicators for research participants, intervention descriptions, and conceptual models.
Research participants
Studies listed a wide range of research participants who provided information on their perceptions and experiences of being involved in implementing integration interventions. We categorised these research participants as follows: policymakers and provincial managers, district managers, clinical managers, clinical healthcare workers, allied healthcare workers, lay healthcare workers, health systems support staff, civil society (i.e. community leaders and chiefs involved in clinic decisions) and health system advisors (researchers, programme managers, non‐governmental organisation (NGO) managers, technical advisors, and operational managers).
Intervention
Health service streams that were integrated
In the literature, we found no predefined, standardised PHC integration intervention categories to describe combinations of health programmes that were being integrated. We created categories based on emerging data. Six categories of health service stream configurations emerged from the analysis.
Mental and behavioural health services
HIV, TB, and sexual and reproductive health (SRH) services
Maternal, child, and women's health (MCWH) services
NCD services
General PHC services
Allied and specialised health services
Some interventions overlapped across the health service streams listed above, and we placed them in the stream where we thought they would fit best. For example, where a mental and behavioural health service was being integrated into an NCD service, we placed it in either the 'Mental and behavioural health service' or the 'NCD service' stream, depending on our assessment of the primary aim and direction of integration for joint service delivery. We used the category of 'General PHC services' for interventions that went beyond the integration of clinical components of health programmes, to focus more explicitly on the integration of cross‐cutting health system functions (such as the functions of management and administration, human resources, or health information systems), as well as integrated interventions that did not easily fit under the other categories. In 'Allied and specialised health services', we highlighted the introduction at the PHC level, of previously specialised services (such as dental services) and services delivered by allied health professionals (e.g. occupational therapists).
Scope of the integration
When we analysed the interventions included in this scoping review, we found a continuum in terms of the scope of health services (e.g. the number and extent of clinical tasks being integrated for joint delivery). There was also a continuum regarding the extent to which cross‐cutting (transversal) health system functions were integrated to enable joint delivery of care (e.g. financial systems, human resource management, information systems, and supply systems). Based on the analysis of the included studies, and drawing on concepts in the literature, we categorised interventions as having a full or partial integration scope, as described below.
Full integration scope
We defined this as the integrated delivery of two or more PHC service programmes previously delivered vertically or in silos (e.g. joint delivery of HIV and TB services), or where there is a substantial expansion of a health service for integrated delivery at PHC level. One example is devolving mental health services from specialised care level to the PHC level in a way that mental health is more fully integrated with the delivery of other PHC services. Another example is where multiple PHC service organisations co‐ordinate and interlink their service delivery for general PHC clients or for a specified target group, such as maternal and child health. For instance, this could be done through the colocation of health services within one facility.
Partial integration scope
This is where only one or a small component of a health service or clinical task is integrated or a limited number of clinical (e.g. disease screening for TB) to a different (main) health service (e.g. HIV treatment services). We refer to this as 'partial integration' to indicate that only a part of the health service (and not all the health service/clinical tasks for that disease programme) were delivered jointly. Another element is when the service is devolved from specialised services to PHC level but is not fully embedded for integrated delivery by general PHC staff. For instance, when specialised staff are employed at the PHC level to deliver a previously specialised service, such as mental health care.
In some studies, the integration scope represented a mix of full and partial integration efforts. The intervention descriptions were not always sufficiently detailed to make well‐informed judgements about its scope. Also, there are no standard definitions of full and partial integration. Therefore, we considered these tentative classifications to provide an initial map of the scope of integration interventions.
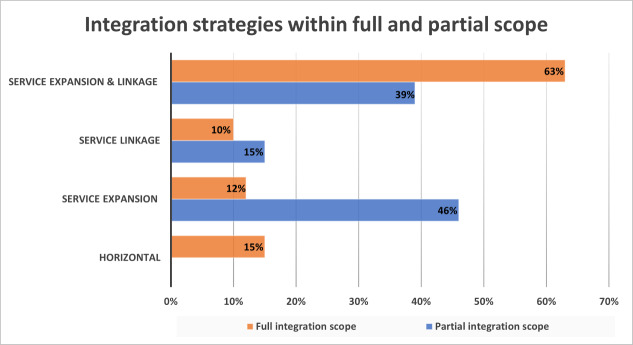
Intervention strategies used
Through an analysis of the included studies, we ascertained that within both full and partial integration, the interventions also differed in terms of the main strategies used for the delivery of integrated care. We did not find standardised categories of service strategies in the literature, so we categorised strategies based on data emerging from our analysis. Table 2 provides a list of the categories of integration strategies we identified.
2. Integration strategies within full and partial integration.
| Full integration |
| 1. Horizontal integration strategy |
| 2. Service expansion strategy |
| 3. Service linkage strategy |
| 4. Service expansion and linkage strategy |
| Partial integration |
| 1. Service expansion strategy |
| 2. Service linkage strategy |
| 3. Service expansion and linkage strategy |
We categorised integration interventions as 'service linkage' when the focus was on linkages between clinical staff in different health services. An example included liaison amongst healthcare workers, or amongst PHC service organisations, delivering different NCDs services, or between different PHC service platforms such as health facility‐based and community‐based service platforms. We categorised integration strategies as 'service expansion' when the focus was on expanding a component of one health service and adding it as standard care in another health programme (e.g. NCDs risk screening for HIV clients). Some integration interventions used a combination of service linkage and service expansion strategies. In full integration, we added a third strategy, named 'horizontal integration'. This is where two or more previously verticalised PHC health services were amalgamated for joint delivery into one health programme. For example, previously verticalised HIV and TB services were now being delivered jointly. The integration scope here is assumed to be wide and to include the integration of supportive health system functions (e.g. financing, human resources management, health information systems, and supply systems).
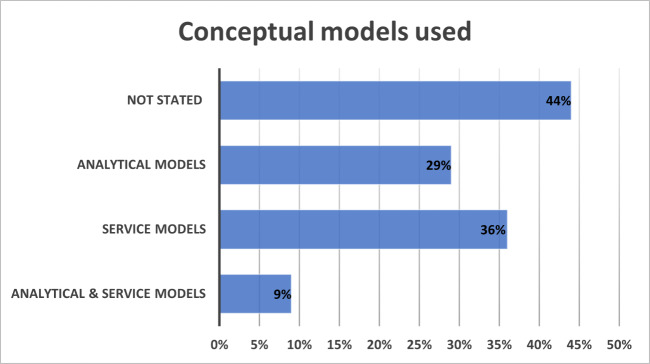
Conceptual frameworks used
We were interested in extracting data on whether an analytical, conceptual model was used to guide the study design, implementation, and evaluation. The assumption was that the use of analytical models in studies may potentially produce deeper conceptual or theoretical insights, as well as promote comparability between study findings. To extract data on analytical models, we used the 'Find' function in the PDF programme to search in the text of each study for the following keywords: 'conceptual', 'framework', 'model', and 'theoretical'. We found that these terms were sometimes used to describe not only analytical models but also for describing a particular model of the PHC integration intervention that was being implemented (e.g. the Chronic care model). We labelled the latter as 'service models' to indicate that it focused only on describing the integration intervention, and not on guiding the evaluation. Therefore, we reported on the use of both analytical and service models. Analytical models include named frameworks (e.g. integrated Promoting Action on Research Implementation in Health Services (i‐PARIHS) framework, and theories, such as Complexity theory).
On a different note, studies also sometimes used terms such as model, framework, or theory, to describe their methodological approach to qualitative data analysis (e.g. 'thematic framework' or grounded theory). We excluded these from our analysis as these are methodological approaches rather than models.
Summary of key characteristics of included studies
We presented a summary of the 'Key characteristics of included studies' in a table that combines study characteristics and key findings. We did not present our findings in the 'Summary of qualitative findings' table as these are scoping review findings that are presented as indicators, with supporting data tables. We did not conduct a critical appraisal of included studies. Scoping reviews do not typically analyse and appraise the data of included studies; rather they provide a map or detailed description of the scope of studies (Peters 2015).
The key items listed in our key characteristics table are author, publication date, study design, country income level, country name, target client population to receive the intervention, research participants, health service streams, scope of integration, and intervention strategies used.
Linking the synthesised qualitative findings to a Cochrane intervention review
The findings of this scoping review were not intended to be integrated with the Cochrane intervention review on PHC integration. Nevertheless, findings from the scoping review could inform future updates of the Cochrane integration effects review (Dudley 2011). Findings can also inform future quantitative and qualitative synthesis questions that take account of the heterogeneity of the evidence, and by informing more approaches to developing search terms and sampling strategies.
Results
Results of the search
We detailed the literature search results according to the PRISMA Statement. Figure 1 shows that we retrieved 10,084 records from searching the electronic databases. After removing duplicates, we assessed 9611 records for eligibility based on title and abstract. We assess the full texts of 723 records, and removed 523 records with reasons for exclusion. Due to many excluded studies, we presented a sample of 63 (12%) excluded studies with reasons in Table 3. We selected these studies by categorising all excluded studies alphabetically and then picked a sample of studies, from the topic of the alphabetical list, under each of the different exclusion criteria categories. The exclusion categories for the sample we describe were: ineligible study design (nine studies), ineligible intervention (18), hypothetical intervention (nine), ineligible outcome population (nine), ineligible setting (nine), and ineligible outcomes (nine).
1.
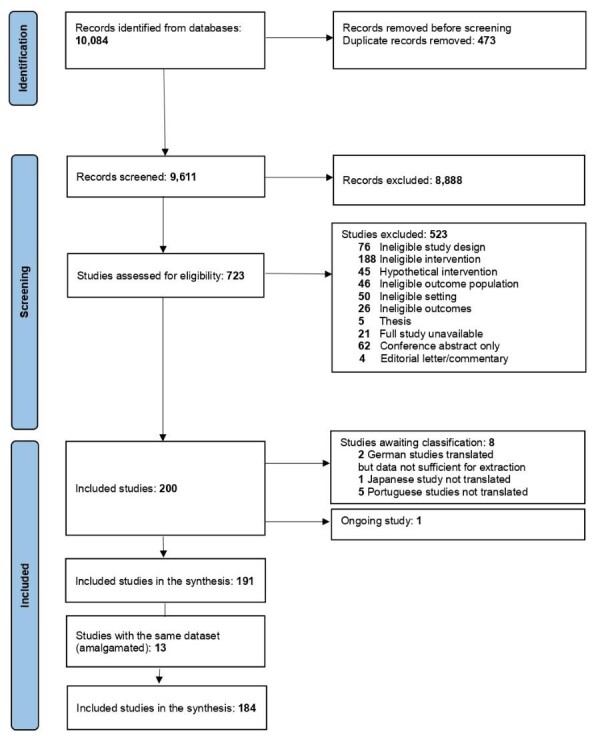
Figure 1: PRISMA flow diagram
3. Characteristics of excluded studies.
Thirteen publications had the same intervention found in at least one other publication. Publications with the same intervention were amalgamated, which resulted in six publications with unique intervention studies. Thus, 184 studies with a unique intervention, based on 191 papers, were analysed in this scoping review.
Eight studies are awaiting classification, and one study is ongoing.
Key characteristics of included studies
Table 4 provides a summary of the key characteristics of included studies. The table contains the following details: author and publication date, study design, country‐income level, country name, client target group, research participants, health service streams integrated, integration type/scope and integration strategy.
4. Key characteristics of included studies and key indicators.
| Author, publication date | Study design | Country income level | Country | Patient target group | Research participants | Health service streams integrated |
Integration type and scope (FI or PI) |
| Aantjes 2014 | Mixed methods | LMIC | Malawi, Zambia, South Africa, Ethiopia | General PHC and HIV patients |
|
HIV, TB, SRH | FI: service expansion and linkage |
| Acri 2018 | Qualitative | HIC | USA | Children 5–18 years old |
|
Mental and behavioural health | PI: service expansion |
| Aerts 2020 | Qualitative | HIC | Belgium | PHC patients with chronic disease |
|
NCDs | FI: service expansion and linkage |
| Aitken 2014 | Qualitative | HIC | Australia | General PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Akatukwasa 2019 | Qualitative | MIC | Uganda | Youth with SRH service needs |
|
HIV, TB, and SRH | FI: horizontal |
| Aleluia 2017 | Qualitative | MIC | Brazil | PHC patients with diabetes and hypertension |
|
NCDs | FI: service linkage |
| Allen 1997 | Mixed methods | HIC | New Zealand | Community members and patients in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Allen 2007 | Qualitative | HIC | Australia | Population who utilises acute and community health services |
|
PHC and other services | FI: service linkage |
| Allen 2015 | Mixed methods | HIC | USA | Community members with chronic disease needs community members with high care needs |
|
NCDs | PI: service expansion |
| Ameh 2017 | Qualitative | MIC | South Africa | People with chronic diseases |
|
NCDs | FI: service expansion and linkage |
| Amo‐Adjei 2014 | Qualitative | MIC | Ghana | People with TB |
|
HIV, TB, SRH | FI: horizontal |
| An 2015a; An 2015b | Mixed methods | MIC | Tanzania | Women attending antenatal care |
|
HIV, TB, and SRH | Mixed: FI + PI |
| Anand 2018 | Qualitative | MIC | India | People with TB |
|
NCDs | PI: service expansion |
| Anku 2020 | Qualitative | MIC | Ghana | People with TB or HIV, or both |
|
HIV, TB, and SRH | FI: horizontal |
| Athié 2016 | Mixed methods | MIC | Brazil | General PHC patients |
|
Mental and behavioural health | FI: service expansion and linkage |
| Ayon 2019 | Mixed methods | MIC | Kenya | Women who inject drugs |
|
Mental and behavioural health | PI: service expansion and linkage |
| Baker 2007 | Mixed methods | MIC | Dominican Republic | Lymphatic filariasis patients |
|
PHC, allied and specialised services | FI: service expansion |
| Baker 2018 | Qualitative | MIC | Tanzania | Patients accessing maternal and newborn services at PHC and hospitals |
|
MCWH | PI: service linkage |
| Banfield 2017 | Qualitative | HIC | Australia | PHC patients, especially patients at risk for NCDs, seeking care via the public‐private partnership |
|
NCDs | FI: service expansion and linkage |
| Beckingsale 2016 | Qualitative | HIC | New Zealand | People with chronic diseases |
|
PHC, allied and specialised services | PI: service expansion and linkage |
| Beehler 2017 | Mixed methods | HIC | USA | People with mental health problems |
|
Mental and behavioural health | FI: service expansion and linkage |
| Beere 2019 | Mixed methods | HIC | Australia | People with mental health problems |
|
Mental and behavioural health | FI: service expansion and linkage |
| Benjumea‐Bedoya 2019 | Mixed methods | HIC | Canada | Refugees in need of TB services |
|
HIV, TB, and SRH | PI: service expansion and linkage |
| Benson 2018 | Mixed methods | HIC | Australia | People with complex medication regimens or multiple comorbidities, or both |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Bentham 2015 | Mixed methods | HIC | USA | People in need of anxiety and depression services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Bentley 2015 | Mixed methods | HIC | USA | Aged care patients in PHC or GP practices |
|
PHC and other services | PI: service linkage |
| Berkel 2019 | Qualitative | HIC | USA | All PHC patients |
|
Mental and behavioural health | FI: service expansion and linkage |
| Bernard 2016 | Mixed methods | HIC | USA | People living with HIV |
|
HIV, TB, and SRH | FI: service expansion and linkage |
| Billings 2019 | Qualitative | HIC | UK | PHC facility, community service and home care service users |
|
PHC and other services | FI: horizontal |
| Blasi 2018 | Qualitative | HIC | USA | PHC patients with behavioural health needs, including support for managing of chronic disease |
|
Mental and behavioural health | FI: service expansion and linkage |
| Bradley 2008 | Qualitative | HIC | UK | All PHC patients – for medication review |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Brooks 2020 | Qualitative | HIC | USA | People with substance use disorder seeking care in outpatient PHC settings |
|
Mental and behavioural health | PI: service expansion and linkage |
| Burgess 2016 | Qualitative | MIC | South Africa | People with mental health needs |
|
Mental and behavioural health | PI: service expansion and linkage |
| Busch 2013 | Qualitative | HIC | Netherlands | New parents and their children |
|
PHC and other services | FI: service expansion and linkage |
| Busetto 2015 | Qualitative | HIC | Netherlands | People with diabetes and geriatric chronic care patients |
|
NCDs | FI: service expansion + linkage |
| Butler 2018 | Qualitative | HIC | USA | People with mental health needs receiving care at PHC level |
|
Mental and behavioural health | FI: service expansion and linkage |
| Carman 2019 | Qualitative | HIC | USA | All PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Church 2015 | Mixed methods | MIC | Eswatini | People with HIV |
|
HIV, TB, and SRH | Mixed: FI + PI |
| Cifuentes 2015 | Mixed methods | HIC | USA | People with behavioural health |
|
Mental and behavioural health | PI: service expansion and linkage |
| Clark 2017; Davis 2015; Gunn 2015 | Mixed methods | HIC | USA | Health users in PHC with behavioural and mental health needs |
|
Mental and behavioural health | FI: service expansion and linkage |
| Cole 2015 | Qualitative | HIC | USA | Uninsured patients in PHC services |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Cooper 2020 | Mixed methods | LIC | Malawi | Mother bringing in their children for immunisation Mothers who were seeking family planning |
|
MCWH | FI: service expansion and linkage |
| Dayton 2019 | Mixed methods | MIC | Dominican Republic | People using HIV services especially those vulnerable to gender‐based violence, e.g. men who had sex with men, commercial sex workers, transgender people |
|
HIV, TB, and SRH | PI: service expansion and linkage |
| De Lusignan 2020 | Mixed methods | HIC | UK | People suspected to have influenza |
|
PHC, allied and specialised services | PI: service expansion |
| De Nóbrega 2014 | Qualitative | MIC | Brazil | Men |
|
PHC and other services | FI: service expansion and linkage |
| Derrett 2014 | Qualitative | HIC | USA | Rural patients accessing PHC services |
|
PHC and other services | FI: service expansion and linkage |
| Donnelly 2013 | Qualitative | HIC | Canada | PHC patients |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Douglas 2017 | Qualitative | HIC | Australia | People using geriatric care at PHC level |
|
PHC and other services | FI: service expansion and linkage |
| Duma 2019 | Qualitative | LIC | Malawi | Women in need of HIV or SRH (or both) services |
|
HIV, TB, and SRH | FI: service expansion and linkage |
| Dunbar 2018 | Qualitative | HIC | USA | People using mental health services at PHC and community‐based centre level |
|
Mental and behavioural health | FI: service expansion and linkage |
| Edelman 2016 | Qualitative | HIC | USA | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Fitzpatrick 2017; Fitzpatrick 2018 | Qualitative | HIC | Australia | People with mental health problems in rural areas |
|
Mental and behavioural health | FI: service expansion |
| Fleury 2016 | Mixed methods | HIC | Canada | People with mental health problems in primary care |
|
Mental and behavioural health | FI: service expansion |
| Fong 2019 | Qualitative | HIC | USA | General paediatric population in need of behavioural health services |
|
Mental and behavioural health | FI: service expansion |
| Foster 2009 | Mixed methods | HIC | Australia | People receiving chronic care treatment by general practitioners |
|
PHC, allied and specialised services | PI: service expansion |
| Foster 2016 | Qualitative | HIC | Australia | People with complex diabetes |
|
NCDs | FI: service expansion |
| Gadomski 2014 | Qualitative | HIC | USA | Children and adolescents |
|
Mental and behavioural health | PI: service expansion |
| Gavin 2008 | Qualitative | HIC | Ireland | PHC patients with mental health needs – for detecting people with serious mental health disease (psychosis) |
|
Mental and behavioural health | PI: service expansion |
| Gear 2016 | Qualitative | HIC | New Zealand | People in need of family violence services at PHC level |
|
Mental and behavioural health | PI: service expansion |
| Geelhoed 2013 | Mixed methods | LIC | Mozambique | Mothers who accessing maternal and child healthcare services |
|
MCWH | FI: horizontal |
| Gerber 2018 | Mixed methods | MIC | South Africa | People in need of mental healthcare care services in PHC |
|
Mental and behavioural health | FI: service expansion and linkage |
| Gerrish 1999 | Qualitative | HIC | UK | General PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Ghorbani 2018 | Qualitative | MIC | Iran | Mothers and children needing access to oral health care at PHC level |
|
PHC, allied and specialised services | PI: service expansion |
| Glasgow 2012 | Mixed methods | HIC | USA | People with diabetes in PHC |
|
NCDs | PI: service expansion |
| Greene 2016 | Mixed methods | HIC | USA | Children in paediatric care services who need access to mental health services |
|
Mental and behavioural health | PI: service linkage |
| Gucciardi 2016 | Qualitative | HIC | Canada | People with diabetes at PHC |
|
NCDs | PI: service expansion and linkage |
| Haddow 2007 | Qualitative | HIC | UK | PHC patients requiring assistance with accessing unscheduled health care at PHC and hospital levels |
|
PHC and other services | FI: service linkage |
| Harnagea 2018 | Qualitative | HIC | Canada | Children in need of oral care |
|
PHC, allied and specialised services | PI: service expansion and linkage |
| Hepworth 2015 | Qualitative | HIC | Australia | Aboriginal and Torres Strait Islander people in need of mental health and chronic disease services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Hlongwa 2019 | Qualitative | MIC | South Africa | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Hunter 2018 | Mixed methods | HIC | USA | People in need of substance use disorder services in PHC |
|
Mental and behavioural health | FI: service expansion |
| Ion 2017 | Mixed methods | HIC | Canada | People in need of mental health care at PHC |
|
Mental and behavioural health | PI: service expansion and linkage |
| Jacobs 2012 | Qualitative | MIC | Lao | Mothers and children accessing immunisation and mother and child health services |
|
MCWH | PI: service expansion and linkage |
| Jauregui 2016 | Mixed methods | HIC | Spain | People in chronic care with multimorbidity |
|
NCDs | PI: service Linkage |
| Jewett 2013 | Qualitative | HIC | USA | People in need of hepatitis C virus services |
|
HIV, TB, and SRH | PI: service expansion |
| Johnson 2020 | Qualitative | MIC | India | People with diabetes in need of mental health services for depression |
|
Mental and behavioural health | PI: service expansion and linkage |
| Jorgenson 2014 | Qualitative | HIC | Canada | People in need of medication review |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Kawonga 2016 | Qualitative | MIC | South Africa | People with HIV |
|
HIV, TB, and SRH | FI: horizontal |
| Khan 2018 | Mixed methods | MIC | Pakistan | PHC patients using hypertension care services |
|
NCDs | PI: service expansion and linkage |
| Kirchner 2004 | Qualitative | HIC | USA | People in need of mental health and substance use services |
|
Mental and behavioural health | PI: service expansion |
| Lane 2017 | Qualitative | HIC | Australia | PHC patients in need of comprehensive clinical and allied medicine care |
|
PHC, allied and specialised services | PI: service expansion and linkage |
| Langer 2014 | Qualitative | HIC | UK | People with chronic obstructive pulmonary disease in PHC in need of psychosocial and mental health services |
|
Mental and behavioural health | PI: service expansion and linkage |
| Lawn 2014 | Qualitative | HIC | Australia | All PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Limbani 2019 | Mixed methods | MIC | South Africa | People with chronic illnesses in rural PHC |
|
NCDs | PI: service expansion and linkage |
| Lombard 2009 | Qualitative | HIC | USA | People diagnosed with HIV, sexual abuse, and mental illness |
|
Mental and behavioural health | PI: service expansion and linkage |
| Lovero 2019 | Mixed methods | MIC | South Africa | People with TB and people in need of mental health services |
|
Mental and behavioural health | PI: service expansion |
| Lucas 2016 | Qualitative | HIC | Australia | People with chronic disease at PHC facilities and community‐based services |
|
NCDs | PI: service linkage |
| Ma 2018 | Qualitative | HIC | USA | Asian‐American immigrants attending PHC |
|
Mental and behavioural health | FI: service expansion and linkage |
| Main 2007 | Qualitative | HIC | UK | People visiting general PHC and general practitioners |
|
PHC and other services | FI: service expansion |
| Malachowski 2019 | Qualitative | HIC | Canada | People with mental health care needs |
|
PHC and other services | FI: service expansion and linkage |
| Marais 2015 | Qualitative | MIC | South Africa | People with mental health care needs in PHC |
|
Mental and behavioural health | FI: service expansion |
| Martin 2018 | Qualitative | MIC | Kenya | Pregnant women receiving antenatal care |
|
MCWH | PI: service expansion |
| Mathibe 2015 | Qualitative | MIC | South Africa | People with HIV receiving antiretroviral treatment |
|
HIV, TB, and SRH | Mixed: FI + PI |
| Mayer 2016 | Qualitative | HIC | USA | People with diabetes and other chronic disease receiving care in PHC and community centres |
|
NCDs | PI: service expansion |
| McGeehan 2007 | Qualitative | HIC | USA | General PHC patients |
|
NCDs | PI: service linkage |
| McNamara 2020 | Mixed methods | HIC | Australia | Adults in the community not diagnosed with cardiovascular disease, and not being treated for hypertension or lipid disorders |
|
NCDs | PI: service expansion and linkage |
| Meyer‐Kalos 2017 | Qualitative | HIC | USA | People with severe mental illness |
|
Mental and behavioural health | PI: service expansion and linkage |
| Miguel‐Esponda 2020 | Mixed methods | MIC | Mexico | People in need of mental health services |
|
Mental and behavioural health | FI: horizontal |
| Mishra 2014 | Qualitative | MIC | India | Rural poor, women, and children |
|
MCWH | PI: service expansion and linkage |
| Mugisha 2016 | Qualitative | LIC | Uganda | People with mental health problems in PHC |
|
Mental and behavioural health | FI: service expansion and Linkage |
| Mulenga 2019 | Qualitative | MIC | Democratic Republic of the Congo | People attending basic care services who might need Human African trypanosomiasis services |
|
PHC, allied or and specialised services | Mixed: FI and PI |
| Murphy 2018 | Mixed methods | MIC | Vietnam | People in need of mental health services |
|
Mental and behavioural health | PI: service expansion and linkage |
| Mutabazi 2020 | Qualitative | MIC | South Africa | Maternal health service users in PHC |
|
HIV, TB, and SRH | FI: service expansion and linkage |
| Mutemwa 2013 | Qualitative | MIC | Kenya | People coming for family planning and postnatal care |
|
HIV, TB, and SRH | PI: service expansion |
| Mykhalovskiy 2009 | Qualitative | HIC | Canada | People with HIV (for HIV prevention) |
|
HIV, TB, and SRH | PI: service expansion and linkage |
| Ndwiga 2014 | Qualitative | MIC | Kenya | People with HIV and reproductive health |
|
HIV, TB, and SRH | FI: horizontal |
| Nelson 2019 | Qualitative | LIC | Liberia | Mothers using child vaccination services |
|
MCWH | PI: service expansion and linkage |
| Newell 2018 | Qualitative | HIC | Ireland | People with diabetes in PHC |
|
NCDs | PI: service expansion and linkage |
| Newmann 2013 | Mixed methods | MIC | Kenya | HIV positive men and women accessing family planning services |
|
HIV, TB, and SRH | PI: service expansion |
