Abstract
Objective
COVID-19 has gravely affected patients with psychiatric conditions. Potential interactions may occur between psychotropic medications and medications used in treatment of COVID-19. This study aimed to compare the online databases in terms of the quality of drug-drug interaction related information available on them.
Methods
216 drug interactions which included fifty-four psychotropic medication interactions with four COVID-19 drugs across six databases were analyzed by four authors independently. The overall grading of the databases was done on Likert scale independently by the authors using the parameters of ease of understanding for consumers and professionals, level of completeness, discussion on level of evidence and the number of available drugs, congruity with other databases and the mean score was tabulated.
Results
Drugbank and Lexicomp had maximum discrepancy. The safety profile of Hydroxychloroquine was the best (eighteen moderate/severe psychotropic medication reactions) while Ritonavir has worst profile with thirty-nine medications. Drugbank had the highest SCOPE score (1.00) for completeness and covid19druginteractions.com had least (0.81). Overall, Liverpool© Drug Interaction Group and Lexicomp scored the highest (23/30 each) and were the best interaction checker software closely followed by Drugs.com (22/30). Medscape and WebMD were the poorest interaction checker databases.
Conclusion
There is significant variability in the available online databases. Liverpool© Drug Interaction Group and Lexicomp were the most reliable sources for healthcare workers whereas for patients, Drugs.com was the easiest to understand (as it segregates the needs of general consumers and professionals distinctly to explain the interaction).
Keywords: Drug-related side effects, Adverse reactions, Psychotropic drugs, COVID-19
INTRODUCTION
Knowledge of drug-drug interaction is highly essential for safe clinical practice of medicine. Poor understanding about drug-drug interaction may result in development of significant adverse drug reactions, treatment failure, and poor adherence to treatment [1]. Patients with multiple medical morbidities are often prescribed with different groups of medication, which may have potential drug-drug interactions. Patients with psychiatric illnesses are at increased risk of medical morbidities and many such patients have multiple medical morbidities, which increases the possibility of serious drug-drug interactions, if appropriate medications are not considered in combination.
Drug-drug interaction results from the pharmacokinetic changes. The pharmacokinetic changes result in increased therapeutic level of the drugs leading to development of adverse drug reactions or it may result in increased metabolism of a drug leading to decreased therapeutic level and hence inadequate response to the drug [2]. Psycho-tropic medications are known to have significant interaction with several medications including those used in the management of COVID-19.
Most of the textbooks and other scientific literature discuss the potential drug-drug interactions broadly but they are deficient in discussing the one-to-one interaction between the pharmacological agents and are neither frequently updated and nor freely accessible. This results in the usage of easily accessible online databases, that provides the details on potential drug-drug interactions and their severity [3].
During this COVID-19 pandemic many mental health issues are emerging [4], which requires psychological and pharmacological intervention. Considering this fact, we have selected four medications (chloroquine, hydroxychloroquine, azithromycin, ritonavir), which were initially used in the management of COVID-19 when specific drugs were unavailable and selected drugs were being repurposed [5]. These drugs are also used for various other medical conditions, commonly. Purposefully, we have not included the newer antiviral medications used for COVID-19, as these drugs are very new and many drug- drug interactions with psychotropic medications are not known, due to paucity of trials. Moreso, this article aimed to compare the online databases in terms of the quality of drug-drug interaction related information available on them. This article discusses the potential interaction of commonly used psychotropic medications with Hydroxy-chloroquine/Chloroquine, Azithromycin, and Ritonavir across various popular drug-drug interaction online search engines.