| Newmann 2016 | Mixed methods | MIC | Kenya | People in need of family planning and HIV services |
|
HIV, TB, and SRH | PI: service expansion |
| Nooteboom 2020 | Qualitative | HIC | Netherlands | Highly vulnerable families |
|
Mental and behavioural health | FI: service linkage |
| Norfleet 2016 | Mixed methods | HIC | USA | People in need of mental health services |
|
Mental and behavioural health | PI: service expansion and linkage |
| Nxumalo 2013 | Qualitative | MIC | South Africa | General PHC patients |
|
PHC and other services | PI: service expansion and linkage |
| Oishi 2003 | Qualitative | HIC | USA | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Ojikutu 2014 | Qualitative | HIC | USA | People with HIV |
|
HIV, TB, and SRH | PI: service linkage |
| Okot‐Chono 2009 | Qualitative | LIC | Uganda | People with HIV or TB |
|
HIV, TB, and SRH | FI: horizontal |
| Oliff 2003 | Qualitative | MIC | Tanzania | People in need of maternal and reproductive care |
|
MCWH | FI: horizontal |
| Patwa 2019 | Qualitative | MIC | South Africa | People with HIV and the general population using the PHC services |
|
HIV, TB, and SRH | FI: service expansion |
| Payne 2017 | Qualitative | HIC | USA | General PHC patients |
|
PHC and other services | FI: service expansion |
| Peer 2020 | Mixed methods | MIC | South Africa | People with both HIV and hypertension |
|
HIV, TB, and SRH | PI: service expansion and linkage |
| Pereira 2011 | Qualitative | MIC | India | People in need of common mental health disorder treatment |
|
Mental and behavioural health | FI: service expansion and linkage |
| Petersen 2009 | Mixed methods | MIC | South Africa | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Petersen 2011 | Qualitative | LMIC | Uganda, South Africa | People in need of mental health services Uganda – people in need of severe mental health services South Africa – people in need of depression services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Petersen 2019 | Qualitative | LMIC | Ethiopia, India, Nepal, Nigeria, South Africa, Uganda | People in need of mental health services |
|
Mental and behavioural health | Mixed: FI + PI |
| Pfitzer 2019 | Mixed methods | LMIC | Kenya and India | Pregnant women and postpartum women |
|
MCWH | PI: service expansion |
| Peer 2020; Pidano 2011 | Qualitative | HIC | USA | Children in need of mental health services |
|
Mental and behavioural health | PI: service linkage |
| Piper 2018 | Qualitative | HIC | USA | PHC and community‐based health users |
|
PHC and Other services | PI: service expansion and linkage |
| Piper 2020 | Mixed methods | HIC | USA | People with HIV |
|
Mental and behavioural health | PI: service expansion and linkage |
| Porter 2002 | Qualitative | MIC | India | People in need of TB services and leprosy services |
|
HIV, TB, and SRH | FI: horizontal |
| Ramanuj 2018 | Qualitative | HIC | USA | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Reinschmidt 2017 | Qualitative | HIC | USA | People with both mental health and chronic care needs |
|
NCDs | PI: service expansion |
| Rissi 2015 | Qualitative | HIC | USA | Community |
|
PHC and other services | FI: service expansion and linkage |
| Robertson 2018 | Qualitative | LIC | Malawi | Children aged under 5 years in need of medical care |
|
MCWH | PI: service expansion |
| Rodriguez 2006 | Qualitative | HIC | Canada | Diabetes patients |
|
NCDs | PI: service linkage |
| Rodriguez 2019 | Qualitative | HIC | USA | Latin children in need of mental healthcare |
|
Mental and behavioural health | FI: service Linkage |
| Rojas 2015 | Qualitative | HIC | USA | Latino and African American adults with poorly controlled type 2 diabetes |
|
NCDs | PI: service linkage |
| Ross 2000 | Mixed methods | HIC | UK | General PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Ryman 2012b | Qualitative | LMIC | Kenya, Mali, Cameroon, and Ethiopia | Mothers taking their children for vaccination in PHC |
|
MCWH | PI: service expansion |
| Ryman 2012c | Mixed methods | MIC | Kenya | Children receiving immunisation at the clinic |
|
MCWH | PI: service expansion |
| Sakeah 2014 | Qualitative | MIC | Ghana | Woman in labour |
|
MCWH | PI: service expansion |
| Sheth 2020 | Mixed methods | HIC | USA | Adolescent and adult women |
|
HIV, TB, and SRH | PI: service expansion |
| Savickas 2020 | Qualitative | HIC | UK | People with long‐term illnesses |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Shattell 2011 | Qualitative | HIC | USA | People with severe mental illness |
|
Mental and behavioural health | PI: service expansion |
| Shelley 2019 | Qualitative | MIC | Tanzania | Mothers with HIV |
|
HIV, TB, and SRH | PI: service expansion |
| Shin 2018 | Qualitative | HIC | South Korea | People with disabilities |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Shrivastava 2020a; Shrivastava 2020b | Qualitative | HIC | Canada | People in need of oral care |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Siantz 2018 | Qualitative | HIC | USA | People with mental health problems |
|
Mental and behavioural health | PI: service expansion and linkage |
| Sieverding 2016 | Qualitative | MIC | Nigeria | General PHC patients |
|
PHC and other services | PI: service expansion |
| Sinai 2018 | Qualitative | MIC | South Africa | People with HIV with suspected latent TB |
|
HIV, TB, and SRH | FI: horizontal |
| Smit 2012 | Qualitative | MIC | South Africa | People with HIV |
|
HIV, TB, and SRH | FI: horizontal |
| Sobo 2008 | Qualitative | HIC | USA | People at risk of HIV |
|
HIV, TB, and SRH | PI: service expansion |
| Souza 2019 | Qualitative | MIC | Brazil | People with mental health problems in PHC |
|
Mental and behavioural health | FI: service expansion and linkage |
| Souza Gleriano 2019 | Qualitative | MIC | Brazil | General PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Ssebunnya 2010 | Qualitative | LIC | Uganda | People in need of PHC services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Stadnick 2020 | Mixed methods | HIC | USA | Children with autism |
|
Mental and behavioural health | PI: service expansion and linkage |
| Surjaningrum 2018 | Qualitative | MIC | Indonesia | Pregnant women and women who recently gave birth |
|
Mental and behavioural health | PI: service expansion |
| Terry 2018 | Qualitative | HIC | USA | People needing services for mental health, cognitive impairment, and substance abuse |
|
Mental and behavioural health | FI: service expansion and linkage |
| Topp 2010 | Mixed methods | MIC | Zambia | People with HIV and people attending outpatients |
|
HIV, TB, and SRH | PI: service expansion |
| Topp 2013 | Mixed methods | MIC | Zambia | People with HIV and general patients attending outpatient |
|
HIV, TB, and SRH | FI: horizontal |
| Treloar 2014 | Qualitative | HIC | New Zealand | People with hepatitis C |
|
PHC and other services | PI: service linkage |
| Tsasis 2012 | Qualitative | HIC | Canada | General PHC patients |
|
PHC and other services | FI: service expansion and linkage |
| Tshililo 2019 | Qualitative | MIC | South Africa | People needing HIV/AIDS services |
|
HIV, TB, and SRH | FI: service linkage |
| Tsui 2018 | Mixed methods | HIC | USA | Long‐term cancer survivors |
|
PHC, allied and specialised services | PI: service linkage |
| Uebel 2013 | Qualitative | MIC | South Africa | People with HIV |
|
HIV, TB, and SRH | PI: service expansion |
| Urada 2014 | Mixed methods | HIC | USA | People in need of mental health and substance use disorder services |
|
Mental and behavioural health | PI: service expansion |
| Uwimana 2013 | Mixed methods | MIC | South Africa | Pregnant woman attending prevention of mother‐to‐child transmission/antenatal services |
|
HIV, TB, and SRH | PI: service expansion |
| Venables 2016 | Qualitative | MIC | Kenya | People stable on HIV and NCD medication |
|
HIV, TB, and SRH | FI: service expansion |
| Venancio 2016 | Mixed methods | MIC | Brazil | People with diabetes and hypertension |
|
NCDs | Unclear |
| Vestjens 2018 | Mixed methods | HIC | Netherlands | Frail elderly people |
|
NCDs | FI: service linkage |
| Vickers 2013 | Qualitative | HIC | USA | People in need of mental health service |
|
Mental and behavioural health | PI: service expansion and linkage |
| Wakida 2018; Wakida 2019 | Qualitative | LIC | Uganda | People in need of mental health services |
|
Mental and behavioural health | FI: service expansion and linkage |
| Wallace 2013 | Mixed methods | HIC | Canada | Clients who needed dental care, but could not afford it |
|
PHC, allied and specialised services | FI: service expansion and linkage |
| Wallace 2014 | Qualitative | MIC | Tanzania | Parents of children coming receiving immunisation |
|
HIV, TB, and SRH | PI: service expansion |
| Waterworth 2015 | Qualitative | HIC | UK | PHC, community and home‐based care patients |
|
PHC and other services | FI: service expansion and linkage |
| Wener 2016 | Qualitative | HIC | Canada | People in need of mental health services in PHC |
|
Mental and behavioural health | FI: service linkage |
| Wiese 2011 | Qualitative | HIC | Australia | Women and others who received care in community health centre |
|
PHC and other services | FI: service linkage |
| Wilunda 2017 | Qualitative | LIC | South Sudan | Pregnant women and women in labour |
|
MCWH | PI: service expansion |
| Yessimov 2019 | Mixed methods | MIC | Republic of Kazakhstan | General PHC patients |
|
PHC and other services | Unclear |
| Young 2019 | Qualitative | MIC | Kenya | Women receiving antenatal services |
|
MCWH | PI: service expansion |
| Zimbudzi 2019 | Qualitative | HIC | Australia | People with both diabetes and chronic kidney disease |
|
NCDs | PI: service linkage |
| Zotti 2010 | Qualitative | HIC | USA | Women receiving reproductive health services |
|
HIV, TB, and SRH | PI: service expansion |
| Zulu 2015 | Qualitative | MIC | Zambia | General PHC patients |
|
PHC and other services | PI: service expansion |
| Zulu 2019 | Qualitative | MIC | Zambia | Young adults in need of SRH services |
|
MCWH | PI: service expansion and Linkage |
FI: full integration; HIC: high‐income country; LMIC: low‐ to middle‐income country; MCWH: maternal, child, and women's health; MIC: middle‐income country; NCD: non‐communicable disease; PHC: primary health care; PI: partial integration; TB: tuberculosis: SRH: sexual and reproductive health.
In the section below, we provided a narrative summary of the key result areas, illustrated by graphs where appropriate. We did not include references for each result area due to the large number of studies included. The references are presented in data tables in the appendices.
Description of studies
In this section, we presented the quantitative results and narrative summaries of results based on the 184 analysed studies.
1. Publication date
The earliest publication was in 1997, and the latest publication was in 2020 (Figure 2). Most studies, 160 (87%), were published in the last 10 years, since 2011. Nearly one‐third, 56 studies (30%), were published between 2011 and 2015. The number of publications doubled in the last five years (2016 to 2022), with more than half of the total number of studies, 104 studies (57%), published in this period.
2.
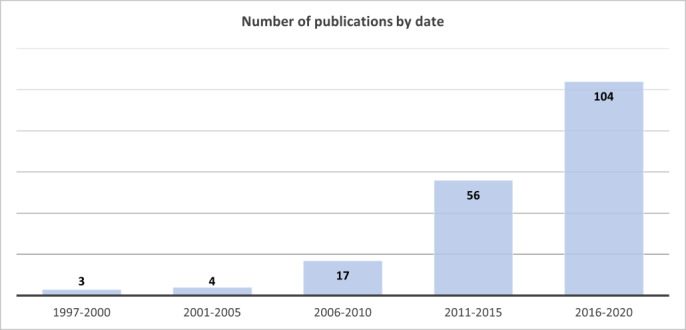
Number of publications by date
2. Study methods
2.1. Study design
Most studies (121 studies, 66%) used only qualitative methods in their study design, and the remainder (63 studies, 34%) were mixed‐method studies. Studies collected data using the following methods: individual interviews (IIs) only in 123 studies (67%), focus group discussions (FGDs) only in 11 studies (6%), and both IIs and FGDs in 27 studies (15%). In 23 studies (12%), researchers used other forms of qualitative data collection methods in addition to IIs and FGDs. These included a combination of document reviews (nine), field/site/clinical observations (15), and research diaries. Only two studies used a more in‐depth, longitudinal study approach described as 'ethnographic' methods.
2.2. Sample size
In total, 14 studies (8%) did not provide details on the sample size and 170 studies (92%) provided sample size. The studies that provided a sample size interviewed 4303 individual participants through IIs, and conducted 186 FGDs. We did not calculate the total number of individuals who participated in FGDs as not all studies provided details on the number of people in each focus group. In Appendix 2 and Appendix 3, we presented references for study designs and sample size.
3. Settings
3.1. Country income level and country
Figure 3 is a diagrammatic presentation of the number of studies per country, as well as the breakdown of the countries represented per country income level. The single‐country studies represented 33 different countries. Amongst the multicountry studies, six countries were also represented in the single‐country studies, while four were not represented. Therefore, the total number of countries represented was 37. Regarding geographic distribution, 104 (56%) single‐country studies were conducted in 10 high‐income countries (HICs). Sixty‐three (34%) single‐country studies were conducted in 17 different middle‐income countries (MICs). Twelve (7%) single‐country studies were conducted in six low‐income countries (LICs). There were also five multicountry studies, all conducted in LMICs.
3.
Geographic distribution and number of studies per country
Within each of the country‐income settings, some countries were more dominant. In HICs, 51 studies (49%) were from the USA only. In MICs, 19 studies (30%) were from South Africa only. In LICs, five studies (42%) were from Uganda.
In Appendix 4; Appendix 5; Appendix 6; and Appendix 7, we presented references of country income level and country.
3.2. Urban/rural
Eighty‐two studies (45%) did not indicate the urban/rural location of the study setting. Of the remaining 102 studies reporting this, 43 studies (42%) were urban, 24 studies (23%) rural, and 35 studies (34%) reported a mix of rural and urban locations for interventions.
There were variations in urban/rural locations for interventions across HICs and LMICs. In HICs, the dominant location was urban only in 33 studies (61%), followed by urban and rural in 17 studies (31%), and rural only in four studies (7%). In MICs, the dominant location was rural only in 14 studies (39%), followed by urban and rural in 13 studies (36%), and urban only in nine studies (25%). In LICs, the dominant location was rural only in five studies (63%), followed by urban and rural in two studies (25%), and urban only in one study (12%). In multicountries, the dominant location was urban and rural in three studies (60%), urban only in one study (20%), and rural only in one study (20%). In Appendix 4; Appendix 5; Appendix 6; and Appendix 7, we presented references of urban/rural location or setting.
3.3. Healthcare level
The review focussed on interventions delivered on the PHC delivery platform. However, there were different forms of PHC service platforms. Most studies referred to PHC clinics as the primary intervention site (144 studies, 78%). Some interventions involved delivering PHC services on a level below, at a community‐based service level (e.g. providing TB services in community health centres) (26 studies, 14%). While in some cases, PHC services were also delivered at the district hospital level as the entry point for care (e.g. family planning, and sexual and reproductive services) (7 studies, 4%). In some cases, PHC interventions were delivered across all three levels of care, PHC clinics, community‐based service level, and hospital level (7 studies, 4%) (e.g. community healthcare workers working with nurses from PHC clinics and nurses work with obstetricians from district hospitals to allow women to access pregnancy and childbirth care).
PHC service platforms also had different institutional arrangements, with some being structured as public–private partnerships (PPPs), where the government contracted non‐governmental agencies (for profit or not for profit) to deliver PHC health services (e.g. Australia, the UK, the USA).
4. Target client populations
We categorised the target client population according to the health service stream configurations described later. We provided proportions when presenting different health service streams and focussed here on providing descriptive details of the different types of the target client population.
4.1. Mental and behavioural health service clients
The target client population in this category was those needing mental health services only; these were common mental disorders such as anxiety and depression, and severe mental disorders such as schizophrenia and major depression. This target client population also included people seeking mental health and other PHC services. These included PHC clients seeking care for substance use disorder, and mental health and behavioural services as part of that care. Clients needing mental health services and support for their chronic illnesses are also included here.
4.2. HIV, tuberculosis, and sexual and reproductive health service clients
The target client population in this category was those needing services for one disease only (HIV, TB, or SRH), or a combination of these services. Examples were refugees needing TB latent services; the youth needing SRH services only; and clients needing a combination of HIV, TB, or SRH services. An example of the latter is clients in need of both a combination of TB and HIV services, or clients with either TB or HIV, or both, who also sought access to other SRH services, such as family planning services.
4.3. Maternal, child, and women's health service clients
The target client population in this category was children and women. The children targeted were aged between five and 18 years. Children were a target group for interventions such as common children's illnesses, behavioural services, and oral healthcare in general PHC settings or within a programme of integrated child management services. Women were a target client population for interventions that included children's services. These included women being offered antenatal and postpartum, HIV, family planning, and sexual and reproductive services alongside those for children such as immunisation services, malaria services, and HIV services.
4.4. Non‐communicable diseases service clients
The target client population in this category was those in need of NCDs services. These groups included the general PHC population, such as clients in need of general NCD prevention services (general PHC clients at risk for NCDs). This also included specific clients at higher risk of NCDs, such as older people. The target client population also include those with specific NCDs (e.g. people with diabetes) and those with multimorbid NCDs and those with complex medical regimens. Clients needing chronic care services, such as chronic services for HIV, TB, mental health, and pulmonary disease were also targets of this health stream.
4.5. General primary healthcare service clients
The target client population for this category was those needing general PHC services. These included acute and minor health needs and general services linked to community healthcare and PHC clinics and clients for health promotion services. These included lay healthcare workers working alongside PHC workers to provide services to people living in rural areas. Also, lay healthcare workers provide health promotion services to the community. One example is the Family Health Strategy in Brazil used to provide PHC that addresses a full package of health promotion, prevention, treatment, rehabilitation, palliative care, and health surveillance services. Another example, also in Brazil, is the integration of services across primary care services to better address men's health needs.
4.6. Allied and specialised health service clients
The target client population for this category was children, youths, and adults needing allied and specialised services that were not always readily available at the PHC level. These included clients with specific needs for occupational or physiotherapy services, such as people living with disabilities. Also included were clients with specific health needs that were previously offered in specialised settings (i.e. children and adults in need of oral health and dental services, adults in need of specialised care for substance use disorder, follow‐up treatment for cancer survivors, people needing gender‐based violence services, and mental health services). The latter was covered under the mental and behavioural health stream mentioned above.
5. Research participants
A range of research participants provided information on their perceptions and experiences of being involved in implementing integration interventions (Figure 4). We categorised participants in terms of their roles in the health system. We found that the clinical healthcare worker category was dominant, listed in 159 studies (86%). This was followed by the category of clinical managers, listed in 36 studies (19%). The allied healthcare worker category was listed in 29 studies (16%), and the lay healthcare worker category was listed in 25 studies (13%). The category of district managers was listed in 14 studies (8%), health system support staff in 13 studies (8%), and health system advisors in 11 studies (6%). The categories of research participants that were least commonly found in studies were policymakers and provincial managers, listed in six studies (3%) and civil society in five studies (2%).
4.
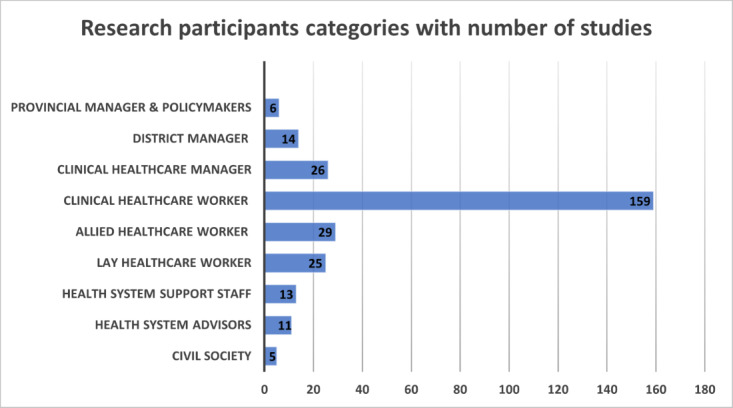
Research participant categories per number of studies
6. Intervention description
6.1. Health service streams
We provided details of the health service streams configured for delivering integrated services. We began by presenting an overview of the health service streams for integration interventions as shown in Figure 5. Thereafter, we presented them per country income level as shown in Figure 6.
5.
Health service streams for integration interventions
6.
Health service streams for integration per country income level
Mental and behavioural health services was the most frequent health programme area of integration of services, making up one‐third (61 studies, 33%) of all studies. Integration of HIV, TB, and SRH services was the second most frequent health programme area for integration (37 studies, 20%), followed by interventions related to the integration of NCD services (24 studies, 13%) and MCWH (16 studies, 9%).
A quarter of the included studies (46 studies, 25%) had wider focus areas, and these could not easily be categorised in the earlier health service stream configuration categories. We subdivided these studies into two different categories. We labelled one as general PHC services (28 studies, 15%). These interventions focused on integration within and across the provision of general PHC services (e.g. facility and community‐based or curative and preventive medicine), and were interventions not limited to specific disease/health programmes. The other category we labelled as allied and specialised services (18 studies, 10%). This included interventions where there was an introduction at the PHC level, of specialised services that were not previously on offer at the PHC level. This included PHC‐based services by allied health professionals (e.g. occupational therapy), or by specialised health professionals (e.g. mental health specialists).
6.1.1. Mental and behavioural health services per country income level
Mental and behavioural health services was the most frequent health service integration stream, with 61 studies (33%). Most (42 studies, 69%) were from HICs. Within the HICs, most (31 studies, 73%) came from only one country, the USA. The remainder (11 studies, 27%) were from six other HICs. Fourteen mental and behavioural health services studies (23%) were from MICs, with six studies (43%) being from one country, South Africa, and the remainder (eight studies, 57%) from six other MICs. Three mental and behavioural health‐related studies were from LICs (5%) (all from Uganda), and two studies (3%) were set in multiple LMICs.
There were different configurations of how mental health services were being integrated at the PHC level. One configuration was devolving whole mental health services from hospital/specialised service settings, for delivery within PHC clinics or general practitioner practices. Such services could be accompanied with specialised mental health staff being placed at the PHC level to provide services directly to clients, or to support general PHC staff to deliver mental health services. On the other end of the spectrum, interventions may introduce a smaller extension of mental health service that was not previously on offer at the PHC level, such as providing mental health screening for common and serious mental health conditions, but with referral to specialised care elsewhere. In Appendix 8, we presented references for studies of mental and behavioural health service stream integration per country income level.
6.1.2. HIV, tuberculosis, and sexual and reproductive health services per country income level
HIV, TB, and SRH services was the second most frequent health service integration stream, with 37 studies (20%) focused on various combinations of integration of HIV, TB, and SRH services. Most studies were from MICs (25 studies, 67%). This was followed by eight studies (22%) from HICs, three studies (8%) from LICs, and one study (3%) set in multiple LMICs. Most MIC‐based studies (10 studies, 40%) came from one country, South Africa, with the remainder (60%) spread across seven other MICs. Of the eight HIC‐based studies, six studies (75%) were from one country, the USA, and the remainder (two studies, 25%) were from Canada. Of the three LICs studies, two (67%) were from Uganda, and one (33%) was from Malawi.
Interventions in this stream consisted of different integration configurations of linking HIV, TB, and SRH services. This included HIV treatment being devolved from the hospital level to be delivered at the PHC level. It also included linkages between and joint delivery at the point of care of previously siloed (vertical) PHC‐based services for HIV, TB, and SRH services. Another configuration was expanding HIV prevention and health promotion services to community‐based settings. For example, at the PHC level or expanding to comprehensive HIV and TB services for maternal and child health (e.g. via the PHC). Other interventions focused on expanding HIV, TB, and SRH screening services (through point‐of‐care testing) for a range of client target groups, including those with NCDs, in maternal and child health care (e.g. via the Prevention of Mother to Child Treatment (PMTCT) programme); also, for gender‐based violence, and other health conditions. In Appendix 9, we presented references for studies of HIV, TB, and SRH service integration per country income level.
6.1.3. Maternal, child, and women's health services per country income level
MCWH integration services was the least common health service integration stream, with 16 studies (9%). Most studies were from MICs (nine studies, 56%). Three of the MICs studies (33%) were from Kenya, and the remainder (6 studies, 67%) were spread across five different MICs. Five studies (31%) were from LICs; amongst these, two studies (40%) were from Malawi. Two studies (13%) were in multicountries, with Kenya found in two multicountry studies. There were no studies set in HICs.
Studies included integrating broader maternal and child services with vaccination services, calcium supplementation for pregnant women, point‐of‐care testing for infectious diseases, linkage with skilled birth attendants and community health workers, and outreach to community‐based settings. In Appendix 10, we presented references for studies of MCWH service integration per country income level.
6.1.4. Non‐communicable diseases services per country income level
NCDs services was the fourth most common health service integration stream, with 24 studies (13%) focusing on the integration of various combinations of NCDs and integration of NCDs programmes with other disease programmes. Of the 24 studies with NCDs service integration, most were from HICs (18 studies, 75%). Six of these studies (33%) were from one country, the USA, and the remainder (12 studies, 67%) were spread across six HICs. Six studies (25%) were from MICs, with two studies (33%) each from South Africa and Brazil, and one study (17%) each from India and Pakistan. There were no NCDs‐related studies from LICs.
Integration interventions in this stream focused on joint management for multiple chronic diseases (such as diabetes and hypertension) that were previously not delivered in an integrated manner. Other configurations involved delivery and linkage of NCDs services within PHC services for prioritised client groups, such as for geriatric care and for those with multimorbid diseases. NCD‐related interventions included mechanisms for more effective and accessible NCD care (e.g. co‐location of NCD services, pharmacist‐led medication reviews, and community health worker outreach for expanding health promotion and prevention services for NCD). Interventions also included expanding components of NCD services to other disease services (e.g. NCD screening and NCD risk assessment for clients with TB, HIV, mental health disorders, or a combination of these; and cardiovascular screening by pharmacists). In Appendix 11, we presented references for studies of NCD service integration per country income level.
6.1.5. General primary healthcare services per country income level
General PHC services was the third most common health service integration stream, with 28 studies (15%). This category comprised integration interventions focussed on improving linkages across different components of the PHC system, without necessarily focussing on specific disease/health programmes. Most studies were from HICs (21 studies, 75%), with six (29%) studies each from the USA and UK, and the remainder (9 studies, 42%) spread across four different HICs. There were seven studies (25%) from MICs, three (43%) from Brazil, and the remainder (4 studies, 57%) spread across four other MICs. There were no studies from LICs settings.
In this stream, we grouped a range of different integration interventions that were difficult to classify as part of the above categories. One set of intervention approaches focused on increased linkages between the management of acute and preventive services (health promotion) at both health facilities and community‐based service levels. Another set of interventions were aimed at increasing linkages between different PHC service organisations, to serve certain target client populations. One example is a purpose‐built 'Super clinic' in Australia that houses general practitioners and allied medical services in one building to improve service linkages for chronic care. Other configurations included integration across adult and child services in a family health strategy approach (e.g. combining the delivery of parent and child health services at one PHC centre). Other examples are linkages across PHC services to address men's health needs (in Brazil, as part of implementing their Men's Health Policy), and linkages across facility, community, and home‐based agencies for aged care.
Another set of interventions focused on studying the implementation and delivery strategies of the integration efforts more generally, be it via a focus on various health system functions, such as administrative and management systems, human resource management, information systems, and or via studying of change management processes. Examples included studies on the evaluation of administrative capacity for integrated monitoring and evaluation of HIV–TB care, use of electronic health information systems in mental health service integration, organisational leadership, and change management processes in implementing integration and studying the political dynamics of the change management process efforts to integrate of HIV–TB service delivery systems. Others focused on studying the introduction of different cadres of health workers into the PHC setting, such as nurse‐led teams, multidisciplinary teams, community health workers, dental and oral health workers, and pharmacists. In Appendix 12, we presented references of studies on general PHC service integration intervention per country income level.
6.1.6. Allied and specialised health services per country income level
Allied and specialised health service was the fifth most common health service integration stream, with 18 studies (10%). The focus was on making allied services (e.g. occupational therapy) or specialised services (e.g. dental services) available for delivery at the PHC level. 'Specialised' services refer here to those services that were previously only provided at a hospital or specialised or standalone level of the healthcare system (e.g. a dental clinic). These services would not previously have been available at the PHC level or where available, it was not considered a comprehensive level service at the PHC level. The majority were from HICs (15 studies, 83%), of which five studies (33%) were from one country, Canada, and the remainder (10 studies, 67%) were spread across five different HICs. Three studies (17%) were from MICs. There were no studies from LICs settings.
In this stream, we included intervention models that aimed to enhance the scope of general PHC services. These included the provision of comprehensive oral health services and dental services, and the provision and integration of occupational therapists, dieticians, and pharmacists into primary care teams. Other interventions included the integrated management of substance use disorders (that include opioid abuse), integrated cancer screening and cancer care, integrated care for disabilities, and molecular point of care testing for influenza and treatment of rare diseases (such as the tropical disease Human African Trypanosomiasis). In Appendix 13, we presented references of studies on allied and specialised health service integration intervention per country income level.
6.2. Scope of the integration
In half of all studies (92 studies, 50%), we categorised the integration scope as 'full Integration', and in 85 studies (46%), we categorised the scope of integration as 'partial integration' (Figure 7). (See the Methods section for details on how we defined full and partial integration.) In five studies (3%), the scope of the intervention was a mixture of full and partial integration. In two studies (1%), there was insufficient information to assess the scope of integration.
7.
Scope of the integration interventions
6.3. Intervention strategies
In terms of integration strategies, the most common strategy across both full and partial integration scope was the strategy that combined service expansion and service linkage, with close to half of all the studies (91 studies, 49%) reporting using this combined strategy (Figure 8). The second most common strategy was service expansion, used in 50 studies (27%), followed by service linkage, used in 22 studies (12%). Fourteen studies (8%) used horizontal integration strategies and only in the full integration intervention scope. (See the Methods section for details on how we defined the different strategies.)
8.
Integration strategies within full and partial integration scope
Within the full integration intervention scope, close to two‐thirds (58 studies, 63%) used the combined strategy of service expansion and linkage making the combined approach the most frequent strategy. This was followed by the horizontal integration strategy in 14 studies (15%), then service expansion (11 studies, 12%), and the least frequent strategy was service linkage (9 studies, 10%).
Within the partial integration intervention scope, 39 studies (46%) used service expansion, making it the most frequent strategy. A total of 33 studies (39%) used combined service linkage and expansion strategies, and 13 studies (15%) used service linkage only. In Appendix 14, we presented references for studies using different integration strategies within the full and partial integration scope.
Within the studies classified as full integration scope, the most frequent health service integration stream was mental and behavioural health services, with just over one‐third of studies (34 studies, 37%) (Figure 9). This was followed by studies classified as general PHC services (21 studies, 23%), and studies with HIV, TB, and SRH services (17 studies, 18%). Allied and specialised health services had 10 studies (11%) with full integration, NCDs integration had seven studies (8%), and MCWH health services had three studies (3%). In Appendix 15, we presented references for studies categorised as having 'full integration' scope across health service integration streams.
9.
Integration scope used within different health service streams
Within the studies classified as partial integration scope, the most frequent health service integration stream was mental and behavioural health services, making up close to one‐third of the studies (27 studies, 31%). This was followed by studies classified as HIV, TB, and SRH services (17 studies, 20%); NCDs integration had 16 studies (19%), and MCWH health services had 13 studies (15%). Allied and specialised health services had seven studies (8%) with partial integration, and general PHC services had six studies (7%). In Appendix 16, we presented references for studies categorised as having 'partial integration' scope across health service integration streams.
Of the five studies categorised as mixed, three studies (60%) were HIV, TB, and SRH services, with one study (20%) each from the mental and behavioural health services and allied and specialised services.
7. Conceptual models
About half of the studies (103 studies, 56%) made reference to using any model (analytical, service, or both) (Figure 10). (See the Methods section for details on how we defined 'analytical' and 'service' models.) Of the total sample, less than one‐third of studies (53 studies, 29%) reported using an analytical model to guide their study design, implementation, evaluation, or a combination of these; and just over one‐third (66 studies, 36%) reported using a service model to describe the integration intervention. Amongst these, some studies (16 studies, 9%) reported using both models.
10.
Conceptual models used in studies
Of the 103 studies that reported any model, 53 studies (51%) reported using an analytical model, while 66 studies (64%) reported using a service model. In Appendix 17, we provided the references for studies in each of these categories.
7.1. Analytical models
A total of 53 studies reported using an analytical model, mostly by itself (37 studies, 70%), or in combination with a service model (16 studies, 30%). Eleven studies (21%) referred to logic models or other frameworks without specifying the name and 42 studies (79%) specified the name of the analytical model. We identified 28 different analytical models that were explicitly named. Most models (18 models, 64%) were referred to in only one study, while 10 models (36%) were referred to twice. The most frequently used model was the Consolidated Framework for Implementation Research (CFIR) which was referred to in four studies. Models referred to in two studies were: Complex Adaptive Systems, Context Mechanism Opportunity (CMO) model, Donabedian's Structure‐Process‐Outcome Quality of Care Framework, Health System Governance approach, i‐PARIHS framework, Organizational theory, Rainbow Integrated Care Model, Realistic Evaluation Method, and the Transtheoretical Model of Behaviour Change. These models included a focus on organisational and behaviour change, as well as on implementation processes and on integration‐related processes.
7.2. Service models
Sixty‐six studies reported using a service model, either by itself (50 studies, 76%) or in combination with other models (16 studies, 24%). The service models mostly described the intervention components in more detail or referred to named intervention models for PHC integration. Examples of service models included those that focused on generic integrated care, for example, Chronic Disease Model, Community‐Based Outreach Model, Collaborative Care Team Model, Consumer‐Directed Care Model, and the C2C Task‐Shifting Model. Others referred to integration models specific to health programmes, for example, Maternal and Child Health Integrated Program (MCHIP), Interdisciplinary Models of HIV Care, Programme for Improving Mental Health Care (PRIME), Primary Care Behavioral Health (PCBH) Model of Integrated Primary Care, and Integrated Behavioral Health Model of Psychiatry in Pediatric Primary Care.
Discussion
Summary of results
PHC integration has been promoted as a healthcare reform for UHC since the late 1970s, but for a range of reasons, implementation and impact remain variable (Kumar 2016). Healthcare workers are known to shape the success of implementing reform interventions (Erasmus 2011). Understanding healthcare workers' perceptions and experiences of PHC integration can provide insights into the role healthcare workers play in shaping implementation efforts and the impact of PHC integration. However, the heterogeneity of the evidence base complicates our understanding of their role in shaping the implementation, delivery, and impact of PHC integration, and the role of contextual factors influencing their responses. This review provides insights into the diversity of the literature in terms of country contexts, stakeholders, and characteristics of integration interventions, and it identifies gaps in the literature.
Despite a 40‐year history of promoting PHC integration, especially in LMICs, and a large evidence base on implementation, we found that most qualitative academic studies on healthcare worker perceptions and experiences of PHC integration were only published since 2011, with a sharp increase since 2016. Recent growth may be due to renewed interest in PHC integration reform for universal healthcare as advocated in international health goal‐setting (Kumar 2016), as well as increased recognition of the influential role of healthcare workers as 'street‐level bureaucrats' in delivering on policy reforms (Erasmus 2011).
About 56% of studies were from HIC countries, and the remainder were from LMIC settings (with the bulk of these being from MIC settings). Of note was the dominance of some countries within HICs (nearly half were from the USA), LMICs (nearly one‐third were from South Africa), and LICs (Uganda). This dominance (especially from the USA) may be skewing the overall picture, with implications for interpreting the findings. For example, while mental health and behavioural service‐related integration was the most frequent type of health service stream (one‐third of studies), most of these were from the USA. A similar, though less dramatic skewing was seen in LMICs, with nearly one‐third of mental health studies from South Africa. In terms of geographical representation of HICs, there are few European and Nordic countries represented. For MICs, there were gaps in studies from Eastern Europe and the Russian Federation. For LICs, there were fewer studies from Asia (Middle, East, and Southeast Asia), Latin America, and from the African countries north of Sub‐Saharan Africa.
The design and implementation of PHC integration interventions are complex. They require appropriate methods for studying complex interventions, such as longitudinal and ethnographic methods, but only two studies used such methods. Further, the use of analytical models can strengthen the study design, deepen theoretical insights, and improve comparability with other studies. Still, less than one‐third of studies used an analytical model.
The minority of studies that referred to using an analytical model named 28 different models, but most of those only appeared in one study. The CFIR was referred to the most frequently (Damschroder 2009). This may indicate a growing interest in implementation science research approaches for studying integration interventions. Of interest is that just over one‐third of studies referred to using a model or conceptual framework that described the components of the integration intervention service (which we referred to as 'service models'). Some of these service models referred to generic approaches to the integration of primary care services, while others referred to integration models specific or customised for a health service (or both), such as for HIV, mental health, chronic care, and paediatric care.
The major finding in this review is the diversity of the evidence base on healthcare workers' perceptions and experience of PHC integration. There was diversity on several levels. The wide geographic spread has implications for variations in health service contexts, and the implication for how this may influence healthcare worker experience and responses. Other areas of diversity include different configurations of health service streams being integrated as well as the various client target populations who were recipients of integrated care. It is unclear if and how the experience and response of healthcare workers may differ based on the type of health service stream configurations they may be implementing. Nevertheless, it may be worth paying attention to this, as, for example, the complexity of the integrated clinical care being delivered, or the healthcare workers' attitudes to integrated service delivery for certain health services may differ. For instance, integrated delivery of mental health services (often considered more specialised by healthcare workers), with other PHC services, may be considered to have more challenges, than for instance integrated delivery of clinical care for hypertension and diabetes. The scope of integration efforts varied on a continuum of full to partial integration. Another level of diversity was the different strategies used to deliver integrated care (such as service expansion and service linkages). Further, there was diversity in the range of different stakeholders who participated in the research and, by proxy, in the delivery of integrated services; ranging from senior to frontline managers, to clinical staff in different healthcare professions and including community‐based stakeholders (such as community healthcare workers and non‐governmental organisations).
Comparison with other studies or reviews
This scoping review offers confirmatory evidence of the heterogeneity of the evidence base on PHC integration, and it goes further by characterising the nature of the heterogeneity. Such heterogeneity has been alluded to in the literature on the taxonomy of health integration interventions (Valentijn 2013; Valentijn 2015). This review identified heterogeneity for country contexts, health service streams, type/scope and strategies used, targeted client populations, and participating healthcare workers, all factors that could potentially influence the context of how healthcare workers perceive and experience PHC integration. A review of reviews on evidence‐to‐practice gaps in complex PHC interventions similarly illustrated diversity on four levels: external context, organisational mechanisms, professionals involved, and the intervention design itself (Lau 2015). The review authors concluded that the "fit" between the intervention and the context is critical in determining the success of implementation (Lau 2015). Other studies point to how different country and health system contexts shape approaches and outcomes of integration interventions (Mounier‐Jack 2017; Ryman 2012a), and suggested that greater emphasis should be placed on describing the context and articulating the relationships between the factors they identified (Lau 2015; Mounier‐Jack 2017).
Strengths and limitations
There are several limitations to our scoping review. We did not search grey literature, but the comprehensive search identified over 10,000 records for screening and many studies are included in our analysis.
We did not explicitly search databases in languages other than English, so some studies published in other languages may have been missed. We focused on English databases and identified some foreign language studies that were eligible for inclusion. Although we had assistance from colleagues and Google Translate, we are not certain of our assessments of these papers at the full‐text stage, given that it was not feasible to obtain full translations. Potentially eligible foreign language papers that we were unable to translate were thus categorised as 'awaiting classification'.
We did not undertake data extraction in duplicate due to feasibility constraints related to the very large data set. However, we performed several quality checks, detailed in the Methods section, to ensure accurate and consistent data extraction between the two main data extractors.
We found inconsistent reporting and gaps in intervention descriptions across studies. This limited the detail we could extract about the intervention descriptions. In some places, this limited our ability to accurately categorise the scope and strategies involved in delivering the intervention. The absence of standard definitions for key terms, such as full and partial integration, horizontal integration, service expansion, and service linkage, further hampered our efforts at categorisation. While we excluded interventions at the screening stage that used service co‐ordination as its core strategy, we found that many included studies used strategies that closely resembled service co‐ordination. To avoid confusion, we labelled these as 'service linkage', but there may still be overlap. In the absence of standard definitions, it will remain difficult to distinguish and categorise differences in integration scope and strategies. Limited intervention description is common in reporting on health systems and researchers may want to consider the use of frameworks to guide their reporting of interventions, such as the template for intervention description and replication (TIDieR) framework (Hoffmann 2014).
The search date was July 2020. As the review identified large numbers of included studies, we suggest that it is unlikely that additional studies published since the last search would change the review findings in important ways. Further, any future QES would be identifying further updated sources, and would most likely need to sample from their included studies, as a large number of studies would create challenges for qualitative analysis. Furthermore, it is uncertain if different types of integration strategies may have emerged had we searched grey literature.
Authors' conclusions
Implications for a subsequent qualitative evidence review
This scoping review provides a systematic, descriptive overview of the heterogeneity in qualitative literature on healthcare worker views of primary healthcare (PHC) integration, pointing to diversity in country settings, study types, target client populations, healthcare worker populations, intervention focus, scope, and strategies. It would be important for researchers and decision‐makers to understand how the diversity in PHC integration intervention design, implementation, and context may influence how healthcare workers shape PHC integration impact. Our classification of studies along various dimensions (e.g. integration focus, strategy, type of healthcare worker) can help to navigate the way the literature varies and to specify potential questions for future qualitative evidence syntheses. In the next step, a full qualitative evidence synthesis on healthcare workers' perceptions and experience of PHC integration would be informative for decision‐makers. Research investigating and synthesising evidence on healthcare workers' experience needs to take account this diversity in the evidence base by, for example, designing more focused research questions, and by paying closer attention to how the diverse characteristics of studies point to complexity and the need for more nuanced understanding of healthcare workers' perceptions and experiences of PHC integration.
Future synthesis questions to consider could include the following.
How do healthcare workers' perceptions and experience of PHC integration differ in terms of country and health service context, interventions focus, scope, and complexity of the intervention?
How do the perceptions and experiences of healthcare workers compare in terms of the different roles they play in implementing PHC integration? For example, as policymakers and planners, managers at different levels of the health systems, clinical oversight roles, frontline workers, and support staff.
How might varied management styles and approaches, resource demands, and implementation support mechanisms differ across the different approaches to integration and be shaping healthcare workers' responses to PHC integration?
What are the common models of integrated care, and how might healthcare workers' experience of integration differ across these models?
The categories in this scoping review can help identify further questions for evidence synthesis, for example, questions could focus on synthesising evidence on specific health stream integration approaches; different types and levels of complexity of the integrated care that is being delivered (e.g. mental health, non‐communicable diseases (NCDs), or broader and cross‐cutting PHC service systems); or on countries with comparable health system contexts. Another area for synthesis is studying the experience of different cadres of healthcare workers depending on their role as implementers (and recipients) of the intervention.
Categories of heterogeneity identified in this review could also help to inform the development of search terms to more accurately focus the search strategy for synthesis questions. It could also guide criteria for sampling strategies in future qualitative evidence synthesis studies.
As noted earlier, the evaluation of complex interventions such as PHC integration would benefit from in‐depth research methods, but we found only two studies that used longitudinal methods that may be better suited for in‐depth study. This has implications for future qualitative evidence syntheses that may, in the absence of such in‐depth studies, have to rely on less in‐depth data sources.
Implications for research
The complex and dynamic nature of PHC integration as a health reform requires that we produce evidence that can provide rich, in‐depth descriptions and analyses of the implementation processes and the responses of stakeholders. Key research areas to consider include:
use of more in‐depth qualitative and mixed‐method research designs. Specifically, research methods using longitudinal and ethnographic research suitable for studying complex health interventions;
use of conceptual frameworks to guide the design, implementation, and evaluation of integration interventions. Frameworks that can help to deepen insights and promote comparability across different interventions. Some of the implementation frameworks mentioned in this scoping review could present a starting point;
use of PHC integration service models for guiding the design of the integration intervention. Design of new integration interventions may gain from drawing on existing models of integrated care;
broader geographical representation in studies, in both high‐income countries and low‐ to middle‐income countries (LMICs);
with the growing burden of NCDs and comorbidity in LMICs, more NCD‐related integration research in LMICs is needed, as these were under‐represented in the literature;
expand the range of healthcare worker stakeholders studied, to increase inclusion of policymakers and managerial level staff, as well as the non‐clinical staff who may be responsible for health system support services (such as those working in human resource management, information, and supply systems);
including an equity lens in the evaluation of integration interventions;
including clients utilising integrated healthcare services. Although not the focus of this scoping review, client voices and the effects of interactions between clients and healthcare workers, are important areas for research.
History
Protocol first published: Issue 5, 2020
Acknowledgements
We thank Marit Johansen, Information Specialist from the Effective Practice and Organisation of Care (EPOC) group in Cochrane, who advised on and executed the search strategy, as well as the following editors and peer reviewers who provided comments to improve the scoping review: Simon Lewin, Claire Glenton, and the main editor, Meghan Bohren. We thank Elizabeth Paulsen for her editorial and administrative guidance and support. We thank Tracey Naledi for sharing her knowledge of integration in practice and policy in the South African healthcare system context, during the conception of the scoping review.
We thank the following colleagues in the SHAPES network who assisted us with the translation of non‐English papers: Hawa Camara (French studies), Elisabeth Paul (French studies), Carmen Klinger (German studies), Fabrizio Tediosi (Italian study), and Emma Sacks (Spanish studies); and we thank our SHAPES network colleague for the French translation.
The following people conducted the editorial process for this review.
Sign‐off Editor (final editorial decision): Simon Lewin, Norwegian University of Science and Technology.
Managing Editors (selected peer reviewers, collated peer reviewer comments, provided editorial guidance to authors, edited the article): Elizabeth Paulsen, Cochrane EPOC and Luisa Fernandez Mauleffinch, Cochrane Central Editorial Service.
Copy Editor (copyediting and production): Anne Lawson, Cochrane Central Production Service.
Peer reviewers (provided comments and recommended an editorial decision): Heather Menzies Munthe‐Kaas, Centre for Epidemic Intervention Research, Norwegian Institute of Public Health (methods review); Angela Harden, University of London (methods review); Dena Javadi, Harvard School of Public Health (clinical/content review); Steve McDonald, Cochrane Australia (search review). One of additional peer reviewers provided clinical peer review but chose not to be publicly acknowledged.
Appendices
Appendix 1. Search strategies
PDQ‐Evidence, Epistemonikos Foundation (searched 28 July 2020)
| Advanced search ‐ Title/Abstract ‐ Filter: Publication type Systematic review "integrated care" OR "integrated primary care" OR "integrated primary‐care" OR "integrated community care" OR "integrated primary health care" OR "integrated community health care" OR "integrated primary healthcare" OR "integrated community healthcare" OR "integrated primary health‐care" OR "integrated community health‐care" OR "integrated health" OR "integrated healthcare" OR "integrated health care" OR "integrated health‐care" OR "integrated medical care" OR "integrated delivery" OR "integrated system" OR "integrated systems" OR "integrated service" OR "integrated services" |
MEDLINE and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions 1946 to 24 July 2020, Ovid (searched 28 July 2020)
| # | Searches | Results |
| 1 | "Delivery of Health Care, Integrated"/ | 12687 |
| 2 | ((integrat* or coordinat* or co ordinat*) and (care or healthcare or primary health or service*)).ti. | 14867 |
| 3 | ((integrat* or coordinat* or co ordinat*) adj1 (care or healthcare or primary health)).ab,kf. | 12039 |
| 4 | ((integrat* or coordinat* or co ordinat*) adj3 service*).ab,kf. | 8349 |
| 5 | or/1‐4 | 38070 |
| 6 | Qualitative Research/ | 55570 |
| 7 | Interviews as Topic/ | 62345 |
| 8 | (qualitative or interview* or themes or mixed method?).ti,ab,kf. | 543496 |
| 9 | or/6‐8 | 562534 |
| 10 | 5 and 9 | 6236 |
Cinahl 1981 – present, EBSCOhost (searched 28 July 2020)
| S10 | S10 Limiters ‐ Exclude MEDLINE records | 4,048 |
| S9 | S10 AND S10 | 6,920 |
| S8 | S10 OR S10 OR S10 | 340,200 |
| S7 | TI ( qualitative or interview* or "thematic analysis" or themes or mixed W0 method* ) OR AB ( qualitative or interview* or "thematic analysis" or themes or mixed W0 method* ) | 301,553 |
| S6 | (MH "Thematic Analysis") | 63,603 |
| S5 | (MH "Qualitative Studies") | 113,715 |
| S4 | S1 OR S10 OR S10 | 37,263 |
| S3 | AB ( integrat* or coordinat* or co W0 ordinat*) N2 (care or healthcare or "primary health" or service*) ) | 21,579 |
| S2 | TI (integrat* or coordinat* or co W0 cordinat*) and TI (care or healthcare or "primary health" or service*) | 12,995 |
| S1 | (MH "Health Care Delivery, Integrated") | 11,680 |
Scopus, Elsevier (searched 28 July 2020) Advanced search (INDEXTERMS ("integrated health care system") OR TITLE‐ABS ("integrated care" OR "integrated primary care" OR "integrated community care" OR "integrated primary health care" OR "integrated community health care" OR "integrated primary healthcare" OR "integrated community healthcare" OR "integrated health" OR "integrated healthcare" OR "integrated health care" OR "integrated medical care") AND TITLE‐ABS‐KEY ("qualitative research" OR "qualitative study" OR "qualitative analysis" OR "thematic analysis" OR interview* OR themes OR "mixed method" OR "mixed methods")) AND NOT INDEX(medline))
Global Index Medicus, WHO (searched 28 July 2020) Advanced search ‐ in title, abstract, subject descriptor
"Delivery of Health Care, Integrated" OR "integrated care" OR "integrated primary care" OR "integrated community care" OR "integrated primary health care" OR "integrated community health care" OR "integrated primary healthcare" OR "integrated community healthcare" OR "integrated health" OR "integrated healthcare" OR "integrated health care" OR "integrated medical care" OR "integrated delivery" OR "integrated system" OR "integrated systems" OR "integrated service" OR "integrated services" AND "qualitative research" OR "qualitative study" OR "qualitative analysis" OR "thematic analysis" OR interview* OR themes OR "mixed method" OR "mixed methods"
Appendix 2. Qualitative design studies: data sources
FGD: focus group discussion; II: individual interview.
Appendix 3. Mixed‐methods design studies: data sources
FGD: focus group discussion; II: individual interview.