METHODS
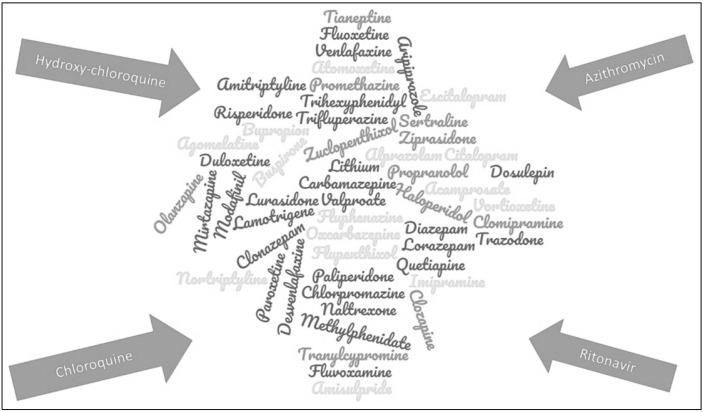
This study aimed to compare the popular online databases that give information about drug-drug interactions and were available for free access. Possible drug interactions between psychotropics and COVID-19 medications were searched on major online databases namely WebMD (“Drug Interaction Checker - Find Interactions Between Medications,” 2020) [6], Medscape (“Drug Inter-actions Checker - Medscape Drug Reference Database,” 2020) [7], Lexicomp [8], Drugbank [9], Drugs.com (“Drugs. com | Prescription Drug Information, Interactions & Side Effects,” 2020.) [10] and Liverpool© Drug Interaction Group [11]. This was done by four independent researchers; each of whom searched one database each and recorded their observations on a table. Symbols ‘+’ and ‘−’ were used where ‘+’ indicated presence of a possible interaction whereas ‘−’ indicated the absence of any possible interaction(s) between the two drugs. This was then compared to understand the congruity and completeness of the different databases. The available mentioned references for each drug interaction were also verified. The four drugs assessed with the psychotropic medications are depicted in Figure 1.
Fig. 1.
Drug interaction measured in the present study.
RESULTS
Comparison of the Databases for Possible Drug Interactions
The data available for interaction between different drugs were compared and tabulated in Table 1. They are compared to assess the level of heterogeneity between the different databases.
Table 1.
Interaction of psychotropic medications with medications used in COVID-19 patients
| Psychotropic medication | Congruity between different databases | Congruity in positive interaction (%) | Medscape | WebMD | Drugs.com | Drugbank | Lexicomp | Liverpool COVID-19 interactions |
|---|---|---|---|---|---|---|---|---|
| Escitalopram | 5/6 (++++), 1/6 (+++) | HCA (6/6)-100% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Sertraline | 3/6 (++++), 2/6 (+++), 1/6 (−−−+) | H (5/6)-83.33% C (5/6)-83.33% A (4/6)-66.67% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(+), C(+), A(+), R(−) | H(−), C(−), A(−), R(+) |
| Paroxetine | 1/6 (++++), 4/6 (+++), 1/6 (+) | H (3/6)-50% C (5/6)-83.33% A (3/6)-50% R (6/6)-100% |
H(−), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(+), C(+), A(−), R(+) |
| Fluoxetine | 4/6 (++++), 2/6 (+++) | H (6/6)-100% C (6/6)-100% A (5/6)-83.33% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(−), R(+) |
| Fluvoxamine | 2/6 (+++), 1/6 (++), 3/6 (+) | H (3/6)-50% C (3/6)-50% A (1/6)-16.33% R (4/6)-66.66% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(−), R(−) | H(+), C(+), A(−), R(+) |
| Citalopram | 5/6 (++++), 1/6 (+++) | H (6/6)-100% C (6/6)-100% A (6/6)-100% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Vortioxetine | 1/6 (++++), 1/6 (++), 3/6 (+), 1/6 (−−−−) | H (2/6)-33.33% C (2/6)-33.33% A (1/6)-16.33% R (4/6)-66.66% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(−) | H(−), C(−), A(−), R(−) |
| Duloxetine | 1/6 (++++), 1/6 (+++), 2/6 (++), 2/6 (−−−−) | H (2/6)-33.33% C (4/6)-66.66% A (1/6)-16.66% R (4/6)-66.66% |
H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) |
| Venlafaxine | 3/6 (++++), 2/6 (++), 1/6 (−−−−) | H (3/6)-50% C (3/6)-50% A (5/6)-83.33% R (5/6)-83.33% |
H(−), C(−), A(+), R(+) | H(−), C(−), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(+), C(+), A(+), R(+) |
| Desvenlafaxine | 1/6 (+++), 1/6 (++), 2/6 (+), 1/6 (−−−−), 1/6-UN | H (5/6, UN)-83.33% C (2/6, UN)-33.33% A (1/6, UN)-16.66% R (4/6, UN)-66.67% |
H(−), C(+), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(−) | H(−), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H, C, A, R |
| Mirtazapine | 2/6 (++++), 1/6 (+++), 3/6 (+) | H (3/6)-50% C (3/6)-50% A (3/6)-50% R (5/6)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(+), C(−), A(−), R(−) | H(+), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Bupropion | 4/6 (++), 1/6 (+), 1/6 (−−−−) | H (0/6)-0% C (3/6)-50% A ( 0/6)-0% R (5/6)-83.33% |
H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(−) |
| Tranylcypromine | 1/6 (++), 5/6 (−−−−) | H (1/6)-16.67% C (1/6)-16.67% A (0/6)-0% R (0/6)-0% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(+), C(+), A(−), R(−) | H(−), C(−), A(−), R(−) |
| Imipramine | 3/6 (++++), 2/6 (+++), 1/6 (+) | H (3/6)-50% C (5/6)-83.33% A (5/6)-83.33% R (6/6)-100% |
H(−), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) |
| Clomipramine | 5/6 (++++), 1/6 (+) | H (5/6)-83.33% C (5/6)-83.33% A (5/6)-83.33% R (6/6)-100% |
H (+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) |
| Amitriptyline | 5/6 (++++), 1/6 (+++) | H (5/6)-83.33% C (6/6)-100% A (6/6)-100% R (6/6)-100% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Nortriptyline | 4/6 (++++), 1/6 (+++), 1/6 (−−−−) | H (4/6)-66.67% C (5/6)-83.33% A (4/6)-66.67% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Trazodone | 2/6 (++++), 2/6 (+++), 1/6 (++) | H (3/6)-50% C (4/6)-66.67% A (5/6)-83.33% R(6/6)-100% |
H(−), C(−), A(+), R(+) | H(−), C(−), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Dosulepin | 1/6 (++++), 1/6 (+) , 1/6 (−−−−), 3/6-UN | H (1/6, 2 UN)-16.67% (1/6, 2 UN)-16.67% A(1/6, 2 UN)-16.67% R(2/6, 2 UN)-33.33% |
H(−), C(−), A(−), R(−) | H, C, A, R | H, C, A, R | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H, C, A, R |
| Agomelatine | 2/6 (+), 1/6 (−−−−), 3/6-UN | H (0/6, 3 UN)-0% C (0/6, 3 UN)-0% A (0/6, 3 UN)-0% R (1/6, 3 UN)-16.67% |
H, C, A, R | H, C, A, R | H, C, A, R | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(+) |
| Tianeptine | 1/6 (+++), 1/6 (+), 1/6 (−−−−), 3/6-UN | H (0/6, 3 UN)-0% C (0/6, 3 UN)-0% A (1/6, 3 UN)-16.67% R (2/6, 3 UN)-16.67% |
H, C, A, R | H, C, A, R | H, C, A, R | H(−), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(+) |
| Clozapine | 6/6 (++++) | HCAR (6/6)-100% | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Olanzapine | 5/6 (++++), 1/6 (+) | H(5/6)-83.33% C(5/6)-83.33% A(5/6)-83.33% R(6/6)-100% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) |
| Risperidone | 4/6 (++++), 2/6 (+++) | HCR (6/6)-100% A (4/6)-66.67% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) |
| Amisulpride | 3/6 (++++), 1/6 (+++), 1/6 (−−−−), 1/6-UN | H (4/6, 1 UN)-66.67% C (4/6, 1 UN)-66.67% A (4/6, 1 UN)-66.67% R (3/6, 1 UN)-50% |
H(−), C(−), A(−), R(−) | H, C, A, R | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Aripiprazole | 3/6 (++++), 2/6 (++), 1/6 (+) | H (3/6)-50% C (5/6)-83.33% A (3/6)-50% R (6/6)-100% |
H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) |
| Ziprasidone | 5/6 (++++), 1/6 (+++) | HCA (6/6)-100% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Quetiapine | 5/6 (++++), 1/6 (+++) | HAR (6/6)-100% C(5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(−), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Lurasidone | 2/6 (++++), 4/6 (+) | H (2/6)-33.33% C (3/6)-50% A (2/6)-33.33% R (6/6)-100% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) |