Appendix 4. High‐income country studies: setting
| References | Country | Urban/rural |
| Aitken 2014 | Australia | Not stated |
| Allen 2007 | Urban | |
| Banfield 2017 | Urban | |
| Beere 2019 | Urban and rural | |
| Benson 2018 | Urban and rural | |
| Douglas 2017 | Not stated | |
| Foster 2009 | Not stated | |
| Foster 2016 | Not stated | |
| Fitzpatrick 2017 | Rural | |
| Lane 2017 | Urban | |
| Lawn 2014 | Not stated | |
| Lucas 2016 | Urban and rural | |
| Hepworth 2015 | Urban | |
| McNamara 2020 | Not stated | |
| Wiese 2011 | Urban | |
| Zimbudzi 2019 | Urban | |
| Aerts 2020 | Belgium | Urban and rural |
| Benjumea‐Bedoya 2019 | Canada | Urban |
| Donnelly 2013 | Urban and rural | |
| Fleury 2016 | Urban and rural | |
| Gucciardi 2016 | Urban | |
| Harnagea 2018 | Urban and rural | |
| Ion 2017 | Urban and rural | |
| Jorgenson 2014 | Urban | |
| Malachowski 2019 | Urban | |
| Mykhalovskiy 2009 | Not stated | |
| Shrivastava 2020a | Not stated | |
| Tsasis 2012 | Not stated | |
| Wallace 2013 | Not stated | |
| Wener 2016 | Urban | |
| Gavin 2008 | Ireland | Not stated |
| Newell 2018 | Urban and rural | |
| Busch 2013 | Netherlands | Urban |
| Busetto 2015 | Not stated | |
| Nooteboom 2020 | Not stated | |
| Vestjens 2018 | Not stated | |
| Allen 1997 | New Zealand | Not stated |
| Beckingsale 2016 | Not stated | |
| Gear 2016 | Urban | |
| Treloar 2014 | Urban | |
| Shin 2018 | South Korea | Not stated |
| Jauregui 2016 | Spain | Not stated |
| Bradley 2008 | UK | Urban and rural |
| Billings 2019 | Not stated | |
| De Lusignan 2020 | Not stated | |
| Gerrish 1999 | Urban | |
| Haddow 2007 | Not stated | |
| Langer 2014 | Not stated | |
| Main 2007 | Not stated | |
| Ross 2000 | Urban and rural | |
| Savickas 2020 | Not stated | |
| Waterworth 2015 | Urban | |
| Acri 2018 | USA | Urban |
| Allen 2015 | Not stated | |
| Beehler 2017 | Not stated | |
| Bentham 2015 | Urban and rural | |
| Bentley 2015 | Not stated | |
| Berkel 2019 | Not stated | |
| Bernard 2016 | Not stated | |
| Blasi 2018 | Urban and rural | |
| Brooks 2020 | Not stated | |
| Butler 2018 | Urban | |
| Carman 2019 | Rural | |
| Cifuentes 2015 | Urban | |
| Clark 2017 | Not stated | |
| Cole 2015 | Not stated | |
| Derrett 2014 | Rural | |
| Edelman 2016 | Not stated | |
| Fong 2019 | Urban | |
| Gadomski 2014 | Urban and rural | |
| Glasgow 2012 | Not stated | |
| Greene 2016 | Not stated | |
| Hunter 2018 | Not stated | |
| Jewett 2013 | Not stated | |
| Kirchner 2004 | Rural | |
| Lombard 2009 | Urban and rural | |
| Ma 2018 | Urban | |
| Main 2007 | Urban | |
| Mayer 2016 | Not stated | |
| McGeehan 2007 | Not clear | |
| Meyer‐Kalos 2017 | Not stated | |
| Norfleet 2016 | Not stated | |
| Oishi 2003 | Urban | |
| Ojikutu 2014 | Urban | |
| Payne 2017 | Not stated | |
| Pidano 2011 | Not stated | |
| Piper 2018 | Urban | |
| Piper 2020 | Urban | |
| Ramanuj 2018 | Urban | |
| Reinschmidt 2017 | Not stated | |
| Rissi 2015 | Not stated | |
| Rodriguez 2019 | Not stated | |
| Rojas 2015 | Urban | |
| Shattell 2011 | Urban and rural | |
| Sheth 2020 | Urban | |
| Siantz 2018 | Urban | |
| Sobo 2008 | Urban | |
| Stadnick 2020 | Urban | |
| Terry 2018 | Urban | |
| Tsui 2018 | Not stated | |
| Urada 2014 | Not stated | |
| Vickers 2013 | Urban | |
| Zotti 2010 | Not stated |
Appendix 5. Middle‐income country studies: setting
| References | Country | Urban/rural |
| Aleluia 2017 | Brazil | Not stated |
| Athié 2016 | Urban | |
| De Nóbrega 2014 | Not stated | |
| Souza Gleriano 2019 | Not stated | |
| Venancio 2016 | Not clear | |
| Baker 2007 | Dominican Republic | Not stated |
| Dayton 2019 | Not clear | |
| Church 2015 | Eswatini | Urban |
| Amo‐Adjei 2014 | Ghana | Not stated |
| Anku 2020 | Not stated | |
| Sakeah 2014 | Not stated | |
| Anand 2018 | India | Not stated |
| Johnson 2020 | Urban | |
| Mishra 2014 | Rural | |
| Pereira 2011 | Not stated | |
| Porter 2002 | Not stated | |
| Surjaningrum 2018 | Indonesia | Not stated |
| Ghorbani 2018 | Iran | Urban and rural |
| Ayon 2019 | Kenya | Urban |
| Martin 2018 | Not stated | |
| Mutemwa 2013 | Urban and rural | |
| Ndwiga 2014 | Not stated | |
| Newmann 2013 | Rural | |
| Newmann 2016 | Not clear | |
| Ryman 2012c | Urban and rural | |
| Venables 2016 | Urban | |
| Young 2019 | Not stated | |
| Jacobs 2012 | Lao | Rural |
| Miguel‐Esponda 2020 | Mexico | Rural |
| Sieverding 2016 | Nigeria | Rural |
| Khan 2018 | Pakistan | Urban |
| Yessimov 2019 | Republic of Kazakhstan | Not clear |
| Ameh 2017 | South Africa | Rural |
| Burgess 2016 | Rural | |
| Gerber 2018 | Urban | |
| Hlongwa 2019 | Urban and rural | |
| Kawonga 2016 | Urban and rural | |
| Limbani 2019 | Rural | |
| Lovero 2019 | Urban and rural | |
| Marais 2015 | Not Clear | |
| Mathibe 2015 | Urban and rural | |
| Mutabazi 2020 | Not stated | |
| Nxumalo 2013 | Urban and rural | |
| Patwa 2019 | Urban | |
| Peer 2020 | Urban and rural | |
| Petersen 2009 | Rural | |
| Sinai 2018 | Rural | |
| Smit 2012 | Not stated | |
| Tshililo 2019 | Rural | |
| Uebel 2013 | Not stated | |
| Uwimana 2013 | Rural | |
| An 2015a | Tanzania | Urban and rural |
| Baker 2018 | Rural | |
| Oliff 2003 | Not stated | |
| Shelley 2019 | Urban and rural | |
| Wallace 2014 | Urban and rural | |
| Murphy 2018 | Vietnam | Urban and rural |
| Topp 2010 | Zambia | Urban |
| Topp 2013 | Not stated | |
| Zulu 2015 | Not stated | |
| Zulu 2019 | Not stated |
Appendix 6. Low‐income country studies: setting
| References | Country | Urban/rural |
| Mulenga 2019 | Democratic Republic of the Congo | Not stated |
| Nelson 2019 | Liberia | Rural |
| Cooper 2020 | Malawi | Rural |
| Duma 2019 | Not stated | |
| Robertson 2018 | Urban | |
| Geelhoed 2013 | Mozambique | Rural |
| Wilunda 2017 | South Sudan | Not stated |
| Akatukwasa 2019 | Uganda | Rural and urban |
| Mugisha 2016 | Not stated | |
| Okot‐Chono 2009 | Rural and urban | |
| Ssebunnya 2010 | Rural | |
| Wakida 2019 | Rural |
Appendix 7. Low‐ and middle‐income country studies: setting
| References | Country | Urban/rural |
| Aantjes 2014 | Ethiopia, Malawi, South Africa, and Zambia | Urban and rural |
| Petersen 2011 | South Africa and Uganda | Rural |
| Petersen 2019 | Ethiopia, India, Nepal, Nigeria, South Africa, and Uganda | Not stated |
| Pfitzer 2019 | Indian and Kenya | Urban and rural |
| Ryman 2012b | Cameroon, Ethiopia, Kenya, and Mali | Urban and rural |
Appendix 8. Mental and behavioural health‐related integration per country income level
HIC: high‐income country; LIC: low‐income country; LMIC: low‐ to middle‐income country; MIC: middle‐income country.
Appendix 9. HIV, tuberculosis, sexual and reproductive health‐related integration per country income level
| References | Country income level |
| Benjumea‐Bedoya 2019; Bernard 2016; Jewett 2013; Mykhalovskiy 2009; Ojikutu 2014; Sheth 2020; Sobo 2008; Zotti 2010 | HIC |
| An 2015a; Amo‐Adjei 2014; Anku 2020; Church 2015; Dayton 2019; Kawonga 2016; Mathibe 2015; Mutemwa 2013; Mutabazi 2020; Ndwiga 2014; Newmann 2013; Newmann 2016; Patwa 2019; Peer 2020; Porter 2002; Sinai 2018; Smit 2012; Tshililo 2019; Topp 2010; Topp 2013; Uebel 2013; Uwimana 2013; Venables 2016; Vestjens 2018; Wallace 2013 | MIC |
| Akatukwasa 2019; Duma 2019; Okot‐Chono 2009 | LIC |
| Aantjes 2014 | LMIC |
HIC: high‐income country; LIC: low‐income country; LMIC: low‐ to middle‐income country; MIC: middle‐income country.
Appendix 10. Maternal, child, and women's health‐related integration per country income level
| References | Country income level |
| Baker 2018; Jacobs 2012; Ma 2018; Martin 2018; Mishra 2014; Oliff 2003; Ryman 2012c; Sakeah 2014; Young 2019; Zulu 2019 | MIC |
| Cooper 2020; Geelhoed 2013; Nelson 2019; Robertson 2018; Wilunda 2017 | LIC |
| Pfitzer 2019; Ryman 2012b | LMIC |
LIC: low‐income country; LMIC: low‐ to middle‐income country; MIC: middle‐income country.
Appendix 11. Non‐communicable diseases‐related integration per country income level
| References | Country income level |
| Aerts 2020; Allen 2015; Banfield 2017; Busetto 2015; Foster 2016; Glasgow 2012; Gucciardi 2016; Jauregui 2016; Lucas 2016; Mayer 2016; McGeehan 2007; McNamara 2020; Newell 2018; Reinschmidt 2017; Rodriguez 2006; Rojas 2015; Vestjens 2018; Zimbudzi 2019 | HIC |
| Aleluia 2017; Ameh 2017; Anand 2018; Khan 2018; Limbani 2019; Venancio 2016 | MIC |
HIC: high‐income country; MIC: middle‐income country.
Appendix 12. General primary healthcare services‐related integration per country‐income level
| References | Country income level |
| Aitken 2014; Allen 2007; Bentley 2015; Billings 2019; Busch 2013; Carman 2019; Derrett 2014; Douglas 2017; Gerrish 1999; Haddow 2007; Lawn 2014; Main 2007; Malachowski 2019; Payne 2017; Piper 2018; Rissi 2015; Ross 2000; Tai‐Seale 2010; Treloar 2014; Waterworth 2015; Wiese 2011 | HIC |
| De Nóbrega 2014; Nxumalo 2013; Sieverding 2016; Souza Gleriano 2019; Yessimov 2019; Zulu 2015 | MIC |
HIC: high‐income country; MIC: middle‐income country.
Appendix 13. Allied and specialised‐related integration per country income‐level
| References | Country income level |
| Beckingsale 2016; Benson 2018; Bradley 2008; Cole 2015; De Lusignan 2020; Donnelly 2013; Foster 2009; Harnagea 2018; Jorgenson 2014; Lane 2017; Savickas 2020; Shin 2018; Shrivastava 2020a; Tsui 2018; Wallace 2013 | HIC |
| Baker 2007; Ghorbani 2018; Mulenga 2019 | MIC |
HIC: high‐income country; MIC: middle‐income country.
Appendix 14. Integration strategies within full and partial integration
Appendix 15. Full integration strategies across health service streams
MCWH: maternal, child, and women's health; NCD: non‐communicable disease; PHC: primary health care; SRH: sexual and reproductive health; TB: tuberculosis.
Appendix 16. Partial integration strategies across health service streams
MCWH: maternal, child, and women's health; NCD: non‐communicable disease; PHC: primary health care; SRH: sexual and reproductive health; TB: tuberculosis.
Appendix 17. Conceptual models used in the studies
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aantjes 2014.
| Study characteristics | ||
| Notes | ||
Acri 2018.
| Study characteristics | ||
| Notes | ||
Aerts 2020.
| Study characteristics | ||
| Notes | ||
Aitken 2014.
| Study characteristics | ||
| Notes | ||
Akatukwasa 2019.
| Study characteristics | ||
| Notes | ||
Aleluia 2017.
| Study characteristics | ||
| Notes | ||
Allen 1997.
| Study characteristics | ||
| Notes | ||
Allen 2007.
| Study characteristics | ||
| Notes | ||
Allen 2015.
| Study characteristics | ||
| Notes | ||
Ameh 2017.
| Study characteristics | ||
| Notes | ||
Amo‐Adjei 2014.
| Study characteristics | ||
| Notes | ||
An 2015a.
| Study characteristics | ||
| Notes | ||
An 2015b.
| Study characteristics | ||
| Notes | ||
Anand 2018.
| Study characteristics | ||
| Notes | ||
Anku 2020.
| Study characteristics | ||
| Notes | ||
Athié 2016.
| Study characteristics | ||
| Notes | ||
Ayon 2019.
| Study characteristics | ||
| Notes | ||
Baker 2007.
| Study characteristics | ||
| Notes | ||
Baker 2018.
| Study characteristics | ||
| Notes | ||
Banfield 2017.
| Study characteristics | ||
| Notes | ||
Beckingsale 2016.
| Study characteristics | ||
| Notes | ||
Beehler 2017.
| Study characteristics | ||
| Notes | ||
Beere 2019.
| Study characteristics | ||
| Notes | ||
Benjumea‐Bedoya 2019.
| Study characteristics | ||
| Notes | ||
Benson 2018.
| Study characteristics | ||
| Notes | ||
Bentham 2015.
| Study characteristics | ||
| Notes | ||
Bentley 2015.
| Study characteristics | ||
| Notes | ||
Berkel 2019.
| Study characteristics | ||
| Notes | ||
Bernard 2016.
| Study characteristics | ||
| Notes | ||
Billings 2019.
| Study characteristics | ||
| Notes | ||
Blasi 2018.
| Study characteristics | ||
| Notes | ||
Bradley 2008.
| Study characteristics | ||
| Notes | ||
Brooks 2020.
| Study characteristics | ||
| Notes | ||
Burgess 2016.
| Study characteristics | ||
| Notes | ||
Busch 2013.
| Study characteristics | ||
| Notes | ||
Busetto 2015.
| Study characteristics | ||
| Notes | ||
Butler 2018.
| Study characteristics | ||
| Notes | ||
Carman 2019.
| Study characteristics | ||
| Notes | ||
Church 2015.
| Study characteristics | ||
| Notes | ||
Cifuentes 2015.
| Study characteristics | ||
| Notes | ||
Clark 2017.
| Study characteristics | ||
| Notes | ||
Cole 2015.
| Study characteristics | ||
| Notes | ||
Cooper 2020.
| Study characteristics | ||
| Notes | ||
Davis 2015.
| Study characteristics | ||
| Notes | ||
Dayton 2019.
| Study characteristics | ||
| Notes | ||
De Lusignan 2020.
| Study characteristics | ||
| Notes | ||
De Nóbrega 2014.
| Study characteristics | ||
| Notes | ||
Derrett 2014.
| Study characteristics | ||
| Notes | ||
Donnelly 2013.
| Study characteristics | ||
| Notes | ||
Douglas 2017.
| Study characteristics | ||
| Notes | ||
Duma 2019.
| Study characteristics | ||
| Notes | ||
Dunbar 2018.
| Study characteristics | ||
| Notes | ||
Edelman 2016.
| Study characteristics | ||
| Notes | ||
Fitzpatrick 2017.
| Study characteristics | ||
| Notes | ||
Fitzpatrick 2018.
| Study characteristics | ||
| Notes | ||
Fleury 2016.
| Study characteristics | ||
| Notes | ||
Fong 2019.
| Study characteristics | ||
| Notes | ||
Foster 2009.
| Study characteristics | ||
| Notes | ||
Foster 2016.
| Study characteristics | ||
| Notes | ||
Gadomski 2014.
| Study characteristics | ||
| Notes | ||
Gavin 2008.
| Study characteristics | ||
| Notes | ||
Gear 2016.
| Study characteristics | ||
| Notes | ||
Geelhoed 2013.
| Study characteristics | ||
| Notes | ||
Gerber 2018.
| Study characteristics | ||
| Notes | ||
Gerrish 1999.
| Study characteristics | ||
| Notes | ||
Ghorbani 2018.
| Study characteristics | ||
| Notes | ||
Glasgow 2012.
| Study characteristics | ||
| Notes | ||
Greene 2016.
| Study characteristics | ||
| Notes | ||
Gucciardi 2016.
| Study characteristics | ||
| Notes | ||
Gunn 2015.
| Study characteristics | ||
| Notes | ||
Haddow 2007.
| Study characteristics | ||
| Notes | ||
Harnagea 2018.
| Study characteristics | ||
| Notes | ||
Hepworth 2015.
| Study characteristics | ||
| Notes | ||
Hlongwa 2019.
| Study characteristics | ||
| Notes | ||
Hunter 2018.
| Study characteristics | ||
| Notes | ||
Ion 2017.
| Study characteristics | ||
| Notes | ||
Jacobs 2012.
| Study characteristics | ||
| Notes | ||
Jauregui 2016.
| Study characteristics | ||
| Notes | ||
Jewett 2013.
| Study characteristics | ||
| Notes | ||
Johnson 2020.
| Study characteristics | ||
| Notes | ||
Jorgenson 2014.
| Study characteristics | ||
| Notes | ||
Kawonga 2016.
| Study characteristics | ||
| Notes | ||
Khan 2018.
| Study characteristics | ||
| Notes | ||
Kirchner 2004.
| Study characteristics | ||
| Notes | ||
Lane 2017.
| Study characteristics | ||
| Notes | ||
Langer 2014.
| Study characteristics | ||
| Notes | ||
Lawn 2014.
| Study characteristics | ||
| Notes | ||
Limbani 2019.
| Study characteristics | ||
| Notes | ||
Lombard 2009.
| Study characteristics | ||
| Notes | ||
Lovero 2019.
| Study characteristics | ||
| Notes | ||
Lucas 2016.
| Study characteristics | ||
| Notes | ||
Ma 2018.
| Study characteristics | ||
| Notes | ||
Main 2007.
| Study characteristics | ||
| Notes | ||
Malachowski 2019.
| Study characteristics | ||
| Notes | ||
Marais 2015.
| Study characteristics | ||
| Notes | ||
Martin 2018.
| Study characteristics | ||
| Notes | ||
Mathibe 2015.
| Study characteristics | ||
| Notes | ||
Mayer 2016.
| Study characteristics | ||
| Notes | ||
Mayhew 2017.
| Study characteristics | ||
| Notes | ||
McGeehan 2007.
| Study characteristics | ||
| Notes | ||
McNamara 2020.
| Study characteristics | ||
| Notes | ||
Meyer‐Kalos 2017.
| Study characteristics | ||
| Notes | ||
Miguel‐Esponda 2020.
| Study characteristics | ||
| Notes | ||
Mishra 2014.
| Study characteristics | ||
| Notes | ||
Mugisha 2016.
| Study characteristics | ||
| Notes | ||
Mulenga 2019.
| Study characteristics | ||
| Notes | ||
Murphy 2018.
| Study characteristics | ||
| Notes | ||
Mutabazi 2020.
| Study characteristics | ||
| Notes | ||
Mutemwa 2013.
| Study characteristics | ||
| Notes | ||
Mykhalovskiy 2009.
| Study characteristics | ||
| Notes | ||
Ndwiga 2014.
| Study characteristics | ||
| Notes | ||
Nelson 2019.
| Study characteristics | ||
| Notes | ||
Newell 2018.
| Study characteristics | ||
| Notes | ||
Newmann 2013.
| Study characteristics | ||
| Notes | ||
Newmann 2016.
| Study characteristics | ||
| Notes | ||
Nooteboom 2020.
| Study characteristics | ||
| Notes | ||
Norfleet 2016.
| Study characteristics | ||
| Notes | ||
Nxumalo 2013.
| Study characteristics | ||
| Notes | ||
Oishi 2003.
| Study characteristics | ||
| Notes | ||
Ojikutu 2014.
| Study characteristics | ||
| Notes | ||
Okot‐Chono 2009.
| Study characteristics | ||
| Notes | ||
Oliff 2003.
| Study characteristics | ||
| Notes | ||
Patwa 2019.
| Study characteristics | ||
| Notes | ||
Payne 2017.
| Study characteristics | ||
| Notes | ||
Peer 2020.
| Study characteristics | ||
| Notes | ||
Pereira 2011.
| Study characteristics | ||
| Notes | ||
Petersen 2009.
| Study characteristics | ||
| Notes | ||
Petersen 2011.
| Study characteristics | ||
| Notes | ||
Petersen 2019.
| Study characteristics | ||
| Notes | ||
Pfitzer 2019.
| Study characteristics | ||
| Notes | ||
Pidano 2011.
| Study characteristics | ||
| Notes | ||
Piper 2018.
| Study characteristics | ||
| Notes | ||
Piper 2020.
| Study characteristics | ||
| Notes | ||
Porter 2002.
| Study characteristics | ||
| Notes | ||
Ramanuj 2018.
| Study characteristics | ||
| Notes | ||
Reinschmidt 2017.
| Study characteristics | ||
| Notes | ||
Rissi 2015.
| Study characteristics | ||
| Notes | ||
Robertson 2018.
| Study characteristics | ||
| Notes | ||
Rodriguez 2006.
| Study characteristics | ||
| Notes | ||
Rodriguez 2019.
| Study characteristics | ||
| Notes | ||
Rojas 2015.
| Study characteristics | ||
| Notes | ||
Ross 2000.
| Study characteristics | ||
| Notes | ||
Ryman 2012b.
| Study characteristics | ||
| Notes | ||
Ryman 2012c.
| Study characteristics | ||
| Notes | ||
Sakeah 2014.
| Study characteristics | ||
| Notes | ||
Savickas 2020.
| Study characteristics | ||
| Notes | ||
Shattell 2011.
| Study characteristics | ||
| Notes | ||
Shelley 2019.
| Study characteristics | ||
| Notes | ||
Sheth 2020.
| Study characteristics | ||
| Notes | ||
Shin 2018.
| Study characteristics | ||
| Notes | ||
Shrivastava 2020a.
| Study characteristics | ||
| Notes | ||
Shrivastava 2020b.
| Study characteristics | ||
| Notes | ||
Siantz 2018.
| Study characteristics | ||
| Notes | ||
Sieverding 2016.
| Study characteristics | ||
| Notes | ||
Sinai 2018.
| Study characteristics | ||
| Notes | ||
Smit 2012.
| Study characteristics | ||
| Notes | ||
Sobo 2008.
| Study characteristics | ||
| Notes | ||
Souza 2019.
| Study characteristics | ||
| Notes | ||
Souza Gleriano 2019.
| Study characteristics | ||
| Notes | ||
Ssebunnya 2010.
| Study characteristics | ||
| Notes | ||
Stadnick 2020.
| Study characteristics | ||
| Notes | ||
Surjaningrum 2018.
| Study characteristics | ||
| Notes | ||
Tai‐Seale 2010.
| Study characteristics | ||
| Notes | ||
Terry 2018.
| Study characteristics | ||
| Notes | ||
Topp 2010.
| Study characteristics | ||
| Notes | ||
Topp 2013.
| Study characteristics | ||
| Notes | ||
Treloar 2014.
| Study characteristics | ||
| Notes | ||
Tsasis 2012.
| Study characteristics | ||
| Notes | ||
Tshililo 2019.
| Study characteristics | ||
| Notes | ||
Tsui 2018.
| Study characteristics | ||
| Notes | ||
Uebel 2013.
| Study characteristics | ||
| Notes | ||
Urada 2014.
| Study characteristics | ||
| Notes | ||
Uwimana 2013.
| Study characteristics | ||
| Notes | ||
Venables 2016.
| Study characteristics | ||
| Notes | ||
Venancio 2016.
| Study characteristics | ||
| Notes | ||
Vestjens 2018.
| Study characteristics | ||
| Notes | ||
Vickers 2013.
| Study characteristics | ||
| Notes | ||
Wakida 2018.
| Study characteristics | ||
| Notes | ||
Wakida 2019.
| Study characteristics | ||
| Notes | ||
Wallace 2013.
| Study characteristics | ||
| Notes | ||
Wallace 2014.
| Study characteristics | ||
| Notes | ||
Waterworth 2015.
| Study characteristics | ||
| Notes | ||
Wener 2016.
| Study characteristics | ||
| Notes | ||
Wiese 2011.
| Study characteristics | ||
| Notes | ||
Wilunda 2017.
| Study characteristics | ||
| Notes | ||
Yessimov 2019.
| Study characteristics | ||
| Notes | ||
Young 2019.
| Study characteristics | ||
| Notes | ||
Zimbudzi 2019.
| Study characteristics | ||
| Notes | ||
Zotti 2010.
| Study characteristics | ||
| Notes | ||
Zulu 2015.
| Study characteristics | ||
| Notes | ||
Zulu 2019.
| Study characteristics | ||
| Notes | ||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adeokun 2002 | Ineligible outcome |
| Aguirre 2013 | Ineligible population outcome |
| Aguirre‐Duarte 2015 | Ineligible intervention |
| Ahmed 2015 | Ineligible study design |
| Almeida 2018 | Ineligible intervention |
| Altabaibeh 2020 | Ineligible setting |
| Anastas 2019 | Ineligible setting |
| Anderson 2016 | Ineligible study design |
| Angus 2018 | Ineligible outcome |
| Antunes 2019 | Ineligible intervention |
| Atchison 2018 | Ineligible study design |
| Au 2018 | Ineligible intervention |
| Aufegger 2020 | Ineligible intervention |
| Aune 2014 | Ineligible intervention |
| Ayangade 1984 | Ineligible study design |
| Bagayogo 2018 | Ineligible setting |
| Bajorek 2015 | Hypothetical intervention |
| Balira 2015 | Ineligible study design |
| Baltaxe 2019 | Ineligible intervention |
| Barchi 2009 | Ineligible intervention |
| Barclay 2019 | Ineligible intervention |
| Bardwell 2019 | Ineligible intervention |
| Barraclough 2016 | Hypothetical intervention |
| Barros 2019 | Ineligible intervention |
| Bauman 2013 | Ineligible setting |
| Baxter 2002 | Ineligible intervention |
| Baxter 2009 | Ineligible intervention |
| Benzer 2015 | Ineligible setting |
| Berenson 2016 | Ineligible intervention |
| Bergmark 2018 | Ineligible outcome population |
| Bertrand 2010 | Ineligible intervention |
| Bhattacharyya 2016 | Ineligible study design |
| Blakey 2014 | Ineligible outcome population |
| Boehmer 2019 | Ineligible outcome population |
| Bourgeault 2000 | Ineligible intervention |
| Bracey 2010 | Ineligible intervention |
| Brant 2020 | Ineligible study design |
| Brechat 2018 | Ineligible study design |
| Breton 2019 | Ineligible setting |
| Brindis 2005 | Ineligible outcome |
| Briones‐Vozmediano 2018 | Ineligible setting |
| Brook 2017 | Ineligible intervention |
| Brousselle 2010 | Ineligible setting |
| Byrne 2019 | Hypothetical intervention |
| Carroll 2018 | Hypothetical intervention |
| Cash‐Gibson 2014 | Ineligible outcome |
| Catalao 2018 | Ineligible study design |
| Chubak 2012 | Hypothetical intervention |
| Coelho 2018 | Ineligible outcome population |
| Contandriopoulos 2015 | Ineligible outcome |
| Cooper 2015 | Hypothetical intervention |
| Correa 2018 | Ineligible outcome population |
| DeBoer 2019 | Hypothetical intervention |
| Dhondt 2017 | Ineligible outcome population |
| Duffy 2017 | Ineligible outcome |
| Evans 2016 | Ineligible outcome population |
| Fernandes 2014 | Ineligible outcome population |
| Freeman 2012 | Hypothetical intervention |
| French 2006 | Hypothetical intervention |
| Hallberg 2005 | Hypothetical intervention |
| Henao‐Martinez 2008 | Ineligible outcome |
| Ingram 2019 | Ineligible outcome |
| Kaehne 2016 | Ineligible outcome |
Characteristics of studies awaiting classification [ordered by study ID]
Amelung 2015.
| Notes | German study, full text was translated. However, the translated data were not sufficient for data extraction. |
Aoki 2017.
| Notes | Portuguese study, full text not translated. We could not find a translator. |
da Silva Bastos 2011.
| Notes | Portuguese study, full text not translated. We could not find a translator. |
Kondo 2014.
| Notes | Japanese study, full text was not translated. We could not find a translator. |
Rodrigues 2010.
| Notes | Portuguese study, full text was not translated. We could not find a translator. |
Ruppert 2017.
| Notes | German study, full text was translated. However, the translated data were not sufficient for data extraction. |
Santos 2011a.
| Notes | Portuguese study, full text was not translated. We could not find a translator. |
Villela 2009.
| Notes | Portuguese study, full text was not translated. We could not find a translator. |
Characteristics of ongoing studies [ordered by study ID]
Wodchis 2018.
| Study name | A research program on implementing Integrated Care for Older Adults with Complex Health Needs (iCOACH): an international collaboration |
| Starting date | |
| Contact information | walter.wodchis@utoronto.ca |
| Notes |
Differences between protocol and review
We started out with a protocol aimed at conducting a qualitative evidence synthesis (QES) of health work perceptions and experiences (Moloi 2020). However, due to the large and heterogeneous database of eligible studies, we changed to a scoping review to map the evidence base. Two of the authors on the original QES protocol (CG and TN) declined to be authors on the scoping review protocol (which is not published) and review report, for reasons of feasibility of time.