| Paliperidone | 4/6 (++++), 2/6 (+++) | H (5/6)-83.33% C (6/6)-100% A (6/6)-100% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Haloperidol | 6/6 (++++) | HCAR(6/6) -100% | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) |
| Chlorpromazine | 4/6 (++++), 1/6 (+++), 1/6 (+++UN) | H (6/6)-100% C (6/6)-100% A (5/6, 1 UN)-83.33% R (5/6)-83.33% |
H(+), C(+), A(+), R(+) | H(+), C(+), R(+) A (UN) |
H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Trifluperazine | 1/6 (+++), 2/6 (−−−−), 3/6-UN | H (0/6, 3 UN)-0% C (1/6)-16.67% A (1/6)-16.67% R (1/6, 3 UN)-16.67% |
H(−), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H, C, A, R | H(−), C(−), A(−), R(−) | H, C, A, R | H, C, A, R |
| Zuclopenthixol | 2/6 (++++), 1/6 (+), 1/6 (−−−−), 2/6-UN | H (2/6)-33.37% C (3/6, 2 UN)-50% A (3/6, 2 UN)-50% R (2/6, 2 UN)-33.33% |
H, C, A, R | H(−), C(−), A(−), R(−) | H, C, A, R | H(+), C(+), A(+), R(+) | H(−), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Flupenthixol | 3/6 (+++), 1/6 (−−−−), 2/6-UN | H (3/6)-50% C (3/6)-50% A (1/6)-16.67% R (2/6)-33.33% |
H, C, A, R | H(−), C(−), A(−), R(−) | H, C, A, R | H(+), C(+), A(−), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(−), R(+) |
| Fluphenazine | 2/6 (++++), 3/6 (+++), 1/6 (−−−−) | H (5/6)-83.33% C (5/6)-83.33% A (3/6)-50% R (4/6)-66.67% |
H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(+), C(+), A(+), R(−) | H(+), C(+), A(−), R(+) |
| Valproate | 1/6 (++++), 3/6 (+), 2/6 (−−−−) | H (1/6)-16.67% C (2/6)-33.33% A (1/6)-16.67% R (4/6)-66.67% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) |
| Carbamazepine | 2/6 (++++), 1/6 (++), 3/6 (+) | H (2/6)-33.33% C (3/6)-50% A (2/6)-33.33% R (6/6)-100% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) |
| Oxcarbazepine | 2/6 (++++), 1/6 (++), 2/6 (+), 1/6 (−−−−) | H (2/6)-33.33% C (3/6)-50% A (2/6)-33.33% R (5/6)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(+), C(+), A(+), R(+) |
| Lithium | 2/6 (++++), 1/6 (+++), 1/6 (++), 2/6 (−−−−) | H (3/6)-50% C (4/6)-66.67% A (4/6)-66.67% R (2/6)-33.33% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(+), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) | H(−), C(+), A(+), R(−) | H(+), C(+), A(+), R(+) |
| Lamotrigine | 1/6 (++++), 5/6 (+) | H (1/6)-16.67% C (2/6)-33.33% A (1/6)-16.67% R (5/6)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(+), A(−), R(−) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) |
| Trihexyphenidyl | 5/6 (−−−−), 1/6-UN | HCAR (5/6)-0% HCAR (1/6)-UN |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H, C, A, R |
| Acamprosate | 5/6 (−−−−), 1/6 -UN | HCAR (5/6)-0% HCAR (1/6)-UN |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H, C, A, R |
| Methylphenidate | 1/6 (++), 4/6 (−−−−), 1/6-UN | HAR (0/6, 1 UN)-0% C(1/6, 1 UN)-16.67% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(+), A(−), R(−) | H(−), C(−), A(−), R(−) | H, C, A, R |
| Atomoxetine | 1/6 (++++), 3/6 (++), 1/6 (−−−−), 1/6-UN | H (1/6, 1 UN)-16.67% C (4/6, 1 UN)-66.67% A (2/6)-33.33% R (3/6)-50% |
H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(−), C(+), A(+), R(−) | H, C, A, R |
| Modafinil | 1/6 (+++), 1/6 (++), 3/6 (+), 1/6-UN | H (0/6, 1 UN)-0% C (1/6, 1 UN)-16.67% A (2/6, 1 UN)-33.33% R (5/6, 1 UN)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(+), R(+) | H(−), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H, C, A, R |
| Lorazepam | 1/6 (++++), 1/6 (+), 4/6 (−−−−) | H (1/6)-16.67% C (1/6)-16.67% A (1/6)-16.67% R (2/6)-33.33% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) |
| Clonazepam | 1/6 (++++), 1/6 (+++), 3/6 (+), 1/6 (−−−−) | H (1/6)-16.67% C (2/6)-33.33% A (1/6)-16.67% R (5/6)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(−), R(+) | H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(+) |
| Diazepam | 1/6 (++++), 1/6 (++), 4/6 (+) | H (1/6)-16.67% C (1/6)-16.67% A (2/6)-33.33% R (6/6)-100% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) |
| Alprazolam | 1/6 (++), 5/6 (+) | H (0/6)-0% C (1/6)-16.67% A (0/6)-0% R (6/6)-100% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) |
| Buspirone | 1/6 (+++), 4/6 (+), 1/6 (−−−−) | H (1/6)-16.67% C (1/6)-16.67% A (0/6)-0% R (5/6)-83.33% |
H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(−) | H(+), C(+), A(−), R(+) | H(−), C(−), A(−), R(+) | H(−), C(−), A(−), R(+) |
| Propranolol | 1/6 (++++), 4/6 (++), 1/6 (−−−−) | H (2/6)-33.33% C (5/6)-83.33% A (1/6)-16.67% R (4/6)-66.67% |
H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(+), A(−), R(+) | H(−), C(−), A(−), R(−) | H(+), C(+), A(−), R(−) | H(+), C(+), A(+), R(+) |
| Naltrexone | 2/6 (++), 3/6 (−−−−), 1/6-UN | H (0/6)-0% C (1/6)-16.67% A (1/6)-16.67% R (2/6)-33.33% |
H(−), C(−), A(−), R(−) | H(−), C(−), A(−), R(−) | H(−), C(−), A(+), R(+) | H(−), C(+), A(−), R(+) | H(−), C(−), A(−), R(−) | H, C, A, R |
| Promethazine | 2/6 (++++), 2/6 (+++), 1/6 (−−−−), 1/6-UN | H (2/6)-33.33% C (4/6)-66.67% A (4/6)-66.67% R (4/6)-66.67% |
H(−), C(+), A(+), R(+) | H(−), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(+), C(+), A(+), R(+) | H(−), C(−), A(−), R(−) | H, C, A, R |
H, hydoxychloroquine; C, chloroquine; A, azithromycin; R, ritonavir; +, symbol corresponds to presence of interaction; −, symbol corresponds to no potential interaction; UN, unknown.
Congruity of databases
The congruity of databases was compared by assessing colour coding of individual drugs depicted in the second row wherein for example escitalopram shows all four (HCAR ++++) interactions in five of the six assessed databases (5/6) whereas one database Lexicomp shows interaction with three of the four drugs (HCAR +++−).
While only comparing drugs for which there was one discrepant database out of all others, it was seen that Drugbank and Lexicomp had maximum discrepancy than other databases (Table 1).
Congruity of databases for each drug (% positive interaction)
The congruity for each drug was also compared with all the databases. For example, Sertraline shows positive interactions with hydroxychloroquine, chloroquine and ritonavir across five databases (5/6, 83.33%) and with azithromycin in four databases (4/6, 66.67%) (Table 1).
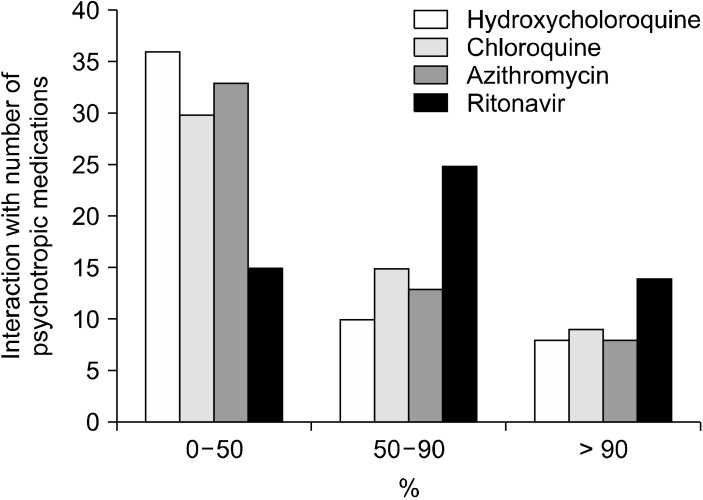
Interaction Grade of Psychotropic Drugs with COVID-19 Drugs
Figure 2 provides pictorial representation of the interaction grade of psychotropic medications with COVID- 19 drugs. All the drugs show maximal frequency in minimal interaction grade across databases except ritonavir which mostly shows moderate and severe interaction with other psychotropic medications. Hydroxychloroquine and azithromycin have least reported severe interactions across all six databases with 100% congruity for drug interaction for eight psychotropic medications. Overall, safety profile of hydroxychloroquine is best as it has moderate and severe interactions (> 50% congruity) with eighteen psychotropic medications while ritonavir has worst profile with thirty-nine medications.