We wrote a scoping review protocol by adapting our published QES. The scoping review protocol was not published but is available as an additional file in Zenodo. We initially identified a larger number of items for extraction in our scoping review protocol, that we judged as potentially useful for understanding intervention complexity. However, for feasibility reasons, we were unable to extract all of those. The database was too large and we also we found inconsistent and limited reporting on the items. The items of interest included: timing and duration of the intervention, timing and duration of the evaluation, who were the drivers of the intervention (was it a researcher‐led or health service‐led intervention), what the clinical, professional, and organisational domains of the integration interventions were, and what the scale of the interventions was. Future reviews should consider including these items to deepen our understanding of intervention scale, scope, and complexity, and the scope of the evaluations.
We wanted to focus on use of analytical models for guiding interpretation of study findings, but for feasibility reasons, it was difficult to identify only analytical models. As mentioned in the Methods section, we consider that our method for identifying models resulted in an underestimate of studies that used 'service models' to guide their integration intervention. We became aware of this towards the end of the extraction process and decided not to redo the data extraction, but to report this as a limitation.
Some key terms were changed from those used in the scoping review protocol to allow for more useful labelling and categorising. For example, we change "healthcare worker" to "health worker" as the latter was thought to reflect the broader, non‐clinical stakeholders who participated in the studies. Other examples were changing "intervention type" to "intervention scope", and "intervention mechanisms" to "intervention strategies".
Contributions of authors
HM, NL, and KD conceptualised the review and developed the study protocol with input from review authors.
HM is the guarantor of the review.
HM and NL co‐ordinated the study process.
All review authors conducted title and abstract screening, as well as full‐text screening for the selection of studies.
HM and NL extracted and synthesised the data, and wrote the draft of the report.
KD provided methodological and analytical advice.
All review authors read, critically revised, and approved the manuscript.
Sources of support
Internal sources
-
The South African Medical Research Council of South Africa, South Africa
The South African Medical Research Council supported the time of HM, CB‐S, WO, SC, and NL.
-
The Kenya Medical Research Institute, Kenya
The Kenya Medical Research Institute supported the time of EK.
External sources
-
The Swedish International Development Cooperation Agency, Sweden
Provided financial support to NL to write the protocol.
-
The Alliance for Health Policy and Systems Research, Switzerland
Provided financial support to HM and KD to write the review.
Declarations of interest
HM: no financial conflict
KD: no financial conflict
CB‐S: no financial conflict
SC: no financial conflict
MT: no financial conflict
WO: no financial conflict
EA: no financial conflict
NL: no financial conflict
Several non‐financial issues, including personal, political, and academic factors, could have influenced the review authors' input when conducting this review. The review authors have discussed this further in the sections on reflexivity in the Methods section.
New
References
References to studies included in this review
Aantjes 2014 {published data only}
- Aantjes C, Quinlan T, Bunders J. Integration of community home based care programmes within national primary health care revitalisation strategies in Ethiopia, Malawi, South-Africa and Zambia: a comparative assessment. Globalization and Health 2014;10(11):85. [DOI: 10.1186/s12992-014-0085-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Acri 2018 {published data only}
- Acri M, Zhang S, Chomanczuk AH, O'Brien KH, De Zitella ML, Scrofani PR, et al. Barriers and facilitators to mental health screening efforts for families in pediatric primary care. Journal of Family Social Work 2018;21(3):191-9. [DOI: 10.1080/10522158.2018.1429212] [DOI] [Google Scholar]
Aerts 2020 {published data only}
- Aerts N, Bogaert P, Bastiaens H, Peremans L. Integration of nurses in general practice: a thematic synthesis of the perspectives of general practitioners, practice nurses and patients living with chronic illness. Journal of Clinical Nursing 2020;29(1-2):251-64. [DOI: 10.1111/jocn.15092] [DOI] [PubMed] [Google Scholar]
Aitken 2014 {published data only}
- Aitken K, Treuer K. Organisational and leadership competencies for successful service integration. Leadership in Health Services 2014;27(2):150-80. [DOI: 10.1108/LHS-08-2012-0028] [DOI] [Google Scholar]
Akatukwasa 2019 {published data only}
- Akatukwasa C, Bajunirwe F, Nuwamanya S, Kansime N, Aheebwe E, Tamwesigire IK. Integration of HIV-sexual reproductive health services for young people and the barriers at public health facilities in Mbarara municipality, southwestern Uganda: a qualitative assessment. International Journal of Reproductive Medicine 2019;2019(10):6725432. [DOI: 10.1155/2019/6725432] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aleluia 2017 {published data only}
- Aleluia IR, Medina MG, Almeida PF, Vilasboas AL. Care coordination in primary health care: an evaluative study in a municipality in the northeast of Brazil. Ciencia & Saude Coletiva 2017;22(6):1845-56. [DOI: 10.1590/1413-81232017226.02042017] [DOI] [PubMed] [Google Scholar]
Allen 1997 {published data only}
- Allen RE, Read J. Integrated mental health care: practitioners' perspectives. Australian & New Zealand Journal of Psychiatry 1997;31(4):496-503. [DOI: 10.3109/00048679709065071] [DOI] [PubMed] [Google Scholar]
Allen 2007 {published data only}
- Allen C, Stevens S. Health service integration: a case study in change management. Australian Health Review 2007;31(2):267-75. [DOI: 10.1071/ah070267] [DOI] [PubMed] [Google Scholar]
Allen 2015 {published data only}
- Allen CG, Escoffery C, Satsangi A, Brownstein JN. Strategies to improve the integration of community health workers into health care teams: "a little fish in a big pond". Preventing Chronic Disease 2015;12:e154. [DOI: 10.5888/pcd12.150199] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ameh 2017 {published data only}
- Ameh S, Klipstein-Grobusch K, D'Ambruoso L, Kahn K, Tollman SM, Gomez-Olive FX. Quality of integrated chronic disease care in rural South Africa: user and provider perspectives. Health Policy & Planning 2017;32(2):257-66. [DOI: 10.1093/heapol/czw118] [DOI] [PMC free article] [PubMed] [Google Scholar]
Amo‐Adjei 2014 {published data only}
- Amo-Adjei J, Kumi-Kyereme A, Fosuah Amo H, Awusabo-Asare K. The politics of tuberculosis and HIV service integration in Ghana. Social Science & Medicine 2014;117:42-9. [DOI: 10.1016/j.socscimed.2014.07.008] [DOI] [PubMed] [Google Scholar]
An 2015a {published data only}
- An SJ, George AS, LeFevre AE, Mpembeni R, Mosha I, Mohan D, et al. Supply-side dimensions and dynamics of integrating HIV testing and counselling into routine antenatal care: a facility assessment from Morogoro Region, Tanzania. BMC Health Services Research 2015;15:451. [DOI: 10.1186/s12913-015-1111-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
An 2015b {published data only}
- An SJ, George AS, LeFevre A, Mpembeni R, Mosha I, Mohan D, et al. Program synergies and social relations: implications of integrating HIV testing and counselling into maternal health care on care seeking. BMC Public Health 2015;15:24. [DOI: 10.1186/s12889-014-1336-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anand 2018 {published data only}
- Anand T, Kishore J, Isaakidis P, Gupte HA, Kaur G, Kumari S, et al. Integrating screening for non-communicable diseases and their risk factors in routine tuberculosis care in Delhi, India: a mixed-methods study. PLOS One 2018;13(8):e0202256. [DOI: 10.1371/journal.pone.0202256] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anku 2020 {published data only}
- Anku PJ, Amo-Adjei J, Doku D, Kumi-Kyereme A. Challenges of scaling-up of TB-HIV integrated service delivery in Ghana. PLOS One 2020;15(7):e0235843. [DOI: 10.1371/journal.pone.0235843] [DOI] [PMC free article] [PubMed] [Google Scholar]
Athié 2016 {published data only}
- Athié K, Lopes do Amaral Menezes A, Machado da Silva A, Campos M, Delgado PG, Fortes S, et al. Perceptions of health managers and professionals about mental health and primary care integration in Rio de Janeiro: a mixed methods study. BMC Health Services Research 2016;16(1):532. [DOI: 10.1186/s12913-016-1740-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayon 2019 {published data only}
- Ayon S, Jeneby F, Hamid F, Badhrus A, Abdulrahman T, Mburu G. Developing integrated community-based HIV prevention, harm reduction, and sexual and reproductive health services for women who inject drugs. Reproductive Health 2019;16(Suppl 1):59. [DOI: 10.1186/s12978-019-0711-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2007 {published data only}
- Baker MC, McFarland DA, Gonzales M, Diaz MJ, Molyneux DH. The impact of integrating the elimination programme for lymphatic filariasis into primary health care in the Dominican Republic. International Journal of Health Planning & Management 2007;22(4):337-52. [DOI: 10.1002/hpm.900] [DOI] [PubMed] [Google Scholar]
Baker 2018 {published data only}
- Baker U, Petro A, Marchant T, Peterson S, Manzi F, Bergström A, et al. Health workers' experiences of collaborative quality improvement for maternal and newborn care in rural Tanzanian health facilities: a process evaluation using the integrated 'Promoting Action on Research Implementation in Health Services' framework. PLOS One 2018;13(12):e0209092. [DOI: 10.1371/journal.pone.0209092] [DOI] [PMC free article] [PubMed] [Google Scholar]
Banfield 2017 {published data only}
- Banfield M, Jowsey T, Parkinson A, Douglas KA, Dawda P. Experiencing integration: a qualitative pilot study of consumer and provider experiences of integrated primary health care in Australia. BMC Family Practice 2017;18(1):2. [DOI: 10.1186/s12875-016-0575-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beckingsale 2016 {published data only}
- Beckingsale L, Fairbairn K, Morris C. Integrating dietitians into primary health care: benefits for patients, dietitians and the general practice team. Journal of Primary Health Care 2016;8(4):372-80. [DOI: 10.1071/HC16018] [DOI] [PubMed] [Google Scholar]
Beehler 2017 {published data only}
- Beehler GP, Lilienthal KR. Provider perceptions of an integrated primary care quality improvement strategy: the PPAQ toolkit. Psychological Services 2017;14(1):50-6. [DOI: 10.1037/ser0000108] [DOI] [PubMed] [Google Scholar]
Beere 2019 {published data only}
- Beere D, Page IS, Diminic S, Harris M. A mixed methods evaluation of an integrated adult mental health service model. BMC Health Services Research 2019;19(1):691. [DOI: 10.1186/s12913-019-4501-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Benjumea‐Bedoya 2019 {published data only}
- Benjumea-Bedoya D, Becker M, Haworth-Brockman M, Balakumar S, Hiebert K, Lutz JA, et al. Integrated care for latent tuberculosis infection (LTBI) at a primary health care facility for refugees in Winnipeg, Canada: a mixed-methods evaluation. Frontiers in Public Health 2019;7:57. [DOI: 10.3389/fpubh.2019.00057] [DOI] [PMC free article] [PubMed] [Google Scholar]
Benson 2018 {published data only}
- Benson H, Sabater-Hernández D, Benrimoj SI, Williams KA. Piloting the integration of non-dispensing pharmacists in the Australian general practice setting: a process evaluation. International Journal of Integrated Care 2018;18(2):4. [DOI: 10.5334/ijic.3293] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bentham 2015 {published data only}
- Bentham WD, Ratzliff A, Harrison D, Chan YF, Vannoy S, Unützer J. The experience of primary care providers with an integrated mental health care program in safety-net clinics. Family & Community Health 2015;38(2):158-68. [DOI: 10.1097/FCH.0000000000000067] [DOI] [PubMed] [Google Scholar]
Bentley 2015 {published data only}
- Bentley M, Minstrell M, Bucher H, Sproule L, Robinson A, Stirling C. Aged care nurse practitioners working in general practice. Journal of Clinical Nursing 2015;24(23-24):3745-7. [DOI: 10.1111/jocn.13066] [DOI] [PubMed] [Google Scholar]
Berkel 2019 {published data only}
- Berkel LaVerne A, Nilsson JE, Joiner AV, Stratmann S, Caldwell KK, Chong WW. Experiences of early career counseling psychologists working in integrated health care. Counseling Psychologist 2019;47(7):1037-60. [DOI: 10.1177/0011000019895495] [DOI] [Google Scholar]
Bernard 2016 {published data only}
- Bernard S, Tailor A, Jones P, Alexander DE. Addressing the medical and support service needs of people living with HIV (PLWH) through Program Collaboration and Service Integration (PCSI). Californian Journal of Health Promotion 2016;14(1):1-14. [DOI: 10.32398/cjhp.v14i1.1860] [DOI] [PMC free article] [PubMed] [Google Scholar]
Billings 2019 {published data only}
- Billings J, Mikelyte R, Coleman A, MacInnes J, Allen P, Croke S, et al. Supporting integrated care in practice: perceptions of a national support programme for the development of new care models in England. Journal of Integrated Care 2019;28(1):27-40. [DOI: 10.1108/JICA-05-2019-0018] [DOI] [Google Scholar]
Blasi 2018 {published data only}
- Blasi PR, Cromp D, McDonald S, Hsu C, Coleman K, Flinter M, et al. Approaches to behavioral health integration at high performing primary care practices. Journal of the American Board of Family Medicine 2018;31(5):691-701. [DOI: 10.3122/jabfm.2018.05.170468] [DOI] [PubMed] [Google Scholar]
Bradley 2008 {published data only}
- Bradley F, Elvey R, Ashcroft DM, Hassell K, Kendall J, Sibbald B, et al. The challenge of integrating community pharmacists into the primary health care team: a case study of local pharmaceutical services (LPS) pilots and interprofessional collaboration. Journal of Interprofessional Care 2008;22(4):387-98. [DOI: 10.1080/13561820802137005] [DOI] [PubMed] [Google Scholar]
Brooks 2020 {published data only}
- Brooks EM, Tong S. Implementing office-based opioid treatment models in primary care. Journal of American Board of Family Medicine 2020;33(4):512-20. [DOI: 10.3122/jabfm.2020.04.190240] [DOI] [PubMed] [Google Scholar]
Burgess 2016 {published data only}
- Burgess RA. Policy, power, stigma and silence: exploring the complexities of a primary mental health care model in a rural South African setting. Transcultural Psychiatry 2016;53(6):719-42. [DOI: 10.1177/1363461516679056] [DOI] [PubMed] [Google Scholar]
Busch 2013 {published data only}
- Busch V, Stel HF, De Leeuw JRJ, Melhuish E, Schrijvers AJ. Multidisciplinary integrated parent and child centres in Amsterdam: a qualitative study. International Journal of Integrated Care 2013;13:e013. [DOI: 10.5334/ijic.887] [DOI] [PMC free article] [PubMed] [Google Scholar]
Busetto 2015 {published data only}
- Busetto L, Luijkx K, Huizing A, Vrijhoef B. Implementation of integrated care for diabetes mellitus type 2 by two Dutch care groups: a case study. BMC Family Practice 2015;16:105. [DOI: 10.1186/s12875-015-0320-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Butler 2018 {published data only}
- Butler DJ, Fons D, Fisher T, Sanders J, Bodenhamer S, Owen JR, et al. A review of the benefits and limitations of a primary care-embedded psychiatric consultation service in a medically underserved setting. International Journal of Psychiatry in Medicine 2018;53(5-6):415-26. [DOI: 10.1177/0091217418791456] [DOI] [PubMed] [Google Scholar]
Carman 2019 {published data only}
- Carman AL, Vanderpool RC, Stradtman LR, Edmiston EA. A change-management approach to closing care gaps in a federally qualified health center: a rural Kentucky case study. Preventing Chronic Disease 2019;16:E105. [DOI: 10.5888/pcd16.180589] [DOI] [PMC free article] [PubMed] [Google Scholar]
Church 2015 {published data only}
- Church K, Wringe A, Lewin S, Ploubidis GB, Fakudze P, Integra Initiative, et al. Exploring the feasibility of service integration in a low-income setting: a mixed methods investigation into different models of reproductive health and HIV care in Swaziland. PLOS One 2015;10(5):e0126144. [DOI: 10.1371/journal.pone.0126144] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cifuentes 2015 {published data only}
- Cifuentes M, Davis M, Fernald D, Gunn R, Dickinson P, Cohen DJ. Electronic health record challenges, workarounds, and solutions observed in practices integrating behavioral health and primary care. Journal of the American Board of Family Medicine 2015;28(Suppl 1):S63-72. [DOI: 10.3122/jabfm.2015.S1.150133] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2017 {published data only}
- Clark KD, Miller BF, Green LA, Gruy FV, Davis M, Cohen DJ. Implementation of behavioral health interventions in real world scenarios: managing complex change. Families, Systems, & Health 2017;35(1):36-45. [DOI: 10.1037/fsh0000239] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cole 2015 {published data only}
- Cole AM, Esplin A, Baldwin LM. Adaptation of an evidence-based colorectal cancer screening program using the Consolidated Framework for Implementation Research. Preventing Chronic Disease 2015;12:E213. [DOI: 10.5888/pcd12.150300] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2020 {published data only}
- Cooper CM, Wille J, Shire S, Makoko S, Tsega A, Schuster A, et al. Integrated family planning and immunization service delivery at health facility and community sites in Dowa and Ntchisi districts of Malawi: a mixed methods process evaluation. International Journal of Environmental Research and Public Health 2020;17(12):4530. [DOI: 10.3390/ijerph17124530] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2015 {published data only}
- Davis MM, Balasubramanian BA, Cifuentes M, Hall J, Gunn R, Fernald D, et al. Clinician staffing, scheduling, and engagement strategies among primary care practices delivering integrated care. Journal of the American Board of Family Medicine 2015;28(Suppl 1):S32-40. [DOI: 10.3122/jabfm.2015.S1.150087] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dayton 2019 {published data only}
- Dayton R, Alvarez B, Morales GJ, Rojas Almonte J, Faccini M, Gomes B, et al. Assessing an inclusive model to increase access to comprehensive gender-based violence response services and improve HIV outcomes in Puerto Plata, Dominican Republic. Culture, Health & Sexuality 2019;22(9):1001-17. [DOI: 10.1080/13691058.2019.1647556] [DOI] [PubMed] [Google Scholar]
De Lusignan 2020 {published data only}
- De Lusignan S, Hoang U, Liyanage H, Tripathy M, Yonova I, Byford R, et al. Integrating molecular point-of-care testing for influenza into primary care: a mixed-methods feasibility study. British Journal of General Practice 2020;70(697):e555-62. [DOI: 10.3399/bjgp20X710897] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Nóbrega 2014 {published data only}
- De Nóbrega de Andrade RM, Montenegro de Albuquerque A, Freitas Maia JK, Pinto MB, Carvalho de Brito Santos NC. Difficulties in the implementation of the national policy of integrated health care of man. Ciencia, Cuidado e Saude 2014;13(5):642-9. [DOI: 10.4025/cienccuidsaude.v13i4.18420] [DOI] [Google Scholar]
Derrett 2014 {published data only}
- Derrett S, Gunter KE, Nocon RS, Quinn MT, Coleman K, Daniel DM, et al. How 3 rural safety net clinics integrate care for patients: a qualitative case study. Medical Care 2014;52(11 Suppl 4):S39-47. [DOI: 10.1097/MLR.0000000000000191] [DOI] [PMC free article] [PubMed] [Google Scholar]
Donnelly 2013 {published data only}
- Donnelly C, Brenchley C, Crawford C, Letts L. The integration of occupational therapy into primary care: a multiple case study design. BMC Family Practice 2013;14:60. [DOI: 10.1186/1471-2296-14-60] [DOI] [PMC free article] [PubMed] [Google Scholar]
Douglas 2017 {published data only}
- Douglas HE, Georgiou A, Tariq A, Prgomet M, Warland A, Armour P, et al. Implementing information and communication technology to support community aged care service integration: lessons from an Australian aged care provider. International Journal of Integrated Care 2017;17(1):9. [DOI: 10.5334/ijic.2437] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duma 2019 {published data only}
- Duma SE, Ngala LC. Nurses' practice of integration of HIV prevention and sexual and reproductive health services in Ntcheu District, Malawi. Curationis 2019;42(1):e1-7. [DOI: 10.4102/curationis.v42i1.1919] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunbar 2018 {published data only}
- Dunbar MS, Towe VL, Ayer L, Martineau M. Connections to Care (C2C): the perspectives of leaders at community-based organizations that are integrating mental health supports. Rand Health Quarterly 2018;7(4):7. [PMC free article] [PubMed] [Google Scholar]
Edelman 2016 {published data only}
- Edelman EJ, Hansen NB, Cutter CJ, Danton C, Fiellin LE, O'Connor PG, et al. Implementation of integrated stepped care for unhealthy alcohol use in HIV clinics. Addiction Science & Clinical Practice 2016;11(1):1. [DOI: 10.1186/s13722-015-0048-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzpatrick 2017 {published data only}
- Fitzpatrick SJ, Perkins D, Luland T, Brown D, Corvan E. The effect of context in rural mental health care: understanding integrated services in a small town. Health & Place 2017;45:70-6. [DOI: 10.1016/j.healthplace.2017.03.004] [DOI] [PubMed] [Google Scholar]
Fitzpatrick 2018 {published data only}
- Fitzpatrick SJ, Perkins D, Handley T, Brown D, Luland T, Corvan E. Coordinating mental and physical health care in rural Australia: an integrated model for primary care settings. International Journal of Integrated Care 2018;18(2):19. [DOI: 10.5334/ijic.3943] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fleury 2016 {published data only}
- Fleury MJ, Grenier G, Vallee C, Aube D, Farand L, Bamvita JM, et al. Implementation of the Quebec mental health reform (2005–2015). BMC Health Services Research 2016;16(1):586. [DOI: 10.1186/s12913-016-1832-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fong 2019 {published data only}
- Fong HF, Tamene M, Morley DS, Morris A, Estela MG, Singerman A, et al. Perceptions of the implementation of pediatric behavioral health integration in 3 community health centers. Clinical Pediatrics 2019;58(11-12):1201-11. [DOI: 10.1177/0009922819867454] [DOI] [PubMed] [Google Scholar]
Foster 2009 {published data only}
- Foster MM, Cornwell PL, Fleming JM, Mitchell GK, Tweedy SM, Hart AL, et al. Better than nothing? Restrictions and realities of enhanced primary care for allied health practitioners. Australian Journal of Primary Health 2009;15(4):326-34. [DOI: 10.1071/PY08065] [DOI] [Google Scholar]
Foster 2016 {published data only}
- Foster M, Burridge L, Donald M, Zhang J, Jackson C. The work of local healthcare innovation: a qualitative study of GP-led integrated diabetes care in primary health care organization, structure and delivery of healthcare. BMC Health Services Research 2016;16:11. [DOI: 10.1186/s12913-016-1270-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gadomski 2014 {published data only}
- Gadomski AM, Wissow LS, Palinkas L, Hoagwood KE, Daly JM, Kaye DL. Encouraging and sustaining integration of child mental health into primary care: interviews with primary care providers participating in Project TEACH (CAPES and CAP PC) in NY. General Hospital Psychiatry 2014;36(6):555-62. [DOI: 10.1016/j.genhosppsych.2014.05.013] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gavin 2008 {published data only}
- Gavin B, Cullen W, Foley S, McWilliams S, Turner N, O'Callaghan E, et al. Integrating primary care and early intervention in psychosis services: a general practitioner perspective. Early Intervention in Psychiatry 2008;2(2):103-7. [DOI: 10.1111/j.1751-7893.2008.00065.x] [DOI] [PubMed] [Google Scholar]
Gear 2016 {published data only}
- Gear C, Koziol-McLain J, Wilson D, Clark F. Developing a response to family violence in primary health care: the New Zealand experience. BMC Family Practice 2016;17(1):115. [DOI: 10.1186/s12875-016-0508-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Geelhoed 2013 {published data only}
- Geelhoed D, Lafort Y, Chissale E, Candrinho B, Degomme O. Integrated maternal and child health services in Mozambique: structural health system limitations overshadow its effect on follow-up of HIV-exposed infants. BMC Health Services Research 2013;13:207. [DOI: 10.1186/1472-6963-13-207] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gerber 2018 {published data only}
- Gerber O. Practitioners' experience of the integration of mental health into primary health care in the West Rand District, South Africa. Journal of Mental Health 2018;27(2):135-41. [DOI: 10.1080/09638237.2017.1340604] [DOI] [PubMed] [Google Scholar]
Gerrish 1999 {published data only}
- Gerrish K. Teamwork in primary care: an evaluation of the contribution of integrated nursing teams. Health & Social Care in the Community 1999;7(5):367-75. [DOI: 10.1046/j.1365-2524.1999.00199.x] [DOI] [PubMed] [Google Scholar]
Ghorbani 2018 {published data only}
- Ghorbani Z, Pakkhesal M, Arshi S, Eghbal MJ, Deghatipour M, Tennant M, et al. Challenges impeding integration of oral health into primary health care. Eastern Mediterranean Health Journal 2018;23(12):802-8. [DOI: 10.26719/2017.23.12.802] [DOI] [PubMed] [Google Scholar]