Fig. 2.
Levels of drug interaction between COVID-19 drugs and psychotropic medications.
References and Grade of Evidence for the Studies Used for Reporting
The databases used for the recommendation were evaluated to ascertain the level of evidence used. Most popular databases like WebMD [6] and Medscape [7] just provided the result without referencing the source for the same.
I. The database Liverpool© Drug Interaction Group [11] for COVID-19 therapies (https://covid19-druginteractions. org), developed by the University of Liverpool provides the most extensive and detailed report after classifying every drug interaction into four categories and further categorizing the level of evidence using GRADE recommen-dations alongside a table reporting all the studies evaluated for the final consensus.
II. Lexicomp [8] is the second most comprehensive and complete database developed by Wolters Kluwer. The risk rating is done as A- no known interaction, B- no action needed, C- Monitor therapy, D- Consider therapy modification, X- Avoid combination. The product monograph provides discussion of available literature and includes PubMed indexed literature links but does not grade the evidence for some of the drug interactions.
III. Drugbank [9] also grades the severity as minor, moderate and major. Some of the references used are from standard Food and Drug Adminisitration (FDA) guidelines while others have references from PubMed indexed studies or manufacturer’s monograph. However, the level of evidence is not graded.
IV. Drugs.com [10] has two separate pages for every drug interaction- one for consumers and one for profes-sionals. The two varies in the type of explanation wherein the consumer tab provides information about potential risks and warning signs whereas professional tab details on the available references, classifies it as major/moderate/minor and also details on the management strategy. The references standards include European medicines agency, FDA and product manufacturer’s monograph but the evidence is not graded.
Comparative Evaluation for Completeness of Database
SCOPE score evaluation revealed that Drugbank had all the assessed drug interactions (1.00) whereas Liverpool© Drug Interaction Group scored the least (0.81) (Table 2). Interaction of 54 commonly used psychotropic medications was evaluated with four medications used for management of COVID-19 (a total of 54 × 4 = 216 interactions). SCOPE score is calculated by dividing the total number of interactions available for a particular database by the total possible interactions (i.e., 216).
Table 2.
SCOPE score evaluation for completeness of database
| Databases | Interacting and non-interacting drug pairs (A) | Unavailable drug pairs (B) | SCOPE score (A/A + B) |
|---|---|---|---|
| Medscape | 200 | 16 | 0.92 |
| WebMD | 200 | 16 | 0.92 |
| Drugs.com | 192 | 24 | 0.88 |
| Drugbank | 216 | 0 | 100 |
| Lexicomp | 212 | 4 | 0.98 |
| Liverpool COVID-19 interactions | 176 | 40 | 0.81 |
| Total- 54*4-216 drug interactions | |||
Comparative Evaluation of Databases
The overall evaluation of the databases was done based on their ‘ease of understanding for consumers’, ‘ease of understanding for professionals’, ‘level of completeness’, ‘discussion on level of evidence’, ‘the number of available drugs’, and ‘congruity with other databases’. These items were graded on Likert scale from 1 (very poor) to 5 (excellent) by the authors of the study independently and their mean scores were calculated and tabulated there-after. The evaluation of the databases on the specific parameters was done by a medical graduate (first author) and confirmed in discussion with psychiatry post-graduate residents (authors of this article) and a faculty of psychiatry. Overall, Liverpool© Drug Interaction Group and Lexicomp scored the highest and were the best interaction checker software closely followed by Drugs.com. Drug bank also has a wide database. Medscape has the poorest interaction checker database without much collaborative evidence followed by WebMD (Table 3).
Table 3.
Comparative evaluation of all the databases for psychotropic medication interaction with COVID-19 drugs
| Parameters of evaluation | Medscape | WebMD | Drugs.com | Drugbank | Lexicomp | Liverpool COVID-19 interactions |
|---|---|---|---|---|---|---|
| Ease of understanding for consumers | 2 | 2 | 5 | 3 | 4 | 4 |
| Ease of understanding for professionals | 2 | 2 | 5 | 3 | 4 | 5 |
| Level of completeness | 1 | 2 | 3 | 3 | 5 | 5 |
| Level of evidence used and classified | 1 | 1 | 3 | 3 | 4 | 5 |
| Number of available drugs | 2 | 3 | 3 | 5 | 4 | 1 |
| Congruity with other databases | 5 | 4 | 3 | 1 | 2 | 3 |
| Average overall score | 13/30 | 14/30 | 22/30 | 18/30 | 23/30 | 23/30 |
Likert scale (1- Very poor, 2- Poor, 3- Acceptable, 4- Good, 5- Excellent).
DISCUSSION
The findings of our study give a gross heterogeneity in the drug-drug interactions between the various online data bases compared, which indicate that information related to drug-drug interaction in the data bases must be referring to different resources or evidences. High congruency in drug-drug interaction is found for some psychotropic medications like – escitalopram, citalopram, clomipramine, amitriptyline, Clozapine, Olanzapine, Ziprasidone, Que-tiapine, Lamotrigine, Haloperidol, Trihexyphenidyl, Acam-prosate and Alprazolam. It might be due to extensive research exiting on these drugs, and consistent pattern of drug-drug interactions reported across the researches.
Our findings included significant incongruity between different databases similar to previous studies [12,13]. Ritonavir being a pan CYP inducer had the maximum moderate to severe drug interactions reported, similar to another study on comparison of antipsychotic drugs with COVID-19 medications [12]. The most reliable databases for checking psychotropic drug interactions with COVID- 19 drugs (used in the 1st wave) was Liverpool© Drug Interaction Group and Lexicomp. Overall, Lexicomp had a wider and more comprehensive database at present with a high SCOPE score, which can be easily used by healthcare professionals. Our findings are further strengthened by other similar studies addressing drug-drug inter-actions. However, it had discrepancy with other databases due to infrequent updates of the available studies on the subject, along with a subscription cost associated with it.
The Liverpool© Drug Interaction Group has also developed separate software for addressing other important drug interactions. It uses GRADE (Grading of Recommen-dations, Assessment, Development, and Evaluations) recommendations for classifying the available studies on the interactions, classifies most of the clinically important ones and provides freely accessible pdf for each drug interaction checked. However, it also faces the drawback of frequently missing or unavailable data. If it is updated rigorously, it can prove to be the most comprehensive drug interaction database for free use by both healthcare professionals and pharmacists.
For patients, Drugs.com can serve as an efficient alternative which not only details on the drug interactions in a simple language but also warns against red flag symp-toms.
This study has several implications for healthcare professionals, care givers, patients, and pharmacists. For healthcare professionals including consultants, residents, and nurses, it is imperative to grade and classify the information available freely through these databases. In most of the low and low- and middle-income countries, the provision of a standardized institutional access database like Stockley’s drug interactions in the UK and the USA is limited. The high individual out-of-pocket subscription costs are prohibitionary to its widespread use especially by residents and interns. Finding the needful interactions in standard textbooks available for reference like is difficult due to the adoption of organ-system based classification and infrequent updates.
For ease of availability and accessibility along with the lack of knowledge regarding standard references, care givers and patients use these online freely available data-bases. However, the most widely used resources like Medscape and WebMD do not refer sources which undermines their authenticity as evident by our study as well.
For trained pharmacists, it is also imperative to keep themselves abreast of the recent studies in the field and rely on their practicing knowledge. Pharmacists are not available in several resource limited settings and incorrect prescription of drugs due to constraints of time and know-ledge leads to life-threatening reactions which could be prevented by using the most updated database.
The limitations of our study include assessment of the drug-drug interactions (DDI) cross-sectionally across the available databases and exclusion of paid databases for which we did not have institutional access. Apart from Liverpool© Drug Interaction Group, we did not classify the available references based on GRADE recommen-dations. The use of online database can prove beneficial but the lack of agreement/congruity between the different databases effects its reliability. While using online databases, healthcare workers should use the most comprehensive and reliable database available.