Glasgow 2012 {published data only}
- Glasgow RE, Kurz D, Dickman JM, Osuna D, Strycker L, King DK. Linking internet-based diabetes self-management to primary care: lessons learned and implications for research translation and practice implementation. Translational Behavioral Medicine 2012;2(3):313-21. [DOI: 10.1007/s13142-012-0109-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Greene 2016 {published data only}
- Greene CA, Ford JD, Ward-Zimmerman B, Honigfeld L, Pidano AE. Strengthening the coordination of pediatric mental health and medical care: piloting a collaborative model for freestanding practices. Child & Youth Care Forum 2016;45(5):729-44. [DOI: 10.1007/s10566-016-9354-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gucciardi 2016 {published data only}
- Gucciardi E, Espin S, Morganti A, Dorado L. Exploring interprofessional collaboration during the integration of diabetes teams into primary care. BMC Family Practice 2016;17:12. [DOI: 10.1186/s12875-016-0407-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gunn 2015 {published data only}
- Gunn R, Davis MM, Hall J, Heintzman J, Muench J, Smeds B, et al. Designing clinical space for the delivery of integrated behavioral health and primary care. Journal of the American Board of Family Medicine 2015;28(Suppl 1):S52-62. [DOI: 10.3122/jabfm.2015.S1.150053] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haddow 2007 {published data only}
- Haddow G, O'Donnell CA, Heaney D. Stakeholder perspectives on new ways of delivering unscheduled health care: the role of ownership and organizational identity. Journal of Evaluation in Clinical Practice 2007;13(2):179-85. [DOI: 10.1111/j.1365-2753.2006.00667.x] [DOI] [PubMed] [Google Scholar]
Harnagea 2018 {published data only}
- Harnagea H, Lamothe L, Couturier Y, Emami E. How primary health care teams perceive the integration of oral health care into their practice: a qualitative study. PLOS One 2018;13(10):e0205465. [DOI: 10.1371/journal.pone.0205465] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hepworth 2015 {published data only}
- Hepworth J, Askew D, Foley W, Duthie D, Shuter P, Combo M, et al. How an urban Aboriginal and Torres Strait Islander primary health care service improved access to mental health care. International Journal for Equity in Health 2015;14:51. [DOI: 10.1186/s12939-015-0183-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hlongwa 2019 {published data only}
- Hlongwa EN, Sibiya MN. A practice framework to enhance the implementation of the Policy on Integration of Mental Health Care into primary health care in KwaZulu-Natal province. African Journal of Primary Health Care & Family Medicine 2019;11(1):e1-8. [DOI: 10.4102/phcfm.v11i1.1865] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunter 2018 {published data only}
- Hunter SB, Ober AJ, McCullough CM, Storholm ED, Iyiewuare PO, Pham C, et al. Sustaining alcohol and opioid use disorder treatment in primary care: a mixed methods study. Implementation Science 2018;13(1):83. [DOI: 10.1186/s13012-018-0777-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ion 2017 {published data only}
- Ion A, Sunderji N, Jansz G, Ghavam-Rassoul A. Understanding integrated mental health care in "real-world" primary care settings: what matters to health care providers and clients for evaluation and improvement? Families, Systems, & Health 2017;35(3):271-82. [DOI: 10.1037/fsh0000294] [DOI] [PubMed] [Google Scholar]
Jacobs 2012 {published data only}
- Jacobs B, Lindelow M, Xayyavong P, Sackett P. Building on community outreach for childhood vaccination to deliver maternal and child health services in Laos: a feasibility assessment. Reproductive Health Matters 2012;20(40):112-21. [DOI: 10.1016/S0968-8080(12)40649-8] [DOI] [PubMed] [Google Scholar]
Jauregui 2016 {published data only}
- Jauregui ML, Silvestre C, Valdes P, Gaminde I. Qualitative evaluation of the implementation of an integrated care delivery model for chronic patients with multi-morbidity in the Basque Country. International Journal of Integrated Care 2016;16(3):9. [DOI: 10.5334/ijic.1975] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jewett 2013 {published data only}
- Jewett A, Al-Tayyib AA, Ginnett L, Smith BD. Successful integration of hepatitis C virus point-of-care tests into the Denver Metro Health Clinic. AIDS Research & Treatment 2013;2013:528904. [DOI: 10.1155/2013/528904] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2020 {published data only}
- Johnson LC, Chwastiak L, Poongothai S, Tandon N, Anjana RM, Aravind S, et al. Adaptations and patient responses to behavioral intervention components in a depression-focused chronic disease care model implemented in India. Translational Behavioral Medicine 2020;10(1):35-45. [DOI: 10.1093/tbm/ibz192] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jorgenson 2014 {published data only}
- Jorgenson D, Laubscher T, Lyons B, Palmer R. Integrating pharmacists into primary care teams: barriers and facilitators. International Journal of Pharmacy Practice 2014;22(4):292-9. [DOI: 10.1111/ijpp.12080] [DOI] [PubMed] [Google Scholar]
Kawonga 2016 {published data only}
- Kawonga M, Blaauw D, Fonn S. The influence of health system organizational structure and culture on integration of health services: the example of HIV service monitoring in South Africa. Health Policy & Planning 2016;31(9):1270-80. [DOI: 10.1093/heapol/czw061] [DOI] [PubMed] [Google Scholar]
Khan 2018 {published data only}
- Khan MA, Walley JD, Khan N, Khan MA, Ali S, King R, et al. Delivering integrated hypertension care at private health facilities in urban Pakistan: a process evaluation. BJGP Open 2018;2(4):bjgpopen18X101613. [DOI: 10.3399/bjgpopen18X101613] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirchner 2004 {published data only}
- Kirchner JE, Cody M, Thrush CR, Sullivan G, Rapp CG. Identifying factors critical to implementation of integrated mental health services in rural VA community-based outpatient clinics. Journal of Behavioral Health Services & Research 2004;31(1):13-25. [DOI: 10.1007/BF02287335] [DOI] [PubMed] [Google Scholar]
Lane 2017 {published data only}
- Lane R, Russell G, Bardoel EA, Advocat J, Zwar N, Davies PG, et al. When colocation is not enough: a case study of General Practitioner Super Clinics in Australia. Australian Journal of Primary Health 2017;23(2):107-13. [DOI: 10.1071/PY16039] [DOI] [PubMed] [Google Scholar]
Langer 2014 {published data only}
- Langer S, Chew-Graham CA, Drinkwater J, Afzal C, Keane K, Hunter C, et al. A motivational intervention for patients with COPD in primary care: qualitative evaluation of a new practitioner role. BMC Family Practice 2014;15:164. [DOI: 10.1186/1471-2296-15-164] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawn 2014 {published data only}
- Lawn S, Lloyd A, King A, Sweet L, Gum L. Integration of primary health services: being put together does not mean they will work together. BMC Research Notes 2014;7:66. [DOI: 10.1186/1756-0500-7-66] [DOI] [PMC free article] [PubMed] [Google Scholar]
Limbani 2019 {published data only}
- Limbani F, Thorogood M, Gomez-Olive FX, Kabudula C, Goudge J. Task shifting to improve the provision of integrated chronic care: realist evaluation of a lay health worker intervention in rural South Africa. BMJ Global Health 2019;4(1):e001084. [DOI: 10.1136/bmjgh-2018-001084] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lombard 2009 {published data only}
- Lombard F, Proescholdbell RJ, Cooper K, Musselwhite L, Quinlivan EB. Adaptations across clinical sites of an integrated treatment model for persons with HIV and substance abuse. AIDS Patient Care and STDs 2009;23(8):631-8. [DOI: 10.1089/apc.2008.0260] [DOI] [PubMed] [Google Scholar]
Lovero 2019 {published data only}
- Lovero KL, Lammie SL, Zyl A, Paul SN, Ngwepe P, Mootz JJ, et al. Mixed-methods evaluation of mental healthcare integration into tuberculosis and maternal-child healthcare services of four South African districts. BMC Health Services Research 2019;19(1):83. [DOI: 10.1186/s12913-019-3912-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lucas 2016 {published data only}
- Lucas E, Halcomb E, McCarthy S. Connecting care in the community: what works and what doesn't. Australian Journal of Primary Health 2016;22(6):539-44. [DOI: 10.1071/PY15141] [DOI] [PubMed] [Google Scholar]
Ma 2018 {published data only}
- Ma KP, Saw A. A qualitative study on primary care integration into an Asian immigrant-specific behavioural health setting in the United States. International Journal of Integrated Care 2018;18(3):2. [DOI: 10.5334/ijic.3719] [DOI] [PMC free article] [PubMed] [Google Scholar]
Main 2007 {published data only}
- Main R, Dunn N, Kendall K. 'Crossing professional boundaries': barriers to the integration of nurse practitioners in primary care. Education for Primary Care 2007;18(4):480-7. [DOI: 10.1080/14739879.2007.11493578] [DOI] [Google Scholar]
Malachowski 2019 {published data only}
- Malachowski C, Skopyk S, Toth K, MacEachen E. The Integrated Health Hub (IHH) model: the evolution of a community based primary care and mental health centre. Community Mental Health Journal 2019;55(4):578-88. [DOI: 10.1007/s10597-018-0339-4] [DOI] [PubMed] [Google Scholar]
Marais 2015 {published data only}
- Marais DL, Petersen I. Health system governance to support integrated mental health care in South Africa: challenges and opportunities. International Journal of Mental Health Systems 2015;9:14. [DOI: 10.1186/s13033-015-0004-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2018 {published data only}
- Martin SL, Wawire V, Ombunda H, Li T, Sklar K, Tzehaie H, et al. Integrating calcium supplementation into facility-based antenatal care services in western Kenya: a qualitative process evaluation to identify implementation barriers and facilitators. Current Developments in Nutrition 2018;2(11):nzy068. [DOI: 10.1093/cdn/nzy068] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathibe 2015 {published data only}
- Mathibe MD, Hendricks SJ, Bergh AM. Clinician perceptions and patient experiences of antiretroviral treatment integration in primary health care clinics, Tshwane, South Africa. Curationis 2015;38(1):1489. [DOI: 10.4102/curationis.v38i1.1489] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mayer 2016 {published data only}
- Mayer MK, Urlaub DM, Guzman-Corrales LM, Kowitt SD, Shea CM, Fisher EB. "They're doing something that actually no one else can do": a qualitative study of peer support and primary care integration. Journal of Ambulatory Care Management 2016;39(1):76-86. [DOI: 10.1097/JAC.0000000000000079] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mayhew 2017 {published data only}
- Mayhew SH, Sweeney S, Warren CE, Collumbien M, Ndwiga C, Mutemwa R, et al. Numbers, systems, people: how interactions influence integration. Insights from case studies of HIV and reproductive health services delivery in Kenya. Health Policy & Planning 2017;32(Suppl 4):iv67-81. [DOI: 10.1093/heapol/czx097] [DOI] [PMC free article] [PubMed] [Google Scholar]
McGeehan 2007 {published data only}
- McGeehan SK, Applebaum R. The evolving role of care management in integrated models of care. Care Management Journals 2007;8(2):64-70. [DOI: 10.1891/152109807780845591] [DOI] [PubMed] [Google Scholar]
McNamara 2020 {published data only}
- McNamara KP, Krass I, Peterson GM, Alzubaidi H, Grenfell R, Freedman B, et al. Implementing screening interventions in community pharmacy to promote interprofessional coordination of primary care – a mixed methods evaluation. Research In Social & Administrative Pharmacy 2020;16(2):160-7. [DOI: 10.1016/j.sapharm.2019.04.011] [DOI] [PubMed] [Google Scholar]
Meyer‐Kalos 2017 {published data only}
- Meyer-Kalos PS, Lee MG, Studer LM, Line TA, Fisher CM. Opportunities for integrating physical health within assertive community treatment teams: results from practitioner focus groups. Community Mental Health Journal 2017;53(3):306-15. [DOI: 10.1007/s10597-016-0043-1] [DOI] [PubMed] [Google Scholar]
Miguel‐Esponda 2020 {published data only}
- Miguel-Esponda G, Bohm-Levine N, Rodríguez-Cuevas FG, Cohen A, Kakuma R. Implementation process and outcomes of a mental health programme integrated in primary care clinics in rural Mexico: a mixed-methods study. International Journal of Mental Health Systems 2020;14:21. [DOI: 10.1186/s13033-020-00346-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2014 {published data only}
- Mishra A. 'Trust and teamwork matter': community health workers' experiences in integrated service delivery in India. Global Public Health 2014;9(8):960-74. [DOI: 10.1080/17441692.2014.934877] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mugisha 2016 {published data only}
- Mugisha J, Ssebunnya J, Kigozi FN. Towards understanding governance issues in integration of mental health into primary health care in Uganda. International Journal of Mental Health Systems 2016;10:25. [DOI: 10.1186/s13033-016-0057-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mulenga 2019 {published data only}
- Mulenga P, Boelaert M, Lutumba P, Vander Kelen C, Coppieters Y, Chenge F, et al. Integration of human African trypanosomiasis control activities into primary health services in the Democratic Republic of the Congo: a qualitative study of stakeholder perceptions. American Journal of Tropical Medicine & Hygiene 2019;100(4):899-906. [DOI: 10.4269/ajtmh.18-0382] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2018 {published data only}
- Murphy J, Corbett KK, Linh DT, Oanh PT, Nguyen VC. Barriers and facilitators to the integration of depression services in primary care in Vietnam: a mixed methods study. BMC Health Services Research 2018;18(1):641. [DOI: 10.1186/s12913-018-3416-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mutabazi 2020 {published data only}
- Mutabazi JC, Gray C, Muhwava L, Trottier H, Ware LJ, Norris S, et al. Integrating the prevention of mother-to-child transmission of HIV into primary healthcare services after AIDS denialism in South Africa: perspectives of experts and health care workers – a qualitative study. BMC Health Services Research 2020;20(1):582. [DOI: 10.1186/s12913-020-05381-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mutemwa 2013 {published data only}
- Mutemwa R, Mayhew S, Colombini M, Busza J, Kivunaga J, Ndwiga C. Experiences of health care providers with integrated HIV and reproductive health services in Kenya: a qualitative study. BMC Health Services Research 2013;13:18. [DOI: 10.1186/1472-6963-13-18] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mykhalovskiy 2009 {published data only}
- Mykhalovskiy E, Patten S, Sanders C, Bailey M, Taylor D. Conceptualizing the integration of HIV treatment and prevention: findings from a process evaluation of a community-based, national capacity-building intervention. International Journal of Public Health 2009;54(3):133-41. [DOI: 10.1007/s00038-009-8078-5] [DOI] [PubMed] [Google Scholar]
Ndwiga 2014 {published data only}
- Ndwiga C, Abuya T, Mutemwa R, Kimani JK, Colombini M, Mayhew S, et al, Integra Initiative. Exploring experiences in peer mentoring as a strategy for capacity building in sexual reproductive health and HIV service integration in Kenya. BMC Health Services Research 2014;14:98. [DOI: 10.1186/1472-6963-14-98] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2019 {published data only}
- Nelson AR, Cooper CM, Kamara S, Taylor ND, Zikeh T, Kanneh-Kesselly C, et al. Operationalizing integrated immunization and family planning services in rural Liberia: lessons learned from evaluating service quality and utilization. Global Health Science & Practice 2019;7(3):418-34. [DOI: 10.9745/GHSP-D-19-00012] [DOI] [PMC free article] [PubMed] [Google Scholar]
Newell 2018 {published data only}
- Newell E, Donnell MO. Integrated care: a qualitative study exploring GPs' and practice nurses' experiences of working with the diabetes nurse specialist. Journal of Diabetes Nursing 2018;22(6):46. [Google Scholar]
Newmann 2013 {published data only}
- Newmann SJ, Mishra K, Onono M, Bukusi EA, Cohen CR, Gage O, et al. Providers' perspectives on provision of family planning to HIV-positive individuals in HIV care in Nyanza Province, Kenya. AIDS Research & Treatment 2013;2013:915923. [DOI: 10.1155/2013/915923] [DOI] [PMC free article] [PubMed] [Google Scholar]
Newmann 2016 {published data only}
- Newmann SJ, Zakaras JM, Tao AR, Onono M, Bukusi EA, Cohen CR, et al. Integrating family planning into HIV care in western Kenya: HIV care providers' perspectives and experiences one year following integration. AIDS Care 2016;28(2):209-13. [DOI: 10.1080/09540121.2015.1080791] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nooteboom 2020 {published data only}
- Nooteboom LA, den Driesschen SI, Kuiper CH, Vermeiren Rrjm, Mulder EA. An integrated approach to meet the needs of high-vulnerable families: a qualitative study on integrated care from a professional perspective. Child and Adolescent Psychiatry and Mental Health 2020;14:18. [DOI: 10.1186/s13034-020-00321-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norfleet 2016 {published data only}
- Norfleet KR, Ratzliff AD, Chan YF, Raney LE, Unutzer J. The role of the integrated care psychiatrist in community settings: a survey of psychiatrists' perspectives. Psychiatric Services 2016;67(3):346-9. [DOI: 10.1176/appi.ps.201400592] [DOI] [PubMed] [Google Scholar]
Nxumalo 2013 {published data only}
- Nxumalo N, Goudge J, Thomas L. Outreach services to improve access to health care in South Africa: lessons from three community health worker programmes. Global Health Action 2013;6:19283. [DOI: 10.3402/gha.v6i0.19283] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oishi 2003 {published data only}
- Oishi SM, Shoai R, Katon W, Callahan C, Unutzer J, Arean P, et al, Improving Mood: Promoting Access to Collaborative Treatment Investigators. Impacting late life depression: integrating a depression intervention into primary care. Psychiatric Quarterly 2003;74(1):75-89. [DOI: 10.1023/A:1021197807029] [DOI] [PubMed] [Google Scholar]
Ojikutu 2014 {published data only}
- Ojikutu B, Holman J, Kunches L, Landers S, Perlmutter D, Ward M, et al. Interdisciplinary HIV care in a changing healthcare environment in the USA. AIDS Care 2014;26(6):731-5. [DOI: 10.1080/09540121.2013.855299] [DOI] [PubMed] [Google Scholar]
Okot‐Chono 2009 {published data only}
- Okot-Chono R, Mugisha F, Adatu F, Madraa E, Dlodlo R, Fujiwara P. Health system barriers affecting the implementation of collaborative TB-HIV services in Uganda. International Journal of Tuberculosis and Lung Disease 2009;13(8):955-61. [PubMed] [Google Scholar]
Oliff 2003 {published data only}
- Oliff M, Mayaud P, Brugha R, Semakafu AM. Integrating reproductive health services in a reforming health sector: the case of Tanzania. Reproductive Health Matters 2003;11(21):37-48. [DOI: 10.1016/S0968-8080(03)02174-8] [DOI] [PubMed] [Google Scholar]
Patwa 2019 {published data only}
- Patwa MC, Bassett J, Holmes L, Mutunga L, Mudavanhu M, Makhomboti T, et al. Integrating safer conception services into primary care: providers' perspectives. BMC Public Health 2019;19(1):532. [DOI: 10.1186/s12889-019-6904-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Payne 2017 {published data only}
- Payne J, Razi S, Emery K, Quattrone W, Tardif-Douglin M. Integrating community health workers (CHWs) into health care organizations. Journal of Community Health 2017;42(5):983-90. [DOI: 10.1007/s10900-017-0345-4] [DOI] [PubMed] [Google Scholar]
Peer 2020 {published data only}
- Peer N, Villiers A, Jonathan D, Kalombo C, Kengne AP. Care and management of a double burden of chronic diseases: experiences of patients and perceptions of their healthcare providers. PLOS One 2020;15(7):e0235710. [DOI: 10.1371/journal.pone.0235710] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pereira 2011 {published data only}
- Pereira B, Andrew G, Pednekar S, Kirkwood BR, Patel V. The integration of the treatment for common mental disorders in primary care: experiences of health care providers in the MANAS trial in Goa, India. International Journal of Mental Health Systems 2011;5(1):26. [DOI: 10.1186/1752-4458-5-26] [DOI] [PMC free article] [PubMed] [Google Scholar]
Petersen 2009 {published data only}
- Petersen I, Bhana A, Campbell-Hall V, Mjadu S, Lund C, Kleintjies S, et al, Mental Health and Poverty Research Programme Consortium. Planning for district mental health services in South Africa: a situational analysis of a rural district site. Health Policy & Planning 2009;24(2):140-50. [DOI: 10.1093/heapol/czn049] [DOI] [PubMed] [Google Scholar]
Petersen 2011 {published data only}
- Petersen I, Ssebunnya J, Bhana A, Baillie K, MhaPP Research Programme Consortium. Lessons from case studies of integrating mental health into primary health care in South Africa and Uganda. International Journal of Mental Health Systems 2011;5:8. [DOI: 10.1186/1752-4458-5-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Petersen 2019 {published data only}
- Petersen I, Rensburg A, Kigozi F, Semrau M, Hanlon C, Abdulmalik J, et al. Scaling up integrated primary mental health in six low- and middle-income countries: obstacles, synergies and implications for systems reform. BJPsych Open 2019;5(5):e69. [DOI: 10.1192/bjo.2019.7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfitzer 2019 {published data only}
- Pfitzer A, Maly C, Tappis H, Kabue M, Mackenzie D, Healy S, et al. Characteristics of successful integrated family planning and maternal and child health services: findings from a mixed-method, descriptive evaluation. F1000Research 2019;8:229. [DOI: 10.12688/f1000research.17208.2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pidano 2011 {published data only}
- Pidano AE, Marcaly KH, Ihde KM, Kurowski EC, Whitcomb JM. Connecticut's enhanced care clinic initiative: early returns from pediatric-behavioral health partnerships. Families, Systems, & Health 2011;29(2):138-43. [DOI: 10.1037/a0023474] [DOI] [PubMed] [Google Scholar]
Piper 2018 {published data only}
- Piper CN, Plescia M, Keener SR, DeHaven M. The Mecklenburg County Interlocal Agreement: an 18-year collaboration between medicine and public health. Journal of Public Health Management & Practice 2018;24(1):e1-7. [DOI: 10.1097/PHH.0000000000000531] [DOI] [PubMed] [Google Scholar]
Piper 2020 {published data only}
- Piper KN, Schiff J, Riddick C, Getachew B, Farber EW, Kalokhe A, et al. Barriers and facilitators to implementation of trauma support services at a large HIV treatment center in the Southern United States. AIDS Care 2020;33(3):316-25. [DOI: 10.1080/09540121.2020.1764473] [DOI] [PMC free article] [PubMed] [Google Scholar]
Porter 2002 {published data only}
- Porter JD, Ogden JA, Rao PV, Rao VP, Rajesh D, Buskade RA, et al. Lessons in integration--operations research in an Indian leprosy NGO. Leprosy Review 2002;73(2):147-59. [PubMed] [Google Scholar]
Ramanuj 2018 {published data only}
- Ramanuj PP, Talley R, Breslau J, Wang SS, Pincus HA. Integrating behavioral health and primary care services for people with serious mental illness: a qualitative systems analysis of integration in New York. Community Mental Health Journal 2018;54(8):1116-26. [DOI: 10.1007/s10597-018-0251-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinschmidt 2017 {published data only}
- Reinschmidt KM, Ingram M, Morales S, Sabo SJ, Blackburn J, Murrieta L, et al. Documenting community health worker roles in primary care: contributions to evidence-based integration into health care teams, 2015. Journal of Ambulatory Care Management 2017;40(4):305-15. [DOI: 10.1097/JAC.0000000000000178] [DOI] [PubMed] [Google Scholar]
Rissi 2015 {published data only}
- Rissi JJ, Gelmon S, Saulino E, Merrithew N, Baker R, Hatcher P. Building the foundation for health system transformation: Oregon's Patient-Centered Primary Care Home program. Journal of Public Health Management & Practice 2015;21(1):34-41. [DOI: 10.1097/PHH.0000000000000083] [DOI] [PubMed] [Google Scholar]
Robertson 2018 {published data only}
- Robertson SK, Manson K, Fioratou E. IMCI and ETAT integration at a primary healthcare facility in Malawi: a human factors approach. BMC Health Services Research 2018;18(1):1014. [DOI: 10.1186/s12913-018-3803-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rodriguez 2006 {published data only}
- Rodriguez C, Contandriopoulos AP, Larouche D. Implementation evaluation of an integrated healthcare delivery initiative for diabetic patients. Healthcare Policy 2006;1(3):99-120. [PMC free article] [PubMed] [Google Scholar]
Rodriguez 2019 {published data only}
- Rodriguez EM, Gulbas LE, George-Jones J, Leija A, Burrows D, Neavel C. Interdisciplinary perspectives on an integrated behavioral health model of psychiatry in pediatric primary care: a community-based participatory research study. Community Mental Health Journal 2019;55(4):569-77. [DOI: 10.1007/s10597-018-0330-0] [DOI] [PubMed] [Google Scholar]
Rojas 2015 {published data only}
- Rojas E, Gerber BS, Tilton J, Rapacki L, Sharp LK. Pharmacists' perspectives on collaborating with community health workers in diabetes care. Journal of the American Pharmacists Association 2015;55(4):429-33. [DOI: 10.1331/JAPhA.2015.14123] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2000 {published data only}
- Ross F, Rink E, Furne A. Integration or pragmatic coalition? An evaluation of nursing teams in primary care. Journal of Interprofessional Care 2000;14(3):259-67. [DOI: 10.1080/jic.14.3.259.267] [DOI] [Google Scholar]
Ryman 2012b {published data only}
- Ryman TK, Wallace A, Mihigo R, Richards P, Schlanger K, Cappelier K, et al. Community and health worker perceptions and preferences regarding integration of other health services with routine vaccinations: four case studies. Journal of Infectious Diseases 2012;205(Suppl 1):S49-55. [DOI: 10.1093/infdis/jir796] [DOI] [PubMed] [Google Scholar]
Ryman 2012c {published data only}
- Ryman TK, Briere EC, Cartwright E, Schlanger K, Wannemuehler KA, Russo ET, et al. Integration of routine vaccination and hygiene interventions: a comparison of 2 strategies in Kenya. Journal of Infectious Diseases 2012;205(Suppl 1):S65-76. [DOI: 10.1093/infdis/jir777] [DOI] [PubMed] [Google Scholar]
Sakeah 2014 {published data only}
- Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reproductive Health 2014;11:90. [DOI: 10.1186/1742-4755-11-90] [DOI] [PMC free article] [PubMed] [Google Scholar]
Savickas 2020 {published data only}
- Savickas V, Veale EL, Bhamra SK, Stewart AJ, Mathie A, Corlett S. Pharmacists detecting atrial fibrillation in general practice: a qualitative focus group study. British Journal of General Practice 2020;4(3):23. [DOI: 10.3399/bjgpopen20X101042] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shattell 2011 {published data only}
- Shattell MM, Donnelly N, Scheyett A, Cuddeback GS. Assertive community treatment and the physical health needs of persons with severe mental illness: issues around integration of mental health and physical health. Journal of the American Psychiatric Nurses Association 2011;17(1):57-63. [DOI: 10.1177/1078390310393737] [DOI] [PubMed] [Google Scholar]
Shelley 2019 {published data only}
- Shelley KD, Frumence G, Mpembeni R, Mwinnyaa G, Joachim J, Kisusi HK, et al. "Because even the person living with HIV/AIDS might need to make babies" – perspectives on the drivers of feasibility and acceptability of an integrated community health worker model in Iringa, Tanzania. International Journal of Health Policy & Management 2019;8(9):538-49. [DOI: 10.15171/ijhpm.2019.38] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheth 2020 {published data only}
- Sheth AN, Hussen SA, Escoffery C, Haddad LB, Powell L, Brown N, et al. Pre-exposure prophylaxis integration into family planning services at Title X Clinics in the Southeastern United States: protocol for a mixed methods hybrid type I effectiveness implementation study (Phase 2 ATN 155). JMIR Research Protocol 2020;9(9):e18784. [DOI: 10.2196/18784] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shin 2018 {published data only}
- Shin DS, Choi YJ. A pilot study of team-based primary health care for people with disabilities in South Korea. Journal of Interprofessional Care 2018;33(1):129-32. [DOI: 10.1080/13561820.2018.1531832] [DOI] [PubMed] [Google Scholar]
Shrivastava 2020a {published data only}
- Shrivastava R, Couturier Y, Girard F, Bedos C, Macdonald ME, Torrie J, et al. Appreciative inquiry in evaluating integrated primary oral health services in Quebec Cree communities: a qualitative multiple case study. Dentistry and Oral Medicine 2020;10(6):e038164. [DOI: 10.1136/bmjopen-2020-038164] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shrivastava 2020b {published data only}
- Shrivastava R, Campeau R, Couturier Y, Torrie J, Girard F, Marie-Pierre B, et al. Anthropological perspectives on Miyupimaatisiiun and the integration of oral health in primary care in the Cree communities of Northern Quebec. PLOS One 2020;15(4):e0231406. [DOI: 10.1371/journal.pone.0231406] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siantz 2018 {published data only}
- Siantz E, Henwood B, Baezcondi-Garbanati L. From physical wellness to cultural brokering: unpacking the roles of peer providers in integrated health care settings. Community Mental Health Journal 2018;54(8):1127-35. [DOI: 10.1007/s10597-018-0320-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sieverding 2016 {published data only}
- Sieverding M, Beyeler N. Integrating informal providers into a people-centered health systems approach: qualitative evidence from local health systems in rural Nigeria. BMC Health Services Research 2016;16(1):526. [DOI: 10.1186/s12913-016-1780-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinai 2018 {published data only}
- Sinai I, Cleghorn F, Kinkel HF. Improving management of tuberculosis in people living with HIV in South Africa through integration of HIV and tuberculosis services: a proof of concept study. BMC Health Services Research 2018;18(1):711. [DOI: 10.1186/s12913-018-3524-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smit 2012 {published data only}
- Smit JA, Church K, Milford C, Harrison AD, Beksinska ME. Key informant perspectives on policy- and service-level challenges and opportunities for delivering integrated sexual and reproductive health and HIV care in South Africa. BMC Health Services Research 2012;12:48. [DOI: 10.1186/1472-6963-12-48] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sobo 2008 {published data only}
- Sobo EJ, Bowman C, Halloran J, Asch SM, Goetz MB, Gifford AL. 'A routine thing': clinician strategies for implementing HIV testing for at-risk patients in a busy healthcare organisation (and implications for implementation of other new practice recommendations). Anthropology & Medicine 2008;15(3):213-25. [DOI: 10.1080/13648470802357489] [DOI] [PubMed] [Google Scholar]
Souza 2019 {published data only}
- Souza AC, Amarante PD, Abrahao AL. Inclusion of mental health in primary health care: care strategy in the territory. Revista Brasileira de Enfermagem 2019;72(6):1677-82. [DOI: 10.1590/0034-7167-2018-0806] [DOI] [PubMed] [Google Scholar]
Souza Gleriano 2019 {published data only}
- Souza Gleriano J, da Luz Zaiaz PC, Pereira Borges A, Lucietto GC, Balderrama P, Almeida Corrêa CR, et al. Integral care in the perception of family health strategy professionals. Journal of Nursing 2019;13:1170-8. [DOI: 10.5205/1981-8963.2019.242241] [DOI] [Google Scholar]
Ssebunnya 2010 {published data only}
- Ssebunnya J, Kigozi F, Kizza D, Ndyanabangi S, MHAPP Research Programme Consortium. Integration of mental health into primary health care in a rural district in Uganda. African Journal of Psychiatry 2010;13(2):128-31. [DOI: 10.4314/ajpsy.v13i2.54359] [DOI] [PubMed] [Google Scholar]
Stadnick 2020 {published data only}
- Stadnick NA, Martinez K, Aarons GA, Lee DA, Cleave J, Brookman-Frazee L. Pediatric primary care perspectives on integrated mental health care for autism. Academic Pediatrics 2020;20(8):1140-7. [DOI: 10.1016/j.acap.2020.03.006] [DOI] [PMC free article] [PubMed] [Google Scholar]
Surjaningrum 2018 {published data only}
- Surjaningrum ER, Minas H, Jorm AF, Kakuma R. The feasibility of a role for community health workers in integrated mental health care for perinatal depression: a qualitative study from Surabaya, Indonesia. International Journal of Mental Health Systems 2018;12(31):27. [DOI: 10.1186/s13033-018-0208-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tai‐Seale 2010 {published data only}
- Tai-Seale M, Kunik ME, Shepherd A, Kirchner J, Gottumukkala A. A case study of early experience with implementation of collaborative care in the Veterans Health Administration. Population Health Management 2010;13(6):331-7. [DOI: 10.1089/pop.2009.0082] [DOI] [PMC free article] [PubMed] [Google Scholar]
Terry 2018 {published data only}
- Terry V, Sandoval A, Garza J, Lowdermilk J, Lerma E, Lapka S, et al. What drives members of an interprofessional care team: a sense of self. Journal of Interprofessional Education and Practice 2018;13:27-32. [DOI: 10.1016/j.xjep.2018.08.009] [DOI] [Google Scholar]
Topp 2010 {published data only}
- Topp SM, Chipukuma JM, Giganti M, Mwango LK, Chiko LM, Tambatamba-Chapula B, et al. Strengthening health systems at facility-level: feasibility of integrating antiretroviral therapy into primary health care services in Lusaka, Zambia. PLOS One 2010;5(7):e11522. [DOI: 10.1371/journal.pone.0011522] [DOI] [PMC free article] [PubMed] [Google Scholar]
Topp 2013 {published data only}
- Topp SM, Chipukuma JM, Chiko MM, Matongo E, Bolton-Moore C, Reid SE. Integrating HIV treatment with primary care outpatient services: opportunities and challenges from a scaled-up model in Zambia. Health Policy & Planning 2013;28(4):347-57. [DOI: 10.1093/heapol/czs065] [DOI] [PMC free article] [PubMed] [Google Scholar]
Treloar 2014 {published data only}
- Treloar C, Gray R, Brener L. A piece of the jigsaw of primary care: health professional perceptions of an integrated care model of hepatitis C management in the community. Journal of Primary Health Care 2014;6(2):129-34. [DOI: 10.1071/HC14129] [DOI] [PubMed] [Google Scholar]
Tsasis 2012 {published data only}
- Tsasis P, Evans JM, Owen S. Reframing the challenges to integrated care: a complex-adaptive systems perspective. International Journal of Integrated Care 2012;12:e190. [DOI: 10.5334/ijic.843] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tshililo 2019 {published data only}
- Tshililo AR, Mangena-Netshikweta L, Nemathaga LH, Maluleke M. Challenges of primary healthcare nurses regarding the integration of HIV and AIDS services into primary healthcare in Vhembe district of Limpopo province, South Africa. Curationis 2019;42(1):e1-6. [DOI: 10.4102/curationis.v42i1.1849] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsui 2018 {published data only}
- Tsui J, Hudson SV, Rubinstein EB, Howard J, Hicks E, Kieber-Emmons A, et al. A mixed-methods analysis of the capacity of the Patient-Centered Medical Home to implement care coordination services for cancer survivors. Translational Behavioral Medicine 2018;8(3):319-27. [DOI: 10.1093/tbm/ibx059] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uebel 2013 {published data only}
- Uebel K, Guise A, Georgeu D, Colvin C, Lewin S. Integrating HIV care into nurse-led primary health care services in South Africa: a synthesis of three linked qualitative studies. BMC Health Services Research 2013;13:171. [DOI: 10.1186/1472-6963-13-171] [DOI] [PMC free article] [PubMed] [Google Scholar]
Urada 2014 {published data only}
- Urada D, Teruya C, Gelberg L, Rawson R. Integration of substance use disorder services with primary care: health center surveys and qualitative interviews. Substance Abuse Treatment, Prevention, & Policy 2014;9:15. [DOI: 10.1186/1747-597X-9-15] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uwimana 2013 {published data only}
- Uwimana J, Jackson D. Integration of tuberculosis and prevention of mother-to-child transmission of HIV programmes in South Africa. International Journal of Tuberculosis & Lung Disease 2013;17(10):1285-90. [DOI: 10.5588/ijtld.12.0068] [DOI] [PubMed] [Google Scholar]
Venables 2016 {published data only}
- Venables E, Edwards JK, Baert S, Etienne W, Khabala K, Bygrave H. "They just come, pick and go." The acceptability of integrated medication adherence clubs for HIV and non communicable disease (NCD) patients in Kibera, Kenya. PLOS One 2016;11(10):e0164634. [DOI: 10.1371/journal.pone.0164634] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venancio 2016 {published data only}
- Venancio SI, da Costa Rosa TE, Sanches Bersusa AA. Comprehensive care to hypertension and diabetes mellitus: implementation of the Care Line in a Health Region of São Paulo, Brazil [Atenção integral à hipertensão arterial e diabetes mellitus: implementação da Linha de Cuidado em uma Região de Saúde do estado de São Paulo, Brasil]. Physis 2016;26(1):113-35. [DOI: 10.1590/S0103-73312016000100008] [DOI] [Google Scholar]
Vestjens 2018 {published data only}
- Vestjens L, Cramm JM, Nieboer AP. An integrated primary care approach for frail community-dwelling older persons: a step forward in improving the quality of care. BMC Health Services Research 2018;18(1):28. [DOI: 10.1371/journal.pone.0164634] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vickers 2013 {published data only}
- Vickers KS, Ridgeway JL, Hathaway JC, Egginton JS, Kaderlik AB, Katzelnick DJ. Integration of mental health resources in a primary care setting leads to increased provider satisfaction and patient access. General Hospital Psychiatry 2013;35(5):461-7. [DOI: 10.1016/j.genhosppsych.2013.06.011] [DOI] [PubMed] [Google Scholar]
Wakida 2018 {published data only}
- Wakida EK, Obua C, Rukundo GZ, Maling S, Talib ZM, Okello ES. Barriers and facilitators to the integration of mental health services into primary healthcare: a qualitative study among Ugandan primary care providers using the COM-B framework. BMC Health Services Research 2018;18(1):890. [DOI: 10.1186/s12913-018-3684-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wakida 2019 {published data only}
- Wakida EK, Okello ES, Rukundo GZ, Akena D, Alele PE, Talib ZM, et al. Health system constraints in integrating mental health services into primary healthcare in rural Uganda: perspectives of primary care providers. International Journal of Mental Health Systems 2019;13:16. [DOI: 10.1186/s13033-019-0272-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 2013 {published data only}
- Wallace BB, MacEntee MI, Harrison R, Hole R, Mitton C. Community dental clinics: providers' perspectives. Community Dentistry & Oral Epidemiology 2013;41(3):193-203. [DOI: 10.1111/cdoe.12012] [DOI] [PubMed] [Google Scholar]
Wallace 2014 {published data only}
- Wallace A, Kimambo S, Dafrossa L, Rusibamayila N, Rwebembera A, Songoro J, et al. Qualitative assessment of the integration of HIV services with infant routine immunization visits in Tanzania. Journal of Acquired Immune Deficiency Syndromes 2014;66(1):e8-14. [DOI: 10.1097/QAI.0000000000000078] [DOI] [PMC free article] [PubMed] [Google Scholar]
Waterworth 2015 {published data only}
- Waterworth C, Willcocks S, Selfe J, Roddam H. Implementing care aims in an integrated team. British Journal of Healthcare Management 2015;21(1):36-45. [DOI: 10.12968/bjhc.2015.21.1.36] [DOI] [Google Scholar]
Wener 2016 {published data only}
- Wener P, Woodgate RL. Collaborating in the context of co-location: a grounded theory study. BMC Family Practice 2016;17:30. [DOI: 10.1186/s12875-016-0427-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiese 2011 {published data only}
- Wiese M, Jolley G, Baum F, Freeman T, Kidd M. Australia's systems of primary healthcare – the need for improved coordination and implications for Medicare locals. Australian Family Physician 2011;40(12):995-9. [PubMed] [Google Scholar]
Wilunda 2017 {published data only}
- Wilunda C, Dall'Oglio G, Scanagatta C, Segafredo G, Lukhele BW, Takahashi R, et al. Changing the role of traditional birth attendants in Yirol West County, South Sudan. PLOS One 2017;12(11):e0185726. [DOI: 10.1371/journal.pone.0185726] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yessimov 2019 {published data only}
- Yessimov N, Aringazina A, Tokmurziyeva G, Izmailova N, Seidumanov D. Assessment of the integration between primary health care and public health in Almaty. Research Journal of Pharmacy and Technology 2019;12(9):4241-9. [DOI: 10.5958/0974-360X.2019.00729.7] [DOI] [Google Scholar]
Young 2019 {published data only}
- Young N, Achieng F, Desai M, Phillips-Howard P, Hill J, Aol G, et al. Integrated point-of-care testing (POCT) for HIV, syphilis, malaria and anaemia at antenatal facilities in western Kenya: a qualitative study exploring end-users' perspectives of appropriateness, acceptability and feasibility. BMC Health Services Research 2019;19(1):74. [DOI: 10.1186/s12913-018-3844-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zimbudzi 2019 {published data only}
- Zimbudzi E, Lo C, Robinson T, Ranasinha S, Teede HJ, Usherwood T, et al. The impact of an integrated diabetes and kidney service on patients, primary and specialist health professionals in Australia: a qualitative study. PLOS One 2019;14(7):e0219685. [DOI: 10.1371/journal.pone.0219685] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zotti 2010 {published data only}
- Zotti ME, Pringle J, Stuart G, Boyd WA, Brantley D, Ravello L. Integrating HIV prevention in reproductive health settings. Journal of Public Health Management & Practice 2010;16(6):512-20. [DOI: 10.1097/PHH.0b013e3181ef1935] [DOI] [PubMed] [Google Scholar]
Zulu 2015 {published data only}
- Zulu JM, Hurtig AK, Kinsman J, Michelo C. Innovation in health service delivery: integrating community health assistants into the health system at district level in Zambia. BMC Health Services Research 2015;15:38. [DOI: 10.1186/s12913-015-0696-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zulu 2019 {published data only}
- Zulu JM, Kinsman J, Hurtig AK, Michelo C, George A, Schneider H. Integrating community health assistant-driven sexual and reproductive health services in the community health system in Nyimba district in Zambia: mapping key actors, points of integration, and conditions shaping the process. Reproductive Health 2019;16(1):122. [DOI: 10.1186/s12978-019-0788-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adeokun 2002 {published data only}
- Adeokun L, Mantell JE, Weiss E, Delano GE, Jagha T, Olatoregun J, et al. Promoting dual protection in family planning clinics in Ibadan, Nigeria. International Family Planning Perspectives 2002;28(2):87-95. [DOI: 10.2307/3088240] [DOI] [Google Scholar]
Aguirre 2013 {published data only}
- Aguirre J, Carrion VG. Integrated behavioral health services: a collaborative care model for pediatric patients in a low-income setting. Clinical Pediatrics 2013;52(12):1178-80. [DOI: 10.1177/0009922812470744] [DOI] [PubMed] [Google Scholar]
Aguirre‐Duarte 2015 {published data only}
- Aguirre-Duarte NA. Increasing collaboration between health professionals: clues and challenges. Colombia Medica 2015;46(2):66-70. [DOI: 10.25100/cm.v46i2.1526] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahmed 2015 {published data only}
- Ahmed S, Ware P, Visca R, Bareil C, Chouinard MC, Desforges J, et al. The prevention and management of chronic disease in primary care: recommendations from a knowledge translation meeting Health Services Research. BMC Research Notes 2015;8:571. [DOI: 10.1186/s13104-015-1514-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Almeida 2018 {published data only}
- Almeida PF de, Oliveira SC de, Giovanella L. Network integration and care coordination: the case of Chile's health system [Integração de rede e coordenação do cuidado: o caso do sistema de saúde do Chile]. Ciênc Saúde Colet 2018;23(7):2213-28. [DOI: 10.1590/1413-81232018237.09622018] [DOI] [PubMed] [Google Scholar]
Altabaibeh 2020 {published data only}
- Altabaibeh A, Caldwell KA, Volante MA. Tracing healthcare organisation integration in the UK using actor–network theory. Journal of Health Organization and Management 2020;34(2):192-206. [DOI: 10.1108/JHOM-12-2019-0339] [DOI] [PubMed] [Google Scholar]
Anastas 2019 {published data only}
- Anastas T, Needham Waddell E, Howk S, Remiker M, Horton-Dunbar G, Fagnan LJ. Building behavioral health homes: clinician and staff perspectives on creating integrated care teams. Journal of Behavioral Health Services & Research 2019;46(3):475-86. [DOI: 10.1007/s11414-018-9622-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 2016 {published data only}
- Anderson K, Bird M, Blair A, MacPherson S. Development and effectiveness of an integrated inpatient and community service for challenging behaviour in late life: from confused and disturbed elderly to transitional behavioural assessment and intervention service. Dementia 2016;15(6):1340-57. [DOI: 10.1177/1471301214559106] [DOI] [PubMed] [Google Scholar]
Angus 2018 {published data only}
- Angus L, Valentijn PP. From micro to macro: assessing implementation of integrated care in Australia. Australian Journal of Primary Health 2018;24(1):59-65. [DOI: 10.1071/PY17024] [DOI] [PubMed] [Google Scholar]
Antunes 2019 {published data only}
- Antunes A, Frasquilho D, Zózimo JR, Silva M, Cardoso G, Ferrão J, et al. Solutions to tackle the mental health consequences of the economic recession: a qualitative study integrating primary health care users and professionals' perspectives. Health Policy 2019;123(12):1267-74. [DOI: 10.1016/j.healthpol.2019.10.003] [DOI] [PubMed] [Google Scholar]
Atchison 2018 {published data only}
- Atchison KA, Weintraub JA, Rozier RG. Bridging the dental-medical divide: case studies integrating oral health care and primary health care. Journal of the American Dental Association 2018;149(10):850-8. [DOI: 10.1016/j.adaj.2018.05.030] [DOI] [PubMed] [Google Scholar]
Au 2018 {published data only}
- Au M, Kehn M, Ireys H, Blyler C, Brown J. Care coordinators in integrated care: burnout risk, perceived supports, and job satisfaction. American Journal of Preventive Medicine 2018;54(6 Suppl 3):S250-7. [DOI: 10.1016/j.amepre.2018.01.044] [DOI] [PubMed] [Google Scholar]
Aufegger 2020 {published data only}
- Aufegger L, Alabi M, Darzi A, Bicknell C. Sharing leadership: current attitudes, barriers and needs of clinical and non-clinical managers in UK's integrated care system. BMJ Leader 2020;4:128-34. [DOI: 10.1136/leader-2020-000228] [DOI] [Google Scholar]
Aune 2014 {published data only}
- Aune I, Olufsen V. 'From fragmented to interdisciplinary understanding of integrated antenatal and postnatal care' – an interprofessional project between public health nursing students and midwifery students. Midwifery 2014;30(3):353-8. [DOI: 10.1016/j.midw.2013.03.007] [DOI] [PubMed] [Google Scholar]
Ayangade 1984 {published data only}
- Ayangade O. Integrated family planning services: a Nigerian experience. East African Medical Journal 1984;61(5):412-9. [PMID: ] [PubMed] [Google Scholar]
Bagayogo 2018 {published data only}
- Bagayogo IP, Turcios-Wiswe K, Taku K, Peccoralo L, Katz CL. Providing mental health services in the primary care setting: the experiences and perceptions of general practitioners at a New York City clinic. Psychiatric Quarterly 2018;89(4):897-908. [DOI: 10.1007/s11126-018-9587-2] [DOI] [PubMed] [Google Scholar]
Bajorek 2015 {published data only}
- Bajorek B, LeMay K, Gunn K, Armour C. The potential role for a pharmacist in a multidisciplinary general practitioner super clinic. Australasian Medical Journal 2015;8(2):52-63. [DOI: 10.4066/AMJ.2015.2278] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balira 2015 {published data only}
- Balira R, Mabey D, Weiss H, Ross DA, Changalucha J, Watson-Jones D. The need for further integration of services to prevent mother-to-child transmission of HIV and syphilis in Mwanza City, Tanzania. International Journal of Gynaecology & Obstetrics 2015;130(Suppl 1):S51-7. [DOI: 10.1016/j.ijgo.2015.04.016] [DOI] [PubMed] [Google Scholar]
Baltaxe 2019 {published data only}
- Baltaxe E, Czypionka T, Kraus M, Reiss M, Askildsen JE, Grenkovic R, et al. Digital health transformation of integrated care in Europe: overarching analysis of 17 integrated care programs. Journal of Medical Internet Research 2019;21(9):e14956. [DOI: 10.2196/14956] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barchi 2009 {published data only}
- Barchi D. Making healthcare delivery personal. Biomedical Instrumentation and Technology 2009;43(3):197-8. [DOI] [PubMed] [Google Scholar]
Barclay 2019 {published data only}
- Barclay L, Lalor A, Migliorini C, Robins L. A comparative examination of models of service delivery intended to support community integration in the immediate period following inpatient rehabilitation for spinal cord injury. Spinal Cord 2019;58(5):528-36. [DOI: 10.1038/s41393-019-0394-x] [DOI] [PubMed] [Google Scholar]
Bardwell 2019 {published data only}
- Bardwell G, Strike C, Mitra S, Scheim A, Barnaby L, Altenberg J, et al. "That's a double-edged sword": exploring the integration of supervised consumption services within community health centres in Toronto, Canada. Health and Place 2019;61:102245. [DOI: 10.1016/j.healthplace.2019.102245] [DOI] [PubMed] [Google Scholar]
Barraclough 2016 {published data only}
- Barraclough F, Longman J, Barclay L. Integration in a nurse practitioner-led mental health service in rural Australia. Australian Journal of Rural Health 2016;24(2):144-50. [DOI: 10.1111/ajr.12233] [DOI] [PubMed] [Google Scholar]
Barros 2019 {published data only}
- Barros S, Nóbrega MD, Santos JC, Fonseca LM, Floriano LS. Mental health in primary health care: health-disease according to health professionals [La salud mental en la atención primaria: el proceso salud-Enfermedad, según los profesionales de la salud]. Revista Brasileira de Enfermagem 2019;72(6):1609-17. [DOI: 10.1590/0034-7167-2018-0743] [DOI] [PubMed] [Google Scholar]
Bauman 2013 {published data only}
- Bauman LJ, Braunstein S, Calderon Y, Chhabra R, Cutler B, Leider J, et al. Barriers and facilitators of linkage to HIV primary care in New York City. Journal of Acquired Immune Deficiency Syndromes 2013;64(Suppl 1):S20-6. [DOI: 10.1097/QAI.0b013e3182a99c19] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baxter 2002 {published data only}
- Baxter C, Levin R, Legaspi MM, Bailey BE, Brown CL. Community health center-led networks: cooperating to compete. Journal of Healthcare Management 2002;46(6):376-88. [PubMed] [Google Scholar]
Baxter 2009 {published data only}
- Baxter P, Markle-Reid M. An interprofessional team approach to fall prevention for older home care clients 'at risk' of falling: health care providers share their experiences. International Journal of Integrated Care 2009;9:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benzer 2015 {published data only}
- Benzer JK, Cramer IE, Burgess JF Jr, Mohr DC, Sullivan JL, Charns MP. How personal and standardized coordination impact implementation of integrated care. BMC Health Services Research 2015;15:448. [DOI: 10.1186/s12913-015-1079-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berenson 2016 {published data only}