In conclusion, there was significant variability in the recommendations available on different databases regarding concomitant prescribing of psychotropic medications with drugs used during first COVID wave. Ritonavir reported the maximum drug interactions with most of them graded as severe. The freely accessible software Liverpool© Drug Interaction Group developed by University of Liverpool was one of the most reliable databases but had the drawback of frequently missing data on several drugs. Lexicomp had the most comprehensible database but had significant variability than other databases due to limited updates. Drugs.com was fairly reliable and easy to understand tool for patients. WebMD and Medscape were the least reliable sources.
Funding Statement
Funding None.
Footnotes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: Sujita Kumar Kar. Data acquisition: Surobhi Chatterjee, Sujita Kumar Kar, Aathira Jaya Prakash, Teena Bansal, Garima Singh. Formal analysis: Surobhi Chatterjee, Sujita Kumar Kar. Supervision: Sujita Kumar Kar. Writing—original draft: Surobhi Chatterjee, Sujita Kumar Kar. Writing—review & editing: Surobhi Chatterjee, Sujita Kumar Kar, Aathira Jaya Prakash, Teena Bansal, Garima Singh.
References
- 1.van Roon EN, Flikweert S, le Comte M, Langendijk PN, Kwee-Zuiderwijk WJ, Smits P, et al. Clinical relevance of drug-drug interactions: A structured assessment procedure. Drug Saf. 2005;28:1131–1139. doi: 10.2165/00002018-200528120-00007. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L, Zhang YD, Zhao P, Huang SM. Predicting drug-drug interactions: An FDA perspective. AAPS J. 2009;11:300–306. doi: 10.1208/s12248-009-9106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monteith S, Glenn T. A comparison of potential psychiatric drug interactions from six drug interaction database programs. Psychiatry Res. 2019;275:366–372. doi: 10.1016/j.psychres.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 4.Kar KS, Yasir Arafat SM, Kabir R, Sharma P, Saxena SK. Coping with mental health challenges during COVID-19. In: Saxena SK, editor. Coronavirus disease 2019 (COVID-19): Epidemio-logy, pathogenesis, diagnosis, and therapeutics. Springer; Singapore: 2020. pp. 199–213. [DOI] [Google Scholar]
- 5.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharma-cologic treatments for coronavirus disease 2019 (COVID-19): A review. JAMA. 2020;323:1824–1836. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 6.Drugs interaction checker- find interactions between medications [Internet] WebMD LLC.; 2020. [cited at 2022 Mar 26]. https://www.webmd.com/interaction-checker/default.htm. [Google Scholar]
- 7.Drugs interaction checker- medscape drug reference database [Internet] WebMD LLC.; 2020. [cited at 2022 Mar 26]. https://reference.medscape.com/drug-interactionchecker. [Google Scholar]
- 8.Lexicomp: Evidence-based drug referential content [Internet] Wolters Kluwer; 2020. [cited at 2022 Mar 26]. https://www.wolterskluwer.com/en/solutions/lexicomp. [Google Scholar]
- 9.Wishart DS, Feunang YD, Guo AC, Lo EJ, Marcu A, Grant JR, et al. DrugBank 5.0: A major update to the DrugBank database for 2018. Nucleic Acids Res. 2018:D1074–D1082. doi: 10.1093/nar/gkx1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prescription drug information, interactions & side effects [Internet] Drugs.com; 2020. [cited at 2022 Mar 26]. https://www.drugs.com/ [Google Scholar]
- 11.Liverpool COVID-19 interactions [Internet] University of Liverpool; Liverpool: 2020. [cited at 2022 Mar 26]. https://www.covid19-druginteractions.org/ [Google Scholar]
- 12.Plasencia-García BO, Rodríguez-Menéndez G, Rico-Rangel MI, Rubio-García A, Torelló-Iserte J, Crespo-Facorro B. Drug- drug interactions between COVID-19 treatments and antipsychotics drugs: Integrated evidence from 4 databases and a systematic review. Psychopharmacology (Berl) 2021;238:329–340. doi: 10.1007/s00213-020-05716-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitry AI. Comparative assessment of four drug interaction compendia. Br J Clin Pharmacol. 2007;63:709–714. doi: 10.1111/j.1365-2125.2006.02809.x. [DOI] [PMC free article] [PubMed] [Google Scholar]