- Berenson RA, Burton RA, McGrath M. Do accountable care organizations (ACOs) help or hinder primary care physicians' ability to deliver high-quality care? Journal of Healthcare 2016;4(3):155-9. [DOI: 10.1016/j.hjdsi.2016.02.011] [DOI] [PubMed] [Google Scholar]
Bergmark 2018 {published data only}
- Bergmark M, Bejerholm U, Svensson B, Markstrom U. Complex interventions and interorganisational relationships: examining core implementation components of assertive community treatment. International Journal of Integrated Care 2018;18(4):11. [DOI: 10.5334/ijic.3547] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bertrand 2010 {published data only}
- Bertrand SW. Inroads to integrative health care: registered nurses' personal use of traditional Chinese medicine affects professional identity and nursing practice. Complementary Health Practice Review 2010;15(1):14-30. [DOI: 10.1177/1533210110374639] [DOI] [Google Scholar]
Bhattacharyya 2016 {published data only}
- Bhattacharyya O, Schull M, Shojania K, Stergiopoulos V, Naglie G, Webster F, et al. Building Bridges to Integrate Care (BRIDGES): incubating health service innovation across the continuum of care for patients with multiple chronic conditions. Healthcare Quarterly 2016;19(2):60-6. [DOI: 10.12927/hcq.2016.24701] [DOI] [PubMed] [Google Scholar]
Blakey 2014 {published data only}
- Blakey JM, Bowers PH. Barriers to integrated treatment of substance abuse and trauma among women. Journal of Social Work Practice in the Addictions 2014;14(3):250-72. [DOI: 10.1080/1533256X.2014.933731] [DOI] [Google Scholar]
Boehmer 2019 {published data only}
- Boehmer KR, Holland DE, Vanderboom CE. Identifying and addressing gaps in the implementation of a community care team for care of patients with multiple chronic conditions. BMC Health Services Research 2019;19(1):843. [DOI: 10.1186/s12913-019-4709-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bourgeault 2000 {published data only}
- Bourgeault IL. Delivering the 'new' Canadian midwifery: the impact on midwifery of integration into the Ontario health care system. Journal of Sociology of Health & Illness 2000;22(2):172-96. [Google Scholar]
Bracey 2010 {published data only}
- Bracey T. Bournemouth, Dorset and Poole Total Place pilot: services and support for older people. Working with Older People 2010;14(2):31-7. [DOI: 10.5042/wwop.2010.0265] [DOI] [Google Scholar]
Brant 2020 {published data only}
- Brant AR, Dhillon P, Hull S, Coleman M, Ye PP, Lotke PS, et al. Integrating HIV pre-exposure prophylaxis into family planning care: a RE-AIM framework evaluation. AIDS Patient Care and STDS 2020;34(6):259-66. [DOI: 10.1089/apc.2020.0004] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brechat 2018 {published data only}
- Brechat PH, Rasmusson K, Briot P, Foury C, Fulton R, Smith D, et al. Benefits of integrated care delivery system for heart failure: a case study of Intermountain Healthcare (USA) [Bénéfices de la prise en charge intégrée de l'insuffisance cardiaque: l'exemple d'Intermountain Healthcare (États-Unis)]. Sante Publique 2018;30(6):877-85. [DOI: 10.3917/spub.187.0877] [DOI] [PubMed] [Google Scholar]
Breton 2019 {published data only}
- Breton M, Wankah P, Guillette M, Couturier Y, Belzile L, Gagnon D, et al. Multiple perspectives analysis of the implementation of an integrated care model for older adults in Quebec. International Journal of Integrated Care 2019;19(4):6. [DOI: 10.5334/ijic.4634] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brindis 2005 {published data only}
- Brindis CD, Loo VS, Adler NE, Bolan GA, Wasserheit JN. Service integration and teen friendliness in practice: a program assessment of sexual and reproductive health services for adolescents. Journal of Adolescent Health 2005;37(2):155-62. [DOI: ] [DOI] [PubMed] [Google Scholar]
Briones‐Vozmediano 2018 {published data only}
- Briones-Vozmediano E, Maquibar A, Vives-Cases C, Öhman A, Hurtig A-K, Goicolea I. Health-sector responses to intimate partner violence: fitting the response into the biomedical health system or adapting the system to meet the response? Journal of Interpersonal Violence 2018;33(10):1653-78. [DOI: 10.1177/0886260515619170] [DOI] [PubMed] [Google Scholar]
Brook 2017 {published data only}
- Brook J, Salmon D, Knight RA. Preparing the sexual health workforce to deliver integrated services: is education the answer? A qualitative study exploring the impact of sexual health education on developing integrated policy and practice. Primary Health Care Research & Development 2017;18(3):270-81. [DOI: 10.1017/S1463423617000123] [DOI] [PubMed] [Google Scholar]
Brousselle 2010 {published data only}
- Brousselle A, Lamothe L, Sylvain C, Foro A, Perreault M. Integrating services for patients with mental and substance use disorders: what matters? Health Care Management Review 2010;35(3):212-23. [DOI: 10.1097/HMR.0b013e3181d5b11c] [DOI] [PMC free article] [PubMed] [Google Scholar]
Byrne 2019 {published data only}
- Byrne JP, Power R, Kiersey R, Varley J, Doherty CP, Saris AJ, et al. The rhetoric and reality of integrated patient-centered care for healthcare providers: an ethnographic exploration of epilepsy care in Ireland. Epilepsy & Behavior 2019;94:87-92. [DOI: 10.1016/j.yebeh.2019.02.011] [DOI] [PubMed] [Google Scholar]
Carroll 2018 {published data only}
- Carroll D, Kemner A, Schootman M. Operationalizing population health management in practice. Missouri Medicine 2018;115(6):533-6. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Cash‐Gibson 2014 {published data only}
- Cash-Gibson L, Rosenmoller M. Project INTEGRATE – a common methodological approach to understand integrated health care in Europe. International Journal of Integrated Care 2014;14(1):e035. [DOI: 10.5334/ijic.1980] [DOI] [PMC free article] [PubMed] [Google Scholar]
Catalao 2018 {published data only}
- Catalao R, Eshetu T, Tsigebrhan R, Medhin G, Fekadu A, Hanlon C. Implementing integrated services for people with epilepsy in primary care in Ethiopia: a qualitative study. BMC Health Services Research 2018;18(1):372. [DOI: 10.1186/s12913-018-3190-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chubak 2012 {published data only}
- Chubak J, Tuzzio L, Hsu C, Alfano CM, Rabin BA, Hornbrook MC, et al. Providing care for cancer survivors in integrated health care delivery systems: practices, challenges, and research opportunities. Journal of Oncology Practice 2012;8(3):184-9. [DOI: 10.1200/JOP.2011.000312] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coelho 2018 {published data only}
- Coelho LP, Motta LB da, Caldas CP. Elderly care network: facilitating factors and barriers to implementation [Rede de atenção ao idoso: fatores facilitadores e barreiras para implementação]. Physis 2018;28(4):e280404. [DOI: 10.1590/S0103-73312018280404] [DOI] [Google Scholar]
Contandriopoulos 2015 {published data only}
- Contandriopoulos D, Brousselle A, Dubois CA, Perroux M, Beaulieu MD, Brault I, et al. A process-based framework to guide nurse practitioners integration into primary healthcare teams: results from a logic analysis. BMC Health Services Research 2015;15(1):78. [DOI: 10.1186/s12913-015-0731-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2015 {published data only}
- Cooper D, Mantell JE, Moodley J, Mall S. The HIV epidemic and sexual and reproductive health policy integration: views of South African policymakers. BMC Public Health 2015;15:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Correa 2018 {published data only}
- Correa VA, Acioli S, Tinoco TF. The care of nurses in the Family Health Strategy: practices and theoretical foundation [Cuidado del enfermero en la Estrategia de Salud Familiar: prácticas y fundaciones teóricas]. Revista Brasileira de Enfermagem 2018;71(Suppl 6):2767-74. [DOI: 10.1590/0034-7167-2018-0383] [DOI] [PubMed] [Google Scholar]
DeBoer 2019 {published data only}
- DeBoer H, Andrews M, Cudd S, Leung E, Petrie A, Chan Carusone S, et al. Where and how does physical therapy fit? Integrating physical therapy into interprofessional HIV care. Disability & Rehabilitation 2019;41(15):1768-77. [DOI: 10.1080/09638288.2018.1448469] [DOI] [PubMed] [Google Scholar]
Dhondt 2017 {published data only}
- Dhondt S, Hermans K, Molema H, Boermans S, Klauw D, Vrijhoef Hubertus JM. Mechanisms of integrated care in Flanders: a bottom-up perspective. International Journal of Care Coordination 2017;20(3):87-97. [DOI: 10.1177/2053434517734464] [DOI] [Google Scholar]
Duffy 2017 {published data only}
- Duffy M, Ojikutu B, Andrian S, Sohng E, Minior T, Hirschhorn LR. Non-communicable diseases and HIV care and treatment: models of integrated service delivery. Tropical Medicine & International Health 2017;22(8):926-37. [DOI: 10.1111/tmi.12901] [DOI] [PubMed] [Google Scholar]
Evans 2016 {published data only}
- Evans JM, Grudniewicz A, Baker GR, Wodchis WP. Organizational context and capabilities for integrating care: a framework for improvement. International Journal of Integrated Care 2016;16(3):15. [DOI: 10.5334/ijic.3187] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fernandes 2014 {published data only}
- Fernandes RZ, Vilela MF. Strategies for integration of health care practices and sanitary surveillance in the context of the implementation of Rede Cegonha – a Brazilian mother and infant health care network [Estratégias de integração das práticas assistenciais de saúde e de vigilância sanitária no contexto de implementação da Rede Cegonha]. Ciênc Saúde Coletiva 2014;19(11):4457-66. [DOI: 10.1590/1413-812320141911.21662013] [DOI] [PubMed] [Google Scholar]
Freeman 2012 {published data only}
- Freeman C, Cottrell WN, Kyle G, Williams I, Nissen L. Integrating a pharmacist into the general practice environment: opinions of pharmacist's, general practitioner's, health care consumer's, and practice manager's. BMC Health Services Research 2012;12:229. [DOI: 10.1186/1472-6963-12-229] [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2006 {published data only}
- French RS, Coope CM, Graham A, Gerressu M, Salisbury C, Stephenson JM, et al. One stop shop versus collaborative integration: what is the best way of delivering sexual health services? Sexually Transmitted Infections 2006;82(3):202-6. [DOI: 10.1136/sti.2005.018093] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hallberg 2005 {published data only}
- Hallberg U, Klingberg G. Medical health care professionals' assessments of oral health needs in children with disabilities: a qualitative study. European Journal of Oral Sciences 2005;113(5):363-8. [DOI: 10.1111/j.1600-0722.2005.00238.x] [DOI] [PubMed] [Google Scholar]
Henao‐Martinez 2008 {published data only}
- Henao-Martinez D, Vazquez-Navarrete ML, Vargas-Lorenzo I, Coderch-Lassaletta J, Llopart-Lopez JR. Integral health provision by two Catalonian health providing entities (Spain) [Integración Asistencial de Dos Organizaciones en Cataluña, España]. Revista de Salud Publica 2008;10(1):33-48. [DOI] [PubMed] [Google Scholar]
Ingram 2019 {published data only}
- Ingram M, Denman CA, Cornejo-Vucovich E, Castro-Vasquez MDC, Aceves B, Ocejo AG, et al. The Meta Salud Diabetes Implementation Study: qualitative methods to assess integration of a health promotion intervention into primary care to reduce CVD risk among an underserved population with diabetes in Sonora, Mexico. Frontiers in Public Health 2019;7:347. [DOI: 10.3389/fpubh.2019.00347] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaehne 2016 {published data only}
- Kaehne A. The Healthy Liverpool Children's Programme. Journal of Integrated Care 2016;24(3):124-38. [DOI: 10.1108/JICA-03-2016-0014] [DOI] [Google Scholar]
References to studies awaiting assessment
Amelung 2015 {published data only}
- Amelung V, Wolf S, Ozegowski S, Eble S, Hildebrandt H, Knieps F, et al. Declared dead? Recommendations regarding integrated care from the perspective of German statutory health insurance [Totgesagte leben länger: Empfehlungen zur Integrierten Versorgung aus Sicht der gesetzlichen Krankenkassen]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2015;58(4-5):352-9. [DOI] [PubMed] [Google Scholar]
Aoki 2017 {published data only}
- Aoki M, Perez Batista MP, Morgani de Almeida MH, Molini-Avejonas DR, Corrêa Oliver F. Challenges on network care considering the perceptions of preceptors of a Pet-Network regarding people with disabilities and at-risk infants: access, comprehensiveness and communication. Cadernos Brasileiros de Terapia Ocupacional [Brazilian Journal of Occupational Therapy] 2017;25(3):519-32. [Google Scholar]
da Silva Bastos 2011 {published data only}
- da Silva Bastos L, Araújo Assis MM, Alves do Nascimento MA, Feltrin de Oliveira LC. Integrality-building in the care of people with diabetes mellitus in a healthcare unit of Feira de Santana, Bahia State [Construção da integralidade no cuidar de pessoas com diabetes mellitus em um centro de saúde em Feira de Santana (BA)]. Ciência & Saúde Coletiva 2011;16(Suppl 1):1417-26. [DOI] [PubMed] [Google Scholar]
Kondo 2014 {published data only}
- Kondo J, Onishi H, Greiner C. Rewarding, positive aspects and nursing characteristics of comprehensive community care practices by clinic nurses. An Official Journal of the Japan Primary Care Association 2014;1(1):10-5. [Google Scholar]
Rodrigues 2010 {published data only}
- Rodrigues Arce VA, De Sousa MF, da Glória Lima M. Mental health praxis within the family health strategy: contributions to build an integrated care. Physis 2010;21(2):541-60. [DOI: 10.1590/S0103-73312011000200011] [DOI] [Google Scholar]
Ruppert 2017 {published data only}
- Ruppert D, Stegbauer C, Bramesfeld A, Bestmann B, Szecsenyi J, Götz K. "Hope Dies Last …" – cross-sectoral cooperation in integrated care: a qualitative study. Psychiatrische Praxis 2017;44(3):134-40. [DOI] [PubMed] [Google Scholar]
Santos 2011a {published data only}
- Santos FA, Carvalho de Sousa IM, Dantas Gurgel ID, Benjamin Bezerra AF, Barros NF. Policy of integrative practices in Recife (Northeastern Brazil): analysis of the participation of the actors [Política de práticas integrativas em Recife: análise da participação dos atores]. Revista de Saúde Pública 2011;45(6):1154-9. [DOI] [PubMed] [Google Scholar]
Villela 2009 {published data only}
- Villela WV, Araujo EC, Ribeiro SA, Cuginotti AP, Hayana ET, Brito FC, et al. Challenges in primary health care: the experience in Vila Mariana District, São Paulo, Brazil [Desafios da atenção básica em saúde: a experiência de Vila Mariana, São Paulo, Brasil]. Cadernos de Saude Publica 2009;25(6):1316-24. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Wodchis 2018 {published and unpublished data}
- Wodchis W, Burau V, Tenbensel T, Breton M, Goldhar J. Implementing integrated Care for Older Adults with Complex Health needs: iCOACH. An international network discussion. International Journal of Integrated Care 2018;18(Suppl 2):1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Arksey 2005
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8(1):19-32. [Google Scholar]
Armitage 2009
- Armitage G, Suter E, Oelke N, Adair C. Health systems integration: state of the evidence. International Journal of Integrated Care 2009;9:e82. [DOI: 10.5334/ijic.316] [DOI] [PMC free article] [PubMed] [Google Scholar]
Atkins 2018
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Medical Research Methodology 2018;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atun 2004
- Atun R, Lennox-Chhugani N, Drobniewski F, Samyshkin Y, Coker R. A framework and toolkit for capturing the communicable disease programmes within health systems: tuberculosis control as an illustrative example. European Journal of Public Health 2004;14(3):267-73. [DOI: 10.1093/eurpub/14.3.267] [DOI] [PubMed] [Google Scholar]
Atun 2008
- Atun RA, Bennett S, Duran A. When do vertical (stand-alone) programmes have a place in health systems? Copenhagen: World Health Organization; 2008. Health Systems and Policy Analysis: policy brief, 5.
Awofeso 2004
- Awofeso N. What is the difference between 'primary care' and 'primary healthcare'? Quality in primary care. Canadian Journal of Public Health 2004;12(2):93-4. [Google Scholar]
Baxter 2018a
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Services Research 2018;18(1):350. [DOI: 10.1186/s12913-018-3161-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baxter 2018b
- Baxter SK, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Understanding new models of integrated care in developed countries: a systematic review. Health Services and Delivery Research 2018;6(1):29. [PubMed] [Google Scholar]
Buse 2012
- Buse K, Mays N, Walt G. Making Health Policy. 2nd edition. London (UK): McGraw-Hill Education, 2012. [Google Scholar]
Chuah 2017
- Chuah FL, Haldane VE, Cervero-Liceras F, Ong SE, Sigfrid LA, Murphy G, et al. Interventions and approaches to integrating HIV and mental health services: a systematic review. Health Policy and Planning 2017;32(Suppl 4):iv27-47. [DOI: 10.1093/heapol/czw169] [DOI] [PMC free article] [PubMed] [Google Scholar]
Damschroder 2009
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science 2009;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dudley 2011
- Dudley L, Garner P. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD003318. [DOI: 10.1002/14651858.CD003318.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Erasmus 2008
- Erasmus E, Gilson L. How to start thinking about investigating power in the organizational settings of policy implementation. Health Policy and Planning 2008;23(5):361-8. [DOI: 10.1093/heapol/czn021] [DOI] [PubMed] [Google Scholar]
Erasmus 2011
- Erasmus E. Important Policy Analysis Theories In-brief: Street Level Bureaucracy. Cape Town (South Africa): University of Cape Town, 2011. [Google Scholar]
Foreit 2002
- Foreit K, Hardee K, Agarwal K. When does it make sense to consider integrating STI and HIV services with family planning services? International Family Planning Perspectives 2002;28(1):105. [DOI: 10.2307/3088242] [DOI] [Google Scholar]
Gilson 2015
- Gilson LL. Michael Lipsky, street-level bureaucracy: dilemmas of the individual in public service. In: Lodge M, Page EC, Balla SJ, editors(s). The Oxford Handbook of the Classics of Public Policy. Oxford (UK): Oxford University Press, 2015:383-404. [Google Scholar]
Haldane 2017
- Haldane V, Cervero-Liceras F, Chuah FL, Ong SE, Murphy G, Sigfrid L, et al. Integrating HIV and substance use services: a systematic review. Journal of the International AIDS Society 2017;20(1):21585. [DOI: 10.7448/IAS.20.1.21585] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haldane 2018
- Haldane V, Legido-Quigley H, Chuah FL, Sigfrid L, Murphy G, Ong SE, et al. Integrating cardiovascular diseases, hypertension, and diabetes with HIV services: a systematic review. AIDS Care 2018;30(1):103-15. [DOI: 10.1080/09540121.2017.1344350] [DOI] [PubMed] [Google Scholar]
Hall 2003
- Hall J, Taylor R. Health for all beyond 2000: the demise of the Alma-Ata Declaration and primary health care in developing countries. Medical Journal of Australia 2003;178(1):17-20. [DOI: 10.5694/j.1326-5377.2003.tb05033.x] [DOI] [PubMed] [Google Scholar]
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;1(1):348. [DOI] [PubMed] [Google Scholar]
Hudson 2009
- Hudson J, Lowe S. Understanding the Policy Process: Analysing Welfare Policy and Practice. 2nd edition. Bristol (UK): Bristol University Press, 2009. [Google Scholar]
Kodner 2002
- Kodner D, Spreeuwenberg C. Integrated care: meaning, logic, applications and implications – a discussion paper. International Journal of Integrated Care 2002;2(1):e12. [DOI: 10.5334/ijic.67] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2016
- Kumar S, Kumar N, Vivekadhish S. Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs): addressing unfinished agenda and strengthening sustainable development and partnership. Indian Journal of Community Medicine 2016;41(1):1-4. [DOI: 10.4103/0970-0218.170955] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lau 2015
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care – causes of the evidence to practice gap: systematic reviews of reviews. Implementation Science 2015;11(1):40. [DOI: 10.1186/s13012-016-0396-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mounier‐Jack 2017
- Mounier-Jack S, Mayhew SH, Mays N. Integrated care: learning between high-income, and low- and middle-income country health systems. Health Policy and Planning 2017;32(Suppl 4):iv6-12. [DOI: 10.1093/heapol/czx039] [DOI] [PMC free article] [PubMed] [Google Scholar]
Msuya 2004
- Msuya J. Horizontal and Vertical Delivery of Health Services: What Are the Trade Offs? Background Paper for the World Development Report. Washington (DC): The World Bank, 2004. [Google Scholar]
Muldoon 2006
- Muldoon L, Hogg W, Levitt M. Primary care (PC) and primary health care (PHC): what is the difference? Revue Canadienne de Sante Publique [Canadian Journal of Public Health] 2006;97(5):409-11. [DOI: 10.1007/BF03405354] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oleribe 2015
- Oleribe O, Crossey M, Taylor-Robinson D. Sustainable health development goals (SHDG): breaking down the walls. Pan African Medical Journal 2015;22:306. [DOI: 10.11604/pamj.2015.22.306.6468] [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2021
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic Reviews 2021;10(1):89. [DOI: 10.1186/s13643-021-01626-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peters 2015
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare 2015;13(3):141-6. [DOI: 10.1097/XEB.0000000000000050] [DOI] [PubMed] [Google Scholar]
Ryman 2012a
- Ryman TK, Wallace A, Mihigo R, Richards P, Schlanger K, Cappelier K, et al. Community and health worker perceptions and preferences regarding integration of other health services with routine vaccinations: four case studies. Journal of Infectious Diseases 2012;205(Suppl 1):S49-55. [DOI] [PubMed] [Google Scholar]
Schierhout 1999
- Schierhout G, Fonn S. The integration of primary health care services: a systematic literature review. Durban, South Africa: Health Systems Trust; 1999.
Sundaram 2017
- Sundaram N, James R, Sreynimol U, Linda P, Yoong J, Saly S, et al. A strong TB programme embedded in a developing primary healthcare system is a lose-lose situation: insights from patient and community perspectives in Cambodia. Health Policy and Planning 2017;32(Suppl 2):ii32-42. [DOI] [PubMed] [Google Scholar]
Sure Collaboration 2011
- The Sure Collaboration. SURE guides for preparing and using evidence-based policy briefs: 5 identifying and addressing barriers to implementing policy options; version 2.1, November 2011. Available at epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/SURE-Guides-v2.1/Collectedfiles/sure_guides.html (accessed 7 July 2023).
Sutton 2019
- Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Information & Libraries Journal 2019;36(3):202-22. [DOI] [PubMed] [Google Scholar]
Tricco 2016
- Tricco AC, Lillie E, Zarin W, O'Brien K, Colquhoun H, Kastner M. A scoping review on the conduct and reporting of scoping reviews. BMC Medical Research Methodology 2016;16:15. [DOI: 10.1186/s12874-016-0116-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tricco 2018
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 2018;169(7):467-73. [DOI: 10.7326/M18-0850] [DOI] [PubMed] [Google Scholar]
Valentijn 2013
- Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. International Journal of Integrated Care 2013;13(e010):1-8. [DOI: 10.5334/ijic.886] [DOI] [PMC free article] [PubMed] [Google Scholar]
Valentijn 2015
- Valentijn PP, Boesveld IC, Klauw DM, Ruwaard D, Struijs JN, Molema JJ, et al. Towards a taxonomy for integrated care: a mixed-methods study. International Journal of Integrated Care 2015;15:e003. [DOI: 10.5334/ijic.1513] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Olmen 2010
- Olmen J, Criel B, Van Damme W, Marchal B, Van Belle S, Van Dormael M, et al. Analysing Health Systems to Make Them Stronger. Antwerp: ITG Press; 2010. Studies in Health Services Organisation & Policy; 27.
Walker 2004
- Walker L, Gilson L. "We are bitter but we are satisfied": nurses as street-level bureaucrats in South Africa. Social Science and Medicine 2004;59(6):1251-61. [DOI: 10.1016/j.socscimed.2003.12.020] [DOI] [PubMed] [Google Scholar]
Walley 2008
- Walley J, Lawn JE, Tinker A, De Francisco A, Chopra M, Rudan I, et al. Primary health care: making Alma-Ata a reality. Lancet 2008;372(9642):1001-7. [DOI: 10.1016/S0140-6736(08)61409-9] [DOI] [PubMed] [Google Scholar]
WHO 1987
- World Health Organization, International Conference on Primary Health Care. Declaration of Alma Ata: International Conference on Primary Health Care. Geneva: World Health Organization, 1987. [Google Scholar]
WHO 2013
- World Health Organization, Regional Office for the Western Pacific. People-centred health care: a policy framework; December 2013. Available at www.who.int/publications/i/item/9789290613176.
WHO 2016
- World Health Organization. Integrated Care Models: an Overview. Geneva: World Health Organization, 2016. [Google Scholar]
WHO 2018
- World Health Organization. Declaration of Astana: Global Conference on Primary Health Care: Astana, Kazakhstan. Global Conference on Primary Healthcare 2018.
References to other published versions of this review
Moloi 2020
- Moloi H, Daniels K, Cooper S, Odendaal WA, Naledi T, Goliath C, et al. Healthcare workers' perceptions and experience of primary healthcare integration: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD013603. [DOI: 10.1002/14651858.CD013603] [DOI] [Google Scholar]